Abstract
Hypoxia triggers complex inter- and intracellular signals that regulate tissue oxygen (O2) homeostasis, adjusting convective O2 delivery and utilization (i.e., metabolism). Human populations have been exposed to high-altitude hypoxia for thousands of years and, in doing so, have undergone natural selection of multiple gene regions supporting adaptive traits. Some of the strongest selection signals identified in highland populations emanate from hypoxia-inducible factor (HIF) pathway genes. The HIF pathway is a master regulator of the cellular hypoxic response, but it is not the only regulatory pathway under positive selection. For instance, regions linked to the highly conserved Notch signaling pathway are also top targets, and this pathway is likely to play essential roles that confer hypoxia tolerance. Here, we explored the importance of the Notch pathway in mediating the cellular hypoxic response. We assessed transcriptional regulation of the Notch pathway, including close cross-talk with HIF signaling, and its involvement in the mediation of angiogenesis, cellular metabolism, inflammation, and oxidative stress, relating these functions to generational hypoxia adaptation.
Keywords: hypobaric hypoxia, adaptation, Notch signaling, hypoxia-inducible factor
1. Introduction
Maintenance of an adequate oxygen (O2) supply is fundamental to cellular homeostasis and is challenged by impaired cellular O2 availability (hypoxia). Adjustments involving all points of the O2 cascade, from delivery to cellular usage, are crucial under hypoxic conditions, including disease states that impact the heart, lungs, and circulation across various life stages. Hypoxia can also be experienced upon exposure to high-altitudes, where barometric pressure falls and so the partial pressure of O2 falls. Despite this hypoxic stress, human populations have resided at altitudes above 3000 m in Tibet, Ethiopia, and the Andes for thousands of years. Over this time, natural selection of multiple gene regions and adaptive physiological traits has occurred [1,2,3,4]. Understanding the genetic variants under selection in these populations, and in other species with multigenerational exposure to hypobaric hypoxia, provides insight into mechanisms critical for tolerance and ultimately survival in hypoxia in all contexts [5].
The hypoxia-inducible factor (HIF) pathway is essential in the cellular hypoxic response. In normoxia, HIF-1α and HIF-2α are hydroxylated by the prolyl-hydroxylase (PHD) enzymes and so are targeted for ubiquitination by the von Hippel–Lindau (VHL) protein and degradation by the proteasome [6]. In conditions of low cellular PO2, HIF-1α/HIF-2α are stabilized, forming heterodimers with the nuclear-localized HIF-1β, and bind hypoxia response elements (HREs) in the promoter regions of hundreds of target genes [7,8]. Activation of the HIF pathway thus elicits a vast array of cellular responses in an O2-dependent manner. This includes genes that mediate O2 delivery, such as erythropoietin (EPO) and vascular endothelial growth factor (VEGF), which support O2 carriage and angiogenesis, respectively [9,10]. Beyond O2 delivery, the HIF pathway regulates cellular O2 utilization by targeting a plethora of metabolic genes, with the effect of enhancing glycolysis and lactate production [11] and attenuating fatty acid oxidation through suppression of peroxisome proliferator-activated receptor α (PPARα) [12,13].
HIF pathway genes play a key role in hypoxia adaptation in high-altitude populations. Genetic variation within the region of EPAS1 (encoding HIF-2α) and EGLN1 (encoding PHD2) have been identified across numerous studies of high-altitude adaptation [3,14,15], in addition to HIF-targeted genes such as PPARA [3] and non-HIF-related targets [2].
Whilst the HIF pathway is undoubtedly an essential mediator of the cellular response, adaptation to hypoxia is polygenic. The interplay of HIF with other genes known to be under selection, as well as those independent of the HIF pathway, are an important area under investigation. One such example is the highly conserved Notch signaling pathway, which functions in many different developmental and homeostatic processes, mediating a strikingly diverse range of downstream signals [14]. In this review, we provide a general overview of the Notch pathway and the studies that have identified NOTCH as a target of hypoxia adaptation. We further delve into the mechanisms by which the Notch pathway mediates cellular responses, and provide insight into its roles within the context of high-altitude adaptation.
2. Canonical Notch Signaling
Evolutionarily, Notch signaling is a highly conserved pathway that mediates communication between neighboring cells to regulate many developmental and homeostatic processes in metazoans. Upon ligand-mediated activation, Notch receptors form a complex that promotes transcription of target genes, leading to regulation of essential processes including cell proliferation and differentiation.
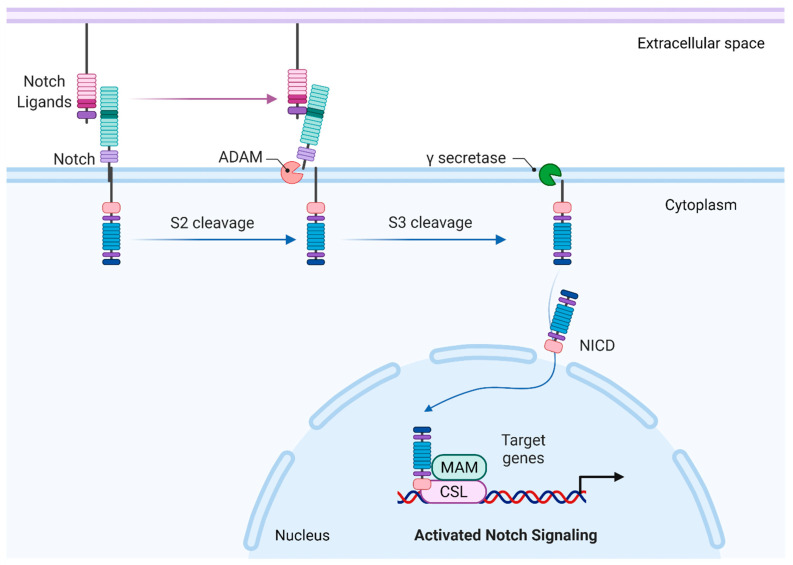
Notch receptors are large single-pass transmembrane proteins composed of an N-terminal extracellular subunit, a C-terminal transmembrane, and an intracellular subunit. Canonical transmembrane Notch ligands belong to the Delta–Serrate–LAG2 (DSL) family. Ligand binding to the extracellular region involves the DSL and amino-terminal domains, which contact epidermal growth factor (EGF)-like repeats 11–12 [15,16]. This exposes the cleavage site for S2 cleavage catalyzed by a disintegrin and metalloprotease (ADAM) family of metalloproteases, rendering the transmembrane-intracellular fragment as a substrate for S3 cleavage by the γ-secretase complex, which catalyzes intramembrane proteolysis, resulting in the release of the Notch intracellular domain (ICD). The Notch ICD comprises a membrane proximal RBP-Jk-associated molecule (RAM) region and an ankyrin repeat domain (ANK), both of which interact with the DNA-binding protein CBF1/Suppressor of Hairless/LAG1 (CSL; also known as RBPJ) and the coactivator Mastermind (MAM) to form a transcriptional complex that promotes the expression of target genes [17,18,19,20]. The Notch ICD also contains a nuclear localization sequence, located between the ANK and C-terminal proline/glutamic acid/serine/threonine-rich (PEST) domain. Termination of the active Notch ICD signal is mediated through ubiquitination of degron sites on the PEST domain and subsequent degradation by the proteasome [19]. A simplified overview of canonical Notch signaling is presented in Figure 1.
Figure 1.
A simplified view of canonical Notch signaling. Summary of the core signaling pathway created with BioRender.com. Canonical Notch ligands bind to the Notch receptors at epidermal growth factor (EGF) repeats 11–12 (dark green sections). Cleavage of the Notch receptor involves two proteolytic cleavage events, the first catalyzed by ADAM metalloproteases at the negative regulatory region (purple sections), the second by γ-secretase. This releases the Notch intracellular domain (NICD). In the nucleus, NICD interacts with DNA binding protein CBF1/Suppressor of Hairless/LAG1 (CSL; also known as RBPJ) and the coactivator Mastermind (MAM) to promote gene transcription.
The output from canonical Notch signaling is enormously diverse and cell-context-dependent, operating in both physiological and pathological states. Activation of Notch signaling can promote cell growth and cancer development in some contexts, but cell death and tumor suppression in others [14]. Studies applying chromatin immunoprecipitation analysis provide insight into the wide array of genes regulated by Notch pathway signaling [21,22]. Notch ICD/CSL target genes include those related to cell-fate determination (HES1 [23] and HEY1 [24]), proliferation (MYC [25]), growth arrest (p21 [26]), cancer stem cell markers (CD44 [27], BMI1 [28]), and Notch signal potentiation (NOTCH3 [25]).
Despite this diversity in outputs, the cascade to activation and downstream signaling is relatively simple, involving the receptor–ligand interactions described to release the bioactive Notch ICD, with no intermediates from which signal amplification can occur. There is also limited diversity within the pathway components, with mammals possessing four Notch paralogues (Notch1–4) and various ligands in the Delta-like (DLL1, DLL3, and DLL4) and jagged pathways (Jagged1, Jagged2). Drosophila melanogaster possesses one Notch receptor and two ligands, the transmembrane proteins Delta and Serrate [14]. The plethora of downstream signals is therefore derived from regulatory mechanisms including ligand-expression patterns, pathway crosstalk, tissue topology, and the nuclear environment [14]. An example of a regulatory mechanism is the post-translational modification of the Notch receptor through addition of N-acetylglucosamine to O-fucose residues located in certain EGF repeats by Fringe family glycosyltransferases [29]. This modification alters relative affinity of ligand–Notch binding [30], leading to activation of Notch in response to Delta-like ligands, but suppression of downstream signaling for Serrate/Jagged ligands [31].
The cellular context for Notch signaling assessed in this review is hypoxia. Whilst interactions between the Notch pathway and the cellular hypoxic response are extensive [32], much of this interaction is related to cancer pathogenesis. Here, we considered Notch signaling in hypoxia through the lens of high-altitude adaptation. We begin by summarizing the evidence to show that genetic regions encoding Notch pathway proteins are under positive selection in hypoxia-adapted populations, and highlight research showing that this pathway is critical for conferring hypoxia tolerance.
3. Notch under Positive Selection
In humans, natural selection of Notch has taken place in highland native Andean and Tibetan populations. Investigations using locus-specific branch-length testing of single-nucleotide polymorphism (SNP) data have revealed positive selection for NOTCH1, alongside numerous HIF pathway candidate genes, in Andeans living above 3600 m [33]. Examination of the chromatin accessibility and transcriptional landscape in Tibetans residing at 3680 m, performed using human umbilical vein endothelial cells (HUVECs), identified two structural variants within the upstream regulatory element of NOTCH1 (chr9:139420177-139429697, 67,694 bp) [34]. These variants, including a 200 bp duplication in chr9:139422831-139423031 and a 1200 bp duplication in chr9:139429296-139430493, were suggested to increase the accessibility of this regulatory element, and so to affect NOTCH1 expression [34]. This finding was made alongside the identification of active regulatory elements cooperating to downregulate expression of EPAS1, encoding HIF-2α [34].
Positive selection of Notch signaling has also been identified in highland populations of some nonhuman species. For example, in Tibetan chickens, whole-genome resequencing identified NOTCH2 as being under positive selection [35], whilst transcriptomic and proteomic analyses revealed enrichment of Notch signaling, specifically differential expression of NOTCH2 [36]. In the Tibetan pig, transcriptome analysis revealed differential expression in RBPJ (CSL), coding a crucial component of the Notch ICD transcriptional complex [37]. In a Tibetan yak, ADAM17 was identified as under selection [38]. NOTCH1 is a substrate for this metalloprotease, and it has been linked to regulation of ligand-independent Notch signaling [39]. The Notch1 pathway function is upregulated in an ADAM17-dependent manner in liver cancer stem cells [40]. However, its relevance in physiological conditions remains controversial, and unlike ADAM10, is reported to be dispensable for Notch activation [41].
These findings are in line with studies highlighting the importance of the Notch system in conferring hypoxia tolerance, a concept explored extensively in Drosophila melanogaster. Through generations of laboratory selection, a hypoxia-tolerant strain of Drosophila has been generated that is capable of survival in normally lethal O2 levels (4% O2) [42]. Examination of gene-expression profiles revealed upregulation of components in the Notch signaling pathway [42,43,44] alongside downregulation of genes encoding glycolytic, tricarboxylic acid (TCA) cycle, and β-oxidation enzymes [42]. The broad suppression of metabolic targets was coordinated by the Notch target transcriptional suppressor hairy, the mammalian homologue of which is HES (hairy and enhancer of split-1). Binding elements for hairy were located on the genes shown to be downregulated, with binding specifically occurring in hypoxia. Loss-of-function hairy mutants abolished the metabolic gene suppression, reducing hypoxia tolerance [42]. The importance of Notch signaling in this response was confirmed through application of a γ-secretase inhibitor, which significantly reduced survival and life span in hypoxia [44].
This evidence, summarized in Table 1 and Table 2, suggests Notch signaling is an important factor in hypoxic adaptation. However, the downstream effects of variants under positive selection at high-altitude are yet to be explored. To gain insight into potential avenues of interest when considering Notch genotype–phenotype interaction at high-altitude, we delved into the current understanding of Notch involvement in the cellular hypoxic response from the point of gene transcription, including interplay with the HIF pathway, to regulation of angiogenesis and vascular tone, metabolism, inflammation, and oxidative stress. The interplay of Notch with established hypoxia response pathways is summarized in Table 3.
Table 1.
Notch under selection at high-altitude.
| Subjects/Species | Highland/Hypoxic Location | Altitude (m) | Data Format | Test for Natural Selection | Positively Selected Notch Gene/Region | Reference |
|---|---|---|---|---|---|---|
|
Human, Andeans (n = 50) |
Cerro de Pasco, Peru (Quechua) La Paz, Bolivia (Aymara) |
4300 3600 |
SNP genotype, Affymetrix, Inc. Gene Chip Human mapping 500 k array | Locus-specific branch length for SNP loci | NOTCH1 | [33] |
|
Human, Tibetans (n = 131) |
Lhasa, Tibet | 3680 | Chromatin accessibility landscape through paired ATAC-seq and RNA-seq, obtained from primary HUVECs | Variant interpretation model by paired expression and chromatin accessibility methodology to identify active selected regulatory elements | NOTCH1 regulatory element | [34] |
| Chicken, Tibetan (n = 9) | Xiangcheng County, Tibet | 3500 | Whole genome resequencing | Aligned to reference genome using SOAP2, detected short InDel and structure variants | NOTCH2 | [35] |
|
Pig, Tibetan (n = 2) |
Diqing Tibetan autonomous prefecture, Yunnan province | 3500 | Lung tissue whole-transcriptome microarrays | Differential gene expression, regulatory and phenotypic impact factor analysis | RBPJ (CSL) | [37] |
| Yak, Tibetan (n = 1) | Huangyuan County, Qinghai province | 3700 | Short oligonucleotide analysis | Whole-genome shotgun assembly | ADAM17 | [38] |
Table 2.
Notch involvement in hypoxia tolerance in laboratory experiments.
| Species | %O2 | Duration of Hypoxia Exposure | Data Format | Test for Natural Selection | Positively Selected Notch Gene/Region | Reference |
|---|---|---|---|---|---|---|
| Drosophila (n = 100) | 5% O2 | 1 week | P-element insertion line screen | Genomewide screening of P-elements related to eclosion rate, rtPCR on selected P-element targets | Dip1, CG14782, mRpS18B, Mys45A, CG6230, Drp1, Rep2, osa, CG8116, Atg1, CG33169, Chro, pzg, polo, lqf, Scrib, Alh, tna, CG14185, ci | [43] |
| Drosophila (n = 200, derived from 27 parental strains) |
6% and 4% O2 | 3 weeks for Notch mutants | Whole genome re-sequencing | Aligned to reference genome using MAQ, identified loci with high-confidence allelic differences and regions with allelic frequency differences | Fixed SNPs/indels: Notch, Delta, Fringe, Sgg Hairless, HDAC4, Fur2, Bon, IP3K2, Nej, Pcaf, Change in gene regulation: E(spl) Cluster Genes, Aph-1, Nct, Ser. |
[44] |
| Chicken, Tibetan (n = 9) | 13% O2 | 11 days | Transcriptomic and proteomic analysis of embryos | Differentially expressed protein. | NOTCH2 | [36] |
Table 3.
Notch involvement in physiological responses to hypoxic exposure.
| Hypoxic Physiological Response | Related Signaling Factors | References | Notch Pathway Interplay | Effect of Notch Interplay | Model/Condition | References |
|---|---|---|---|---|---|---|
| Modification of gene transcription | HIF-1α, HIF-2α | Reviewed in [6] | Notch ICD | Recruitment of HIF to HREs | Mouse myogenic and embryonic teratocarcinoma cells, hypoxia (1% O2) | [45,46] |
| DLL4, HEY2 | Notch pathway activation | Mouse myogenic and embryonic teratocarcinoma cells and human epithelial and embryonic kidney cells, hypoxia (1% O2) | [46,47] | |||
| γ-Secretase complex | Enhanced cleavage of Notch ICD | Human epithelial and breast cancer cells, hypoxia (NiCl2 and 1% O2) | [48,49] | |||
| Factor inhibiting HIF (FIH) | [50] | Notch ICD | Cellular differentiation | Mouse myogenic and embryonic teratocarcinoma cells, hypoxia (1% O2) | [45,46] | |
| Mindbomb 1 and 2 | Angiogenesis | Zebrafish embryos | [51] | |||
| DNA methylation | [52,53] | NOTCH1, NOTCH3, DLL1 | Notch pathway expression | Rat hepatic stellate cells and human gastric cancer cells | [54,55] | |
| CSL (or RBP-J) | Methylation-dependent DNA binding | Human leukemia cells | [56] | |||
| Angiogenesis | HIF via VEGF | Reviewed in [57] | Notch via DLL4 and Jagged1 | Differential VEGFR expression for selection of tip and stalk cells | Mouse embryo | [58,59] |
| Increased vascular tone | Pulmonary vascular remodeling | [60] | Notch3 pathway | Smooth muscle cell proliferation in small pulmonary arteries | Human and rodent pulmonary hypertension | [61] |
| Increased intracellular Ca2+ | Reviewed in [62] | Notch3 pathway | Upregulation of TPRC channels and increased expression of the Ca2+-sending receptor | [63,64] | ||
| Loss of insulin sensitivity | Increased plasma glucose and insulin | [65,66] | Notch ICD via FoxO1 | Insulin resistance, increased glucose-6 phosphatase expression | Mouse liver, normoxia | [67] |
| Upregulated glycolysis | HIF via PDK | [68] | Notch via PI3K/AKT serine/threonine kinase | Increased glucose uptake, and upregulation of glycolytic genes | Human breast cancer cells and Drosophila | [69,70] |
| Notch via p53 | Glycolytic dependency, suppressed mitochondrial activity | Human breast cancer cells | [69] | |||
| Glutamine metabolism | HIF-2α | [71] | Notch1 pathway | Decreased glutamine consumption and expression of glutaminase, ornithine aminotransferase and glutamine dehydrogenase 1 | Human immortalized leukemia cells and T lymphocytes | [72] |
| Loss in mitochondrial density | HIF via PGC1α | [73,74] | HES1 | Suppressed PGC1α | Mouse adipocytes | [75] |
| Suppressed respiratory complex I | HIF via mir-210 | [76] | Notch1 pathway | Decreased complex I activity and subunit expression | Breast cancer and immortalized leukemia cells | [72] |
| Complex IV subunit switch | HIF | [77] | Notch1 via p53 | Downregulated CIV | Breast cancer | [32] |
| Suppression of β-oxidation | HIF, PPARα | [3,12,78] | Notch1 pathway | Notch1 pathway inhibition increased PPARA and CPT1 expression | Mouse models of Notch deficiency, liver and adipose | [75,79] |
| Inflammation | HIF, NF-kB | [65,80,81,82] | Notch ICD | Interaction with NF-kB subunit | Human T cells | [83] |
| Oxidative stress | ROS via HIF, NF-kB, Nrf2 | [84,85,86] | Notch1 via Nrf2 | Increased cell viability, reduced ROS formation, increased antioxidant activities | Neonate rat myocardial cells, hypoxia–reoxygenation | [87] |
| Notch1 via JAK2/STAT3 | Activated mitochondrial SOD expression and decreased ROS production | Rat myocardium, burn injury | [88] |
4. Gene Transcription
4.1. Notch and HIF Cross-Talk
A multitude of evidence has demonstrated involvement of the Notch pathway in the transcriptional response to hypoxia, both up- and downstream of Notch ICD activation [32]. Upstream, the expression of Notch ligands Jagged2 [89,90] and Delta-like Ligand 4 (DLL4) [91] are upregulated in hypoxia. Downstream of Notch ICD activation, hypoxia induces expression of NOTCH1 and targets such as HES1, as shown initially in human neuroblastoma cells cultured in 1% O2 [92]. Examination of mouse myogenic (C2C12) and neural precursor (P19) cells revealed a Notch1-dependent block on differentiation in hypoxia (1% O2), accompanied by the upregulation of Notch target genes HES1 and HES2 [46]. This effect was reversed with the use of an γ-secretase inhibitor, indicating Notch cleavage was essential for maintaining the undifferentiated cell state in hypoxia [46]. Direct interaction between HIF and Notch signaling was shown to be crucial in mediating this hypoxic cellular response.
An interaction interface between HIF-1α and Notch1 ICD was identified on the N-terminal region of HIF-1α, yet hypoxia-dependent activation of Notch signaling was shown to require the C-terminal region of HIF-1α [46]. Elsewhere in the Notch system, HIF-1α and HIF-2α interact with the promoters of Notch ligand DLL4 and Notch targets HEY1 and HEY2 [46,47]. HIF-1α also interacts with the γ-secretase complex, leading to enhanced cleavage of the Notch ICD, and so Notch activation. The HIF- γ-secretase complex interaction occurs via the promoter region of subunit APH-1A in HeLa cells [48], but via the enzymatic component PS1 in breast cancer cells [49].
HIF–Notch interaction is bidirectional, as the Notch system has also been shown to mediate various components of the HIF pathway. Notch ICD activation increased recruitment of HIF-1α to the HRE-containing region of hypoxic-responsive genes GLUT1, EPO, and VEGF [45,46]. Notch ICD activation also upregulates HIF-2α at the transcriptional level, coinciding with increased expression of target genes VEGF and AREG, yet this interaction did not involve the HIF-2α proximal promoter [93]. In human medulloblastoma and breast cancer cell lines, the Notch-mediated upregulation of HIF-2α was accompanied by downregulation of HIF-1α, which the authors postulated may drive the potential transition from shorter-term HIF-1α supported responses to hypoxia to the more sustained responses characterized by HIF-2α signaling [93].
Cross-talk between the Notch and HIF pathways extends to regulators of HIF signaling, including interaction between factor inhibiting HIF (FIH)-1 with Notch ICD [46]. FIH is an asparaginyl hydroxylase that acts at residue 803 of HIF-1α to block HIF coactivator binding [50]. FIH-1 hydroxylates the Notch ICD at two conserved asparagine residues (N1945 and N2012) [45,94], binding with a higher affinity than it does to HIF-1α [45]. This binding negatively regulates Notch ICD activity, abrogating the Notch-mediated repression of neuronal and myogenic differentiation [45]. Interaction with FIH extends to other components of the Notch system, including E3 ubiquitin ligases Mindbomb 1 and 2 required for Notch activation [51,95], whilst in zebrafish, FIH mediates the antiangiogenic function of Mindbomb via VEGF-A [51]. Finally, an interaction was demonstrated between Notch 3 and the HIF pathway regulator VHL in breast carcinoma cells [96].
These studies indicated that the transcriptional response to hypoxia involves close interaction between the HIF and Notch pathways. The actions of both are therefore considered throughout the remainder of this review.
4.2. Epigenetic and Post-Transcriptional Modifications
In hypoxia, both epigenetic events and post-transcriptional modifications, including splice variation and the action of microRNAs, are crucial in the regulation of HIF and Notch signaling systems.
4.2.1. Methylation
Epigenetic processes have been described as a central hub that connects environmental, physiological, and genomic inputs [97]. DNA methylation is an epigenetic modification that regulates chromatin organization and gene expression. The major site for DNA methylation in mammals is the cytosine-rich CpG dinucleotide, specifically at the 5′ position of the cytosine ring, mediated through the action of DNA methyltransferases (DNMTs). Whilst the vast majority of CpG sites across the human genome are methylated, interspersed among these are regions containing a high-density sequence of CpGs, or CpG islands, that often cluster within the promoter [98]. Hypomethylation of CpG islands most often enhances transcription-factor binding to activate gene expression, whereas hypermethylation often prohibits transcription-factor binding, leading to a quiescent chromatin state [99]. Global methylation status can be inferred through examination of long interspersed nuclear element-1 (LINE1) methylation, with decreased methylation being associated with genomic instability and cancer risk [100]. At high-altitude (above 4000 m), LINE1 methylation was greater in native Andean Quechua, compared with those of European ancestry [52,53]. In the lowlanders, this may be linked to increased reactive oxygen species (ROS) production (discussed below), as oxidative stress is associated with impaired methylation capacity [101].
Epigenetic silencing through methylation occurs in genes crucial to HIF expression and stabilization. An Andean Quechua resident at 4388 m showed decreased EPAS1 methylation in comparison with those residing at sea level [52], whereas altitude exposure (4240 m) in subjects of European descent was associated with increased EPAS1 methylation [53]. In line with the lowlander response, increased methylation of EPAS1 has been observed in human renal tubule epithelial cells, occurring through the action of DNMT3a. This prevented the activation of HIF-2α and expression of downstream target genes, limiting the proliferative capacity of these differentiated cells under hypoxia [102]. Hypermethylation has also been observed on a CpG island within the 5′ region of VHL in human renal carcinoma, leading to inactivation [103].
Methylation affects the binding of HIF to its target genes, as the consensus core HRE contains a CpG dinucleotide, and upon methylation, HIF-1 DNA binding is abolished [104]. Indeed, HIF-induced expression of EPO is reliant upon a methylation-free HRE [104,105]. Methylation of CpGs within the EPO promoter impair transcriptional activation and block association of nuclear proteins, and this was suggested to act in concert with the CpG island in the 5′-untranslated region (UTR), which recruited methyl-CpG binding to the promoter, together silencing the EPO gene [106]. At high-altitude, EPO methylation decreased in subjects of European ancestry with ascent from 1400 m to 4240 m, thus facilitating increased expression in support of the erythropoietic response [53]. Alterations in other HIF targets included increased methylation of PPARA with increasing altitude, potentially suppressing fatty acid oxidation capacity [53].
Notch signaling is itself also closely regulated through DNA methylation [107]. Expression of NOTCH1 and NOTCH3 were methylation-dependent in hepatic satellite cells (HSC) [54], whilst the transcription factor downstream of the Notch receptor RBP-J (or CSL) binds DNA in a methylation-dependent manner [56]. DNA methylation also impacts Notch ligands, with hypermethylation of the DLL1 promoter silencing expression in gastric cancer cells [55]. Treatment with a methylation inhibitor 5-aza-2′deoxycitidine resulted in increased DLL1 expression and activation of the Notch cascade, including the downstream target HES1 [55]. However, methylation is not always linked to expression of Notch pathway genes, as exemplified by JAG2, whereby methylation pattern of the promoter did not correlate with expression [108].
4.2.2. Alternative Splicing
Alternative splicing of pre-mRNA increases transcriptomic and proteomic diversity by enabling the generation of multiple mRNA products from a single gene. Hypoxia is reported to drive intron retention above other splicing methods [109], and this may influence the fine tuning of both the HIF and Notch signaling systems.
Cassette exon skipping leads to several splice isoforms of HIF-1α [110,111,112], with the majority of isoforms conferring downregulation of HIF function [113]. An example is HIF-1α736, which lacks the C-terminal transactivation domain and displays a 3-fold lower activity than the full-length HIF-1α [111]. Conversely, HIF-1α417, which results from the skipping of exon 10, lacks a transactivation domain, yet promotes the nuclear translocation of HIF-1β, amplifying transcription of EPO [112]. Splice variation can also impact on factors interacting with HIF, such as peptidyl prolyl isomerase-1 (Pin1), a cis/trans isomerase that binds and stabilizes HIF-1α. Specifically, PIN1 transcript variant 2, identified as a long noncoding RNA, downregulated HIF-1α under hypoxia [114].
Multiple genes with characteristics of splice regulators display HIF1-α-dependent expression patterns, of which C1QBP, HNRNPH3, JMJD6, and SF3B1 contain HREs within their promoters [115]. In myocardial hypoxia, regulation of splice factor 3b subunit 1 (SF3B1) by HIF-1α was shown to mediate the splicing of ketohexokinase (KHK) pre-mRNA, switching KHK-A for KHK-C. KHK-C displays a superior affinity for fructose, and this switch enforced fructolysis, a metabolic shift crucial for pathological growth [115]. Hypoxia-induced alternative splicing also impacts the regulation of glycolysis through HIF-1α-mediated splicing of glycolytic enzymes Hk1 and Pfkfb3 in myocardial hypoxia [115], as well as differential regulation of lactate dehydrogenase (LDHA) variants through intron retention in breast cancer cells [109]. In the context of both cancer [116] and myocardial infarction [117], a switch in the expression of pyruvate kinase isoforms occurs, with the embryonic isoform PKM2 being re-expressed above the level of the adult isoform PKM1. This was mediated through RNA binding proteins and sequence-specific splicing repressors hnRNAP1 and hnRNAP2, and was linked to the promotion of aerobic glycolysis [116,117]. PKM2 acts in a positive feedback loop through interaction with PHD-3 to promote HIF-1α transactivation and reprogram glucose metabolism [118].
Alternative splicing of components of the Notch signaling system has been investigated extensively in the context of chronic lymphocytic leukemia (CLL), where Notch1 and 2, along with ligands Jagged1 and 2, are constitutively expressed [119]. Recurrent ‘noncoding’ mutations were clustered at the 3′-UTR region of NOTCH1 in ~2% of patients with CLL or monoclonal B-cell lymphocytosis, with the most common being located at chr9:139390152 [120,121]. These mutations were characterized by within-exon splicing, and were predicted to remove the PEST domain of Notch1, constitutively activating downstream signaling [120]. In some instances, noncoding variants occurred alongside mutations in the splicing factor SF3B1 [121], which increased Notch signaling through an alternate splice variant of the Wnt pathway member DVL2 [122].
4.2.3. MicroRNA
MicroRNAs (miRs) are a class of noncoding RNAs with a functional ~20–22 nt sequence that targets mRNAs, thereby inducing translational repression or RNA degradation [123]. Again, this method of modification interacts with both the HIF and Notch signaling systems.
HIF-1α enhances the induction of miR-210, the targets of which include regulators of mitochondrial respiratory function, as shown through alterations in placental metabolism [76], DNA repair, cell survival, and angiogenesis [124]. On the latter, induction of miR-210 was linked to upregulation of the Notch1 protein, and in turn to stimulation of angiogenesis following cerebral ischemia [125]. In the trophoblast, miR-210 represses cytoplasmic polyadenylation element binding 2 (CPEB2), which is a negative regulator of HIF-1α translation, thus forming a positive feedback loop of HIF-1α induction [126].
Encoded within intron 4 of the Notch1 locus is miR-4673. Transcription of miR-4673 altered cell cycle function in breast cancer [127] and neurogenic [128] cells, involving indirect regulation of Notch function alongside β-catenin and p53, and this has been linked to loss of mitochondrial membrane potential and ROS generation in human carcinoma cells through targeting 8-oxoguanine DNA glycosylase 1 [129]. Proximal to the Notch1 locus is miR-4674, which regulates angiogenesis through interaction with p38 VEGF signaling in endothelial cells [130].
Cross-talk between epigenetic and post-transcriptional elements has also been noted. For instance, methylation of miR-34a was linked to the expression of Notch pathway genes (NOTCH1, NOTCH2, and JAG1) in cholangiocarcinoma cells [131], whilst changes in methylation pattern are known to alter inclusion levels of alternatively spiced exons [132].
The evidence thus suggests that the Notch pathway plays a key role in the regulation of transcriptional response to hypoxia at multiple levels. In addition, the Notch pathway is known to mediate numerous processes linked to cellular and tissue remodeling upon high-altitude exposure, including regulation of angiogenesis and vascular tone, metabolism, inflammation, and oxidative stress.
5. Hypoxic-Induced Cellular and Tissue Remodeling
5.1. O2 Delivery
5.1.1. Erythropoiesis
In most nonadapted individuals, high-altitude exposure induces the generation of red blood cells from hematopoietic stem cells (HSCs); i.e., erythropoiesis. Whilst this response increases O2 carriage capacity, in excess it can result in high blood viscosity. This impairs tissue blood flow and O2 delivery, and is a feature of chronic mountain sickness (CMS) [133]. In native highlanders, the erythropoietic response is variable. Andeans display elevated hemoglobin and hematocrit alongside a high prevalence for CMS [134,135]. The majority of Tibetan highlanders, however, maintain hemoglobin and hematocrit at levels comparable to those of populations living at sea level, and lower than many of their Andean counterparts for any given altitude [134,136]. In line with this, Tibetans present lower blood oxygen saturations [1] and are protected from the detrimental effects of polycythemia and a lower prevalence of CMS [135].
An essential mediator of erythropoiesis in hypoxia is the increased production of EPO from kidney interstitial cells, which binds erythroid progenitors in bone marrow, stimulating their survival, proliferation, and differentiation. HIFs directly regulate EPO expression and also impact iron metabolism in hypoxia [137,138]. In the Tibetan population, the decreased hemoglobin phenotype has been linked to a variant in EGLN1, which promotes HIF degradation [3,139], as well as putatively adaptive copies of EPAS1 and PPARA loci [3], the latter being a HIF target. However, HIF is not the only regulator of erythropoiesis, which is a multistage process mediated through complex intracellular networks involving coordinated gene expression by transcription factors, chromatin modifiers, and miRNAs [140]. Genes related to different stages of erythropoiesis have been identified in highland populations [141], such as SENP1, which has been associated with development of CMS in Andeans [142,143].
Notch signaling is crucial for regulating stem cells in various settings [144], including embryonic hematopoiesis [145]. For example, disruption of NOTCH1 and downstream signaling in the mouse embryo was shown to impair HSC formation [146,147]. However, the involvement of Notch signaling in HSC homeostasis post development is less clear. Multiple reports from gain-of-function experiments demonstrate increased Notch signaling enhanced self-renewal of HSCs [148]. Notch is also expressed in human bone marrow CD34+ hematopoietic precursors [149], and there is interplay between Notch and HSC regulatory factors, including parathyroid hormone and stem cell factor (SCF). Parathyroid hormone increased the levels of Jagged1 in the bone marrow, and hematopoietic cell growth was abrogated through γ-secretase inhibition [150]. SCF-induced expression of Notch2 and SCF-mediated expansion of primary erythroid precursors were linked to Jagged1 [151]. Blocking Notch2 signaling inhibited the proliferative effects of SCF [151]. However, evidence also implies Notch activity is dispensable in the maintenance of HSCs, as shown through blockage of canonical HSCs in adult bone marrow [152] and through low levels of Notch receptors in purified HSCs [153]. The relevance of Notch signaling in the regulation of erythropoiesis at high-altitude has not been explored, but warrants further investigation, particularly given the role of Notch in maintaining cells in the stem/progenitor state in hypoxia [46].
5.1.2. Angiogenesis
Adequate tissue perfusion is critical for maintaining O2 homeostasis. Adaptation of the vascular system to hypoxia includes angiogenesis, a process requiring upregulation of proangiogenic signals to mediate each stage of growth, from extracellular matrix re-modelling to tube formation [154]. Examination of native highland human populations and other species has shown angiogenic pathway genes to be under positive selection at high-altitude. For instance, gene network analysis revealed selection of integrin subnetworks in Tibetan and Sherpa populations [155], whilst assessment of SNP data revealed selection for VEGF in Andean populations [33]. In the Tibetan chicken, whole genome re-sequencing and comparative transcriptomic and proteomic analyses revealed strong selection for VEGF [35,36], whilst genome wide analysis of the Tibetan sheep identified selection of genes within the Ras/ERK signaling pathway [156]. At a tissue-specific level, assessment of protein expression in placentas of Andean pregnancies revealed lower levels of the antiangiogenic factor sFlt-1 (soluble fms-like tyrosine kinase) and a lower sFlt-1/placental growth factor (PLGF) ratio, alongside higher uterine artery blood flow and birthweight compared with European pregnancies at the same altitude (3600 m) [157]. This is in line with findings demonstrating graduated protection against reduced birthweight in high-altitude pregnancies in Andean mothers compared to those with European ancestry [158].
A multitude of proangiogenic factors have been identified as HIF targets, including VEGF, PLGF, and integrin [57]. HIF regulation of hypoxic proangiogenic signals has been implicated during development and both adaptive physiological and pathological states [57]. Notch signaling is also a key mediator of angiogenesis at all life stages, with disruption to this pathway impacting trophoblast invasion [159] and embryo development [160] through mature tissue function [161]. Angiogenic mediation via the Notch system has, to date, largely focused upon interplay with VEGF and the effects on vascular integrity.
The initiation of blood vessel branching during angiogenesis, termed sprouting, requires coordination of endothelial cell behavior with selection of a filopodia-rich leading tip cell and following stalk cells. This process is mediated through a tight interplay between the VEGF-A receptor VEGFR, the Notch ligands DLL4 and Jagged, and downstream Notch signaling [59,162]. Key to the selection of tip and stalk cells are differential VEGFR1 and VEGFR2 levels mediated via DLL4 [59]. High levels of DLL4 in endothelial tip cells activate Notch in adjacent stalk cells to downregulate VEGFR expression, suppressing the tip phenotype and instead enabling formation of the stable vasculature [163,164]. DLL4–Notch signaling is antagonized by Jagged1, which competes with DLL4 binding in cells expressing Fringe family glycosyltransferases, promoting endothelial sprouting and tip formation [58].
The Notch system is therefore critical for mediation of vascular integrity and homeostasis. Indeed, gene inactivation of either Notch1 or DLL4 is embryonic lethal due to deregulation of angiogenesis and the loss of artery–vein specification [160,165]. Notch signaling is also critical to the regulation of vascular function in numerous pathologies characterized by tissue hypoxia, including tumor angiogenesis [166]. Blockade of Notch/DLL4 enhanced hypoxia in mouse subcutaneous C6 tumors [167], and decreased tumor growth [167,168]. However, the effect of Notch blockade on tumor development is context-dependent, as activation of the Notch system in endothelial cells promotes metastasis in the lung [169], but represses metastasis in the liver [170].
To add to the complexity of angiogenic regulation, VEGF-A, alongside its receptors VEGFR1 and VEGFR2, exhibit splice variation, with differing effects on bioavailability, binding capacity, and downstream signaling [113,171]. For instance, activation of VEGF-A121 induced a reduced rate of VEGFR2 phosphorylation, resulting in impaired motility and sprouting in human endothelial cells [172]. Alternative splicing can also result in soluble isoforms of VEGFR1, which are largely similar through exon 13, but differ in the C-terminus, including sVEGFR1-i13. Regulation of sVEGFR1-i13 involves splicing factors SRSF2 [173] and U2AF65 [174] alongside the NOTCH1 signaling system, with differential regulation exhibited by the Jagged and DLL ligands [175].
5.1.3. Vascular Tone
Hypoxic exposure can lead to onset of pulmonary hypertension (PH). This disorder is prevalent in high-altitude populations [176], although evidence suggests Tibetans may be protected by displaying a lack of muscularization of pulmonary arteries and low hypoxic pulmonary vasoconstriction [177]. Notch signaling has been linked to the onset of this disorder, specifically via Notch3. Expression of Notch3 mRNA and Notch3 ICD were increased in lung tissue obtained from PH patients, mice with hypoxia-induced PH, and rats with monocrotaline-induced PH [61]. In mice, PH was prevented via homozygous deletion of Notch3 and administration of a γ-secretase inhibitor [61]. Expression of both Notch3 and target Hes-5 were confined to vascular smooth muscles within small pulmonary arteries, and were required for cell proliferation and development [61]. Notch3 signaling was associated with increased vascular resistance, characteristic of PH, through regulation of intracellular Ca2+, achieved via enhancing store-operated Ca2+ entry through upregulation of canonical transient receptor potential (TRPC) channels [63] and increased expression of the Ca2+-sending receptor [64].
Another pathology associated with vascular control and Notch signaling is pre-eclampsia, a major cause of maternal and fetal morbidity and mortality [178] that increases in prevalence at high-altitude [179,180]. This multisystem pregnancy disorder is characterized by hypertension, proteinuria, and placental hypoxia and dysfunction that is attributed to the shallow implantation and defective spiral artery remodeling [181]. Specifically, HIF-1α promotes invasion of human trophoblast cells and angiogenesis via Notch1, with upregulation of proangiogenic factors including endothelin receptor type B (ETBR) via activator of transcription 3 (STAT3) and VEGF [159]. This signaling was disrupted in patients with pre-eclampsia, with downregulation of placental HIF-1α, Notch1, and ETBR [159].
5.2. Cellular Metabolism
Hypoxia is a particular stressor on metabolic homeostasis, and specifically oxidative metabolism. In hypoxia, metabolic adjustments are required to sustain mitochondrial ATP production in the face of a reduced O2 supply and increased oxidative stress [12,65]. Metabolic remodeling is thus an essential component of the hypoxic cellular response [78,182]. This can be observed through proteomic [183,184] and metabolomic [12,166,168] analyses, which have demonstrated significant remodeling of metabolic pathways and tissue metabolites upon ascent to high-altitude.
Metabolic remodeling in the face of hypoxic exposure broadly includes modulation of insulin sensitivity, glycolysis, mitochondrial oxidative phosphorylation, and lipid oxidation. HIF is a well-established regulator of the metabolic hypoxic response, acting as a metabolic switch to optimize mitochondrial respiratory function [68,185]. Notch signaling is also a key modulator of metabolic homeostasis [186], with activation being associated with raised mitochondrial membrane potential alongside increased ATP/ADP and NADH/NAD ratios [72]. Whilst much of the evidence supporting this has been obtained in normoxia or in the context of cancer, it involves a multitude of metabolic targets and systems known to influence metabolic remodeling at high-altitude.
5.2.1. Glucose Homeostasis and Insulin Sensitivity
Hypoxic exposure impacts glucose handling via modulation of insulin sensitivity, which is in turn influenced by factors including ethnicity [187] and pathologies associated with nutrient excess and chronic inflammation [188]. The response in hypoxia appears to be dependent on degree and duration of exposure. Loss of insulin sensitivity has been reported with prolonged exposure to extreme altitude [65,66] and intermittent hypoxia [189], whereas shorter duration of moderate hypoxia improved insulin sensitivity in obese subjects [190]. Notch signaling has been linked to regulation of glucose uptake by liver and adipose tissue, with overactivation of the Notch system impairing insulin sensitivity [67,75,79]. In the liver, Notch signaling occurred in concordance with the transcription factor forkhead box protein O1 (FoxO1) via the Notch ICD, with Notch1 gain-of-function promoting insulin resistance and glucose-6-phosphatase expression in a FoxO1-dependent manner [67]. Notch activity in endothelial cells has been linked to the regulation of muscle insulin uptake via caveolae genes, with sustained Notch signaling lowering insulin sensitivity and increasing blood glucose; however, inhibition resulted in improved insulin sensitivity and improved glucose regulation [191].
5.2.2. Glycolysis
Downstream of glucose uptake, hypoxia is commonly reported to enhance anaerobic glycolysis and increase the production of extracellular lactate, which can itself be transported into cells for use as metabolic substrate. This effect has been observed upon high-altitude exposure in lowlanders [192], whilst enhanced capacity for lactate production was observed in Sherpa skeletal muscle through higher lactate dehydrogenase (LDH) enzyme activity [12]. Increased reliance upon glycolysis is a common observation in hypoxic animal models [193] and in pathological contexts, such as tumors or ischemic injury [194]. HIF mediates this response through upregulating genes that encode glycolytic enzymes [11], alongside a shunting of pyruvate toward lactate production through the upregulation of pyruvate dehydrogenase kinase [68,185]. Notch also mediates glycolytic function through two distinct mechanisms. The first involves hyperactivated Notch signaling via the phosphatidylinositol 3-kinase (PI3K)/AKT serine/threonine kinase pathway to upregulate glycolytic targets such as the enzyme hexokinase and glucose transporter 1, as seen in breast cancer cells [69] and Drosophila [70]. The second mechanism involves hypoactivated Notch signaling, leading to reduced p53 levels, which enhanced glucose uptake at the expense of suppressed mitochondrial activity [32]. The ability of the Notch pathway to act as a metabolic switch for glucose flux has further been demonstrated in macrophages, in which M1 macrophage activation was reliant on Notch1-dependent induction of pyruvate dehydrogenase phosphatase 1 expression, pyruvate dehydrogenase activity, and glucose flux into the TCA cycle [195].
5.2.3. Glutamine Metabolism
In hypoxia, the shift toward greater lactate production leads to the lack of reduced carbon for a functional electron transport chain, fatty acid synthesis, and ultimately cell proliferation [196]. An alternative carbon source is therefore sought in the form of glutamine [196,197]. Through an HIF-2α-dependent mechanism, reductive metabolism of glutamine to the TCA cycle intermediate α-ketoglutarate is redirected toward de novo lipogenesis via formation of the fatty acid palmitate [71]. This pathway has been implicated in high-altitude exposure, with increased expression of skeletal muscle glutamine synthetase [184]. Through proteomic analysis, activation of the Notch system was associated with decreased glutamine consumption alongside downregulation of three glutamate catabolism enzymes: glutaminase, ornithine aminotransferase, and glutamate dehydrogenase 1 [72].
5.2.4. Mitochondrial Network and Respiration
Suppression of mitochondrial function with hypoxic exposure can occur through multiple mechanisms, including regulation of the mitochondrial network. For instance, expression of mitochondrial biogenesis factor peroxisome proliferator-activated receptor gamma coactivator 1 alpha (PCG1α) declined in human skeletal muscle following prolonged exposure to extreme high-altitude [74], occurring alongside a loss of muscle mitochondrial volume density, particularly within the subsarcolemmal population [74,198]. PGC1α is mediated both by HIF [73] and also Notch, as the proximal promoter region of PGC1α contains a binding site for the Notch target HES1. Binding of Hes1 suppressed Pgc1α expression in mouse adipocytes, whilst deficiency of Notch1 led to elevated Pgc1α protein levels [75].
Specific alterations of the respiratory chain induced by hypoxic exposure include suppression of complex I, demonstrated in hypoxic rat heart [199], human skeletal muscle [184], and placenta [76]; whilst complex IV is altered through an HIF-mediated switch of subunits to optimize respiratory efficiency [77]. The Notch system should be considered in this context, as hypoactive Notch induces a decrease in complex I activity and in expression of the complex IV subunit COXII through p53 signaling in breast cancer [32]. Conversely, Notch1 hyperactivation has also been associated with downregulation of complex I subunits NDUFS1 and NDUFV2, as assessed through proteomic analysis of human immortalized leukemia cells (K562) [72].
5.2.5. β-Oxidation
Hypoxic exposure is associated with suppressed β-oxidation capacity [12,193], a response modulated by HIF through repression of the fatty-acid-activated transcription factor peroxisome proliferator-activated receptor α (PPARα) [12,78,194], with changes to its downstream targets including the mitochondrial transporter carnitine palmitoyl transferase (CPT) [12,193]. A putatively advantageous PPARA haplotype has been identified in Tibetans [3], and this was associated with metabolic adaptation in Sherpas at high-altitude [12].
Notch signaling has profound effects on the regulation of β-oxidation, although these are likely to be cell-context dependent. Notch1 deficiency has been associated with increased expression of Ppara and Cpt1 in liver [79] and adipose tissue [75]. Disruption of Notch signaling has been linked to browning of white adipose tissue, with higher metabolic rate dependent on increased uncoupling protein 1 expression and resistance to obesity induced by a high-fat diet [75]. Similarly in the liver, abrogated Notch signaling was associated with enhanced β-oxidation capacity, resulting in decreased hepatic lipid accumulation [79]. Notch signaling is positively correlated with fatty liver disease [200] and stimulation of lipogenesis has been linked to Notch-dependent stabilization of mammalian target of rapamycin complex 1 (mTORC1) [84]. The interaction with mTORC1 is bidirectional, as mTORC1 stimulated via excess amino acid consumption upregulates Notch1 signaling through STAT3 [201]. In leukemia cells, Notch activation was associated with increased levels of the β-oxidation enzyme mitochondrial enoyl-CoA hydratase [72].
5.3. Inflammation
Tissue hypoxia is known to augment inflammatory signaling. For instance, sustained exposure of lowlanders to high-altitude (6–8 weeks, >5300 m) led to a sharp rise in circulating interleukin (IL)-6, a target of the immune system regulator nuclear factor (NF)-kB [65]. NF-kB is of particular interest given its cross-talk with HIF [202]. This interaction involves amplification of NF-kB signaling through HIF binding Toll-like receptors [80] and enhanced HIF transcriptional activity through direct binding of the NF-kB precursor IkBα to FIH [81]. ROS-mediated upregulation of HIF-1α was shown to be dependent on NF-kB, and transfection experiments revealed an unidentified NF-kB binding element on the HIF-1α promoter [82]. HIF–NF-kB cross-talk has been implicated in diseases in which chronic hypoxia occurs concurrently with chronic inflammation, including cancer [203].
Regulation of NF-kB also involves complex cross-talk with Notch signaling at multiple points of each pathway [204,205], with physical interaction between the N-terminal portion of Notch ICD and NF-kB subunit p50 [83]. Cooperation of Notch with other immune system regulators includes interaction between Notch1 and transforming growth factor-β (TGFβ) in the maintenance of regulatory T cells through the transcription factor Foxp3 [206]. Indeed, Notch signaling is an important regulator of both the innate and adaptive immune responses and regulates immune cell development and function. This includes determination of cell lineage in developing lymphocytes and regulation of T- and B-cell differentiation and function [207], with Notch inactivation leading to accumulation of B cells in the thymus and blocking of T-cell development [206,208].
As with all aspects of Notch signaling, Notch regulation of immune system function is context-dependent [205]. In endothelial cells, Notch1 ICD activity in human carcinomas and melanoma orchestrated tumor progression and metastasis through increasing expression of chemokines and the adhesion molecule VCAM1, which promotes neutrophil infiltration and tumor cell adhesion [169]. In luminal endothelial cells derived from the aorta of coronary artery disease patients, upregulation of Notch pathway components at atherosclerotic lesions resulted in upregulation of inflammatory signaling, including IL-6 and ICAM1 and induction of endothelial cell senescence [209].
5.4. Oxidative Stress
ROS production is a key element of the cellular hypoxic response, involving multiple cellular sources, including mitochondrial complexes I and III. ROS signaling affects a multitude of downstream pathways, including HIF-1α, NF-kB, and nuclear factor erythroid-2 related factor 2 (Nrf2), with the latter being a regulator of genes that modulate oxidative stress, including GSTA2 and NQO1 [85,86,210,211]. An imbalance between ROS production and antioxidant capacity leads to oxidative stress, resulting in production of lipid and protein oxidation products. Markers of oxidative stress have been reported in lowland subjects ascending to high-altitude, leading to increased circulating isoprostanes [65] and increased skeletal muscle oxidized/reduced glutathione and sulfoxide/total methionine [12]. Of note, no such change was observed in an adapted Sherpa population following the same ascent profile [12]. Increased oxidative stress has been demonstrated in Andeans at high-altitude compared to lowlanders in normoxia [212,213]. This included elevated levels of circulating ascorbate free radicals alongside depressed antioxidants, an effect that was more pronounced in sufferers of chronic mountain sickness [212,213].
Notch signaling is an important modulator of oxidative stress. In the rat heart, Notch1 signaling via Nrf2 decreased ROS production and increased antioxidant activities to exert myocardial protection in ischemia–reperfusion injury [87]. Myocardial Notch signaling also acts via the Janus kinase 2 (JAK2)/signal transducer and STAT3 to activate mitochondrial superoxide dismutase expression and decrease ROS production [88]. In hepatocytes, Notch–STAT3 cross-talk has also been demonstrated, again in the context of ischemia–reperfusion injury, attributed to HES5-dependent STAT3 activation [214]. Conversely, ROS production has been linked to the regulation of Notch signaling function via NADPH oxidase 1, impacting cell proliferation and postmitotic differentiation [215].
6. Future Directions
Further investigation into the downstream effects of the specific NOTCH variants under selection in highland populations could reveal novel insights into mechanisms crucial to adaptation to hypoxia. A vast range of methodology exists to enable identification of specific variants and investigation into functional mechanisms [216]. In the identification of variants under selection, whole-genome sequencing provides the opportunity to obtain greater resolution of large-scale genome datasets alongside insight into noncoding regions. The functional mechanisms of Notch signaling in hypoxia are clearly complex, from the point of transcriptional regulation to a multitude of downstream pathways. Application of systemwide omics techniques would enable the molecular intricacies of this cross-talk to be captured, from the transcriptome and epigenome to the proteome and metabolome [192,217]. The application of these approaches in human subjects is crucial for providing insight into the genotype–phenotype association, whilst insight into direct causal links can be probed through genome-editing technologies [216].
7. Conclusions
Positively selected genetic regions that include Notch pathway components have been identified in highland populations, whilst Notch signaling has also been attributed to hypoxia tolerance. Together, this suggests that the Notch pathway is a key player in the complex interaction of regulatory pathways mediating hypoxic adaptation. The implications of Notch genetic variants under selection at high-altitude are, however, largely unexplored and warrant further investigation. Crucially, the Notch system exhibits close cross-talk with multiple elements of the HIF pathway, and is known to mediate numerous processes that are linked to cellular and tissue remodeling upon high-altitude exposure. Unravelling the intricacies of the high-altitude-selected Notch variant genotype–phenotype interaction will thus require a multisystem approach that spans from the transcriptome to the proteome and metabolome.
Author Contributions
The manuscript was written by K.A.O. and edited and reviewed by A.J.M. and T.S.S. All authors have read and agreed to the published version of the manuscript.
Funding
K.A.O. received funding from the European Union’s Horizon 2020 research and innovation program under a Marie Skłodowska-Curie grant agreement (No. 890768). A.J.M. was funded by the Research Councils UK (EP/E500552/1). T.S.S. was funded by the National Institutes of Health (R01HL145470), National Geographic Explorer Award, and the John B. West Endowed Chair in Respiratory Physiology.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Beall C.M. Two Routes to Functional Adaptation: Tibetan and Andean High-Altitude Natives. Proc. Natl. Acad. Sci. USA. 2007;104((Suppl. 1)):8655–8660. doi: 10.1073/pnas.0701985104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simonson T.S. Altitude Adaptation: A Glimpse Through Various Lenses. High Alt. Med. Biol. 2015;16:125–137. doi: 10.1089/ham.2015.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simonson T.S., Yang Y., Huff C.D., Yun H., Qin G., Witherspoon D.J., Bai Z., Lorenzo F.R., Xing J., Jorde L.B., et al. Genetic Evidence for High-Altitude Adaptation in Tibet. Science. 2010;329:72–75. doi: 10.1126/science.1189406. [DOI] [PubMed] [Google Scholar]
- 4.Beall C.M. Andean, Tibetan, and Ethiopian Patterns of Adaptation to High-Altitude Hypoxia. Integr. Comp. Biol. 2006;46:18–24. doi: 10.1093/icb/icj004. [DOI] [PubMed] [Google Scholar]
- 5.Pamenter M.E., Hall J.E., Tanabe Y., Simonson T.S. Cross-Species Insights Into Genomic Adaptations to Hypoxia. Front. Genet. 2020;11:743. doi: 10.3389/fgene.2020.00743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Semenza G.L. Hypoxia-Inducible Factors in Physiology and Medicine. Cell. 2012;148:399–408. doi: 10.1016/j.cell.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortiz-Barahona A., Villar D., Pescador N., Amigo J., del Peso L. Genome-Wide Identification of Hypoxia-Inducible Factor Binding Sites and Target Genes by a Probabilistic Model Integrating Transcription-Profiling Data and in Silico Binding Site Prediction. Nucleic Acids Res. 2010;38:2332–2345. doi: 10.1093/nar/gkp1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Semenza G.L. The Genomics and Genetics of Oxygen Homeostasis. Annu. Rev. Genom. Hum. Genet. 2020;21:183–204. doi: 10.1146/annurev-genom-111119-073356. [DOI] [PubMed] [Google Scholar]
- 9.Iyer N.V., Kotch L.E., Agani F., Leung S.W., Laughner E., Wenger R.H., Gassmann M., Gearhart J.D., Lawler A.M., Yu A.Y., et al. Cellular and Developmental Control of O2 Homeostasis by Hypoxia-Inducible Factor 1α. Genes Dev. 1998;12:149–162. doi: 10.1101/gad.12.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Semenza G.L., Wang G.L. A Nuclear Factor Induced by Hypoxia via de Novo Protein Synthesis Binds to the Human Erythropoietin Gene Enhancer at a Site Required for Transcriptional Activation. Mol. Cell. Biol. 1992;12:5447–5454. doi: 10.1128/mcb.12.12.5447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Semenza G.L., Roth P.H., Fang H.M., Wang G.L. Transcriptional Regulation of Genes Encoding Glycolytic Enzymes by Hypoxia-Inducible Factor 1. J. Biol. Chem. 1994;269:23757–23763. doi: 10.1016/S0021-9258(17)31580-6. [DOI] [PubMed] [Google Scholar]
- 12.Horscroft J.A., Kotwica A.O., Laner V., West J.A., Hennis P.J., Levett D.Z.H., Howard D.J., Fernandez B.O., Burgess S.L., Ament Z., et al. Metabolic Basis to Sherpa Altitude Adaptation. Proc. Natl. Acad. Sci. USA. 2017;114:6382–6387. doi: 10.1073/pnas.1700527114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ge R.-L., Simonson T.S., Gordeuk V., Prchal J.T., McClain D.A. Metabolic Aspects of High-Altitude Adaptation in Tibetans. Exp. Physiol. 2015;100:1247–1255. doi: 10.1113/EP085292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bray S.J. Notch Signalling in Context. Nat. Rev. Mol. Cell Biol. 2016;17:722–735. doi: 10.1038/nrm.2016.94. [DOI] [PubMed] [Google Scholar]
- 15.Cordle J., Johnson S., Tay J.Z.Y., Roversi P., Wilkin M.B., de Madrid B.H., Shimizu H., Jensen S., Whiteman P., Jin B., et al. A Conserved Face of the Jagged/Serrate DSL Domain Is Involved in Notch Trans-Activation and Cis-Inhibition. Nat. Struct. Mol. Biol. 2008;15:849–857. doi: 10.1038/nsmb.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rebay I., Fleming R.J., Fehon R.G., Cherbas L., Cherbas P., Artavanis-Tsakonas S. Specific EGF Repeats of Notch Mediate Interactions with Delta and Serrate: Implications for Notch as a Multifunctional Receptor. Cell. 1991;67:687–699. doi: 10.1016/0092-8674(91)90064-6. [DOI] [PubMed] [Google Scholar]
- 17.Nam Y., Sliz P., Song L., Aster J.C., Blacklow S.C. Structural Basis for Cooperativity in Recruitment of MAML Coactivators to Notch Transcription Complexes. Cell. 2006;124:973–983. doi: 10.1016/j.cell.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 18.Wilson J.J., Kovall R.A. Crystal Structure of the CSL-Notch-Mastermind Ternary Complex Bound to DNA. Cell. 2006;124:985–996. doi: 10.1016/j.cell.2006.01.035. [DOI] [PubMed] [Google Scholar]
- 19.Kopan R., Ilagan M.X.G. The Canonical Notch Signaling Pathway: Unfolding the Activation Mechanism. Cell. 2009;137:216–233. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kitagawa M. Notch Signalling in the Nucleus: Roles of Mastermind-like (MAML) Transcriptional Coactivators. J. Biochem. 2016;159:287–294. doi: 10.1093/jb/mvv123. [DOI] [PubMed] [Google Scholar]
- 21.Weng A.P., Millholland J.M., Yashiro-Ohtani Y., Arcangeli M.L., Lau A., Wai C., Del Bianco C., Rodriguez C.G., Sai H., Tobias J., et al. C-Myc Is an Important Direct Target of Notch1 in T-Cell Acute Lymphoblastic Leukemia/Lymphoma. Genes Dev. 2006;20:2096–2109. doi: 10.1101/gad.1450406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palomero T., Lim W.K., Odom D.T., Sulis M.L., Real P.J., Margolin A., Barnes K.C., O’Neil J., Neuberg D., Weng A.P., et al. NOTCH1 Directly Regulates C-MYC and Activates a Feed-Forward-Loop Transcriptional Network Promoting Leukemic Cell Growth. Proc. Natl. Acad. Sci. USA. 2006;103:18261–18266. doi: 10.1073/pnas.0606108103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jarriault S., Le Bail O., Hirsinger E., Pourquié O., Logeat F., Strong C.F., Brou C., Seidah N.G., Isra l A. Delta-1 Activation of Notch-1 Signaling Results in HES-1 Transactivation. Mol. Cell. Biol. 1998;18:7423–7431. doi: 10.1128/MCB.18.12.7423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maier M.M., Gessler M. Comparative Analysis of the Human and Mouse Hey1 Promoter: Hey Genes Are New Notch Target Genes. Biochem. Biophys. Res. Commun. 2000;275:652–660. doi: 10.1006/bbrc.2000.3354. [DOI] [PubMed] [Google Scholar]
- 25.Stoeck A., Lejnine S., Truong A., Pan L., Wang H., Zang C., Yuan J., Ware C., MacLean J., Garrett-Engele P.W., et al. Discovery of Biomarkers Predictive of GSI Response in Triple-Negative Breast Cancer and Adenoid Cystic Carcinoma. Cancer Discov. 2014;4:1154–1167. doi: 10.1158/2159-8290.CD-13-0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rangarajan A., Talora C., Okuyama R., Nicolas M., Mammucari C., Oh H., Aster J.C., Krishna S., Metzger D., Chambon P., et al. Notch Signaling Is a Direct Determinant of Keratinocyte Growth Arrest and Entry into Differentiation. EMBO J. 2001;20:3427–3436. doi: 10.1093/emboj/20.13.3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.García-Peydró M., Fuentes P., Mosquera M., García-León M.J., Alcain J., Rodríguez A., de Miguel P.G., Menéndez P., Weijer K., Spits H., et al. The NOTCH1/CD44 Axis Drives Pathogenesis in a T Cell Acute Lymphoblastic Leukemia Model. J. Clin. Investig. 2018;128:2802–2818. doi: 10.1172/JCI92981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.López-Arribillaga E., Rodilla V., Pellegrinet L., Guiu J., Iglesias M., Roman A.C., Gutarra S., González S., Muñoz-Cánoves P., Fernández-Salguero P., et al. Bmi1 Regulates Murine Intestinal Stem Cell Proliferation and Self-Renewal Downstream of Notch. Development. 2015;142:41–50. doi: 10.1242/dev.107714. [DOI] [PubMed] [Google Scholar]
- 29.Haltiwanger R.S., Stanley P. Modulation of Receptor Signaling by Glycosylation: Fringe Is an O-Fucose-Β1, 3-N-Acetylglucosaminyltransferase. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2002;1573:328–335. doi: 10.1016/S0304-4165(02)00400-2. [DOI] [PubMed] [Google Scholar]
- 30.Brückner K., Perez L., Clausen H., Cohen S. Glycosyltransferase Activity of Fringe Modulates Notch–Delta Interactions. Nature. 2000;406:411–415. doi: 10.1038/35019075. [DOI] [PubMed] [Google Scholar]
- 31.Yang L.-T., Nichols J.T., Yao C., Manilay J.O., Robey E.A., Weinmaster G. Fringe Glycosyltransferases Differentially Modulate Notch1 Proteolysis Induced by Delta1 and Jagged1. Mol. Biol. Cell. 2005;16:927–942. doi: 10.1091/mbc.e04-07-0614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Landor S.K.-J., Lendahl U. The Interplay between the Cellular Hypoxic Response and Notch Signaling. Exp. Cell Res. 2017;356:146–151. doi: 10.1016/j.yexcr.2017.04.030. [DOI] [PubMed] [Google Scholar]
- 33.Bigham A.W., Mao X., Mei R., Brutsaert T., Wilson M.J., Julian C.G., Parra E.J., Akey J.M., Moore L.G., Shriver M.D. Identifying Positive Selection Candidate Loci for High-Altitude Adaptation in Andean Populations. Hum. Genom. 2009;4:79–90. doi: 10.1186/1479-7364-4-2-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xin J., Zhang H., He Y., Duren Z., Bai C., Chen L., Luo X., Yan D.-S., Zhang C., Zhu X., et al. Chromatin Accessibility Landscape and Regulatory Network of High-Altitude Hypoxia Adaptation. Nat. Commun. 2020;11:4928. doi: 10.1038/s41467-020-18638-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang Z., Qiu M., Du H., Li Q., Yu C., Gan W., Peng H., Xia B., Xiong X., Song X., et al. Whole Genome Re-Sequencing Identifies Unique Adaption of Single Nucleotide Polymorphism, Insertion/Deletion and Structure Variation Related to Hypoxia in Tibetan Chickens. Gene Expr. Patterns. 2021;40:119181. doi: 10.1016/j.gep.2021.119181. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y., Zheng X., Zhang Y., Zhang H., Zhang X., Zhang H. Comparative Transcriptomic and Proteomic Analyses Provide Insights into Functional Genes for Hypoxic Adaptation in Embryos of Tibetan Chickens. Sci. Rep. 2020;10:11213. doi: 10.1038/s41598-020-68178-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jia C., Kong X., Koltes J.E., Gou X., Yang S., Yan D., Lu S., Wei Z. Gene Co-Expression Network Analysis Unraveling Transcriptional Regulation of High-Altitude Adaptation of Tibetan Pig. PLoS ONE. 2016;11:e0168161. doi: 10.1371/journal.pone.0168161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qiu Q., Zhang G., Ma T., Qian W., Wang J., Ye Z., Cao C., Hu Q., Kim J., Larkin D.M., et al. The Yak Genome and Adaptation to Life at High Altitude. Nat. Genet. 2012;44:946–949. doi: 10.1038/ng.2343. [DOI] [PubMed] [Google Scholar]
- 39.Bozkulak Esra Cagavi; Weinmaster Gerry Selective Use of ADAM10 and ADAM17 in Activation of Notch1 Signaling. Mol. Cell. Biol. 2009;29:5679–5695. doi: 10.1128/MCB.00406-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang R., Li Y., Tsung A., Huang H., Du Q., Yang M., Deng M., Xiong S., Wang X., Zhang L., et al. INOS Promotes CD24+ CD133+ Liver Cancer Stem Cell Phenotype through a TACE/ADAM17-Dependent Notch Signaling Pathway. Proc. Natl. Acad. Sci. USA. 2018;115:E10127–E10136. doi: 10.1073/pnas.1722100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Groot A.J., Cobzaru C., Weber S., Saftig P., Blobel C.P., Kopan R., Vooijs M., Franzke C.-W. Epidermal ADAM17 Is Dispensable for Notch Activation. J. Investig. Dermatol. 2013;133:2286–2288. doi: 10.1038/jid.2013.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou D., Xue J., Lai J.C.K., Schork N.J., White K.P., Haddad G.G. Mechanisms Underlying Hypoxia Tolerance in Drosophila Melanogaster: Hairy as a Metabolic Switch. PLoS Genet. 2008;4:e1000221. doi: 10.1371/journal.pgen.1000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Azad P., Zhou D., Zarndt R., Haddad G.G. Identification of Genes Underlying Hypoxia Tolerance in Drosophila by a P-Element Screen. G3. 2012;2:1169–1178. doi: 10.1534/g3.112.003681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou D., Udpa N., Gersten M., Visk D.W., Bashir A., Xue J., Frazer K.A., Posakony J.W., Subramaniam S., Bafna V., et al. Experimental Selection of Hypoxia-Tolerant Drosophila Melanogaster. Proc. Natl. Acad. Sci. USA. 2011;108:2349–2354. doi: 10.1073/pnas.1010643108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zheng X., Linke S., Dias J.M., Zheng X., Gradin K., Wallis T.P., Hamilton B.R., Gustafsson M., Ruas J.L., Wilkins S., et al. Interaction with Factor Inhibiting HIF-1 Defines an Additional Mode of Cross-Coupling between the Notch and Hypoxia Signaling Pathways. Proc. Natl. Acad. Sci. USA. 2008;105:3368–3373. doi: 10.1073/pnas.0711591105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gustafsson M.V., Zheng X., Pereira T., Gradin K., Jin S., Lundkvist J., Ruas J.L., Poellinger L., Lendahl U., Bondesson M. Hypoxia Requires Notch Signaling to Maintain the Undifferentiated Cell State. Dev. Cell. 2005;9:617–628. doi: 10.1016/j.devcel.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 47.Diez H., Fischer A., Winkler A., Hu C.-J., Hatzopoulos A.K., Breier G., Gessler M. Hypoxia-Mediated Activation of Dll4-Notch-Hey2 Signaling in Endothelial Progenitor Cells and Adoption of Arterial Cell Fate. Exp. Cell Res. 2007;313:1–9. doi: 10.1016/j.yexcr.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 48.Wang R., Zhang Y.-W., Zhang X., Liu R., Zhang X., Hong S., Xia K., Xia J., Zhang Z., Xu H. Transcriptional Regulation of APH-1A and Increased g-Secretase Cleavage of APP and Notch by HIF-1 and Hypoxia. FASEB J.-Fed. Am. Soc. Exp. Biol. 2006;20:1275. doi: 10.1096/fj.06-5839fje. [DOI] [PubMed] [Google Scholar]
- 49.Villa J.C., Chiu D., Brandes A.H., Escorcia F.E., Villa C.H., Maguire W.F., Hu C.-J., de Stanchina E., Simon M.C., Sisodia S.S., et al. Nontranscriptional Role of Hif-1α in Activation of γ-Secretase and Notch Signaling in Breast Cancer. Cell Rep. 2014;8:1077–1092. doi: 10.1016/j.celrep.2014.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lando D., Peet D.J., Gorman J.J., Whelan D.A., Whitelaw M.L., Bruick R.K. FIH-1 Is an Asparaginyl Hydroxylase Enzyme That Regulates the Transcriptional Activity of Hypoxia-Inducible Factor. Genes Dev. 2002;16:1466–1471. doi: 10.1101/gad.991402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.So J.-H., Kim J.-D., Yoo K.-W., Kim H.-T., Jung S.-H., Choi J.-H., Lee M.-S., Jin S.-W., Kim C.-H. FIH-1, a Novel Interactor of Mindbomb, Functions as an Essential Anti-Angiogenic Factor during Zebrafish Vascular Development. PLoS ONE. 2014;9:e109517. doi: 10.1371/journal.pone.0109517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Childebayeva A., Jones T.R., Goodrich J.M., Leon-Velarde F., Rivera-Chira M., Kiyamu M., Brutsaert T.D., Dolinoy D.C., Bigham A.W. LINE-1 and EPAS1 DNA Methylation Associations with High-Altitude Exposure. Epigenetics. 2019;14:1–15. doi: 10.1080/15592294.2018.1561117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Childebayeva A., Harman T., Weinstein J., Goodrich J.M., Dolinoy D.C., Day T.A., Bigham A.W., Brutsaert T.D. DNA Methylation Changes Are Associated With an Incremental Ascent to High Altitude. Front. Genet. 2019;10:1062. doi: 10.3389/fgene.2019.01062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Reister S., Kordes C., Sawitza I., Häussinger D. The Epigenetic Regulation of Stem Cell Factors in Hepatic Stellate Cells. Stem Cells Dev. 2011;20:1687–1699. doi: 10.1089/scd.2010.0418. [DOI] [PubMed] [Google Scholar]
- 55.Piazzi G., Fini L., Selgrad M., Garcia M., Daoud Y., Wex T., Malfertheiner P., Gasbarrini A., Romano M., Meyer R.L., et al. Epigenetic Regulation of Delta-Like1 Controls Notch1 Activation in Gastric Cancer. Oncotarget. 2011;2:1291–1301. doi: 10.18632/oncotarget.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bartels S.J.J., Spruijt C.G., Brinkman A.B., Jansen P.W.T.C., Vermeulen M., Stunnenberg H.G. A SILAC-Based Screen for Methyl-CpG Binding Proteins Identifies RBP-J as a DNA Methylation and Sequence-Specific Binding Protein. PLoS ONE. 2011;6:e25884. doi: 10.1371/journal.pone.0025884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hirota K., Semenza G.L. Regulation of Angiogenesis by Hypoxia-Inducible Factor 1. Crit. Rev. Oncol. Hematol. 2006;59:15–26. doi: 10.1016/j.critrevonc.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 58.Benedito R., Roca C., Sörensen I., Adams S., Gossler A., Fruttiger M., Adams R.H. The Notch Ligands Dll4 and Jagged1 Have Opposing Effects on Angiogenesis. Cell. 2009;137:1124–1135. doi: 10.1016/j.cell.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 59.Jakobsson L., Franco C.A., Bentley K., Collins R.T., Ponsioen B., Aspalter I.M., Rosewell I., Busse M., Thurston G., Medvinsky A., et al. Endothelial Cells Dynamically Compete for the Tip Cell Position during Angiogenic Sprouting. Nat. Cell Biol. 2010;12:943–953. doi: 10.1038/ncb2103. [DOI] [PubMed] [Google Scholar]
- 60.Stenmark K.R., Fagan K.A., Frid M.G. Hypoxia-Induced Pulmonary Vascular Remodeling: Cellular and Molecular Mechanisms. Circ. Res. 2006;99:675–691. doi: 10.1161/01.RES.0000243584.45145.3f. [DOI] [PubMed] [Google Scholar]
- 61.Li X., Zhang X., Leathers R., Makino A., Huang C., Parsa P., Macias J., Yuan J.X.-J., Jamieson S.W., Thistlethwaite P.A. Notch3 Signaling Promotes the Development of Pulmonary Arterial Hypertension. Nat. Med. 2009;15:1289–1297. doi: 10.1038/nm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ward J.P.T., McMurtry I.F. Mechanisms of Hypoxic Pulmonary Vasoconstriction and Their Roles in Pulmonary Hypertension: New Findings for an Old Problem. Curr. Opin. Pharmacol. 2009;9:287–296. doi: 10.1016/j.coph.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith K.A., Voiriot G., Tang H., Fraidenburg D.R., Song S., Yamamura H., Yamamura A., Guo Q., Wan J., Pohl N.M., et al. Notch Activation of Ca2+ Signaling in the Development of Hypoxic Pulmonary Vasoconstriction and Pulmonary Hypertension. Am. J. Respir. Cell Mol. Biol. 2015;53:355–367. doi: 10.1165/rcmb.2014-0235OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Guo Q., Xu H., Yang X., Zhao D., Liu S., Sun X., Huang J.-A. Notch Activation of Ca 2+-Sensing Receptor Mediates Hypoxia-Induced Pulmonary Hypertension. Hypertens. Res. 2017;40:117–129. doi: 10.1038/hr.2016.118. [DOI] [PubMed] [Google Scholar]
- 65.Siervo M., Riley H.L., Fernandez B.O., Leckstrom C.A., Martin D.S., Mitchell K., Levett D.Z., Montgomery H.E., Mythen M.G., Grocott M.P., et al. Caudwell Xtreme Everest Research Group Effects of Prolonged Exposure to Hypobaric Hypoxia on Oxidative Stress, Inflammation and Gluco-Insular Regulation: The Not-so-Sweet Price for Good Regulation. PLoS ONE. 2014;9:e94915. doi: 10.1371/journal.pone.0094915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Young P.M., Rose M.S., Sutton J.R., Green H.J., Cymerman A., Houston C.S. Operation Everest II: Plasma Lipid and Hormonal Responses during a Simulated Ascent of Mt. Everest. J. Appl. Physiol. 1989;66:1430–1435. doi: 10.1152/jappl.1989.66.3.1430. [DOI] [PubMed] [Google Scholar]
- 67.Pajvani U.B., Shawber C.J., Samuel V.T., Birkenfeld A.L., Shulman G.I., Kitajewski J., Accili D. Inhibition of Notch Signaling Ameliorates Insulin Resistance in a FoxO1-Dependent Manner. Nat. Med. 2011;17:961–967. doi: 10.1038/nm.2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim J.-W., Tchernyshyov I., Semenza G.L., Dang C.V. HIF-1-Mediated Expression of Pyruvate Dehydrogenase Kinase: A Metabolic Switch Required for Cellular Adaptation to Hypoxia. Cell Metab. 2006;3:177–185. doi: 10.1016/j.cmet.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 69.Landor S.K.-J., Mutvei A.P., Mamaeva V., Jin S., Busk M., Borra R., Grönroos T.J., Kronqvist P., Lendahl U., Sahlgren C.M. Hypo- and Hyperactivated Notch Signaling Induce a Glycolytic Switch through Distinct Mechanisms. Proc. Natl. Acad. Sci. USA. 2011;108:18814–18819. doi: 10.1073/pnas.1104943108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Slaninova V., Krafcikova M., Perez-Gomez R., Steffal P., Trantirek L., Bray S.J., Krejci A. Notch Stimulates Growth by Direct Regulation of Genes Involved in the Control of Glycolysis and the Tricarboxylic Acid Cycle. Open Biol. 2016;6:150155. doi: 10.1098/rsob.150155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Metallo C.M., Gameiro P.A., Bell E.L., Mattaini K.R., Yang J., Hiller K., Jewell C.M., Johnson Z.R., Irvine D.J., Guarente L., et al. Reductive Glutamine Metabolism by IDH1 Mediates Lipogenesis under Hypoxia. Nature. 2011;481:380–384. doi: 10.1038/nature10602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Basak N.P., Roy A., Banerjee S. Alteration of Mitochondrial Proteome Due to Activation of Notch1 Signaling Pathway. J. Biol. Chem. 2014;289:7320–7334. doi: 10.1074/jbc.M113.519405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang H., Gao P., Fukuda R., Kumar G., Krishnamachary B., Zeller K.I., Dang C.V., Semenza G.L. HIF-1 Inhibits Mitochondrial Biogenesis and Cellular Respiration in VHL-Deficient Renal Cell Carcinoma by Repression of C-MYC Activity. Cancer Cell. 2007;11:407–420. doi: 10.1016/j.ccr.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 74.Levett D.Z., Radford E.J., Menassa D.A., Graber E.F., Morash A.J., Hoppeler H., Clarke K., Martin D.S., Ferguson-Smith A.C., Montgomery H.E., et al. Acclimatization of Skeletal Muscle Mitochondria to High-Altitude Hypoxia during an Ascent of Everest. FASEB J. 2012;26:1431–1441. doi: 10.1096/fj.11-197772. [DOI] [PubMed] [Google Scholar]
- 75.Bi P., Shan T., Liu W., Yue F., Yang X., Liang X.-R., Wang J., Li J., Carlesso N., Liu X., et al. Inhibition of Notch Signaling Promotes Browning of White Adipose Tissue and Ameliorates Obesity. Nat. Med. 2014;20:911–918. doi: 10.1038/nm.3615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Colleoni F., Padmanabhan N., Yung H.-W., Watson E.D., Cetin I., Tissot van Patot M.C., Burton G.J., Murray A.J. Suppression of Mitochondrial Electron Transport Chain Function in the Hypoxic Human Placenta: A Role for MiRNA-210 and Protein Synthesis Inhibition. PLoS ONE. 2013;8:e55194. doi: 10.1371/journal.pone.0055194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fukuda R., Zhang H., Kim J.-W., Shimoda L., Dang C.V., Semenza G.L. HIF-1 Regulates Cytochrome Oxidase Subunits to Optimize Efficiency of Respiration in Hypoxic Cells. Cell. 2007;129:111–122. doi: 10.1016/j.cell.2007.01.047. [DOI] [PubMed] [Google Scholar]
- 78.O’Brien K.A., Simonson T.S., Murray A.J. Metabolic Adaptation to High Altitude. Curr. Opin. Endocr. Metab. Res. 2020;11:33–41. doi: 10.1016/j.coemr.2019.12.002. [DOI] [Google Scholar]
- 79.Song N.-J., Yun U.J., Yang S., Wu C., Seo C.-R., Gwon A.-R., Baik S.-H., Choi Y., Choi B.Y., Bahn G., et al. Notch1 Deficiency Decreases Hepatic Lipid Accumulation by Induction of Fatty Acid Oxidation. Sci. Rep. 2016;6:19377. doi: 10.1038/srep19377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kuhlicke J., Frick J.S., Morote-Garcia J.C., Rosenberger P., Eltzschig H.K. Hypoxia Inducible Factor (HIF)-1 Coordinates Induction of Toll-like Receptors TLR2 and TLR6 during Hypoxia. PLoS ONE. 2007;2:e1364. doi: 10.1371/journal.pone.0001364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rius J., Guma M., Schachtrup C., Akassoglou K., Zinkernagel A.S., Nizet V., Johnson R.S., Haddad G.G., Karin M. NF-KappaB Links Innate Immunity to the Hypoxic Response through Transcriptional Regulation of HIF-1alpha. Nature. 2008;453:807–811. doi: 10.1038/nature06905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bonello S., Zähringer C., BelAiba R.S., Djordjevic T., Hess J., Michiels C., Kietzmann T., Görlach A. Reactive Oxygen Species Activate the HIF-1α Promoter Via a Functional NFκB Site. Arterioscler. Thromb. Vasc. Biol. 2007;27:755–761. doi: 10.1161/01.ATV.0000258979.92828.bc. [DOI] [PubMed] [Google Scholar]
- 83.Wang J., Shelly L., Miele L., Boykins R., Norcross M.A., Guan E. Human Notch-1 Inhibits NF-ΚB Activity in the Nucleus Through a Direct Interaction Involving a Novel Domain. J. Immunol. 2001;167:289–295. doi: 10.4049/jimmunol.167.1.289. [DOI] [PubMed] [Google Scholar]
- 84.Pajvani U.B., Qiang L., Kangsamaksin T., Kitajewski J., Ginsberg H.N., Accili D. Inhibition of Notch Uncouples Akt Activation from Hepatic Lipid Accumulation by Decreasing MTorc1 Stability. Nat. Med. 2013;19:1054–1060. doi: 10.1038/nm.3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nguyen T., Nioi P., Pickett C.B. The Nrf2-Antioxidant Response Element Signaling Pathway and Its Activation by Oxidative Stress. J. Biol. Chem. 2009;284:13291–13295. doi: 10.1074/jbc.R900010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kamata H., Manabe T., Oka S.-I., Kamata K., Hirata H. Hydrogen Peroxide Activates IκB Kinases through Phosphorylation of Serine Residues in the Activation Loops. FEBS Lett. 2002;519:231–237. doi: 10.1016/S0014-5793(02)02712-6. [DOI] [PubMed] [Google Scholar]
- 87.Zhou X.-L., Wu X., Zhu R.-R., Xu H., Li Y.-Y., Xu Q.-R., Liu S., Lai S.-Q., Xu X., Wan L., et al. Notch1-Nrf2 Signaling Crosstalk Provides Myocardial Protection by Reducing ROS Formation. Biochem. Cell Biol. 2020;98:106–111. doi: 10.1139/bcb-2018-0398. [DOI] [PubMed] [Google Scholar]
- 88.Cai W., Yang X., Han S., Guo H., Zheng Z., Wang H., Guan H., Jia Y., Gao J., Yang T., et al. Notch1 Pathway Protects against Burn-Induced Myocardial Injury by Repressing Reactive Oxygen Species Production through JAK2/STAT3 Signaling. Oxid. Med. Cell. Longev. 2016;2016:5638943. doi: 10.1155/2016/5638943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pietras A., von Stedingk K., Lindgren D., Påhlman S., Axelson H. JAG2 Induction in Hypoxic Tumor Cells Alters Notch Signaling and Enhances Endothelial Cell Tube Formation. Mol. Cancer Res. 2011;9:626–636. doi: 10.1158/1541-7786.MCR-10-0508. [DOI] [PubMed] [Google Scholar]
- 90.Xing F., Okuda H., Watabe M., Kobayashi A., Pai S.K., Liu W., Pandey P.R., Fukuda K., Hirota S., Sugai T., et al. Hypoxia-Induced Jagged2 Promotes Breast Cancer Metastasis and Self-Renewal of Cancer Stem-like Cells. Oncogene. 2011;30:4075–4086. doi: 10.1038/onc.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lanner F., Lee K.L., Ortega G.C., Sohl M., Li X., Jin S., Hansson E.M., Claesson-Welsh L., Poellinger L., Lendahl U., et al. Hypoxia-Induced Arterial Differentiation Requires Adrenomedullin and Notch Signaling. Stem Cells Dev. 2013;22:1360–1369. doi: 10.1089/scd.2012.0259. [DOI] [PubMed] [Google Scholar]
- 92.Jögi A., Øra I., Nilsson H., Lindeheim A., Makino Y., Poellinger L., Axelson H., Påhlman S. Hypoxia Alters Gene Expression in Human Neuroblastoma Cells toward an Immature and Neural Crest-like Phenotype. Proc. Natl. Acad. Sci. USA. 2002;99:7021–7026. doi: 10.1073/pnas.102660199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mutvei A.P., Landor S.K.-J., Fox R., Braune E.-B., Tsoi Y.L., Phoon Y.P., Sahlgren C., Hartman J., Bergh J., Jin S., et al. Notch Signaling Promotes a HIF2α-Driven Hypoxic Response in Multiple Tumor Cell Types. Oncogene. 2018;37:6083–6095. doi: 10.1038/s41388-018-0400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Coleman M.L., McDonough M.A., Hewitson K.S., Coles C., Mecinovic J., Edelmann M., Cook K.M., Cockman M.E., Lancaster D.E., Kessler B.M., et al. Asparaginyl Hydroxylation of the Notch Ankyrin Repeat Domain by Factor Inhibiting Hypoxia-Inducible Factor. J. Biol. Chem. 2007;282:24027–24038. doi: 10.1074/jbc.M704102200. [DOI] [PubMed] [Google Scholar]
- 95.Tseng L.-C., Zhang C., Cheng C.-M., Xu H., Hsu C.-H., Jiang Y.-J. New Classes of Mind Bomb-Interacting Proteins Identified from Yeast Two-Hybrid Screens. PLoS ONE. 2014;9:e93394. doi: 10.1371/journal.pone.0093394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shareef M.M., Udayakumar T.S., Sinha V.K., Saleem S.M., Griggs W.W. Interaction of HIF-1 and Notch3 Is Required for the Expression of Carbonic Anhydrase 9 in Breast Carcinoma Cells. Genes Cancer. 2013;4:513–523. doi: 10.1177/1947601913481670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Julian C.G. Epigenomics and Human Adaptation to High Altitude. J. Appl. Physiol. 2017;123:1362–1370. doi: 10.1152/japplphysiol.00351.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jones P.A., Liang G. Rethinking How DNA Methylation Patterns Are Maintained. Nat. Rev. Genet. 2009;10:805–811. doi: 10.1038/nrg2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Miranda T.B., Jones P.A. DNA Methylation: The Nuts and Bolts of Repression. J. Cell. Physiol. 2007;213:384–390. doi: 10.1002/jcp.21224. [DOI] [PubMed] [Google Scholar]
- 100.Ogino S., Nosho K., Kirkner G.J., Kawasaki T., Chan A.T., Schernhammer E.S., Giovannucci E.L., Fuchs C.S. A Cohort Study of Tumoral LINE-1 Hypomethylation and Prognosis in Colon Cancer. J. Natl. Cancer Inst. 2008;100:1734–1738. doi: 10.1093/jnci/djn359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.James S.J., Cutler P., Melnyk S., Jernigan S., Janak L., Gaylor D.W., Neubrander J.A. Metabolic Biomarkers of Increased Oxidative Stress and Impaired Methylation Capacity in Children with Autism. Am. J. Clin. Nutr. 2004;80:1611–1617. doi: 10.1093/ajcn/80.6.1611. [DOI] [PubMed] [Google Scholar]
- 102.Lachance G., Uniacke J., Audas T.E., Holterman C.E., Franovic A., Payette J., Lee S. DNMT3a Epigenetic Program Regulates the HIF-2α Oxygen-Sensing Pathway and the Cellular Response to Hypoxia. Proc. Natl. Acad. Sci. USA. 2014;111:7783–7788. doi: 10.1073/pnas.1322909111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Herman J.G., Latif F., Weng Y., Lerman M.I., Zbar B., Liu S., Samid D., Duan D.S., Gnarra J.R., Linehan W.M. Silencing of the VHL Tumor-Suppressor Gene by DNA Methylation in Renal Carcinoma. Proc. Natl. Acad. Sci. USA. 1994;91:9700–9704. doi: 10.1073/pnas.91.21.9700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wenger R.H., Kvietikova I., Rolfs A., Camenisch G., Gassmann M. Oxygen-Regulated Erythropoietin Gene Expression Is Dependent on a CpG Methylation-Free Hypoxia-Inducible Factor-1 DNA-Binding Site. Eur. J. Biochem. 1998;253:771–777. doi: 10.1046/j.1432-1327.1998.2530771.x. [DOI] [PubMed] [Google Scholar]
- 105.Rössler J., Stolze I., Frede S., Freitag P., Schweigerer L., Havers W., Fandrey J. Hypoxia-Induced Erythropoietin Expression in Human Neuroblastoma Requires a Methylation Free HIF-1 Binding Site. J. Cell. Biochem. 2004;93:153–161. doi: 10.1002/jcb.20133. [DOI] [PubMed] [Google Scholar]
- 106.Yin H., Blanchard K.L. DNA Methylation Represses the Expression of the Human Erythropoietin Gene by Two Different Mechanisms. Blood. 2000;95:111–119. doi: 10.1182/blood.V95.1.111. [DOI] [PubMed] [Google Scholar]
- 107.Schwanbeck R. The Role of Epigenetic Mechanisms in Notch Signaling during Development. J. Cell. Physiol. 2015;230:969–981. doi: 10.1002/jcp.24851. [DOI] [PubMed] [Google Scholar]
- 108.Ghoshal P., Nganga A.J., Moran-Giuati J., Szafranek A., Johnson T.R., Bigelow A.J., Houde C.M., Avet-Loiseau H., Smiraglia D.J., Ersing N., et al. Loss of the SMRT/NCoR2 Corepressor Correlates with JAG2 Overexpression in Multiple Myeloma. Cancer Res. 2009;69:4380–4387. doi: 10.1158/0008-5472.CAN-08-3467. [DOI] [PubMed] [Google Scholar]
- 109.Han J., Li J., Ho J.C., Chia G.S., Kato H., Jha S., Yang H., Poellinger L., Lee K.L. Hypoxia Is a Key Driver of Alternative Splicing in Human Breast Cancer Cells. Sci. Rep. 2017;7:4108. doi: 10.1038/s41598-017-04333-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Green L., Cookson A., Bruce I.N., Donn R.P., Ray D.W. Identification of Multiple, Oxygen-Stable HIF1 Alpha Isoforms, and Augmented Expression of Adrenomedullin in Rheumatoid Arthritis. Clin. Exp. Rheumatol. 2013;31:672–682. [PubMed] [Google Scholar]
- 111.Gothié E., Richard D.E., Berra E., Pagès G. Identification of Alternative Spliced Variants of Human Hypoxia-Inducible Factor-1α. J. Biol. 2000;275:6922–6927. doi: 10.1074/jbc.275.10.6922. [DOI] [PubMed] [Google Scholar]
- 112.Lee K.-H., Park J.-W., Chun Y.-S. Non-Hypoxic Transcriptional Activation of the Aryl Hydrocarbon Receptor Nuclear Translocator in Concert with a Novel Hypoxia-Inducible Factor-1alpha Isoform. Nucleic Acids Res. 2004;32:5499–5511. doi: 10.1093/nar/gkh880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bowler E., Oltean S. Alternative Splicing in Angiogenesis. Int. J. Mol. Sci. 2019;20:2067. doi: 10.3390/ijms20092067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Choi Y.-J., Kim I., Lee J.E., Park J.-W. PIN1 Transcript Variant 2 Acts as a Long Non-Coding RNA That Controls the HIF-1-Driven Hypoxic Response. Sci. Rep. 2019;9:10599. doi: 10.1038/s41598-019-47071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mirtschink P., Krishnan J., Grimm F., Sarre A., Hörl M., Kayikci M., Fankhauser N., Christinat Y., Cortijo C., Feehan O., et al. HIF-Driven SF3B1 Induces KHK-C to Enforce Fructolysis and Heart Disease. Nature. 2015;522:444–449. doi: 10.1038/nature14508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.David C.J., Chen M., Assanah M., Canoll P., Manley J.L. HnRNP Proteins Controlled by C-Myc Deregulate Pyruvate Kinase MRNA Splicing in Cancer. Nature. 2010;463:364–368. doi: 10.1038/nature08697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Williams A.L., Khadka V., Tang M., Avelar A., Schunke K.J., Menor M., Shohet R.V. HIF1 Mediates a Switch in Pyruvate Kinase Isoforms after Myocardial Infarction. Physiol. Genom. 2018;50:479–494. doi: 10.1152/physiolgenomics.00130.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Luo W., Hu H., Chang R., Zhong J., Knabel M., O’Meally R., Cole R.N., Pandey A., Semenza G.L. Pyruvate Kinase M2 Is a PHD3-Stimulated Coactivator for Hypoxia-Inducible Factor 1. Cell. 2011;145:732–744. doi: 10.1016/j.cell.2011.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rosati E., Sabatini R., Rampino G., Tabilio A., Di Ianni M., Fettucciari K., Bartoli A., Coaccioli S., Screpanti I., Marconi P. Constitutively Activated Notch Signaling Is Involved in Survival and Apoptosis Resistance of B-CLL Cells. Blood. 2009;113:856–865. doi: 10.1182/blood-2008-02-139725. [DOI] [PubMed] [Google Scholar]
- 120.Puente X.S., Pinyol M., Quesada V., Conde L., Ordóñez G.R., Villamor N., Escaramis G., Jares P., Beà S., González-Díaz M., et al. Whole-Genome Sequencing Identifies Recurrent Mutations in Chronic Lymphocytic Leukaemia. Nature. 2011;475:101–105. doi: 10.1038/nature10113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Larrayoz M., Rose-Zerilli M.J.J., Kadalayil L., Parker H., Blakemore S., Forster J., Davis Z., Steele A.J., Collins A., Else M., et al. Non-Coding NOTCH1 Mutations in Chronic Lymphocytic Leukemia; Their Clinical Impact in the UK CLL4 Trial. Leukemia. 2017;31:510–514. doi: 10.1038/leu.2016.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang L., Brooks A.N., Fan J., Wan Y., Gambe R., Li S., Hergert S., Yin S., Freeman S.S., Levin J.Z., et al. Transcriptomic Characterization of SF3B1 Mutation Reveals Its Pleiotropic Effects in Chronic Lymphocytic Leukemia. Cancer Cell. 2016;30:750–763. doi: 10.1016/j.ccell.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Adams B.D., Kasinski A.L., Slack F.J. Aberrant Regulation and Function of MicroRNAs in Cancer. Curr. Biol. 2014;24:R762–R776. doi: 10.1016/j.cub.2014.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Devlin C., Greco S., Martelli F., Ivan M. MiR-210: More than a Silent Player in Hypoxia. IUBMB Life. 2011;63:94–100. doi: 10.1002/iub.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lou Y.-L., Guo F., Liu F., Gao F.-L., Zhang P.-Q., Niu X., Guo S.-C., Yin J.-H., Wang Y., Deng Z.-F. MiR-210 Activates Notch Signaling Pathway in Angiogenesis Induced by Cerebral Ischemia. Mol. Cell. Biochem. 2012;370:45–51. doi: 10.1007/s11010-012-1396-6. [DOI] [PubMed] [Google Scholar]
- 126.Wang H., Zhao Y., Luo R., Bian X., Wang Y. A positive feedback self-regulatory loop between miR-210 and HIF-1α mediated by CPEB2 is involved in trophoblast syncytialization: Implication of trophoblast malfunction in preeclampsia. Biol. Reprod. 2020;102:560–570. doi: 10.1093/biolre/ioz196. [DOI] [PubMed] [Google Scholar]
- 127.Dökümcü K., Simonian M., Farahani R.M. MiR4673 Improves Fitness Profile of Neoplastic Cells by Induction of Autophagy. Cell Death Dis. 2018;9:1068. doi: 10.1038/s41419-018-1088-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Farahani R., Rezaei-Lotfi S., Simonian M., Hunter N. Bi-Modal Reprogramming of Cell Cycle by MiRNA-4673 Amplifies Human Neurogenic Capacity. Cell Cycle. 2019;18:848–868. doi: 10.1080/15384101.2019.1595873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Huang H.-L., Shi Y.-P., He H.-J., Wang Y.-H., Chen T., Yang L.-W., Yang T., Chen J., Cao J., Yao W.-M., et al. MiR-4673 Modulates Paclitaxel-Induced Oxidative Stress and Loss of Mitochondrial Membrane Potential by Targeting 8-Oxoguanine-DNA Glycosylase-1. Cell. Physiol. Biochem. 2017;42:889–900. doi: 10.1159/000478644. [DOI] [PubMed] [Google Scholar]
- 130.Icli B., Li H., Pérez-Cremades D., Wu W., Ozdemir D., Haemmig S., Guimaraes R.B., Manica A., Marchini J.F., Orgill D.P., et al. MiR-4674 Regulates Angiogenesis in Tissue Injury by Targeting P38K Signaling in Endothelial Cells. Am. J. Physiol. Cell Physiol. 2020;318:C524–C535. doi: 10.1152/ajpcell.00542.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kwon H., Song K., Han C., Zhang J., Lu L., Chen W., Wu T. Epigenetic Silencing of MiRNA-34a in Human Cholangiocarcinoma via EZH2 and DNA Methylation: Impact on Regulation of Notch Pathway. Am. J. Pathol. 2017;187:2288–2299. doi: 10.1016/j.ajpath.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Shayevitch R., Askayo D., Keydar I., Ast G. The Importance of DNA Methylation of Exons on Alternative Splicing. RNA. 2018;24:1351–1362. doi: 10.1261/rna.064865.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Monge C. LIFE IN THE ANDES AND CHRONIC MOUNTAIN SICKNESS. Science. 1942;95:79–84. doi: 10.1126/science.95.2456.79. [DOI] [PubMed] [Google Scholar]
- 134.Beall C.M., Brittenham G.M., Strohl K.P., Blangero J., Williams-Blangero S., Goldstein M.C., Decker M.J., Vargas E., Villena M., Soria R., et al. Hemoglobin Concentration of High-Altitude Tibetans and Bolivian Aymara. Am. J. Phys. Anthropol. 1998;106:385–400. doi: 10.1002/(SICI)1096-8644(199807)106:3<385::AID-AJPA10>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 135.Moore L.G., Niermeyer S., Zamudio S. Human Adaptation to High Altitude: Regional and Life-Cycle Perspectives. Am. J. Phys. Anthropol. 1998;107:25–64. doi: 10.1002/(SICI)1096-8644(1998)107:27+<25::AID-AJPA3>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 136.Winslow R.M., Chapman K.W., Gibson C.C., Samaja M., Monge C.C., Goldwasser E., Sherpa M., Blume F.D., Santolaya R. Different Hematologic Responses to Hypoxia in Sherpas and Quechua Indians. J. Appl. Physiol. 1989;66:1561–1569. doi: 10.1152/jappl.1989.66.4.1561. [DOI] [PubMed] [Google Scholar]
- 137.Semenza G.L. Involvement of Oxygen-Sensing Pathways in Physiologic and Pathologic Erythropoiesis. Blood. 2009;114:2015–2019. doi: 10.1182/blood-2009-05-189985. [DOI] [PubMed] [Google Scholar]
- 138.Haase V.H. Hypoxic Regulation of Erythropoiesis and Iron Metabolism. Am. J. Physiol. Renal Physiol. 2010;299:F1–F13. doi: 10.1152/ajprenal.00174.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lorenzo F.R., Huff C., Myllymäki M., Olenchock B., Swierczek S., Tashi T., Gordeuk V., Wuren T., Ri-Li G., McClain D.A., et al. A Genetic Mechanism for Tibetan High-Altitude Adaptation. Nat. Genet. 2014;46:951–956. doi: 10.1038/ng.3067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hattangadi S.M., Wong P., Zhang L., Flygare J., Lodish H.F. From Stem Cell to Red Cell: Regulation of Erythropoiesis at Multiple Levels by Multiple Proteins, RNAs, and Chromatin Modifications. Blood. 2011;118:6258–6268. doi: 10.1182/blood-2011-07-356006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Azad P., Stobdan T., Zhou D., Hartley I., Akbari A., Bafna V., Haddad G.G. High-Altitude Adaptation in Humans: From Genomics to Integrative Physiology. J. Mol. Med. 2017;95:1269–1282. doi: 10.1007/s00109-017-1584-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhou D., Udpa N., Ronen R., Stobdan T., Liang J., Appenzeller O., Zhao H.W., Yin Y., Du Y., Guo L., et al. Whole-Genome Sequencing Uncovers the Genetic Basis of Chronic Mountain Sickness in Andean Highlanders. Am. J. Hum. Genet. 2013;93:452–462. doi: 10.1016/j.ajhg.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hsieh M.M., Callacondo D., Rojas-Camayo J., Quesada-Olarte J., Wang X., Uchida N., Maric I., Remaley A.T., Leon-Velarde F., Villafuerte F.C., et al. SENP1, but Not Fetal Hemoglobin, Differentiates Andean Highlanders with Chronic Mountain Sickness from Healthy Individuals among Andean Highlanders. Exp. Hematol. 2016;44:483–490e2. doi: 10.1016/j.exphem.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Chiba S. Concise Review: Notch Signaling in Stem Cell Systems. Stem Cells. 2006;24:2437–2447. doi: 10.1634/stemcells.2005-0661. [DOI] [PubMed] [Google Scholar]
- 145.Bigas A., Espinosa L. Hematopoietic Stem Cells: To Be or Notch to Be. Blood J. Am. Soc. Hematol. 2012;119:3226–3235. doi: 10.1182/blood-2011-10-355826. [DOI] [PubMed] [Google Scholar]
- 146.Robert-Moreno A., Espinosa L., de la Pompa J.L., Bigas A. RBPjkappa-Dependent Notch Function Regulates Gata2 and Is Essential for the Formation of Intra-Embryonic Hematopoietic Cells. Development. 2005;132:1117–1126. doi: 10.1242/dev.01660. [DOI] [PubMed] [Google Scholar]
- 147.Kumano K., Chiba S., Kunisato A., Sata M., Saito T., Nakagami-Yamaguchi E., Yamaguchi T., Masuda S., Shimizu K., Takahashi T., et al. Notch1 but Not Notch2 Is Essential for Generating Hematopoietic Stem Cells from Endothelial Cells. Immunity. 2003;18:699–711. doi: 10.1016/S1074-7613(03)00117-1. [DOI] [PubMed] [Google Scholar]
- 148.Pajcini K.V., Speck N.A., Pear W.S. Notch Signaling in Mammalian Hematopoietic Stem Cells. Leukemia. 2011;25:1525–1532. doi: 10.1038/leu.2011.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Milner L.A., Kopan R., Martin D.I., Bernstein I.D. A Human Homologue of the Drosophila Developmental Gene, Notch, Is Expressed in CD34 Hematopoietic Precursors. Blood. 1994;83:2057–2062. doi: 10.1182/blood.V83.8.2057.2057. [DOI] [PubMed] [Google Scholar]
- 150.Calvi L.M., Adams G.B., Weibrecht K.W., Weber J.M., Olson D.P., Knight M.C., Martin R.P., Schipani E., Divieti P., Bringhurst F.R., et al. Osteoblastic Cells Regulate the Haematopoietic Stem Cell Niche. Nature. 2003;425:841–846. doi: 10.1038/nature02040. [DOI] [PubMed] [Google Scholar]
- 151.Zeuner A., Francescangeli F., Signore M., Venneri M.A., Pedini F., Felli N., Pagliuca A., Conticello C., De Maria R. The Notch2–Jagged1 Interaction Mediates Stem Cell Factor Signaling in Erythropoiesis. Cell Death Differ. 2010;18:371–380. doi: 10.1038/cdd.2010.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Maillard I., Koch U., Dumortier A., Shestova O., Xu L., Sai H., Pross S.E., Aster J.C., Bhandoola A., Radtke F., et al. Canonical Notch Signaling Is Dispensable for the Maintenance of Adult Hematopoietic Stem Cells. Cell Stem Cell. 2008;2:356–366. doi: 10.1016/j.stem.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Heng T.S.P., The Immunological Genome Project Consortium. Painter M.W., Elpek K., Lukacs-Kornek V., Mauermann N., Turley S.J., Koller D., Kim F.S., Wagers A.J., et al. The Immunological Genome Project: Networks of Gene Expression in Immune Cells. Nat. Immunol. 2008;9:1091–1094. doi: 10.1038/ni1008-1091. [DOI] [PubMed] [Google Scholar]
- 154.Marsboom G., Rehman J. Hypoxia Signaling in Vascular Homeostasis. Physiology. 2018;33:328–337. doi: 10.1152/physiol.00018.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gnecchi-Ruscone G.A., Abondio P., De Fanti S., Sarno S., Sherpa M.G., Sherpa P.T., Marinelli G., Natali L., Di Marcello M., Peluzzi D., et al. Evidence of Polygenic Adaptation to High Altitude from Tibetan and Sherpa Genomes. Genome Biol. Evol. 2018;10:2919–2930. doi: 10.1093/gbe/evy233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wei C., Wang H., Liu G., Zhao F., Kijas J.W., Ma Y., Lu J., Zhang L., Cao J., Wu M., et al. Genome-Wide Analysis Reveals Adaptation to High Altitudes in Tibetan Sheep. Sci. Rep. 2016;6:26770. doi: 10.1038/srep26770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dávila R.D., Julian C.G., Wilson M.J., Browne V.A., Rodriguez C., Bigham A.W., Shriver M.D., Vargas E., Moore L.G. Do Anti-Angiogenic or Angiogenic Factors Contribute to the Protection of Birth Weight at High Altitude Afforded by Andean Ancestry? Reprod. Sci. 2010;17:861–870. doi: 10.1177/1933719110372418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Soria R., Julian C.G., Vargas E., Moore L.G., Giussani D.A. Graduated Effects of High-Altitude Hypoxia and Highland Ancestry on Birth Size. Pediatr. Res. 2013;74:633–638. doi: 10.1038/pr.2013.150. [DOI] [PubMed] [Google Scholar]
- 159.Yu N., Wu J.-L., Xiao J., Fan L., Chen S.-H., Li W. HIF-1α Regulates Angiogenesis via Notch1/STAT3/ETBR Pathway in Trophoblastic Cells. Cell Cycle. 2019;18:3502–3512. doi: 10.1080/15384101.2019.1689481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Limbourg F.P., Takeshita K., Radtke F., Bronson R.T., Chin M.T., Liao J.K. Essential Role of Endothelial Notch1 in Angiogenesis. Circulation. 2005;111:1826–1832. doi: 10.1161/01.CIR.0000160870.93058.DD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Dill M.T., Rothweiler S., Djonov V., Hlushchuk R., Tornillo L., Terracciano L., Meili-Butz S., Radtke F., Heim M.H., Semela D. Disruption of Notch1 Induces Vascular Remodeling, Intussusceptive Angiogenesis, and Angiosarcomas in Livers of Mice. Gastroenterology. 2012;142:967–977.e2. doi: 10.1053/j.gastro.2011.12.052. [DOI] [PubMed] [Google Scholar]
- 162.Benedito R., Hellström M. Notch as a Hub for Signaling in Angiogenesis. Exp. Cell Res. 2013;319:1281–1288. doi: 10.1016/j.yexcr.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 163.Harrington L.S., Sainson R.C.A., Williams C.K., Taylor J.M., Shi W., Li J.-L., Harris A.L. Regulation of Multiple Angiogenic Pathways by Dll4 and Notch in Human Umbilical Vein Endothelial Cells. Microvasc. Res. 2008;75:144–154. doi: 10.1016/j.mvr.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 164.Hellström M., Phng L.-K., Hofmann J.J., Wallgard E., Coultas L., Lindblom P., Alva J., Nilsson A.-K., Karlsson L., Gaiano N., et al. Dll4 Signalling through Notch1 Regulates Formation of Tip Cells during Angiogenesis. Nature. 2007;445:776–780. doi: 10.1038/nature05571. [DOI] [PubMed] [Google Scholar]
- 165.Gale N.W., Dominguez M.G., Noguera I., Pan L., Hughes V., Valenzuela D.M., Murphy A.J., Adams N.C., Lin H.C., Holash J., et al. Haploinsufficiency of Delta-like 4 Ligand Results in Embryonic Lethality Due to Major Defects in Arterial and Vascular Development. Proc. Natl. Acad. Sci. USA. 2004;101:15949–15954. doi: 10.1073/pnas.0407290101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Katoh M., Katoh M. Precision Medicine for Human Cancers with Notch Signaling Dysregulation (Review) Int. J. Mol. Med. 2020;45:279–297. doi: 10.3892/ijmm.2019.4418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Noguera-Troise I., Daly C., Papadopoulos N.J., Coetzee S., Boland P., Gale N.W., Lin H.C., Yancopoulos G.D., Thurston G. Blockade of Dll4 Inhibits Tumour Growth by Promoting Non-Productive Angiogenesis. Nature. 2006;444:1032–1037. doi: 10.1038/nature05355. [DOI] [PubMed] [Google Scholar]
- 168.Ridgway J., Zhang G., Wu Y., Stawicki S., Liang W.-C., Chanthery Y., Kowalski J., Watts R.J., Callahan C., Kasman I., et al. Inhibition of Dll4 Signalling Inhibits Tumour Growth by Deregulating Angiogenesis. Nature. 2006;444:1083–1087. doi: 10.1038/nature05313. [DOI] [PubMed] [Google Scholar]
- 169.Wieland E., Rodriguez-Vita J., Liebler S.S., Mogler C., Moll I., Herberich S.E., Espinet E., Herpel E., Menuchin A., Chang-Claude J., et al. Endothelial Notch1 Activity Facilitates Metastasis. Cancer Cell. 2017;31:355–367. doi: 10.1016/j.ccell.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 170.Wohlfeil S.A., Häfele V., Dietsch B., Schledzewski K., Winkler M., Zierow J., Leibing T., Mohammadi M.M., Heineke J., Sticht C., et al. Hepatic Endothelial Notch Activation Protects against Liver Metastasis by Regulating Endothelial-Tumor Cell Adhesion Independent of Angiocrine Signaling. Cancer Res. 2019;79:598–610. doi: 10.1158/0008-5472.CAN-18-1752. [DOI] [PubMed] [Google Scholar]
- 171.Woolard J., Bevan H.S., Harper S.J., Bates D.O. Molecular Diversity of VEGF-A as a Regulator of Its Biological Activity. Microcirculation. 2009;16:572–592. doi: 10.1080/10739680902997333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Pan Q., Chathery Y., Wu Y., Rathore N., Tong R.K., Peale F., Bagri A., Tessier-Lavigne M., Koch A.W., Watts R.J. Neuropilin-1 Binds to VEGF121 and Regulates Endothelial Cell Migration and Sprouting. J. Biol. Chem. 2007;282:24049–24056. doi: 10.1074/jbc.M703554200. [DOI] [PubMed] [Google Scholar]
- 173.Abou Faycal C., Gazzeri S., Eymin B. A VEGF-A/SOX2/SRSF2 Network Controls VEGFR1 Pre-MRNA Alternative Splicing in Lung Carcinoma Cells. Sci. Rep. 2019;9:336. doi: 10.1038/s41598-018-36728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Boeckel J.-N., Guarani V., Koyanagi M., Roexe T., Lengeling A., Schermuly R.T., Gellert P., Braun T., Zeiher A., Dimmeler S. Jumonji Domain-Containing Protein 6 (Jmjd6) Is Required for Angiogenic Sprouting and Regulates Splicing of VEGF-Receptor 1. Proc. Natl. Acad. Sci. USA. 2011;108:3276–3281. doi: 10.1073/pnas.1008098108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kangsamaksin T., Murtomaki A., Kofler N.M., Cuervo H., Chaudhri R.A., Tattersall I.W., Rosenstiel P.E., Shawber C.J., Kitajewski J. NOTCH Decoys That Selectively Block DLL/NOTCH or JAG/NOTCH Disrupt Angiogenesis by Unique Mechanisms to Inhibit Tumor Growth. Cancer Discov. 2015;5:182–197. doi: 10.1158/2159-8290.CD-14-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Xu X.-Q., Jing Z.-C. High-Altitude Pulmonary Hypertension. Eur. Respir. Rev. 2009;18:13–17. doi: 10.1183/09059180.00011104. [DOI] [PubMed] [Google Scholar]
- 177.Groves B.M., Droma T., Sutton J.R., McCullough R.G., McCullough R.E., Zhuang J., Rapmund G., Sun S., Janes C., Moore L.G. Minimal Hypoxic Pulmonary Hypertension in Normal Tibetans at 3,658 m. J. Appl. Physiol. 1993;74:312–318. doi: 10.1152/jappl.1993.74.1.312. [DOI] [PubMed] [Google Scholar]
- 178.Mol B.W.J., Roberts C.T., Thangaratinam S., Magee L.A., de Groot C.J.M., Hofmeyr G.J. Pre-Eclampsia. Lancet. 2016;387:999–1011. doi: 10.1016/S0140-6736(15)00070-7. [DOI] [PubMed] [Google Scholar]
- 179.Keyes L.E., Armaza J.F., Niermeyer S., Vargas E., Young D.A., Moore L.G. Intrauterine Growth Restriction, Preeclampsia, and Intrauterine Mortality at High Altitude in Bolivia. Pediatr. Res. 2003;54:20–25. doi: 10.1203/01.PDR.0000069846.64389.DC. [DOI] [PubMed] [Google Scholar]
- 180.Palmer S.K., Moore L.G., Young D., Cregger B., Berman J.C., Zamudio S. Altered Blood Pressure Course during Normal Pregnancy and Increased Preeclampsia at High Altitude (3100 Meters) in Colorado. Am. J. Obstet. Gynecol. 1999;180:1161–1168. doi: 10.1016/S0002-9378(99)70611-3. [DOI] [PubMed] [Google Scholar]
- 181.Esteve-Valverde E., Ferrer-Oliveras R., Gil-Aliberas N., Baraldès-Farré A., Llurba E., Alijotas-Reig J. Pravastatin for Preventing and Treating Preeclampsia: A Systematic Review. Obstet. Gynecol. Surv. 2018;73:40–55. doi: 10.1097/OGX.0000000000000522. [DOI] [PubMed] [Google Scholar]
- 182.Murray A.J. Energy Metabolism and the High-altitude Environment. Exp. Physiol. :2016. doi: 10.1113/EP085317. [DOI] [PubMed] [Google Scholar]
- 183.Chicco A.J., Le C.H., Gnaiger E., Dreyer H.C., Muyskens J.B., D’Alessandro A., Nemkov T., Hocker A.D., Prenni J.E., Wolfe L.M., et al. Adaptive Remodeling of Skeletal Muscle Energy Metabolism in High-Altitude Hypoxia: Lessons from AltitudeOmics. J. Biol. Chem. 2018;293:6659–6671. doi: 10.1074/jbc.RA117.000470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Levett D.Z.H., Viganò A., Capitanio D., Vasso M., De Palma S., Moriggi M., Martin D.S., Murray A.J., Cerretelli P., Grocott M.P.W., et al. Changes in Muscle Proteomics in the Course of the Caudwell Research Expedition to Mt. Everest. Proteomics. 2015;15:160–171. doi: 10.1002/pmic.201400306. [DOI] [PubMed] [Google Scholar]
- 185.Papandreou I., Cairns R.A., Fontana L., Lim A.L., Denko N.C. HIF-1 Mediates Adaptation to Hypoxia by Actively Downregulating Mitochondrial Oxygen Consumption. Cell Metab. 2006;3:187–197. doi: 10.1016/j.cmet.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 186.Bi P., Kuang S. Notch Signaling as a Novel Regulator of Metabolism. Trends Endocrinol. Metab. 2015;26:248–255. doi: 10.1016/j.tem.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kodama K., Tojjar D., Yamada S., Toda K., Patel C.J., Butte A.J. Ethnic Differences in the Relationship Between Insulin Sensitivity and Insulin Response: A Systematic Review and Meta-Analysis. Diabetes Care. 2013;36:1789–1796. doi: 10.2337/dc12-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Schenk S., Saberi M., Olefsky J.M. Insulin Sensitivity: Modulation by Nutrients and Inflammation. J. Clin. Investig. 2008;118:2992–3002. doi: 10.1172/JCI34260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Iiyori N., Alonso L.C., Li J., Sanders M.H., Garcia-Ocana A., O’Doherty R.M., Polotsky V.Y., O’Donnell C.P. Intermittent Hypoxia Causes Insulin Resistance in Lean Mice Independent of Autonomic Activity. Am. J. Respir. Crit. Care Med. 2007;175:851–857. doi: 10.1164/rccm.200610-1527OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Lecoultre V., Peterson C.M., Covington J.D., Ebenezer P.J., Frost E.A., Schwarz J.-M., Ravussin E. Ten Nights of Moderate Hypoxia Improves Insulin Sensitivity in Obese Humans. Diabetes Care. 2013;36:e197–e198. doi: 10.2337/dc13-1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hasan S.S., Jabs M., Taylor J., Wiedmann L., Leibing T., Nordström V., Federico G., Roma L.P., Carlein C., Wolff G., et al. Endothelial Notch Signaling Controls Insulin Transport in Muscle. EMBO Mol. Med. 2020;12:e09271. doi: 10.15252/emmm.201809271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.O’Brien K.A., Atkinson R.A., Richardson L., Koulman A., Murray A.J., Harridge S.D.R., Martin D.S., Levett D.Z.H., Mitchell K., Mythen M.G., et al. Metabolomic and Lipidomic Plasma Profile Changes in Human Participants Ascending to Everest Base Camp. Sci. Rep. 2019;9:2297. doi: 10.1038/s41598-019-38832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Cole M.A., Abd Jamil A.H., Heather L.C., Murray A.J., Sutton E.R., Slingo M., Sebag-Montefiore L., Tan S.C., Aksentijević D., Gildea O.S., et al. On the Pivotal Role of PPARa in Adaptation of the Heart to Hypoxia and Why Fat in the Diet Increases Hypoxic Injury. FASEB J. 2016;30:2684–2697. doi: 10.1096/fj.201500094R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ivashkiv L.B. The Hypoxia–Lactate Axis Tempers Inflammation. Nat. Rev. Immunol. 2019;20:85–86. doi: 10.1038/s41577-019-0259-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Xu J., Chi F., Guo T., Punj V., Lee W.N.P., French S.W., Tsukamoto H. NOTCH Reprograms Mitochondrial Metabolism for Proinflammatory Macrophage Activation. J. Clin. Investig. 2015;125:1579–1590. doi: 10.1172/JCI76468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.DeBerardinis R.J., Mancuso A., Daikhin E., Nissim I., Yudkoff M., Wehrli S., Thompson C.B. Beyond Aerobic Glycolysis: Transformed Cells Can Engage in Glutamine Metabolism That Exceeds the Requirement for Protein and Nucleotide Synthesis. Proc. Natl. Acad. Sci. USA. 2007;104:19345–19350. doi: 10.1073/pnas.0709747104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wang Y., Bai C., Ruan Y., Liu M., Chu Q., Qiu L., Yang C., Li B. Coordinative Metabolism of Glutamine Carbon and Nitrogen in Proliferating Cancer Cells under Hypoxia. Nat. Commun. 2019;10:201. doi: 10.1038/s41467-018-08033-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Hoppeler H., Howald H., Cerretelli P. Human Muscle Structure after Exposure to Extreme Altitude. Experientia. 1990;46:1185–1187. doi: 10.1007/BF01936933. [DOI] [PubMed] [Google Scholar]
- 199.Ashmore T., Fernandez B.O., Branco-Price C., West J.A., Cowburn A.S., Heather L.C., Griffin J.L., Johnson R.S., Feelisch M., Murray A.J. Dietary Nitrate Increases Arginine Availability and Protects Mitochondrial Complex I and Energetics in the Hypoxic Rat Heart. J. Physiol. 2014;592:4715–4731. doi: 10.1113/jphysiol.2014.275263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Valenti L., Mendoza R.M., Rametta R., Maggioni M., Kitajewski C., Shawber C.J., Pajvani U.B. Hepatic Notch Signaling Correlates with Insulin Resistance and Nonalcoholic Fatty Liver Disease. Diabetes. 2013;62:4052–4062. doi: 10.2337/db13-0769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Li H., Lee J., He C., Zou M.-H., Xie Z. Suppression of the MTORC1/STAT3/Notch1 Pathway by Activated AMPK Prevents Hepatic Insulin Resistance Induced by Excess Amino Acids. Am. J. Physiol. Endocrinol. Metab. 2014;306:E197–E209. doi: 10.1152/ajpendo.00202.2013. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 202.Eltzschig H.K., Carmeliet P. Hypoxia and Inflammation. N. Engl. J. Med. 2011;364:656–665. doi: 10.1056/NEJMra0910283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Korbecki J., Simińska D., Gąssowska-Dobrowolska M., Listos J., Gutowska I., Chlubek D., Baranowska-Bosiacka I. Chronic and Cycling Hypoxia: Drivers of Cancer Chronic Inflammation through HIF-1 and NF-ΚB Activation: A Review of the Molecular Mechanisms. Int. J. Mol. Sci. 2021;22:10701. doi: 10.3390/ijms221910701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Osipo C., Golde T.E., Osborne B.A., Miele L.A. Off the Beaten Pathway: The Complex Cross Talk between Notch and NF-ΚB. Lab. Investig. 2007;88:11–17. doi: 10.1038/labinvest.3700700. [DOI] [PubMed] [Google Scholar]
- 205.Poellinger L., Lendahl U. Modulating Notch Signaling by Pathway-Intrinsic and Pathway-Extrinsic Mechanisms. Curr. Opin. Genet. Dev. 2008;18:449–454. doi: 10.1016/j.gde.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 206.Samon J.B., Champhekar A., Minter L.M., Telfer J.C., Miele L., Fauq A., Das P., Golde T.E., Osborne B.A. Notch1 and TGFβ1 Cooperatively Regulate Foxp3 Expression and the Maintenance of Peripheral Regulatory T Cells. Blood J. Am. Soc. Hematol. 2008;112:1813–1821. doi: 10.1182/blood-2008-03-144980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Radtke F., MacDonald H.R., Tacchini-Cottier F. Regulation of Innate and Adaptive Immunity by Notch. Nat. Rev. Immunol. 2013;13:427–437. doi: 10.1038/nri3445. [DOI] [PubMed] [Google Scholar]
- 208.Radtke F., Wilson A., Stark G., Bauer M., van Meerwijk J., MacDonald H.R., Aguet M. Deficient T Cell Fate Specification in Mice with an Induced Inactivation of Notch1. Immunity. 1999;10:547–558. doi: 10.1016/S1074-7613(00)80054-0. [DOI] [PubMed] [Google Scholar]
- 209.Liu Z.-J., Tan Y., Beecham G.W., Seo D.M., Tian R., Li Y., Vazquez-Padron R.I., Pericak-Vance M., Vance J.M., Goldschmidt-Clermont P.J., et al. Notch Activation Induces Endothelial Cell Senescence and Pro-Inflammatory Response: Implication of Notch Signaling in Atherosclerosis. Atherosclerosis. 2012;225:296–303. doi: 10.1016/j.atherosclerosis.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Görlach A., Dimova E.Y., Petry A., Martínez-Ruiz A., Hernansanz-Agustín P., Rolo A.P., Palmeira C.M., Kietzmann T. Reactive Oxygen Species, Nutrition, Hypoxia and Diseases: Problems Solved? Redox Biol. 2015;6:372–385. doi: 10.1016/j.redox.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Lando D., Pongratz I., Poellinger L., Whitelaw M.L. A Redox Mechanism Controls Differential DNA Binding Activities of Hypoxia-Inducible Factor (HIF) 1α and the HIF-like Factor. J. Biol. Chem. 2000;275:4618–4627. doi: 10.1074/jbc.275.7.4618. [DOI] [PubMed] [Google Scholar]
- 212.Bailey D.M., Rimoldi S.F., Rexhaj E., Pratali L., Salinas Salmòn C., Villena M., McEneny J., Young I.S., Nicod P., Allemann Y., et al. Oxidative-Nitrosative Stress and Systemic Vascular Function in Highlanders with and without Exaggerated Hypoxemia. Chest. 2013;143:444–451. doi: 10.1378/chest.12-0728. [DOI] [PubMed] [Google Scholar]
- 213.Bailey D.M., Brugniaux J.V., Filipponi T., Marley C.J., Stacey B., Soria R., Rimoldi S.F., Cerny D., Rexhaj E., Pratali L., et al. Exaggerated Systemic Oxidative-Inflammatory-Nitrosative Stress in Chronic Mountain Sickness Is Associated with Cognitive Decline and Depression. J. Physiol. 2019;597:611–629. doi: 10.1113/JP276898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Yu H.-C., Qin H.-Y., He F., Wang L., Fu W., Liu D., Guo F.-C., Liang L., Dou K.-F., Han H. Canonical Notch Pathway Protects Hepatocytes from Ischemia/Reperfusion Injury in Mice by Repressing Reactive Oxygen Species Production through JAK2/STAT3 Signaling. Hepatology. 2011;54:979–988. doi: 10.1002/hep.24469. [DOI] [PubMed] [Google Scholar]
- 215.Coant N., Ben Mkaddem S., Pedruzzi E., Guichard C., Tréton X., Ducroc R., Freund J.-N., Cazals-Hatem D., Bouhnik Y., Woerther P.-L., et al. NADPH Oxidase 1 Modulates WNT and NOTCH1 Signaling to Control the Fate of Proliferative Progenitor Cells in the Colon. Mol. Cell. Biol. 2010;30:2636–2650. doi: 10.1128/MCB.01194-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Hall J.E., Lawrence E.S., Simonson T.S., Fox K. Seq-Ing Higher Ground: Functional Investigation of Adaptive Variation Associated With High-Altitude Adaptation. Front. Genet. 2020;11:471. doi: 10.3389/fgene.2020.00471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.O’Brien K.A., Griffin J.L., Murray A.J., Edwards L.M. Mitochondrial Responses to Extreme Environments: Insights from Metabolomics. Extrem. Physiol. Med. 2015;4:7. doi: 10.1186/s13728-015-0026-9. [DOI] [PMC free article] [PubMed] [Google Scholar]