Abstract
We assessed physicians’ experiences of prescribing once-weekly (OW) semaglutide to patients with type 2 diabetes (T2D) in Canada. Physicians who had prescribed OW semaglutide to ≥2 patients with T2D in the past 12 months and had been doing so for ≥3 months were surveyed during 1–17 October 2018. Prescribing reasons, treatment satisfaction and reasons for discontinuation were assessed. Of the 50 participants, 72% and 54% were prescribed OW semaglutide due to its superior glycemic control and effect on weight, respectively. Most physicians were more satisfied with injection frequency (62%), effect on weight (60%), achieving HbA1c target (54%) and therapy simplicity (50%) with OW semaglutide versus other glucagon-like peptide-1 receptor agonists. Treatment discontinuations in 13% of OW semaglutide-treated patients were reported by physicians, primarily due to gastrointestinal symptoms (70%). The survey suggests that physicians are satisfied with the OW semaglutide clinical effects.
Video Abstract: http://links.lww.com/CAEN/A34
Keywords: injection, once-weekly, physician experience, semaglutide, survey, treatment satisfaction, type 2 diabetes
Introduction
Once-weekly (OW) subcutaneous semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) approved in Canada on 4 January 2018 for treating adults with type 2 diabetes (T2D) [1]. OW semaglutide was proven to be a safe and efficacious intervention across multiple patient populations with T2D, as monotherapy and combined with oral antihyperglycemic drugs (OADs) or insulin [2–8].
The Diabetes Canada pharmacotherapy guidelines recommend GLP-1 RAs as add-on to metformin if glycemic target cannot be attained with metformin alone [9]. This survey studied the characteristics of patients initiating OW semaglutide and the characteristics, perception, behavior and experiences of physicians who have prescribed OW semaglutide to patients with T2D in Canada.
Methods
Survey design and participants
A structured online survey for primary care practitioners (PCPs) and specialists treating patients with T2D was conducted from 1–17 October 2018 in Canada (end of the survey); the target sample size of 50 physicians was met. Eligible physicians included those who had prescribed OW semaglutide to at least two patients with T2D in the past 12 months and had been doing so for at least 3 months.
Informed consent process, confidentiality and data protection
Participants consented to have their contact details forwarded to the sponsor for reporting of adverse effects. Personal information and responses of participants were kept confidential, and applicable data protection laws were followed.
Survey questionnaire and administration
The survey questionnaire extracted information on characteristics of prescribing physicians and patients who were prescribed OW semaglutide, prescribing reasons, treatment response, physicians’ satisfaction, reasons for discontinuation, and physician and patient concerns with OW semaglutide, compared with other GLP-1 RAs (Supplementary Material, Supplemental Digital Content 2, http://links.lww.com/CAEN/A35).
Physicians were asked to rank statements from one to five regarding reasons to prescribe OW semaglutide (rank 1–2 = agree; rank 3 = neither agree nor disagree; rank 4–5 = disagree) and characteristics of patients receiving OW semaglutide. Physicians ranked statements regarding satisfaction level in five increments, from ‘much more satisfied with OW semaglutide than other GLP-1 RAs’ to ‘much more satisfied with other GLP-1 RAs than OW semaglutide’, or ‘don’t know’.
Analysis
All data were based on the fully completed surveys and analyzed using a t-test at a 90% confidence limit.
Results
Characteristics of physicians who prescribed and patients who were prescribed once-weekly semaglutide
On average, for each physician, 546 patients with T2D were seen in the past 12 months, and 42 were treated with OW semaglutide (overall 50 participants, Table 1). Nearly half (48%) of physicians had at least 4 months of experience prescribing OW semaglutide. Of the patients prescribed OW semaglutide, 94% had inadequately controlled blood glucose, and 78% were overweight/obese (Table 2).
Table 1.
Characteristics of 50 surveyed physicians prescribing once-weekly semaglutide to patients with type 2 diabetes in Canada
| Total | PCPs | Specialists | |
|---|---|---|---|
| 50 (100) | 25 (100) | 25 (100) | |
| Primary specialty | |||
| General/family practice | 23 (46) | 23 (92) | ND |
| Internal medicine | 2 (4) | 2 (8) | ND |
| Cardiology | 9 (18) | ND | 9 (36) |
| Endocrinology | 13 (26) | ND | 13 (52) |
| Diabetology | 3 (6) | ND | 3 (12) |
| Time since first prescription of OW semaglutide | |||
| 3 months | 16 (32) | 7 (28) | 9 (36) |
| 3 to ≤4 months | 10 (20) | 6 (24) | 4 (16) |
| 4 to ≤5 months | 5 (10) | 2 (8) | 3 (12) |
| 5 to ≤6 months | 14 (28) | 6 (24) | 8 (32) |
| 6 to ≤7 months | 5 (10) | 4 (16) | 1 (4) |
| Time since last prescription of OW semaglutide | |||
| <14 days | 35 (70) | 19 (76) | 16 (64) |
| 15 days to ≤1 month | 9 (18) | 5 (20) | 4 (16) |
| 1 to ≤2 months | 5 (10) | 1 (4) | 4 (16) |
| 2 to ≤3 months | 0 (0) | 0 (0) | 0 (0) |
| 3 to ≤4 months | 1 (2) | 0 (0) | 1 (4) |
| Average number of patients with T2D seen per responder in the last 12 months | 546 (100) | 385 (100) | 707 (100) |
| Patients with T2D treated with OW semaglutide per responder | 42 (8) | 39 (10) | 45 (6) |
Data presented are n (%) unless otherwise stated.
OW, once-weekly; ND, no data; PCPs, primary care practitioners; T2D, type 2 diabetes.
Table 2.
Characteristics of patients with type 2 diabetes at once-weekly semaglutide initiation, as reported by 50 prescribing physicians in Canada
| Total | PCPs | Specialists | |
|---|---|---|---|
| Baseline treatment regimen, % | |||
| 1 OAD | 26 | 27 | 24 |
| 2 OADsa | 28 | 36 | 19 |
| ≥3 OADs | 14 | 11 | 18 |
| GLP-1 RA ± OAD | 7 | 7 | 8 |
| Basal ± OAD | 12 | 9 | 14 |
| Basal + bolus ± OADa | 7 | 4 | 10 |
| Basal + GLP-1 RA ± OAD | 5 | 4 | 5 |
| CSII/insulin pump | 0 | 0 | 0 |
| Treatment-naïve | 1 | 1 | 2 |
| Age, % | |||
| <18 years | 1 | 1 | 1 |
| 18–25 years | 7 | 5 | 9 |
| 36–50 years | 33 | 34 | 33 |
| 51–65 years | 40 | 43 | 36 |
| >65 years | 19 | 17 | 21 |
| BMI, % | |||
| <30 kg/m2 | 13 | 12 | 14 |
| 30–35 kg/m2 | 46 | 47 | 46 |
| >35 kg/m2 | 38 | 40 | 36 |
| Unknown | 3 | 2 | 5 |
| HbA1c, % | |||
| <7.0% (53 mmol/mol) | 4 | 3 | 5 |
| 7.0–7.5% (53–59 mmol/mol) | 14 | 15 | 14 |
| 7.5–8.0% (59–64 mmol/mol) | 24 | 23 | 25 |
| 8.0–8.5% (64–69 mmol/mol) | 27 | 29 | 25 |
| 8.5–9.0% (69–75 mmol/mol) | 18 | 20 | 17 |
| >9.0% (75 mmol/mol) | 12 | 10 | 15 |
| Patients with inadequately controlled blood glucose (HbA1c), % | 94 | 92 | 96 |
| Patients with excess weight, % | 78 | 88 | 68 |
| Patients who find adherence to previous treatment difficult, % | 60 | 64 | 56 |
| Patients with established CV risk, such as previous stroke or MIa, % | 56 | 76 | 36 |
| Patients with risk of hypoglycemia, % | 46 | 52 | 40 |
Percentage values may not total 100 due to rounding.
CSII, continuous subcutaneous insulin infusion; CV, cardiovascular; GLP-1 RA, glucagon-like peptide-1 receptor agonist; HbA1c, glycated hemoglobin; MI, myocardial infarction; n, number of patients; OADs, oral antihyperglyemic drugs; OW, once-weekly; PCPs, primary care practitioners; T2D, type 2 diabetes.
aSignificant difference between PCPs and specialists at the 90% confidence limit.
Reasons for prescribing once-weekly semaglutide to patients with type 2 diabetes
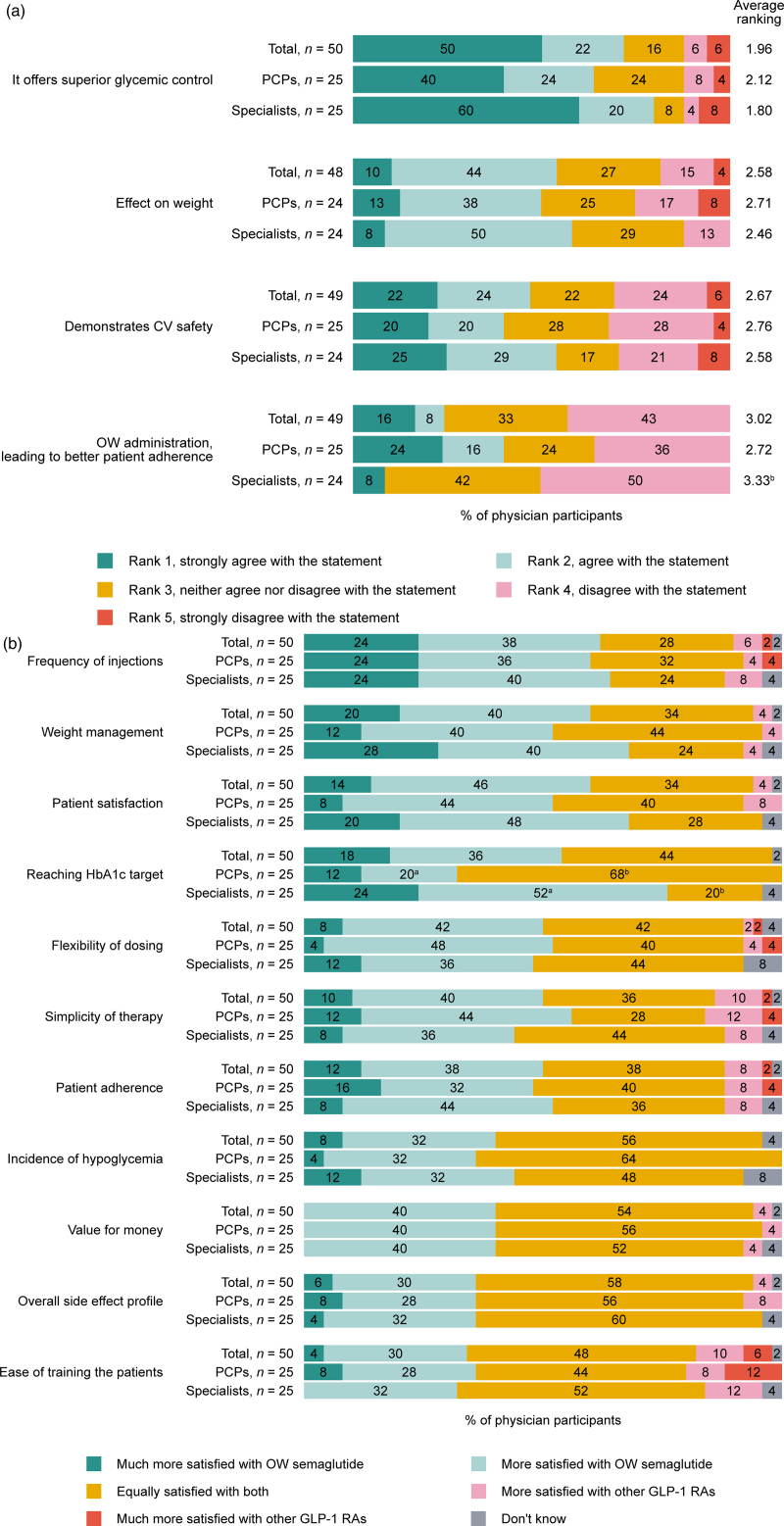
Of all the participating physicians, 72% and 54% cited superior glycemic control versus other GLP-1 RAs and effect on weight as their reasons for prescribing OW semaglutide, respectively (Fig. 1a). Fewer physicians cited cardiovascular (CV) safety (46%) and OW administration (24%) as their reasons for prescribing OW semaglutide (Fig. 1a).
Fig. 1.
(a) Reasons for prescribing OW semaglutide for patients with T2Da, as reported by 50 prescribing physicians in Canada. (b) Physicians’ satisfaction level with OW semaglutide compared with other GLP-1 RAs for patients with T2D. (a) Percentage values may not total 100 due to rounding. Question: What are your main reasons for prescribing Ozempic (semaglutide) to your patients with T2D? aOther reasons included: it provides immediate results and better device option, it offers value for money and it is not applicable. bThe average ranking from specialists was significantly higher than that from the PCPs at 90% confidence limit. CV, cardiovascular; n, number of patients; OW, once-weekly; PCPs, primary care practitioners; T2D, type 2 diabetes. (b) Question: please compare your level of satisfaction when treating patients with Ozempic (semaglutide) compared with other GLP-1 RAs based on each of the following. aSignificantly more specialists were satisfied with OW semaglutide compared with PCPs at 90% confidence limit. bSignificantly more PCPs were equality satisfied with OW semaglutide and other GLP-1 RAs, compared with specialists at 90% confidence limit. GLP-1 RA, glucagon-like peptide-1 receptor agonist; HbA1c, glycated hemoglobin; OW, once-weekly; n, number of participants; PCP, primary care practitioner; T2D, type 2 diabetes.
Treatment response
Physicians prescribed OW semaglutide alone, OW semaglutide + OADs and OW semaglutide + insulin to 12%, 69% and 19% of their patients, respectively. Following OW semaglutide initiation, physicians reported that 65% of their patients had reached their glycemic target, and 55% of patients’ HbA1c was lower than 7% (Supplementary Material, Fig. S1, Supplemental Digital Content 2, http://links.lww.com/CAEN/A35). Furthermore, PCPs were more inclined to use the 0.5-mg maintenance dose of OW semaglutide, whereas specialists were inclined to use the 1-mg maintenance dose (Fig. S2, Supplemental Digital Content 2, http://links.lww.com/CAEN/A35).
Physicians’ satisfaction compared with other glucagon-like peptide-1 receptor agonists
Most physicians were more satisfied with frequency of injections (62%), weight management (60%), achieving HbA1c target (54%) and simplicity of therapy (50%) with OW semaglutide versus other GLP-1 RAs (Fig. 1b).
Discontinuation of once-weekly semaglutide
According to physicians, ~13% of their patients who initiated OW semaglutide discontinued the treatment due to gastrointestinal (GI) side effects (70%), treatment affordability (69%), insufficient weight loss (39%) and desired blood glucose control not fully achieved (39%) (Supplementary Material, Fig. S3, Supplemental Digital Content 2, http://links.lww.com/CAEN/A35). Of the patients who discontinued the treatment, 43% were reported to have done so within the first month and 78% within the first 3 months of initiation.
Physician and patient concerns with once-weekly semaglutide
According to the participating physicians, the most common patient concerns with OW semaglutide were treatment affordability and GI side effects (Supplementary Material, Fig. S4, Supplemental Digital Content 2, http://links.lww.com/CAEN/A35). When asked to compare these concerns with OW semaglutide versus other GLP-1 RAs, 98% and 92% of physicians, respectively, stated they were either equally or less concerned with OW semaglutide. Regarding patients’ confidence in treatments, 68% of physicians reported that patients felt more motivated to reach their glycemic target, and an additional 30% of physicians reported patients felt equally motivated to reach their glycemic target with OW semaglutide versus other GLP-1 RAs.
Discussion
Results in this survey provide insights into the real-world experiences of physicians who prescribed OW semaglutide to patients with T2D in Canada.
Most physicians prescribed OW semaglutide due to its superior glycemic control and weight loss benefit, consistent with previous studies [2,3,5–8,10,11]. CV safety was the third most popular reason, probably because at the time of the survey, no CV benefit of OW semaglutide was cited by any regulatory labels [12–14]. However, current guidelines are shifting focus to the CV benefit of glucose-lowering medications [15–17], and the CV safety/benefit of OW semaglutide has been included [9,17].
Top reasons for treatment discontinuation cited by the physicians were GI side effects and treatment affordability, consistent with the safety of OW semaglutide [2–5,7,8] and previous literature [18,19].
Of note, at the time of the survey, OW semaglutide was not publicly reimbursed in Canada and was only recommended to be reimbursed in 2019 [20]. Given the cost-effectiveness of OW semaglutide [21–28], it may represent a more cost-effective treatment option versus other GLP-1 RAs. Moreover, given the timing of the survey in 2018, when OW semaglutide was new to the market, our report likely provides conservative opinions. Physician experience in 2022 may be increasingly positive, as OW semaglutide is more widely prescribed [29,30] and recommended as a second-line agent in the Diabetes Canada Guidelines [17].
One limitation is that the findings are heavily based on a small number of physicians’ experiences.
Conclusion
In this survey, most physicians prescribed OW semaglutide due to its superior glycemic effects and effect on weight, and were more satisfied with OW semaglutide versus other GLP-1 RAs. Participating physicians believed that patients with T2D taking OW semaglutide were more satisfied with the frequency of injections and more confident in reaching their glycemic target versus other GLP-1 RAs.
Acknowledgements
Writing and editorial support was provided by Jin Heppell, PhD, and Izabel James, MBBS, of Ashfield MedComms, an Ashfield Health company, funded by Novo Nordisk A/S (Søborg, Denmark). This study and the journal’s Rapid Service were sponsored by Novo Nordisk A/S (Søborg, Denmark).
Part of the manuscript has been previously presented at the Diabetes Canada/Canadian Society of Endocrinology and Metabolism Professional Conference, 2–5 October 2019, Winnipeg, MB, Canada.
Participating physicians provided their consent to participate in the study and waived confidentiality so that their names/contact details could be forwarded to the sponsor’s pharmacovigilance department in the event of reported adverse effects. However, no mechanisms were in place to associate names of the physicians with responses given. Personal information of participants were anonymized, and responses remained confidential. Participating physicians were informed that data would be stored securely on IQVIA servers, in accordance with applicable data protection laws, only for as long as necessary, for the purposes of use outlined in study agreement. The study was performed in accordance with the General Data Protection Regulation and Novo Nordisk A/S adverse events and compliance requirements.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of interest
K.Q.: honoraria and/or grant support from Novo Nordisk, Merck, Eli Lily, BI, AstraZeneca and Abbot. A.A.M.Z. and A.L.: employees of Novo Nordisk Canada Inc. A.R.K. and M.L.W.: employees and shareholders of Novo Nordisk A/S.
Supplementary Material
Footnotes
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.cardiovascularendocrinology.com.
References
- 1.Novo Nordisk Canada. Ozempic product monograph including patient medication information. https://www.novonordisk.ca/content/dam/Canada/AFFILIATE/www-novonordisk-ca/OurProducts/PDF/ozempic-product-monograph.pdf. [Accessed on 2 December 2020]
- 2.Ahmann AJ, Capehorn M, Charpentier G, Dotta F, Henkel E, Lingvay I, et al. Efficacy and safety of once-weekly semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN 3): a 56-week, open-label, randomized clinical trial. Diabetes Care 2018;41:258–266. [DOI] [PubMed] [Google Scholar]
- 3.Ahrén B, Masmiquel L, Kumar H, Sargin M, Karsbøl JD, Jacobsen SH, Chow F. Efficacy and safety of once-weekly semaglutide versus once-daily sitagliptin as an add-on to metformin, thiazolidinediones, or both, in patients with type 2 diabetes (SUSTAIN 2): a 56-week, double-blind, phase 3a, randomised trial. Lancet Diabetes Endocrinol 2017;5:341–354. [DOI] [PubMed] [Google Scholar]
- 4.Rodbard HW, Lingvay I, Reed J, de la Rosa R, Rose L, Sugimoto D, et al. Semaglutide added to basal insulin in type 2 diabetes (SUSTAIN 5): a randomized, controlled trial. J Clin Endocrinol Metab 2018;103:2291–2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aroda VR, Bain SC, Cariou B, Piletič M, Rose L, Axelsen M, et al. Efficacy and safety of once-weekly semaglutide versus once-daily insulin glargine as add-on to metformin (with or without sulfonylureas) in insulin-naive patients with type 2 diabetes (SUSTAIN 4): a randomised, open-label, parallel-group, multicentre, multinational, phase 3a trial. Lancet Diabetes Endocrinol 2017;5:355–366. [DOI] [PubMed] [Google Scholar]
- 6.Capehorn MS, Catarig AM, Furberg JK, Janez A, Price HC, Tadayon S, et al. Efficacy and safety of once-weekly semaglutide 1.0mg vs once-daily liraglutide 1.2mg as add-on to 1-3 oral antidiabetic drugs in subjects with type 2 diabetes (SUSTAIN 10). Diabetes Metab 2020;46:100–109. [DOI] [PubMed] [Google Scholar]
- 7.Lingvay I, Catarig AM, Frias JP, Kumar H, Lausvig NL, le Roux CW, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes (SUSTAIN 8): a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol 2019;7:834–844. [DOI] [PubMed] [Google Scholar]
- 8.Pratley RE, Aroda VR, Lingvay I, Lüdemann J, Andreassen C, Navarria A, Viljoen A; SUSTAIN 7 investigators. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol 2018;6:275–286. [DOI] [PubMed] [Google Scholar]
- 9.Ivers NM, Jiang M, Alloo J, Singer A, Ngui D, Casey CG, Yu CH. Diabetes Canada 2018 clinical practice guidelines: key messages for family physicians caring for patients living with type 2 diabetes. Can Fam Physician 2019;65:14–24. [PMC free article] [PubMed] [Google Scholar]
- 10.Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al.; SUSTAIN-6 Investigators. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834–1844. [DOI] [PubMed] [Google Scholar]
- 11.Matza LS, Curtis SE, Jordan JB, Adetunji O, Martin SA, Boye KS. Physician perceptions of GLP-1 receptor agonists in the UK. Curr Med Res Opin 2016;32:857–864. [DOI] [PubMed] [Google Scholar]
- 12.Food and Drug Administration. Ozempic prescribing information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209637lbl.pdf. [Accessed on January 2021]
- 13.Novo Nordisk Canada. Ozempic product monograph. 2018. https://pdf4pro.com/amp/fullscreen/product-monograph-template-novo-nordisk-243a55.html. [Accessed on January 2021]
- 14.European Medicines Agency. Ozempic assessment report. 2017. https://www.ema.europa.eu/en/documents/assessment-report/ozempic-epar-public-assessment-report_en.pdf. [Accessed on January 2021]
- 15.Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2019:dci190066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2021. Diabetes Care 2021;44(Suppl 1):S111–S124. [DOI] [PubMed] [Google Scholar]
- 17.Lipscombe L, Butalia S, Dasgupta K, Eurich DT, MacCallum L, Shah BR, et al. Pharmacologic glycemic management of type 2 diabetes in adults: 2020 update. Can J Diabetes 2020;44:575–591. [DOI] [PubMed] [Google Scholar]
- 18.Sikirica MV, Martin AA, Wood R, Leith A, Piercy J, Higgins V. Reasons for discontinuation of GLP1 receptor agonists: data from a real-world cross-sectional survey of physicians and their patients with type 2 diabetes. Diabetes Metab Syndr Obes 2017;10:403–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brod M, Basse A, Markert M, Pfeiffer KM. Post-basal insulin intensification and healthcare resource use in type 2 diabetes: a web-based physician survey in the United States and United Kingdom. Diabetes Ther 2019;10:1323–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Canadian Agency for Drugs and Technologies in Health. Canadian druy expert committee recommendation for Ozempic. 2019. https://www.cadth.ca/sites/default/files/cdr/complete/SR0594%20Ozempic%20-%20CDEC%20Final%20Recommendation%20May%2017%2C%202019%20%28redacted%29_For%20posting.pdf. [Accessed on January 2021]
- 21.Goldenberg RM, Steen O. Semaglutide: review and place in therapy for adults with type 2 diabetes. Can J Diabetes 2019;43:136–145. [DOI] [PubMed] [Google Scholar]
- 22.Johansen P, Håkan-Bloch J, Liu AR, Bech PG, Persson S, Leiter LA. Cost effectiveness of once-weekly semaglutide versus once-weekly dulaglutide in the treatment of type 2 diabetes in Canada. Pharmacoecon Open 2019;3:537–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Viljoen A, Hoxer CS, Johansen P, Malkin S, Hunt B, Bain SC. Evaluation of the long-term cost-effectiveness of once-weekly semaglutide versus dulaglutide for treatment of type 2 diabetes mellitus in the UK. Diabetes Obes Metab 2019;21:611–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunt B, Malkin SJP, Moes RGJ, Huisman EL, Vandebrouck T, Wolffenbuttel BHR. Once-weekly semaglutide for patients with type 2 diabetes: a cost-effectiveness analysis in the Netherlands. BMJ Open Diabetes Res Care 2019;7:e000705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. 2019 update to: management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2020;63:221–228. [DOI] [PubMed] [Google Scholar]
- 26.Ericsson Å, Fridhammar A. Cost-effectiveness of once-weekly semaglutide versus dulaglutide and lixisenatide in patients with type 2 diabetes with inadequate glycemic control in Sweden. J Med Econ 2019;22:997–1005. [DOI] [PubMed] [Google Scholar]
- 27.Johansen P, Chubb B, Hunt B, Malkin SJP, Sandberg A, Capehorn M. Evaluating the long-term cost-effectiveness of once-weekly semaglutide versus once-daily liraglutide for the treatment of type 2 diabetes in the UK. Adv Ther 2020;37:2427–2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gæde P, Johansen P, Tikkanen CK, Pollock RF, Hunt B, Malkin SJP. Management of patients with type 2 diabetes with once-weekly semaglutide versus dulaglutide, exenatide er, liraglutide and lixisenatide: a cost-effectiveness analysis in the danish setting. Diabetes Ther 2019;10:1297–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown RE, Bech PG, Aronson R. Semaglutide once weekly in people with type 2 diabetes: real-world analysis of the Canadian LMC diabetes registry (SPARE study). Diabetes Obes Metab 2020;22:2013–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yale JF, Catarig AM, Grau K, Harris S, Klimek-Abercrombie A, Rabasa-Lhoret R, et al. Use of once-weekly semaglutide in patients with type 2 diabetes in routine clinical practice: results from the SURE Canada multicentre, prospective, observational study. Diabetes Obes Metab 2021;23:2269–2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.