Abstract
Since ancient times, people have tattooed their skin for various reasons. In the past, tattoos were associated with low social status; nowadays, tattoos are very popular and are considered a form of art. However, tattoos are associated with various clinical problems, including immune reactions, inflammatory disorders, infections, and even skin cancer. Epidemiological and clinical data of infections on tattoos are scarce. Tattoo-related infections are mostly bacterial; only a few localized viral infections have been reported so far and are caused by molluscum contagiosum virus (MCV), human papillomavirus (HPV), and herpes simplex virus (HSV). In most cases, the lesions were strictly confined to the area of the tattoo. In this review, we have analysed reported cases of viral infections localized on tattoos and discussed the possible mechanisms involved in the occurrence of these infections.
Keywords: tattoo, viral infections, molluscum contagiosum, warts, herpes simplex
1. Introduction
Tattoos represent the introduction of exogenous pigments into the skin to obtain a permanent design [1]. In the last two decades, the prevalence of tattoos has increased significantly [2], ranging from 5 to 40% in adults [3]. Many individuals will have their first tattoo at the age of 16–20 years [4]. Throughout history, tattoos have been performed for various purposes, representing simple decorative elements, a marker of social rank, or the sign of belonging to a certain group [5]. Varying by circumstances, tattoos acquired positive valuations (heralds of distinction and spiritual devotion) and negative overtones (symbols of shame) [6]. Individuals with tattoos may experience stigma, stereotyping, and discrimination [7]. While the temptation of valuing the act of tattooing has been displayed since archaic epochs (Herodotus documents Thracians and Scythians distinguishing tattoos as emblems of nobility, while Greeks and Romans are reported to equate them with stigmata, slavery, and punitive measures) [8], the scientific evidence supporting tattoo correlation with deviant behaviour is demure [9,10].
Tattoos are classified as traumatic, cosmetic, or decorative and can be performed in professional settings or by amateurs [3]. Tattoos can be black or polychrome, but the black colour is predominant; in over 60% of cases, this type of ink is used. They are found in almost all areas of the human body [11]. Histological examination of the tattooed skin revealed the presence of pigment particles in the cytoplasm of various cells, such as fibroblasts and macrophages [11]. Recently, a pigment capture–release–recapture model was described in mice [12]. Macrophages loaded with pigment die after a variable period, the pigment is released, and neighbouring macrophages take it up; in this way, the long-term persistence of tattoos is possible [12,13]. Tattooing represents an important aggression of the skin that leads to the disruption of the epidermal basement membrane and even cell necrosis [1]. Between 1–5% of those who get a tattoo experience tattoo-related skin infections [4]. Infections after tattooing can be caused by endogenous microorganisms, i.e., microorganisms that are part of the normal flora, as a result of altered skin barrier or exogenous microorganisms that enter the skin by inoculation during tattooing [14]. Epidemiological and clinical data regarding infections on tattoos are scarce. The aim of our review is to bring together data on viral infections located on tattoos and to discuss the possible mechanisms involved in the occurrence of these infections.
2. Brief History of Tattoos
Throughout centuries, tattooing has served a deluge of socio-cultural functions, eliciting the perusal of anthropologists, historians, philosophers, sociologists, art critiques, or behavioural economists. Early tattoos employed homemade tools, as indicated in a detailed record of Egyptian practices of the 19th century [15]. In terms of colouring schemes, antique practice examination recounts the prevalence of dark pigments. Nonetheless, brighter colours have also been heavily used, as artefacts of ancient Egyptians and Romans demonstrate a fascination for colours, with red, blue, green, and yellow as prevalent chromatic options [16].
While tattooing is an ancient art, academic consensus over the world’s oldest tattoos was only reached in late 2015. Following archaeologists’ perusal through extensive radiocarbon dating, in which an unidentified mummy specimen belonging to the Chinchorro preceramic culture has been compared with Ötzi (a Tyrolean Iceman), the latter obtained the title of the world’s oldest tattoo remains. Discovered in 1991 at the Austrian–Italian border, the specimen had been preserved in ice for more than 5000 years, thus allowing for comprehensive scrutiny of 61 tattoo marks across his body. The body parts (wrist, legs, lower back, torso), alongside the tattoos pattern distribution, hinted at social, symbolic, and therapeutic functions [17].
In Ancient Egypt, it was a tradition employed by women, assumed to have consider it to have protective powers, as a remedy during pregnancy. Historical and ethnographic texts register women tattooing as an aid during the reproductive process, as fertility amulet, or for protection in pregnancy and birth phases [18].
Polynesian cultures alone provide a full-bodied universe for examination, with heavily infused cultural expressions and meticulous geometries. Tattoos compensated for the absence of a form of written culture, thus acting as ways of signaling ancestry, identity narratives, abilities, awards, social status, personal accomplishments, and collective experiences [19]. Thereupon, the etymology of the modern term “tattoo” stems from this cultural space, where tatatau or tattau means to hit or to strike [16].
The configuration of modern Western tattoos was shaped by colonialism, seafaring, electric tattoo machine technology, health regulations, and the consumer marketplace [20]. Academic papers and public discourse alike mention Captain James Cook as the bearer who introduced cross-cultural tattooing practices into the continent, following his 1770s Tahiti, New Zealand and the Pacific region explorations. Nonetheless, recent scrutiny of primary sources indicates the dissemination value of these voyages, rather than the acquisition of novel cultural contacts, in an attempt to demystify the absence of recorded European tattoo practices before the adventures of Captain Cook [21].
The 18th and 19th century in Europe and the U.S.A. present tattoos as constitutive characteristics of marginalized communities (financially destitute or socially corrupted groups). The late 19th century captivated cultural elites into pursuing tattoos as an endeavour to signal exoticism or distinction, a short-lived frivolity [22] that ended with the democratization of the practice in 1891. Both a Navy member and a convict, Irish American Samuel O’Reilly acquired the patent number 464,801 for the first tattooing machine [23].
These were centuries dominated by the use of contaminated ink and needles; a 19th century medical report on a syphilis outbreak in the outskirts of a naval barrack reveals the use of saliva during the process [24]. A tattoo artist of the 1950s explains this misunderstanding by referencing an article in the Journal of the American Medical Association; imported folklore misinterpreted tattooing risk factors with a syphilis cure, augmenting the confusion between the adverse and therapeutic effects of mercury-based pigments [25].
The middle of the 20th century is acknowledged as a period of tattoo renaissance, with the 1960’s counterculture relocating conventions through shifts in civil rights, public rhetoric, visual culture, corporality, subcultures, peripheral group perception, and the representation of alterity [26].
Aided by the systemic shift from trade to art [9], tattoos of the 21st century are crafted in schools for tattoo artists and deliberated within aesthetic, art history, and cultural theories. The commodification of the praxis has been, in the realm of popular culture, heavily augmented by the mainstream discourse and digital content [20].
3. Materials and Methods
We performed a narrative review by interrogating the PubMed and Google Scholar databases with the following combinations of terms, “tattoo and infection”, “tattoo and molluscum contagiosum”, “tattoo and warts”, “tattoo and verruca”, and “tattoo and herpes simplex”. We have selected the articles presenting cases of viral infections confined to tattoos. We have excluded the cases reporting systemic infections after tattooing. After applying these criteria, we have identified 14 case reports of molluscum contagiosum virus (MCV) infection; 18 case reports, 2 reports of two cases, and 2 case series of warts; and 4 case reports of herpes simplex virus (HSV) infection.
4. Viral Infections Localized on Tattoos
The proliferation of tattoo artists, studios, and parlours, the emergence of technological innovations such as ink variety, the rise in media reports fed insignificant complementary changes in regulations for sterilization process, and hygiene standard practices [27]. Whereas tattoo shops have formalized safety and sanitation measures, appropriate institutional control on the practice is lax, since tattooing is considered a beautification activity, except for two requisite resolutions (ResAp in 2003 and revised ResAp in 2008) from the Council of Europe [28]. When measured against other cultural production modes, tattooing is one of the most extensively regulated processes [29].
Amid deliberation on the formal placement and regulation of the praxis, medical research continues to gather a body of data that can offer further insight into compliant technologies, potential risks, and adverse reactions. The past decade generated abundant clinical reports of tattoo complications, investigating reactions based on the quality of the pigments, the techniques, after-care exposure, body parts, and even on ink colours [28].
The main complications after tattoo placement include immunologic reactions (allergic dermatitis, immunohypersensitivity, etc.), inflammatory skin disorders (psoriasis, lichen planus, pseudolymphoma, etc.), infections (viral, bacterial and fungal), and neoplasms (lymphoma, melanoma, basal cell carcinoma, etc.) [1,30,31]. Infections may be localized or systemic; most are bacterial. Serious viral infections include hepatitis B and C and human immunodeficiency virus (HIV) infection. Localized skin infections are rare and are caused by MCV, human papillomavirus (HPV), and HSV [32,33,34].
4.1. Molluscum Contagiosum
Molluscum contagiosum (MC) is a self-limited cutaneous viral infection that affects mainly children, sexually active adults, and immunosuppressed individuals [35,36]. MC is caused by MCV, a double-stranded DNA virus that belongs to the Poxviridae family. MCV has four different genotypes, with MCV-1 being the most common genotype (75 to 96% of cases) [37]. MCV infects the epidermis and replicates in the cytoplasm of cells, but does not exceed the basement membrane [35,38]. The incubation period varies between 2 weeks and 6 months [39]. The replication of the virus in keratinocytes promotes the formation of characteristic eosinophilic cytoplasmic inclusions (Henderson–Paterson bodies) [37]. Clinically, MC is characterized by firm, pearly white or pink, dome-shaped, centrally umbilicated papules that range in size from 1 to 5 mm in diameter. In most cases the lesions are asymptomatic; pruritus is uncommon. The lesions may appear grouped or may adopt a linear arrangement in the case of autoinoculation [36]. MCV infects almost exclusively the skin and rarely the mucous membranes [38].
Table 1 summarizes the cases of MC on tattoos reported in the medical literature. The cases have been reported mainly in young males. In no cases, immunosuppression was specified. The ages of the patients ranged from 16 to 64 years.
Table 1.
Epidemiological and clinical characteristics of the reported cases of molluscum contagiosum on tattoos.
| Sex | Age (Years) | Tattoo Localisation | Ink Colour | Latency Period |
Reference |
|---|---|---|---|---|---|
| male | 20 | left arm | polychrome- carbon pigment * |
3 months | Foulds (1982) [40] |
| female | 20 | left forearm | black | 3 weeks | Salmaso et al. (2001) [41] |
| male | 20 | left calf | polychrome-brownish-grey ink * | 5 months | Perez Gala et al. (2006) [42] |
| male | 59 | chest | monochromatic | 3 months | Kluger et al. (2007) [43] |
| male | 24 | right lumbar region | black | 2 weeks | Panasiti et al. (2008) [44] |
| male | 36 | right arm | black | 3 weeks | Perez-Barrio et al. (2009) [45] |
| male | 30 | arm | black | 20 days | De Giorgi et al. (2010) [46] |
| male | 22 | back | black | 4 weeks | Molina et al. (2011) [47] |
| male | 33 | right upper arm | polychrome | 5 months | Grillo et al. (2012) [48] |
| male | 32 | left abdominal flank | black | 3 weeks | Tampa et al. (2012) [49] |
| male | 23 | right abdominal flank | black | N/A | Ruiz-Villaverde et al. (2013) [50] |
| male | 33 | right arm | black | 3 months | Blasco Morente et al. (2016) [51] |
| female | 16 | posterior thorax | blue | N/A | Cortes et al. (2017) [52] |
| female | 64 | right eyebrow | dark | 1 month | Marcelino et al. (2021) [53] |
* Colour of the ink on which the lesions appeared. N/A—not available.
In 1982, Foulds reported the first case of MC on a tattoo performed using carbon, scarlet lake, and chlorinated copper pigments. The authors described the case of a 20-year-old man who presented with seven lesions of MC confined to the area of the tattoo performed with carbon pigment. The lesions healed spontaneously after 6 months [40]. However, it seems that the first case was described by Bergh in 1903 [54].
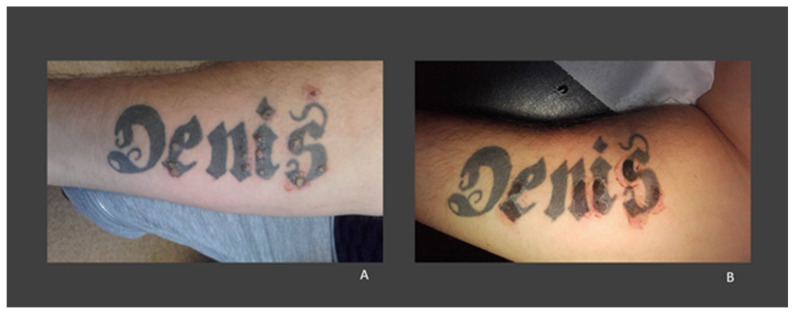
Most cases reported in the literature show that MC lesions are confined to the tattooed skin, with no involvement of the surrounding skin (Figure 1). Ruiz-Villaverde et al. have reported the case of a 23-year-old immunocompetent male, who presented with MC lesions both on his black tattoo and on the adjacent skin [50]. Furthermore, the analysis of the reported cases showed that black ink was used in most cases. The latency period between tattooing and the appearance of MC lesions ranged from 2 weeks to 5 months.
Figure 1.
(A) A 32-year-old man with molluscum contagiosum on a black tattoo located on his left abdominal flank; (B) molluscum contagiosum papules strictly confined to the tattooed skin (images from our clinic, previously published in Tampa et al., 2012 [49]).
4.2. Warts
HPV is a DNA virus with tropism for the skin and mucous membranes that can be classified into five genera (Alpha, Beta, Gamma, Mu, and Nu). Depending on the oncogenic risk, HPV types are divided into high-risk types associated with malignant lesions and low-risk types that cause benign lesions, in most cases asymptomatic, with limited evolution. Usually, the host’s immune response induces the viral clearance [55,56,57,58]. Warts are the most common skin manifestations of HPV infection. According to their morphology and anatomical site, several subtypes of warts (common, plantar, and flat warts) have been described. Common warts, also known as verruca vulgaris, are the most frequently seen and classically appear as hyperkeratotic papules [59]. Flat warts (verruca plana) are less common and manifest as flat-topped papules. Generally, the incubation period of warts varies between 1 and 6 months [60].
We have analyzed 22 case reports of warts on tattoos (Table 2). It seems that Fox was the first to describe warts on a tattoo in 1864; however, at that time their viral etiology was unknown [61].
Table 2.
Epidemiological and clinical characteristics of the reported cases of warts on tattoos.
| Sex | Age (Years) | Tattoo Localisation | Ink Colour | Latency Period | Reference |
|---|---|---|---|---|---|
| male | 21 | left arm | black | soon after tattooing | Watkins (1961) [62] |
| male | 24 | left scapula | black | 2 years | Young et al. (1979) [63] |
| male | 21 | N/A | black | 6 months | Baxter et al. (1993) [64] |
| male | 27 | right scapular area | dark blue | 8 years | Ragland et al. (1994) [65] |
| male | 33 | right upper arm | black | 8 years | Miller et al. (1994) [66] |
| male | 29 | left arm | polychrome-dark blue * | 8 years | Trefzer et al. (2004) [67] |
| male | 32 | back (left scapular area) after sunburn |
dark blue | 2.5 years | Brajac et al. (2005) [68] |
| female | 17 | left leg | dark blue and red-dark blue * | 3 months | Saez et al. (2006) [69] |
| female | 39 | face | dark | 1 year | Jung et al. (2009) [70] |
| female | 31 | right ankle | polychrome | 2 years | Wanat et al. (2014) [71] |
| male | 25 | the back of the left hand | polychrome | N/A | Navarro-Vidal et al. (2015) [72] |
| male | 24 | right arm | polychrome-dark, red * | 4.5 years | Fania et al. (2017) [73] |
| male | 35 | left arm | polychrome-dark * | 3.6 years | Fania et al. (2017) [73] |
| male | 47 | forearm | black | 12 years | Krecke et al. (2017) [74] |
| female | 66 | both eyebrows | dark grey/black | 8 years | Nemer et al. (2018) [75] |
| male | 30 | left forearm | black | 3 months | Georgescu et al. (2017) [76] |
| male | 36 | right forearm | black | more than 20 years | Kirchhof et al. (2019) [77] |
| male | 25 | right upper arm | dark blue | 3 months | Yuan (2019) [78] |
| female | 27 | left leg | black | 2 years | Chen et al. (2020) [79] |
| male | 39 | left calf | polychrome | 1 year | Veasey et al. (2020) [80] |
| male | 33 | left upper limb | polychrome | 6 years | Veasey et al. (2020) [80] |
| female | 44 | left lower leg | polychrome-black *, red | 26 years | Cohen(2021) [81] |
* Colour of the ink on which the lesions appeared. N/A—not available.
The age of the patients ranged from 17 to 66 years, but most cases were reported among young men. The period from when the tattoo was obtained and the appearance of warts varied between 2 months and over 20 years. In most cases, the warts were restricted to the tattooed skin and were preferentially located on black tattoos (Figure 2). Veasey et al. reported two cases: in one case, the patient was immunocompetent; in the second, the patient was infected with HIV (the only case identified in an immunocompromised patient). In the first case, the warts were located only on the tattooed skin, in contrast to the second case, in which they were also observed on healthy skin [80]. However, in the case of an immunocompetent woman, reported by Jung et al., warts initially appeared on the tattooed skin (eyebrow), but later spread to her face [70]. In all other cases, the warts were located exclusively on the tattooed area. In most cases, HPV testing was not performed; the diagnosis was made from the clinical and histopathological aspects. When HPV testing was performed, HPV 27 [71], HPV 47 [74], and HPV6B [66] types were identified.
Figure 2.
(A) A 30-year-old man with warts on a tattoo with black pigment on his left forearm. (B) The aspect of the tattoo after curettage and electrosurgery of the lesions (images from our clinic, previously published in Georgescu et al., 2017 [76]).
Kluger et al. analysed eight cases of warts on tattoos (not included in Table 2). In seven of the eight cases, warts developed on black tattoos. The latency period varied between 6 and 18 months. One patient stated that the warts were present prior to the tattoo placement [82]. In line with this, Ramey et al. analysed 5 cases of warts on tattoos (not included in Table 2) and identified 181 lesions that were located mainly on the areas with black ink [83]. Warts were seven times more likely to be localized on the skin where the black ink was used compared to coloured ink and normal skin [83].
4.3. Herpes Simplex
HSV-1 and HSV-2 are DNA viruses, members of the Herpesviridae family, with a short reproductive cycle, but with the ability to establish latency in the sensory ganglia and may recur in response to various stimuli to produce disease. Classically, HSV-1 causes orofacial lesions and HSV-2 genital lesions [84]. However, today it is known that there is significant overlap between the sites of HSV infection [85]. HSV-1 infections are more common; over 60% of individuals have antibodies against HSV-1, but only 10% of individuals against HSV-2 [86]. In many cases, the infection is asymptomatic and manifests, depending on the affected area, as oral ulcerations, vesicles, or genital lesions [87].
Marshall et al. reported the first case of herpes simplex that appeared as a complication of a tattoo in a 30-year-old man. Bacteriological examination revealed a co-infection with methicillin-susceptible Staphylococcus aureus. The patient had no history of herpes simplex and was treated with intravenous flucloxacillin and oral famciclovir, and the outcome was favourable. Marshall et al. proposed the term herpes compuctorum to describe cutaneous HSV infection that complicates tattoos [88]. In the medical literature, four cases of herpes simplex were reported on tattoos, with three identified in females (Table 3). The age of the patients ranged from 30 to 48 years. Two of the patients had a positive history of HSV infection. Unlike MC and warts, the latency period was very short as 2–3 days.
Table 3.
Epidemiological and clinical characteristics of the reported cases of herpes simplex on tattoos.
| Sex | Age (Years) | Tattoo Localisation | Ink Colour | Latency Period | Reference |
|---|---|---|---|---|---|
| male | 30 | left arm | black | 3 days | Marshall et al. (2007) [88] |
| female | 31 | right flank | black | 3 days | Kluger et al. (2017) [89] |
| female | 48 | lips | red | 2 days | AlQuorain et al. (2017) [90] |
| female | 46 | lips | red | 2 days | Begolli Gerqari et al. (2018) [91] |
5. Summary of the Characteristics of Viral Infections Confined to Tattoos
In terms of age, the highest mean age was observed among patients with HSV infection. In patients with MC and warts, the values were similar. The small number of patients with HSV infection should be considered. In the group of patients with HSV infection, the number of women was higher, unlike the other two groups in which men were predominant. With regard to the latency period, the differences between groups were significant, ranging from years to days (Table 4). In all cases, the lesions predominantly involved the dark area of the tattoo.
Table 4.
Demographic characteristics of the reported cases.
| Parameter | Molluscum Contagiosum | Warts | Herpes Simplex |
|---|---|---|---|
| Age (mean ± SD) | 30.85 ± 14.38 years | 32.04 ± 10.7 years | 38.75 ± 9.56 years |
| Male:Female ratio | 3.6:1 | 2.6:1 | 0.3:1 |
| Latency period (mean ± SD) |
2.04 ± 1.69 months | 5.93 ± 6.77 years | 2.5 ± 0.56 days |
6. Potential Mechanisms Involved in the Occurrence of Viral Infections on Tattoos
Over time, several theories have been postulated about the mechanisms of viral infections located on tattoos. The microorganisms can be inoculated through contaminated instruments, ink, or artist saliva, or in some cases, the tattoo is placed on already infected skin [79,83,92]. The procedure itself can lead to the activation of the virus in the case of previously infected people [91]. In addition, overinfection of a freshly healing wound may be possible [89].
Ramey et al. suggested that the use of contaminated ink is unlikely to be the source of infection for warts given that HPV is a fastidious virus and has a low chance of surviving in ink [83]. Moreover, Krecke et al. identified HPV-47 in tattoo-associated flat warts. HPV-47 is a member of the Beta genus, whose reservoir is the hair follicle. It should be noted that the act of tattooing could promote the release of the virus [74]. Additionally, Cortes et al. highlighted that MCV cannot survive in the dermis and therefore direct inoculation is less likely [52].
Immunity plays an important role in the development and evolution of infections. Human leukocyte antigens (HLAs), which represent genetic markers with important functions in the immune response to microorganisms, vary considerably among individuals. For example, a recent study showed that the HLA-A * 02, HLA-DQA1 * 03:01, and DQA1 * 05:01 genes are more prevalent in patients with warts than in healthy subjects [93]. Another theory that tries to explain the mechanism of the occurrence of viral infections on tattoos is the theory of the immunocompromised district, which refers to a local alteration of the skin’s immune system [94]. Ruocco et al. stated that skin areas that have suffered burns, irradiation, or trauma should be considered ‘loci minoris resistentiae’, i.e., areas likely to develop subsequent skin diseases [94]. This theory is supported by the appearance of several infectious dermatological diseases [95] and non-infectious dermatological diseases (pemphigus [96], basal cell carcinoma [97], fixed post drug rash [98]) on damaged skin. The tattoo pigment reaches the dermis, where it can stimulate an abnormal immune response that contributes to local immunosuppression. In addition, the decomposed pigment in the lymph nodes may be responsible for the immunosuppressed areas located proximal to the tattoo [52]. The long periods between the time of tattoo placement and the development of the infection suggest that microorganisms contracted incidentally, replicated preferentially within the immunocompromised area where the local immune response was altered by ink [99].
The localization of the viral infections predominantly within black tattoo areas can be explained by the fact that the black ink causes the alteration of local humoral and cellular immunity [43]. Since 1994, it has been suggested that black dye induces a local immunosuppressive effect [66]. Black inks are produced by imperfect combustion and contain high amounts of polycyclic aromatic hydrocarbons (PAHs) [100,101]. After exposure to ultraviolet (UV) light, PAHs lead to the generation of reactive oxygen species (ROS) that exert harmful effects on cells, causing the peroxidation of membrane lipids and proteins and consequent deterioration of the skin barrier [102,103,104,105]. In addition, black ink contains nanoparticles, unlike coloured ink, which contains larger particles, and the nanoparticles stimulate the production of ROS to a greater extent [103,106]. It should be noted that PAHs do not remain localized only in the dermis. PAHs are also transported to other organs [107].
Ultraviolets are involved in the pathogenesis of many skin diseases [108,109]. UV radiation may have a role in the activation of HPV. UVB radiation promotes HPV activity in keratinocytes, which could also explain the variation in the latency period [110]. Brajac et al. reported the case of a 32-year-old man who developed multiple warts on a tattoo performed 2.5 years previously. The warts appeared two weeks after an acute sunburn involving tattooed and normal skin, but the warts were confined to the tattooed area, suggesting that the virus was probably inoculated at the time of tattooing and remained latent, and the UV light acted as a trigger inducing its activation [68]. Rho et al. highlighted the onset of flat warts on the Q-switched laser-assisted tattoo removal site in a 23-year-old patient, 3 weeks after the procedure [111]. The authors suggested that HPV was probably latent within tattooed skin, and that the treatment caused the alteration of the epidermal barrier that allowed the virus to spread. This observation is based on the report of Amella et al. who, using an animal model, showed that HPV activation could occur after mild skin irritation [112].
7. Conclusions
Viral infections localized to tattoos have been reported mainly in young, immunocompetent adults, predominantly males. The lesions were confined to the tattooed area, rarely affecting the surrounding skin. Moreover, the lesions involved preferentially black tattoos. The mechanism of infection remains unclear. The increased latency periods between tattoo placement and lesion appearance support the hypothesis of altered local immunity; however, the use of contaminated ink or instruments cannot be ruled out. Tattoos are becoming more common in modern society and it is important to know all the possible complications, even the rarest.
Author Contributions
All authors have equally contributed to the writing and editing of the manuscript. Conceptualization, M.T., A.A.B. and C.M.; writing—original draft preparation, M.I.M., C.I.M., A.A. and A.A.B.; writing—review and editing, M.T. and S.R.G.; supervision, S.R.G.; funding acquisition, C.M. All authors have read and agreed to the published version of the manuscript.
Funding
The article processing charges are funded by Carol Davila University of Medicine and Pharmacy within the project Publish not perish.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Islam P.S., Chang C., Selmi C., Generali E., Huntley A., Teuber S.S., Gershwin M.E. Medical Complications of Tattoos: A Comprehensive Review. Clin. Rev. Allerg. Immunol. 2016;50:273–286. doi: 10.1007/s12016-016-8532-0. [DOI] [PubMed] [Google Scholar]
- 2.Luebberding S., Alexiades-Armenakas M. New Tattoo Approaches in Dermatology. Dermatol. Clin. 2014;32:91–96. doi: 10.1016/j.det.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Gualdi G., Fabiano A., Moro R., Venturuzzo A., Monari P., Calzavara-Pinton P., Amerio P. Tattoo: Ancient Art and Current Problems. J. Cosmet. Dermatol. 2021;20:602–604. doi: 10.1111/jocd.13548. [DOI] [PubMed] [Google Scholar]
- 4.Laux P., Tralau T., Tentschert J., Blume A., Dahouk S.A., Bäumler W., Bernstein E., Bocca B., Alimonti A. A Medical-Toxicological View of Tattooing. Lancet. 2016;387:395–402. doi: 10.1016/S0140-6736(15)60215-X. [DOI] [PubMed] [Google Scholar]
- 5.Byard R.W. Tattoos: Forensic Considerations. Forensic Sci. Med. Pathol. 2013;9:534–542. doi: 10.1007/s12024-013-9476-9. [DOI] [PubMed] [Google Scholar]
- 6.Atkinson M. Tattooed: The Sociogenesis of a Body Art. University of Toronto Press; Toronto, ON, Canada: 2003. [Google Scholar]
- 7.Farley C.L., Van Hoover C., Rademeyer C. Women and Tattoos: Fashion, Meaning, and Implications for Health. J. Midwifery Women’s Health. 2019;64:154–169. doi: 10.1111/jmwh.12932. [DOI] [PubMed] [Google Scholar]
- 8.Lineberry C. Tattoos: The Ancient and Mysterious History. 2007. [(accessed on 9 May 2021)]. Available online: https://www.smithsonianmag.com/history/tattoos-144038580/
- 9.Sanders C., Vail D.A. Customizing the Body: The Art and Culture of Tattooing. Temple University Press; Philadelphia, PA, USA: 2009. [Google Scholar]
- 10.Kosut M. Tattoos and Body Modification. In: James D., editor. Wright (Editor-in-Chief), International Encyclopedia of the Social & Behavioral Sciences. 2nd ed. Volume 24. Elsevier; Oxford, UK: 2015. pp. 34–35. [Google Scholar]
- 11.Weiß K.T., Schreiver I., Siewert K., Luch A., Haslböck B., Berneburg M., Bäumler W. Tattoos—More than Just Colored Skin? Searching for Tattoo Allergens. JDDG J. Dtsch. Dermatol. Ges. 2021;19:657–669. doi: 10.1111/ddg.14436. [DOI] [PubMed] [Google Scholar]
- 12.Baranska A., Shawket A., Jouve M., Baratin M., Malosse C., Voluzan O., Vu Manh T.-P., Fiore F., Bajénoff M., Benaroch P. Unveiling Skin Macrophage Dynamics Explains Both Tattoo Persistence and Strenuous Removal. J. Exp. Med. 2018;215:1115–1133. doi: 10.1084/jem.20171608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bäumler W. Chemical Hazard of Tattoo Colorants. La Presse Médicale. 2020;49:104046. doi: 10.1016/j.lpm.2020.104046. [DOI] [PubMed] [Google Scholar]
- 14.Patel M., Cobbs C.G. Infections from Body Piercing and Tattoos. Infect. Leis. 2016:307–323. doi: 10.1128/microbiolspec.IOL5-0016-2015. [DOI] [PubMed] [Google Scholar]
- 15.Lane E.W. An Account of the Manners and Customs of the Modern Egyptians. American University in Cairo Press; Cairo, Egypt: 2014. [Google Scholar]
- 16.DeMello M. Encyclopedia of Body Adornment. Greenwood Press; Westport, CT, USA: 2007. [Google Scholar]
- 17.Deter-Wolf A., Robitaille B., Krutak L., Galliot S. The World’s Oldest Tattoos. J. Archaeol. Sci. Rep. 2016;5:19–24. doi: 10.1016/j.jasrep.2015.11.007. [DOI] [Google Scholar]
- 18.Paszik J. Master’s Thesis. University College London; London, UK: 2017. AE Ink: Investigating the Mechanics and Meanings of Ancient Egyptian Tattoos. [DOI] [Google Scholar]
- 19.Gell A. Wrapping in Images: Tattooing in Polynesia. Oxford University Press; New York, NY, USA: 1993. [Google Scholar]
- 20.DeMello M., Rubin G.S. Bodies of Inscription. Duke University Press; Durham, NC, USA: 2000. [Google Scholar]
- 21.Lodder M. Too Many Cooks. The origins of Western Tattooing: Exploding a Popular Myth. Total Tattoo Magazine. Sep 23, 2015. pp. 70–71.
- 22.Kosut M. The Artification of Tattoo: Transformations within a Cultural Field. Cult. Sociol. 2013;8:2–8. doi: 10.1177/1749975513494877. [DOI] [Google Scholar]
- 23.Unwin P. ‘An Extremely Useful Invention’: Edison’s Electric Pen and the Unravelling of Old and New Media. Convergence. 2019;25:607–626. doi: 10.1177/1354856519846790. [DOI] [Google Scholar]
- 24.Barker F. Notes of Cases on an Outbreak of Syphilis Following on Tattooing. Br. Med. J. 1889;1:985–989. doi: 10.1136/bmj.1.1479.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steward S.M. Bad Boys and Tough Tattoos: A Social History of the Tattoo with Gangs, Sailors, and Street-Corner Punks 1950–1965. Routledge; London, UK: 2013. [Google Scholar]
- 26.Rubin A. The Tattoo Renaissance. Museum of Cultural History; University of California; Los Angeles, CA, USA: 1988. [Google Scholar]
- 27.Ralf M. Manufacturing of Tattoo Ink Products Today and in Future: Europe. In: Serup J., Kluger N., Bäumler W., editors. Tattooed Skin and Health. Volume 48. Karger; Basel, Switzerland: 2015. pp. 197–199. [Google Scholar]
- 28.Bonadonna L. Survey of Studies on Microbial Contamination of Marketed Tattoo Inks. In: Serup J., Kluger N., Baumler W., editors. Current Problems in Dermatology. Volume 48. S. Karger AG; Basel, Switzerland: 2015. pp. 190–195. [DOI] [PubMed] [Google Scholar]
- 29.Hodder I. The Meanings of Things: Material Culture and Symbolic Expression. Routledge; London, UK: 2013. [Google Scholar]
- 30.Petrochko J.M., Krakowski A.C., Donnelly C., Wilson J.B., Irick J.B., Stawicki S.P. Tattoo-associated complications and related topics: A comprehensive review. Int. J. Acad. Med. 2019;5:19. [Google Scholar]
- 31.Juhas E., English J.C. Tattoo-Associated Complications. J. Pediatric Adolesc. Gynecol. 2013;26:125–129. doi: 10.1016/j.jpag.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Serup J., Hutton Carlsen K., Sepehri M. Tattoo Complaints and Complications: Diagnosis and Clinical Spectrum. In: Serup J., Kluger N., Baumler W., editors. Current Problems in Dermatology. Volume 48. S. Karger AG; Basel, Switzerland: 2015. pp. 48–60. [DOI] [PubMed] [Google Scholar]
- 33.Kluger N. An Update on Cutaneous Complications of Permanent Tattooing. Expert Rev. Clin. Immunol. 2019;15:1135–1143. doi: 10.1080/1744666X.2020.1676732. [DOI] [PubMed] [Google Scholar]
- 34.Cohen P.R. Tattoo-Associated Viral Infections: A Review. Clin. Cosmet. Investig. Dermatol. 2021;14:1529. doi: 10.2147/CCID.S284796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meza-Romero R., Navarrete-Dechent C., Downey C. Molluscum Contagiosum: An Update and Review of New Perspectives in Etiology, Diagnosis, and Treatment. CCID. 2019;12:373–381. doi: 10.2147/CCID.S187224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robinson G., Townsend S., Jahnke M.N. Molluscum Contagiosum: Review and Update on Clinical Presentation, Diagnosis, Risk, Prevention, and Treatment. Curr. Dermatol. Rep. 2020;9:83–92. doi: 10.1007/s13671-020-00289-z. [DOI] [Google Scholar]
- 37.Leung A.K.C., Barankin B., Hon K.L.E. Molluscum Contagiosum: An Update. IAD. 2017;11:22–31. doi: 10.2174/1872213X11666170518114456. [DOI] [PubMed] [Google Scholar]
- 38.Chen X., Anstey A.V., Bugert J.J. Molluscum Contagiosum Virus Infection. Lancet Infect. Dis. 2013;13:877–888. doi: 10.1016/S1473-3099(13)70109-9. [DOI] [PubMed] [Google Scholar]
- 39.Ruby K.N., Perry A.E., Linos K. Expanding the Morphologic Heterogeneity of Stromal Changes in Molluscum Contagiosum Infection. Am. J. Dermatopathol. 2018;40:941–943. doi: 10.1097/DAD.0000000000001015. [DOI] [PubMed] [Google Scholar]
- 40.Foulds I.S. Molluscum Contagiosum: An Unusual Complication of Tattooing. BMJ. 1982;285:607. doi: 10.1136/bmj.285.6342.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salmaso F., Gnecchi L., Gianotti R., Veraldi S. Molluscum Contagiosum on a Tattoo. Acta Derm.-Venereol. 2001;81:146–147. doi: 10.1080/00015550152384362. [DOI] [PubMed] [Google Scholar]
- 42.Perez Gala S., Alonso Perez A., Rios Buceta L., Aragues Montanes M., Garcia Diez A. Molluscum Contagiosum on a Multicoloured Tattoo. J. Eur. Acad. Dermatol. Venerol. 2006;20:221–222. doi: 10.1111/j.1468-3083.2005.01363.x. [DOI] [PubMed] [Google Scholar]
- 43.Kluger N., Comte C., Guillot B. Molluscum contagiosum sur tatouage. Ann. Dermatol. Vénéréol. 2007;134:506–507. doi: 10.1016/S0151-9638(07)89231-3. [DOI] [PubMed] [Google Scholar]
- 44.Panasiti V., Devirgiliis V., Roberti V., Curzio M., Calvieri S. Molluscum Contagiosum on a Tattoo: Usefulness of Dermoscopy. Int. J. Dermatol. 2008;47:1318–1319. doi: 10.1111/j.1365-4632.2008.03747.x. [DOI] [PubMed] [Google Scholar]
- 45.Pérez-Barrio S., González-Hermosa M.R., Ratón J.A., Díaz-Pérez J.L. Molusco contagioso sobre tatuaje. Actas Dermo-Sifiliográficas. 2009;100:152–154. doi: 10.1016/S0001-7310(09)70237-6. [DOI] [PubMed] [Google Scholar]
- 46.De Giorgi V., Grazzini M., Lotti T. A Three-Dimensional Tattoo: Molluscum Contagiosum. Can. Med. Assoc. J. 2010;182:E382. doi: 10.1503/cmaj.091480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Molina L., Romiti R. Molusco Contagioso Em Tatuagem. An. Bras. Dermatol. 2011;86:352–354. doi: 10.1590/S0365-05962011000200022. [DOI] [PubMed] [Google Scholar]
- 48.Grillo E., Urech M., Vano-Galvan S., Pedro J. Lesions on Tattooed Skin: A Case Study. Aust. Fam. Physician. 2012;41:308–309. [PubMed] [Google Scholar]
- 49.Tampa M., Sarbu I., Neamtu V., Anghel A., Mihele D., Benea V., Georgescu S. O complicatie rara a tatuarii: Infectia cutanata cu virusul molluscum contagiosum. Rev. Med. Mod. 2012;19:129–132. [Google Scholar]
- 50.Ruiz-Villaverde R., Sánchez-Cano D. Pearled Papules over Tattoo: Molluscum Cotagiosum. Pan Afr. Med. J. 2013;16 doi: 10.11604/pamj.2013.16.49.3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blasco-Morente G., Naranjo-Díaz M.J., Pérez-López I., Martínez-López A., Garrido-Colmenero C. Molluscum Contagiosum Over Tattooed Skin. SQUMJ. 2016;16:e257–e258. doi: 10.18295/squmj.2016.16.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cortés V.O., Alcudia A.A.G., Díaz N.P. Molusco contagioso sobre tatuaje: Reporte de caso. Dermatol. CMQ. 2018;16:28–31. [Google Scholar]
- 53.Marcelino F.F.N., de Oliveira-Filho J., Junqueira G.M.D., Nogueira M.F., Michalany A.O. Molusco Contagioso Como Complicação de Tatuagem: Um Relato de Caso e Revisão Da Literatura. Surg. Cosmet. Dermatol. 2021;13:e20210008. doi: 10.5935/scd1984-8773.2021130008. [DOI] [Google Scholar]
- 54.Bergh R. Über Eigentümliche Geschwulstbildung in Einer Tätowierungsmarke. Mschr. Dermat. 1903;37:49–52. [Google Scholar]
- 55.Tampa M., Mitran C.I., Mitran M.I., Nicolae I., Dumitru A., Matei C., Manolescu L., Popa G.L., Caruntu C., Georgescu S.R. The Role of Beta HPV Types and HPV-Associated Inflammatory Processes in Cutaneous Squamous Cell Carcinoma. J. Immunol. Res. 2020;2020:5701639. doi: 10.1155/2020/5701639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Egawa N., Doorbar J. The Low-Risk Papillomaviruses. Virus Res. 2017;231:119–127. doi: 10.1016/j.virusres.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 57.Okunade K.S. Human Papillomavirus and Cervical Cancer. J. Obstet. Gynaecol. 2020;40:602–608. doi: 10.1080/01443615.2019.1634030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Georgescu S.R., Mitran C.I., Mitran M.I., Caruntu C., Sarbu M.I., Matei C., Nicolae I., Tocut S.M., Popa M.I., Tampa M. New Insights in the Pathogenesis of HPV Infection and the Associated Carcinogenic Processes: The Role of Chronic Inflammation and Oxidative Stress. J. Immunol. Res. 2018;2018:5315816. doi: 10.1155/2018/5315816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lynch M.D., Cliffe J., Morris-Jones R. Management of Cutaneous Viral Warts. BMJ. 2014;348:g3339. doi: 10.1136/bmj.g3339. [DOI] [PubMed] [Google Scholar]
- 60.McLaughlin J.S., Shafritz A.B. Cutaneous Warts. J. Hand Surg. 2011;36:343–344. doi: 10.1016/j.jhsa.2010.11.036. [DOI] [PubMed] [Google Scholar]
- 61.Fox T. Warts Occurring on Tattooed Lines. J. Cutan. Vener. Dis. 1884;2:216. [Google Scholar]
- 62.Watkins D.B. Viral Disease in Tattoos: Verruca Vulgaris. Arch. Dermatol. 1961;84:306–309. doi: 10.1001/archderm.1961.01580140132017. [DOI] [PubMed] [Google Scholar]
- 63.Young D.F., Cole G.W. The Verrucous Mermaid. Int. J. Dermatol. 1979;18:816–817. doi: 10.1111/j.1365-4362.1979.tb04472.x. [DOI] [PubMed] [Google Scholar]
- 64.Baxter S., Deck D. Tattoo-Acquired Verruca Plana. Am. Fam. Physician. 1993;47:732. [PubMed] [Google Scholar]
- 65.Patrick Ragland H., Hubbell C., Stewart K.R., Nesbitt L.T. Verruca vulgaris inoculated during tattoo placement. Int. J. Dermatol. 1994;33:796–797. doi: 10.1111/j.1365-4362.1994.tb00998.x. [DOI] [PubMed] [Google Scholar]
- 66.Miller D.M., Brodell R.T. Verruca Restricted to the Areas of Black Dye within a Tattoo. Arch. Dermatol. 1994;130:1453–1454. doi: 10.1001/archderm.1994.01690110123029. [DOI] [PubMed] [Google Scholar]
- 67.Trefzer U., Schmollack K.-P., Stockfleth E., Sterry W., Kolde G. Verrucae in a Multicolored Decorative Tattoo. J. Am. Acad. Dermatol. 2004;50:478–479. doi: 10.1016/S0190-9622(03)02096-6. [DOI] [PubMed] [Google Scholar]
- 68.Brajac I., Loncarek K., Stojnic-Sosa L., Gruber F. Delayed Onset of Warts over Tattoo Mark Provoked by Sunburn. J. Eur. Acad. Dermatol. Venerol. 2005;19:247–248. doi: 10.1111/j.1468-3083.2004.01121.x. [DOI] [PubMed] [Google Scholar]
- 69.Saez M., Rodriguez-Martin M., Sidro-Sarto M., Cabrera de Paz R., Rodriguez-Garcia F., Fagundo-Gonzalez E., Carnerero A., Guimera F., Garcia-Bustinduy M., Sanchez R., et al. Multiple Verrucae Vulgaris in a Young Woman’s Tattoo. J. Eur. Acad. Dermatol. Venerol. 2006;20:356–357. doi: 10.1111/j.1468-3083.2006.01438.x. [DOI] [PubMed] [Google Scholar]
- 70.Jung J.Y., Shin H.S., Won C.H., Cho S. Facial Verruca Plana That Developed after Semipermanent Tattooing. Ann. Dermatol. 2009;21:92. doi: 10.5021/ad.2009.21.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wanat K.A., Tyring S., Rady P., Kovarik C.L. Human Papillomavirus Type 27 Associated with Multiple Verruca within a Tattoo: Report of a Case and Review of the Literature: HPV27 Associated with Multiple Verruca in a Tattoo. Int. J. Dermatol. 2014;53:882–884. doi: 10.1111/j.1365-4632.2012.05644.x. [DOI] [PubMed] [Google Scholar]
- 72.Navarro-Vidal B., González-Olivares M., Aguado-Lobo M., Borbujo Martinez J.M. Vulgaris Verruca on a Tattoo. Med. Clín. Engl. Ed. 2015;145:e35. doi: 10.1016/j.medcle.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 73.Fania L., Sordi D., Pagnanelli G., CavanI A., Mazzanti C. Tattoo and Warts: Efficacy of Topical Immunotherapy. Eur. J. Dermatol. 2017;27:322–323. doi: 10.1684/ejd.2017.2995. [DOI] [PubMed] [Google Scholar]
- 74.Krecké N., Smola S., Vogt T., Müller C.S.L. HPV-47-Induced and Tattoo-Associated Verrucae Planae: Report of a Case and Review of the Literature. Dermatol. Ther. 2017;7:549–554. doi: 10.1007/s13555-017-0197-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nemer K.M., Hurst E.A. Confluent Verruca Vulgaris Arising within Bilateral Eyebrow Tattoos: Successful Treatment with Ablative Laser and Topical 5% Imiquimod Cream. Dermatol. Surg. 2019;45:473–475. doi: 10.1097/DSS.0000000000001540. [DOI] [PubMed] [Google Scholar]
- 76.Georgescu S.R., Musa E., Limbau A., Benea V., Tampa M. A rare complication of tattooing: Verruca restricted to the black pigment in a tattoo; Proceedings of the 14th EADV Spring Symposium; Brussels, Belgium. 25–28 May 2017. [Google Scholar]
- 77.Kirchhof M.G., Wong S.M. Tattoos and Human Papilloma Virus: A Case Report of Tattoo-Associated Flat Warts (Verrucae Planae) SAGE Open Med. Case Rep. 2019;7:2050313X1985741. doi: 10.1177/2050313X19857416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yuan T. Multiple Verrucae Vulgaris in a Young Man’s Tattoo: A Case Report. Int. J. Dermatol. Venereol. 2019;2:120–121. doi: 10.1097/01.JD9.0000559514.78062.30. [DOI] [Google Scholar]
- 79.Chen Y.J., Nabi O., Diao P., Wan R.Y., Li L. Verruca Plana on a Tattoo: A Case Report. Medicine. 2020;99:e19744. doi: 10.1097/MD.0000000000019744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Veasey J.V., Erthal A.L.N., Lellis R.F. In Vivo and Ex Vivo Dermoscopy of Lesions from Implantation of Human Papillomavirus in Tattoos: Report of Two Cases. An. Bras. Dermatol. 2020;95:78–81. doi: 10.1016/j.abd.2019.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cohen P.R. Verruca Vulgaris Occurring on a Tattoo: Case Report and Review of Tattoo-Associated Human Papillomavirus Infections. Cureus. 2021;13:e17575. doi: 10.7759/cureus.17575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kluger N. Viral Warts and Seborrhoeic Keratoses on Tattoos: A Review of Nine Cases. J. Eur. Acad. Dermatol. Venereol. 2017;31:e340–e342. doi: 10.1111/jdv.14134. [DOI] [PubMed] [Google Scholar]
- 83.Ramey K., Ibrahim J., Brodell R.T. Verruca Localization Predominately in Black Tattoo Ink: A Retrospective Case Series. J. Eur. Acad. Dermatol. Venereol. 2016;30:e34–e36. doi: 10.1111/jdv.13283. [DOI] [PubMed] [Google Scholar]
- 84.Widener R.W., Whitley R.J. Handbook of Clinical Neurology. Volume 123. Elsevier; Amsterdam, The Netherlands: 2014. Herpes Simplex Virus; pp. 251–263. [DOI] [PubMed] [Google Scholar]
- 85.Whitley R., Baines J. Clinical Management of Herpes Simplex Virus Infections: Past, Present, and Future. F1000Research. 2018;7:1726. doi: 10.12688/f1000research.16157.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Singh N., Tscharke D.C. Herpes Simplex Virus Latency Is Noisier the Closer We Look. J. Virol. 2020;94:e01701-19. doi: 10.1128/JVI.01701-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nath P., Kabir M.A., Doust S.K., Ray A. Diagnosis of Herpes Simplex Virus: Laboratory and Point-of-Care Techniques. Infect. Dis. Rep. 2021;13:518–539. doi: 10.3390/idr13020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Marshall C.S., Murphy F., McCarthy S.E., Cheng A.C. Herpes Compunctorum: Cutaneous Herpes Simplex Virus Infection Complicating Tattooing. Med. J. Aust. 2007;187:598. doi: 10.5694/j.1326-5377.2007.tb01435.x. [DOI] [PubMed] [Google Scholar]
- 89.Kluger N., Armingaud P. Herpes Simplex Infection on a Recent Tattoo. A New Case of “Herpes Compuctorum”. Int. J. Dermatol. 2017;56:e9–e10. doi: 10.1111/ijd.13388. [DOI] [PubMed] [Google Scholar]
- 90.AlQuorain N.A., Yousef H.A., AlJabre S.H., AlAkloby O.M., Al-Natour S.H. Cosmetic Lip Tattoo Sequelae: A Case Report and Review of Literature. J. Dermatol. Dermatol. Surg. 2017;21:87–90. doi: 10.1016/j.jdds.2017.03.001. [DOI] [Google Scholar]
- 91.Begolli Gerqari A., Ferizi M., Kotori M., Halimi S., Daka A., Hapciu S., Begolli I., Begolli M., Gerqari I. Activation of Herpes Simplex Infection after Tattoo. Acta Dermatovenerol. Croat. 2018;26:75. [PubMed] [Google Scholar]
- 92.De Cuyper C., Maria Luisa Pérez-Cotapos S. Dermatologic Complications with Body Art. Springer; Berlin/Heidelberg, Germany: 2010. [Google Scholar]
- 93.Gülseren D., Tan Ç., Yaz İ., Özbek B., Çağdaş D., Tezcan İ. Expression of HLA Class I and Class II Genes in Patients with Multiple Skin Warts. Exp. Dermatol. 2021;30:1642–1649. doi: 10.1111/exd.14362. [DOI] [PubMed] [Google Scholar]
- 94.Ruocco V., Brunetti G., Puca R., Ruocco E. The Immunocompromised District: A Unifying Concept for Lymphoedematous, Herpes-Infected and Otherwise Damaged Sites. J. Eur. Acad. Dermatol. Venereol. 2009;23:1364–1373. doi: 10.1111/j.1468-3083.2009.03345.x. [DOI] [PubMed] [Google Scholar]
- 95.Karakass M., Durdu M., Özbilen A. Molluscum Contagiosum on Region of Burned Skin: Wolf” s Isotopic Response. J. Eur. Acad. Dermatol. Venereol. 2006;20:1014–1016. doi: 10.1111/j.1468-3083.2006.01608.x. [DOI] [PubMed] [Google Scholar]
- 96.Hasson A., Requena L., Arias D., Martin L., De Castro A. Linear Pemphigus Vulgaris along a Surgical Scar. Dermatology. 1991;182:191–192. doi: 10.1159/000247781. [DOI] [PubMed] [Google Scholar]
- 97.Hendricks W.M. Basal Cell Carcinoma Arising in a Chickenpox Scar. Arch. Dermatol. 1980;116:1304–1305. doi: 10.1001/archderm.1980.01640350094025. [DOI] [PubMed] [Google Scholar]
- 98.Mizukawa Y., Shiohara T. Trauma-Localized Fixed Drug Eruption: Involvement of Burn Scars, Insect Bites and Venipuncture Sites. Dermatology. 2002;205:159–161. doi: 10.1159/000063892. [DOI] [PubMed] [Google Scholar]
- 99.Huynh T.N., Jackson J.D., Brodell R.T. Tattoo and Vaccination Sites: Possible Nest for Opportunistic Infections, Tumors, and Dysimmune Reactions. Clin. Dermatol. 2014;32:678–684. doi: 10.1016/j.clindermatol.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 100.Lehner K., Santarelli F., Vasold R., König B., Landthaler M., Bäumler W. Black Tattoo Inks Are a Source of Problematic Substances Such as Dibutyl Phthalate. Contact Dermat. 2011;65:231–238. doi: 10.1111/j.1600-0536.2011.01947.x. [DOI] [PubMed] [Google Scholar]
- 101.Lehner K., Santarelli F., Vasold R., Penning R., Sidoroff A., König B., Landthaler M., Bäumler W. Black tattoos entail substantial uptake of genotoxicpolycyclic aromatic hydrocarbons (PAH) in human skin and regional lymph nodes. PLoS ONE. 2014;9:e92787. doi: 10.1371/journal.pone.0092787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Georgescu S.R., Ene C.D., Tampa M., Matei C., Benea V., Nicolae I. Oxidative Stress-Related Markers and Alopecia Areata through Latex Turbidimetric Immunoassay Method. Mater. Plast. 2016;53:522–526. [Google Scholar]
- 103.Jacobsen N.R., Clausen P.A. Carbon Black Nanoparticles and Other Problematic Constituents of Black Ink and Their Potential to Harm Tattooed Humans. Curr. Probl. Dermatol. 2015;48:170–175. doi: 10.1159/000369319. [DOI] [PubMed] [Google Scholar]
- 104.El-Beltagi H.S., Mohamed H.I. Reactive Oxygen Species, Lipid Peroxidation and Antioxidative Defense Mechanism. Not. Bot. Horti Agrobot. Cluj-Napoca. 2013;41:44–57. doi: 10.15835/nbha4118929. [DOI] [Google Scholar]
- 105.Mitran C.I., Nicolae I., Tampa M., Mitran M.I., Caruntu C., Sarbu M.I., Ene C.D., Matei C., Ionescu A.C., Georgescu S.R., et al. The Relationship between the Soluble Receptor for Advanced Glycation End Products and Oxidative Stress in Patients with Palmoplantar Warts. Medicina. 2019;55:706. doi: 10.3390/medicina55100706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Stone V., Johnston H., Clift M.J. Air Pollution, Ultrafine and Nanoparticle Toxicology: Cellular and Molecular Interactions. IEEE Trans. Nanobiosci. 2007;6:331–340. doi: 10.1109/TNB.2007.909005. [DOI] [PubMed] [Google Scholar]
- 107.Regensburger J., Lehner K., Maisch T., Vasold R., Santarelli F., Engel E., Gollmer A., König B., Landthaler M., Bäumler W. Tattoo Inks Contain Polycyclic Aromatic Hydrocarbons That Additionally Generate Deleterious Singlet Oxygen: PAHs in Tattoo Inks. Exp. Dermatol. 2009;19:e275–e281. doi: 10.1111/j.1600-0625.2010.01068.x. [DOI] [PubMed] [Google Scholar]
- 108.Christensen L., Suggs A., Baron E. Ultraviolet Photobiology in Dermatology. Adv. Exp. Med. Biol. 2017;996:89–104. doi: 10.1007/978-3-319-56017-5_8. [DOI] [PubMed] [Google Scholar]
- 109.Nicolae I., Ene C.D., Georgescu S.R., Tampa M., Matei C., Ceausu E. Effects of UV Radiation and Oxidative DNA Adduct 8-Hydroxy-2′-deoxiguanosine on the Skin Diseases. Rev. Chim. 2014;65:1036–1041. [Google Scholar]
- 110.Akgul B., Lemme W., Garcia-Escudero R., Storey A., Pfister H.J. UV-B Irradiation Stimulates the Promoter Activity of the High-Risk, Cutaneous Human Papillomavirus 5 and 8 in Primary Keratinocytes. Arch. Virol. 2005;150:145–151. doi: 10.1007/s00705-004-0398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rho N. Activation of Flat Warts (Verrucae Planae) on the Q-Switched Laser-Assisted Tattoo Removal Site. Med. Lasers. 2014;3:84–86. doi: 10.25289/ML.2014.3.2.84. [DOI] [Google Scholar]
- 112.Amella C.A., Lofgren L.A., Ronn A.M., Nouri M., Shikowitz M.J., Steinberg B.M. Latent Infection Induced with Cottontail Rabbit Papillomavirus. A Model for Human Papillomavirus Latency. Am. J. Pathol. 1994;144:1167–1171. [PMC free article] [PubMed] [Google Scholar]