Abstract
Background:
Children with cancer experience a wide range of conditions that require urgent evaluation in the emergency department (ED), yet variation in admission rates is poorly documented.
Procedure:
We performed a retrospective cohort study using the Pediatric Health Information System of ED encounters by children with cancer between July 2012 and June 2015. We compared demographics for admitted versus discharged using univariate statistics, and calculated admission rates by hospital, diagnosis, day of the week, and weekend versus weekday. We assessed the degree of interhospital admission rates using the index of dispersion (ID).
Results:
Children with cancer had 60 054 ED encounters at 37 hospitals. Overall, 62.5% were admitted (range 43.2%-92.1%, ID 2.6) indicating overdispersed admission rates with high variability. Children with cancer that visited the ED for a primary diagnosis of fever experienced the largest amount of variability in admission with rates ranging from 10.4% to 74.1% (ID 8.1). Less variability existed among hospital admission rates for both neutropenia (range 60%-100%, ID 1.0) and febrile neutropenia (FN) (range 66.7%-100%, ID 0.83). Admission rates by day of the week did not demonstrate significant variability for any of the scenarios examined (overall P = 0.91). There were no differences by weekend versus weekday either (overall P = 0.52).
Conclusion:
The percentage of children with cancer admitted through the ED varies widely by institution and diagnosis. Standardization of best practices for children with cancer admitted through the ED should be an area of continued improvement.
Keywords: outcomes research, pediatric oncology, support care
1 ∣. BACKGROUND
Children with cancer experience a wide range of symptoms and complications that require urgent evaluation.1,2 Although some pediatric oncology clinics have the capacity to evaluate patients during the weekdays, many children with cancer are evaluated and treated in the emergency department (ED) based on patient distance from clinic, clinic resources, and patient severity. The ED is also the primary avenue for evaluation and admission to the hospital during non-business hours and weekends. ED admission rates have been explored in other pediatric conditions including neonatal fevers and gastroenteritis with demonstration of significant interhospital variation in management and admission rates.3,4 Yet, variation has not been explored among children with cancer.
Variation for this population should be explored due to unique features related to ED utilization by children with cancer. Previous studies of ED utilization among children with cancer have revealed that this unique population comprises a small proportion of all visits to the ED,1,2 which may lead to less familiarity among ED providers. There are also differences in provider practices and inconsistent recommendations for those patients who live further away from their treating institution.5
There are no studies specifically describing the variation in admission rates from the ED for children with cancer. Therefore, the objective of this study was to determine interhospital variation in admission rates for children with cancer who present to the ED, stratified by presenting complaint and day of the week. Our hypothesis is that variation exists among hospitals and that the variation would be greatest during the weekdays when outpatient clinic resources are available.
2 ∣. METHODS
2.1 ∣. Study design and data source
We conducted a retrospective cohort study using the Pediatric Health Information System (PHIS), an administrative and resource utilization database from 49 children’s hospitals in noncompeting markets. All hospitals are affiliated with the Children’s Hospital Association (CHA, Shawnee Mission, KS) and are in 26 states plus the District of Columbia. They account for ~20% of all pediatric hospitalizations in the United States.6 Hospitals were included in this study if they provided consistent inpatient and ED data between July 1, 2012, and June 30, 2015, resulting in 37 hospitals included. The CHA (Overland Park, KS) and participating hospitals jointly monitor both the quality and integrity of data, described previously.7 The data warehouse function for the PHIS database is managed by Thomson Reuters (Ann Arbor, MI). Participating hospitals provide deidentified patient discharge/encounter data including demographics, billing data, diagnoses, and procedures. This analysis was based on deidentified data and was therefore considered exempt from institutional review board approval by the Indiana University School of Medicine. Identifying hospital numbers were anonymized for the study analysis.
2.2 ∣. Study population/identification of cases
ED encounters by children with cancer were identified by the inclusion of an International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) code for a malignancy (140.x-209.x, 235.x-239.x), as previously described.1,2 We chose not to use ICD-10 data, as there are inconsistencies across diagnoses. An ED encounter was defined as either an inpatient or observation encounter with an associated ED charge flag (i.e., admission) or an ED encounter with discharge to home (i.e., discharge). We also determined the following demographic variables for each subject: gender, race, ethnicity, insurance type, and age. Age in years was transformed into a categorical variable as follows: ages 0-4, 5-9, 10-14, and 15 and older. Encounters for patients older than age 25 were excluded. Type of insurance was categorized as public, private, and other. Race and ethnicity variables were combined as non-Hispanic white, non-Hispanic black, Hispanic, Asian, and other/unknown.
2.3 ∣. Exploratory variables
In order to explore variation among ED admissions, we chose to evaluate the admission rates in several different ways. Because fever, neutropenia, and febrile neutropenia (FN) are the most common reasons for ED visits among children with cancer,1,2 we made variables for each of these conditions. The primary diagnosis for the ED visit was defined as the first ICD-9-CM discharge diagnosis, unless the first diagnosis was a cancer diagnosis. In cases where a cancer diagnosis was the first diagnosis, the second listed ICD-9-CM diagnosis was considered to be the reason prompting the ED visit. Cancer diagnoses were not considered the reason prompting an ED visit because we intended to focus on symptoms or complications associated with ED visits made by children with cancer. A primary diagnosis of fever was defined as an ICD-9-CM discharge diagnosis of 780.6, 780.60, or 780.61. A primary diagnosis of neutropenia was defined as an ICD-9-CM discharge diagnosis of 288.0, 288.00, 288.03, 288.04, or 288.09. Given that the presence of FN has clinical importance but does not have a unique ICD-9-CM code, we combined codes for fever and neutropenia as previously published.2 Among patients with a primary diagnosis of fever, all associated diagnoses were evaluated for the presence of neutropenia and vice versa. Then, an encounter was labeled as FN if their primary diagnosis was fever with neutropenia in any of the diagnostic fields or primary diagnosis of neutropenia with fever in any of the diagnostic fields.
2.4 ∣. Statistical analyses
We compared subject demographics for those who were admitted versus discharged using univariate analysis with the chi-square test, because all of our variables were categorical variables. Hospital-level admission rates were calculated for a series of scenarios. First, we calculated overall admission rates by hospital for the entire time period, then by day of the week. Admission rates for a primary diagnosis of fever, neutropenia, and the FN variable were calculated both overall and by day of the week.
The degree of interhospital variation in admission rates for each of the specific scenarios listed above were evaluated using a common statistical test called the index of dispersion (ID), which represents an estimate of the overall randomness of a sample, and is useful when comparing percentages (e.g., admission rates) across multiple institutions. This measure was chosen to assess variation because it is dimensionless and can be less sensitive to a small number of outliers. ID values greater than 1 indicate data that are overdispersed (e.g., greater variability). Hospitals that had a total number of encounters that were less than five for a specific diagnosis or day of the week were excluded from that calculation to avoid a skewed variability measurement based on a small N.
Finally, we performed a one-way ANOVA to compare variation by hospital, by diagnosis (fever, neutropenia, and FN diagnoses), and by day of the week. We compared weekend (Saturday and Sunday) versus weekday using Student t test. All analyses were performed using SAS v9.4 (SAS Institute, Cary, NC) and Microsoft Excel.
3 ∣. RESULTS
We identified 60 054 ED encounters for children with cancer at 37 hospitals during the three-year study period. Of those encounters, 62.5% were admitted to the hospital, and 37.5% were discharged home from the ED. The study population (shown in Table 1) was mostly male (54.2%) and the most common race/ethnicity was non-Hispanic white (47.2%). The majority of patients had public insurance (54.8%), followed by private (40.4%), and other (4.7%). There were more younger children with 33.2% age 4 years or under and 27.2% were between ages 5 and 9 years. There were statistically significant differences in all demographics between admitted and discharged, which was explored in a previous publication.1
TABLE 1.
Encounter-level characteristics of children with cancer presenting to the emergency department, both overall and by admission status
| Patient characteristics | Overall N = 60,054 |
Admitted N = 37 547 (62.5) |
Discharged N = 22 507 (37.5) |
P value |
|---|---|---|---|---|
| N (% by column) | ||||
| Gender | 0.003 | |||
| Female | 27 521 (45.8) | 17 380 (46.3) | 10 141 (45.1) | |
| Male | 32 530 (54.2) | 20 165 (53.7) | 12 365 (54.9) | |
| Race | <0.001 | |||
| Non-Hispanic white | 28 335 (47.2) | 18 670 (49.7) | 9665 (42.9) | |
| Non-Hispanic black | 6339 (10.6) | 3961 (10.6) | 2378 (10.6) | |
| Hispanic | 17 037 (28.4) | 9622 (25.6) | 7415 (33.0) | |
| Asian | 2309 (3.8) | 1446 (3.9) | 863 (3.8) | |
| Other/unknown | 6034 (10.1) | 3848 (10.3) | 2186 (9.7) | |
| Payer | <0.001 | |||
| Public | 32 933 (54.8) | 20 084 (53.5) | 12 849 (57.1) | |
| Private | 24 280 (40.4) | 15 786 (42.0) | 8494 (37.7) | |
| Other | 2841 (4.7) | 1677 (4.5) | 1164 (5.2) | |
| Age (years) | <0.001 | |||
| 0-4 | 19 955 (33.2) | 12 879 (34.3) | 7076 (31.4) | |
| 5-9 | 16 334 (27.2) | 9395 (25.0) | 6939 (30.8) | |
| 10-14 | 11 836 (19.7) | 7553 (20.1) | 4283 (19.0) | |
| 15+ | 11 929 (19.9) | 7720 (20.6) | 4209 (18.7) |
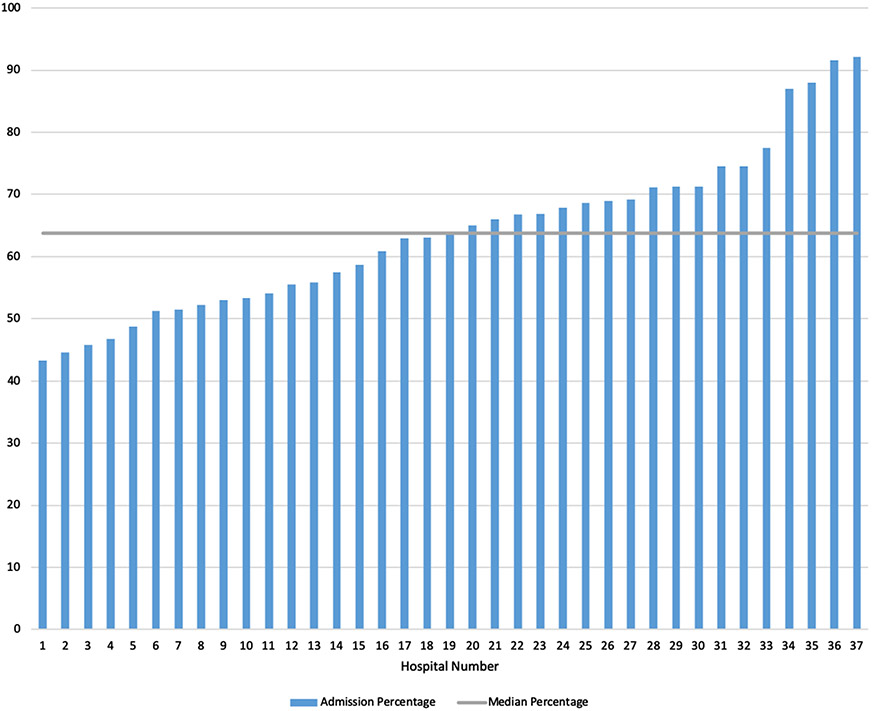
In the evaluation of overall variation in hospital admission rates, admission rates ranged from 43.2% to 92.1%, with a median of 63.7% (Figure 1). For overall admission rates by hospital, the ID was 2.6 (N = 37), indicating overdispersed admission rates with high variability.
FIGURE 1.
Overall emergency department admission rates for children with cancer by hospital
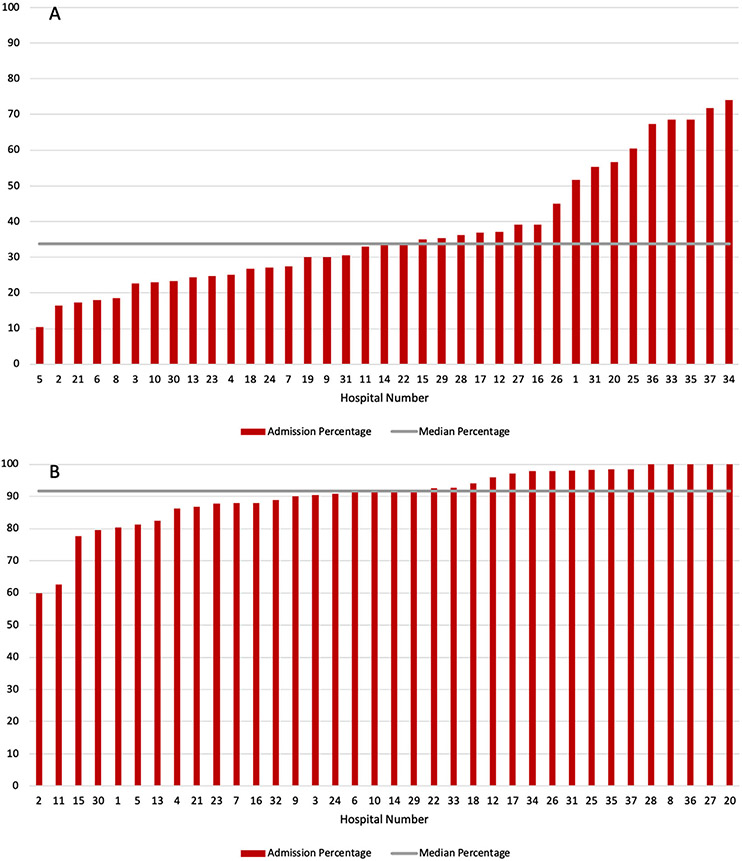
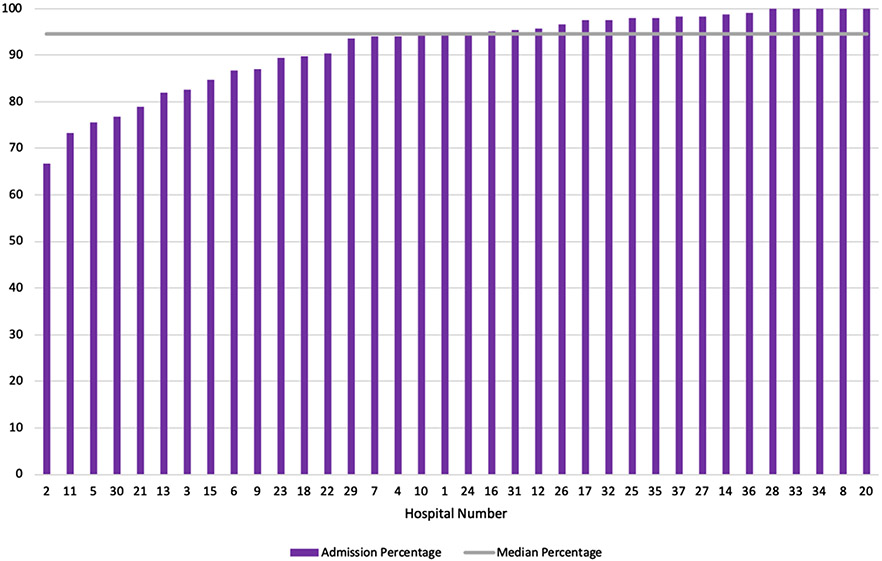
On further evaluation by primary diagnosis of fever or neutropenia, differences in variation persisted (Figure 2A and B). There were 6593 ED visits with a diagnosis of fever, 2506 visits with a diagnosis of neutropenia, and 3,008 visits that met our definition of fever with neutropenia. Children with cancer who visited the ED for a primary diagnosis of fever experienced the greatest amount of variability in admission rates ranging from 10.4% to 74.1% (median 33.8%; see Figure 2A). For fever diagnosis, we calculated an ID of 8.1 (N = 37 hospitals), indicating a large dispersion in this measure. Admission rates for a primary diagnosis of neutropenia ranged from 60% to 100% (median 91.7%; see Figure 2B). For neutropenia diagnosis, we calculated an ID of 1.0 (N = 36 hospitals). Finally, when evaluating encounters that had a diagnosis of FN, admission rates ranged from 66.7% to 100% (median 94.5%; see Figure 3). For FN, we calculated an ID of 0.83 (N = 36). These results indicate a high degree of variability for fever alone, but markedly less dispersion of data with neutropenia alone or when both fever and neutropenia was present.
FIGURE 2.
Emergency department admission rates for children with cancer by primary diagnosis of (a) fever and (b) neutropenia, by hospital
FIGURE 3.
Emergency department admission rates for children with cancer by diagnosis of febrile neutropenia, by hospital
When comparing hospital rates between institutions, we found no statistically significant effect of day of the week on variation for overall admission rates (P = 0.91). For each of the subanalyses, we found no difference among hospitals by day of the week for fever (P = 0.80), neutropenia (P = 0.49), or FN (P = 0.73). There were also no differences found when comparing weekend versus weekday for overall admission rates (P = 0.52), fever (P = 0.58), neutropenia (P = 0.93), and FN (P = 0.10)
4 ∣. DISCUSSION
In this retrospective cohort study using administrative data from 37 U.S. children’s hospitals, we found wide variability in overall admission rates between hospitals for children with cancer who sought care in the ED. Previous literature has demonstrated that there was variation in admission rates by reason for ED visit,1,2 and we have now shown that there is also variation by hospital both overall and for each of the scenarios investigated. The greatest variability was for a primary diagnosis of fever, with less variability among a primary diagnosis of neutropenia or FN. Day of the week or weekend versus weekday did not have a significant impact on between hospital variation.
We found the highest amount of variability for ED admission rates overall and for ED visits with a primary diagnosis of fever. There was less variability when the primary diagnosis was neutropenia or if the patient met the criteria to be labeled as FN. Interestingly, there was no significant impact on admission rates for this population in any of the clinical scenarios when evaluating by day of the week or weekend versus weekday. These findings highlight several important areas for future investigation. For the variation in admissions by hospital seen for the primary diagnosis of fever, patient-level information is needed to better understand the circumstances surrounding the ED visits. Specifically, evaluating if there was an objective fever documented and the impact of their laboratory values including their absolute neutrophil count. The lack of effect by day of the week was a surprising finding, and thus deserves future investigation to understand the role of communication and triage decision-making that occurs between ED providers and oncologists when children with cancer present to the ED, and how it may differ from other conditions.
When considering the variation for overall admission rates by hospital, the causes are likely multifactorial and include both hospital-system, provider-level, and patient-level contributions. Some of the variation may be due to differences in triaging practices among institutions and also among providers within the same institution. Some institutions routinely send all children with cancer to the ED for management, whereas others have the capacity to evaluate and manage urgent clinical needs in the pediatric oncology clinic. From a provider level, there are differences in preferences and practices specifically around the treatment of fevers in pediatric oncology patients,5 which may influence ED admission rates.
When an ED visit had a primary diagnosis of fever with any associated diagnosis of neutropenia, the variation in admission rates went down significantly, and the median admission rates were much higher. These findings appear to suggest that the general clinical expectations is that children with cancer who present to the ED with FN are treated similarly with upfront inpatient admission for treatment and monitoring.8,9 Yet interestingly, there continues to be a lack of a clear consensus among pediatric oncologists on the management of FN, despite continued evidence that there are risk stratification schemas that can be instituted.10-15
Previous analyses show differences in admission rates and outcomes for patients who seek care in the ED during the weekends.16-23 We thought that the ability to access outpatient resources during the weekdays might affect admission rates, yet this was not found to be a significant factor in admission rates for children with cancer. Because ED encounters by children with cancer are a very small proportion of national ED visits,2 ED providers may not be as familiar with their care and management. Typically, oncology providers provide phone consultation to discuss each patient who presents to the ED. An important research avenue to explore would be to evaluate and quantify if there is variation in management practices by oncology providers both within and between hospital systems. Additionally, future research could focus on qualitative differences among ED providers’ views of shared patient care for children with cancer, which could determine the ways in which clinical decisions are made and how to optimize those points of communication.
5 ∣. LIMITATIONS
Although this study provided insight into admission rate variation among hospitals, several important limitations should be considered. As with previous analyses of PHIS data, we used ICD-9-CM codes to capture our patient population and evaluate the reasons for their ED encounter. Therefore, it is possible we are not accurately identifying all patients with cancer if their diagnosis was not included on an encounter, which could lead to overestimation or underestimation of ED cases. PHIS data set does not reliably determine the chief complaint that led to the ED visit, so the reason for the ED visit was extrapolated from ICD-9-CM codes. Differences in coding of diagnosis by hospital may also contribute to some of the variability measured in this evaluation. PHIS does not include all hospitals that diagnose and treat children with cancer, thus it was not possible to accurately determine if a subject presented to the ED for a new diagnosis or continued care. We chose not to include ICD-10 data in order to decrease the chance for inconsistencies with conversion. We also did not have access to important clinical data such as vital signs and physical exam findings, laboratory results, or imaging results, which impact clinical decision-making. We attempted to evaluate for differences by day of the week, but our evaluation does not account for holidays which may impact hospital resources, such as staffing patterns, that could affect decision-making. For this evaluation, we also did not intend to address the necessity or preventability of the hospital admission because we do not have access to key clinical features, severity of illness, or sociodemographic factors that may have impacted clinical decision-making.
6 ∣. CONCLUSION
In conclusion, we found that the admission rates of children with cancer who sought care in the ED vary widely by institution both overall and for diagnosis of fever. When evaluated by diagnosis, patients who presented with fever had the highest amount of variation in admission rates. Further research is needed to better understand the sources of the variation including patient-level clinical presentation details, provider preferences, or institutional policies that lead to the greatest amount of variability. Next steps would then be to use this information to create standards of best practices for children with cancer who are evaluated in the ED.
FUNDING INFORMATION
A portion of Anneli Cochrane’s salary was provided by the Jeff Gordon Children’s Foundation.
Abbreviations:
- ED
emergency department
- FN
febrile neutropenia
- ICD-9-CM
International Classification of Diseases, Ninth Edition, Clinical Modification
- ID
index of dispersion
- PHIS
Pediatric Health Information System
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
LINKED CONTENT
This article is linked to an article by Seethal A. Jacob et al. https://onlinelibrary.wiley.com/doi/epdf/10.1002/pbc.28067
DATA SHARING
The data that support the findings of this study are openly available through the Pediatric Health Information System at https://www.childrenshospitals.org/phis.References.
REFERENCES
- 1.Mueller EL, Hall M, Shah SS, August KJ, Radhi MA, Macy ML. Characteristics of children with cancer discharged or admitted from the emergency department. Pediatr Blood Cancer. 2016;63(5):853–858. [DOI] [PubMed] [Google Scholar]
- 2.Mueller EL, Sabbatini A, Gebremariam A, Mody R, Sung L, Macy ML. Why pediatric patients with cancer visit the emergency department: United States, 2006–2010. Pediatr Blood Cancer. 2015;62(3):490–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aronson PL, Thurm C, Alpern ER, et al. Variation in care of the febrile young infant <90 days in US pediatric emergency departments. Pediatrics. 2014;134(4):667–677. [DOI] [PubMed] [Google Scholar]
- 4.Jain S, Elon LK, Johnson BA, Frank G, DeGuzman M. Physician practice variation in the pediatric emergency department and its impact on resource use and quality of care. Pediatr Emerg Care. 2010;26(12):902–909. [DOI] [PubMed] [Google Scholar]
- 5.Mueller EL, Walkovich KJ, Yanik GA, Clark SJ Variation in management of fever and neutropenia among pediatric patients with cancer: a survey of providers in Michigan. Pediatr Hematol Oncol. 2015;32(5):331–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colvin JD, Hall M, Berry JG, et al. Financial loss for inpatient care of Medicaid-insured children. JAMA Pediatr. 2016;170(11):1055–1062. [DOI] [PubMed] [Google Scholar]
- 7.Mongelluzzo J, Mohamad Z, Ten Have TR, Shah SS. Corticosteroids and mortality in children with bacterial meningitis. JAMA. 2008;299(17):2048–2055. [DOI] [PubMed] [Google Scholar]
- 8.Freifeld AG, Bow EJ,Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52(4):e56–93. [DOI] [PubMed] [Google Scholar]
- 9.Pizzo PA. Management of fever in patients with cancer and treatment-induced neutropenia. N Engl J Med. 1993;328(18):1323–1332. [DOI] [PubMed] [Google Scholar]
- 10.Henry M, Sung L. Supportive care in pediatric oncology: oncologic emergencies and management of fever and neutropenia. Pediatr Clin North Am. 2015;62(1):27–46. [DOI] [PubMed] [Google Scholar]
- 11.Lehrnbecher T, Robinson P, Fisher B, et al. Guideline for the management of fever and neutropenia in children with cancer and hematopoietic stem-cell transplantation recipients: 2017 update. J Clin Oncol. 2017;35(18):2082–2094. [DOI] [PubMed] [Google Scholar]
- 12.Manji A, Beyene J, Dupuis LL, Phillips R, Lehrnbecher T, Sung L. Outpatient and oral antibiotic management of low-risk febrile neutropenia are effective in children-a systematic review of prospective trials. Support Care Cancer. 2012;20(6):1135–1145. [DOI] [PubMed] [Google Scholar]
- 13.Paolino J, Mariani J, Lucas A, et al. Outcomes of a clinical pathway for primary outpatient management of pediatric patients with low-risk febrile neutropenia. Pediatr Blood Cancer. 2019;66:e27679. [DOI] [PubMed] [Google Scholar]
- 14.Teuffel O, Ethier MC, Alibhai SM, Beyene J, Sung L. Outpatient management of cancer patients with febrile neutropenia: a systematic review and meta-analysis. Ann Oncology. 2011;22(11):2358–2365. [DOI] [PubMed] [Google Scholar]
- 15.Vidal L, Ben dor I, Paul M, Pokroy E, Soares-Weiser K, Leibovici L. Oral versus intravenous antibiotic treatment for febrile neutropenia. Cochrane Database Syst Rev. 2013;10:CD003992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson RT, Bennett WE Jr, Finnell SM, Downs SM, Carroll AE. Increased length of stay and costs associated with weekend admissions for failure to thrive. Pediatrics. 2013;131(3):e805–810. [DOI] [PubMed] [Google Scholar]
- 17.Kostis WJ, Demissie K, Marcella SW, et al. Weekend versus weekday admission and mortality from myocardial infarction. NEJM. 2007;356(11):1099–1109. [DOI] [PubMed] [Google Scholar]
- 18.Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke. Stroke. 2007. Apr;38(4):1211–1215. [DOI] [PubMed] [Google Scholar]
- 19.Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009. ;7(3):296–302. [DOI] [PubMed] [Google Scholar]
- 20.Aujesky D, Jimenez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009. Feb 24;119(7):962–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crowley RW, Yeoh HK, Stukenborg GJ, Ionescu AA, Kassell NF, Dumont AS. Influence of weekend versus weekday hospital admission on mortality following subarachnoid hemorrhage. Clinical article. J Neurosurg. 2009. Jul;111(1):60–66. [DOI] [PubMed] [Google Scholar]
- 22.Crowley RW, Yeoh HK, Stukenborg GJ, Medel R, Kassell NF, Dumont AS. Influence of weekend hospital admission on short-term mortality after intracerebral hemorrhage. Stroke. 2009. Jul;40(7):2387–2392. [DOI] [PubMed] [Google Scholar]
- 23.Barba R, Zapatero A, Losa JE, Marco J, Plaza S, Rosado C, Canora J. The impact of weekends on outcome for acute exacerbations of COPD. Eur Respir J. 2012. Jan;39(1):46–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available through the Pediatric Health Information System at https://www.childrenshospitals.org/phis.References.