Abstract
Metabolic reprogramming is a hallmark of cancer and has proven to be critical in viral infections. Metabolic reprogramming provides the cell with energy and biomass for large-scale biosynthesis. Based on studies of the cellular changes that contribute to metabolic reprogramming, seven main hallmarks can be identified: (1) increased glycolysis and lactic acid, (2) increased glutaminolysis, (3) increased pentose phosphate pathway, (4) mitochondrial changes, (5) increased lipid metabolism, (6) changes in amino acid metabolism, and (7) changes in other biosynthetic and bioenergetic pathways. Viruses depend on metabolic reprogramming to increase biomass to fuel viral genome replication and production of new virions. Viruses take advantage of the non-metabolic effects of metabolic reprogramming, creating an anti-apoptotic environment and evading the immune system. Other non-metabolic effects can negatively affect cellular function. Understanding the role metabolic reprogramming plays in viral pathogenesis may provide better therapeutic targets for antivirals.
Keywords: metabolic reprogramming, Warburg effect, virus, viral replication, glycolysis, glutaminolysis, pentose phosphate pathway, mitochondria, lipid metabolism, amino acid metabolism, biomass, biosynthetic and bioenergetic pathways
1. Introduction
Metabolic reprogramming is a crucial area of study in cancer and is listed as a hallmark of cancer [1]. Dr. Otto Warburg first described metabolic reprogramming while studying the properties of tumorigenic cells. He observed an increase in the metabolism of glucose, known as glycolysis, and a subsequent high concentration of lactic acid [2]. Dr. Warburg noted that this increase in glycolysis was taking place even in the presence of oxygen. Typically, the cell utilizes mitochondrial oxidative phosphorylation (OXPHOS) when oxygen is the only available resort to upregulating glycolysis in a hypoxic environment. For that reason, the finding that cancer cells act as hypoxic cells was surprising. The term for this phenomenon is the Warburg effect and is defined as an increase in glucose uptake and increase in lactate production even in the presence of oxygen [3]. A significant role of the Warburg effect is to provide the rapidly proliferating cancer cells with enough “building blocks” to fuel cellular division. These building blocks are also known as biomass (nucleotides, amino acids, and lipids) and are essential for creating new cells [4]. Biomass is generated in a significant quantity, partly through the Warburg effect. Since its characterization, the Warburg effect remains a part of a broader phenomenon referred to as metabolic reprogramming [5].
In addition to cancer cells, viruses also depend on biomass to fuel viral replication and production of new virions; therefore, they depend on metabolic reprogramming [6,7,8]. Most studies concerning metabolic reprogramming arise from cancer models and cancer samples. Like cancer, metabolic reprogramming contributes to viral infections. Here, we summarized the current literature that defines the hallmarks of metabolic reprogramming and their involvement in viral replication.
2. Hallmarks of Metabolic Reprogramming
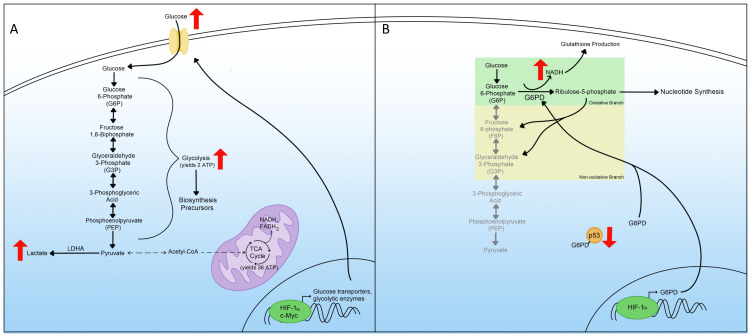
Metabolic reprogramming is an integral part of both cancer and viral infections, not only to provide the materials for the large-scale biosynthesis for rapid replication and survival but also to provide energy for these processes [9,10]. We classified changes in cellular metabolism that contribute to metabolic reprogramming in six main hallmarks: (1) increased glycolysis and lactic acid, (2) increased pentose phosphate pathway (PPP), (3) increased glutaminolysis, (4) mitochondrial changes, (5) increased lipid metabolism, (6) changes in amino acid metabolism, and (7) changes in other biosynthetic and bioenergetic pathways (Figure 1). These hallmarks play crucial roles in viral pathogenesis. Hence, it is necessary to describe these hallmarks’ involvement before understanding how viruses take advantage of them.
Figure 1.
Hallmarks of metabolic reprogramming. The illustration represents the seven hallmarks of metabolic reprogramming: 1—increased glycolysis, 2—increased glutaminolysis, 3—increased pentose phosphate pathway, 4—mitochondrial changes and TCA rewiring, 5—increased lipid metabolism, 6—changes in amino acid metabolism, and 7—changes in other biosynthetic and bioenergetic pathways.
3. Glycolysis
An increase in glycolysis, glucose uptake, and lactic acid production was the first hallmark of metabolic reprogramming recognized by Dr. Warburg in 1924; therefore, it is referred to as the Warburg effect [3,11]. In normal cells, glucose is converted into pyruvate through regulated enzymatic reactions called glycolysis. Pyruvate is then transformed into acetyl coenzyme A (acetyl-CoA), which fuels the tricarboxylic acid cycle (TCA cycle), also known as the Krebs cycle [12,13]. Through the TCA cycle, the cell generates nicotinamide adenine dinucleotide (NAD) + hydrogen (H) (NADH) and flavin adenine dinucleotide (FAD) + 2 hydrogens (H2) (FADH2). These products are used in the mitochondrial respiratory chain through oxidative phosphorylation (OXPHOS) to produce 36 molecules of cellular energy in the form of adenosine triphosphate (ATP) [14]. However, during metabolic reprogramming, cells favorably use glycolysis without pyruvate production to produce lactic acid instead, even in the presence of oxygen (Figure 2A). This phenomenon of glycolysis in the presence of oxygen is known as aerobic glycolysis [15,16]. Because glycolysis produces only two molecules of ATP, cells must compensate for the reduction of ATP by upregulating the amount of glucose that undergoes glycolysis [17,18]. Hence, cells first need to increase the uptake of glucose. Many cells achieve this by activating glucose transporters [19,20]. Additionally, metabolic reprogrammed cells exhibit an increase in glycolytic enzymes to promote further glycolysis [4,21]. Cells experiencing metabolic reprogramming utilize HIF-1α and c-Myc transcription factors, master inducers of glycolysis, to upregulate glucose transporters and glycolytic enzymes (Figure 2A) [15].
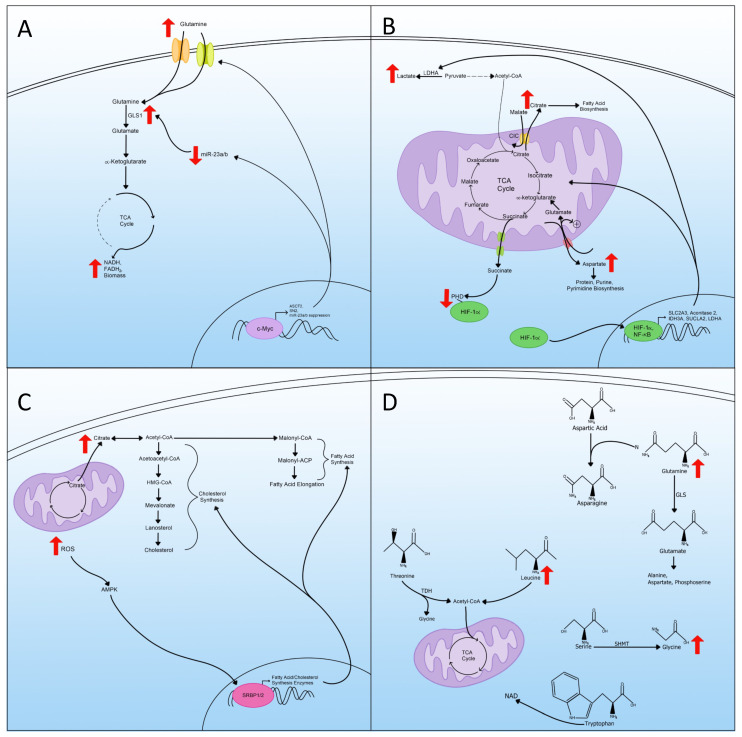
Figure 2.
Glycolysis and the pentose phosphate pathway in metabolic reprogramming. (A) Upregulated glycolysis in metabolic reprogramming including the transcriptional regulation and increased expression of glucose transporters as well as the consequences of increased glycolysis. (B) Mechanisms leading to pentose phosphate pathway (PPP) upregulation during metabolic reprogramming include both branches and transcriptional regulation of critical enzymes.
Increased glucose uptake and decreased pyruvate, available to enter the TCA cycle, activates the glycolytic pathway. In normal cells, the end product of glycolysis is acetyl-CoA, converted from pyruvate, and this acetyl-CoA can then be converted to citrate and continue through the TCA cycle to produce 36 ATP molecules. However, in metabolic reprogramming, the major end product of glycolysis is lactate instead, which does not enter the TCA cycle [22]. The switch between producing acetyl-CoA from pyruvate to lactate contributes to the upregulation of lactate dehydrogenase A (LDHA), and this switch is beneficial since it helps regenerate NADH to continue the increase in glycolysis (Figure 2A) [23,24].
Increased glycolysis results in the accumulation of many biosynthesis precursors. Many glycolytic metabolites are utilized as building blocks in the biosynthesis of needed cellular products. One of these metabolites, glucose-6-phosphate (G6P), is consumed in the PPP, generating precursors for nucleotide synthesis [25]. Another beneficial glycolytic metabolite is dihydroxyacetone phosphate (DHAP), which is utilized in lipid synthesis. Other metabolites are important in amino acid production and macromolecule synthesis [26,27,28]. The importance of these metabolites in other aspects of cellular maintenance makes increasing glycolysis a considerable step in metabolic reprogramming and a therapeutic target for diseases associated with metabolic reprogramming.
4. Pentose Phosphate Pathway
The pentose phosphate pathway (PPP) is a metabolic pathway composed of two arms. The oxidative arm generates NADPH and converts G6P into ribulose-5-phosphate to produce nucleotides through nucleic acid synthesis [29]. The other axis of the PPP is the non-oxidative one that generates fructose-6-phosphate (F6P) and glyceraldehyde-3-phosphate (G3P) from G6P [30]. These products can participate in glycolysis and other metabolic pathways (Figure 2B). The first branch is essential for supplying the cells with ribulose-5-phosphate because of the increased demand for nucleotides. Therefore, the generated NADPH is used for glutathione production, which protects the cell from oxidative stress and apoptosis [31]. NADPH is also used by the cell in the biosynthesis of lipids and other macromolecules, and the increase in NADPH contributes to overall metabolic reprogramming [32].
The increase in the PPP associated with metabolic reprogramming is the result of increased expression of enzymes in the PPP [33,34]. One of the essential elevated enzymes during metabolic reprogramming is glucose-6-phosphate dehydrogenase (G6PD), the first enzyme of the PPP, and it aids in converting G6P to ribulose-5-phosphate (Figure 2B) [29]. G6PD’s enzymatic activity is regulated by the tumor suppressor protein, where in normal cells, p53 associates with G6PD and prevents it from forming heterodimers and becoming enzymatically active [35]. In cells where p53 activity is downregulated, such as cancer cells, G6PD is no longer negatively regulated and contributes to metabolic reprogramming (Figure 2B). Transcriptionally, G6PD can be induced through the HIF-1α protein [36,37]. The activity of HIF-1α increases in metabolic reprogrammed cells [38]. Overall, the increase in the PPP is a hallmark of metabolic reprogramming and understanding how it contributes to this phenomenon may help find better therapeutic targets for diseases associated with metabolic reprogramming.
5. Glutaminolysis
Glutaminolysis is a process in which multiple enzymes convert glutamine into TCA cycle metabolites by way of α-ketoglutarate [39]. Glutamine is considered the most abundant amino acid found within the body and is necessary for protein, nucleotide, and lipid synthesis [40]. In metabolic reprogrammed cells, since pyruvate is diverted away from entering the TCA cycle, glutamine is utilized to replenish important metabolites from the TCA cycle to synthesize biomass [41]. The use of glutamine as an anaplerotic substrate for the TCA cycle is the continued production of NADH, FADH2, and electrons that are utilized for ATP production through mitochondrial OXPHOS [42,43].
To trigger glutaminolysis, cells rely on the actions of c-Myc to upregulate glutamine transporters and enzymes required for glutaminolysis (Figure 3A) [44,45]. C-Myc protein increases the expression of glutamine transporters alanine-serine-cysteine transporter 2 (ASCT2) and SN2, resulting in increased cellular uptake of glutamine (Figure 3A) [46]. C-Myc also increases glutaminolysis by suppressing miR-23a/b, which negatively regulates the expression of GLS1, the enzyme required for glutaminolysis [47]. The suppression of miR-23a/b allows the expression of GLS1, which induces the amount of glutamate converted from glutamine that can replenish the TCA cycle (Figure 3A). Glutaminolysis is therefore used to assess the metabolic state of the cell. The dependence on glutamine in metabolic reprogrammed cells may be exploited in therapies for diseases associated with metabolic reprogramming.
Figure 3.
Glutaminolysis, mitochondrial changes, lipid metabolism, and amino acid metabolism in metabolic reprogramming. (A) Upregulation of glutaminolysis via transcriptional regulation and the status of miR-23. The cartoon also displays an increased expression of glutamine transporters and enzymes. (B) A schematic representation of mitochondrial rewiring of the TCA cycle during metabolic reprogramming includes transporting key TCA metabolites outside the mitochondria and the transcriptional regulation of critical enzymes and transporters. (C) Increased lipid metabolism, ROS, and the transportation of citrate out of the mitochondria used for lipid synthesis as a part of metabolic reprogramming. (D) Amino acid metabolism regulation in metabolic reprogramming includes the increase in certain amino acids that act as precursors for others.
6. Mitochondrial Changes and TCA Cycle Rewiring
Mitochondria are essential components for many metabolic pathways, namely the TCA cycle and the electron chain. They are crucial for maintaining many aspects of cellular homeostasis [48,49]. During metabolic reprogramming, mitochondria change from primarily being used for energy production, by way of the mitochondrial electron transport chain, to playing a role in generating TCA cycle metabolites to be used in the biogenesis and redox balance [50]. This phenomenon was initially proposed in the Warburg effect as being primarily caused by mitochondrial dysfunction but has since been found to be more of a “rewiring” in the TCA cycle [51].
The rewiring of the metabolic pathway within the mitochondria involves many metabolites, such as citrate, which is the first intermediate in the TCA cycle [52]. In metabolic reprogramming, increased exportation of citrate from the mitochondria to the cytosol occurs (Figure 3B). Once out of the mitochondria, the citrate no longer contributes to the TCA cycle; thus, a “rewiring” has occurred. This exportation is achieved by the mitochondrial citrate carrier (CIC), which exchanges citrate for malate. Once exported, the citrate is used for the biosynthesis of fatty acids [53,54]. In addition to fatty acid biosynthesis, cytosolic citrate produces acetyl-CoA and oxaloacetate, which can be converted further into malate and transported back into the mitochondria by the CIC [55,56].
Another TCA cycle intermediate impacted by this rewiring is aspartate, where the production and exportation to the cytosol are altered (Figure 3B) [57]. Aspartate moves to the cytosol in exchange for glutamate and a proton by the mitochondrial aspartate/glutamate carriers (AGC1 and AGC2) [55]. The newly incoming glutamate can then enter the TCA cycle as α-ketoglutarate as an anaplerotic substrate to continue to fuel the TCA in the absence of pyruvate, characteristic of metabolic reprogramming (Figure 3B). The exportation of aspartate is essential for protein, purine, and pyrimidine biosynthesis and is the rate-limiting event in the biosynthesis of these in tumor cells [58]. The transport of aspartate is part of the larger malate/aspartate shuttle (MAS) and is essential to regenerate cytosolic NAD+ for use in glycolysis [59].
Succinate, another TCA cycle intermediate, acts as a signaling messenger linking TCA cycle rewiring and metabolic reprogramming [60]. Succinate is transported out of the inner mitochondria by the dicarboxylic acid carrier to the cytosol by a voltage-dependent anion channel (Figure 3B) [61,62]. Cytosolic succinate can then interact with and inhibit the oxygen-dependent prolyl hydroxylase (PHD) enzyme, which is responsible for targeting HIF-1α for degradation [63]. Therefore, as succinate is transferred out of the TCA cycle, it contributes to the increase in HIF-1α and thus metabolic reprogramming.
Some of these changes seen in TCA cycle rewiring are due to altered gene expression of either transporters or the enzymes that make up the TCA cycle [50]. One regulator of cell metabolism in the context of metabolic reprogramming is nuclear factor kappa B (NF-κB) [64,65]. NF-κB upregulates the expression of the glucose transporter SLC2A3 and enhances the expression of three TCA cycle enzymes, aconitase 2, isocitrate dehydrogenase 3A (IDH3A), and succinyl-CoA ligase (SUCLA2) [66,67]. Through this regulation, NF-κB upregulates glycolysis and contributes to the rewiring of the TCA cycle and metabolic reprogramming (Figure 3B).
Along with NF-κB, HIF-1α plays a role in switching the mitochondria from an energy producer to processing TCA intermediates for biosynthesis. HIF-1α acts as a master regulator of metabolic reprogramming through the upregulation of genes important for glycolysis [68,69]. Along with upregulating the genes for glycolysis, HIF-1α also increases the expression of lactate dehydrogenase A (LDHA), which inhibits pyruvate dehydrogenase (PDH) through phosphorylation [70,71]. The inhibition of PDH drives the conversion of pyruvate to lactate and away from acetyl-CoA, reducing the amount of acetyl-CoA that enters the TCA cycle for energy production (Figure 3B) [72,73]. In these ways, HIF-1α contributes to metabolic reprogramming by regulating gene expression associated with mitochondrial changes and TCA cycle rewiring.
7. Lipid Metabolism
The increase in lipid metabolism is another hallmark because lipids are essential building blocks for cancer and viruses to create new organelles, cells, and virions [74,75]. Lipid synthesis is a multi-enzyme process involving many steps, usually starting with acetyl-CoA and ending in fatty acids [76,77]. In metabolic reprogrammed cells, the majority of acetyl-CoA for lipid synthesis comes from citrate produced by the TCA cycle, and that has been transported out of the mitochondria. In the cytosol, citrate can then be converted back into acetyl-CoA and undergo lipid synthesis (Figure 3C) [78].
Cholesterol is another lipid that increases during metabolic reprogramming [79]. The cholesterol synthesis pathway, the mevalonate, is another branch of lipid synthesis that starts with acetyl-CoA and ends with the conversion of lanosterol into cholesterol (Figure 3C) [80,81]. Cholesterol synthesis is a crucial component of membranes and controls the membrane fluidity and formation of lipid rafts [82]. Cholesterol activates the Ras-Raf signaling pathway, which is often utilized by viruses and cancers to manipulate cellular transcription [83,84].
The sterol regulatory element-binding proteins (SREBPs), a family of transcription factors, control many enzymes involved in fatty acid and cholesterol synthesis [78]. Two different SREBPs are involved in this regulation of lipid synthesis; the first, SRBP1, regulates fatty acid synthesis, while the second, SRBP2, regulates cholesterol synthesis [85,86]. The SREBPs are controlled by AMP-activated protein kinase (AMPK) signaling, and in metabolic reprogramming, increased accumulation of ROS can activate AMPK, thus increasing the transcription of SREBPs, resulting in increased lipid and cholesterol synthesis (Figure 3C) [87,88].
8. Amino Acid Metabolism
For metabolic reprogrammed cells to produce biomass at a high rate, amino acids need to be either synthesized, used as carbon sources, used as nitrogen sources, or used as electron transporters [89]. Cells can also use branched-chain amino acids (BCAA), leucine, isoleucine, and valine, to fuel the TCA cycle [90]. Of the BCAAs, leucine is elevated with metabolic reprogramming and is converted into acetyl-CoA, and then fed into the TCA cycle (Figure 3D) [91,92]. Other than BCAAs, threonine can also be catabolized by threonine dehydrogenase (TDH), producing glycine and acetyl-CoA, and subsequentially can enter the TCA cycle as well (Figure 3D) [93,94].
In addition to being used as alternative ways to produce acetyl-CoA for use in the TCA cycle, amino acids can also be used as material for biomass and are required for the synthesis of proteins, lipids, and nucleic acids [89]. Glutamine is used in the synthesis of many non-essential amino acids (NEAAs). For example, in the synthesis of asparagine, glutamine supplies the nitrogen to be used in the conversion of aspartic acid to asparagine (Figure 3D) [95]. Glutamine is also converted to glutamate by glutaminase (GLS), and then glutamate can be further converted to other amino acids such as alanine, aspartate, and phosphoserine [39,96].
Arginine is another amino acid used as a precursor for other NEAAs. An increase in arginine promotes proline synthesis and can also be used as another source of glutamate in metabolic reprogrammed cells [97]. Another amino acid metabolism pathway that is important in the biosynthesis of nucleotides is the conversion of serine to glycine through the serine hydroxymethyltransferase (SHMT), which provides pools of one-carbon methyl groups to be used in de novo nucleotide biosynthesis (Figure 3D) [98].
In addition to NEAA synthesis, amino acid metabolism also supplies carbon atoms for lipid biosynthesis and contributes to acetyl-CoA supply [99]. Amino acid metabolism also contributes nitrogen and carbon for nucleic acid synthesis and is required for purine synthesis [100,101]. The essential amino acid tryptophan can be used in NAD de novo synthesis to replenish NAD levels to continue to fuel the increase in metabolic redox reactions (Figure 3D) [102,103]. In all, amino acid metabolism is essential for metabolic reprogramming through many different pathways ranging from alternative energy to providing materials for the synthesis of proteins, lipids, and nucleotides.
9. Other Biosynthetic and Bioenergetic Pathways
The fatty acid oxidation (FAO) pathway is another pathway that is promoted during metabolic reprogramming and provides the cell with ATP through fatty acids (FA) being oxidized in the mitochondria or by cytoplasmic lipophagy [104,105]. FAO is where fatty acids are oxidized into acetyl-CoA and produce NADH and FADH2. Then, the acetyl-CoA is imported into the TCA cycle to generate more NADH and FADH2. Afterward, the NADH and FADH2 are used to fuel OXPHOS for ATP production [106]. Metabolic reprogrammed cells use the acetyl-CoA produced by FAO to energize the TCA cycle, generating additional TCA cycle intermediates, such as citrate, succinate, and aspartate [107,108,109,110].
The increase of citrate through the FAO-fueled TCA cycle turns into α-ketoglutarate or pyruvate, and both reactions generate NADPH [111]. NADPH is essential for maintaining redox homeostasis and cell survival and promoting enzymes to sustain large-scale biosynthesis [112]. The balance between NADPH used in lipid synthesis and NADPH produced in FAO is critical in metabolic reprogramming and is controlled by AMPK [113,114].
The use and production of acetyl-CoA are important in many biosynthesis pathways and post-translational modification of the synthesized products [115,116]. Because of this importance, another pathway metabolic reprogrammed cells can take advantage of to replenish the acetyl-CoA is the conversion of acetate into acetyl-CoA by the mitochondrial-localized acetyl-CoA synthetase 1 (ACSS1) [117]. The production of acetyl-CoA from acetate is crucial for metabolic reprogramming to continuously fuel biosynthesis [118].
10. Metabolic Reprogramming and Viruses
Although most metabolic research was performed in the cancer field, viruses also take advantage of these pathways to produce the material and environment needed to sustain a large output of virions [9]. The results of metabolic reprogramming in viral infections provide the virus with free nucleotides for viral genome replication, amino acids for virion assembly, and lipids for membrane formation to envelope the virion [119]. That said, viral infections have been shown to alter the hallmark pathways of metabolic reprogramming.
11. Viruses and Glycolysis
Increased glycolysis and lactate production are the typical metabolic changes associated with viral infection [120]. Increased glycolysis also correlates with an increase in glucose consumption and lactate production. This was confirmed using primary human foreskin fibroblast (HFF) cells and non-tumorigenic breast epithelial cells infected with the human cytomegalovirus (HCMV) or adenovirus, respectively [121,122,123,124]. A decrease in oxygen consumption used in mitochondrial OXPHOS was demonstrated in adenovirus-infected non-tumorigenic breast epithelial cells [124]. Similar changes were described in human hepatoma (Huh7) cells infected with the hepatitis C virus (HCV) [125].
Further, HCV also increases the expression of glycolytic enzymes in these cells [126]. Increased glycolysis, lactate production, and glucose uptake have also been shown in Influenza A H1N1-infected cells between 8 and 12 h post-infection and HIV-infected CD4+ T-cells, respectively [127,128,129]. An increase in glycolysis has been directly linked to an active replication of the Dengue virus that continues to manifest for at least 48 h post-infection [130].
Using primary neural progenitor cells infected with Enterovirus A71 (EV-A71), targeted metabolomics analysis resulted in increased glycolytic metabolites. These results indicated that EV-A71 causes a metabolic switch to activate glycolysis. It also demonstrated that increased metabolites are associated with other processes involved in metabolic reprogramming, such as increased pentose phosphate pathway, increased gluconeogenesis, and increased glutamate metabolism [131].
Latent viral infection also increases glycolysis, as demonstrated using endothelial cells infected with latent Kaposi’s sarcoma-associated herpesvirus (KSHV) [132]. KSHV infection also promotes glucose uptake by activating the glucose transporter 3 (GLUT3) and the glycolytic enzyme hexokinase 2 (HK2). HK2 is a glycolysis rate-limiting enzyme [133]. Additionally, KSHV infection encodes multiple microRNAs present in latently expressed regions. These viral miRNAs target two glycolysis regulatory genes, EGLN2 and HSPA9. The repression of these two genes induces HIF-1α and glucose transporter 1 (GLUT1) expression, resulting in increased glycolysis and lactate production in endothelial cells where the KSHV miRNAs were overexpressed [134].
Similarly, the Epstein–Barr virus (EBV) increases the expression of HK2 through the induction of the viral protein latent membrane protein 1 (LMP-1), resulting in an increase in glycolysis [135,136]. This increase in glycolysis has also been observed in cells infected with latent EBV. Latent EBV and KSHV induce glycolysis using viral miRNAs or proteins, suggesting that metabolic reprogramming may be active during viral latency [119].
12. Viruses and Pentose Phosphate Pathway
As mentioned, viruses promote changes in the host cell that contribute to metabolic reprogramming. These changes help generate nucleic acids and lipids. The large number of generated nucleotides needed for viral genome replication are supplied by the increases in the non-oxidative branch of the pentose phosphate pathway [137,138]. Proteomics studies showed increased expression of two regulators of the non-oxidative PPP branch, the transketolase (TKT) and transaldolase 1 (TALDO1) enzymes in SARS-CoV-2-infected human Caco-2 cells [139]. Cells infected with the influenza virus display upregulation of two enzymes of the PPP, G6PD and 6-phosphogluconate dehydrogenase (6PGD), resulting in an increased conversion of NADPH and nucleotide production [140].
Several enzymes involved in the PPP were also shown to increase in human adenocarcinoma alveolar epithelial cells (A549). An established cell line uses the AdV-5 viral protein, E1A. The E1A protein induces the expression of 6-phosphogluconolactonase (6PGL) and TALDO1 enzymes, both involved in the non-oxidative branch of the PPP [141]. In latent HCV-infected cells, the rate-limiting PPP enzyme, G6PD, is upregulated, as is NADPH production [142]. In addition to NADPH production, there is also an increase in purine synthesis through the PPP in these cells. In HIV latency, an increase in G6PD and NADPH conversion and the shuttling of glycolytic metabolites to the PPP away from pyruvate production were observed [143]. Therefore, many viruses utilize the non-oxidative branch of the PPP to produce nucleotides needed for replication.
13. Viruses and Glutaminolysis
Viral infection also increases glutaminolysis, a hallmark of metabolic reprogramming. In support of this observation, HCMV infection augments the uptake of glucose and glutamine [122]. Further, in cells infected with HCMV and labeled with 13C-labeled glucose, an increase in the citrate, malate, and α-ketoglutarate expressions were observed. These results indicate an upregulation of glutaminolysis and subsequent anaplerosis of the TCA cycle [123]. HCMV infection also increases the expression of GLS and glutamate dehydrogenase (GDH) enzymes, both involved in the glutaminolysis pathway. These results indicate that HCMV increases the glutaminolysis to supplement the TCA cycle and maintain the TCA cycle intermediates along with ATP production in the mitochondria [144]. Further, the upregulation of glutamine importer ASCT2 and the increased activity of glutaminolysis regulator c-Myc induce the expression level of glutamine in cells infected with HCMV [132].
In another study where 13C-labeled glucose was used in conjunction with HSV-1 infected cells, an increase in oxaloacetate produced by the TCA cycle and increased glutamine anaplerosis was detected [145]. HSV-1 infected cells also showed increased uptake and consumption of glutamine as well as decreased viral output in the presence of a pharmacological inhibitor of GLS [146]. The increase in glutamine consumption and the decrease of viral replication associated with GLS inhibitor suggests that HSV-1 uses metabolic reprogramming, specifically glutaminolysis, to produce virions.
Adenovirus infection causes the same metabolic switch of increasing aerobic glycolysis and glutaminolysis. The induction of glutamine consumption in adenovirus type 5 (AdV-5)-infected cells occurs early during the infectious cycle [124]. Like HSV1, AdV-5 infection increases glutamine transporters ASCT2 and LAT1, allowing for increased glutamine uptake [146]. The increase in glutamine consumption in cells infected with AdV-5 infections is made possible via the reductive carboxylation pathway, which results in glutamine conversion to α-ketoglutarate and further conversion to citrate to generate acetyl-CoA [146].
Other viruses also induce glutaminolysis; for instance, rhinovirus increases glutaminolysis reliance [147]. HeLa cells infected with rhinovirus RV-B114, grown in glutamine-free media, show reduced viral replication, indicating the importance of glutaminolysis in viral replication. Huh7.5 cells infected with HCV showed the same reliance on glutamine, and when infected cells were grown in glutamine-free media, viral replication was hindered [148]. Additionally, HCV-infected Huh7.5 cells showed increased glutamine transport and glutaminolysis-associated anaplerosis of amino acid synthesis [148]. Similarly, HIV-1-infected CD4+ T-cells have also been shown to depend on increased glutaminolysis conversion to α-ketoglutarate to fuel the PPP [149]. We concluded that many viruses rely on metabolic reprogramming, specifically glutaminolysis, for their replication and virion production.
14. Viruses and Mitochondrial Changes and TCA Cycle Rewiring
Rewiring of the TCA cycle and changes in mitochondrial function are parts of metabolic reprogramming in infected cells and used in response to ROS to fuel fatty acid synthesis or deregulate cellular acetylation [150]. Increased citrate efflux out of the mitochondria is important to the TCA cycle rewiring. In HCMV-infected cells, there is an increase in citrate cataplerosis through activation of the machinery to transport citrate from the mitochondria to the cytosol [151]. Increased levels of citrate and malate were observed in fibroblasts and epithelial cells infected with HCMV or HSV-1. Using fibroblasts and epithelial cells labeled with 13C-glucose, HCMV and HSV-1 trigger a large amount of labeled carbon to incorporate into citrate [145]. However, the number of labeled carbons in citrate varies between the two infections, suggesting different pathways of upregulating citrate are used, indicating TCA cycle rewiring is occurring. In HCV-infected Huh7 cells, increased expression of ATP citrate lyase, an enzyme that converts citrate to acetyl-CoA, correlates with more citrate conversion to acetyl-CoA and increased citrate production from the TCA cycle to fuel the conversion to acetyl-CoA [152,153].
In a metabolomic study of the cerebrospinal fluid (CSF) from people with HIV with neurocognitive impairment (NCI), there were higher levels of citrate and succinate than in the CSF from people without HIV [154]. Interestingly, in patients with HIV, the increase in plasma citrate and succinate correlates with the degree of NCI observed, hinting at the importance of these metabolites, and metabolic reprogramming in a broader sense, in NCI [155]. In CSF from HIV patients on cART, there is still an increase in malate and succinate compared to CSF of uninfected patients, suggesting traditional antivirals may not be targeted enough to restore the TCA rewiring that has occurred [156].
Aspartate is another TCA cycle metabolite that is often altered during metabolic reprogramming. In HCMV, there is an increase in asparagine synthetase (ASNS), the enzyme that converts aspartate to asparagine, and it has been found that a knockout of ASNS inhibits HCMV replication [157,158]. In 13C-labeled studies using HSV-1-infected fibroblasts, there is increased incorporation of labeled carbons in aspartate compared to non-infected cells, indicating increased aspartate synthesis [145]. As was seen, many viruses rewire the TCA cycle and use overall metabolic reprogramming for viral replication.
Viruses also cause changes in metabolism, mitochondrial shape, and size [159]. The HIV-1 Vpr alters mitochondrial cristae, which results in mitochondrial swelling and irregular shape [160]. A similar effect was observed in cells infected with SARS-CoV-2 [161]. In neural cells (SF268) infected with Enterovirus 71 (EV71), in addition to cristae loss, the mitochondrial inner membrane appeared discontinuous [162].
An additional mitochondrial function disrupted during viral infections is the production of ROS. Viral infections cause increased cellular ROS through mitochondrial deregulation [163]. Viruses depolarize the mitochondrial transmembrane potential (MMP), which contributes to the accumulation of ROS. HBV depolarizes the mitochondrial membrane through its HBx protein that interacts with VDAC [164]. HCV infections also result in depolarization of the MMP; however, HCV achieves this through inhibiting ETC complex I, resulting in inhibition of electron transfer and increased ROS [165]. HIV-1 increases ROS through mitochondrial damage and dysfunction through the Vpr protein [166,167]. The Enterovirus A71 (EV-A71) protein also increases ROS through the electron transport chain and the loss of cristae structure, resulting in reduced electron transfer [162].
Hence, we concluded that viruses change mitochondrial function due to their abilities to reprogram metabolism. These changes rewire the TCA cycle, which aids in viral replication and contributes to cellular dysfunction.
15. Viruses and Lipid Metabolism
Lipid synthesis is essential for viral replication since viruses use lipid membranes to enter the host cell membrane. Lipids are also involved in viral protein maturation and viral envelope production [9]. In HCMV-infected primary HFF cells, and during lytic replication, lipid synthesis is induced by the influx of carbons from glycolysis that enter the fatty acid synthesis pathway [123]. Along with the increase in metabolites in the fatty acid synthesis pathway, HCMV also induces the expression of many enzymes involved in this pathway as well, such as ACC1 and SREBPs [151,168,169,170]. HCMV causes an induction of the carbohydrate-response binding element protein (ChREBP). The expression of ChREBP then induces the expression of many proteins responsible for reactions in the fatty acid synthesis pathway, indicating this pathway may be used by the virus for lipid metabolism [171].
In human epithelial tongue cells infected with EBV, there is an induction of the enzyme fatty acid synthase (FASN). FASN is responsible for the conversion of acetyl-CoA to long-chain fatty acids through the direct induction by the viral protein BRLF1 [172,173]. Further, the EBV latent membrane protein 1 (LMP1) increases the fatty acid synthesis and induces FASN, resulting in increased fatty acids and lipid droplets in EBV-negative Burkitt’s lymphoma (BL) cells [174]. The replication of varicella-zoster (VZV) depends on lipid synthesis. However, the addition of an FASN inhibitor alters this replication and slows fatty acid synthesis, suggesting the importance of lipid metabolism in VZV infection [175].
RNA viruses use lipid synthesis to alter the host cytoplasmic environment to make it more conducive to viral replication [176,177]. HCV infections rely heavily on lipid synthesis since lipids play a role in all aspects of the HCV viral life cycle, from cellular entry through replication on lipid rafts to viral assembly on lipid droplets [178,179]. HCV infection also increases FASN expression and induces SREBPs, resulting in increased fatty acid and lipid synthesis [180,181]. Dengue virus as well requires fatty acid synthesis to replicate [182,183]. This observation confirms that FASN is critical for Dengue virus replication and inhibition of FASN, through chemical intervention or siRNA knockdown, results in decreased viral production.
KSHV infection has been found to induce fatty acid synthesis where latently infected endothelial cells upregulate long-chain fatty acids, and there is a significant increase in lipid droplet staining [132]. If FASN or acetyl-CoA carboxylase, another enzyme responsible for fatty acid synthesis, are inhibited in latently infected cells, these cells undergo apoptosis. The addition of FASN or acetyl-CoA carboxylase inhibitors induces cell death by apoptosis, indicating that fatty acid synthesis is necessary for lipid production and as anti-apoptotic signaling in viral infection.
In HIV-infected RH9 cells, many enzymes in the fatty acid synthesis pathway are elevated, as well as the proteins responsible for an increase in low-density lipoproteins, cellular lipid metabolism, and lipid transport [184]. Similarly, HIV-infected 293T cells show an increase in FASN expression. The addition of an FASN inhibitor reduces HIV virion production by 90% compared to noninhibited infection, indicating the importance of fatty acid synthesis in HIV infection [185].
16. Viruses and Amino Acids
Amino acid synthesis is another part of metabolic reprogramming essential for viral infections and viral replication [186]. A significant quantity of amino acids is required to fuel protein synthesis and respond to the high demand for viral protein production [187,188]. In HCMV-infected MRC5 cells, it has been shown that amino acids were taken up from the cell culture medium at a much higher rate than in uninfected MRC5 cells [189]. In addition to increased uptake of amino acids, HCMV infection of MRC5 cells resulted in increased synthesis and secretion of amino acids proline and alanine [189]. Telomerase-immortalized microvascular endothelial (TIME) cells infected with KSHV also showed increases in many NEAAs, including arginine and proline, and increased amino acid metabolism pathways, including proline, arginine, alanine, and aspartate [190].
In EV71-infected Vero cells, the levels of threonine, aspartate, alanine, and glycine decreased, while glutamate, tryptophan, tyrosine, phenylalanine, and leucine increased. Interestingly, EV17 replication depends on the glutamate catabolism pathway [191].
In primary HFFs infected with the Vaccinia virus (VACV), the conversion of aspartate to asparagine was seen to be a rate-limiting step in viral replication and limits the synthesis of viral protein production [192]. Studies also demonstrated a decrease in the expression of argininosuccinate synthetase 1 (AS1) in HSV-infected fibroblasts (an enzyme that converts aspartate to arginine). However, AS1 overexpression decreases viral replication in HSV-infected fibroblasts [193]. The decreased conversion of aspartate to arginine allows for an increased concentration of aspartate to fuel the synthesis of nucleotides [194].
Patients infected with HIV have shown an increase in amino acid breakdown products, mainly the breakdown of tryptophan, and an increase in the amino acid phenylalanine in their blood [195]. Further, HIV infections lead to the depletion of tryptophan, resulting in adverse effects on normal T-cell function [196,197]. It has been shown that HIV infection causes more amino acids to be absorbed from the blood of infected patients to fuel protein synthesis, with threonine and methionine being identified as protein synthesis rate-limiting amino acids [198,199].
17. Viruses and Other Biosynthetic and Bioenergetic Pathways
Viral infections can affect other pathways involved in metabolic reprogramming as well; for instance, HCV infection increases the mitochondrial fatty acid oxidation enzyme dodecanoyl coenzyme A-delta isomerase (DCI), resulting in increased FAO [200]. In Dengue-infected Huh7 cells, an increase in FAO, through increased β-oxidation, augments the reliance on fatty acids as an energy source [201]. In SARS-CoV-2 infections, a genome assay discovered that many enzymes in the FAO and β-oxidation pathways are deregulated, resulting in changes in fatty acid synthesis and cellular energy production [202]. In HIV-infected patients, deregulated FAO results in increased fatty acids, leading to fatty liver disease [203].
α-Ketoglutarate production from glutamine has also been identified as a key conversion in many viral infections. For instance, cells infected with HCMV show an increase in GDH activity, resulting in an increase in α-ketoglutarate production [144,177]. Similarly, human respiratory syncytial virus (HRSV)-infected cells display a surge in α-ketoglutarate along with the precursors for α-ketoglutarate conversion [204]. Metabolic analysis performed on samples isolated from patients infected with SARS-CoV-2 showed an accumulation of α-ketoglutarate, suggesting that α-ketoglutarate helps replenish NAD levels to boost the glycolysis pathway [205]. In a cohort of patients with HIV undergoing cART, an increase in α-ketoglutarate and other metabolites was observed. These increases correlate with metabolic syndrome seen in these patients [206].
In metabolic reprogrammed cells, the increased production of α-ketoglutarate also corresponds with an increase in NADPH production through the conversion of α-ketoglutarate to succinyl-CoA through the enzyme alpha-ketoglutarate dehydrogenase (α-KGDH) [207,208]. The increase in NADPH then can be used in many biosynthesis pathways as well as ROS production through NADPH oxidase (NOX) enzymes [209,210]. In H1N1-infected human mucoepidermoid pulmonary carcinoma cells (NCI-H292), an increase in NOX family enzymes, mainly NOX2 and NOX4, was observed. This rise in NOX enzymes led to an accumulation in ROS production [211]. HCV-infected Huh7.5 cells also demonstrated an increased expression of NOX4 and the associated increase of ROS through NOX enzymatic reactions [212]. In SARS-CoV-2 infected patients, a surge in NOX2 was associated with the rise of oxidative stress and was predictive of coronary heart disease associated with SARS-CoV-2 infections [213]. The transfection of astrocytes with an HIV-1 gp120 expression plasmid increases NOX2 and NOX4 expression levels and ROS accumulation [214]. HIV infection also increases NOX1, NOX2, and NOX4 expression levels, all contributing to augmenting ROS production [215]. Thus, metabolic reprogramming also promotes ROS production and cellular oxidative stress.
Viral infections also alter the folate-mediated one-carbon metabolism pathway. The one-carbon metabolism pathway is essential for nucleotide and fatty acid synthesis [216]. In addition to biosynthesis, the one-carbon metabolism modifies the epigenetic pathways through DNA and histone methylation using the folate cycle metabolite S-adenosyl methionine (SAM). SAM is the methyl-donating substrate of methyltransferases that methylates DNA and histones [217]. This phenomenon depends on the serine-glycine-one-carbon pathway (SGOC). Indeed, several genes associated with the folate cycle and glycine biosynthesis were upregulated in mice infected with the Influenza A virus [218]. Inhibition of the folate cycle through targeting dihydrofolate reductase (DHFR) reduces the replication of Influenza A, Influenza B, and RSV [219]. The reduction of viral replication is the result of reduced nucleotide production associated with one-carbon metabolism [220]. Further, cells infected with SARS-CoV-2 showed increased metabolites in the methionine cycle. Hence, SARS-CoV-2 is another virus that relies on one-carbon metabolism to fuel the synthesis of viral RNA and proteins [221].
The folate cycle contributes to the overall cellular metabolic reprogramming [222]. One way the folate one-carbon pathway aids in other metabolic reprogramming pathways is through the recycling of NADP to NADPH, used in the pentose phosphate pathway [223]. Finally, the folate cycle also influences other metabolic pathways through the regulation of serine that helps the conversion of glycine from serine [224]. Serine is a key regulator of glycolysis through the regulation of pyruvate kinase enzymatic activity [225].
18. Non-Metabolic Effects of Metabolic Reprogramming
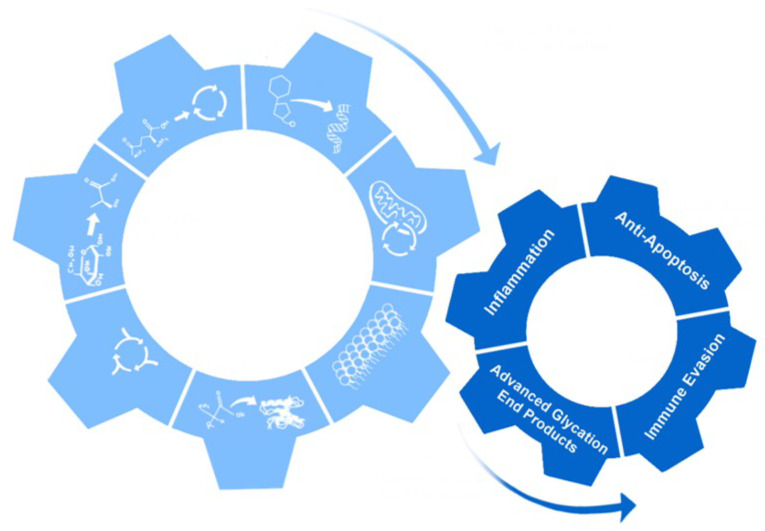
Metabolic reprogramming has many non-metabolic effects on the cell. These can include increased inflammation, anti-apoptosis, immune evasion, and the production and accumulation of advanced glycation end products (AGEs) [226]. Some of these effects are essential for viral replication and promotion of tumors, while others are byproducts of the changes that occur with metabolic reprogramming and help modify the cellular environment (Figure 4) [227].
Figure 4.
Non-metabolic effects of metabolic reprogramming. The cartoon shows how the seven hallmarks of metabolic reprogramming led to non-metabolic effects: inflammation, anti-apoptosis, immune evasion, and production of advanced glycation end products.
Inflammation produced by metabolic reprogramming can occur from the increased lactic acid output of pro-inflammatory cytokines produced through increased glycolysis and increased ROS (Figure 4) [228,229,230,231,232,233]. The inflammation produced by metabolic reprogramming can help drive molecular changes to promote more metabolic reprogramming and promote angiogenesis to supply the cells with more nutrients to sustain large amounts of biosynthesis [234,235]. Inflammation produced by metabolic reprogramming can also recruit macrophages that respond to the inflammation but also provide the cell with cytokines such as TNF-α and interleukins, which help promote metabolic reprogramming and growth and inhibit cytotoxic T-cells [236,237,238].
Metabolic reprogramming also acts as an anti-apoptotic signal mainly through the induction of glycolysis (Figure 4) [10]. During metabolic reprogramming, the cells evade apoptosis through HIF-1α. The HIF-1α protein induces glycolytic enzymes, resulting in the decrease of apoptotic signals [239,240]. The HIF-1α protein also decreases the apoptotic pathway through its direct interaction and suppression of the pro-apoptotic protein BH3 interacting-domain death agonist (BID) [241,242]. Like HIF-1α, the Akt protein also regulates glycolysis in metabolic reprogrammed cells. The Akt protein inhibits apoptosis through suppression of the p53 upregulated modulator of apoptosis (PUMA) and glycogen synthase kinase 3 (GSK-3) [243]. Several other molecules of glycolysis are also involved in apoptosis resistance. These include phosphorylation of BCL2-associated agonist of cell death (BAD), modification of cytochrome c by glucose, and the increased role NADPH has in the reduction of apoptosis induced by ROS [243,244,245].
Another result of metabolic reprogramming is the ability of the cells to evade cell death associated with the immune response (Figure 4). One way cells evade the immune system is by increasing lactate production from metabolic reprogramming, which can interfere with T-cell metabolism and decrease T-cell response [246,247]. Lactate can also damage dendritic cells and inhibit monocyte migration, further aiding in the evasion of the immune system [248,249,250,251]. In addition to the acidification of the extracellular space, metabolites can also play roles in the evasion of the immune system through the inhibition of T-cells [252]. There are multiple ways metabolic reprogramming metabolites can affect T-cells; one way is through the alterations in differentiation through the effect of kynurenine, a product of tryptophan catabolism [253]. T-cells can also be affected by an enzyme in the tryptophan catabolism pathway, indoleamine-2,3-dioxygenase (IDO), which inhibits T-cell proliferation and induces T-cell apoptosis [254,255].
Metabolic reprogramming can also result in the formation of AGEs (Figure 4). AGE formation can take place through two different pathways, both resulting in highly reactive dicarbonyls. One pathway that results in dicarbonyls is the formation and degradation of Amadori products. The first step in this reaction is the formation of Schiff bases and rearrangement to form an Amadori product [256]. These Amadori products and Schiff bases can undergo further oxidative breakdown in the presence of metal ions, which produce reactive intermediates, dicarbonyls, such as glyoxal (GO) and methylglyoxal (MG) (Figure 5) [257].
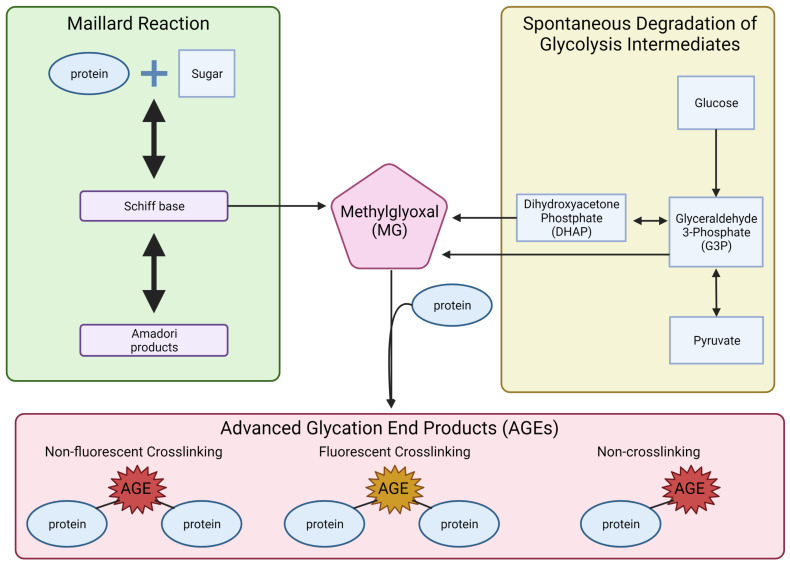
Figure 5.
Formation of the advanced glycation end products. The illustration displays two pathways: Maillard reactions and the spontaneous degradation of glycolysis intermediates that lead to the formation of three types of advanced glycation end products.
While the production of dicarbonyls by way of Amadori products can take hours to days, dicarbonyls can be formed much faster through the spontaneous degradation of glycolytic intermediates [258]. In this process, glycolytic intermediates DHAP and G3P undergo nonenzymatic degradation and form the dicarbonyl MG (Figure 5) [259]. The reactive dicarbonyls, MG, GO, and 3-deoxyglucosone (3-DG), can then form AGEs by nonenzymatically reacting with the free amino group on lysine and arginine residues [257,260,261,262].
AGEs are classified into three groups with unique characteristics: (1) fluorescent crosslinking AGEs, (2) non-fluorescent crosslinking AGEs, and (3) non-crosslinking AGEs (Figure 5) [260]. Crosslinking AGEs result in the linkage of two proteins through the binding of the AGE to lysine or arginine residues on the proteins [240,263,264]. Non-crosslinking AGEs are AGEs that bind to lysine or arginine residues and create protein adducts. Crosslinking AGEs have been shown to affect protein structure and function and result in reduced enzymatic activity, protein aggregation, altered biophysical properties, and changes in protein–protein interactions [265,266,267,268]. Non-crosslinking AGEs have been shown to change receptor ligands, block receptors, block protein cleavage sites, cause misfolding of protein, and inhibit protein degradation [240,264,269,270,271].
The involvement of AGEs in diabetes is well-documented due to the increased glucose uptake [259]. In patients with diabetes, the increase in AGEs has been linked to increased inflammation, cardiovascular failure, decreased renal function, and diabetic nephropathy [272,273,274,275,276]. AGEs have also been shown to play a role in many different cancers [277]. The binding of AGEs to the receptor for advanced glycation end products (RAGE) promotes angiogenesis and inflammation, leading to increased proliferation, migration, and invasion in cancers [278]. In viral infections, it has been shown that AGE binding to RAGE is the leading cause of inflammation and pro-inflammatory cytokine production [279,280].
In addition to diabetes and cancer, there is additional evidence that AGEs play a role in Alzheimer’s and other neurogenerative diseases [281,282]. We demonstrated that the HIV protein gp120 augments AGE production through increased glycolysis and ROS. This links increased AGE concentration to neurodegeneration and HIV-associated neurocognitive disease (HAND) [283]. Increased inflammation associated with AGEs acts through RAGE in the hippocampus of Alzheimer’s patients and promotes the pathogenesis of the disease [284,285]. AGEs may also accelerate beta-amyloid aggregate formation in Alzheimer’s patients [286,287]. Therefore, the ability of AGEs to bind to an array of proteins aids in the progression of many diseases and implicates metabolic reprogramming in disease pathogenesis.
19. Conclusions
The hallmarks of metabolic reprogramming represent the cellular processes deregulated in diseases that affect cellular metabolism. These diseases include cancers and viruses that hijack a cell’s energy source and rewire it to produce biomass needed for proliferation and virion production. However, with more research conducted, more metabolic reprogramming hallmarks could be identified.
Many of the hallmarks of metabolic reprogramming outlined here represent ways in which a cell may feed metabolites back into the TCA cycle. As glycolysis is continuing to be promoted and yet the conversion of pyruvate to acetyl-CoA is not occurring, the use of the TCA cycle for energy slows down. However, the TCA cycle is critical for producing metabolites used in the production of biomass. Therefore, viruses may target any number of enzymes or shuttles at any step along the way to ensure the cell is only working to produce more virions. Over time, as viruses continued to benefit from the non-metabolic effects of metabolic reprogramming, they evolved to generate an environment conducive to the replication of virions and immune evasion. Comprehension of the mechanisms behind metabolic reprogramming and how this phenomenon benefits viruses and cancers will help researchers develop better-targeted drugs and therapies.
Author Contributions
C.N.S.A. and S.P.A. wrote and formatted the paper. S.P.A. designed the figures, while M.S. and B.E.S. edited the paper. All authors have read and agreed to the published version of the manuscript.
Funding
The research was funded by the National Institute of Health–National Institute on Aging (NIH-NIA # AG054411) and previous NIH grants (NS076402 and MH093331) awarded to B.E.S.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Medina M.Á. Metabolic Reprogramming is a Hallmark of Metabolism Itself. Bioessays. 2020;42:e2000058. doi: 10.1002/bies.202000058. [DOI] [PubMed] [Google Scholar]
- 2.Warburg O., Posener K., Negelein E. Ueber den Stoffwechsel der Tumoren. Biochem. Z. 1924;152:319–344. (In German). Reprinted in English in the book On metabolism of tumors by O. Warburg, Publisher: Constable, London, 1930. [Google Scholar]
- 3.Liberti M.V., Locasale J.W. The Warburg Effect: How Does it Benefit Cancer Cells? Trends Biochem. Sci. 2016;41:211–218. doi: 10.1016/j.tibs.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vander Heiden M.G., Cantley L.C., Thompson C.B. Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaupel P., Schmidberger H., Mayer A. The Warburg effect: Essential part of metabolic reprogramming and central contributor to cancer progression. Int. J. Radiat. Biol. 2019;95:912–919. doi: 10.1080/09553002.2019.1589653. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin C.M., Xu S., Munger J. Stealing the Keys to the Kitchen: Viral Manipulation of the Host Cell Metabolic Network. Trends Microbiol. 2015;23:789–798. doi: 10.1016/j.tim.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Purdy J.G., Luftig M.A. Reprogramming of cellular metabolic pathways by human oncogenic viruses. Curr. Opin. Virol. 2019;39:60–69. doi: 10.1016/j.coviro.2019.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thyrsted J., Holm C.K. Virus-induced metabolic reprogramming and innate sensing hereof by the infected host. Curr. Opin. Biotechnol. 2021;68:44–50. doi: 10.1016/j.copbio.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Polcicova K., Badurova L., Tomaskova J. Metabolic reprogramming as a feast for virus replication. Acta Virol. 2020;64:201–215. doi: 10.4149/av_2020_210. [DOI] [PubMed] [Google Scholar]
- 10.Schiliro C., Firestein B.L. Mechanisms of Metabolic Reprogramming in Cancer Cells Supporting Enhanced Growth and Proliferation. Cells. 2021;10:1056. doi: 10.3390/cells10051056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaupel P., Multhoff G. Revisiting the Warburg effect: Historical dogma versus current understanding. J. Physiol. 2021;599:1745–1757. doi: 10.1113/JP278810. [DOI] [PubMed] [Google Scholar]
- 12.Li X.B., Gu J.D., Zhou Q.H. Review of aerobic glycolysis and its key enzymes-new targets for lung cancer therapy. Thorac. Cancer. 2015;6:17–24. doi: 10.1111/1759-7714.12148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams N.C., O’Neill L.A.J. A Role for the Krebs Cycle Intermediate Citrate in Metabolic Reprogramming in Innate Immunity and Inflammation. Front. Immunol. 2018;9:141. doi: 10.3389/fimmu.2018.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryan D.G., O’Neill L.A.J. Krebs cycle rewired for macrophage and dendritic cell effector functions. FEBS Lett. 2017;591:2992–3006. doi: 10.1002/1873-3468.12744. [DOI] [PubMed] [Google Scholar]
- 15.DeBerardinis R.J., Lum J.J., Hatzivassiliou G., Thompson C.B. The biology of cancer: Metabolic reprogramming fuels cell growth and proliferation. Cell Metab. 2008;7:11–20. doi: 10.1016/j.cmet.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Feng J., Li J., Wu L., Yu Q., Ji J., Wu J., Dai W., Guo C. Emerging roles and the regulation of aerobic glycolysis in hepatocellular carcinoma. J. Exp. Clin. Cancer Res. 2020;39:126. doi: 10.1186/s13046-020-01629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marelli-Berg F.M., Fu H., Mauro C. Molecular mechanisms of metabolic reprogramming in proliferating cells: Implications for T-cell-mediated immunity. Immunology. 2012;136:363–369. doi: 10.1111/j.1365-2567.2012.03583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jassim A.H., Coughlin L., Harun-Or-Rashid M., Kang P.T., Chen Y.R., Inman D.M. Higher Reliance on Glycolysis Limits Glycolytic Responsiveness in Degenerating Glaucomatous Optic Nerve. Mol. Neurobiol. 2019;56:7097–7112. doi: 10.1007/s12035-019-1576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsu P.P., Sabatini D.M. Cancer cell metabolism: Warburg and beyond. Cell. 2008;134:703–707. doi: 10.1016/j.cell.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 20.Reckzeh E.S., Karageorgis G., Schwalfenberg M., Ceballos J., Nowacki J., Stroet M.C.M., Binici A., Knauer L., Brand S., Choidas A., et al. Inhibition of Glucose Transporters and Glutaminase Synergistically Impairs Tumor Cell Growth. Cell Chem. Biol. 2019;26:1214–1228.e25. doi: 10.1016/j.chembiol.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 21.Faas M., Ipseiz N., Ackermann J., Culemann S., Grüneboom A., Schröder F., Rothe T., Scholtysek C., Eberhardt M., Böttcher M., et al. IL-33-induced metabolic reprogramming controls the differentiation of alternatively activated macrophages and the resolution of inflammation. Immunity. 2021;54:2531–2546.e5. doi: 10.1016/j.immuni.2021.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen A.N., Luo Y., Yang Y.H., Fu J.T., Geng X.M., Shi J.P., Yang J. Lactylation, a Novel Metabolic Reprogramming Code: Current Status and Prospects. Front. Immunol. 2021;12:688910. doi: 10.3389/fimmu.2021.688910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martínez-Ordoñez A., Seoane S., Avila L., Eiro N., Macía M., Arias E., Pereira F., García-Caballero T., Gómez-Lado N., Aguiar P., et al. POU1F1 transcription factor induces metabolic reprogramming and breast cancer progression via LDHA regulation. Oncogene. 2021;40:2725–2740. doi: 10.1038/s41388-021-01740-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phypers B., Pierce T. Lactate physiology in health and disease. Contin. Educ. Anaesth. Crit. Care Pain. 2006;6:128–132. doi: 10.1093/bjaceaccp/mkl018. [DOI] [Google Scholar]
- 25.Ge T., Yang J., Zhou S., Wang Y., Li Y., Tong X. The Role of the Pentose Phosphate Pathway in Diabetes and Cancer. Front. Endocrinol. 2020;11:365. doi: 10.3389/fendo.2020.00365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Vitto H., Arachchige D.B., Richardson B.C., French J.B. The Intersection of Purine and Mitochondrial Metabolism in Cancer. Cells. 2021;10:2603. doi: 10.3390/cells10102603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hay N. Reprogramming glucose metabolism in cancer: Can it be exploited for cancer therapy? Nat. Rev. Cancer. 2016;16:635–649. doi: 10.1038/nrc.2016.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shaw R.J. Glucose metabolism and cancer. Curr. Opin. Cell Biol. 2006;18:598–608. doi: 10.1016/j.ceb.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Riganti C., Gazzano E., Polimeni M., Aldieri E., Ghigo D. The pentose phosphate pathway: An antioxidant defense and a crossroad in tumor cell fate. Free Radic. Biol. Med. 2012;53:421–436. doi: 10.1016/j.freeradbiomed.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 30.Patra K.C., Hay N. The pentose phosphate pathway and cancer. Trends Biochem. Sci. 2014;39:347–354. doi: 10.1016/j.tibs.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moreno-Sánchez R., Gallardo-Pérez J.C., Rodríguez-Enríquez S., Saavedra E., Marín-Hernández Á. Control of the NADPH supply for oxidative stress handling in cancer cells. Free Radic. Biol. Med. 2017;112:149–161. doi: 10.1016/j.freeradbiomed.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 32.Hong S., Chen T., Liu L., Cao C., Lv F., Rabinowitz J.D., Huang Y., Chen X. Live-cell imaging of NADPH production from specific pathways. CCS Chem. 2020;3:1642–1648. doi: 10.31635/ccschem.020.202000346. [DOI] [Google Scholar]
- 33.Polat I.H., Tarrado-Castellarnau M., Benito A., Hernandez-Carro C., Centelles J., Marin S., Cascante M. Glutamine Modulates Expression and Function of Glucose 6-Phosphate Dehydrogenase via NRF2 in Colon Cancer Cells. Antioxidants. 2021;10:1349. doi: 10.3390/antiox10091349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vizán P., Alcarraz-Vizán G., Díaz-Moralli S., Solovjeva O.N., Frederiks W.M., Cascante M. Modulation of pentose phosphate pathway during cell cycle progression in human colon adenocarcinoma cell line HT29. Int. J. Cancer. 2009;124:2789–2796. doi: 10.1002/ijc.24262. [DOI] [PubMed] [Google Scholar]
- 35.Jiang P., Du W., Wang X., Mancuso A., Gao X., Wu M., Yang X. p53 regulates biosynthesis through direct inactivation of glucose-6-phosphate dehydrogenase. Nat. Cell Biol. 2011;13:310–316. doi: 10.1038/ncb2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gao L., Mejías R., Echevarría M., López-Barneo J. Induction of the glucose-6-phosphate dehydrogenase gene expression by chronic hypoxia in PC12 cells. FEBS Lett. 2004;569:256–260. doi: 10.1016/j.febslet.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Bayar İ., Bildik A. Investigation of glucose catabolism in hypoxic Mcf 7 breast cancer culture. Cytotechnology. 2021;73:217–232. doi: 10.1007/s10616-021-00459-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corcoran S.E., O’Neill L.A. HIF1α and metabolic reprogramming in inflammation. J. Clin. Investig. 2016;126:3699–3707. doi: 10.1172/JCI84431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang L., Venneti S., Nagrath D. Glutaminolysis: A Hallmark of Cancer Metabolism. Annu. Rev. Biomed. Eng. 2017;19:163–194. doi: 10.1146/annurev-bioeng-071516-044546. [DOI] [PubMed] [Google Scholar]
- 40.Mayers J.R., Vander Heiden M.G. Famine versus feast: Understanding the metabolism of tumors in vivo. Trends Biochem. Sci. 2015;40:130–140. doi: 10.1016/j.tibs.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gaglio D., Metallo C.M., Gameiro P.A., Hiller K., Danna L.S., Balestrieri C., Alberghina L., Stephanopoulos G., Chiaradonna F. Oncogenic K-Ras decouples glucose and glutamine metabolism to support cancer cell growth. Mol. Syst. Biol. 2011;7:523. doi: 10.1038/msb.2011.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeBerardinis R.J., Cheng T. Q’s next: The diverse functions of glutamine in metabolism, cell biology and cancer. Oncogene. 2010;29:313–324. doi: 10.1038/onc.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoo H.C., Yu Y.C., Sung Y., Han J.M. Glutamine reliance in cell metabolism. Exp. Mol. Med. 2020;52:1496–1516. doi: 10.1038/s12276-020-00504-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DeBerardinis R.J., Mancuso A., Daikhin E., Nissim I., Yudkoff M., Wehrli S., Thompson C.B. Beyond aerobic glycolysis: Transformed cells can engage in glutamine metabolism that exceeds the requirement for protein and nucleotide synthesis. Proc. Natl. Acad. Sci. USA. 2007;104:19345–19350. doi: 10.1073/pnas.0709747104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bott A.J., Peng I.C., Fan Y., Faubert B., Zhao L., Li J., Neidler S., Sun Y., Jaber N., Krokowski D., et al. Oncogenic Myc Induces Expression of Glutamine Synthetase through Promoter Demethylation. Cell Metab. 2015;22:1068–1077. doi: 10.1016/j.cmet.2015.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nicklin P., Bergman P., Zhang B., Triantafellow E., Wang H., Nyfeler B., Yang H., Hild M., Kung C., Wilson C., et al. Bidirectional transport of amino acids regulates mTOR and autophagy. Cell. 2009;136:521–534. doi: 10.1016/j.cell.2008.11.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gao P., Tchernyshyov I., Chang T.C., Lee Y.S., Kita K., Ochi T., Zeller K.I., De Marzo A.M., Van Eyk J.E., Mendell J.T., et al. c-Myc suppression of miR-23a/b enhances mitochondrial glutaminase expression and glutamine metabolism. Nature. 2009;458:762–765. doi: 10.1038/nature07823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wallace D.C. Mitochondria and cancer. Nat. Rev. Cancer. 2012;12:685–698. doi: 10.1038/nrc3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ryan D.G., Yang M., Prag H.A., Blanco G.R., Nikitopoulou E., Segarra-Mondejar M., Powell C.A., Young T., Burger N., Miljkovic J.L., et al. Disruption of the TCA cycle reveals an ATF4-dependent integration of redox and amino acid metabolism. Elife. 2021;10:e72593. doi: 10.7554/eLife.72593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Todisco S., Convertini P., Iacobazzi V., Infantino V. TCA Cycle Rewiring as Emerging Metabolic Signature of Hepatocellular Carcinoma. Cancers. 2019;12:68. doi: 10.3390/cancers12010068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tan A.S., Baty J.W., Dong L.F., Bezawork-Geleta A., Endaya B., Goodwin J., Bajzikova M., Kovarova J., Peterka M., Yan B., et al. Mitochondrial genome acquisition restores respiratory function and tumorigenic potential of cancer cells without mitochondrial DNA. Cell Metab. 2015;21:81–94. doi: 10.1016/j.cmet.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 52.Petillo A., Abruzzese V., Koshal P., Ostuni A., Bisaccia F. Extracellular Citrate Is a Trojan Horse for Cancer Cells. Front. Mol. Biosci. 2020;7:593866. doi: 10.3389/fmolb.2020.593866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Menendez J.A., Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat. Rev. Cancer. 2007;7:763–777. doi: 10.1038/nrc2222. [DOI] [PubMed] [Google Scholar]
- 54.Liu D., Zhang T., Chen X., Zhang B., Wang Y., Xie M., Ji X., Sun M., Huang W., Xia L. ONECUT2 facilitates hepatocellular carcinoma metastasis by transcriptionally upregulating FGF2 and ACLY. Cell Death Dis. 2021;12:1113. doi: 10.1038/s41419-021-04410-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Palmieri F. The mitochondrial transporter family (SLC25): Physiological and pathological implications. Pflug. Arch. 2004;447:689–709. doi: 10.1007/s00424-003-1099-7. [DOI] [PubMed] [Google Scholar]
- 56.Broeks M.H., van Karnebeek C.D.M., Wanders R.J.A., Jans J.J.M., Verhoeven-Duif N.M. Inborn disorders of the malate aspartate shuttle. J. Inherit. Metab. Dis. 2021;44:792–808. doi: 10.1002/jimd.12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alkan H.F., Bogner-Strauss J.G. Maintaining cytosolic aspartate levels is a major function of the TCA cycle in proliferating cells. Mol. Cell Oncol. 2019;6:e1536843. doi: 10.1080/23723556.2018.1536843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Birsoy K., Wang T., Chen W.W., Freinkman E., Abu-Remaileh M., Sabatini D.M. An Essential Role of the Mitochondrial Electron Transport Chain in Cell Proliferation Is to Enable Aspartate Synthesis. Cell. 2015;162:540–551. doi: 10.1016/j.cell.2015.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sullivan L.B., Luengo A., Danai L.V., Bush L.N., Diehl F.F., Hosios A.M., Lau A.N., Elmiligy S., Malstrom S., Lewis C.A., et al. Aspartate is an endogenous metabolic limitation for tumour growth. Nat. Cell Biol. 2018;20:782–788. doi: 10.1038/s41556-018-0125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tannahill G.M., Curtis A.M., Adamik J., Palsson-McDermott E.M., McGettrick A.F., Goel G., Frezza C., Bernard N.J., Kelly B., Foley N.H., et al. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Nature. 2013;496:238–242. doi: 10.1038/nature11986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Robinson A.J., Overy C., Kunji E.R. The mechanism of transport by mitochondrial carriers based on analysis of symmetry. Proc. Natl. Acad. Sci. USA. 2008;105:17766–17771. doi: 10.1073/pnas.0809580105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhunussova A., Sen B., Friedman L., Tuleukhanov S., Brooks A.D., Sensenig R., Orynbayeva Z. Tumor microenvironment promotes dicarboxylic acid carrier-mediated transport of succinate to fuel prostate cancer mitochondria. Am. J. Cancer Res. 2015;5:1665–1679. [PMC free article] [PubMed] [Google Scholar]
- 63.Lukyanova L.D., Kirova Y.I., Germanova E.L. The Role of Succinate in Regulation of Immediate HIF-1α Expression in Hypoxia. Bull. Exp. Biol. Med. 2018;164:298–303. doi: 10.1007/s10517-018-3976-2. [DOI] [PubMed] [Google Scholar]
- 64.Johnson R.F., Perkins N.D. Nuclear factor-κB, p53, and mitochondria: Regulation of cellular metabolism and the Warburg effect. Trends Biochem. Sci. 2012;37:317–324. doi: 10.1016/j.tibs.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 65.Londhe P., Yu P.Y., Ijiri Y., Ladner K.J., Fenger J.M., London C., Houghton P.J., Guttridge D.C. Classical NF-κB Metabolically Reprograms Sarcoma Cells Through Regulation of Hexokinase 2. Front. Oncol. 2018;8:104. doi: 10.3389/fonc.2018.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kawauchi K., Araki K., Tobiume K., Tanaka N. p53 regulates glucose metabolism through an IKK-NF-kappaB pathway and inhibits cell transformation. Nat. Cell Biol. 2008;10:611–618. doi: 10.1038/ncb1724. [DOI] [PubMed] [Google Scholar]
- 67.Zhou F., Xu X., Wu J., Wang D., Wang J. NF-κB controls four genes encoding core enzymes of tricarboxylic acid cycle. Gene. 2017;621:12–20. doi: 10.1016/j.gene.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 68.Gordan J.D., Simon M.C. Hypoxia-inducible factors: Central regulators of the tumor phenotype. Curr. Opin. Genet. Dev. 2007;17:71–77. doi: 10.1016/j.gde.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dong S., Liang S., Cheng Z., Zhang X., Luo L., Li L., Zhang W., Li S., Xu Q., Zhong M., et al. ROS/PI3K/Akt and Wnt/β-catenin signalings activate HIF-1α-induced metabolic reprogramming to impart 5-fluorouracil resistance in colorectal cancer. J. Exp. Clin. Cancer Res. 2022;41:15. doi: 10.1186/s13046-021-02229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kim J.W., Tchernyshyov I., Semenza G.L., Dang C.V. HIF-1-mediated expression of pyruvate dehydrogenase kinase: A metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 2006;3:177–185. doi: 10.1016/j.cmet.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 71.Cui X.G., Han Z.T., He S.H., Wu X.D., Chen T.R., Shao C.H., Chen D.L., Su N., Chen Y.M., Wang T., et al. HIF1/2α mediates hypoxia-induced LDHA expression in human pancreatic cancer cells. Oncotarget. 2017;8:24840–24852. doi: 10.18632/oncotarget.15266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McFate T., Mohyeldin A., Lu H., Thakar J., Henriques J., Halim N.D., Wu H., Schell M.J., Tsang T.M., Teahan O., et al. Pyruvate dehydrogenase complex activity controls metabolic and malignant phenotype in cancer cells. J. Biol. Chem. 2008;283:22700–22708. doi: 10.1074/jbc.M801765200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jin L., Cho M., Kim B.S., Han J.H., Park S., Lee I.K., Ryu D., Kim J.H., Bae S.J., Ha K.T. Drug evaluation based on phosphomimetic PDHA1 reveals the complexity of activity-related cell death in A549 non-small cell lung cancer cells. BMB Rep. 2021;54:563–568. doi: 10.5483/BMBRep.2021.54.11.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Heaton N.S., Randall G. Multifaceted roles for lipids in viral infection. Trends MicroBiol. 2011;19:368–375. doi: 10.1016/j.tim.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Snaebjornsson M.T., Janaki-Raman S., Schulze A. Greasing the Wheels of the Cancer Machine: The Role of Lipid Metabolism in Cancer. Cell Metab. 2020;31:62–76. doi: 10.1016/j.cmet.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 76.Mashima T., Seimiya H., Tsuruo T. De novo fatty-acid synthesis and related pathways as molecular targets for cancer therapy. Br. J. Cancer. 2009;100:1369–1372. doi: 10.1038/sj.bjc.6605007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Karagiota A., Chachami G., Paraskeva E. Lipid Metabolism in Cancer: The Role of Acylglycerolphosphate Acyltransferases (AGPATs) Cancers. 2022;14:228. doi: 10.3390/cancers14010228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Santos C.R., Schulze A. Lipid metabolism in cancer. FEBS J. 2012;279:2610–2623. doi: 10.1111/j.1742-4658.2012.08644.x. [DOI] [PubMed] [Google Scholar]
- 79.Giacomini I., Gianfanti F., Desbats M.A., Orso G., Berretta M., Prayer-Galetti T., Ragazzi E., Cocetta V. Cholesterol Metabolic Reprogramming in Cancer and Its Pharmacological Modulation as Therapeutic Strategy. Front. Oncol. 2021;11:682911. doi: 10.3389/fonc.2021.682911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ačimovič J., Goyal S., Košir R., Goličnik M., Perše M., Belič A., Urlep Ž., Guengerich F.P., Rozman D. Cytochrome P450 metabolism of the post-lanosterol intermediates explains enigmas of cholesterol synthesis. Sci. Rep. 2016;6:28462. doi: 10.1038/srep28462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Luo J., Yang H., Song B.L. Mechanisms and regulation of cholesterol homeostasis. Nat. Rev. Mol. Cell Biol. 2020;21:225–245. doi: 10.1038/s41580-019-0190-7. [DOI] [PubMed] [Google Scholar]
- 82.Vona R., Iessi E., Matarrese P. Role of Cholesterol and Lipid Rafts in Cancer Signaling: A Promising Therapeutic Opportunity? Front. Cell Dev. Biol. 2021;9:622908. doi: 10.3389/fcell.2021.622908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hu T., Shen H., Huang H., Yang Z., Zhou Y., Zhao G. Cholesterol-lowering drug pitavastatin targets lung cancer and angiogenesis via suppressing prenylation-dependent Ras/Raf/MEK and PI3K/Akt/mTOR signaling. Anticancer Drugs. 2020;31:377–384. doi: 10.1097/CAD.0000000000000885. [DOI] [PubMed] [Google Scholar]
- 84.Konstantinopoulos P.A., Karamouzis M.V., Papavassiliou A.G. Post-translational modifications and regulation of the RAS superfamily of GTPases as anticancer targets. Nat. Rev. Drug Discov. 2007;6:541–555. doi: 10.1038/nrd2221. [DOI] [PubMed] [Google Scholar]
- 85.Horton J.D. Sterol regulatory element-binding proteins: Transcriptional activators of lipid synthesis. Biochem. Soc. Trans. 2002;30:1091–1095. doi: 10.1042/bst0301091. [DOI] [PubMed] [Google Scholar]
- 86.Xue L., Qi H., Zhang H., Ding L., Huang Q., Zhao D., Wu B.J., Li X. Targeting SREBP-2-Regulated Mevalonate Metabolism for Cancer Therapy. Front. Oncol. 2020;10:1510. doi: 10.3389/fonc.2020.01510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hardie D.G. AMP-activated/SNF1 protein kinases: Conserved guardians of cellular energy. Nat. Rev. Mol. Cell Biol. 2007;8:774–785. doi: 10.1038/nrm2249. [DOI] [PubMed] [Google Scholar]
- 88.Zhao Y., Hu X., Liu Y., Dong S., Wen Z., He W., Zhang S., Huang Q., Shi M. ROS signaling under metabolic stress: Cross-talk between AMPK and AKT pathway. Mol. Cancer. 2017;16:79. doi: 10.1186/s12943-017-0648-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lieu E.L., Nguyen T., Rhyne S., Kim J. Amino acids in cancer. Exp. Mol. Med. 2020;52:15–30. doi: 10.1038/s12276-020-0375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Keenan M.M., Chi J.T. Alternative fuels for cancer cells. Cancer J. 2015;21:49–55. doi: 10.1097/PPO.0000000000000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mayers J.R., Wu C., Clish C.B., Kraft P., Torrence M.E., Fiske B.P., Yuan C., Bao Y., Townsend M.K., Tworoger S.S., et al. Elevation of circulating branched-chain amino acids is an early event in human pancreatic adenocarcinoma development. Nat. Med. 2014;20:1193–1198. doi: 10.1038/nm.3686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sheen J.H., Zoncu R., Kim D., Sabatini D.M. Defective regulation of autophagy upon leucine deprivation reveals a targetable liability of human melanoma cells in vitro and in vivo. Cancer Cell. 2011;19:613–628. doi: 10.1016/j.ccr.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tian S., Feng J., Cao Y., Shen S., Cai Y., Yang D., Yan R., Wang L., Zhang H., Zhong X., et al. Glycine cleavage system determines the fate of pluripotent stem cells via the regulation of senescence and epigenetic modifications. Life Sci. Alliance. 2019;2:e201900413. doi: 10.26508/lsa.201900413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang J., Alexander P., Wu L., Hammer R., Cleaver O., McKnight S.L. Dependence of mouse embryonic stem cells on threonine catabolism. Science. 2009;325:435–439. doi: 10.1126/science.1173288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chiu M., Taurino G., Bianchi M.G., Kilberg M.S., Bussolati O. Asparagine Synthetase in Cancer: Beyond Acute Lymphoblastic Leukemia. Front. Oncol. 2020;9:1480. doi: 10.3389/fonc.2019.01480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Curthoys N.P., Watford M. Regulation of glutaminase activity and glutamine metabolism. Annu. Rev. Nutr. 1995;15:133–159. doi: 10.1146/annurev.nu.15.070195.001025. [DOI] [PubMed] [Google Scholar]
- 97.Burke L., Guterman I., Palacios Gallego R., Britton R.G., Burschowsky D., Tufarelli C., Rufini A. The Janus-like role of proline metabolism in cancer. Cell Death Discov. 2020;6:104. doi: 10.1038/s41420-020-00341-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ducker G.S., Rabinowitz J.D. One-Carbon Metabolism in Health and Disease. Cell Metab. 2017;25:27–42. doi: 10.1016/j.cmet.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wang Y., Bai C., Ruan Y., Liu M., Chu Q., Qiu L., Yang C., Li B. Coordinative metabolism of glutamine carbon and nitrogen in proliferating cancer cells under hypoxia. Nat. Commun. 2019;10:201. doi: 10.1038/s41467-018-08033-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yamamoto N., Sampei G., Kawai G. Free-Energy Profile Analysis of the Catalytic Reaction of Glycinamide Ribonucleotide Synthetase. Life. 2022;12:281. doi: 10.3390/life12020281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhang Y., Morar M., Ealick S.E. Structural biology of the purine biosynthetic pathway. Cell Mol. Life Sci. 2008;65:3699–3724. doi: 10.1007/s00018-008-8295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Navas L.E., Carnero A. NAD+ metabolism, stemness, the immune response, and cancer. Signal Transduct. Target. Ther. 2021;6:2. doi: 10.1038/s41392-020-00354-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Stein L.R., Imai S. The dynamic regulation of NAD metabolism in mitochondria. Trends Endocrinol. Metab. 2012;23:420–428. doi: 10.1016/j.tem.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Carracedo A., Cantley L.C., Pandolfi P.P. Cancer metabolism: Fatty acid oxidation in the limelight. Nat. Rev. Cancer. 2013;13:227–232. doi: 10.1038/nrc3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Singh R., Cuervo A.M. Lipophagy: Connecting autophagy and lipid metabolism. Int. J. Cell Biol. 2012;2012:282041. doi: 10.1155/2012/282041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lim S.C., Tajika M., Shimura M., Carey K.T., Stroud D.A., Murayama K., Ohtake A., McKenzie M. Loss of the Mitochondrial Fatty Acid β-Oxidation Protein Medium-Chain Acyl-Coenzyme A Dehydrogenase Disrupts Oxidative Phosphorylation Protein Complex Stability and Function. Sci. Rep. 2018;8:153. doi: 10.1038/s41598-017-18530-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dalla Pozza E., Dando I., Pacchiana R., Liboi E., Scupoli M.T., Donadelli M., Palmieri M. Regulation of succinate dehydrogenase and role of succinate in cancer. Semin. Cell Dev. Biol. 2020;98:4–14. doi: 10.1016/j.semcdb.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 108.Liu Y. Fatty acid oxidation is a dominant bioenergetic pathway in prostate cancer. Prostate Cancer Prostatic Dis. 2006;9:230–234. doi: 10.1038/sj.pcan.4500879. [DOI] [PubMed] [Google Scholar]
- 109.Schönfeld P., Wieckowski M.R., Lebiedzińska M., Wojtczak L. Mitochondrial fatty acid oxidation and oxidative stress: Lack of reverse electron transfer-associated production of reactive oxygen species. Biochim. Biophys. Acta. 2010;1797:929–938. doi: 10.1016/j.bbabio.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 110.Umemoto T., Johansson A., Ahmad S.A.I., Hashimoto M., Kubota S., Kikuchi K., Odaka H., Era T., Kurotaki D., Sashida G., et al. ATP citrate lyase controls hematopoietic stem cell fate and supports bone marrow regeneration. EMBO J. 2022:e109463. doi: 10.15252/embj.2021109463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Oeggl R., Neumann T., Gätgens J., Romano D., Noack S., Rother D. Citrate as Cost-Efficient NADPH Regenerating Agent. Front. Bioeng. Biotechnol. 2018;6:196. doi: 10.3389/fbioe.2018.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chiarugi A., Dölle C., Felici R., Ziegler M. The NAD metabolome--a key determinant of cancer cell biology. Nat. Rev. Cancer. 2012;12:741–752. doi: 10.1038/nrc3340. [DOI] [PubMed] [Google Scholar]
- 113.Jeon S.M., Chandel N.S., Hay N. AMPK regulates NADPH homeostasis to promote tumour cell survival during energy stress. Nature. 2012;485:661–665. doi: 10.1038/nature11066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Luo L., Qin B., Jiang M., Xie L., Luo Z., Guo X., Zhang J., Li X., Zhu C., Du Y., et al. Regulating immune memory and reversing tumor thermotolerance through a step-by-step starving-photothermal therapy. J. Nanobiotechnol. 2021;19:297. doi: 10.1186/s12951-021-01011-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lyssiotis C.A., Cantley L.C. Acetate fuels the cancer engine. Cell. 2014;159:1492–1494. doi: 10.1016/j.cell.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 116.Bae J.M., Kim J.H., Oh H.J., Park H.E., Lee T.H., Cho N.Y., Kang G.H. Downregulation of acetyl-CoA synthetase 2 is a metabolic hallmark of tumor progression and aggressiveness in colorectal carcinoma. Mod. Pathol. 2017;30:267–277. doi: 10.1038/modpathol.2016.172. [DOI] [PubMed] [Google Scholar]
- 117.Schug Z.T., Voorde J.V., Gottlieb E. The metabolic fate of acetate in cancer. Nat. Rev. Cancer. 2016;16:708–717. doi: 10.1038/nrc.2016.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lakhter A.J., Hamilton J., Konger R.L., Brustovetsky N., Broxmeyer H.E., Naidu S.R. Glucose-independent Acetate Metabolism Promotes Melanoma Cell Survival and Tumor Growth. J. Biol. Chem. 2016;291:21869–21879. doi: 10.1074/jbc.M115.712166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sanchez E.L., Lagunoff M. Viral activation of cellular metabolism. Virology. 2015;479–480:609–618. doi: 10.1016/j.virol.2015.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Thaker S.K., Ch’ng J., Christofk H.R. Viral hijacking of cellular metabolism. BMC Biol. 2019;17:59. doi: 10.1186/s12915-019-0678-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Harrison M.A.A., Hochreiner E.M., Benjamin B.P., Lawler S.E., Zwezdaryk K.J. Metabolic Reprogramming of Glioblastoma Cells during HCMV Infection Induces Secretome-Mediated Paracrine Effects in the Microenvironment. Viruses. 2022;14:103. doi: 10.3390/v14010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Munger J., Bajad S.U., Coller H.A., Shenk T., Rabinowitz J.D. Dynamics of the cellular metabolome during human cytomegalovirus infection. PLoS Pathog. 2006;2:e132. doi: 10.1371/journal.ppat.0020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Munger J., Bennett B.D., Parikh A., Feng X.J., McArdle J., Rabitz H.A., Shenk T., Rabinowitz J.D. Systems-level metabolic flux profiling identifies fatty acid synthesis as a target for antiviral therapy. Nat. Biotechnol. 2008;26:1179–1186. doi: 10.1038/nbt.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Thai M., Graham N.A., Braas D., Nehil M., Komisopoulou E., Kurdistani S.K., McCormick F., Graeber T.G., Christofk H.R. Adenovirus E4ORF1-induced MYC activation promotes host cell anabolic glucose metabolism and virus replication. Cell Metab. 2014;19:694–701. doi: 10.1016/j.cmet.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ripoli M., D’Aprile A., Quarato G., Sarasin-Filipowicz M., Gouttenoire J., Scrima R., Cela O., Boffoli D., Heim M.H., Moradpour D., et al. Hepatitis C virus-linked mitochondrial dysfunction promotes hypoxia-inducible factor 1 alpha-mediated glycolytic adaptation. J. Virol. 2010;84:647–660. doi: 10.1128/JVI.00769-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Diamond D.L., Syder A.J., Jacobs J.M., Sorensen C.M., Walters K.A., Proll S.C., McDermott J.E., Gritsenko M.A., Zhang Q., Zhao R., et al. Temporal proteome and lipidome profiles reveal hepatitis C virus-associated reprogramming of hepatocellular metabolism and bioenergetics. PLoS Pathog. 2010;6:e1000719. doi: 10.1371/journal.ppat.1000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chan E.Y., Sutton J.N., Jacobs J.M., Bondarenko A., Smith R.D., Katze M.G. Dynamic host energetics and cytoskeletal proteomes in human immunodeficiency virus type 1-infected human primary CD4 cells: Analysis by multiplexed label-free mass spectrometry. J. Virol. 2009;83:9283–9295. doi: 10.1128/JVI.00814-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hallenberger S., Bosch V., Angliker H., Shaw E., Klenk H.D., Garten W. Inhibition of furin-mediated cleavage activation of HIV-1 glycoprotein gp160. Nature. 1992;360:358–361. doi: 10.1038/360358a0. [DOI] [PubMed] [Google Scholar]
- 129.Ritter J.B., Wahl A.S., Freund S., Genzel Y., Reichl U. Metabolic effects of influenza virus infection in cultured animal cells: Intra- and extracellular metabolite profiling. BMC Syst. Biol. 2010;4:61. doi: 10.1186/1752-0509-4-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fontaine K.A., Sanchez E.L., Camarda R., Lagunoff M. Dengue virus induces and requires glycolysis for optimal replication. J. Virol. 2015;9:2358–2366. doi: 10.1128/JVI.02309-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zou Z., Tsang J.O., Yan B., Chik K.K., Chan C.C., Cao J., Liang R., Tang K., Yin F., Ye Z.W., et al. Metabolic Profiling Reveals Significant Perturbations of Intracellular Glucose Homeostasis in Enterovirus-Infected Cells. Metabolites. 2020;10:302. doi: 10.3390/metabo10080302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Delgado T., Sanchez E.L., Camarda R., Lagunoff M. Global metabolic profiling of infection by an oncogenic virus: KSHV induces and requires lipogenesis for survival of latent infection. PLoS Pathog. 2012;8:e1002866. doi: 10.1371/journal.ppat.1002866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Delgado T., Carroll P.A., Punjabi A.S., Margineantu D., Hockenbery D.M., Lagunoff M. Induction of the Warburg effect by Kaposi’s sarcoma herpesvirus is required for the maintenance of latently infected endothelial cells. Proc. Natl. Acad. Sci. USA. 2010;107:10696–10701. doi: 10.1073/pnas.1004882107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Yogev O., Lagos D., Enver T., Boshoff C. Kaposi’s sarcoma herpesvirus microRNAs induce metabolic transformation of infected cells. PLoS Pathog. 2014;10:e1004400. doi: 10.1371/journal.ppat.1004400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hulse M., Caruso L.B., Madzo J., Tan Y., Johnson S., Tempera I. Poly(ADP-ribose) polymerase 1 is necessary for coactivating hypoxia-inducible factor-1-dependent gene expression by Epstein-Barr virus latent membrane protein 1. PLoS Pathog. 2018;14:e1007394. doi: 10.1371/journal.ppat.1007394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Xiao L., Hu Z.Y., Dong X., Tan Z., Li W., Tang M., Chen L., Yang L., Tao Y., Jiang Y., et al. Targeting Epstein-Barr virus oncoprotein LMP1-mediated glycolysis sensitizes nasopharyngeal carcinoma to radiation therapy. Oncogene. 2014;33:4568–4578. doi: 10.1038/onc.2014.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rashida Z., Laxman S. The pentose phosphate pathway and organization of Metabolic Networks Enabling Growth Programs. Curr. Opin. Syst. Biol. 2021;28:100390. doi: 10.1016/j.coisb.2021.100390. [DOI] [Google Scholar]
- 138.Stincone A., Prigione A., Cramer T., Wamelink M.M., Campbell K., Cheung E., Olin-Sandoval V., Grüning N.M., Krüger A., Tauqeer Alam M., et al. The return of metabolism: Biochemistry and physiology of the pentose phosphate pathway. Biol. Rev. Camb. Philos. Soc. 2015;90:927–963. doi: 10.1111/brv.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bojkova D., Klann K., Koch B., Widera M., Krause D., Ciesek S., Cinatl J., Münch C. Proteomics of SARS-CoV-2-infected host cells reveals therapy targets. Nature. 2020;583:469–472. doi: 10.1038/s41586-020-2332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Keshavarz M., Solaymani-Mohammadi F., Namdari H., Arjeini Y., Mousavi M.J., Rezaei F. Metabolic host response and therapeutic approaches to influenza infection. Cell Mol. Biol. Lett. 2020;25:15. doi: 10.1186/s11658-020-00211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Prusinkiewicz M.A., Tu J., Dodge M.J., MacNeil K.M., Radko-Juettner S., Fonseca G.J., Pelka P., Mymryk J.S. Differential Effects of Human Adenovirus E1A Protein Isoforms on Aerobic Glycolysis in A549 Human Lung Epithelial Cells. Viruses. 2020;12:610. doi: 10.3390/v12060610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Sugiyama K., Ebinuma H., Nakamoto N., Sakasegawa N., Murakami Y., Chu P.S., Usui S., Ishibashi Y., Wakayama Y., Taniki N., et al. Prominent steatosis with hypermetabolism of the cell line permissive for years of infection with hepatitis C virus. PLoS ONE. 2014;9:e94460. doi: 10.1371/journal.pone.0094460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Shytaj I.L., Procopio F.A., Tarek M., Carlon-Andres I., Tang H.Y., Goldman A.R., Munshi M., Kumar Pal V., Forcato M., Sreeram S., et al. Glycolysis downregulation is a hallmark of HIV-1 latency and sensitizes infected cells to oxidative stress. EMBO Mol. Med. 2021;13:e13901. doi: 10.15252/emmm.202013901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Chambers J.W., Maguire T.G., Alwine J.C. Glutamine metabolism is essential for human cytomegalovirus infection. J. Virol. 2010;84:1867–1873. doi: 10.1128/JVI.02123-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Vastag L., Koyuncu E., Grady S.L., Shenk T.E., Rabinowitz J.D. Divergent effects of human cytomegalovirus and herpes simplex virus-1 on cellular metabolism. PLoS Pathog. 2011;7:e1002124. doi: 10.1371/journal.ppat.1002124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Thai M., Thaker S.K., Feng J., Du Y., Hu H., Ting Wu T., Graeber T.G., Braas D., Christofk H.R. MYC-induced reprogramming of glutamine catabolism supports optimal virus replication. Nat. Commun. 2015;6:8873. doi: 10.1038/ncomms9873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gualdoni G.A., Mayer K.A., Kapsch A.M., Kreuzberg K., Puck A., Kienzl P., Oberndorfer F., Frühwirth K., Winkler S., Blaas D., et al. Rhinovirus induces an anabolic reprogramming in host cell metabolism essential for viral replication. Proc. Natl. Acad. Sci. USA. 2018;115:E7158–E7165. doi: 10.1073/pnas.1800525115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lévy P.L., Duponchel S., Eischeid H., Molle J., Michelet M., Diserens G., Vermathen M., Vermathen P., Dufour J.F., Dienes H.P., et al. Hepatitis C virus infection triggers a tumor-like glutamine metabolism. Hepatology. 2017;65:789–803. doi: 10.1002/hep.28949. [DOI] [PubMed] [Google Scholar]
- 149.Clerc I., Moussa D.A., Vahlas Z., Tardito S., Oburoglu L., Hope T.J., Sitbon M., Dardalhon V., Mongellaz C., Taylor N. Entry of glucose- and glutamine-derived carbons into the citric acid cycle supports early steps of HIV-1 infection in CD4 T cells. Nat. Metab. 2019;1:717–730. doi: 10.1038/s42255-019-0084-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sánchez-García F.J., Pérez-Hernández C.A., Rodríguez-Murillo M., Moreno-Altamirano M.M.B. The Role of Tricarboxylic Acid Cycle Metabolites in Viral Infections. Front. Cell. Infect. Microbiol. 2021;11:725043. doi: 10.3389/fcimb.2021.725043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Yu Y., Clippinger A.J., Alwine J.C. Viral effects on metabolism: Changes in glucose and glutamine utilization during human cytomegalovirus infection. Trends MicroBiol. 2011;19:360–367. doi: 10.1016/j.tim.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kapadia S.B., Chisari F.V. Hepatitis C virus RNA replication is regulated by host geranylgeranylation and fatty acids. Proc. Natl. Acad. Sci. USA. 2005;102:2561–2566. doi: 10.1073/pnas.0409834102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Vescovo T., Refolo G., Manuelli M.C., Tisone G., Piacentini M., Fimia G.M. The Impact of Mevastatin on HCV Replication and Autophagy of Non-Transformed HCV Replicon Hepatocytes Is Influenced by the Extracellular Lipid Uptake. Front. Pharmacol. 2019;10:718. doi: 10.3389/fphar.2019.00718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Dickens A.M., Anthony D.C., Deutsch R., Mielke M.M., Claridge T.D., Grant I., Franklin D., Rosario D., Marcotte T., Letendre S., et al. Cerebrospinal fluid metabolomics implicate bioenergetic adaptation as a neural mechanism regulating shifts in cognitive states of HIV-infected patients. AIDS. 2015;29:559–569. doi: 10.1097/QAD.0000000000000580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Hileman C.O., Kalayjian R.C., Azzam S., Schlatzer D., Wu K., Tassiopoulos K., Bedimo R., Ellis R.J., Erlandson K.M., Kallianpur A., et al. Plasma Citrate and Succinate Are Associated with Neurocognitive Impairment in Older People With HIV. Clin. Infect. Dis. 2021;73:e765–e772. doi: 10.1093/cid/ciab107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cassol E., Misra V., Dutta A., Morgello S., Gabuzda D. Cerebrospinal fluid metabolomics reveals altered waste clearance and accelerated aging in HIV patients with neurocognitive impairment. AIDS. 2014;28:1579–1591. doi: 10.1097/QAD.0000000000000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lee C.H., Griffiths S., Digard P., Pham N., Auer M., Haas J., Grey F. Asparagine Deprivation Causes a Reversible Inhibition of Human Cytomegalovirus Acute Virus Replication. mBio. 2019;10:e01651-19. doi: 10.1128/mBio.01651-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Pan Y., Wang N., Zhou Z., Liang H., Pan C., Zhu D., Liu F., Zhang C.Y., Zhang Y., Zen K. Circulating human cytomegalovirus-encoded HCMV-miR-US4-1 as an indicator for predicting the efficacy of IFNα treatment in chronic hepatitis B patients. Sci. Rep. 2016;6:23007. doi: 10.1038/srep23007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Brault C., Levy P., Bartosch B. Hepatitis C virus-induced mitochondrial dysfunctions. Viruses. 2013;5:954–980. doi: 10.3390/v5030954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Santerre M., Arjona S.P., Allen C.N., Callen S., Buch S., Sawaya B.E. HIV-1 VPR protein impairs lysosome clearance causing SNCA/alpha-synuclein accumulation in neurons. Autophagy. 2021;17:1768–1782. doi: 10.1080/15548627.2021.1915641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Gibellini L., De Biasi S., Paolini A., Borella R., Boraldi F., Mattioli M., Lo Tartaro D., Fidanza L., Caro-Maldonado A., Meschiari M., et al. Altered bioenergetics and mitochondrial dysfunction of monocytes in patients with Covid-19 pneumonia. EMBO Mol. Med. 2020;12:e13001. doi: 10.15252/emmm.202013001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Cheng M.L., Weng S.F., Kuo C.H., Ho H.Y. Enterovirus 71 induces mitochondrial reactive oxygen species generation that is required for efficient replication. PLoS ONE. 2014;9:e113234. doi: 10.1371/journal.pone.0113234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Foo J., Bellot G., Pervaiz S., Alonso S. Mitochondria-mediated oxidative stress during viral infection. Trends MicroBiol. 2022;S0966-842X:00318-8. doi: 10.1016/j.tim.2021.12.011. [DOI] [PubMed] [Google Scholar]
- 164.Lee H.R., Cho Y.Y., Lee G.Y., You D.G., Yoo Y.D., Kim Y.J. A direct role for hepatitis B virus X protein in inducing mitochondrial membrane permeabilization. J. Viral Hepat. 2018;25:412–420. doi: 10.1111/jvh.12831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Piccoli C., Scrima R., Quarato G., D’Aprile A., Ripoli M., Lecce L., Boffoli D., Moradpour D., Capitanio N. Hepatitis C virus protein expression causes calcium-mediated mitochondrial bioenergetic dysfunction and nitro-oxidative stress. Hepatology. 2007;46:58–65. doi: 10.1002/hep.21679. [DOI] [PubMed] [Google Scholar]
- 166.Couret J., Chang T.L. Reactive Oxygen Species in HIV Infection. EC Microbiol. 2016;3:597–604. [PMC free article] [PubMed] [Google Scholar]
- 167.Mukerjee R., Chang J.R., Del Valle L., Bagashev A., Gayed M.M., Lyde R.B., Hawkins B.J., Brailoiu E., Cohen E., Power C., et al. Deregulation of microRNAs by HIV-1 Vpr protein leads to the development of neurocognitive disorders. J. Biol. Chem. 2011;286:34976–34985. doi: 10.1074/jbc.M111.241547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Spencer C.M., Schafer X.L., Moorman N.J., Munger J. Human cytomegalovirus induces the activity and expression of acetyl-coenzyme A carboxylase, a fatty acid biosynthetic enzyme whose inhibition attenuates viral replication. J. Virol. 2011;85:5814–5824. doi: 10.1128/JVI.02630-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Xi Y., Harwood S., Wise L.M., Purdy J.G. Human Cytomegalovirus pUL37x1 Is Important for Remodeling of Host Lipid Metabolism. J. Virol. 2019;93:e00843-19. doi: 10.1128/JVI.00843-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Mokry R.L., Schumacher M.L., Hogg N., Terhune S.S. Nitric Oxide Circumvents Virus-Mediated Metabolic Regulation during Human Cytomegalovirus Infection. mBio. 2020;11:e02630-20. doi: 10.1128/mBio.02630-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yu Y., Maguire T.G., Alwine J.C. ChREBP, a glucose-responsive transcriptional factor, enhances glucose metabolism to support biosynthesis in human cytomegalovirus-infected cells. Proc. Natl. Acad. Sci. USA. 2014;111:1951–1956. doi: 10.1073/pnas.1310779111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Li Y., Webster-Cyriaque J., Tomlinson C.C., Yohe M., Kenney S. Fatty acid synthase expression is induced by the Epstein-Barr virus immediate-early protein BRLF1 and is required for lytic viral gene expression. J. Virol. 2004;78:4197–4206. doi: 10.1128/JVI.78.8.4197-4206.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lo A.K., Lung R.W., Dawson C.W., Young L.S., Ko C.W., Yeung W.W., Kang W., To K.F., Lo K.W. Activation of sterol regulatory element-binding protein 1 (SREBP1)-mediated lipogenesis by the Epstein-Barr virus-encoded latent membrane protein 1 (LMP1) promotes cell proliferation and progression of nasopharyngeal carcinoma. J. Pathol. 2018;246:180–190. doi: 10.1002/path.5130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Hulse M., Johnson S.M., Boyle S., Caruso L.B., Tempera I. Epstein-Barr Virus-Encoded Latent Membrane Protein 1 and B-Cell Growth Transformation Induce Lipogenesis through Fatty Acid Synthase. J. Virol. 2021;95:e01857-20. doi: 10.1128/JVI.01857-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Namazue J., Kato T., Okuno T., Shiraki K., Yamanishi K. Evidence for attachment of fatty acid to varicella-zoster virus glycoproteins and effect of cerulenin on the maturation of varicella-zoster virus glycoproteins. Intervirology. 1989;30:268–277. doi: 10.1159/000150102. [DOI] [PubMed] [Google Scholar]
- 176.Chukkapalli V., Heaton N.S., Randall G. Lipids at the interface of virus-host interactions. Curr. Opin. MicroBiol. 2012;15:512–518. doi: 10.1016/j.mib.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Zhang Z., He G., Han G.S., Zhang J., Catanzaro N., Diaz A., Wu Z., Carman G.M., Xie L., Wang X. Host Pah1p phosphatidate phosphatase limits viral replication by regulating phospholipid synthesis. PLoS Pathog. 2018;14:e1006988. doi: 10.1371/journal.ppat.1006988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Schaefer E.A., Chung R.T. HCV and host lipids: An intimate connection. Semin. Liver Dis. 2013;33:358–368. doi: 10.1055/s-0033-1358524. [DOI] [PubMed] [Google Scholar]
- 179.Wang X., Xie Q. Metabolic Dysfunction-associated Fatty Liver Disease (MAFLD) and Viral Hepatitis. J. Clin. Transl. Hepatol. 2022;10:128–133. doi: 10.14218/JCTH.2021.00200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yang W., Hood B.L., Chadwick S.L., Liu S., Watkins S.C., Luo G., Conrads T.P., Wang T. Fatty acid synthase is up-regulated during hepatitis C virus infection and regulates hepatitis C virus entry and production. Hepatology. 2008;48:1396–1403. doi: 10.1002/hep.22508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Meng Z., Liu Q., Sun F., Qiao L. Hepatitis C virus nonstructural protein 5A perturbs lipid metabolism by modulating AMPK/SREBP-1c signaling. Lipids Health Dis. 2019;18:191. doi: 10.1186/s12944-019-1136-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Heaton N.S., Perera R., Berger K.L., Khadka S., Lacount D.J., Kuhn R.J., Randall G. Dengue virus nonstructural protein 3 redistributes fatty acid synthase to sites of viral replication and increases cellular fatty acid synthesis. Proc. Natl. Acad. Sci. USA. 2010;107:17345–17350. doi: 10.1073/pnas.1010811107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Tongluan N., Ramphan S., Wintachai P., Jaresitthikunchai J., Khongwichit S., Wikan N., Rajakam S., Yoksan S., Wongsiriroj N., Roytrakul S., et al. Involvement of fatty acid synthase in dengue virus infection. Virol. J. 2017;14:28. doi: 10.1186/s12985-017-0685-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Rasheed S., Yan J.S., Lau A., Chan A.S. HIV replication enhances production of free fatty acids, low density lipoproteins and many key proteins involved in lipid metabolism: A proteomics study. PLoS ONE. 2008;3:e3003. doi: 10.1371/journal.pone.0003003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kulkarni M.M., Ratcliff A.N., Bhat M., Alwarawrah Y., Hughes P., Arcos J., Loiselle D., Torrelles J.B., Funderburg N.T., Haystead T.A., et al. Cellular fatty acid synthase is required for late stages of HIV-1 replication. Retrovirology. 2017;14:45. doi: 10.1186/s12977-017-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Ligat G., Da Re S., Alain S., Hantz S. Identification of Amino Acids Essential for Viral Replication in the HCMV Helicase-Primase Complex. Front. Microbiol. 2018;9:2483. doi: 10.3389/fmicb.2018.02483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Walsh D., Mohr I. Viral subversion of the host protein synthesis machinery. Nat. Rev. MicroBiol. 2011;9:860–875. doi: 10.1038/nrmicro2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Wan L., Juszkiewicz S., Blears D., Bajpe P.K., Han Z., Faull P., Mitter R., Stewart A., Snijders A.P., Hegde R.S., et al. Translation stress and collided ribosomes are co-activators of cGAS. Mol. Cell. 2021;81:2808–2822.e10. doi: 10.1016/j.molcel.2021.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Rodríguez-Sánchez I., Schafer X.L., Monaghan M., Munger J. The Human Cytomegalovirus UL38 protein drives mTOR-independent metabolic flux reprogramming by inhibiting TSC2. PLoS Pathog. 2019;15:e1007569. doi: 10.1371/journal.ppat.1007569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Choi U.Y., Lee J.J., Park A., Zhu W., Lee H.R., Choi Y.J., Yoo J.S., Yu C., Feng P., Gao S.J., et al. Oncogenic human herpesvirus hijacks proline metabolism for tumorigenesis. Proc. Natl. Acad. Sci. USA. 2020;117:8083–8093. doi: 10.1073/pnas.1918607117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Cheng M.L., Chien K.Y., Lai C.H., Li G.J., Lin J.F., Ho H.Y. Metabolic Reprogramming of Host Cells in Response to Enteroviral Infection. Cells. 2020;9:473. doi: 10.3390/cells9020473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Pant A., Cao S., Yang Z. Asparagine Is a Critical Limiting Metabolite for Vaccinia Virus Protein Synthesis during Glutamine Deprivation. J. Virol. 2019;93:e01834-18. doi: 10.1128/JVI.01834-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Grady S.L., Purdy J.G., Rabinowitz J.D., Shenk T. Argininosuccinate synthetase 1 depletion produces a metabolic state conducive to herpes simplex virus 1 infection. Proc. Natl. Acad. Sci. USA. 2013;110:E5006-15. doi: 10.1073/pnas.1321305110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ariav Y., Ch’ng J.H., Christofk H.R., Ron-Harel N., Erez A. Targeting nucleotide metabolism as the nexus of viral infections, cancer, and the immune response. Sci. Adv. 2021;7:eabg6165. doi: 10.1126/sciadv.abg6165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Gostner J.M., Becker K., Kurz K., Fuchs D. Disturbed Amino Acid Metabolism in HIV: Association with Neuropsychiatric Symptoms. Front. Psychiatry. 2015;6:97. doi: 10.3389/fpsyt.2015.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Murray M.F. Tryptophan depletion and HIV infection: A metabolic link to pathogenesis. Lancet Infect. Dis. 2003;3:644–652. doi: 10.1016/S1473-3099(03)00773-4. [DOI] [PubMed] [Google Scholar]
- 197.Zhou Y.H., Sun L., Chen J., Sun W.W., Ma L., Han Y., Jin X., Zhao Q.X., Li T., Lu H., et al. Tryptophan Metabolism Activates Aryl Hydrocarbon Receptor-Mediated Pathway to Promote HIV-1 Infection and Reactivation. mBio. 2019;10:e02591-19. doi: 10.1128/mBio.02591-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Laurichesse H., Tauveron I., Gourdon F., Cormerais L., Champredon C., Charrier S., Rochon C., Lamain S., Bayle G., Laveran H., et al. Threonine and methionine are limiting amino acids for protein synthesis in patients with AIDS. J. Nutr. 1998;128:1342–1348. doi: 10.1093/jn/128.8.1342. [DOI] [PubMed] [Google Scholar]
- 199.Sitole L.J., Tugizimana F., Meyer D. Multi-platform metabonomics unravel amino acids as markers of HIV/combination antiretroviral therapy-induced oxidative stress. J. Pharm. Biomed. Anal. 2019;176:112796. doi: 10.1016/j.jpba.2019.112796. [DOI] [PubMed] [Google Scholar]
- 200.Rasmussen A.L., Diamond D.L., McDermott J.E., Gao X., Metz T.O., Matzke M.M., Carter V.S., Belisle S.E., Korth M.J., Waters K.M., et al. Systems virology identifies a mitochondrial fatty acid oxidation enzyme, dodecenoyl coenzyme A delta isomerase, required for hepatitis C virus replication and likely pathogenesis. J. Virol. 2011;85:11646–11654. doi: 10.1128/JVI.05605-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Fernandes-Siqueira L.O., Zeidler J.D., Sousa B.G., Ferreira T., Da Poian A.T. Anaplerotic Role of Glucose in the Oxidation of Endogenous Fatty Acids during Dengue Virus Infection. mSphere. 2018;3:e00458-17. doi: 10.1128/mSphere.00458-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Nanda P., Ghosh A. Genome Scale-Differential Flux Analysis reveals deregulation of lung cell metabolism on SARS-CoV-2 infection. PLoS Comput. Biol. 2021;17:e1008860. doi: 10.1371/journal.pcbi.1008860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ahmed D., Roy D., Cassol E. Examining Relationships between Metabolism and Persistent Inflammation in HIV Patients on Antiretroviral Therapy. Mediat. Inflamm. 2018;2018:6238978. doi: 10.1155/2018/6238978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Martín-Vicente M., González-Riaño C., Barbas C., Jiménez-Sousa M.Á., Brochado-Kith O., Resino S., Martínez I. Metabolic changes during respiratory syncytial virus infection of epithelial cells. PLoS ONE. 2020;15:e0230844. doi: 10.1371/journal.pone.0230844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Páez-Franco J.C., Torres-Ruiz J., Sosa-Hernández V.A., Cervantes-Díaz R., Romero-Ramírez S., Pérez-Fragoso A., Meza-Sánchez D.E., Germán-Acacio J.M., Maravillas-Montero J.L., Mejía-Domínguez N.R., et al. Metabolomics analysis reveals a modified amino acid metabolism that correlates with altered oxygen homeostasis in COVID-19 patients. Sci. Rep. 2021;11:6350. doi: 10.1038/s41598-021-85788-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Gelpi M., Mikaeloff F., Knudsen A.D., Benfeitas R., Krishnan S., Svenssson Akusjärvi S., Høgh J., Murray D.D., Ullum H., Neogi U., et al. The central role of the glutamate metabolism in long-term antiretroviral treated HIV-infected individuals with metabolic syndrome. Aging. 2021;13:22732–22751. doi: 10.18632/aging.203622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Tretter L., Adam-Vizi V. Alpha-ketoglutarate dehydrogenase: A target and generator of oxidative stress. Philos. Trans. R Soc. B Biol. Sci. 2005;360:2335–2345. doi: 10.1098/rstb.2005.1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Fu X., Li K., Niu Y., Lin Q., Liang H., Luo X., Liu L., Li N. The mTOR/PGC-1α/SIRT3 Pathway Drives Reductive Glutamine Metabolism to Reduce Oxidative Stress Caused by ISKNV in CPB Cells. Microbiol. Spectr. 2022;10:e0231021. doi: 10.1128/spectrum.02310-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ju H.Q., Lin J.F., Tian T., Xie D., Xu R.H. NADPH homeostasis in cancer: Functions, mechanisms and therapeutic implications. Signal Transduct. Target. Ther. 2020;5:231. doi: 10.1038/s41392-020-00326-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Panday A., Sahoo M.K., Osorio D., Batra S. NADPH oxidases: An overview from structure to innate immunity-associated pathologies. Cell. Mol. Immunol. 2015;12:5–23. doi: 10.1038/cmi.2014.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Amatore D., Sgarbanti R., Aquilano K., Baldelli S., Limongi D., Civitelli L., Nencioni L., Garaci E., Ciriolo M.R., Palamara A.T. Influenza virus replication in lung epithelial cells depends on redox-sensitive pathways activated by NOX4-derived ROS. Cell. Microbiol. 2015;17:131–145. doi: 10.1111/cmi.12343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Boudreau H.E., Emerson S.U., Korzeniowska A., Jendrysik M.A., Leto T.L. Hepatitis C virus (HCV) proteins induce NADPH oxidase 4 expression in a transforming growth factor beta-dependent manner: A new contributor to HCV-induced oxidative stress. J. Virol. 2009;83:12934–12946. doi: 10.1128/JVI.01059-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Violi F., Oliva A., Cangemi R., Ceccarelli G., Pignatelli P., Carnevale R., Cammisotto V., Lichtner M., Alessandri F., De Angelis M., et al. Nox2 activation in COVID-19. Redox Biol. 2020;36:101655. doi: 10.1016/j.redox.2020.101655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Shah A., Kumar S., Simon S.D., Singh D.P., Kumar A. HIV gp120- and methamphetamine-mediated oxidative stress induces astrocyte apoptosis via cytochrome P450 2E1. Cell Death Dis. 2013;4:e850. doi: 10.1038/cddis.2013.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Ivanov A.V., Valuev-Elliston V.T., Ivanova O.N., Kochetkov S.N., Starodubova E.S., Bartosch B., Isaguliants M.G. Oxidative Stress during HIV Infection: Mechanisms and Consequences. Oxid. Med. Cell Longev. 2016;2016:8910396. doi: 10.1155/2016/8910396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Amelio I., Cutruzzolá F., Antonov A., Agostini M., Melino G. Serine and glycine metabolism in cancer. Trends Biochem. Sci. 2014;39:191–198. doi: 10.1016/j.tibs.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Serefidou M., Venkatasubramani A.V., Imhof A. The Impact of One Carbon Metabolism on Histone Methylation. Front. Genet. 2019;10:764. doi: 10.3389/fgene.2019.00764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ayari A., Rosa-Calatrava M., Lancel S., Barthelemy J., Pizzorno A., Mayeuf-Louchart A., Baron M., Hot D., Deruyter L., Soulard D., et al. Influenza infection rewires energy metabolism and induces browning features in adipose cells and tissues. Commun. Biol. 2020;3:237. doi: 10.1038/s42003-020-0965-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Francesconi V., Giovannini L., Santucci M., Cichero E., Costi M.P., Naesens L., Giordanetto F., Tonelli M. Synthesis, biological evaluation and molecular modeling of novel azaspiro dihydrotriazines as influenza virus inhibitors targeting the host factor dihydrofolate reductase (DHFR) Eur. J. Med.Chem. 2018;155:229–243. doi: 10.1016/j.ejmech.2018.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Tonelli M., Naesens L., Gazzarrini S., Santucci M., Cichero E., Tasso B., Moroni A., Costi M.P., Loddo R. Host dihydrofolate reductase (DHFR)-directed cycloguanil analogues endowed with activity against influenza virus and respiratory syncytial virus. Eur. J. Med. Chem. 2017;135:467–478. doi: 10.1016/j.ejmech.2017.04.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Zhang Y., Guo R., Kim S.H., Shah H., Zhang S., Liang J.H., Fang Y., Gentili M., Leary C.N.O., Elledge S.J., et al. SARS-CoV-2 hijacks folate and one-carbon metabolism for viral replication. Nat. Commun. 2021;12:1676. doi: 10.1038/s41467-021-21903-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Zgheib R., Battaglia-Hsu S.F., Hergalant S., Quéré M., Alberto J.M., Chéry C., Rouyer P., Gauchotte G., Guéant J.L., Namour F. Folate can promote the methionine-dependent reprogramming of glioblastoma cells towards pluripotency. Cell Death Dis. 2019;10:596. doi: 10.1038/s41419-019-1836-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Chen L., Zhang Z., Hoshino A., Zheng H.D., Morley M., Arany Z., Rabinowitz J.D. NADPH production by the oxidative pentose-phosphate pathway supports folate metabolism. Nat. Metab. 2019;1:404–415. doi: 10.1038/s42255-019-0043-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Yang M., Vousden K.H. Serine and one-carbon metabolism in cancer. Nat. Rev. Cancer. 2016;16:650–662. doi: 10.1038/nrc.2016.81. [DOI] [PubMed] [Google Scholar]
- 225.Yu L., Teoh S.T., Ensink E., Ogrodzinski M.P., Yang C., Vazquez A.I., Lunt S.Y. Cysteine catabolism and the serine biosynthesis pathway support pyruvate production during pyruvate kinase knockdown in pancreatic cancer cells. Cancer Metab. 2019;7:13. doi: 10.1186/s40170-019-0205-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Sun L., Suo C., Li S.T., Zhang H., Gao P. Metabolic reprogramming for cancer cells and their microenvironment: Beyond the Warburg Effect. Biochim. Biophys. Acta Rev. Cancer. 2018;1870:51–66. doi: 10.1016/j.bbcan.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 227.Jacquet P., Stéphanou A. Metabolic Reprogramming, Questioning, and Implications for Cancer. Biology. 2021;10:129. doi: 10.3390/biology10020129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Adam C., Paolini L., Gueguen N., Mabilleau G., Preisser L., Blanchard S., Pignon P., Manero F., Le Mao M., Morel A., et al. Acetoacetate protects macrophages from lactic acidosis-induced mitochondrial dysfunction by metabolic reprograming. Nat. Commun. 2021;12:7115. doi: 10.1038/s41467-021-27426-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Biswas S.K. Metabolic Reprogramming of Immune Cells in Cancer Progression. Immunity. 2015;43:435–449. doi: 10.1016/j.immuni.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 230.Jing C., Castro-Dopico T., Richoz N., Tuong Z.K., Ferdinand J.R., Lok L.S.C., Loudon K.W., Banham G.D., Mathews R.J., Cader Z., et al. Macrophage metabolic reprogramming presents a therapeutic target in lupus nephritis. Proc. Natl. Acad. Sci. USA. 2020;117:15160–15171. doi: 10.1073/pnas.2000943117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Kim J., Kim J., Bae J.S. ROS homeostasis and metabolism: A critical liaison for cancer therapy. Exp. Mol. Med. 2016;48:e269. doi: 10.1038/emm.2016.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Palsson-McDermott E.M., O’Neill L.A. The Warburg effect then and now: From cancer to inflammatory diseases. Bioessays. 2013;35:965–973. doi: 10.1002/bies.201300084. [DOI] [PubMed] [Google Scholar]
- 233.Wang F., Zhang S., Jeon R., Vuckovic I., Jiang X., Lerman A., Folmes C.D., Dzeja P.D., Herrmann J. Interferon Gamma Induces Reversible Metabolic Reprogramming of M1 Macrophages to Sustain Cell Viability and Pro-Inflammatory Activity. EBioMedicine. 2018;30:303–316. doi: 10.1016/j.ebiom.2018.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Aguilar-Cazares D., Chavez-Dominguez R., Carlos-Reyes A., Lopez-Camarillo C., Hernadez de la Cruz O.N., Lopez-Gonzalez J.S. Contribution of Angiogenesis to Inflammation and Cancer. Front. Oncol. 2019;9:1399. doi: 10.3389/fonc.2019.01399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.D’Ignazio L., Batie M., Rocha S. Hypoxia and Inflammation in Cancer, Focus on HIF and NF-κB. Biomedicines. 2017;5:21. doi: 10.3390/biomedicines5020021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Schoppmann S.F., Birner P., Stöckl J., Kalt R., Ullrich R., Caucig C., Kriehuber E., Nagy K., Alitalo K., Kerjaschki D. Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral lymphangiogenesis. Am. J. Pathol. 2002;161:947–956. doi: 10.1016/S0002-9440(10)64255-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Wang L.X., Talebian F., Liu J.Q., Khattabi M., Yu L., Bai X.F. IL-10 contributes to the suppressive function of tumour-associated myeloid cells and enhances myeloid cell accumulation in tumours. Scand. J. Immunol. 2012;75:273–281. doi: 10.1111/j.1365-3083.2011.02662.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Tarasenko T.N., Jestin M., Matsumoto S., Saito K., Hwang S., Gavrilova O., Trivedi N., Zerfas P.M., Barca E., DiMauro S., et al. Macrophage derived TNFα promotes hepatic reprogramming to Warburg-like metabolism. J. Mol. Med. 2019;97:1231–1243. doi: 10.1007/s00109-019-01786-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Kilic M., Kasperczyk H., Fulda S., Debatin K.M. Role of hypoxia inducible factor-1 alpha in modulation of apoptosis resistance. Oncogene. 2007;26:2027–2038. doi: 10.1038/sj.onc.1210008. [DOI] [PubMed] [Google Scholar]
- 240.Del Rey M.J., Valín Á., Usategui A., García-Herrero C.M., Sánchez-Aragó M., Cuezva J.M., Galindo M., Bravo B., Cañete J.D., Blanco F.J., et al. Hif-1α Knockdown Reduces Glycolytic Metabolism and Induces Cell Death of Human Synovial Fibroblasts Under Normoxic Conditions. Sci. Rep. 2017;7:3644. doi: 10.1038/s41598-017-03921-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Fulda S., Debatin K.M. HIF-1-regulated glucose metabolism: A key to apoptosis resistance? Cell Cycle. 2007;6:790–792. doi: 10.4161/cc.6.7.4084. [DOI] [PubMed] [Google Scholar]
- 242.Xiong Z., Guo M., Yu Y., Zhang F.F., Ge M.K., Chen G.Q., Shen S.M. Downregulation of AIF by HIF-1 contributes to hypoxia-induced epithelial-mesenchymal transition of colon cancer. Carcinogenesis. 2016;37:1079–1088. doi: 10.1093/carcin/bgw089. [DOI] [PubMed] [Google Scholar]
- 243.Matsuura K., Canfield K., Feng W., Kurokawa M. Metabolic Regulation of Apoptosis in Cancer. Int. Rev. Cell Mol. Biol. 2016;327:43–87. doi: 10.1016/bs.ircmb.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Vaughn A.E., Deshmukh M. Glucose metabolism inhibits apoptosis in neurons and cancer cells by redox inactivation of cytochrome c. Nat. Cell Biol. 2008;10:1477–1483. doi: 10.1038/ncb1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Luo M., Fu A., Wu R., Wei N., Song K., Lim S., Luo K.Q. High Expression of G6PD Increases Doxorubicin Resistance in Triple Negative Breast Cancer Cells by Maintaining GSH Level. Int. J. Biol. Sci. 2022;18:1120–1133. doi: 10.7150/ijbs.65555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Fischer K., Hoffmann P., Voelkl S., Meidenbauer N., Ammer J., Edinger M., Gottfried E., Schwarz S., Rothe G., Hoves S., et al. Inhibitory effect of tumor cell-derived lactic acid on human T cells. Blood. 2007;109:3812–3819. doi: 10.1182/blood-2006-07-035972. [DOI] [PubMed] [Google Scholar]
- 247.Kumagai S., Koyama S., Itahashi K., Tanegashima T., Lin Y.T., Togashi Y., Kamada T., Irie T., Okumura G., Kono H., et al. Lactic acid promotes PD-1 expression in regulatory T cells in highly glycolytic tumor microenvironments. Cancer Cell. 2022;40:201–218.e9. doi: 10.1016/j.ccell.2022.01.001. [DOI] [PubMed] [Google Scholar]
- 248.Caronni N., Simoncello F., Stafetta F., Guarnaccia C., Ruiz-Moreno J.S., Opitz B., Galli T., Proux-Gillardeaux V., Benvenuti F. Downregulation of Membrane Trafficking Proteins and Lactate Conditioning Determine Loss of Dendritic Cell Function in Lung Cancer. Cancer Res. 2018;78:1685–1699. doi: 10.1158/0008-5472.CAN-17-1307. [DOI] [PubMed] [Google Scholar]
- 249.Goetze K., Walenta S., Ksiazkiewicz M., Kunz-Schughart L.A., Mueller-Klieser W. Lactate enhances motility of tumor cells and inhibits monocyte migration and cytokine release. Int. J. Oncol. 2011;39:453–463. doi: 10.3892/ijo.2011.1055. [DOI] [PubMed] [Google Scholar]
- 250.Gottfried E., Kunz-Schughart L.A., Ebner S., Mueller-Klieser W., Hoves S., Andreesen R., Mackensen A., Kreutz M. Tumor-derived lactic acid modulates dendritic cell activation and antigen expression. Blood. 2006;107:2013–2021. doi: 10.1182/blood-2005-05-1795. [DOI] [PubMed] [Google Scholar]
- 251.Ratter J.M., Rooijackers H.M.M., Hooiveld G.J., Hijmans A.G.M., de Galan B.E., Tack C.J., Stienstra R. In vitro and in vivo Effects of Lactate on Metabolism and Cytokine Production of Human Primary PBMCs and Monocytes. Front. Immunol. 2018;9:2564. doi: 10.3389/fimmu.2018.02564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Huang H., Li S., Tang Q., Zhu G. Metabolic Reprogramming and Immune Evasion in Nasopharyngeal Carcinoma. Front. Immunol. 2021;12:680955. doi: 10.3389/fimmu.2021.680955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Li X., Wenes M., Romero P., Huang S.C., Fendt S.M., Ho P.C. Navigating metabolic pathways to enhance antitumour immunity and immunotherapy. Nat. Rev. Clin. Oncol. 2019;16:425–441. doi: 10.1038/s41571-019-0203-7. [DOI] [PubMed] [Google Scholar]
- 254.Munn D.H., Mellor A.L. Indoleamine 2,3-dioxygenase and tumor-induced tolerance. J. Clin. Investig. 2007;117:1147–1154. doi: 10.1172/JCI31178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Fox J.M., Sage L.K., Huang L., Barber J., Klonowski K.D., Mellor A.L., Tompkins S.M., Tripp R.A. Inhibition of indoleamine 2,3-dioxygenase enhances the T-cell response to influenza virus infection. J. Gen. Virol. 2013;94:1451–1461. doi: 10.1099/vir.0.053124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.de Oliveira F.C., Coimbra J.S., de Oliveira E.B., Zuñiga A.D., Rojas E.E. Food Protein-polysaccharide Conjugates Obtained via the Maillard Reaction: A Review. Crit. Rev. Food Sci. Nutr. 2016;56:1108–1125. doi: 10.1080/10408398.2012.755669. [DOI] [PubMed] [Google Scholar]
- 257.Thorpe S.R., Baynes J.W. Maillard reaction products in tissue proteins: New products and new perspectives. Amino Acids. 2003;25:275–281. doi: 10.1007/s00726-003-0017-9. [DOI] [PubMed] [Google Scholar]
- 258.Allaman I., Bélanger M., Magistretti P.J. Methylglyoxal, the dark side of glycolysis. Front. Neurosci. 2015;9:23. doi: 10.3389/fnins.2015.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Kold-Christensen R., Johannsen M. Methylglyoxal Metabolism and Aging-Related Disease: Moving from Correlation toward Causation. Trends Endocrinol. Metab. 2020;31:81–92. doi: 10.1016/j.tem.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 260.Ahmed N. Advanced glycation endproducts-role in pathology of diabetic complications. Diabetes Res. Clin. Pract. 2005;67:3–21. doi: 10.1016/j.diabres.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 261.Angeloni C., Zambonin L., Hrelia S. Role of methylglyoxal in Alzheimer’s disease. BioMed Res. Int. 2014;2014:238485. doi: 10.1155/2014/238485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Vistoli G., De Maddis D., Cipak A., Zarkovic N., Carini M., Aldini G. Advanced glycoxidation and lipoxidation end products (AGEs and ALEs): An overview of their mechanisms of formation. Free Radic. Res. 2013;47((Suppl S1)):3–27. doi: 10.3109/10715762.2013.815348. [DOI] [PubMed] [Google Scholar]
- 263.Nandi S.K., Nahomi R.B., Rankenberg J., Glomb M.A., Nagaraj R.H. Glycation-mediated inter-protein cross-linking is promoted by chaperone-client complexes of α-crystallin: Implications for lens aging and presbyopia. J. Biol. Chem. 2020;295:5701–5716. doi: 10.1074/jbc.RA120.012604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Ulrich P., Cerami A. Protein glycation, diabetes, and aging. Recent Prog. Horm. Res. 2001;56:1–21. doi: 10.1210/rp.56.1.1. [DOI] [PubMed] [Google Scholar]
- 265.Facchiano F., Lentini A., Fogliano V., Mancarella S., Rossi C., Facchiano A., Capogrossi M.C. Sugar-induced modification of fibroblast growth factor 2 reduces its angiogenic activity in vivo. Am. J. Pathol. 2002;161:531–541. doi: 10.1016/S0002-9440(10)64209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Iannuzzi C., Irace G., Sirangelo I. Differential effects of glycation on protein aggregation and amyloid formation. Front. Mol. Biosci. 2014;1:9. doi: 10.3389/fmolb.2014.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Kass D.A. Getting better without AGE: New insights into the diabetic heart. Circ. Res. 2003;92:704–706. doi: 10.1161/01.RES.0000069362.52165.C9. [DOI] [PubMed] [Google Scholar]
- 268.Sirangelo I., Iannuzzi C. Understanding the Role of Protein Glycation in the Amyloid Aggregation Process. Int. J. Mol. Sci. 2021;22:6609. doi: 10.3390/ijms22126609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Bouma B., Kroon-Batenburg L.M., Wu Y.P., Brünjes B., Posthuma G., Kranenburg O., de Groot P.G., Voest E.E., Gebbink M.F. Glycation induces formation of amyloid cross-beta structure in albumin. J. Biol. Chem. 2003;278:41810–41819. doi: 10.1074/jbc.M303925200. [DOI] [PubMed] [Google Scholar]
- 270.Kichev A., Ilieva E.V., Piñol-Ripoll G., Podlesniy P., Ferrer I., Portero-Otín M., Pamplona R., Espinet C. Cell death and learning impairment in mice caused by in vitro modified pro-NGF can be related to its increased oxidative modifications in Alzheimer disease. Am. J. Pathol. 2009;175:2574–2585. doi: 10.2353/ajpath.2009.090018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Mendez D.L., Jensen R.A., McElroy L.A., Pena J.M., Esquerra R.M. The effect of non-enzymatic glycation on the unfolding of human serum albumin. Arch. Biochem. Biophys. 2005;444:92–99. doi: 10.1016/j.abb.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 272.Groener J.B., Oikonomou D., Cheko R., Kender Z., Zemva J., Kihm L., Muckenthaler M., Peters V., Fleming T., Kopf S., et al. Methylglyoxal and Advanced Glycation End Products in Patients with Diabetes-What We Know so Far and the Missing Links. Exp. Clin. Endocrinol. Diabetes. 2019;127:497–504. doi: 10.1055/s-0043-106443. [DOI] [PubMed] [Google Scholar]
- 273.Hanssen N.M., Beulens J.W., van Dieren S., Scheijen J.L., van der A D.L., Spijkerman A.M., van der Schouw Y.T., Stehouwer C.D., Schalkwijk C.G. Plasma advanced glycation end products are associated with incident cardiovascular events in individuals with type 2 diabetes: A case-cohort study with a median follow-up of 10 years (EPIC-NL) Diabetes. 2015;64:257–265. doi: 10.2337/db13-1864. [DOI] [PubMed] [Google Scholar]
- 274.Saulnier P.J., Wheelock K.M., Howell S., Weil E.J., Tanamas S.K., Knowler W.C., Lemley K.V., Mauer M., Yee B., Nelson R.G., et al. Advanced Glycation End Products Predict Loss of Renal Function and Correlate With Lesions of Diabetic Kidney Disease in American Indians With Type 2 Diabetes. Diabetes. 2016;65:3744–3753. doi: 10.2337/db16-0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Beisswenger P.J., Howell S.K., Russell G.B., Miller M.E., Rich S.S., Mauer M. Early progression of diabetic nephropathy correlates with methylglyoxal-derived advanced glycation end products. Diabetes Care. 2013;36:3234–3239. doi: 10.2337/dc12-2689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Fishman S.L., Sonmez H., Basman C., Singh V., Poretsky L. The role of advanced glycation end-products in the development of coronary artery disease in patients with and without diabetes mellitus: A review. Mol. Med. 2018;24:59. doi: 10.1186/s10020-018-0060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Bellier J., Nokin M.J., Lardé E., Karoyan P., Peulen O., Castronovo V., Bellahcène A. Methylglyoxal, a potent inducer of AGEs, connects between diabetes and cancer. Diabetes Res. Clin. Pract. 2019;148:200–211. doi: 10.1016/j.diabres.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 278.Azizian-Farsani F., Abedpoor N., Hasan Sheikhha M., Gure A.O., Nasr-Esfahani M.H., Ghaedi K. Receptor for Advanced Glycation End Products Acts as a Fuel to Colorectal Cancer Development. Front. Oncol. 2020;10:552283. doi: 10.3389/fonc.2020.552283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.van Zoelen M.A., van der Sluijs K.F., Achouiti A., Florquin S., Braun-Pater J.M., Yang H., Nawroth P.P., Tracey K.J., Bierhaus A., van der Poll T. Receptor for advanced glycation end products is detrimental during influenza A virus pneumonia. Virology. 2009;391:265–273. doi: 10.1016/j.virol.2009.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Passos F.R.S., Heimfarth L., Monteiro B.S., Corrêa C.B., Moura T.R., Araújo A.A.S., Martins-Filho P.R., Quintans-Júnior L.J., Quintans J.S.S. Oxidative stress and inflammatory markers in patients with COVID-19: Potential role of RAGE, HMGB1, GFAP and COX-2 in disease severity. Int. Immunopharmacol. 2022;104:108502. doi: 10.1016/j.intimp.2021.108502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Takeuchi M., Kikuchi S., Sasaki N., Suzuki T., Watai T., Iwaki M., Bucala R., Yamagishi S. Involvement of advanced glycation end-products (AGEs) in Alzheimer’s disease. Curr. Alzheimer Res. 2004;1:39–46. doi: 10.2174/1567205043480582. [DOI] [PubMed] [Google Scholar]
- 282.Batkulwar K., Godbole R., Banarjee R., Kassaar O., Williams R.J., Kulkarni M.J. Advanced Glycation End Products Modulate Amyloidogenic APP Processing and Tau Phosphorylation: A Mechanistic Link between Glycation and the Development of Alzheimer’s Disease. ACS Chem. Neurosci. 2018;9:988–1000. doi: 10.1021/acschemneuro.7b00410. [DOI] [PubMed] [Google Scholar]
- 283.Allen C.N., Arjona S.P., Santerre M., De Lucia C., Koch W.J., Sawaya B.E. Metabolic Reprogramming in HIV-Associated Neurocognitive Disorders (HAND) Front. Cell Neurosci. 2022 doi: 10.3389/fncel.2022.812887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Kong Y., Liu C., Zhou Y., Qi J., Zhang C., Sun B., Wang J., Guan Y. Progress of RAGE Molecular Imaging in Alzheimer’s Disease. Front. Aging Neurosci. 2020;12:227. doi: 10.3389/fnagi.2020.00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Takeuchi M., Yamagishi S. Possible involvement of advanced glycation end-products (AGEs) in the pathogenesis of Alzheimer’s disease. Curr. Pharm. Des. 2008;14:973–978. doi: 10.2174/138161208784139693. [DOI] [PubMed] [Google Scholar]
- 286.Vitek M.P., Bhattacharya K., Glendening J.M., Stopa E., Vlassara H., Bucala R., Manogue K., Cerami A. Advanced glycation end products contribute to amyloidosis in Alzheimer disease. Proc. Natl. Acad. Sci. USA. 1994;91:4766–4770. doi: 10.1073/pnas.91.11.4766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Alghamdi A., Forbes S., Birch D.J.S., Vyshemirsky V., Rolinski O.J. Detecting beta-amyloid glycation by intrinsic fluorescence-Understanding the link between diabetes and Alzheimer’s disease. Arch. Biochem. Biophys. 2021;704:108886. doi: 10.1016/j.abb.2021.108886. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.