Abstract
Skin, an exterior interface of the human body is home to commensal microbiota and also acts a physical barrier that protects from invasion of foreign pathogenic microorganisms. In recent years, interest has significantly expanded beyond the gut microbiome to include the skin microbiome and its influence in managing several skin disorders. Probiotics play a major role in maintaining human health and disease prevention. Topical probiotics have demonstrated beneficial effects for the treatment of certain inflammatory skin diseases such as acne, rosacea, psoriasis etc., and also found to have a promising role in wound healing. In this review, we discuss recent insights into applications of topical probiotics and their influence on health and diseases of the skin. Patents, commercially available topical probiotics, and novel probiotic impregnated fabrics have been emphasized. A thorough understanding of the relationship between probiotics and the skin microbiome is important for designing novel therapeutic approaches in using topical probiotics.
Keywords: probiotics, inflammatory, microorganisms, dermatitis
1. Introduction
Probiotics are live microorganisms which when taken in an appropriate amount help in maintaining good health. The naturally occurring microorganisms typically constitute the first-generation probiotics, while the genetically engineered strains are the secondary probiotics. The importance of microorganisms in human health dates back to the era when Louis Pasteur first discovered the importance of fermentation and also brought attention to the fact that the consumption of fermented food may be beneficial for health and longevity. Oral and topical probiotics have been used for treating several skin conditions [1].
Microorganisms reside inside our body, in both the gut and on our skin. Commensal bacteria play a vital role in human health; it also helps in maintaining a healthy immune system. The skin microbiome comprises several species of microorganisms. Any imbalance in these microorganisms results in skin disorders. Acne, atopic dermatitis, psoriasis, and rosacea are some common skin conditions that arise due to an imbalance in the existing skin microbiome [2].
Probiotics are well known for their clinical applications in certain skin disorders and probiotic bacterial therapy may have a great potential in preventing and treating several skin conditions [3]. Research studies have established a link between the disturbed gut microbiome and inflammatory skin diseases, thereby increasing the potential of oral probiotics as a treatment option for skin disorders [4]. However, there is very little information and clinical studies that have studied the efficacy of topically applied probiotic products. The topical application of probiotic bacteria may help to enhance the skin’s natural barrier by having a direct effect at the site of application. This may be by the virtue of the resident bacteria and the probiotic bacteria that produce certain antimicrobial amino peptides which benefit the immune responses in the skin and help in eliminating pathogens. Some cosmetic formulations may help in fostering the normal skin microbiome by being selective in their activity [5].
Although topical probiotics have been used to maintain a healthy skin microbiome since the beginning of the 20th century, the last decade has seen a dramatic rise in commercially available topical probiotics [6]. With the increasing popularity of these topical products and the dearth of clinical trials or efficacy studies to establish their clinical efficiency, we aimed to write a detailed review on the use of topical probiotics in treating skin disorders. This review includes details about the normal skin microbiome, various skin disorders and the commonly used topical probiotic formulations to treat these skin conditions. We have also discussed functional clothing with probiotics embedded into the fabric as a future solution for protecting the skin microbiome.
2. The Skin Microbiome and Its Functions
Human skin is the largest organ of the human body and is home to several microorganisms. The microbiome is referred to a collective genome of microorganisms. Hence, the skin microbiome is a collection of genomes that serves to maintain a complex relationship on the skin. Similar to the gut, the microorganisms residing on the skin are responsible for several functions. However, distinct from the microbiome in the gut, nose or stool, the skin microbiome is still being studied by microbiologists and dermatologists [7].
The skin microbiome comprises two main groups of microbes. The resident microbiome is the core and fixed group which can replenish itself following any perturbations. The transient microbiome, on the other hand, has a microbiome that does not permanently reside on the skin but appears for a few hours or days depending on the environment. In healthy skin, both types of microbiomes are non-pathogenic. The common phyla residing on the skin include Actinobacteria, Firmicutes, Proteobacteria and Bacteroides. The three most common genera are Corynebacteria, Propionibacteria and Staphylococci. Each microenvironment on the skin will harbor its microorganisms. While the sebaceous follicles, which is an anaerobic, lipid-rich environment, harbors the Propionibacterium, the axillar area mainly consists of gram-positive bacteria of the genera Staphylococcus, Micrococcus, Corynebacterium as well as Propionibacterium. The Staphylococcus, Propionibacterium, Micrococcus, Corynebacterium, Enhydrobacter and Streptococcus species mostly grow in the drier regions of the body [7]. Malassezia yeast is especially present on the scalp, with Demodex folliculorum a mite species. The areas of skin either fall into dry, sebaceous, or moist environments. Very little information is available about the viruses that reside on the skin. Their minuscule genomic sizes make metagenomic detection a difficult task. Fungi species such as Malassezia include the most common M. globosa, M. restricta, and M. sympodialis, which are lipophilic microbes frequently associated with sebum-rich areas of the skin. These Malassezia spp. Are especially prevalent in sebaceous areas. The Demodex mites (such as Demodex folliculorum and Demodex brevis), which are microscopic arthropods, are also regarded as part of the normal skin flora and are the permanent ectoparasites of humans and other mammalian pilosebaceous units. Hence, Malassezia spp. And Demodex are found inhabiting the same space on the skin [8,9]. Other fungi species such as Aspergillus, Cryptococcus, Epicoccum and Rhodotorula are present near the foot skin sites [10]. Interestingly on average, every human hand has more than 25 phyla present on the surface [11].
All of these species of bacteria, fungi, bacteroid, and other microbes that dwell in the skin utilize the limited resources of lipids and sebum on the skin and adapt to live in the dry, desiccated environment [12].
Different species have developed their strategies to adapt and thrive on the skin. Staphylococcus are halotolerant and utilize the salt in the sweat, while some have adapted by producing ‘adherens’ to adhere to the stratum corneum while using protease enzyme to liberate nutrients from the stratum corneum to survive [13].
We acquire the skin microbiome at birth, and it remains dynamic throughout our life. During birth, the flora is less diverse and acquires the composition of the site of delivery whether vaginal birth or cesarean section. The skin colonization by the commensal microbes continues during breastfeeding and even further to finally achieve an equilibrium during adulthood. Skin is a unique ecosystem that hosts the microbiome. The microbiome has several interactions within and with the skin [7]. The skin microbiome performs the following functions:
The residing bacteria provides the first line of defense against invading pathogens. The bac-terium Staphylococcus epidermidis secrete a protease that inhibits biofilm formation and colo-nization by Staphylococcus aureus in the anterior nostrils [13];
The skin bacteria have a synergistic relationship with the skin’s arsenal. By upregulating the secretion of several defensive biomarkers, the skin microbiome boosts the skin’s immune function. For example, S. epidermidis activates the production of the Toll-like receptors TLR2 to amplify the keratinocytes response to pathogens. On the other hand, the same bacteria func-tions to inhibit TLR3 activated inflammation in wound healing activity and help to speed the process of wound healing [13];
Human skin also shows the abundant presence of coagulase-negative staphylococci that through various mechanisms include the epidermal barrier environment and innate and adaptive immune systems within the epidermis and dermis. Some species and strains of this bacteria also produce beneficial products that augment host immunity by exerting specifically targeted antimicrobial, anti-inflammatory, or anti-neoplastic activity while also promoting broad innate and adaptive immune responses [14];
The skin’s stratum corneum has endogenous urocanic acid that protects against the harmful ultraviolet radiations by a behavior similar to sunscreens [15]. S. aureus in the skin can convert histidine to the amino acid that further converts to trans urocanic acid, thereby offering UV protection to the skin [13];
Corynebacterium species can modify the lipid composition on the skin’s surface and provide the thick sebum barrier [13];
The coagulase-negative staphylococcus species produce bacteriocins that have antibacterial properties that limit the survival of pathogenic bacteria on the skin surface [14];
S. epidermidis also has an antineoplastic activity that may protect the skin from cancer [16].
3. Skin Disorders
Most of the time, the microorganisms constituting the skin microbiome are in harmony with each other and perform their functions of protecting the skin. However, environmental stresses and other factors may cause a shift of the commensal microbes to pathogenic microbes resulting in inflammation, itching, scaling and other clinical signs suggesting an imbalance between our skin and its microbiome [17]. The disruption in the skin microbiome composition is termed dysbiosis. Functional dysbiosis affects the microbe-host interactions and results in skin disorders. The host factors such as age, sex, hygiene, use of certain medications, skin pH, sweating tendency, hair growth on the skin, sebum production, use of skin cosmetics and lifestyle play a significant role in the microbiome host interactions [10]. An imbalance in the skin microbiome results in several skin disorders due to loss of homeostasis. The most common skin conditions that are presented to primary care physicians are acne, atopic dermatitis, rosacea, psoriasis, and dandruff. These conditions affect majority of the population and are the most studied as they also affect psychosocial health [18]. Therefore, these skin conditions offer more avenues for research of probiotics for topical benefits [19].
3.1. Acne
Almost up to 90% of adolescents and young adults are affected by acne [20]. The pathophysiology of acne includes hyper seborrhea, follicular hyperkeratinization, increased colonization by microbes and inflammation [21]. The primary bacterium associated with this condition is Cutibacterium acnes (formerly Propionibacterium acnes) [22,23]. It colonizes sebaceous follicles that provide the bacterium with an anaerobic and lipid-rich environment. Secretion of several enzymes such as hyaluronidases, lipases and proteases, causes local injury and inflammation. The sebaceous gland produces and secretes a rich lipid secretion, which forms a hydrophobic layer on the skin that protects and lubricates hair and skin. Although the sebum has antibacterial functions, P. acnes hydrolyzes triglycerides present in secretions and releases free fatty acids that promote bacterial adherence by facilitating the colonization of these glands.
During adolescence several hormonal changes take place. There is an increased production of androgens including insulin growth factor-1, that is responsible for increased sebum production which in turn results in increased colonization of P. acnes. In addition to this, S. epidermidis, S. aureus, Streptococcus pneumoniae, Enterobacter and Klebsiella pneumoniae are the other bacteria that contribute to the inflammatory process by changing the expression of enzymes such as lipases and delta-hemolysins. The changes in the skin microbiome under the influence of age-related hormonal changes, stress, anxiety and lifestyle changes result in a breakout of acne on the skin [24].
While oral antibiotics are prescribed to treat acne in addition to isotretinoin and other topical antibacterial formulations [24], oral and topical probiotics have also been a recent addition to this treatment [25,26].
3.2. Atopic Dermatitis
Atopic dermatitis (AD) is a common inflammatory skin disease, affecting 15% to 20% of children and 1% to 3% of adults worldwide. The prevalence of AD has increased by 2-fold to 3-fold during the past decade in western countries [14]. Atopic dermatitis is a common term used in the medical literature, but according to The Nomenclature Review Committee of The World Allergy Organization, the name which should be used is eczema [27]. Atopic dermatitis is a chronic inflammatory skin condition that is one of the most frequent skin conditions around the world. The condition is characterized by dryness, redness of the skin followed by erythematous lesions. Quite often, people with atopic dermatitis also experience eczema, scaling of the skin and itching. Sometimes it is also associated with comorbidities such as allergic rhinoconjunctivitis and asthma [28]. The signs and symptoms of atopic dermatitis depend on age. While children are particularly at a high risk of developing atopic dermatitis, it is also seen in adolescents and adults [29].
There appears to be a tri-directional Atopic dermatitis-Skin microbiome-skin barrier relationship that marks the etiology of the condition. Studies have shown large colonies of S. aureus residing in the dry skin of people with this condition. The dysbiosis in the skin microbiome characterized by low bacterial diversity and increased S. aureus population in the skin results in flaring of the condition [29]. The excess S. aureus in the skin triggers the production of interleukins IL-36α and IL-1α in keratinocytes, which in turn induces IL-17 production in γδT cells, innate lymphoid cell type 3, and CD4+ T cells, and enhances neutrophil recruitment. In addition, S. aureus also produces various proteases enzymes to disrupt the keratinocytes thereby compromising the physical barrier of the skin. Furthermore, in these patients, there are deformed or irregular corneocytes due to filaggrin deficiency resulting in dry itchy skin [30]. Such skin is now open for abnormal entry of microbes into the dermis. The excess S. aureus also plays with the Th-2 immune responses and results in a dysregulation of the innate antimicrobial immune responses [14].
The use of a conventional line of treatment has not been very successful in treating the severity of this condition. Restoring the skin diversity is an important treatment strategy for treating atopic dermatitis [29]. A large number of immune cells triggered by commensals have several roles in restoring the integrity of the epidermal barrier [31,32]. Furthermore, the commensal-specific immune responses help provide heterologous protection against dermal pathogens. As a result, the use of commensal bacterial species in a topical formulation as a probiotic has been under several clinical studies at present [30]. Increased colonization with Staphylococcus aureus (S. aureus) and reduced bacterial diversity in skin microbiome has been identified as the promoter of atopic dermatitis. S. aureus aggravates the condition of atopic dermatitis. Monoclonal antibodies such as Dupilumab have shown improvement in atopic dermatitis, immune abnormalities, and epidermal barrier function by blocking IL-4Rα signaling. Studies indicate the increased Shannon diversity and decreased proportion of the genus Staphylococcus and S. aureus and an increase in S. hominis and S. epidermidis after treatment of atopic dermatitis with dupilumab therapy. Studies suggest that dupilumab therapy results in pronounced changes in the microbiome in lesional and non-lesional skin and in the nose, with significant changes in bacterial community structure favoring reduction in S. aureus population [33].
3.3. Psoriasis
Psoriasis is a chronic skin disease with an autoimmune origin and has affected almost 2.5–3.5% of the world population [34,35]. Around 20% of people with psoriasis experience red, scaling painful skin lesions accompanied by psoriatic arthritis. Psoriasis typically arises when there is a dysregulation in the immune responses of individuals who have a genetic predisposition to this skin condition [36].
The pathophysiology of the condition includes abnormal keratinocyte proliferation and immune cell infiltration in the dermis and epidermis involving the innate and adaptive immune systems, with important roles for dendritic cells and T cells, among other cells [37]. Studies carried out on the psoriatic lesions of the skin have shown a dysbiosis in the skin microbiome that is responsible for the dysregulation of the skin immune responses, thereby leading to an inflammatory condition. The lesions show the abundant presence of Streptococcus and a decreased level of Propionibacterium. This also indicates a lack of microbial diversity which in addition to dysbiosis is mainly responsible for psoriasis [36].
Studies have been carried out to explore the potential of probiotics in the treatment of psoriasis along with the conventional mode of treatment [3]. Conventional treatment of psoriasis involves topical as well as systemic medications depending upon the severity of the disease. Topical therapies include use of corticosteroids, vitamin D analogues, and retinoids. Systemic therapies involve administration of as methotrexate, retinoids, and ciclosporin are effective for patients with refractory or extensive cutaneous disease. In more extensive cases of disease phototherapy may be given. Characteristically, the microbiome in psoriasis patients exhibit a reduced population of beneficial microorganisms, viz., Parabacteroides, Coprobacillus, Lactobacillus spp., Bifidobacterium spp., and F. prausnitzii. Thus, restoring the gut microbiome balance has potential for the effective management of psoriasis. Oral administration of Lactobacillus pentosus significantly reduced the erythema, scaling, and epidermal thickening associated with psoriasis in animal model. [38] Reduced expression of inflammatory cytokines viz., expression of TNF-α, IL-6, and proinflammatory cytokines in the IL-23/IL-17 cytokine axis on the administration of probiotics suggest a possible therapeutic modality to manage psoriasis [39]. The administration of L. sporogens has also significantly improved severe pustular psoriasis in patients, who were unresponsive to conventional therapy. Encouragingly, these patients exhibited complete remission after 4 weeks of probiotic therapy [40]. However, topical use of probiotics is not yet explored for management of psoriasis. Animal studies have confirmed the effect of probiotic Lactobacillus sakei proBio-65 extract on the severity of skin inflammation due to psoriasis in a Mouse Model [41].
3.4. Rosacea
Rosacea is another chronic inflammatory skin condition that occurs due to an interplay between genetics, immune dysregulation, presence of pathogenic microorganisms and neurological dysregulation. As high as 18% of the global population suffers from this skin condition. The condition is characterized by flushing and erythema as the first signs that may appear during younger ages. Telangiectasias appear as rosacea lesions in older ages. The overall rosacea manifestations are flushing, transient or persistent erythema, telangiectasia, papules, pustules, phymata, and microedema [42].
Multiple stimuli are responsible for increased levels of cathelicidin and kallikrein 5, TLR2 matrix metalloproteinases, and mast cells within the skin. The condition further progresses due to the presence of unwanted microorganisms and exposure to harmful UV radiations [43]. Emotional stress, hot and dry weather, extreme cold, alcohol, beverages and certain medications can trigger the skin condition.
Rosacea has been found to be associated with alterations in skin microbiome. Microbial examination of the rosacea-affected skin reveals colonization of the demodex species excess presence of S. epidermidis [44]. An overgrowth of commensal skin microorganisms has been observed in the skin of rosacea patients. Demodex folliculorum were found to be in higher density which can increase from 0.7/cm2 (in control subjects) to 10.8/cm2 in rosacea patients. Additionally, the role of Bacillus oleronius and Staphylococcus epidermidis is also suspected in causing rosacea. Interestingly, rosacea severity increased with age and the relative abundance of C. acnes decreased, whereas the relative abundance of Snodgrassella alvi increased. Geobacillus and Gordonia has also been found to be significantly associated with severity of rosacea. [45,46] Other microorganisms such as Helicobacter pylori, and Bartonella quintana are also associated with the condition. Patients with rosacea demonstrate increased densities of Demodex mites (both D. brevis and D. folliculorum) in their skin compared with controls. D. folliculorum’s exoskeleton itself incites the production of inflammatory markers that activates the innate immune system [47]. The products from the microbes are responsible for activation of the TLRs and the G-protein-coupled receptor proteinase-activated receptor 2 that are expressed by keratinocytes. Activation of both receptors promotes the activation of cathelicidin an anti-microbial peptide that is also overexpressed in rosacea. Increased cathelicidin levels in rosacea patients affect both vasoactive and pro-inflammatory properties [48]. Activation of TLR2 releases pro-inflammatory cytokines, chemokines, proteases, and pro-angiogenic factors, which are mediators associated with rosacea symptoms such as erythema, telangiectasia, or inflammation or a combination of these symptoms. This affects the integrity of the skin barrier resulting in more inflammation [42]. Additionally, the endobacterium B. oleronius, which resides inside D. folliculorum, secretes heat-shock proteins and a lipoprotein. It is understood that these proteins stimulate TLR2 and therefore can cause inflammation [49]. The condition is treated by symptom-based treatment modalities. A case study where scalp rosacea has been treated with oral probiotics has been reported [50]. The use of topical probiotics in the treatment of this condition needs proper clinical trials.
3.5. Dandruff and Seborrheic Dermatitis
Dandruff is a skin condition affecting almost 50% of the world population. The severe form of dandruff may affect the skin by causing seborrheic dermatitis. The fungal species in the skin microbiome play an important role in dandruff and seborrheic dermatitis. Malassezia restricta, Malassezia furfur, and Malassezia 6eborrh are the most abundant species of the Malassezia genus [45]. The excess Malassezia spp. Growth on the skin results in inflammatory responses and results in seborrheic dermatitis [51]. Excess growth occurs in the sebum-rich area of the skin and scalp. Studies have shown bacterial imbalance in Cutibacterium and Staphylococcus species in this condition. While the conventional treatment involves antifungal, antibacterial shampoos, studies on probiotics efficiency in this condition due to the involvement of gut microbiome imbalance are being carried out [45]. Keratolytic agents or keratinization regulators are commonly used to treat dandruff conditions. These agents are applied topically. There are no studies reported for the interaction of keratolytic and probiotics. A patent (EP2149368B1) describes use of Lactobacillus spp. For management of dandruff. Lactobacillus paracasei showed positive effects in reducing the dandruff by increasing the hydration and restoring the barrier function of the scalp [52].
In addition to these commonly observed skin conditions, some skin cancer patients have also reported having an imbalance in the skin microbiome, suggesting new avenues for treating skin cancers [45].
4. The Importance of Gut-Skin Axis in Skin Disorders
The gut has its microbiome similar to the skin. Several research studies link inflammatory skin diseases with the imbalanced gut microbiome. The gut microbiome influences the human immune system. The immune system protects against exogenous pathogens. If there is dysbiosis in the gut microbiome, then the altered gut microflora may result in autoimmune and inflammatory conditions not only in the gut but also in distant organs such as the skin [4]. Several studies support the concept that an imbalance in the gut microbiome may result in skin conditions such as acne [53,54], atopic dermatitis [55], psoriasis [56] and rosacea [57]. The connection between the skin and gut seems to be mediated by the host immune system. The interaction between the microorganisms and the host immune system is important to maintain skin homeostasis [45]. Therefore, balancing the skin microbiome is a logical approach in treating several skin conditions. Probiotics play a vital role in restoring the microbiome and are an important therapeutic modality in the treatment of inflammatory skin diseases [4].
5. Role of Topical Probiotics in the Skin Microbiome
Scientists continue to explore the gut-skin axis connection in various skin disorders. With our growing knowledge about the role of the microbiome in various skin diseases, modulating the immune system by restoring the balance in the microbiome becomes a new avenue of research. The direct approach to this kind of treatment involves the use of probiotics in oral and topical form [58]. Probiotics are body-friendly bacteria that restore the body’s natural flora.
Over the past decade, there has been a surge in the use of oral and topical probiotics for skincare cosmetic formulations and the treatment of skin diseases. While new products are introduced in the market several scientists are carrying out studies to determine their efficacy, mechanism of action, safety, and indications. Topical probiotics are considered as safe a treatment modality and devoid of any adverse effects, especially if compared to conventional treatment options for skin disorders [1,59]. However, there are a limited number of clinical trials and efficacy studies in this regard. Most topical preparations are still being used as personal beauty products and the clinical trials are ongoing [60,61].
Although the precise mechanisms by which probiotics improve skin health are not yet known, the beneficial effects on skin health have been demonstrated in several papers and patents and the literature continues to grow. Table 1 lists several patents related to the application of topical probiotics for skin care.
Table 1.
Several patents related to the use of topical probiotics for the treatment of various skin disorders.
| Sr. No. | Title of Invention | Probiotic Strain Used | Use of the Product | Date of Publication | Patent Number |
|---|---|---|---|---|---|
| 1 | Cosmetic composition having probiotic bacteria | Bifidobacteria longum; Bifidobacteria bifidum; Bifidobacteria breve; Bifidobacteria pseudolongum, or mixtures thereof | Cleaning and antiageing treatment | 20 April 2017 | WO2017063066A1 |
| Skin probiotic | Probiotic commensal skin bacteria, and probiotic commensal skin bacteria fermentation extract. The probiotic commensal skin bacteria from one of a Propionibacterium species, a Paenibacillus species, or a Staphylococcus species. | For producing or maintaining skin microbiome balance |
16 July 2015 | WO2015106175A1 | |
| 3 | Composition, topical probiotic, postbiotic, pharmaceutical and topical compositions, methods for treating skin or mucosal infections, for treating a dermatological disorder associated with c. acnes and for diagnosing a skin disease or disorder, and formulation for topical application |
S. capitis N030_E12, S. epidermidis AMT5_C5, S. epidermidis N009_G7, S. epidermidis N018_F3 |
For the topical treatment of dysbiosis disorders of the skin, scalp or mucous membranes; and acne. | 13 September 2019 19 March 2020 |
BR112021004538A2 WO 2020/056359 |
| 4 | Method for inhibiting the growth, migration, proliferation and/or metastasis of a precancerous, cancerous or neoplastic cell or inhibiting a pathogen, topical probiotic composition, bandage or dressing, method of treating skin damage due to UV radiation and pharmaceutical composition | S. epidermidis MO34 or MO38 or MO34 and MO38 | Useful for treating infections, cancer and neoplastic diseases and neoplastic disorders. | 27 March 2018 4 October 2018 |
BR112019017962A2 WO 2018/183288 |
| 5 | Skin microbiome colonizer formulations and methods for use | Bacillus licheniformis, Bifidobacterium breve, Bifidobacterium infantis, Lactobacillus fermentum, Lactobacillus plantarum, Lactobacillus rhamnosus, Lactobacillus sakei, Lactobacillus paracasei, Staphylococcus epidermidis, and Staphylococcus xylosus. | For treating dysbiosis of the skin | 30 June 2020 | US10695386B2 |
| 6 | Probiotic treatment of skin diseases, disorders, and infections: formulations, methods and systems | Lactobacillus jensenii, Lactobacillus vaginalis | For reducing dandruff of the scalp | 26 March 2019 | US10238597B2 |
| 7 | Method of using topical probiotics for the inhibition of surface contamination by a pathogenic microorganism and composition therefor | Lactobacillus acidophilus NCFM®; Lactobacillus acidophilus La-14; Lactobacillus paracasei Lpc-37 | Prevent contamination by pathogenic microorganisms | 8 May 2008 | US20080107699A1 |
| 8 | Cosmetic composition comprising cocoa bean hydrolysate and at least one prebiotic and probiotic | Lysate of the genus Bacillus | Treatment and/or alleviation of seborrheic disorders, in particular sebum-dependent inflammation and/or bacterial proliferation. | 28 August 2020 | CN111601583A |
| 9 | Use of probiotic microorganisms to limit skin irritations | Lactobacillus paracasei species | To prevent skin irritation due to external aggressions | 2 April 2020 | ES2751994T3 |
| 10 | Cosmetic and dermatological use of probiotic microorganisms Lactobacillus paracasei for the treatment of fatty disorders of the scalp | Lactobacillus paracasei, or a lysate thereof. | Treatment of fatty disorders of the scalp | 7 August 2018 | ES2677905T3 |
| 11 | Cosmetic composition comprising a eborrheic spinosa extract, a kappaphycus alvarezii extract, at least one prebiotic and a probiotic |
Lysate of Lactobacillus bacteria | To maintain the balance of the cutaneous microbiota, and reinforce the cutaneous barrier | 28 October 2020 | EP3727594A1 |
| 12 | Cosmetic and/or dermatological composition for preventing and/or treating sensitive or dry skin | Lactobacillus johnsonii (CNCM I-1225), Lactobacillus paracasei (CNCM I-2116), Bifidobacterium adrecentis (CNCM I-2168), Bifidobacterium longum (CNCM 1-2170)), Bifidobacterium lactis (CNCM I-3446), Bifidobacterium longum (BB536) | Prevention and/or treatment of sensitive and/or dry skin | 29 January 2009 | JP2009503042A |
| 13 | Antibacterial lysate of probiotic bacteria | Lactobacillus rhamnosus | For skin tissue repair, wound repair | 12 March 2015 | WO2015/181534 A1 |
| 14 | Probiotic stick formulation for skin maintenance and methods of use |
Streptococcus thermophilus, Streptococcus salivarus subspecies thermophilus type 1131, Bifidobacterium longum, Lactobacillus paracasei and Streptococcus salivarius. | Hydration of skin, reduction in lines or wrinkles, treating acne and skin inflammation | 16 May 2017 | US9649346B2 |
| 15 | Probiotic bacteria for the topical treatment of skin disorders | Cell lysates from Bifidobacterium, Brevibacterium, Propionibacterium, Lactococcus, Streptococcus, Lactobacillus (e.g., L. acidophilus), Enterococcus, Pediococcus, Leuconostoc, and/or Oenococcus | Improvement of tight junction integrity between normal human epidermal keratinocytes. |
26 September 2018 08 November 2012 |
EP 2 704 704 B1 WO 2012/150269 |
| 16 | Topical compositions containing probiotic bacillus bacteria, spores, and extracellular products and uses thereof |
Bacillus coagulans
Pseudomonas lindbergii |
Inhibit the growth of bacterium, yeast, fungi. | 20 April 2008 | US6723326B1 |
| 17 | Use of cosmetic agent of probiotic microorganism in particular of Lactobacillus and Bifidobacterium species genus, for treating scalp disorders e.g., dandruff condition, pruritis or eborrheic dermatitis |
Lactobacillus or bifodobacterium | Restoration of normal scalp, reduces irritation, itching and dandruff | 21 May 2010 | FR2938429B1 |
| 18 | Use of Lactobacillus plantarum gmnl-6 composition for skin care | Lactobacillus plantarum | Improving skin condition by collagen secretion and ceramide synthesis | 18 May 2021 | US11007137B2 |
| 19 | Topical use of probiotic bacillus spores to prevent or control microbial infections | Bacillus species, spores or an extracellular product of a B. coagulans strain | inhibiting growth of yeast, fungus, bacteria or Herpes simplex virus | 9 November 2009 | EPO975227A1 |
| 20 | Use of probiotic bacteria for the preparation of topical compositions for skin protection | L plantarum P 17630 | Preventing and treating microbial diseases of the skin | 9 February 2006 | WO 2006/013441A2 |
6. Topical Probiotics for the Management of Skin Disorders
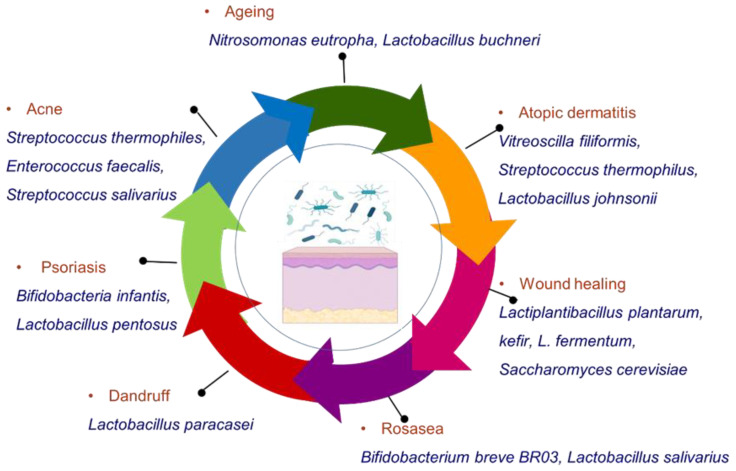
Some studies on animals and in humans have been conducted in order to define the exact role of topical probiotics in maintaining microbial balance in skin disorders and their role in dermatology as a whole. Figure 1 represents the various probiotic microorganisms that have shown beneficial effects in the management of some common disorders.
Figure 1.
Different probiotic microorganisms useful in the management of various skin disorders.
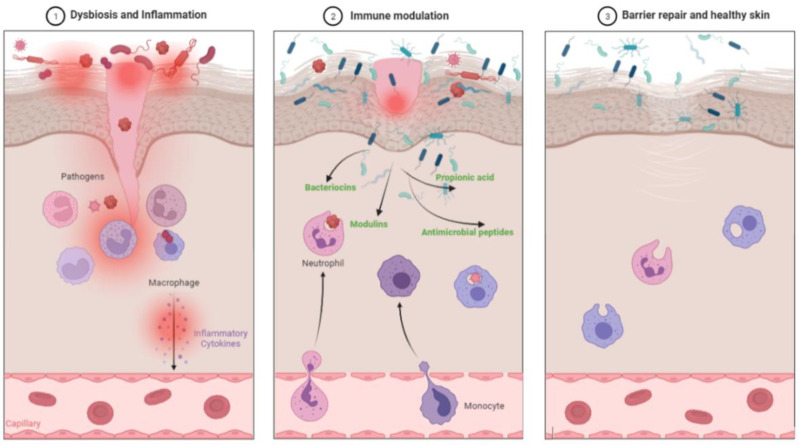
Probiotics are known to block the release of inflammatory cytokines and thus help reduce the skin inflammation [63]. Probiotics such as L. plantarum and L. acidophilus inhibit several activities of several inflammatory mediators, cytokines, and related signaling pathways. Probiotics accelerates the recovery of skin barrier function and inhibits P-induced skin inflammation [63]. We will discuss the various topical probiotics and their role in different skin disorders and also in skin aging, photoaging and wound healing. Figure 2 shows mechanism of action of probiotics in improving the skin health.
Figure 2.
The mechanism of improving skin health by probiotics via blocking the inflammatory pathways. (1) Picture depicts dysbiosis and infection due to pathogenic bacteria (Red colored) causing inflammation. (2) Probiotic bacteria (Blue-green colored) occupy a similar ecological niche to that of pathogenic microbes and avoiding their colonization. Probiotics improve immune tolerance, reduce inflammation, and also release important biochemicals such as bacteriocins, modulins, antimicrobial peptides and propionic acid that inhibit growth of harmful microbes. (3) Recovery of the skin barrier function leading to healthy skin with healthy commensal bacteria. Following are several skin problems in which topical probiotics have shown results.
6.1. Acne
Individuals with acne have a unique skin microbiome. The current topical treatment for acne has several challenges since it disrupts the physical barrier of the skin, thus making it dry and irritating. Research that studies the skin-gut axis relation in acne indicated that the use of probiotics can help in improving immune reactions beyond the gut and expand them towards the skin [1]. Growing evidence suggests that topical probiotics also improved the skin barrier and produced a secondary increase in antimicrobial peptides. For example, the lactic acid bacterium Streptococcus thermophiles enhance ceramide production both in vitro and in vivo when applied as a cream for a week [64,65,66]. Ceramides are well-known for confining water in the skin, and certain ceramide sphingolipids such as Phyto sphingosine show antimicrobial activity against Cutibacterium acnes, thereby improving acne. By producing ceramides, probiotics help strengthen the skin barrier, this is beneficial to acne-affected skin as the ceramides soothe the irritated skin [67].
Furthermore, the topical application of phytosphingosine has been shown to reduce papules and pustules in acne patients [68]. An in vitro study evaluated the symbiotic ability of probiotic bacteria and konjac glucomannan hydrolysates to inhibit P. acnes growth. The authors found that different probiotic bacteria strains were able to inhibit the growth of this skin bacterium species and the presence of the GMH prebiotic significantly enhanced the inhibition [69].
In another study, a lotion containing Enterococcus faecalis significantly reduced pustules compared to placebo lotion. This may be attributed to the anti-P. acnes activity produced by E. faecalis SL-5. It may thus have a potential role in the treatment of acne and could be possibly used as an alternative to topical antibiotics [70].
While one study on Streptococcus salivarius, a prominent member of healthy humans’ oral microbiota shows inhibition of P. acnes [53,54,71], and some studies indicate that certain probiotic strains also showed inhibition of E. coli, P. acnes, and P. aeruginosa in vitro studies [72].
Hence, topical probiotics may act as protective barriers, inhibit acne-causing bacteria, reduce the pustules, and provide relief from skin irritation in acne patients.
6.2. Atopic Dermatitis
Atopic dermatitis primarily arises due to a reduction in the microbial diversity; the predominant microorganism in these patients is S. aureus, as discussed above. Several recent studies indicate that topical probiotics, in addition to emollients, may be a good alternative for treating the condition [73]. A study suggested that a 5% Vitreoscilla filiformis extract-containing ointment significantly reduced eczema associated with atopic dermatitis and also reduced the severity of the symptoms in a randomized, double-blind, vehicle-controlled trial [74]. Another study showed the effectiveness of the lactic acid bacterium Streptococcus thermophilus on the stratum corneum by improving ceramide concentrations in the skin [64]. In a randomized double-blind trial on individuals with atopic dermatitis, the researchers studied the application of a Lactobaciilus containing emollient as compared to a normal emollient application. The emollient containing L. sakei inhibited the growth of S. aureus, provided a physical barrier and showed improved symptoms in individuals with atopic dermatitis [75]. A trial investigating the effects of a lotion containing the heat-treated probiotic strain Lactobacillus johnsonii NCC on S. aureus colonization depicted an improvement in the clinical symptoms of individuals with atopic dermatitis. Similarly, another trial that studied the use of Roseomonas mucosa as a form of treatment was associated with a significant reduction in disease severity, topical steroid requirement, and S. aureus burden. The trial reported no adverse effects or complications [76]. Most trials conducted to date have indicated a positive effect of topical probiotics in individuals with atopic dermatitis.
6.3. Psoriasis
Psoriasis, an autoimmune chronic skin condition, has been treated with topical emollients and oral immunosuppressants. Very few studies that include topical probiotics for treating psoriasis have been conducted. While studies have indicated that the alteration in the skin microbiome may be useful in controlling psoriasis symptoms, oral probiotics have shown improvement in the clinical symptoms in some studies. However, research work that studied the efficacy of topical probiotics in individuals with psoriasis is required to clinically prove the effectiveness of topical probiotics [58].
6.4. Seborrheic Dermatitis
Excess growth of yeast on the scalp with reduced diversity of microbiome results in dandruff and seborrheic dermatitis. Some studies have been carried out to evaluate the use of topical probiotics in this condition. A research study carried out on 60 patients showed a reduction in erythema, scaling and pruritis after topical application of Vitreoscilla filiformis [74,77]. Another study revealed increased IL-10 production by dendritic cells and increased Treg activity due to Vitreoscilla filiformis lysate [78]. Dandruff, seborrheic dermatitis and scalp related conditions have shown improvement after oral administration of Lactobacillus paracasei. There is a need for more studies on the topical efficacy of probiotics to treat this condition [79].
6.5. Wound Healing
Wounds due to injury to the skin result in the alteration of the skin microbiome. Studies have been carried out to find the efficacy of topical probiotics in infection prevention during wound healing [1]. Effect of Lactiplantibacillus plantarum, kefir, L. fermentum, and Saccharomyces cerevisiae has been studied in animal models with thermal wound injuries, diabetic ulcers, and uninfected wounds. Out of the models studied, mixed results were obtained. Some studies reported a positive wound healing effects by increased granulation tissue deposition, improved collagen concentration, and stimulation of angiogenesis, while some models did not improve the wound healing process [25,26].
In another study, Kefir, although originally a cultured probiotic beverage, has also shown topical antimicrobial activity against Salmonella, Helicobacter, Shigella and Staphylococcus, and E. coli. The probable mechanisms for this activity may be the production of exopolysaccharides that have immunostimulatory activity, activation of macrophages and lymphocytes [80,81], species-specific antagonism and through the regulation of antimicrobial peptides that help to maintain the integrity of the skin. They modulate skin microflora, improve skin integrity, and decrease inflammation [25,26]. Topical probiotics may also have the potential to inhibit the formation of biofilm over the wounds. An in-vitro study suggests commensal organisms antagonize the pathogenic strains that may produce a biofilm. [82] More clinical trials are required to prove the efficacy of topical probiotics in wound healing and for improved reproducibility of results [26].
6.6. Photoaging and Skin Aging
Topical probiotics have made the latest entry into the skincare world with their use in photoaging and skin aging. While the clinical trials for the same are underway, there has been a study that depicts the use of probiotics in slowing the process of photoaging, reducing oxidative stress and improving the barrier function of the skin [83]. Another research has studied plant extracts fermented with Lactobacillus buchneri for photoaging effect in the in-vitro models [70]. One study shows the use of topical Nitrosomonas eutropha to treat facial wrinkles. The researchers have found a significant improvement in wrinkle-depth severity, hyperpigmentation of the forehead and glabella in the group receiving high topical concentration of the probiotic formula [84].
6.7. Rosacea
Rosacea arises due to overexpression of TLR2 receptors leading to inflammatory reactions and altered skin microbiome [25,26]. Scalp rosacea has been treated using an oral probiotic in addition to doxycycline as antibiotic, however, topical probiotics have not yet been explored for rosacea treatment [50].
7. Marketed Topical Probiotics Skin Care Products
While the use of topical biotherapy dates back to 1912 when the topical application of Lactobacillus bulgaricus improved the conditions such as acne and seborrhea, the skincare industry has recently seen a surge in the topical formulations containing microorganisms [6,19]. Various different skincare products containing probiotics marketed globally are listed in Table 2.
Table 2.
Commercially available skincare products throughout the world.
| Sr. No | Brand/Manufacturer | Type of Skin-Care Product | Probiotic Used | Benefits Claimed |
|---|---|---|---|---|
| 1 | Okana | Eye care serum | Bacillus bacterial ferment extract | Helps skin retain its firmness and elasticity and keeps it feeling smooth and plump. |
| 2 | Amperna | Probiotic+ Ds Soothing Serum | Unique probiotic complex | Soothe irritated skin and calm redness. Tested on eczema, dermatitis, perioral dermatitis, rosacea and acne-prone skin. |
| 3 | Elissah Bio P2 Laviol Skin Care | All in One Essence, triple action, concentrated topical facial serum | 16 types and 35 strains of bacteria including 14 Bifidobacterium and Lactobacilli. | Strengthen the skin’s barrier against environmental threats and reduce the factors that trigger skin sensitivities, redness and irritation. |
| 4 | Probiotic Skin Cream Melvory | Face Cream | Lactobacilli probiotic (Lactobacillus ferment filtrate) | Cleans away the bad bacteria on the skin. For acne-prone or teenage skin |
| 5 | Andalou Brightening Probiotic + C Renewal Cream | Cream | Bacillus coagulans | Skin-friendly vegan probiotic microflora enzymatically supports dermal vitality, targeting over-exposed surface cells for a lighter, tighter, brighter looking appearance and a luminous complexion. |
| 6 | Biossance Squalane + Probiotic Gel | Face moisturizer | Lactococcus ferment lysate | Help restore the skin’s balance and renew the skin barrier |
| 7 | Neogen Dermalogy Probiotics Double Action | Facial Serum | The patented complex of Bifida ferment lysate, Lactobacillus, and Streptococcus thermophilus ferment | Protect the skin barrier |
| 8 | Elemis Dynamic Resurfacing Facial Pads | Facial Pads | Lactococcus ferment lysate | Stimulate skin-cell renewal and reinforce the skin barrier |
| 9 | Missha Time Revolution—The First Treatment Essence Rx | Toner | Bifida ferment lysate | Promotes better product absorption, as well as moisture retention and elasticity of the skin. |
| 10 | Éminence Organic Skin Care Clear Skin Probiotic Masque | Face mask for oily skin | Lactic acid bacteria derived from yogurt | Exfoliates and moisturizes the skin. Improve the skin’s moisture absorption and ward off the signs of aging. Reduce the intensity of wrinkles and tightens pores. |
| 11 | Manyo Factory Bifida Complex Ampoule | Facial serum | Bifida ferment lysate, Bifida ferment filtrate, Lactobacillus ferment lysate, and Lactococcus ferment lysate | Encourages self repair of skin, hydrates, replenishes moisture and prevents aging |
| 12 | La Roche-Posay Lipikar Balm AP+ Intense Repair Moisturizing Cream | Cream for dry skin | APF, a patented version of the waterborne bacteria Vitreoscilla filiformis | Improve severely dry skin and keep it hydrated. |
| 13 | Mother Dirt AO+ Mist |
Toner for oily, acne-prone skin | The soil-derived Nitrosomonas eutropha bacteria | Mist protects and maintains healthy skin by restoring and balancing your microbiome |
| 14 | LaFlore Probiotic Serum Concentrate |
Facial serum for sensitive, irritated, and rosacea-prone skin | Lactococcus ferment lysate and live kefir probiotics (Hansenula/Kloeckera/Lactobacillus/Lactococcus/Leuconostoc/Pediococcus/Saccharomyces) | Helps calm and smooth fine lines and wrinkles and boosts the skin’s natural defense system. |
| 15 | Marie Veronique Pre+Probiotic Daily Mist | Toner for all types of skin | A proprietary microbiotic complex that contains a combination of 34 probiotic live strains including a high concentration of Bifidobacterium | Balances the skin’s microbiota, thereby reducing skin irritations that lead to inflammation |
| 16 | Columbia Skincare Probiotic Concentrate |
Serum for sensitive, irritated, and rosacea-prone skin | Lactococcus ferment lysate | Enhance skin’s immune function |
| 17 | Elizabeth Arden Superstart Probiotic Boost Skin Renewal Biocellulose Mask | Face mask for dull and damaged skin | Lactococcus ferment lysate; inactivated strains of Lactobacillus casei and Lactobacillus acidophilus | Optimizes skin’s microflora and natural defence. Moisturizes and smoothes skin. |
| 18 | Glowbiotics HydraGlow Cream Oil | Hydrating oil for dull, sun-damaged skin | Lactococcus ferment lysate | Stimulates the skin’s renewal process |
| 19 | FCL Pre+ Probiotic Body lotion | Body lotion for skin nutrition, improving skin protective barrier and provides moisture | Probiotic bifido culture | Detoxifies skin, provides natural skin repair, promotes microbiota balance and hydration. |
| 20 | Herbostra Probiotic hand cream | Non-greasy hand cream to overcome dryness | Probiotic enzymes | Moisturizes and nourishes hands, nails, cuticles. Rich and smooth texture with antimicrobial properties keep hands moisturized. |
| 21 | Dot and Key 72 h hydrating gel and Probiotics | Hydrating, oil-free gel for dry parched skin | Saccharomyces black tea ferment, lactobacillus | Provides long hours of moisturization, restores microbiome balance |
| 22 | Tula Instant Depuff eye renewal serum | Balm available as a stick | Yogurt Powder, Algae Extract, Bacillus Ferment, Lactococcus Ferment Lysate | Ideal for aging skin, crow feet near eyes, under-eye dark circles, and eye puffiness. |
| 23 | Ren Perfect Canvas clean primer | Hydrating drops | Lactococcus Ferment Lysate | Minimizes skin pores and fine lines. Creates a base for a perfect make up |
| 24 | Clinique redness solutions daily relief cream. | Oil-free moisturizing cream | Lactobacillus | Restores microbiome and skin barrier, reduces redness and irritation of the skin by calming it. |
| 25 | Pretty pop probiotic power whipped cream | Whipped cream with encapsulated probiotics | Lactobacillus Ferment, Lactococcus Ferment Lysate, Bifida Ferment Lysate, Lactobacillus, Streptococcus thermophilus Ferment, | Treats dryness, wrinkles, fine lines, loss of elasticity and firmness. |
| 26 | Korres Greek Yoghurt Skin nourishing probiotic gel-cream | Gel-cream for dryness and redness of the skin | Lactobacillus, Greek yogurt, yoghurt powder | Nourishes, hydrates and gives a bouncy feeling skin. |
| 27 | Edible beauty probiotic radiance tonic | Serum to soothe skin from redness and irritation | Lactobacillus Ferment Filtrate | Reduces redness, aging effects and irritation of the skin |
| 28 | Glamglow berry glow probiotic recovery mask | Recovery mask packed with super berries and probiotics | Lactobacillus Ferment | Balances and supports skin microbiome, replenishes hydration, and protects skin moisture barrier. |
| 29 | Korres Probiotic Superdose facemask | Facemask containing Greek yoghurt and pre and probiotics | Lactobacillus, Greek yogurt | Nourishes and replenishes the skin, restores microbiome |
| 30 | Beekman 1802 Bloom Cream daily moisturizer | Daily moisturizing cream for glowing radiance | Bifida Ferment Lysate | Microbiome friendly, hydrates skin, gives healthy youthful glowing skin |
| 31 | Kinship Self Reflect Rose Probiotic Moisturizing Sunscreen Zinc Oxide SPF 32 | Probiotic moisturizing sunscreen cream | Lactobacillus Ferment, Plant-based probiotics | Works as a moisturizer, primer and Sunscreen with broad-spectrum UV protection |
| 32 | Clinique Redness Solutions Makeup Broad Spectrum SPF 15 With Probiotic Technology Foundation | Oil-free liquid foundation with SPF | Lactobacillus Ferment | Covers flushing. Blushing, redness and irritation of the skin. Protects against UV radiation |
| 33 | Beekman 1802 Milk Drops Probiotic Ceramide Serum | lightweight probiotic milk serum | Bifida Ferment Lysate | Moisturizes and restores the skin, microbiome friendly formula that boosts the dull skin, cleans pores, helps control oil |
| 34 | Beekman 1802 Mini Milk Wash Exfoliating Jelly Cleanser | a light jelly formula that transforms into a deep-cleansing milk | Bifida Ferment Lysate | Deeply cleanses and exfoliates for clearer, brighter skin, helps control oily skin, clears pores, and fights blemishes |
| 35 | Beekman 1802 Milk Bar Probiotic Facial Cleansing Bar | Solid bar that transforms into foaming cleanser with little water | Bifida Ferment Lysate | Deeply cleanses skin with ultra-foaming lather |
| 36 | Ulta probiotic cream mask | Cream mask | Yogurt Extract, Lactobacillus | Nourishes, clarifies and soothes skin. It also conditions and tones the skin |
| 37 | WLDKAT Prebiotic + Probiotic Pleasure Serum | Water-based intimate serum for vaginal use | Lactobacillus Ferment, | Fights vaginosis, maintains natural moisture, pH, enhances pleasure and has antibacterial properties |
| 38 | Skyn Iceland Nordic Renewal Pre + Probiotic Cream Starter Set | Pre + Probiotic Cream | three potent fermented extracts of probiotics | Skin renewal, enhances skin microbiome, deeply nourishes and moisturizes |
| 39 | Boscia Prebiotic + Probiotic Freshening All-Over Body Deodorant | Body deodorant | Lactococcus Ferment Lysate | Neutralizes odor, restores skin balance, combats wetness and soothes for clean, long-lasting protection |
| 40 | Pacifica Sun + Skincare Mineral Face Shade Coconut Probiotic SPF 30 | Moisturizing face lotion that applies evenly and leaves skin hydrated | Lactococcus Ferment Lysate | Provides water-resistant protection with a sheer application. |
8. Recent Novel Approach in Topical Probiotics: Probiotic Coated Apparels
The hospital clothes, aprons, gowns, and other apparel worn by the hospital staff and patients are contaminated with microorganisms which increases the chances of hospital-acquired infections. Although the incorporation of antimicrobials has been used in wash liquids to kill the pathogens in the clothes, the use of probiotics in hospital clothing is a novel approach in using topical probiotics for skin infections and conditions. In one such study, the researchers have incorporated probiotics in the form of paste in the fabric of the hospital apparel that stayed even after five washes. Including probiotics in hospital linens and uniforms may protect against infections [85]. Another study successfully demonstrated probiotics printing using a paste containing probiotic spores on a polyester fabric. The probiotic printed fabric had higher contact angles and lower wettability [86].
Such clothing with probiotics embedded in the fabric may be the future of functional clothing to combat nosocomial pathogens and to treat infections. While it positively interacts with the skin microbiome, it also helps in keeping pathogens at bay and helps to handle skin odor, skin conditions and infections [87].
9. Regulatory Aspects of Probiotics in Topical Skin Care and the Challenges
Since there are several potential applications for probiotics in management of skin related disorders, a proper regulation of the labelling and marketing standards is essential. Almost all of the probiotic-containing topical formulations have yet not gone beyond the personal care product category. Additionally, these topical care products are non-sterile and may contain antimicrobial preservatives that may affect the probiotic strain viability and further alter the microbiota of the recipient in an already diseased state [84]. Therefore, regulations of probiotics primarily need to be concerned with safety. At present, there are no specific guidelines for commercializing probiotics, and products are regulated according to their final use either as a drug, medical device, food, dietary supplement, or cosmetic. Probiotic-based products with health claims could be notified as pharmaceuticals or medicines [88]. If the product contains non-viable microorganisms, it will be considered as a medical device. Probiotic skin care products are a very recent innovation and there is a lack of scientifically validated clinical data about the efficacy and safety of topically applied probiotics. Additionally, the sharp demarcation between foods, drugs, and cosmetics, makes the development and notification of probiotic cosmetic products a challenge.
Topically applied products are not produced in sterile conditions and hence a sterility test is not required. These products often contain preservatives to control the growth of microbes. These preservatives can potentially affect the probiotic strain viability and also inadvertently alter the microbiota of the recipient [19]. Probiotic-containing topical formulations have yet not gone beyond the personal care product category; since they have high load of colony forming units, it is difficult for such preparations to pass the USFDA regulatory requirements for microbial load. Preservative effectiveness test is a major hurdle in testing these products. Topical probiotic formulations for treating acne were tested for microbial enumeration testing as per United States Pharmacopoeia (USP). It was found that topical products do not contain “objectionable” quantity of live microorganism and hence is not required to be below 1000 CFU as per USP [60].
Performing the bacterial challenge test is a big challenge for preparations containing live bacteria. In 1 particular study, blank formulations were put through challenge tests for 14 and 28 days. The blank formulation showed a decreased load of inoculated bacteria and no increase in yeast or mould after 14th and 28th day of challenge test. The results proved that in that particular formulation, low water activity is a reason for self-preservation of the formulation and no external preservative is needed [89].
10. Concluding Remarks
In recent years, significant advances have been made in understanding the composition of the skin-microbiome and how the dysbiosis affects the skin health. Topical probiotics in the form of various dermatological formulations are an important part of the treatment of skin conditions. While the skin microbiome, its functions and protective nature maintain the skin homeostasis, an imbalance results in inflammatory skin conditions that are difficult to get completely cured by conventional treatments. Several clinical trials are being carried out in order to study the efficacy as well as the adverse effects of topical probiotic formulations for the treatment of conditions such as atopic dermatitis, acne, psoriasis, wound healing and many other skin problems. We hope that this review forms a contribution to promoting enhanced research activities in the field of topical probiotics as a novel therapeutic approach for the treatment of skin disorders.
Acknowledgments
Authors thanks Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia for supporting for this project.
Author Contributions
Conceptualization, M.H., P.N.S., R.K.K., S.N., S.M.B.A., M.K.A., S.F.; writing—original draft preparation, M.H., P.N.S., R.K.K., M.K.A., S.F.; writing—review and editing, M.H., R.K.K., S.N., S.M.B.A., M.K.A., S.F. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported through the Annual Funding track by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia [Project No. AN000149].
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.França K. Topical Probiotics in Dermatological Therapy and Skincare: A Concise Review. Dermatol. Ther. 2021;11:71–77. doi: 10.1007/s13555-020-00476-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Navarro-López V., Núñez-Delegido E., Ruzafa-Costas B., Sánchez-Pellicer P., Agüera-Santos J., Navarro-Moratalla L. Probiotics in the Therapeutic Arsenal of Dermatologists. Microorganisms. 2021;9:1513. doi: 10.3390/microorganisms9071513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roudsari M.R., Karimi R., Sohrabvandi S., Mortazavian A.M. Health effects of probiotics on the skin. Crit. Rev. Food Sci. Nutr. 2015;55:1219–1240. doi: 10.1080/10408398.2012.680078. [DOI] [PubMed] [Google Scholar]
- 4.Szántó M., Dózsa A., Antal D., Szabó K., Kemény L., Bai P. Targeting the gut-skin axis-Probiotics as new tools for skin disorder management? Exp. Dermatol. 2019;28:1210–1218. doi: 10.1111/exd.14016. [DOI] [PubMed] [Google Scholar]
- 5.Al-Ghazzewi F.H., Tester R.F. Impact of prebiotics and probiotics on skin health. Benef. Microbes. 2014;5:99–107. doi: 10.3920/BM2013.0040. [DOI] [PubMed] [Google Scholar]
- 6.Lee G.R., Maarouf M., Hendricks A.J., Lee D.E., Shi V.Y. Topical probiotics: The unknowns behind their rising popularity. Dermatol. Online J. 2019;25:15–21. doi: 10.5070/D3255044062. [DOI] [PubMed] [Google Scholar]
- 7.Dréno B., Araviiskaia E., Berardesca E., Gontijo G., Sanchez Viera M., Xiang L.F., Martin R., Bieber T. Microbiome in healthy skin, update for dermatologists. J. Eur. Acad. Dermatol. Venereol. 2016;30:2038–2047. doi: 10.1111/jdv.13965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grice E.A., Segre J.A. The skin microbiome. Nat. Rev. Microbiol. 2011;9:244–253. doi: 10.1038/nrmicro2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Litwin D., WenChieh C., Dzika E., Korycińska J. Human permanent ectoparasites; recent advances on biology and clinical significance of Demodex mites: Narrative review article. Iran. J. Parasitol. 2017;12:12. [PMC free article] [PubMed] [Google Scholar]
- 10.Schommer N.N., Gallo R.L. Structure and function of the human skin microbiome. Trends Microbiol. 2013;21:660–668. doi: 10.1016/j.tim.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egert M., Simmering R. The microbiota of the human skin. Microbiota Hum. Body. 2016;902:61–81. doi: 10.1007/978-3-319-31248-4_5. [DOI] [PubMed] [Google Scholar]
- 12.Byrd A.L., Belkaid Y., Segre J.A. The human skin microbiome. Nat. Rev. Microbiol. 2018;16:143–155. doi: 10.1038/nrmicro.2017.157. [DOI] [PubMed] [Google Scholar]
- 13.Scharschmidt T.C., Fischbach M.A. What lives on our skin: Ecology, genomics and therapeutic opportunities of the skin microbiome. Drug Discov. Today Dis. Mech. 2013;10:e83–e89. doi: 10.1016/j.ddmec.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakatsuji T., Gallo R.L. The role of the skin microbiome in atopic dermatitis. Ann. Allergy Asthma Immunol. 2019;122:263–269. doi: 10.1016/j.anai.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gibbs N.K., Norval M. Urocanic acid in the skin: A mixed blessing? J. Investig. Dermatol. 2011;131:14–17. doi: 10.1038/jid.2010.276. [DOI] [PubMed] [Google Scholar]
- 16.Nakatsuji T., Chen T.H., Butcher A.M., Trzoss L.L., Nam S.-J., Shirakawa K.T., Zhou W., Oh J., Otto M., Fenical W. A commensal strain of Staphylococcus epidermidis protects against skin neoplasia. Sci. Adv. 2018;4:eaao4502. doi: 10.1126/sciadv.aao4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sfriso R., Egert M., Gempeler M., Voegeli R., Campiche R. Revealing the secret life of skin-with the microbiome you never walk alone. Int. J. Cosmet. Sci. 2020;42:116–126. doi: 10.1111/ics.12594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barankin B., DeKoven J. Psychosocial effect of common skin diseases. Can. Fam. Physician. 2002;48:712–716. [PMC free article] [PubMed] [Google Scholar]
- 19.Puebla-Barragan S., Reid G. Probiotics in cosmetic and personal care products: Trends and challenges. Molecules. 2021;26:1249. doi: 10.3390/molecules26051249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borse V.A., Gangude A.B., Deore A.B. Formulation and Evaluation of Antibacterial Topical Gel of Doxycycline Hyclate, Neem Oil and Tea Tree Oil. Indian J. Pharm. Educ. Res. 2020;54:206–212. doi: 10.5530/ijper.54.1.24. [DOI] [Google Scholar]
- 21.Goodarzi A., Mozafarpoor S., Bodaghabadi M., Mohamadi M. The potential of probiotics for treating acne vulgaris: A review of literature on acne and microbiota. Dermatol. Ther. 2020;33:e13279. doi: 10.1111/dth.13279. [DOI] [PubMed] [Google Scholar]
- 22.Dréno B., Pécastaings S., Corvec S., Veraldi S., Khammari A., Roques C. Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: A brief look at the latest updates. J. Eur. Acad. Dermatol. Venereol. 2018;32:5–14. doi: 10.1111/jdv.15043. [DOI] [PubMed] [Google Scholar]
- 23.Elston M.J., Dupaix J.P., Opanova M.I., Atkinson R.E. Cutibacterium acnes (formerly Proprionibacterium acnes) and shoulder surgery. Hawaii J. Health Soc. Welf. 2019;78:3. [PMC free article] [PubMed] [Google Scholar]
- 24.Rocha M., Bagatin E. Skin barrier and microbiome in acne. Arch. Dermatol. Res. 2018;310:181–185. doi: 10.1007/s00403-017-1795-3. [DOI] [PubMed] [Google Scholar]
- 25.Knackstedt R., Knackstedt T., Gatherwright J. The role of topical probiotics in skin conditions: A systematic review of animal and human studies and implications for future therapies. Exp. Dermatol. 2020;29:15–21. doi: 10.1111/exd.14032. [DOI] [PubMed] [Google Scholar]
- 26.Knackstedt R., Knackstedt T., Gatherwright J. The role of topical probiotics on wound healing: A review of animal and human studies. Int. Wound J. 2020;17:1687–1694. doi: 10.1111/iwj.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rożalski M., Rudnicka L., Samochocki Z. Atopic and non-atopic eczema. Acta Dermatovenerol. Croat. 2016;24:110. [PubMed] [Google Scholar]
- 28.Pothmann A., Illing T., Wiegand C., Hartmann A.A., Elsner P. The microbiome and atopic dermatitis: A review. Am. J. Clin. Dermatol. 2019;20:749–761. doi: 10.1007/s40257-019-00467-1. [DOI] [PubMed] [Google Scholar]
- 29.Baldwin H., Aguh C., Andriessen A., Benjamin L., Ferberg A.S., Hooper D., Jarizzo J.L., Lio P.A., Tlougan B., Woolery-Lloyd H.C. Atopic Dermatitis and the Role of the Skin Microbiome in Choosing Prevention, Treatment, and Maintenance Options. J. Drugs Dermatol. 2020;19:935–940. doi: 10.36849/JDD.2020.5393. [DOI] [PubMed] [Google Scholar]
- 30.Paller A.S., Kong H.H., Seed P., Naik S., Scharschmidt T.C., Gallo R.L., Luger T., Irvine A.D. The microbiome in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2019;143:26–35. doi: 10.1016/j.jaci.2018.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morelli P., Gaspari M., Gabriele C., Dastoli S., Bennardo L., Pavel A.B., Patruno C., Del Duca E., Nisticò S.P. Proteomic analysis from skin swabs reveals a new set of proteins identifying skin impairment in atopic dermatitis. Exp. Dermatol. 2021;30:811–819. doi: 10.1111/exd.14276. [DOI] [PubMed] [Google Scholar]
- 32.Nguyen A.V., Soulika A.M. The Dynamics of the Skin’s Immune System. Int. J. Mol. Sci. 2019;20:1811. doi: 10.3390/ijms20081811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olesen C.M., Ingham A.C., Thomsen S.F., Clausen M.-L., Andersen P.S., Edslev S.M., Yüksel Y.T., Guttman-Yassky E., Agner T. Changes in Skin and Nasal Microbiome and Staphylococcal Species Following Treatment of Atopic Dermatitis with Dupilumab. Microorganisms. 2021;9:1487. doi: 10.3390/microorganisms9071487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Albarraq A.A., Alqahtani S.S., Ahmad S., Banji D. Prevalence and Pharmacotherapeutic Management of Pediatric Psoriasis–A Descriptive Review. Indian J. Pharm. Educ. Res. 2019;53:569–576. doi: 10.5530/ijper.53.4.118. [DOI] [Google Scholar]
- 35.Mestry M., Rane M., Bajaj A. Commiphora mukul and Quercetin Loaded Liposphere Gel: Potential Treatment for Psoriasis. Indian J. Pharm. Educ. Res. 2020;54:654–667. doi: 10.5530/ijper.54.3.115. [DOI] [Google Scholar]
- 36.Thio H.B. The microbiome in psoriasis and psoriatic arthritis: The skin perspective. J. Rheumatol. Suppl. 2018;94:30–31. doi: 10.3899/jrheum.180133. [DOI] [PubMed] [Google Scholar]
- 37.Greb J.E., Goldminz A.M., Elder J.T., Lebwohl M.G., Gladman D.D., Wu J.J., Mehta N.N., Finlay A.Y., Gottlieb A.B. Psoriasis. Nat. Rev. Dis. Primers. 2016;2:1–17. doi: 10.1038/nrdp.2016.82. [DOI] [PubMed] [Google Scholar]
- 38.Chen Y.H., Wu C.S., Chao Y.H., Lin C.C., Tsai H.Y., Li Y.R., Chen Y.Z., Tsai W.H., Chen Y.K. Lactobacillus pentosus GMNL-77 inhibits skin lesions in imiquimod-induced psoriasis-like mice. J. Food Drug Anal. 2017;25:559–566. doi: 10.1016/j.jfda.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nermes M., Kantele J.M., Atosuo T.J., Salminen S., Isolauri E. Interaction of orally administered Lactobacillus rhamnosus GG with skin and gut microbiota and humoral immunity in infants with atopic dermatitis. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2011;41:370–377. doi: 10.1111/j.1365-2222.2010.03657.x. [DOI] [PubMed] [Google Scholar]
- 40.Vijayashankar M., Raghunath N. Pustular psoriasis responding to probiotics–A new insight. Our Dermatol. Online. 2012;3:326. doi: 10.7241/ourd.20124.71. [DOI] [Google Scholar]
- 41.Rather I.A., Bajpai V.K., Huh Y.S., Han Y.-K., Bhat E.A., Lim J., Paek W.K., Park Y.-H. Probiotic Lactobacillus sakei proBio-65 extract ameliorates the severity of imiquimod induced psoriasis-like skin inflammation in a mouse model. Front. Microbiol. 2018;9:1021. doi: 10.3389/fmicb.2018.01021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buddenkotte J., Steinhoff M. Recent advances in understanding and managing rosacea. F1000Research. 2018;7:1885. doi: 10.12688/f1000research.16537.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahn C.S., Huang W.W. Rosacea Pathogenesis. Dermatol. Clin. 2018;36:81–86. doi: 10.1016/j.det.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 44.Murillo N., Raoult D. Skin microbiota: Overview and role in the skin diseases acne vulgaris and rosacea. Future Microbiol. 2013;8:209–222. doi: 10.2217/fmb.12.141. [DOI] [PubMed] [Google Scholar]
- 45.De Pessemier B., Grine L., Debaere M., Maes A., Paetzold B., Callewaert C. Gut-Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms. 2021;9:353. doi: 10.3390/microorganisms9020353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Woo Y.R., Lee S.H., Cho S.H., Lee J.D., Kim H.S. Characterization and Analysis of the Skin Microbiota in Rosacea: Impact of Systemic Antibiotics. J. Clin. Med. 2020;9:185. doi: 10.3390/jcm9010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Daou H., Paradiso M., Hennessy K., Seminario-Vidal L. Rosacea and the Microbiome: A Systematic Review. Dermatol. Ther. 2021;11:1–12. doi: 10.1007/s13555-020-00460-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Searle T., Ali F.R., Carolides S., Al-Niaimi F. Rosacea and the gastrointestinal system. Australas. J. Dermatol. 2020;61:307–311. doi: 10.1111/ajd.13401. [DOI] [PubMed] [Google Scholar]
- 49.Costa C.P., Kirschning C.J., Busch D., Dürr S., Jennen L., Heinzmann U., Prebeck S., Wagner H., Miethke T. Role of chlamydial heat shock protein 60 in the stimulation of innate immune cells by Chlamydia pneumoniae. Eur. J. Immunol. 2002;32:2460–2470. doi: 10.1002/1521-4141(200209)32:9<2460::AID-IMMU2460>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 50.Fortuna M.C., Garelli V., Pranteda G., Romaniello F., Cardone M., Carlesimo M., Rossi A. A case of Scalp Rosacea treated with low dose doxycycline and probiotic therapy and literature review on therapeutic options. Dermatol. Ther. 2016;29:249–251. doi: 10.1111/dth.12355. [DOI] [PubMed] [Google Scholar]
- 51.DeAngelis Y.M., Gemmer C.M., Kaczvinsky J.R., Kenneally D.C., Schwartz J.R., Dawson T.L., Jr. Three etiologic facets of dandruff and seborrheic dermatitis: Malassezia fungi, sebaceous lipids, and individual sensitivity. J. Investig. Dermatol. Symp. Proc. 2005;10:295–297. doi: 10.1111/j.1087-0024.2005.10119.x. [DOI] [PubMed] [Google Scholar]
- 52.Castiel I., Gueniche A. Cosmetic and Dermatological Use of Probiotic Lactobacillus paracasei Microorganisms for the Treatment of Greasy Scalp Disorders (Kosmetische und Dermatologische Verwendung von Probiotischen Lactobacillus paracasei. EP2149368B1. European Patent. 2018 May 30;
- 53.Bowe W.P., Filip J.C., DiRienzo J.M., Volgina A., Margolis D.J. Inhibition of propionibacterium acnes by bacteriocin-like inhibitory substances (BLIS) produced by Streptococcus salivarius. J. Drugs Dermatol. 2006;5:868–870. [PMC free article] [PubMed] [Google Scholar]
- 54.Bowe W.P., Logan A.C. Acne vulgaris, probiotics and the gut-brain-skin axis-back to the future? Gut Pathog. 2011;3:1. doi: 10.1186/1757-4749-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim B.-J., Lee S.-Y., Kim H.-B., Lee E., Hong S.-J. Environmental changes, microbiota, and allergic diseases. Allergy Asthma Immunol. Res. 2014;6:389–400. doi: 10.4168/aair.2014.6.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hidalgo-Cantabrana C., Gómez J., Delgado S., Requena-López S., Queiro-Silva R., Margolles A., Coto E., Sánchez B., Coto-Segura P. Gut microbiota dysbiosis in a cohort of patients with psoriasis. Br. J. Dermatol. 2019;181:1287–1295. doi: 10.1111/bjd.17931. [DOI] [PubMed] [Google Scholar]
- 57.Nam J.H., Yun Y., Kim H.S., Kim H.N., Jung H.J., Chang Y., Ryu S., Shin H., Kim H.L., Kim W.S. Rosacea and its association with enteral microbiota in Korean females. Exp. Dermatol. 2018;27:37–42. doi: 10.1111/exd.13398. [DOI] [PubMed] [Google Scholar]
- 58.Yu Y., Dunaway S., Champer J., Kim J., Alikhan A. Changing our microbiome: Probiotics in dermatology. Br. J. Dermatol. 2020;182:39–46. doi: 10.1111/bjd.18659. [DOI] [PubMed] [Google Scholar]
- 59.Bindurani S. Probiotics in dermatology. J. Ski. Sex. Transm. Dis. 2019;1:66–71. [Google Scholar]
- 60.Osborne D., Tan P., Varma Y., Carbol J. Formulating topical products containing live microorganisms as the active ingredient. Pharm. Technol. 2018;42:32–36. [Google Scholar]
- 61.Blanchet-Réthoré S., Bourdès V., Mercenier A., Haddar C.H., Verhoeven P.O., Andres P. Effect of a lotion containing the heat-treated probiotic strain Lactobacillus johnsonii NCC 533 on Staphylococcus aureus colonization in atopic dermatitis. Clin. Cosmet. Investig. Dermatol. 2017;10:249. doi: 10.2147/CCID.S135529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Myles I.A., Williams K.W., Reckhow J.D., Jammeh M.L., Pincus N.B., Sastalla I., Saleem D., Stone K.D., Datta S.K. Transplantation of human skin microbiota in models of atopic dermatitis. JCI Insight. 2016;1:e86955. doi: 10.1172/jci.insight.86955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jeong J.H., Lee C.Y., Chung D.K. Probiotic Lactic Acid Bacteria and Skin Health. Crit. Rev. Food Sci. Nutr. 2016;56:2331–2337. doi: 10.1080/10408398.2013.834874. [DOI] [PubMed] [Google Scholar]
- 64.Di Marzio L., Centi C., Cinque B., Masci S., Giuliani M., Arcieri A., Zicari L., De Simone C., Cifone M.G. Effect of the lactic acid bacterium Streptococcus thermophilus on stratum corneum ceramide levels and signs and symptoms of atopic dermatitis patients. Exp. Dermatol. 2003;12:615–620. doi: 10.1034/j.1600-0625.2003.00051.x. [DOI] [PubMed] [Google Scholar]
- 65.Di Marzio L., Cinque B., Cupelli F., De Simone C., Cifone M.G., Giuliani M. Increase of skin-ceramide levels in aged subjects following a short-term topical application of bacterial sphingomyelinase from Streptococcus thermophilus. Int. J. Immunopathol. Pharmacol. 2008;21:137–143. doi: 10.1177/039463200802100115. [DOI] [PubMed] [Google Scholar]
- 66.Di Marzio L., Cinque B., De Simone C., Cifone M.G. Effect of the lactic acid bacterium Streptococcus thermophilus on ceramide levels in human keratinocytes in vitro and stratum corneum in vivo. J. Investig. Dermatol. 1999;113:98–106. doi: 10.1046/j.1523-1747.1999.00633.x. [DOI] [PubMed] [Google Scholar]
- 67.Lee Y.B., Byun E.J., Kim H.S. Potential Role of the Microbiome in Acne: A Comprehensive Review. J. Clin. Med. 2019;8:987. doi: 10.3390/jcm8070987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pavicic T., Wollenweber U., Farwick M., Korting H.C. Anti-microbial and -inflammatory activity and efficacy of phytosphingosine: An in vitro and in vivo study addressing acne vulgaris. Int. J. Cosmet. Sci. 2007;29:181–190. doi: 10.1111/j.1467-2494.2007.00378.x. [DOI] [PubMed] [Google Scholar]
- 69.Al-Ghazzewi F.H., Tester R.F. Effect of konjac glucomannan hydrolysates and probiotics on the growth of the skin bacterium Propionibacterium acnes in vitro. Int. J. Cosmet. Sci. 2010;32:139–142. doi: 10.1111/j.1468-2494.2009.00555.x. [DOI] [PubMed] [Google Scholar]
- 70.Kang B.S., Seo J.G., Lee G.S., Kim J.H., Kim S.Y., Han Y.W., Kang H., Kim H.O., Rhee J.H., Chung M.J., et al. Antimicrobial activity of enterocins from Enterococcus faecalis SL-5 against Propionibacterium acnes, the causative agent in acne vulgaris, and its therapeutic effect. J. Microbiol. 2009;47:101–109. doi: 10.1007/s12275-008-0179-y. [DOI] [PubMed] [Google Scholar]
- 71.Cosseau C., Devine D.A., Dullaghan E., Gardy J.L., Chikatamarla A., Gellatly S., Yu L.L., Pistolic J., Falsafi R., Tagg J., et al. The commensal Streptococcus salivarius K12 downregulates the innate immune responses of human epithelial cells and promotes host-microbe homeostasis. Infect. Immun. 2008;76:4163–4175. doi: 10.1128/IAI.00188-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lopes E.G., Moreira D.A., Gullón P., Gullón B., Cardelle-Cobas A., Tavaria F.K. Topical application of probiotics in skin: Adhesion, antimicrobial and antibiofilm in vitro assays. J. Appl. Microbiol. 2017;122:450–461. doi: 10.1111/jam.13349. [DOI] [PubMed] [Google Scholar]
- 73.Ambrożej D., Kunkiel K., Dumycz K., Feleszko W. The use of probiotics and bacteria-derived preparations in topical treatment of atopic dermatitis-A systematic review. J. Allergy Clin. Immunol. Pract. 2021;9:570–575. doi: 10.1016/j.jaip.2020.07.051. [DOI] [PubMed] [Google Scholar]
- 74.Guéniche A., Cathelineau A.C., Bastien P., Esdaile J., Martin R., Queille Roussel C., Breton L. Vitreoscilla filiformis biomass improves seborrheic dermatitis. J. Eur. Acad. Dermatol. Venereol. JEADV. 2008;22:1014–1015. doi: 10.1111/j.1468-3083.2007.02508.x. [DOI] [PubMed] [Google Scholar]
- 75.Park S.B., Im M., Lee Y., Lee J.H., Lim J., Park Y.H., Seo Y.J. Effect of emollients containing vegetable-derived lactobacillus in the treatment of atopic dermatitis symptoms: Split-body clinical trial. Ann. Dermatol. 2014;26:150–155. doi: 10.5021/ad.2014.26.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Myles I.A., Castillo C.R., Barbian K.D., Kanakabandi K., Virtaneva K., Fitzmeyer E., Paneru M., Otaizo-Carrasquero F., Myers T.G., Markowitz T.E., et al. Therapeutic responses to Roseomonas mucosa in atopic dermatitis may involve lipid-mediated TNF-related epithelial repair. Sci. Transl. Med. 2020;12:eaaz8631. doi: 10.1126/scitranslmed.aaz8631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Guéniche A., Hennino A., Goujon C., Dahel K., Bastien P., Martin R., Jourdain R., Breton L. Improvement of atopic dermatitis skin symptoms by Vitreoscilla filiformis bacterial extract. Eur. J. Dermatol. EJD. 2006;16:380–384. [PubMed] [Google Scholar]
- 78.Volz T., Skabytska Y., Guenova E., Chen K.M., Frick J.S., Kirschning C.J., Kaesler S., Röcken M., Biedermann T. Nonpathogenic bacteria alleviating atopic dermatitis inflammation induce IL-10-producing dendritic cells and regulatory Tr1 cells. J. Investig. Dermatol. 2014;134:96–104. doi: 10.1038/jid.2013.291. [DOI] [PubMed] [Google Scholar]
- 79.Reygagne P., Bastien P., Couavoux M.P., Philippe D., Renouf M., Castiel-Higounenc I., Gueniche A. The positive benefit of Lactobacillus paracasei NCC2461 ST11 in healthy volunteers with moderate to severe dandruff. Benef. Microbes. 2017;8:671–680. doi: 10.3920/BM2016.0144. [DOI] [PubMed] [Google Scholar]
- 80.Foligné B., Dewulf J., Breton J., Claisse O., Lonvaud-Funel A., Pot B. Probiotic properties of non-conventional lactic acid bacteria: Immunomodulation by Oenococcus oeni. Int. J. Food Microbiol. 2010;140:136–145. doi: 10.1016/j.ijfoodmicro.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 81.Nayak B.S., Marshall J.R., Isitor G. Wound healing potential of ethanolic extract of Kalanchoe pinnata Lam. leaf--a preliminary study. Indian J. Exp. Biol. 2010;48:572–576. [PubMed] [Google Scholar]
- 82.Malic S., Hill K.E., Playle R., Thomas D.W., Williams D.W. In vitro interaction of chronic wound bacteria in biofilms. J. Wound Care. 2011;20:569–577. doi: 10.12968/jowc.2011.20.12.569. [DOI] [PubMed] [Google Scholar]
- 83.Sharma D., Kober M.M., Bowe W.P. Anti-Aging Effects of Probiotics. J. Drugs Dermatol. 2016;15:9–12. [PubMed] [Google Scholar]
- 84.Notay M., Saric-Bosanac S., Vaughn A.R., Dhaliwal S., Trivedi M., Reiter P.N., Rybak I., Li C.C., Weiss L.B., Ambrogio L., et al. The use of topical Nitrosomonas eutropha for cosmetic improvement of facial wrinkles. J. Cosmet. Dermatol. 2020;19:689–693. doi: 10.1111/jocd.13060. [DOI] [PubMed] [Google Scholar]
- 85.Niehaus K.-L., Dural-Erem A., Nierstrasz V.A. Probiotic printed PET fabrics for biocontrol in hospital textiles. Tekst. Konfeksiyon. 2018;28:195–198. [Google Scholar]
- 86.Erem A.D., Niehaus K.-L., Nierstrasz V. Development of Probiotic Printings for Polyester Fabrics. Tekst. Mühendis. 2018;25:208–213. doi: 10.7216/1300759920182511104. [DOI] [Google Scholar]
- 87.Broadhead R., Craeye L., Callewaert C. The Future of Functional Clothing for an Improved Skin and Textile Microbiome Relationship. Microorganisms. 2021;9:1192. doi: 10.3390/microorganisms9061192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Von Wright A. Regulatory Aspects of Probiotics and Other Microbial Products Intended for Skin Care: The European Approach. Ski. Microbiome Handb. Basic Res. Prod. Dev. 2020:321–341. [Google Scholar]
- 89.Sharma G., Sharma M., Sood R., Neelamraju J., Lakshmi S.G., Madempudi R.S., Rishi P., Kaur I.P. Self-preserving gelatin emulgel containing whole cell probiotic for topical use: Preclinical safety, efficacy, and germination studies. Expert Opin. Drug Deliv. 2021;18:1777–1789. doi: 10.1080/17425247.2021.1947239. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.