Abstract
COVID-19 is a life-threatening contagious virus that has spread across the globe rapidly. To reduce the outbreak impact of COVID-19 virus illness, continual identification and remote surveillance of patients are essential. Medical service delivery based on the Internet of Things (IoT) technology backed up by the fog-cloud paradigm is an efficient and time-sensitive solution for remote patient surveillance. Conspicuously, a comprehensive framework based on Radio Frequency Identification Device (RFID) and body-wearable sensor technologies supported by the fog-cloud platform is proposed for the identification and management of COVID-19 patients. The J48 decision tree is used to assess the infection degree of the user based on corresponding symptoms. RFID is used to detect Temporal Proximity Interactions (TPI) among users. Using TPI quantification, Temporal Network Analysis is used to analyze and track the current stage of the COVID-19 spread. The statistical performance and accuracy of the framework are assessed by utilizing synthetically-generated data for 250,000 users. Based on the comparative analysis, the proposed framework acquired an enhanced measure of classification accuracy, and sensitivity of 96.68% and 94.65% respectively. Moreover, significant improvement has been registered for proposed fog-cloud-based data analysis in terms of Temporal Delay efficacy, Precision, and F-measure.
Keywords: COVID-19, Intelligent framework, Temporal analysis, Self organized mapping
1. Introduction
The spread of infectious diseases such as SARS-CoV-2, MERS, West-Nile has become one of the critical concerns confronted by the modern healthcare industry. Factually, nearly $10,586 per person is spent by the USA on healthcare annually, followed by Switzerland ($7317) and Norway ($6187).1 Presently, COVID-19 is one of the deadliest and most contagious viruses that has spread and affected a significant number of people globally. The COVID-19 outbreak has high pandemic potential due to an increase in the number of COVID-19 patients and transmission from one nation to another [1]. The COVID-19 infection produces a severe viral hemorrhagic fever and other symptoms such as respiratory discomfort, nausea, anorexia, stomach discomfort, headache, and sore throat [2]. The detailed symptoms-based comparison of several overlapping diseases is presented in Table 1 . The incubation period for COVID-19 ranges from 1 to 14 days, averaging 5 days. Moreover, the new COVID-19 variants of Delta (B.1.617.2) have an incubation period of 4 days, and Omicron (B1.1.1.529) has an incubation period of 2 days as per South Africa and UK studies.2 According to the WHO Coronavirus report, “globally, as of 1 March 2022, there have been 437,346,293 confirmed cases of COVID-19, including 5,975,535 deaths”.3 The detailed geographical distribution of confirmed cases is depicted in Fig. 1 .
Table 1.
Symptoms-based analysis (1 high, 11 very high, 111 very high, 0 low).
| Symptoms | West Nile | Japanese virus | COVID-19 |
|---|---|---|---|
| Fever | 111 | 111 (high fever) | 111 |
| Head ache | 111 | 111 | 111 |
| Confusion/disorientation | 111 | 111 | 111 |
| Loss of memory | 0 | 11 | 11 |
| Muscle and joint pain | 11 | 11 | 111 (severe) |
| Coma | 111 | 111 | 111 |
| Nausea or vomiting | 111 | 111 | 111 |
| Paralysis | 111 | 111 | 111 |
| Tremors | 111 | 111 | 0 |
| Drowsiness | 111 | 111 | 111 (extreme tiredness) |
| Neck stiffness | 1/0 | 1/0 | 1 |
| Unconsciousness | 1/0 | 11 | 11 |
| Seizures | 0 | 11 | 11 |
| Aversion of bright light | 0 | 0 | 1 |
| Problem with speech or hearing | 0 | 1/− | 11 |
Fig. 1.
COVID-19 confirmed cases over geographical distribution by WHO (as on 10 December 2021).
Moreover, healthcare workers who treat COVID-19 patients may unwittingly get the virus, spreading the infection further. According to Ng et al. [3], healthcare staff is hesitant to associate with COVID-19 patients because of the significant risk of disease. COVID-19 outbreaks in China, USA, and India were the most severe in 2020 and 2021. Till 10 December 2021, the maximal mortality rate is registered for Mexico (7.6%), followed by Bulgaria (4.1%), and Hungary (3.1%).4 However, patients with COVID-19 can be treated with adequate information and therapy. Fig. 2 5 depicts the overview of COVID-19 risk index analysis. The continual monitoring of the pandemic shifts the focus away from the sickness and toward predicting and preventing the virus's spread. As a result, antiviral medications, vaccinations, and IT-based methodologies are required to decrease the virus's detrimental impacts [4]. Henceforth, it becomes indispensable to explore novel technologies of IoT-Fog-Cloud computing to provision individualistic medical-care delivery in real-time.
Fig. 2.
COVID-19 risk index analysis.
1.1. IoT-fog-cloud computing healthcare
Remote identification and prolonged monitoring of patients with infectious disorders have become increasingly vital [5]. Existing healthcare systems cannot effectively handle and monitor such illnesses while maintaining a low-cost [6], [7]. Conspicuously, a comprehensive and effective framework is indispensable to deliver time-sensitive medical service-delivery utilizing Information and Communication Technology (ICT) [8], [9]. Collecting medical data from patients in a time-sensitive manner, demand for massive storage, and enhanced computing for data analysis are some critical hurdles in the global healthcare system [10], [11]. Recent breakthroughs in wireless distributed sensing networks such as the Internet of Things (IoT) and fog-cloud computing have made it feasible to construct an intelligent medical framework that allows for smooth remote monitoring of patients [12], [13]. Fig. 3 depicts an overview of the layered architecture of IoT-Fog-Cloud computing for smart healthcare. Using collaborative IoT-Fog-Cloud technology not only minimizes the number of health personnel needed but also reduces the cost of health-oriented service delivery [14], [15]. Additionally, the incorporation of Artificial Intelligence (AI) technologies for the development of vaccinations for the COVID-19 has significantly boosted the healthcare industry. AI-inspired machine learning approaches, including Random Forest (RF), Recursive Feature Selection (RFE), and Support Vector Machine (SVM) have been incorporated for identifying antigens from protein sequences. Moreover, Deep Convolutional Neural Networks (DCNN) have proven to be an effective tool for the binding prediction of peptides [2]. Furthermore, supervised neural network-driven frameworks have been used to identify potential T-cell epitopes for COVID-19 with 2019-nCoV spike receptor-binding domain [2]. Additionally, deep-learning RNN provided simulated sequences to determine probable solutions for vaccine design [16]. Fog-Cloud computing can provide nearly limitless storage, and analysis of massive data gathered from acquired ambient IoT data [1]. In conjunction with the IoT-Fog-Cloud, Artificial Intelligent techniques of Deep and Machine learning can be used effectively for patient surveillance and assessment in real-time [17]. IoT comprises several compact and lightweight body sensors connected to the patient's body (Wireless Body Area Network (WBAN)) and captures important physiological attributes enlisted in Table 3 that may be utilized for long-term chronic illness monitoring [18]. Sensors generate enormous amounts of data to be stored and analyzed in a time-sensitive manner [19]. Moreover, Fog-Cloud computing offers enormous processing power, scalability, and storage [20]. Conspicuously, by combining IoT-Fog-Cloud computing, RFID, and AI techniques, an effective medical care framework for monitoring and detecting COVID-19 can be implemented [21]. Furthermore, doctors, healthcare organizations, and government agencies can exchange physiological data generated by IoT via fog-cloud computing [22]. The most challenging aspect of healthcare is continual surveillance of infectious illness and real-time intervention. Proximity contacts between infected and uninfected patients must be stopped to limit the spread of the disease [23]. Radio Frequency Identification (RFID) technology is utilized to detect the temporal interactions between patients and users [24]. To save millions of lives, dedicated and scalable resources are necessary to interpret massive sensor data from a widely impacted population in a single geographical region [25].
Fig. 3.
Layered architecture of IoT-fog-cloud computing.
Table 3.
Physiological attributes for COVID-19.
| S. no. | Parameter | Description |
|---|---|---|
| 1 | FCN | Mobile number (family member) |
| 2 | Age | Age of user |
| 3 | Name | Name of user |
| 4 | Mobno | Mobile number (personal) |
| 5 | Gender | Male or female or transgender |
| 6 | Address | Social address |
1.2. Major contribution
The current research aims to present a fog-cloud-based framework for efficiently forecasting and tracking COVID-19 outbreaks in a time-sensitive manner by utilizing the data acquisition efficiency of IoT sensors and data processing platform efficacy of Fog-Cloud computing. Based on the aforementioned aspects, the major contributions of the current research are detailed ahead.
-
1.
A fog-cloud-based scalable and effective monitoring framework is proposed for COVID-19 outbreak assessment in real-time.
-
2.
The presented framework has been proposed by incorporating IoT and RFID technology over the fog-cloud computing paradigm to gather and analyze healthcare data.
-
3.
J48 decision tree has been utilized to categorize patients into different groups. The proposed algorithm is executed regularly to keep track of alterations in the user group.
-
4.
RFID technology has been used to acquire user interactions. The proposed framework generates an alarm message to an uninfected user for preventing contact with the infected user.
-
5.
Temporal Network Analysis (TNA)-based graphical structure has been presented to indicate the interactions between infected and uninfected users. TNA metrics identify affected users or locations implicated in the disease's propagation.
-
6.
Proposed framework's performance is assessed by extensive experimental testing on the Amazon EC2 cloud.
Table 2 provides the details of the nomenclature used in the current article.
Table 2.
Nomenclature used.
| S. no. | Abbreviation | Description |
|---|---|---|
| 1 | WBAN | Wireless Body Area Network |
| 2 | AWS | Amazon web services |
| 3 | UID | Unique Identification number |
| 4 | IoT | Internet of Things |
| 5 | TNA | Temporal Network Analysis |
| 6 | SEIR | Susceptible, Exposed, Infectious, Recovered |
| 7 | TPI | Temporal proximity interaction |
| 8 | GPS | Geographic positioning system |
| 9 | COVID-19 | Coronavirus disease |
1.3. Paper organization
Section 2 explores related research on COVID-19 infection and the utility of IoT-Fog-Cloud technologies to detect and monitor COVID-19 patients. Section 3 proposes a comprehensive framework for monitoring and detecting COVID-19. Section 4 discusses the proposed RFID-based COVID-19 outbreak control mechanism. The experimental findings of the presented framework are presented in Section 5. Finally, Section 6 concludes the paper with future research directions.
2. Related work
The current section reviews some of the vital contributions by the researchers in the current domain of study that indicate the utility of IoT in the prevention of COVID-19 disease. Moreover, a sub-section has been formulated to review intelligent healthcare analysis using the IoT-Fog-Cloud computing platform.
2.1. IoT-based COVID-19 monitoring
IoT technology has been considerably used by researchers for monitoring COVID-19 patients. Rahman et al. [25] proposed an edge computing-based IoT network for effective data management during the COVID-19 pandemic. Specifically, the authors formulated a software-defined networking layer for real-time data assessment from a remote location. Moreover, the authors demonstrated the integration of IoT and Industry 4.0 in the current era of COVID-19. Shariq et al. [33] presented a RFID security technique for IoT-healthcare data of COVID-19 patients. The authors registered a minimal computation overhead compared to the related approaches and concluded that the proposed technique is more resistant to several IoT data attacks and vulnerabilities. Chen et al. [2] surveyed that AI has made significant advances in COVID-19 disease detection and diagnosis, virology and pathogenesis, treatment, and vaccine development. Moreover, the authors have discussed some of the vital issues faced by AI against COVID-19 prediction. De et al. [1] proposed an intelligent framework in which wearable sensors are used to monitor patients with coronavirus illness. The presented technique has been successfully implemented in a Brazilian critical care unit for COVID-19 patients. Chen et al. [11] presented a Disease Diagnosis and Treatment Recommendation System (DDTRS) to optimize the use of current medical technology and the extensive medical knowledge of experienced clinicians. Moreover, a Density-Peaked Clustering Analysis (DPCA) technique for disease-symptom clustering has been developed. Liu et al. [15] developed a new region-to-boundary deep learning model. It begins with the creation of two branches of a U-shaped network that creates the target probabilities. Mukati et al. [34] presented survey research for the exploration of COVID-19 management techniques using IoT technology. Authors have proposed several techniques for identifying and tracking COVID-19 patients using IoT devices and WBAN. The authors concluded that the IoT technology backed up by Fog-Cloud could overcome the limitations faced by the healthcare professional for the management of COVID-19 data. Poongodi et al. [35] proposed a robust and smart healthcare system for enhancing COVID-19 management using IoT technology. The proposed architecture depicted enhanced accuracy compared to the state-of-the-art computing techniques for statistical parameters. Mukherjee et al. [36] presented an interesting approach for predictive analytics for the COVID-19 disease classification using the enhanced KNN technique. The proposed model is based on the mathematical formulation for depicting the prediction procedure. The presented approach registered better performance based on the comparative analysis with state-of-the-art classification techniques. Jung et al. [14] proposed a software-defined networking model for monitoring and tracking information of the COVID-19 patient in real-time using an IoT platform. IoT nodes were used as public nodes for engaging information providers to improve the overall quality of the data. The performance of the proposed model is analyzed in terms of scalability and reliability based on the comparative analysis with state-of-the-art techniques. Moreover, the authors registered a reduced latency delay for the presented technique. Jahmunah et al. [18] conducted a state-of-the-art literature review for contact tracing methods of COVID-19 patients in a time-sensitive manner. Moreover, an intelligent tool has been proposed for tracking purposes, comprising of mobile-phone-based applications and IoT devices to analyze the COVID-19 spread. Enhanced performance was registered for the proposed model compared to the related approach.
2.2. Smart healthcare analysis
Sood and Mahajan [37] proposed an IoT-based algorithm to predict the Chikungunya virus outbreak. Authors presented a symptom-based Zika and West Nile virus investigation. Specifically, authors used a real-time application system to deliver a fuzzy approach for detecting sick persons and sending an alarm message to healthcare practitioners. Bhatia and Sood [38] introduced an intelligent IoT-inspired platform for efficiently analyzing healthcare conditions. The authors presented a 3-level ANN model to assess, and monitor healthcare vitals during regular exercises. Vani and Neeralagi [39] proposed a fuzzy logic-based remote monitoring system that would produce an alarm if any acute illness was discovered. The authors collected data from individuals with chronic conditions using IoT wearable sensor devices, which are forwarded to the fog layer for processing. The authors focused on context-sensitive data to diagnose chronic conditions. Verma and Sood [40] proposed a novel paradigm for monitoring and analyzing patient health state. The presented approach is used to forecast illness severity. For the severity analysis, the authors focused on student health. The authors used the UCI repository for data collection and classification algorithms to predict health vulnerability in the application. Bhatia et al. [41] presented a system for analyzing health status and probabilistic forecasting vulnerability in real-time. To test the applicability of the proposed framework, the authors used IoT sensors-based simulation for 14 days. Sood and Mahajan [42] suggested a unique remote control method for detecting and preventing Mosquito-Borne Diseases (MBD). The authors focused on diagnosing MBD-infected users at an early stage. Data is extracted and collected using an automated keyword extraction technique and an IoT-based device. Information is stored and processed in fog-cloud storage. To distinguish between contagious and non-viral users, a decision tree is utilized. Sareen et al. [43] suggested an IoT and cloud technology paradigm for monitoring and regulating Ebola virus patients based on RFID methods. The data was processed using temporal network analysis. Compared to state-of-the-art models, experimental findings revealed improved accuracy for evaluating the Ebola epidemic. Tuli et al. [44] presented Healthfog, a fog-based intelligent healthcare system that uses deep learning to diagnose cardiovascular problems. The suggested approach efficiently handles patient health data derived from various sensor devices and delivers healthcare services. It is combined with deep learning to create real-time predictive healthcare software. FogBus framework was proposed to test the system in a fog computing environment. The suggested system's efficiency is assessed in terms of power consumption and testing efficiency. Based on the comprehensive literature review, a comparative analysis has been presented in Table 4 to depict the novel aspects of the proposed approach.
Table 4.
State-of-the-art comparison (1 available, 0 not available).
| References | Anjali et al. [26] | Shorfuzzaman et al. [27] | Firouzi et al. [28] | Rajasekar et al. [29] | Lin et al. [30] | Al et al. [31] | Dwivedi et al. [32] | Proposed |
|---|---|---|---|---|---|---|---|---|
| Sensing technology | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Fog computing | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 |
| Quantification | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| Data repository | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 |
| Predictive behavior | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 |
| Temporal analysis | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| Data visualization | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| COVID-19 classification | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Security | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Reliability | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Stability | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
3. Proposed model
Fig. 4 depicts the layered approach for detecting and monitoring COVID-19 outspread. The presented strategy primarily focuses on cloud computing-based continuous remote monitoring of infected patients in real-time.
Fig. 4.
Layered architecture of proposed model.
3.1. Data accumulation layer
The data accumulation layer collects personal information, vital physiological symptoms, and social contact information. Each user must initially register with the system by inputting mobile phone numbers and other personal information. Each user is assigned a unique identifier (UID) used for future conversations. WBAN captures primary symptoms (such as body temperature, and blood pressure) and sends them to a mobile phone via Bluetooth. The acquired data is transferred in real-time to a fog-node server over WiFi or a 4G/5G network. At the same time, users can utilize the mobile application's interface to enter secondary and advanced symptoms. Once the user has registered corresponding symptoms, the data is transferred to the cloud. For data generated by WBAN, a scalable storage solution is presented that can manage large amounts of data efficiently. Table 5 lists the characteristics of COVID-19 symptoms and the replies given by different users. ‘1’ or ‘0’ represents the values associated with specific instances. Primary, secondary, and advanced symptoms are the three types of symptoms. Secondary symptoms may appear in any user, depending on the medical state. A coronavirus replicates in the body and causes progressive symptoms that aggravate a virus-infected patient's health, necessitating rapid hospitalization and treatment. Healthcare staff and uninfected users must take steps to avoid coming into close contact with a user who has advanced symptoms. RFID connected to the user's body captures physical and social contacts between various users. A user's mobile phone with an RFID reader detects the RFID tag and sends the information to the fog node. The aggregated data is uploaded to the cloud via an Android application for in-depth analysis. Table 6 depicts the proximity interaction qualities of several individuals utilized to develop and update the TNA graph. 3 categories of information from the patient are collected in the data collection component: (1) COVID-19 symptoms; (2) Physiological Attributes; and (3) Proximity interactions. The patient's physiological attributes must be kept private. The presented system uses a secret key-based information sharing technique to keep personal information confidential.
Table 5.
COVID-19 symptoms, 0 indicates no or below threshold; 1 indicates yes or above threshold.
| Primary symptoms | Measure | Secondary symptoms | Measure | Advanced symptoms | Measure |
|---|---|---|---|---|---|
| Sore throat | 0/1 | Chest pain | 0/1 | Delirium | 0/1 |
| Fever | 0/1 | Diarrhea | 0/1 | Kidney disease | 0/1 |
| Low immunity level | 0/1 | Weakness | 0/1 | Seizure | 0/1 |
| Severe headache | 0/1 | Skin rash | 0/1 | Lever disease | 0/1 |
| Muscle pain | 0/1 | Vomiting | 0/1 | Loss of consciousness | 0/1 |
| Oxygen level | 0/1 | Watery eyes | 0/1 | Internal bleeding | 0/1 |
| Heart rate | 0/1 | Gastrointestinal | 0/1 | External bleeding | 0/1 |
Table 6.
COVID-19 interaction parameter for closed proximity users.
| S. no. | Parameter | Description |
|---|---|---|
| 1 | UID target | UID of target patient |
| 2 | Category target | Category of target patient as infected or uninfected |
| 3 | End time | End time of interaction |
| 4 | Start time | Start time of interaction |
| 5 | Category source | Category of source patient as infected or uninfected |
| 6 | UID source | UID of source patient |
3.2. Data Classification Layer
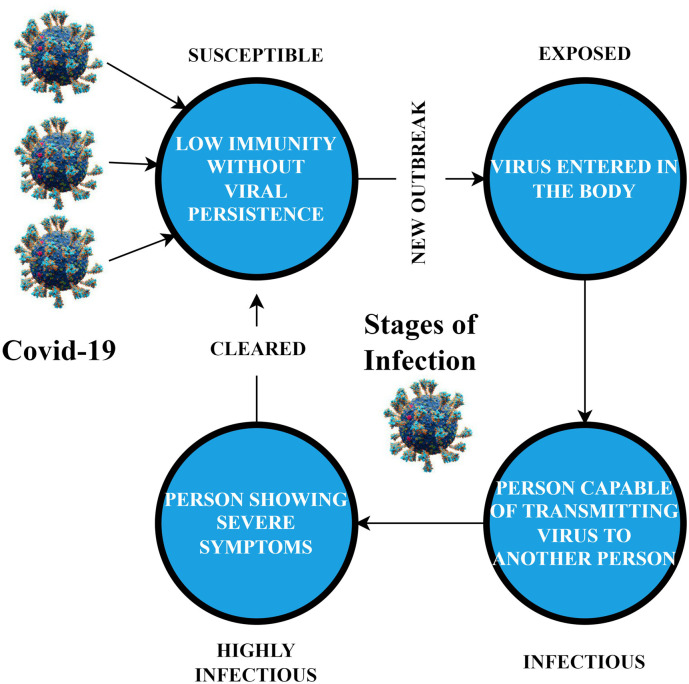
Data Classification Layer is used to classify the user as category U (uninfected), category S (susceptible), category E (exposed), category I (infectious), category H (highly infectious), or category R (recovered) based on COVID-19 attributes data. A decision tree-based technique is utilized to categorize a specific COVID-19 characteristic for predefined output categories. The J48 decision tree is generated using the data-mining program Weka 3.6, which has a variety of machine learning algorithms for data mining applications. Each user is classified as infected under category S if he has no illness, low-level immunity, and a cough or sore throat. The infected patient's category E symptoms include a slight fever, cough, and sore throat. The degree of infection in the patient's body is minimal during the initial period. Suppose the patient has a high fever, sore throat, and secondary symptoms such as headaches or body discomfort. In that case, the patient is infectious, and the infection category is I. The patient has acquired a significant infection to spread to other vulnerable people in I category. Infected individuals in category H have severe symptoms, and those seen in category I. Finally, after the parasite or infection has been removed by the patient's immune system and the patient is no longer contagious, the patient is considered recovered (R). If the user does not have any of the above symptoms, he is uninfected. Fig. 5 depicts the life cycle of COVID-19 as it progresses through several phases.
Fig. 5.
Life cycle of COVID-19 infection disease.
3.3. COVID-19 patient surveillance
Users infected with COVID-19 must be monitored for at least 21 days in cooperation with the appropriate health agency. It refers to the system's regular inspection of individual users' treatment and symptoms to keep a comprehensive history of progress reports for each patient. The patient is monitored at various periods depending on the infected categories as determined by a J48 decision tree. The severely infected individuals are monitored every 2 h since they have significant symptoms regularly. However, a qualified doctor can adjust the monitoring period if necessary. The monitoring time intervals for different types of infected individuals are shown in Table 7. Patients who have been affected are constantly watched and evaluated until they have fully recovered from the virus. The technology generates alert messages to be delivered to affected patients' cell phones. Depending on the GPS position of the patient's mobile phone, alert messages are also sent to local hospitals or healthcare services. As stated in Procedure 1 (Table 8), the proposed system executed the classification procedure regularly to evaluate the patient's category. If the patient's category is modified, the system generates alarm messages delivered to the user and the nearest hospital. In addition, the patient's record is updated.
Table 7.
Monitoring assessment time of COVID-19-patients.
| S. no. | Class | Monitoring time-delay |
|---|---|---|
| 1 | Highly infected (H) | 3 |
| 2 | Infected (I) | 9 |
| 3 | Exposed (E) | 13 |
| 4 | Susceptible (S) | 13–25 |
| 5 | Recovered (R) | 25–50 |
Table 8.
Procedure 1: updated class assessment for COVID-19 patient.
| Procedure 1: estimate accurate class of patient |
|---|
| Input: Patient UID and corresponding COVID-19 symptoms |
| Step 1: Assess the primary symptoms via WBAN and Patient UID |
| Step 2: If Patient UID Exist |
| Then Update the record with recent data |
| Else Create a new record with acquired patient UID and primary symptoms |
| End if |
| Step 3: Enter the secondary and advanced parameters for COVID-19 virus as per scheduled time |
| Step 4: Execute J48 decision tress methodology to estimate the revised class of patient |
| Step 5: If revised class = old class |
| Then Notify Next assessment time of patient |
| Step 6: Update the database record |
| Step 7: Else Update evaluation period; |
| Update patient class is database; |
| Generate alert signal to doctor; |
| Notify next evaluation of patient |
| Step 8: End if |
| Output: Updated Class of the patient based on recent symptoms |
3.4. Novel COVID-19 outbreak prevention
One of the critical elements in the presented methodology is to stop the COVID-19 outbreak from spreading. The proposed framework employs Temporal Network Analysis (TNA) to represent each user as a node, with edges established between users who have temporal proximity interactions (TPIs). The nodes are colored differently to signify different types of infection among users. TNA is a valuable tool for describing the status of pandemics. The evolution of pandemic propagation can be determined using TNA graphs, and infected users mainly responsible for the disease's transmission can be recognized. TNA graph is created with Gephi 0.9.1. Gephi is a free and open-source program for viewing and studying graphs of temporal networks. To display graphs in real-time and speed up research, Gephi employs a 3D render engine. As illustrated in Fig. 6 , infected individuals and respective relationships with other vulnerable or uninfected users may be efficiently portrayed using the technology.
Fig. 6.
TNA visualization (a) region 1; (b) region 2; (c) region 3.
4. RFID-based COVID-19 outbreak prevention
Some infections, such as COVID-19, can spread in various ways. COVID-19 disease is spread mainly through the air by droplets. In airborne transmission, pathogens are transmitted by coughing and inhaling infected users. The infections can travel up to a given distance in the air, depending on the environmental circumstances, and an uninfected user can inhale them. When droplets from an infected user come into contact with uninfected users, TPIs become extremely important for viral propagation. Identifying close-range proximity or interaction between infected and uninfected users is critical in the proposed architecture, which is utilized to restrict the spread of the COVID-19 pandemic. The government and healthcare institutions will manage the pandemic sooner if a clear image of the network structure shows the interactions between infected and uninfected people. The use of an RFID to identify high-resolution proximity between infected and uninfected users is proposed. When two RFID tags are close to one other, they exchange radio waves, making RFID one of the most promising technologies in the field of automated item identification. RFID devices have advanced to the point where they are compact, lightweight, and have long battery life, making them optimal for social network analysis. RFID tags are placed on the chests of users in a specific geographic region monitored for a COVID-19 outbreak to identify contacts only when people come close to each other. The RFID tag worn by another user is detected using a mobile phone equipped with an RFID reader. When an uninfected user with a mobile phone comes into contact with an infected person wearing an RFID tag, the phone detects the tag and recognizes the infected user's presence. The distance between them should be within 1–2 m. The threshold determines the sensation range of specific TPIs within which COVID-19 can be transmitted. The mobile phone's contact information is transferred to the cloud for storage, processing, and continual monitoring through a 4G/5G internet connection. The system will automatically produce and send an alert message to an uninfected user's mobile phone. The goal is to avoid coming into contact with an infected patient to prevent the epidemic from spreading. The proximity detection is done regularly, and each RFID tag sends contact information to another user's phone every few seconds. A 20-second window is specified during which the closeness may be evaluated with a 99% confidence level. Fig. 7 depicts an architecture of infected and non-infected user interactions.
Fig. 7.
Closed proximity.
4.1. Temporal network graph
An edge connecting two nodes (users) in the TNA graph appears or disappears based on whether they are near one other at a given time. This type of graph, based on user interactions, exhibits a continual change in the structure that corresponds to dynamic user activity. Recent technology advancements, such as RFID and mobile devices, have made it easier to collect data about human-to-human interactions in real-time. When the classification component detects a user's category, a TNA graph is built and updated regularly when new TPI data is received from other users. Procedure 2 (Table 9) is used to produce or update the TNA graph in real-time utilizing TPI data supplied by the RFID. Some key implications may be derived from the TNA graph that will aid healthcare organizations in controlling the COVID-19 outbreak.
Table 9.
Procedure 2: TNA graph creation and updation.
| Procedure 2: TNA graph updation |
|---|
| Input: COVID-19 proximity interaction details |
| Step 1: For every user do |
| Step 2: Read Source UID, target UID, class source, class target; |
| Step 3: Read Start time and end time of the proximity interaction |
| Step 4: If source UID and target UID already exist |
| Then Create an edge between source UID and target UID |
| Step 5: If revised class = old class |
| Then Notify Next assessment time of patient |
| Step 6: Else Create a new source and target node; |
| Label the nodes with the infection class; |
| Color the nodes with respective infection class; |
| Create an edge between source UID and target UID |
| Step 7: End if |
| Step 8: End for |
| Output: Updated TNA Graph |
4.2. TNA metrics
A crucial stage in the presented methodology is identifying significant users (nodes) who are responsible for COVID-19's propagation. Furthermore, an infected user with high proximity to other users can swiftly disseminate COVID-19 to vast groups of people. Henceforth, the current section defines some of the key metrics derived from TNA graphs.
Definition 1
Temporal route length: the temporal route length of a COVID-19 reflects how quickly it may spread from one infected user to another on the network. COVID-19 transmission is speeded up when the temporal route length is minimal. It is the average temporal distance between all pairs of nodes. Mathematically,
where M represents the node collection and sji indicates the shortest path from node j to i. Conspicuously, the global efficacy of temporal graph can be estimated as
Definition 2
Coefficient of temporal correlation (CTC): it represents the criticality of how likely it is for COVID-19-infected people to develop clusters in any given region. It will aid government authorities in isolating and prohibiting all forms of travel from that region. The proposed framework employs the temporal correlation coefficient value to determine the likelihood of cluster formation. Mathematically,
where Dj(tn, tn+1)is the topographic overlapping of the adjacent nodes for patient j in the temporal window of (tn, tn+1) and described mathematically as
Definition 3
Temporal centrality: temporal centrality is a powerful statistic for determining how involved every infected user is in spreading the pandemic. A user who is infected and has a large number of neighbors will contribute more to the outbreak's spread. The proportion of the temporal shortest path going through a node j's temporal centrality is defined as follows:
where ϕ ik represents the temporally shortest distance from patient i to patient k, and ϕ ik (j) is the total number of paths via patient j.
Definition 4
Temporal eccentricity: when a user is not in direct contact with a COVID-19-infected patient, they may know another infected patient. Any patient's centrality specifies how near that user is to other infected or uninfected patients. The inverse of the average length of the temporal shortest path between patient j and i may be calculated as
The entire step-wise procedure of the presented approach has been depicted in Fig. 8 .
Fig. 8.
Step-wise depiction of the presented approach; different phases have been formulated for data acquisition where data is acquired in real-time. The data acquired is pre-processed and classified using J48 classifier. Finally, based on the specific class of the patient, temporal graph is formulated for real-time graphical assessment.
5. Experimental simulation
A major effort was made to look for accurate data on COVID-19 patients based on symptoms on the internet. However, no relevant dataset was obtained to test the proposed model. Synthetic data is created to conduct tests and evaluate the proposed model's performance. The entire experimental simulation is confined to the following sub-sections.
-
1.
Creation of synthetic data
-
2.
Temporal Delay Analysis
-
3.
J48 decision tree classification assessment
-
4.
Amazon EC2 cloud testing
-
5.
TNA-based pandemic quantification
-
6.
Cost-benefit analysis
5.1. Generating synthetic data
The presented model cannot be adequately evaluated because data on COVID-19 patients' symptoms are not accessible. Synthetic data is created so that it includes every potential combination of symptoms. Table 10 depicts the odds of each COVID-19 virus symptom that is included in every freshly made case while building a synthetic COVID-19 virus dataset. Procedure 3 (Table 11) is intended to generate such a patient dataset. RFID-generated data concerning proximity contact information is also essential for evaluating the monitoring procedure adequately. An actual dataset was collected by the Socio-Patterns infrastructure that contained student contact information across 5 days. Each of the 22,500 items in the dataset depicts a proximity interaction (TPI) between 2 pupils at 19 s intervals. Each interaction comprises information about the source, target, start time, and finish time, where source and target are the IDs of the students who come within 1–2 m of the start and end times. Procedure 4 (Table 12) is aimed to produce synthetic data for 250,000 users by mapping TPI data among students at various periods with 22,500 COVID-19 cases generated. TNA graph will be created using massive data.
Table 10.
COVID-19 symptoms probabilistic measures.
| Primary symptoms | Probabilistic value | Secondary symptoms | Probabilistic value | Advanced symptoms | Probabilistic value |
|---|---|---|---|---|---|
| Sore throat | 0.59 | Chest pain | 0/1 | Delirium | 0/1 |
| Fever | 0.75 | Diarrhea | 0/1 | Kidney disease | 0/1 |
| Low immunity level | 0.61 | Weakness | 0/1 | Seizure | 0/1 |
| Severe headache | 0.85 | Skin rash | 0/1 | Lever disease | 0/1 |
| Muscle pain | 0.45 | Vomiting | 0/1 | Consciousness loss | 0/1 |
| Oxygen level | 0.85 | Watery eyes | 0/1 | Internal bleeding | 0/1 |
| Heart rate | 0.35 | Gastrointestinal | 0/1 | External bleeding | 0/1 |
Table 11.
Procedure 3: COVID-19 dataset generation.
| Procedure 3: dataset generation |
|---|
| Input: Data instances for COVID-19 symptoms |
| Step 1: Let n = 1, where n is the number of cases |
| Step 2: For n < required cases + 1 do |
| Step 3: Assigns measures to primary symptoms using probabilistic measures; |
| Assigns measures to secondary symptoms using probabilistic measures; |
| Assigns measures to advanced symptoms using probabilistic measures; |
| Step 4: Combine the values for Coivd-19 from Step-3 |
| Step 5: If the new case exist, then discard the current case |
| Step 6: Else Add the new case; |
| n = n + 1; |
| Step 7: End if |
| Step 8: End for |
| Output: Database Repository for COVID-19 Infection Class |
Table 12.
Procedure 4: obtaining 250,000 COVID-19 patient instances.
| Procedure 4: massive dataset generation |
|---|
| Input: TPI information of 2,50,000 users |
| Step 1: Let n = 1, where n is the number of cases |
| Step 2: For n < required cases + 1 do |
| Step 3: Select a random record from COVID-19 class; |
| Read the instance for TPI data; |
| Create a new user by accumulating data from TPI and symptoms; |
| Assign new UID to patient |
| Step 4: if UID is existing then discard the record |
| Step 5: Else Add the new user |
| Step 6: End if |
| Step 7: End for |
| Output: Database Repository for COVID-19 Infection Class |
5.2. Temporal delay analysis
Temporal delay computes the overall running time of the presented model for information sensing, classifying, and temporal data analysis. Moreover, the overall calculated time is assessed for estimating the delay for optimal delivery of services. Temporal delay is computed as follows;
The mean results are computed for the variable number of data instances for deployment purposes. Moreover, it is indispensable to mention that the temporal analysis is calculated at the fog node (Raspberry Pi). Henceforth, the actual data instances are considered due to memory constraints. The entire execution time for entire datasets is shown in Fig. 9 . The average data categorization latency for diverse datasets is 29.36 s. A delay of 32.16 s occurred during the data mining task. Finally, the decision-making took 50.16 s to complete. The total execution time for the performance estimation is averaged to 122.63 s due to the accumulation of these sub-delays.
Fig. 9.

Temporal delay.
5.3. J48 decision tree-based classification efficacy
After Procedure 4 has generated 250,000 COVID-19 virus cases, distinct classes are formulated using the J48 decision tree in Weka 3.6. The J48 decision tree's performance is evaluated using a 10-fold cross-validation method. Weka 3.6 is used to test data from 250,000 users. Fig. 10 shows the pictorial illustration of the J48 Tree in the Weka tool. It can be seen that each user can be categorized as Category U with non-infectious. Category E indicates patients with mild fever along with cough symptoms. Moreover, if the fever is high along with secondary symptoms then the category of the patient is updated to H. Category I reflects the additional symptoms as that of category H. Finally, the cured patent is assigned the category S or non-infectious. Various statistical findings are obtained and shown in Table 13, Table 14, Table 15. Averagely, the decision tree correctly identifies the COVID-19 patients with 95.26% accuracy. The accuracy of each category categorized by the J48 decision tree is shown in Table 14. True positives (TP), also known as sensitivity, refers to the classifier's percentage of COVID-19 cases diagnosed correctly. The fraction of COVID-19 cases incorrectly interpreted by the classifier is known as false positives (FP). With an average TP rate of 94.65% and an FP rate of 5.2%, the J48 classification method generates a maximal TP rate of 97.48% and a minimal FP rate of 2.36%. Precision and recall are 2 characteristics that determine the relevance of the results. The accuracy and recall of the proposed classification method are numerated to 95.68% and 92.45%, respectively. F-Measure and ROC area are 2 more statistical measures that reflect classification accuracy. The F-Measure and ROC area of an algorithm with a maximal value is accurate. The presented J48 decision tree has F-Measure and ROC area of 89.65% and 90.15%, respectively. Conspicuously, the utility of the J48 classifier is justified in the proposed approach.
Fig. 10.
Illustration of J48 classifier tree with estimation of different categories of patients; the box value indicate the number of infected patients in different category with respect to total sample size; SS Starting State, ST Intermediary State.
Table 13.
10-Fold cross validation for J48 decision-tree; number of data instance: 250,000.
| Attributes | Output (in %) |
|---|---|
| Accurate classification | 95.26 |
| Inaccurate classification | 4.74 |
| Mean absolute error | 2.36 |
| Root mean squared error | 3.45 |
| Root relative squared error | 3.28 |
| Kappa statistic | 85.36 |
| Relative absolute error | 4.65 |
Table 14.
Performance assessment: class-wise categorization using J48 technique.
| Class | True positive rate | False positive rate | Precision | ROC area | F-measure | Recall |
|---|---|---|---|---|---|---|
| H | 92.36 | 1.23 | 98.56 | 89.36 | 98.25 | 93.25 |
| I | 92.45 | 2.32 | 96.25 | 95.23 | 95.25 | 94.25 |
| E | 93.56 | 4.25 | 94.36 | 94.25 | 94.36 | 96.25 |
| S | 95.36 | 1.23 | 95.65 | 96.25 | 93.25 | 95.22 |
| R | 97.36 | 1.26 | 96.25 | 94.25 | 94.25 | 95.02 |
| U | 98.36 | 1.25 | 95.25 | 93.25 | 95.87 | 96.02 |
| Mean | 97.25 | 0.56 | 94.36 | 94.56 | 96.33 | 95.54 |
Table 15.
WEKA 3.6 confusion matrix.
| Classified class → | E | I | S | U | R | H |
|---|---|---|---|---|---|---|
| Actual class | ||||||
| E | 3958 | NA | NA | 5244 | NA | |
| I | 2848 | NA | NA | NA | NA | 575 |
| S | NA | NA | 2547 | NA | NA | |
| U | NA | NA | 1042 | 4272 | 4574 | 110 |
| R | 2659 | NA | 3569 | 638 | 788 | |
| H | NA | 2548 | NA | NA | NA | 757 |
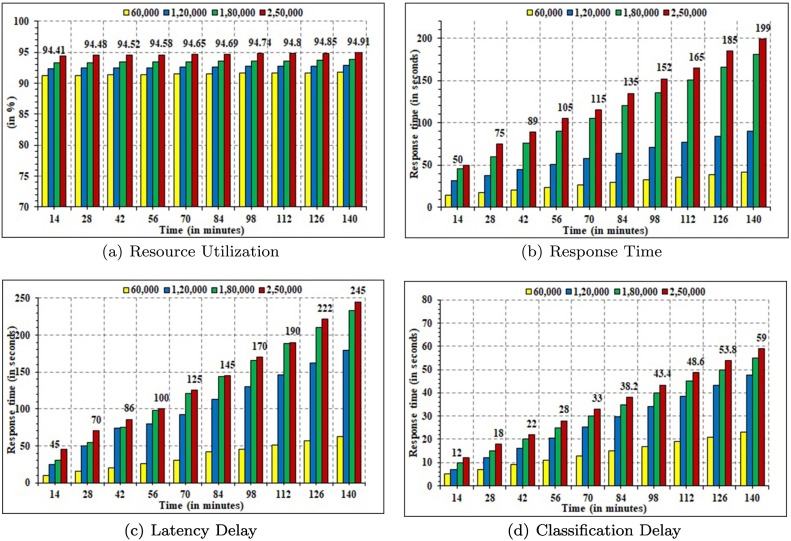
5.4. Amazon EC2 cloud-based analysis
The proposed framework's performance was assessed in real-time by hosting it on the cloud. Amazon EC2 provides cloud storage for synthetically manufactured COVID-19 cases. General-purpose compute-optimized c3.xlarge (Amazon 2016) instances are employed to build up an application in the cloud. The performance is assessed using synthetic data from 250,000 users. The system was initially loaded with 9999 requests. After each 6-min, the request was raised by 9999, and the system's performance was monitored for a total of 140 min. Fig. 11(a) depicts the proposed model's resource usage, which varies depending on the number of users. When the number of users reaches 250,000, the system quickly reaches saturation since more resources are required to handle them. Similarly, Fig. 11(b) shows the reaction time of the presented model for various numbers of users. Because there are fewer entries in the database to execute each function, the system has a fast response time for a small number of users. Fig. 11(c) depicts the presented model's delay time for various users. Fig. 11(d) illustrates the performance of the J48 decision tree method in terms of classification time. As mentioned earlier, the performance of the classifiers was tested on the Amazon EC2 cloud on a simulated dataset of 250,000 users. The presented J48 classification algorithm's performance is assessed in terms of the confusion matrix, as shown in Table 15. In the proposed framework, correct user classification is a critical step. Weka 3.6 is used to evaluate the performance of several categorization methods such as Random Tree, Naive Bayes, and REPTree. Classifying an extensive dataset of users into distinct illness groups necessitates a high degree of efficiency. Table 16 compares the classification performance of the various classification models examined in Weka 3.6. The J48 decision tree outperforms other classifiers in terms of accuracy. It indicates the percentage of infected and non-infected users correctly classified in the respective categories. Due to a significant dataset, the J48 decision tree has an elevated accuracy with time. The classification process takes longer for the large dataset.
Fig. 11.
Comparative temporal analysis.
Table 16.
Performance analysis.
| Parameters | Random tree (%) | REP tree (%) | Naive Bayes (%) | J48 (%) |
|---|---|---|---|---|
| Accuracy | 92.99 | 94.12 | 93.14 | 96.78 |
| Sensitivity | 90.12 | 91.45 | 90.98 | 96.45 |
| Specificity | 91.98 | 90.45 | 95.15 | 94.78 |
| F-measure | 92.15 | 91.45 | 93.15 | 95.15 |
| Mean absolute error (MAE) | 4.45 | 5.17 | 6.34 | 3.15 |
| Root mean square error (RMSE) | 3.19 | 2.32 | 2.45 | 1.24 |
5.5. TNA-based pandemic quantification
Controlling the pandemic will need a thorough examination of the TPI network structure. Vaccination is one of the most widely utilized control methods since it can lower the amount of infection in an infected patient and prevent it from spreading [45], [46]. Furthermore, vaccination of the entire population is impossible to prevent pandemics [47]. The TNA graph is used to calculate several metrics that can be used to detect heavily infected locations or people spreading the disease. In Gephi 0.9.1, synthetic data of 250,000 users are simulated for outbreak prevention utilizing TNA approaches. Table 17 shows the results of evaluating several temporal metrics. Multiple pandemic metrics derived with Gephi 0.9.1 can be identified from the TNA graph. According to the results of the experiments, TNA is an efficient and effective tool for analyzing the state of the pandemic using specific parameters.
Table 17.
Result summation.
| S. no. | Attribute | Results |
|---|---|---|
| 1 | Average path length | 53,659 |
| 2 | Average weighted degree | 12,235 |
| 3 | Number of strongly connected components | 201,326 |
| 4 | Network diameter | 201 |
| 5 | Number of weakly connected components | 300,215 |
| 6 | Average degree | 25,125 |
5.6. Cost computation
Even in developed nations like USA, Russia, and UK, the cost is crucial when evaluating the presented approach's economic feasibility. Acquiring cloud services is a fundamentally useful strategy as there is no need for maintenance or installation. The upfront cost may be entirely erased by employing a pay-per-use payment mechanism that charges the customer by rounding up to the nearest hour of usage time. Amazon Web Services (AWS) offers 2 use tiers at a relatively low price: on-demand, one-year reserved, and three-year reserved. To implement the proposed framework, Amazon provides the EC2 service, which allows users to rent virtual computers (known as instances) with a choice of hardware requirements. The most basic example is a single-core CPU with 2 GB RAM, costing $0.014 per hour in the USA. RFID tags have become much less expensive in recent years, ranging from $0.06 to $0.09. Fog-cloud computing services and sensor technologies are cost-effective and may be carried by any nation's government during an outbreak.
6. Conclusion
COVID-19 is a global threat to any country's healthcare system. Using Temporal Network Analysis and IoT-fog-cloud technology, a comprehensive architecture for predicting and preventing COVID-19 outbreak has been proposed in the current research. IoT and RFID acquire bodily symptoms and social interactions, respectively. The presented framework is focused on acquiring time-sensitive close-proximity contacts and health data to restrict the spread of the disease. The J48 decision tree is used to categorize the users into a specific category. TNA is used to represent each COVID-19-affected user on the TNA graph. Numerous temporal metrics, including Temporal Proximity Index (TPI), are calculated to identify infected people or places heavily impacted in the pandemic outbreak. The presented framework is validated on the Amazon EC2 cloud, as it registered an average classification accuracy, and sensitivity of 96.68% and 94.65% respectively. Moreover, significant improvement has been registered for proposed fog-cloud-based data analysis in terms of Temporal Delay efficacy, Precision, and F-measure. For future research exploration, the missing data insertion technique will be used for the acquired data instances to increase the system's efficiency.
Compliance with ethical standards
No funding was received for the study. All Authors declare that they have no conflict of interest. This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
References
- 1.de Morais Barroca Filho Itamir, Aquino Gibeon, Malaquias Ramon Santos, Girão Gustavo, Melo Sávio Rennan Menêzes. An iot-based healthcare platform for patients in icu beds during the covid-19 outbreak. IEEE Access. 2021;9:27262–27277. doi: 10.1109/ACCESS.2021.3058448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Jianguo, Li Kenli, Zhang Zhaolei, Li Keqin, Yu Philip S. A survey on applications of artificial intelligence in fighting against covid-19. ACM Comput Surv. 2021;54(8):1–32. [Google Scholar]
- 3.Ng Kangqi, Poon Beng Hoong, Puar Troy Hai Kiat, Quah Jessica Li Shan, Loh Wann Jia, Wong Yu Jun, Tan Thean Yen, Raghuram Jagadesan. Covid-19 and the risk to health care workers: a case report. Ann Intern Med. 2020;172(11):766–767. doi: 10.7326/L20-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aljohani Abdulah Jeza, Shuja Junaid. Waleed alasmary, and abdulaziz alashaikh. Evaluating the dynamics of bluetooth low energy based covid-19 risk estimation for educational institutes. Sensors. 2021;21(19):6667. doi: 10.3390/s21196667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar Krishna, Kumar Narendra, Shah Rachna. Role of iot to avoid spreading of covid-19. Int J Intell Netw. 2020;1:32–35. [Google Scholar]
- 6.Bhatia Munish, Sood Sandeep K. Temporal informative analysis in smart-icu monitoring: M-healthcare perspective. J Med Syst. 2016;40(8):190. doi: 10.1007/s10916-016-0547-9. [DOI] [PubMed] [Google Scholar]
- 7.Sharma Sunil Kumar, Ahmed Sameh S. Iot-based analysis for controlling & spreading prediction of covid-19 in Saudi Arabia. Soft Comput. 2021;25(18):12551–12563. doi: 10.1007/s00500-021-06024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhatia Munish, Sood Sandeep K., Kaur Simranpreet. Quantum-based predictive fog scheduler for iot applications. Comput Ind. 2019;111(10):51–67. [Google Scholar]
- 9.Shuja Junaid, Humayun Mohammad Ali, Alasmary Waleed, Sinky Hassan, Alanazi Eisa, Khan Muhammad Khurram. Resource efficient geo-textual hierarchical clustering framework for social iot applications. IEEE Sensors Journal. 2021;21(22):25114–25122. [Google Scholar]
- 10.Singh Ravi Pratap, Javaid Mohd, Haleem Abid, Suman Rajiv. Internet of things (iot) applications to fight against covid-19 pandemic. Diabetes Metab Syndr Clin Res Rev. 2020;14(4):521–524. doi: 10.1016/j.dsx.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen Jianguo, Li Kenli, Rong Huigui, Bilal Kashif, Yang Nan, Li Keqin. A disease diagnosis and treatment recommendation system based on big data mining and cloud computing. Inform Sci. 2018;435:124–149. [Google Scholar]
- 12.Ndiaye Musa, Oyewobi Stephen S., Abu-Mahfouz Adnan M., Hancke Gerhard P., Kurien Anish M., Djouani Karim. Iot in the wake of covid-19: A survey on contributions, challenges and evolution. IEEE Access. 2020;8:186821–186839. doi: 10.1109/ACCESS.2020.3030090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdul Haseeb-Ur-Rehman Rana M., Liaqat Misbah, Aman Azana Hafizah Mohd, Hamid Siti Hafizah Ab, Ali Rana Liaqat, Shuja Junaid, Khan Muhammad Khurram. Sensor cloud frameworks: State-of-the-art, taxonomy, and research issues. IEEE Sensors Journal. 2021;21(20):22347–22370. [Google Scholar]
- 14.Jung Younchan, Agulto Ronnel. A public platform for virtual iot-based monitoring and tracking of covid-19. Electronics. 2021;10(1):12. [Google Scholar]
- 15.Liu Xiaowei, Yang Lei, Chen Jianguo, Siyang Yu., Li Keqin. Region-to-boundary deep learning model with multi-scale feature fusion for medical image segmentation. Biomed Signal Process Control. 2022;71:103–165. [Google Scholar]
- 16.Dangi Mehak, Kumari Rinku, Singh Bharat, Chhillar Anil Kumar. Advanced in silico tools for designing of antigenic epitope as potential vaccine candidates against coronavirus. Vol. 10. 2018. pp. 329–357. [Google Scholar]
- 17.Chakraborty C., Roy S., Sharma S., Tran T., Dwivedi P., Singha M. Iot based wearable healthcare system: post covid-19. The Impact of the COVID-19Pandemic on Green Societies. Environ Sustain. 2021;13(13):305–321. [Google Scholar]
- 18.Jahmunah Vicnesh, Sudarshan Vidya K., Oh Shu Lih, Gururajan Raj, Gururajan Rashmi, Zhou Xujuan, Tao Xiaohui, Faust Oliver, Ciaccio Edward J., Ng Kwan Hoong, et al. Future iot tools for covid-19 contact tracing and prediction: A review of the state-of-the-science. Int J Imaging Syst Technol. 2021;31(2):455–471. doi: 10.1002/ima.22552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghimire Awishkar, Thapa Surendrabikram, Jha Avinash Kumar, Kumar Amit, Kumar Arunish, Adhikari Surabhi. 2020 4th International Conference on Electronics, Communication and Aerospace Technology (ICECA) IEEE; 2020. Ai and iot solutions for tackling covid-19 pandemic; pp. 1083–1092. [Google Scholar]
- 20.Rathee Geetanjali, Garg Sahil, Kaddoum Georges, Wu Yulei, Jayakody Dushantha Nalin K., Alamri Atif. Ann assisted-iot enabled covid-19 patient monitoring. IEEE Access. 2021;9:42483–42492. doi: 10.1109/ACCESS.2021.3064826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adil Muhammad, Khan Muhammad Khurram. Emerging iot applications in sustainable smart cities for covid-19: Network security and data preservation challenges with future directions. Sustainable Cities and Society. 2021;75:1–33. doi: 10.1016/j.scs.2021.103311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abdur Rahman M., Hossain Shamim, Alrajeh Nabil A., Alsolami Fawaz. Adversarial examples–security threats to covid-19 deep learning systems in medical iot devices. IEEE Internet Things J. 2020;8(12):9603–9610. doi: 10.1109/JIOT.2020.3013710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karmore Swapnili, Bodhe Rushikesh, Fadi Al-Turjman R., Kumar Lakshmana, Pillai Sofia. Iot based humanoid software for identification and diagnosis of covid-19 suspects. IEEE Sens J. 2020 doi: 10.1109/JSEN.2020.3030905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shwet Ketu and Pramod Kumar Mishra Enhanced gaussian process regression-based forecasting model for covid-19 outbreak and significance of iot for its detection. Appl Intell. 2021;51(3):1492–1512. doi: 10.1007/s10489-020-01889-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahman Anichur, Chakraborty Chinmay, Anwar Adnan, Karim Md, Islam Md, Kundu Dipanjali, Rahman Ziaur, Band Shahab S., et al. Sdn–iot empowered intelligent framework for industry 4.0 applications during covid-19 pandemic. Cluster Computing. 2021:1–18. doi: 10.1007/s10586-021-03367-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anjali K., Anand Reshmi, Prabhu Sradha D., Geethu R.S. 2021 6th International Conference on Communication and Electronics Systems (ICCES) IEEE; 2021. Iot based smart healthcare system to detect and alert covid symptom; pp. 685–692. [Google Scholar]
- 27.Shorfuzzaman Mohammad. Iot-enabled stacked ensemble of deep neural networks for the diagnosis of covid-19 using chest ct scans. Computing. 2021;6:1–22. [Google Scholar]
- 28.Firouzi Farshad, Farahani Bahar, Daneshmand Mahmoud, Grise Kathy, Song Jae Seung, Saracco Roberto, Wang Lucy Lu, Lo Kyle, Angelov Plamen, Soares Eduardo, et al. Harnessing the power of smart and connected health to tackle covid-19: Iot, ai, robotics, and blockchain for a better world. IEEE Internet of Things Journal. 2021;8(16):12826–12846. doi: 10.1109/JIOT.2021.3073904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rajasekar Sakthi Jaya Sundar. An enhanced iot based tracing and tracking model for covid-19 cases. SN Comput Sci. 2021;2(1):1–4. doi: 10.1007/s42979-020-00400-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin Wei-Ling, Hsieh Chun-Hung, Chen Tung-Shou, Chen Jeanne, Lee Jian-Le, Chen Wei-Chung. Apply iot technology to practice a pandemic prevention body temperature measurement system: a case study of response measures for covid-19. Int J Distrib Sens Netw. 2021;17(5):1–13. [Google Scholar]
- 31.Bassam Nizar Al, Hussain Shaik Asif, Qaraghuli Ammar Al, Khan Jibreal, Sumesh E.P., Lavanya Vidhya. Informatics in Medicine Unlocked. Vol. 24. 2021. Iot based wearable device to monitor the signs of quarantined remote patients of covid-19; pp. 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dwivedi Priyanka, Singha Monoj Kumar. The impact of the COVID-19 pandemic on green societies. Vol. 13. 2021. Iot based wearable healthcare system: post covid-19; pp. 305–321. [Google Scholar]
- 33.Shariq Mohd, Singh Karan, Bajuri Mohd Yazid, Pantelous Athanasios A., Ahmadian Ali, Salimi Mehdi. A secure and reliable rfid authentication protocol using digital schnorr cryptosystem for iot-enabled healthcare in covid-19 scenario. Sustain Cities Soc. 2021;75(9):1–13. doi: 10.1016/j.scs.2021.103354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mukati Naveen, Neha Namdev R., Dilip N.Hemalatha, Dhiman Viney, Sahu Bharti. Healthcare assistance to covid-19 patient using internet of things (iot) enabled technologies. Mater Today: Proc. 2021;7:1–5. doi: 10.1016/j.matpr.2021.07.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poongodi M., Nguyen Tu.N., Hamdi Mounir, Cengiz Korhan. A measurement approach using smart-iot based architecture for detecting the covid-19. Neur Process Lett. 2021;7:1–15. doi: 10.1007/s11063-021-10602-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mukherjee Rajendrani, Kundu Aurghyadip, Mukherjee Indrajit, Gupta Deepak, Tiwari Prayag, Khanna Ashish, Shorfuzzaman Mohammad. Iot-cloud based healthcare model for covid-19 detection: an enhanced k-nearest neighbour classifier based approach. Computing. 2021;4:1–21. [Google Scholar]
- 37.Sood Sandeep K., Mahajan Isha. Wearable iot sensor based healthcare system for identifying and controlling chikungunya virus. Comput Ind. 2017;91:33–44. doi: 10.1016/j.compind.2017.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bhatia Munish, Sood Sandeep K. A comprehensive health assessment framework to facilitate iot-assisted smart workouts: a predictive healthcare perspective. Comput Ind. 2017;92:50–66. [Google Scholar]
- 39.Vani K.S., Neeralagi Rajesh Rayappa. Iot based health monitoring using fuzzy logic. Int. J. Comput. Intell. Res. 2017;13(10):2419–2429. [Google Scholar]
- 40.Verma Prabal, Sood Sandeep K. Cloud-centric iot based disease diagnosis healthcare framework. J Parallel Distrib Comput. 2018;116:27–38. [Google Scholar]
- 41.Bhatia Munish, Sood Sandeep K. Exploring temporal analytics in fog-cloud architecture for smart office healthcare. Mobile Netw Appl. 2019;24(4):1392–1410. [Google Scholar]
- 42.Sood Sandeep K., Mahajan Isha. Fog-cloud based cyber-physical system for distinguishing, detecting and preventing mosquito borne diseases. Future Generation Computer Systems. 2018;88:764–775. [Google Scholar]
- 43.Sareen Sanjay, Sood Sandeep K., Gupta Sunil Kumar. Iot-based cloud framework to control ebola virus outbreak. J Ambient Intell Humaniz Comput. 2018;9(3):459–476. doi: 10.1007/s12652-016-0427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tuli Shreshth, Basumatary Nipam, Gill Sukhpal Singh, Kahani Mohsen, Arya Rajesh Chand, Wander Gurpreet Singh, Buyya Rajkumar. Healthfog: An ensemble deep learning based smart healthcare system for automatic diagnosis of heart diseases in integrated iot and fog computing environments. Future Generation Computer Systems. 2020;104:187–200. [Google Scholar]
- 45.Arshadi Arash Keshavarzi, Webb Julia, Salem Milad, Cruz Emmanuel, Calad-Thomson Stacie, Ghadirian Niloofar, Collins Jennifer, Diez-Cecilia Elena, Kelly Brendan, Goodarzi Hani, et al. Artificial intelligence for covid-19 drug discovery and vaccine development. Front Artif Intell. 2020;3:1–13. doi: 10.3389/frai.2020.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thomas Sunil, Abraham Ann, Baldwin Jeremy, Piplani Sakshi, Petrovsky Nikolai. Vaccine Design. Vol. 12. Springer; 2021. Artificial intelligence in vaccine and drug design; pp. 131–146. [DOI] [PubMed] [Google Scholar]
- 47.Almars Abdulqader M., Gad Ibrahim, Atlam El-Sayed. Medical informatics and bioimaging using artificial intelligence. Vol. 12. Springer; 2021. Applications of ai and iot in covid-19 vaccine and its impact on social life; pp. 115–127. [Google Scholar]