Abstract
Background
Covid-19 pandemic caused relevant psychological consequences in the general population. Since people with Multiple Sclerosis (pwMS) are usually at higher risk of psychological distress than age-matched healthy controls (HC), a meta-analytic study was conducted, aimed at evaluating i) differences between pwMS and HC in the psychological variables during the pandemic, ii) differences in the levels of anxiety, depression, stress, sleep disturbances and quality of life before and during the Covid-19 pandemic in pwMS.
Methods
The literature search on three electronic databases yielded 196 studies (113 after the duplicates removal). Seven studies compared psychological variables between pwMS and HC during the pandemic, while seven studies evaluated the pre- vs during the pandemic differences in pwMS. The following outcomes were selected: depression, anxiety, physical QoL, mental QoL, stress, sleep quality/disturbances. Mean weighted effect sizes (ES) were calculated using Hedges'g, via Prometa3 software.
Results
During the pandemic, pwMS showed higher levels of depression (g = 0.51, p=.001), anxiety (g = 0.41, p=.032), and stress (g = 0.51, p=.016) compared to HC. The comparison on psychological outcomes before and during the pandemic in pwMS revealed no significant increase during the pandemic on levels of anxiety (g = 0.08, p=.380), depression (g = 0.02, p=.772), mental QoL (g= -0.14, p=.060), physical QoL (g = 0.00, p=.986), whereas sleep quality deteriorated during the pandemic (g = 0.52, p<.001).
Conclusions
In agreement with pre-pandemic literature, pwMS showed higher levels of psychological distress than HC also during the Covid-19 pandemic. Contrariwise, longitudinal studies revealed that, in pwMS, the only psychological-associated variable that worsened significantly was the sleep quality, but this outcome was evaluated only in two studies. Future studies will have to assess/evaluate the long-term psychological consequences of the pandemic on pwMS.
Keywords: Covid-19, Multiple sclerosis, Depression, Anxiety, Sleep, QoL
1. Introduction
Coronavirus Disease 2019 (Covid-19) was declared a global pandemic on March 11, 2020 by the World Health Organization (Cucinotta and Vanelli, 2020) and rapidly spread all around the word (World Health Organization 2021). Being afraid and worried of contracting a yet largely unknown and potentially deadly disease, even in healthy people, together with the stringent health measures adopted by governments to contain the outbreak, such as quarantine, social distancing, or lockdowns, produced dramatic and relevant consequences on psychological health; it is well known, indeed, that prolonged isolation and a sense of uncertainty related to the pandemic may strongly increase levels of psychological distress (Pietrabissa and Simpson, 2020). To date, several reviews and meta-analyses on psychological consequences of Covid-19 pandemic revealed that healthcare workers, general population at every age (Lebrasseur et al., 2021; Luo et al., 2020; Singh et al., 2020; Xiong et al., 2020) and people affected by chronic diseases (Al-Rahimi et al., 2021; Cohen et al., 2020; Wang et al., 2020) suffered of high rates of anxiety, depression, stress, sleep disturbances and post-traumatic stress disorder. Nonetheless, studies on the psychological consequences of the Covid-19 pandemic on people with Multiple Sclerosis (pwMS) revealed inconsistent results: some studies (Naser Moghadasi, 2020; Stojanov et al., 2020) reported an increase of psychological distress during the pandemic, while other studies did not (Capuano et al., 2021; Chiaravalloti et al., 2021). Therefore, to better understand how the pandemic impacted on psychological status of pwMS, a meta-analytic study was conducted, aimed at i) evaluating possible differences between pwMS and healthy controls (HC) in the psychological variables during the pandemic, ii) evaluating possible differences in the levels of anxiety, depression, stress, sleep disturbances and QoL before and during the Covid-19 pandemic in pwMS.
2. Methods
2.1. Literature search and inclusion criteria
The literature search was performed on October 11, 2021 on three electronic databases (PsycINFO, PubMed, Scopus), by employing the following keywords: Multiple Sclerosis AND (Covid-19 OR coronavirus OR Sars-Cov-2) AND (psycholog* OR depress* OR anxi* OR sleep OR stress OR quality of life OR coping). The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement (Moher et al., 2009) was employed to select eligible articles. To try to better control the publication bias, gray literature (i.e., conference proceedings) was included by manual search (Paez, 2017). Primary studies were included in the meta-analysis if they: (a) were written in English, (b) included a group of pwMS; (c) reported the comparison between scores of psychological questionnaires (assessing one or more of the following outcomes: anxiety, depression, mental and physical quality of life (QoL), stress, sleep disturbances) completed before and during the Covid-19 pandemic by pwMS, or they compared scores of psychological questionnaires between pwMS and HC during the Covid-19 pandemic.
2.2. Data collection and coding
Two reviewers (MA and RC) performed the data collection and coding; in case of disagreement, agreement was reached by discussion between the two reviewers and authors with expertise on psychology. For the purposes of the present meta-analytic study, psychological variables in the primary studies were coded in the following outcomes: anxiety, depression, mental and physical quality of life (QoL), stress, sleep disturbances, coping strategies. We collected for each primary study, when available, the following data: country of primary study, time period of data collection, government restrictions at the time of data collection, evaluated by means of the government response stringency index (Hale et al., 2021). The Government Response Stringency Index ranges from 0 to 100, where 100 is the strictest government response. Moreover, for both HC and pwMS groups, we collected: (a) number of participants, (b) mean age of the sample, (c) mean years of education, (d) percentage of females in the sample. For only pwMS group we collected: a) MS phenotype (RR vs mixed sample) and mean EDSS. Nonetheless, for clarity purposes, we also reported other data (i.e., data reported as number and% of educational qualification, or as number and% of participants <50 years; or as number and% of people with education higher than diploma, or as median and interquartile range) that could not be added in the meta-analysis software.
2.3. Statistical analysis
A random-effect model was used for this meta-analytic study; each effect size (ES) of each primary study was calculated in Hedges’ g; all ESs were pooled together as mean weighted ES of each outcome. Positive ESs were indicative of (a) higher levels of psychological distress in the pwMS group compared to HC during the lockdown, or (b) an increase of psychological distress during the lockdown compared to pre-pandemic psychological status, Cochran's Q, and I2 statistics served to analyze inter-study heterogeneity. Values of I2 above 25%, 50%, and 75% were interpreted as low, moderate and high inter-study heterogeneity, respectively. Sensitivity analysis was performed on outcomes showing high levels of heterogeneity. A p value <0.05 was considered for significance in both random-effects model and heterogeneity statistics. All statistical analyses were performed by employing ProMeta3 software.
3. Results
3.1. Literature search and characteristics of included studies
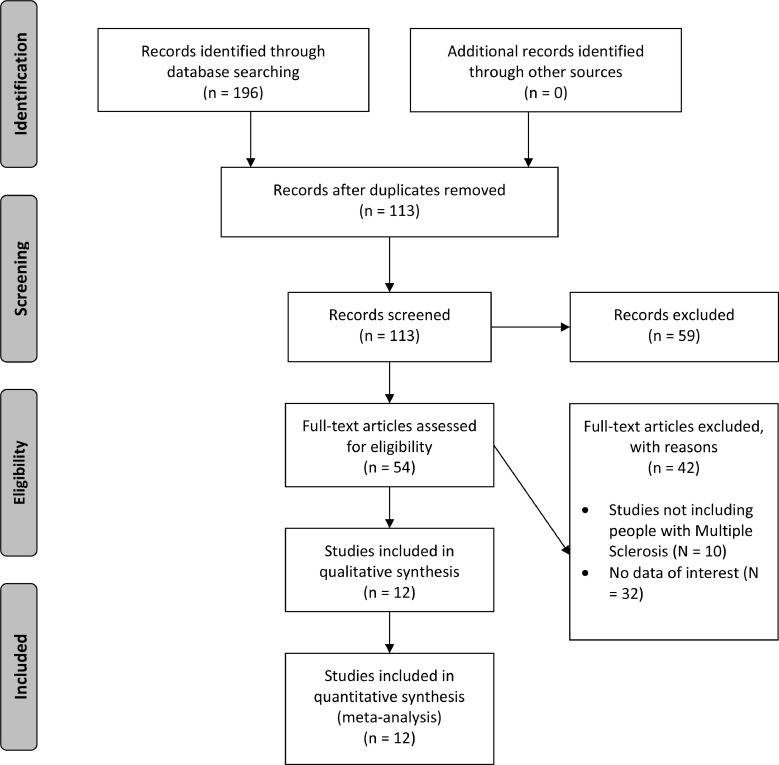
Fig. 1 shows the flow diagram based on the PRISMA statement. The initial literature search yielded 196 studies, which became 113 after removing duplicates. Successively, 59 studies were excluded based on their title and abstract and 54 articles were assessed for eligibility. The quantitative analysis was performed on 12 studies (characteristics of primary studies are available in Table 1 ; time period of data collection of the primary studies during the COVID-19 pandemic, and government restrictions at the time of data collection are available in Table 2 ). Twelve studies were found by means of a literature search supplemented by electronic databases. No studies from gray literature were added in the final analysis. Seven studies (overall N = 5537; HC = 1925; pwMS = 3612) reported a comparison on psychological variables between pwMS and HC during the lockdown (Bonavita et al., 2020; (Costabile et al., 2021); Garjani et al., 2021; Motolese et al., 2020; Shaygannejad et al., 2020; Stojanov et al., 2020; Talaat et al., 2020), whereas seven studies (overall N = 2692) reported a comparison between the psychological status of pwMS before and during the 2020 lockdown ((Andreu-Caravaca et al., 2021); (Capuano et al., 2021); (Chiaravalloti et al., 2021) Demir et al., 2020; Garjani et al., 2021; Sbragia et al., 2021; Stojanov et al., 2020). Two studies (Garjani et al., 2021; Stojanov et al., 2020) reported data on both the comparisons between HC and pwMS during the Covid-19 pandemic and the scores of pwMS obtained before vs during the pandemic. All primary studies were performed in Europe, except for a) (Chiaravalloti et al., 2021) which was a multicentric study including a sample from the United States of America, b) Shaygannejad et al. (2020) which was performed in an Asian contry (Iran) and c) Talaat et al. (2020) which was performed in an African country (Egypt). Government restrictions in the countries of primary studies at the time of data collection were heterogeneous, but always present, ranging from a score of 42.59 for (Shaygannejad et al., 2020) in Iran to a score of 100 of (Stojanov et al., 2020) in Serbia (see Table 2). It was not possible to perform a meta-analysis on the coping strategies outcome due to lack of primary studies; for the same reason, the meta-analysis on the differences between pwMS and HC on mental and physical QoL, and the meta-analysis on levels of stress in pwMS before and during the 2020 Covid-19 lockdown could not be performed.
Fig. 1.
Study selection process. PRISMA flowchart.
Table 1.
Characteristics of primary studies included in the meta-analytic study.
| Study | Contry | HC | pwMS | Scales | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean Age (SD) | Mean years of education | F (%) | n | Mean Age (SD) | Mean years of education | F (%) | Phenotype (n) | Mean EDSS (SD) | |||
| Andreu-Caravaca et al., 2021 | Spain | 17 | 43.5 (11.2) | N.A. | 58.8% | RRMS: 15 SPMS: 2 |
2.87 (1.38) | MSQoL-54 KSD (sleep quality score) |
||||
| Bonavita et al., 2020 | Italy | 674 | 44 (11.1) | Primary school: 6 (0.9%)a Middle school: 65 (9.6%)a High school: 229 (34%)a Graduation: 374 (55.5%)a |
72.7% | 612 | 43 (10) | Primary school: 4 (0.7%)a Middle school: 96 (15.7%)a High school: 323 (52.8%)a Graduation: 189 (30.9%)a |
76% | RRMS: 498 PMS: 114 |
N.A. | PHQ-2 PSS |
| Capuano et al., 2020 | Italy | 67 | 37.5 (11.1) | 13.7 (3.5) | 55.3% | RRMS: 67 | 2.0 (1.0-2.0)d | BDI-II STAI-Y1 MSQoL-54 |
||||
| Chiaravalloti et al., 2020 | Multicentric (Belgium, Canada, Denmark, United Kingdom, Italy, United States) | 131 | 52.1 (6.9) | 13.1 (3.1) | 63,4% | PMS: 131 | 6.0 (4-6.5)d | BDI-II HADS-A MSIS-29 |
||||
| Costabile et al., 2021 | Italy | 348 | 40.8 (11.9) | 16.6 (2.8) | 75.9% | 497 | 42.4 (10.7) | 14 (3.3) | 70,6% | N.A. | N.A. | Neuro-QoL |
| Demir et al., 2020 | Turkey | 50 | 30 (7) | 84% | N.A. | 1.1 (0.5) | BDI-II BAI MSQoL-54 PSQI |
|||||
| Garjani et al., 2021 | United Kingdom | 380 | 49 (37-61)d | N.A. | 73.6% | 2226 (for longitudinal analysis in pwMS)z 1982 (comparison between pwMS and HC) |
56 (48-63)d | N.A. | 74.3% | RRMS: 1114 PMS: 781 Other: 87 |
N.A. | GAD-7 PHQ-9 (for pwMS and HC comparison) HADS-D HADS-A (for longitudinal analysis in pwMS) |
| Motolese et al., 2020 | Italy | 50 | <50 yearsb: 34 (68%) >50 yearsb: 16 (32%) |
Higher educationa: 24 (48%) High schoola: 16 (32%) Upper secondary school or lowera: 10 (20%) |
62% | 60 | <50 yearsb: 40 (66.7%) >50 yearsb: 20 (33.3%) |
Higher educationa: 9 (15%) High schoola: 32 (53.3%) Upper secondary school or lowera: 19 (31.7%) |
68,3% | RR: 47 PPMS: 4 SPMS: 9 |
N.A. | BDI-II GAD-7 PSQI |
| Sbragia et al., 2021 | Italy | 106 | 43.1 (10.9) | 14.3 (2.9) | 69.8% | RR: 69 SP: 20 PP: 17 |
2.5 (1.5-5.5)d | HADS-D HADS-A |
||||
| Shaygannejad et al., 2020 | Iran | 245 | 34.2 (7.48) | 154 (62.9%)c | 75.5% | 223 | 35.8 (7.5) | 158 (70.9%)c | 82.1% | N.A. | 2 (1)d | DASS |
| Stojanov et al., 2020 | Serbia | 99 | 44.3 (9.3) | Primary studiesa: 33.3% Secondary studiesa: 43% University degreea: 23.7% |
66.3% | 95 | 43.4 (9.7) | Primary studiesa: 25.3% Secondary studiesa: 47.3% University degreea: 27.4% |
67.6% | RRMS = 95 | 3.6 (1.3) | HAM-D HAM-A MSQoL-54 |
| Talaat et al., 2020 | Egypt | 129 | 31.7 (8.8) | Schoola: 4 (3.2%) Faculty/institutea: 73 (57.9%) Postgraduatea: 49 (38.9%) |
77.4% | 115 | 34.4 (8.5) | Schoola: 22 (19.1%) Faculty/institutea: 81 (70.4%) Postgraduatea: 110 (95.7%) |
72.1% | RRMS = 96 PPMS = 3 SPMS = 16 |
2.2 (2.1) | DASS |
Notes. F(%) = percentage of females in the sample; HC = Healthy controls; pwMS = people with Multiple Sclerosis; MSQoL-54 = Multiple Sclerosis Quality of Life – 54; KSD = Karolinska Sleep Diary; PHQ-2 = Patient Health Questionnaire-2; PSS = Perceived Stress Scale; HADS-A= Hospital Anxiety Depression Scale – Anxiety Subscale; HADS-D= Hospital Anxiety Depression Scale – Depression Subscale; MSIS-29 = Multiple Sclerosis Impact Scale; Neuro-QoL=Quality of Life in Neurological Disorders measurement system; BAI = Beck Anxiety Inventory; PSQI=Pittsburgh Sleep Quality Index; DASS = Depression Anxiety Stress Scale; HAM-A= Hamilton anxiety scale; HAM-D = Hamilton depression scale.
= Data reported as number and/or % of educational qualification
= Data reported as number and % of people with education higher than diploma
= Data reported as number and% of people with education higher than diploma.
= Data reported as median and interquartile range or minimum-maximum
Table 2.
Time period of data collection during the COVID-19 pandemic and government response stringency index of primary studies.
| Study | Contry | Start data collection (date) | Government Response Stringency Index at the beginning of data collection (0: no restrictions – 100: strictest restrictions) | End data collection (date) | Government Response Stringency Index at the end of data collection (0: no restrictions – 100: strictest restrictions) |
|---|---|---|---|---|---|
| Andreu-Caravaca et al., 2020 | Spain | June 8, 2020 | 57.41 | June 12, 2020 | 57.41 |
| Bonavita et al., 2020 | Italy | April 1, 2020 | 85.19 | April 15, 2020 | 93.52 |
| Capuano et al., 2020 | Italy | April 16, 2020 | 85.19 | April 23, 2020 | 93.52 |
| Chiaravalloti et al., 2020 | Multicentric (Belgium, Canada, Denmark, United Kingdom, Italy, United States) | May 4, 2020 | Belgium: 81.48 Canada: 72.69 Denmark: 68.52 Italy: 75.00 United Kingdom: 79.63 United States: 72.69 |
July 5, 2020 | Belgium: 50.00 Canada: 68.98 Denmark:57.41 Italy: 67.59 United Kingdom: 69.91 United States: 68.98 |
| Costabile et al., 2020 | Italy | April 22, 2020 | 93.52 | May 7, 2020 | 75.00 |
| Demir et al., 2020 | Turkey | April 23, 2020 | 75.93 | April 23, 2020 | 75.93 |
| Garjani et al., 2021 | United Kingdom | May 22, 2020 | 79.63 | May 22, 2020 | 79.63 |
| Motolese et al., 2020 | Italy | Late April, 2020 | 93.52 | Early May, 2020 | 75.00 |
| Sbragia et al., 2021 | Italy | April 29, 2020 | 93.52 | May 6, 2020 | 75.00 |
| Shaygannejad et al., 2020 | Iran | March 8, 2020 | 42.59 | April 7, 2020 | 59.26 |
| Stojanov et al., 2020 | Serbia | April 1, 2020 | 100.00 | April 30, 2020 | 96.30 |
| Talaat et al., 2020 | Egypt | March 23, 2020 | 40.74 | April 4, 2020 | 84.26 |
3.2. Meta-analytic results: comparison of levels of psychological distress between pwMS and HC during the 2020 Covid-19 lockdown
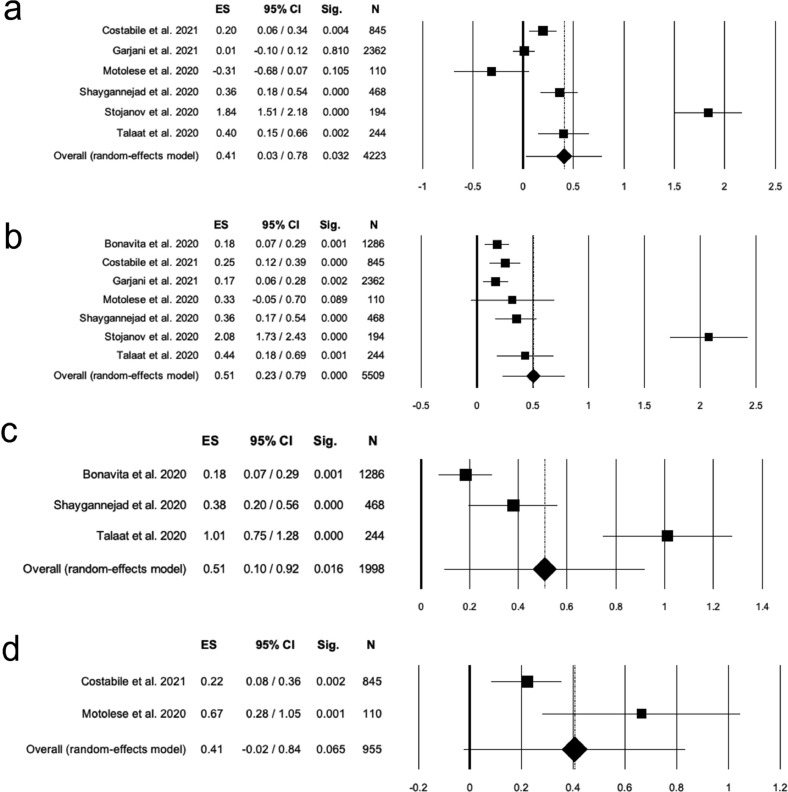
Anxiety: the pooled ES (Table 3 ; Fig. 2 a) was significant and moderate (N = 4223; k = 6; g = 0.41, 95% CI [.03, 0.78]; p=.032), with high inter-study heterogeneity (Q = 115.61, df=5, p<.001, I2=95.67). The publication bias was non-significant (t = 1.30, p=.265). After the sensitivity analysis, the removal of one study (Stojanov et al., 2020) lead to a non-significant ES (N = 4029; k = 5; g = 0.16, 95% CI [−0.03, 0.35]; p=.095); inter-study heterogeneity decreased but remained high (Q = 21.12, df =4, p<.001, I2=81.06), with a non-significant publication bias (t = 0.27, p=.804).
Table 3.
Summary of meta-analytic results.
| Domains/Outcomes | K | N | Pooled effect size Hedges’g (p) | 95% Confidence Intervals | Heterogeneity statistics | Egger's t test for publication bias (p) | Trim and fill | |||
|---|---|---|---|---|---|---|---|---|---|---|
| LL | UL | Q (df) | P | I2 | ||||||
| Comparison of levels of psychological distress between pwMS and HC during the Covid-19 pandemic | ||||||||||
| Depression | 7 | 5509 | 0.51 (0.001) | 0.23 | 0.79 | 111.60 (6) | <0.001 | 94.62 | 2.19 (0.080) | 0 |
| Anxiety | 6 | 4223 | 0.41 (0.032) | 0.03 | 0.78 | 115.61 (5) | <0.001 | 95.67 | 1.30 (0.265) | 0 |
| Sleep disturbances | 2 | 955 | 0.41 (0.065) | -0.02 | 0.84 | 4.60 (1) | 0.032 | 78.25 | - | - |
| Stress | 3 | 1998 | 0.51 (0.016) | 0.10 | 0.92 | 32.41 (2) | <0.001 | 93.83 | 3.30 (0.188) | 0 |
| Comparison of levels of psychological distress in pwMS before and during the Covid-19 lockdown | ||||||||||
| Depression | 6 | 2675 | 0.02 (0.772) | -0.10 | 0.13 | 14.19 (5) | 0.014 | 64.76 | 0.00 (0.997) | 0 |
| Anxiety | 6 | 2675 | 0.08 (0.380) | -0.10 | 0.26 | 38.12 (5) | <0.001 | 86.89 | 0.61 (0.572) | 0 |
| Mental QoL | 5 | 460 | -0.14 (0.060) | -0.28 | 0.01 | 8.31 (4) | 0.081 | 51.86 | -0.01 (0.992) | 0 |
| Physical QoL | 5 | 460 | 0.00 (0.986) | -0.10 | 0.10 | 4.56 (4) | 0.335 | 12.31 | 0.14 (0.900) | 0 |
| Sleep disturbances | 2 | 67 | 0.52 (<0.001) | 0.27 | 0.77 | 0.15 (1) | 0.703 | 0 | - | - |
K= number of studies; N= total number of participants; LL= Lower Limit; UP= Upper Limit; Q and I2 =heterogeneity statistics; df= degrees of freedom; pwMS = people with Multiple Sclerosis; HC = Healthy Controls. Statistically significant values are reported in bold.
Fig. 2.
Meta-analysis on comparison of levels of psychological distress between pwMS and HC during the 2020 Covid-19 lockdown. Forest plots for (A) anxiety, (B) depression, (C) stress, (D) sleep disturbances. ES = effect size; 95% CI = confidence intervals; Sig = statistical significance; N = total sample size.
Depression: the pooled ES (Table 3, Fig. 2b) was significant and moderate (N = 5509; k = 7; g = 0.51, 95% CI [.23, 0.79]; p< .001), with high and significant inter-study heterogeneity (Q = 111.60, df = 6, p<.001, I2= 94.62 and a non-significant publication bias (t = 2.19; p=.080). The sensitivity analysis revealed that by removing the study of (Stojanov et al., 2020), the pooled ES remained significant, but the magnitude of the effect became small (N = 5315; k = 6; g = 0.24, 95% CI [.17, 0.31]; p< .001), with non-significant heterogeneity (Q = 6.43, df =5, p=.267, I2=22.19) and a non-significant publication bias (t = 2.78, p=.051).
Stress: the pooled ES (Table 3, Fig. 2c) was moderate and significant (N = 1998; k = 3; g = 0.51, 95% CI [.10, 0.92]; p=.016); the inter-study heterogeneity was significant and high (Q = 32.41, df =2, p<.001, I2=93.83), but the publication bias was not significant (t = 3.30, p=.188). By removing (Shaygannejad et al., 2020) the ES became not significant (N = 1530; k = 2; g = 0.59, 95% CI [−0.22, 0.1.40]; p=.155), with high heterogeneity (Q = 31.92, df 1, p<.001, I2=96.87).
Sleepdisturbances: the meta-analysis revealed a non-significant pooled ES (Table 3, Fig. 2d) (N = 955; k = 2; g = 0.41, 95% CI [−0.02, 0.84]; p=.065), with high inter-study heterogeneity (Q = 4.60, df =1, p=.008, I2=74.77), with a non-significant publication bias (t=−0.62, p=.599).
3.3. Meta-analytic results: levels of psychological distress in pwMS before and during the 2020 Covid-19 lockdown
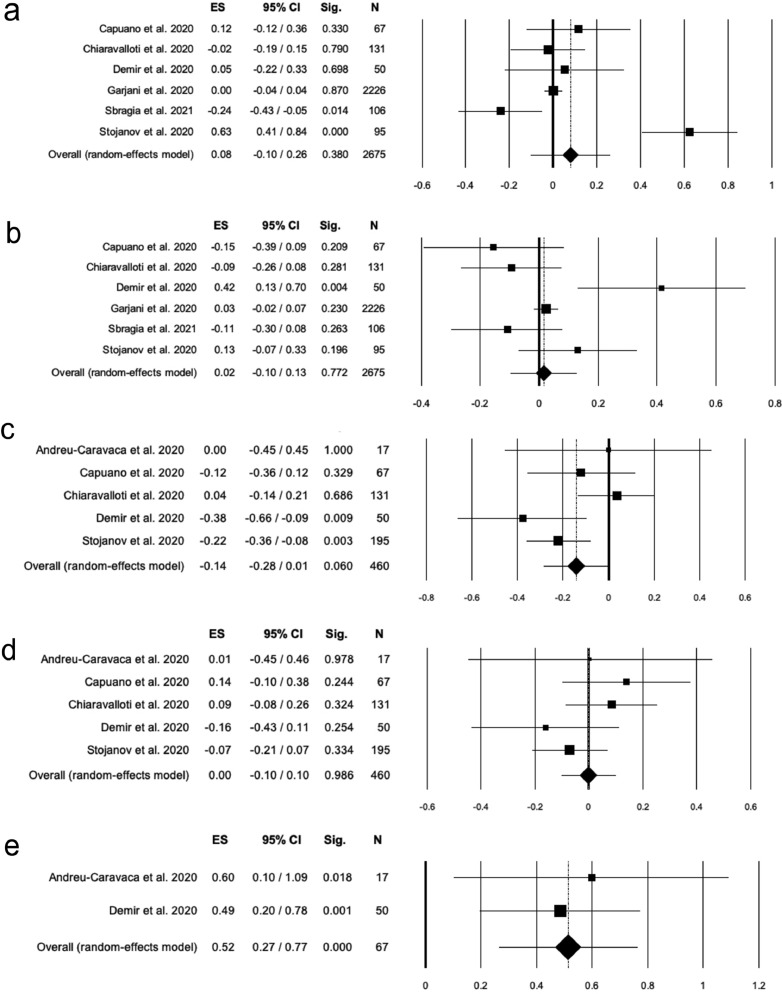
Anxiety: A non-significant pooled ES (see Table 3, Fig. 3 a) was found (N = 2674; k = 6; g = 0.08, 95% CI [.08, 0.26]; p=.383), with high and significant inter-study heterogeneity (Q = 38.24, df =5, p<.001, I2=86.93) and a non-significant publication bias (t = 0.63, p=.564). Removing each study, one at a time, did not change the magnitude of ES.
Fig. 3.
Meta-analysis on the comparison of levels of psychological distress in pwMS before and during the 2020 Covid-19 lockdown. Forest plots for (A) anxiety, (B) depression, (C) mental QoL, (D) physical QoL, (E) sleep disturbances. ES = effect size; 95% CI = confidence intervals; Sig = statistical significance; N = total sample size.
Depression: The pooled ES (Table 3, Fig. 3b) was not significant (N = 2674; k = 6; g = 0.02, 95% CI [−0.10, 0.13]; p=.782); the heterogeneity among studies was significant and moderate (Q = 14.13, df =5, p=.015, I2=64.62), and the publication bias was not significant (t = 0.02, p=.983).
Mental and physical QoL: Mental and physical QoL were entered in the meta-analysis as separate outcomes. As for mental QoL (Table 3, Fig. 3c), the pooled ES was small and non-significant (N = 460; k = 5; g= −0.14, 95% CI [−0.28, 0.01]; p=.060). The inter-study heterogeneity was not significant (Q = 8.31, df =4, p=.081, I2=51.86), and the publication bias was not significant (t=−0.01, p=.992). As regards physical QoL (Table 2, Fig. 3d), the results revealed a non-significant pooled ES (N = 460; k = 5; g = 0; 95% CI [−0.10, 0.10]; p=.986), with non-significant interstudy heterogeneity (Q = 4.56, df =4, p=.335, I2=12.31). The publication bias was not significant (t = 0.14, p=.90).
Sleep disturbances: The meta-analysis (see Table 3, Fig. 3e) revealed a moderate and significant pooled ES (N = 67; k = 2; g = 0.52, 95% CI [.27, 0.77]; p<.001), with non-significant inter-study heterogeneity (Q = 0.15, df =1, p=.703, I2=0). The publication bias could not be calculated due to the exiguity of primary studies.
4. Discussion
This meta-analytic study aimed at evaluating possible differences between pwMS and HC in the psychological consequences during the Covid-19 pandemic, and to explore whether the Covid-19 pandemic and restrictions increased the level of psychological distress within the pwMS population.
Studies carried on before the pandemic revealed that pwMS are at major risk of developing psychological disturbances than their healthy peers; as regards depressive disorders, (Patten et al., 2003) used data of a large-scale Canadian survey on 115.071 individuals and found that, in adults ranging from 18 to 45 years, the major depression prevalence was 25.7% in pwMS, and 8.9% in healthy peers, with the odds of having depression 2.3 times greater in pwMS with respect to HC. A more recent meta-analysis (Boeschoten et al., 2017) also found a higher pooled mean prevalence of a current depressive disorder in pwMS (17%) with respect with the annual prevalence rates of general population (2–10%). As for anxiety disorders, several studies found that pwMS show higher levels of anxiety with respect to their healthy peers, as revealed by Santangelo and colleagues (Santangelo et al., 2016), that found that pwMS scored significantly higher on both state-anxiety and trait-anxiety subscales of the State-Trait Anxiety Inventory than HC. Another study that examined population-based administrative Canadian data revealed that, compared to controls, pwMS patients had an elevated annual prevalence ratio of anxiety disorders of 1.46 (Marrie et al., 2017). Moreover, levels of stress in pwMS were, on average, slightly higher than those of a healthy population (Wu and Amtmann, 2013). Studies on sleep disturbances revealed that over 50% of pwMS have significant sleep problems (Stanton et al., 2006), and that these difficulties were significantly more frequent than the general population (Bamer et al., 2008).
In analogy with the abovementioned studies, the medium pooled ESs of our meta-analysis revealed that pwMS reported higher levels of anxiety, depression, and stress than HC during the Covid-19 pandemic. However, when considering the high inter-study heterogeneity and after performing a sensitivity analysis, the positive ESs were mainly ascribed to one study for anxiety and depression outcomes (Stojanov et al., 2020), and to another study (Shaygannejad et al., 2020) for the stress outcome. Accordingly, when these studies were removed from the analyses, the ES became not significant (for the anxiety and stress outcomes) or small (for the depression outcome). This may be due to methodological differences with respect with other studies, or, as in the case of (Stojanov et al., 2020), to the different severity of government restrictions at the time of the data collection. In fact, government restrictions in Serbia were the most restrictive according to the Government Response Stringency Index based on the database provided by Hale and colleagues (2021). Such restrictions may have caused more severe psychological disturbances in fragile people like pwMS compared to HC, with a significantly higher ES with respect with other studies on the same outcomes.
The results of our meta-analysis after sensitivity analysis, by revealing none-to-small differences on depression, anxiety and stress outcomes between pwMS and HC during the pandemic, let us argue that, since the Covid-19 pandemic had a strong impact on mental health and well-being in the general population (O'Connor et al., 2020), the expected differences in the psychological variables between pwMS and HC might have significantly attenuated. Further research is needed to corroborate these results.
When analyzing possible differences between pwMS and HC on sleep disturbances, a non-significant pooled ES between pwMS and HC was found, a finding not consistent with pre-pandemic literature (Stanton et al., 2006; Bamer et al., 2008). As regards sleep quality in general population during the Covid-19 pandemic, the results are contrasting: some studies reported a proportion of insomnia similar to the population prevalence in the pre-pandemic period (Gupta et al., 2020) whereas other studies highlighted a worsening of sleep disturbances during the pandemic (Gualano et al., 2020). It has to be noted, however, that no certain conclusion can be drawn from our results, since only two primary studies were available and added in our meta-analytic study
As for the second objective of our meta-analysis, aiming at exploring possible differences in the psychological distress of pwMS before and during the Covid-19 pandemic, we observed, indeed, a substantial stability of levels of anxiety, depression and mental and physical QoL in pwMS. The only significant and moderate ES was ascribed to the sleep disturbances outcome, with a reduction of sleep quality during the lockdown. However, this result must be taken with caution, because: a) the resulting ES derived from a pooled ES of only two studies, with a total sample size of 67 participants, and b) one study (Andreu-Caravaca et al., 2021) compared sleep quality before and few days after the end of home confinement, and not during the pandemic.
The stability of levels of psychological distress during the pandemic might seem surprising at first glance, but it may be due to the fact that most pwMS are already accustomed to high levels of anxiety, depression and low levels of QoL, and this may constitute a sort of “ceiling effect”. In fact, pwMS already had scores in the upper ranges, so it would have been harder to significantly increase their scores with respect to HC, which usually have/show lower levels of anxiety, depression, stress, and a higher QoL. Moreover, since the disease course of MS is unpredictable, pwMS may be more used to feelings of uncertainty with respect to their healthy peers, and therefore they may have already begun/been trained (the process of acquiring specific strategies) to cope with events characterized by extreme uncertainty (like a pandemic), unlike the HC group. Finally, most MS Centers provide psychological support to their patients and many of them continued to provide this service during the pandemic, so that many pwMS received psychological support and/or underwent specific programs to increase their resilience and coping abilities. This latter hypothesis, however, deserves to be further investigated, since this information was missing from primary studies.
This meta-analytic study is not exempt from limitations. Firstly, we could not assess possible causes of high inter-study heterogeneity due to the low number of primary studies. Indeed, since less than 10 studies were available for each outcome, it was not possible to perform a moderator analysis with a meta-regression approach (Borenstein et al., 2009). In our opinion, high heterogeneity could be ascribed to differences in the methodology of the study, different tools employed to evaluate the psychological status of pwMS and HC, and/or to the degree of severity of government restriction at the time of data collection of primary studies. Moreover, primary studies were conducted during the first wave of pandemic, so it was not possible to assess long-term consequences of the pandemic on the explored psychological outcomes. Future studies with a longer follow-up/observation period will have to address this issue/question in order to evaluate the long-term effects of Covid-19 pandemic on psychological distress of pwMS as compared to HC. Finally, for some outcomes of the meta-analysis (i.e., sleep disturbances) only two studies were available, so the findings could not be generalized.
In conclusion, our results revealed that, although pwMS seemed to show slightly higher levels of anxiety, depression, and stress than their healthy peers during the Covid-19 pandemic, we were not able to detect a significant increase of psychological distress in pwMS during the Covid-19 pandemic, compared to the pre-pandemic period/phase. Our result of a reduction of sleep quality in pwMS during the Covid-19 pandemic was based on a limited sample size and only on two primary studies, so future investigations are necessary.
Author contributions
MA: review concept and design, literature search, data extraction, statistical analyses, interpretation of data, drafting and revision of manuscript; GS and AG: review concept and design, interpretation of data, drafting and revision of manuscript; RC: data extraction, interpretation of data, drafting and revision of manuscript; AB, AdA, DB, GT: interpretation of data, drafting and revision of manuscript.
Declaration of Competing Interest
MA, RC, AdA, DB and GS have no disclosures. AB has received speaker honoraria and/or compensation for consulting service from Biogen, Merck and Genzyme. GT has received compensation for consulting services and/or speaking activities from Biogen, Novartis, Merck, Genzyme, Roche, Teva; and receives research support from Biogen Idec, Merck Serono, and Fondazione Italiana Sclerosi Multipla. AG received honoraria for speaking and travel grants from Merck, Genzyme, Teva, Mylan, Roche and Novartis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Al-Rahimi J.S., Nass N.M., Hassoubah S.A., Wazqar D.Y., Alamoudi S.A. Levels and predictors of fear and health anxiety during the current outbreak of COVID-19 in immunocompromised and chronic disease patients in Saudi Arabia: a cross-sectional correlational study. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0250554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreu-Caravaca L., Ramos-Campo D., Manonelles P., Abellán-Aynés O., Chung L.H., Rubio-Arias J.Á. Effect of COVID-19 home confinement on sleep monitorization and cardiac autonomic function in people with multiple sclerosis: a prospective cohort study. Physiol. behav. 2021;237 doi: 10.1016/j.physbeh.2021.113392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamer A., Johnson K., Amtmann D., Kraft G. Prevalence of sleep problems in individuals with multiple sclerosis. Multiple Sclerosis Journal. 2008;14:1127–1130. doi: 10.1177/1352458508092807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeschoten R.E., Braamse A.M.J., Beekman A.T.F., Cuijpers P., van Oppen P., Dekker J., Uitdehaag B.M.J. Prevalence of depression and anxiety in Multiple Sclerosis: a systematic review and meta-analysis. J. Neurol. Sci. 2017;372:331–341. doi: 10.1016/j.jns.2016.11.067. [DOI] [PubMed] [Google Scholar]
- Bonavita S., Sparaco M., Russo A., Borriello G., Lavorgna L. Perceived stress and social support in a large population of people with multiple sclerosis recruited online through the COVID-19 pandemic. Eur. J. Neurol. 2020 doi: 10.1111/ene.14697. [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H. John Wiley&Sons; Chichester, U.K: 2009. Introduction to Meta-Analysis. [Google Scholar]
- Capuano R., Altieri M., Bisecco A., d’Ambrosio A., Docimo R., Buonanno D., Matrone F., Giuliano F., Tedeschi G., Santangelo G., Gallo A. Psychological consequences of COVID-19 pandemic in Italian MS patients: signs of resilience? J. Neurol. 2021;268:743–750. doi: 10.1007/s00415-020-10099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiaravalloti N.D., Amato M.P., Brichetto G., Chataway J., Dalgas U., DeLuca J., Meza C., Moore N.B., Feys P., Filippi M., Freeman J., Inglese M., Motl R., Rocca M.A., Sandroff B.M., Salter A., Cutter G., Feinstein A. The emotional impact of the COVID-19 pandemic on individuals with progressive multiple sclerosis. J. Neurol. 2021;268:1598–1607. doi: 10.1007/s00415-020-10160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen G., Russo M.J., Campos J.A., Allegri R.F. COVID-19 Epidemic in Argentina: worsening of Behavioral Symptoms in Elderly Subjects With Dementia Living in the Community. Front Psychiatry. 2020;11:866. doi: 10.3389/fpsyt.2020.00866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costabile T., Carotenuto A., Lavorgna L., Borriello G., Moiola L., Inglese M., Petruzzo M., Trojsi F., Ianniello A., Nozzolillo A., Cellerino M., Boffa G., Rosa L., Servillo G., Moccia M., Bonavita S., Filippi M., Lanzillo R., Brescia Morra V., Petracca M. COVID-19 pandemic and mental distress in multiple sclerosis: implications for clinical management. Eur. J. Neurol. 2021;28:3375–3383. doi: 10.1111/ene.14580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demir C.F., Bilek F., Balgetir F. Neuropsychiatric changes during the COVID-19 pandemic in multiple sclerosis patients. Arq. Neuropsiquiatr. 2020;78:570–575. doi: 10.1590/0004-282X20200122. [DOI] [PubMed] [Google Scholar]
- Garjani A., Hunter R., Law G.R., Middleton R.M., Tuite-Dalton K.A., Dobson R., Ford D.V., Hughes S., Pearson O.R., Rog D., Tallantyre E.C., Nicholas R., Morriss R., Evangelou N., das Nair R. Mental health of people with multiple sclerosis during the COVID-19 outbreak: a prospective cohort and cross-sectional case–control study of the UK MS Register. Mult. Scler. J. 2021 doi: 10.1177/13524585211020435. [DOI] [PubMed] [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 Lockdown on Mental Health and Sleep Disturbances in Italy. Int. J. Environ. Res. Public Health. 2020;17:4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R., Grover S., Basu A., Krishnan V., Tripathi A., Subramanyam A., Nischal A., Hussain A., Mehra A., Ambekar A., Saha G., Mishra K.K., Bathla M., Jagiwala M., Manjunatha N., Nebhinani N., Gaur N., Kumar N., Dalal P.K., Kumar P., Midha P.K., Daga R., Tikka S.K., Praharaj S.K., Goyal S.K., Kanchan S., Sarkar S., Das S., Sarkhel S., Padhy S.K., Sahoo S., Satyanarayana Rao T.S., Dubey V., Menon V., Chhabra V., Lahan V., Avasthi A. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62:370–378. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., Webster S., Cameron-Blake E., Hallas L., Majumdar S., Tatlow H. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nat. hum. behav. 2021;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- Lebrasseur A., Fortin-Bédard N., Lettre J., Raymond E., Bussières E.L., Lapierre N., Faieta J., Vincent C., Duchesne L., Ouellet M.-.C., Gagnon E., Tourigny A., Lamontagne M.-.È., Routhier F. Impact of the COVID-19 Pandemic on Older Adults: rapid Review. JMIR Aging. 2021;4:e26474. doi: 10.2196/26474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrie R.A., Walld R., Bolton J.M., Sareen J., Walker J.R., Patten S.B., Singer A., Lix L.M., Hitchon C.A., El-Gabalawy R., Katz A., Fisk J.D., Bernstein C.N. Estimating annual prevalence of depression and anxiety disorder in multiple sclerosis using administrative data. BMC res. notes. 2017;10:619. doi: 10.1186/s13104-017-2958-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. Neurodegener Dis Manag. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motolese F., Rossi M., Albergo G., Stelitano D., Villanova M., Di Lazzaro V., Capone F. The Psychological Impact of COVID-19 Pandemic on People With Multiple Sclerosis. Front Neurol. 2020;11 doi: 10.3389/fneur.2020.580507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser Moghadasi A. One Aspect of Coronavirus disease (COVID-19) Outbreak in Iran: high Anxiety among MS Patients. Mult Scler Relat Disord. 2020;41 doi: 10.1016/j.msard.2020.102138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor R.C., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., O’Carroll R.E., O’Connor D.B., Platt S., Scowcroft E., Watson B., Zortea T., Ferguson E., Robb K.A. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paez A. Gray literature: an important resource in systematic reviews. J Evid Based Med. 2017;10:233–240. doi: 10.1111/jebm.12266. [DOI] [PubMed] [Google Scholar]
- Patten S.B., Beck C.A., Williams J.V.A., Barbui C., Metz L.M. Major depression in multiple sclerosis: a population-based perspective. Neurology. 2003;61:1524–1527. doi: 10.1212/01.wnl.0000095964.34294.b4. [DOI] [PubMed] [Google Scholar]
- Pietrabissa G., Simpson S.G. Psychological Consequences of Social Isolation During COVID-19 Outbreak. Front Psychol. 2020;11:2201. doi: 10.3389/fpsyg.2020.02201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santangelo G., Sacco R., Siciliano M., Bisecco A., Muzzo G., Docimo R., De Stefano M., Bonavita S., Lavorgna L., Tedeschi G., Trojano L., Gallo A. Anxiety in Multiple Sclerosis: psychometric properties of the State-Trait Anxiety Inventory. Acta Neurol. Scand. 2016;134:458–466. doi: 10.1111/ane.12564. [DOI] [PubMed] [Google Scholar]
- Sbragia E., Colombo E., Pollio C., Cellerino M., Lapucci C., Inglese M., Mancardi G., Boffa G. Embracing resilience in multiple sclerosis: a new perspective from COVID-19 pandemic. Psychol Health Med. 2021:1–9. doi: 10.1080/13548506.2021.1916964. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Shaygannejad V., Afshari-Safavi A., Hatef B. Assessment of mental health, knowledge, and attitude of patients with multiple sclerosis and neuromyelitis optica spectrum disorder in response to 2019 novel coronavirus. Neurol Sci. 2020:1–11. doi: 10.1007/s10072-020-04905-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton B.R., Barnes F., Silber E. Sleep and fatigue in multiple sclerosis. Mult. Scler. 2006;12:481–486. doi: 10.1191/135248506ms1320oa. [DOI] [PubMed] [Google Scholar]
- Stojanov A., Malobabic M., Milosevic V., Stojanov J., Vojinovic S., Stanojevic G., Stevic M. Psychological status of patients with relapsing-remitting multiple sclerosis during coronavirus disease-2019 outbreak. Mult. Scler. Relat. Disord. 2020;45 doi: 10.1016/j.msard.2020.102407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talaat F., Ramadan I., Aly S., Hamdy E. Are multiple sclerosis patients and their caregivers more anxious and more committed to following the basic preventive measures during the COVID-19 pandemic? Mult. Scler. Relat. Disord. 2020;46 doi: 10.1016/j.msard.2020.102580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Duan Z., Ma Z., Mao Y., Li X., Wilson A., Qin H., Ou J., Peng K., Zhou F., Li C., Liu Z., Chen R. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiatry. 2020;10:263. doi: 10.1038/s41398-020-00950-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Coronavirus disease (COVID-19). URL https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed 7.16.21). 2022.
- Wu S.M., Amtmann D. Psychometric evaluation of the perceived stress scale in multiple sclerosis: Int Sch Res Notice. 2013;9 doi: 10.1155/2013/608356. [DOI] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]