Abstract
Bladder leiomyomas are rare, benign tumors with a variety of clinical presentations. Surgical approach is typically based on symptomatology and leiomyoma location. Literature on robotic excision is limited. We present our case of a unique transvesical approach. The patient had rapid convalescence with no complications, suggesting robotic transvesical excision is a safe, effective treatment for bladder leiomyoma for suitable candidates.
1. Introduction
Bladder leiomyomas are rare, benign entities comprising 0.43% of all bladder tumors. While some leiomyomas cause symptoms such as irritative voiding symptoms, hematuria or obstruction, others are diagnosed incidentally.1 Treatment consists of surgical management which ranges from transurethral resection to partial cystectomy. Few cases of robotic leiomyoma excision exist in current literature.2
We present a rare surgical approach to bladder leiomyoma excision. Our surgical approach included robotic transvesical resection of an enlarging bladder leiomyoma.
2. Case presentation
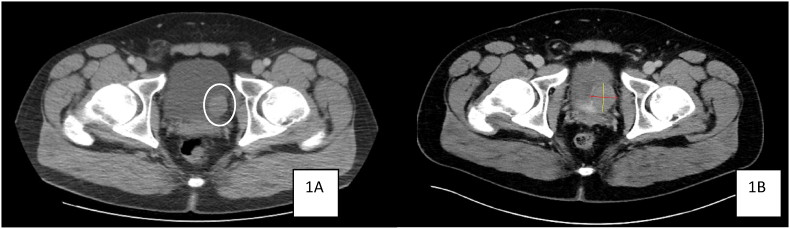
Our patient was a 30-year-old male with a history of a left lateral bladder wall mass found incidentally on imaging obtained for the evaluation of an umbilical hernia. The patient was otherwise healthy and presented to our clinic with an outside computed tomography (CT) scan showing a left-sided 2.7 x 3.0 × 2.3 cm bladder wall lesion (Fig. 1A). Laboratory workup was negative, and the decision was made to perform cystoscopy with transurethral biopsy of the bladder wall mass.
Fig. 1.
1A (left), 1B (right). Bladder wall lesion progression.
Biopsy confirmed a pathologic diagnosis of benign smooth muscle suggestive of leiomyoma, along with benign bladder mucosa. After counseling on the possibility of concealed malignant neoplasm, the patient decided to return in 6 months for repeat cross-sectional imaging. Repeat CT scan showed new peripheral calcification and increased size of the mass to 4.1 x 2.9 × 3.4 cm (Fig. 1B).
The patient was thoroughly counseled on management options, and he decided to proceed with robotic excision of the mass. At this point, the patient had developed some mild lower urinary tract symptoms as well which further influenced the decision for surgical management. Based on the location near the left lateral base of the bladder, the decision was made to perform cystourethroscopy with 5-french ureteral localizing stent placement at the time of surgery. Additionally, the decision was made to perform a transvesical approach to visualize the ureteral orifice more closely during the resection of the mass.
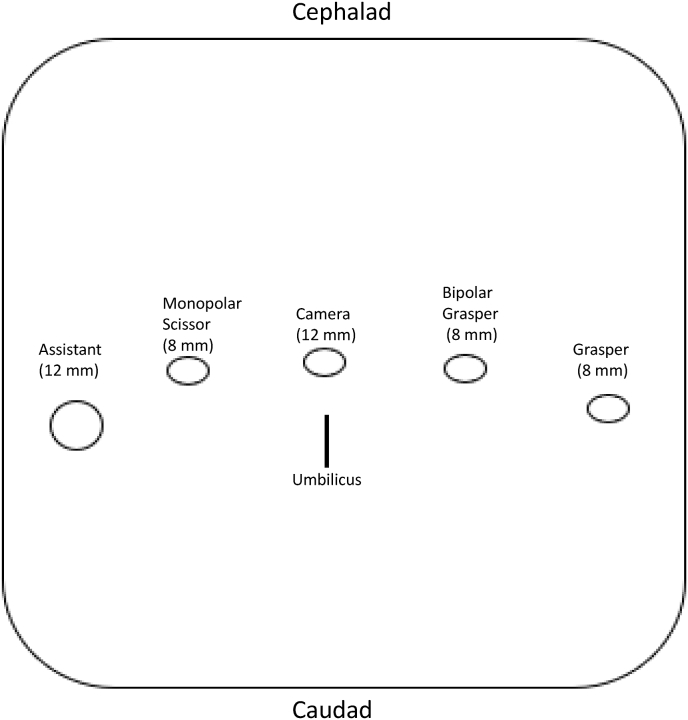
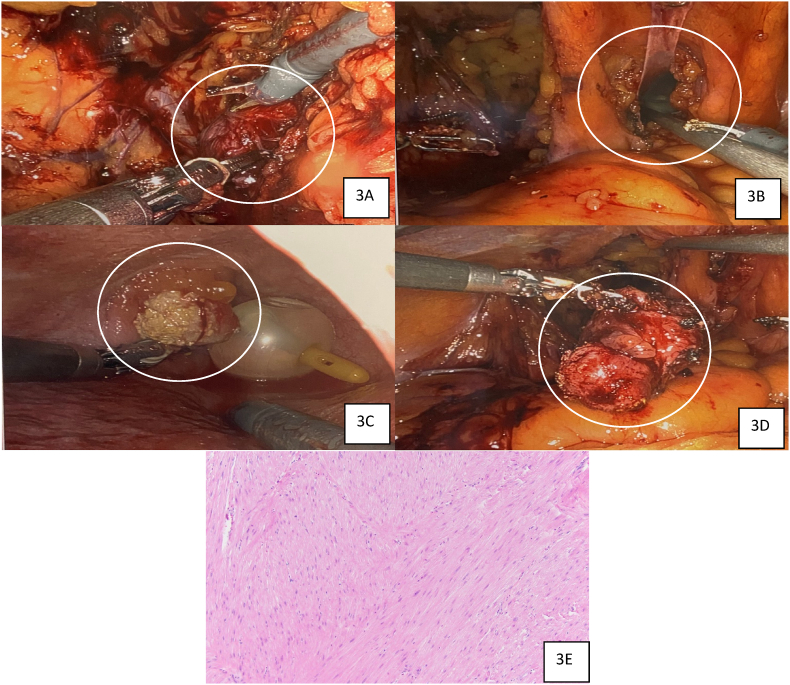
After cystourethroscopy with left ureteral stent placement, a 20-french Foley catheter was placed, and we pursued the robotic portion of the case. Standard port placement for robotic cystectomy was used (Fig. 2). The left ureter was identified below the iliac vessels and dissected to the level of the ureterovesical junction to ensure there was no involvement of the mass with the ureter and to separate the ureter from the excision. The mass was noted and outlined with cautery around the borders of the mass (Fig. 3A). A 3cm, midline cystotomy was made over the bladder dome with a small handle used for retraction (Fig. 3B). The mass was identified inside the bladder and excised from inside to outside taking note of the left ureteral orifice (Fig. 3C). The mass was freed and eventually removed through the camera port-site (Fig. 3D).
Fig. 2.
Port placement.
Fig. 3.
3A (upper left, excision of the leiomyoma), 3B (upper right, surgical cystotomy for transvesical approach), 3C (middle left, leiomyoma as seen from inside the bladder), 3D (middle right, leiomyoma excised and held in robotic arm), 3E (bottom middle, 400X microscopic analysis showing smooth muscle cells without mitotic figures or necrosis consistent with leiomyoma). Robotic Surgical Field Views of Leiomyoma Excision and Pathologic Confirmation.
The cystotomy at the left lateral side was closed with a running 2-0 Vicryl suture in 2 layers as was the cystotomy at the dome. A new 7-french, 26cm double-J stent was placed with fluoroscopic guidance to ensure there were no edematous side effects or healing changes to the left ureteral orifice. A new 20-french Foley catheter was placed.
There were no complications, and the patient's catheter and stent were removed approximately 3 weeks later. Final pathology showed leiomyoma with calcifications and no malignancy (Fig. 3E). At the last visit, the patient had no voiding symptoms and was recovering well.
3. Discussion
Bladder leiomyomas are rare, although they are the most common nonepithelial, benign bladder tumor. While some leiomyomas can cause symptoms, others may be found incidentally. Surgical resection is the mainstay treatment for leiomyoma with laparoscopic and robotic excision having been performed.2, 3, 4
There are no cases documented of malignant transformation of bladder leiomyoma. If patients are asymptomatic and there is certainty of a leiomyoma diagnosis, patients can typically be monitored.5 If there is growth of the leiomyoma or onset of symptoms, surgical treatment is typically necessary.
To our knowledge, there is limited literature on the robotic excision of bladder leiomyomas. This appears to be the first documented case of transvesical excision of a bladder leiomyoma using the Da Vinci Xi system (Intuitive Surgical, Sunnyvale, CA).
4. Conclusion
Bladder leiomyomas are rare with variable symptoms ranging from pain to gross hematuria to obstructive lower urinary tract symptoms. With limited data on the robotic excision of bladder leiomyoma, we present favorable outcomes associated with a robotic transvesical approach.
Acknowledgements
This research did not receive any specific grant or funding from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Zachariou A., Filiponi M., Dimitriadis F., Kaltsas A., Sofikitis N. Transurethral resection of a bladder trigone leiomyoma: a rare case report. BMC Urol. 2020;20(1):152. doi: 10.1186/s12894-020-00722-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thiel D.D., Williams B.F., Krishna M., Leroy T.J., Igel T.C. Robot-assisted laparoscopic excision of bladder wall leiomyoma. J Endourol. 2009;23(4):579–582. doi: 10.1089/end.2008.0621. discussion 582. [DOI] [PubMed] [Google Scholar]
- 3.Patrozos K., Westphal J., Trawinski J., Wagner W. [Total laparoscopic excision of a leiomyoma of the urinary bladder -- a case report] Aktuelle Urol. 2005;36(1):58–60. doi: 10.1055/s-2004-818527. [DOI] [PubMed] [Google Scholar]
- 4.Yoshioka T., Kawakita M., Kameoka H. Cystoscope-Assisted laparoscopic enucleation of a large progressive bladder leiomyoma. J Endourol Case Rep. 2019;5(3):120–123. doi: 10.1089/cren.2019.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornella J.L., Larson T.R., Lee R.A., Magrina J.F., Kammerer-Doak D. Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am J Obstet Gynecol. 1997;176(6):1278–1285. doi: 10.1016/s0002-9378(97)70346-6. [DOI] [PubMed] [Google Scholar]