Abstract
Background
Adolescents and young adults (AYA) in the United States, and in Washington, District of Columbia (DC), specifically, are disproportionately affected by HIV. Both the national Ending the HIV Epidemic initiative and DC-specific plans emphasize HIV testing, and innovative strategies to encourage testing among AYA are needed.
Objective
The purpose of this study is to identify sexual behaviors, HIV knowledge, HIV perceptions (eg, susceptibility and severity), and perceived barriers and facilitators to HIV testing among AYA at risk for HIV in DC.
Methods
This study was part of a larger study to determine the acceptability of using a life-and-dating simulation game to increase HIV testing among AYA. Focus groups and surveys stratified by self-reported sexual orientation were conducted among, and administered to, AYA aged 13-24 years in DC. HIV knowledge was explored during focus groups and measured using an adapted version of the Brief HIV Knowledge Questionnaire. Survey data were summarized using descriptive statistics and compared by self-reported sexual orientation. Transcripts were thematically analyzed.
Results
Of the 46 AYA who participated in the focus groups, 30 (65%) identified as heterosexual and 16 (35%) as lesbian, gay, bisexual, transgender, or queer. A higher proportion of lesbian, gay, bisexual, transgender, or queer AYA reported sexual activity (12/16, 75%, vs 18/30, 60%), condomless sex (11/12, 92%, vs 15/18, 83%), and HIV testing (13/16, 81%, vs 17/29, 58%) than heterosexual AYA. HIV prevention (“condoms” and “...PrEP”) and transmission (“exchange of fluids”) knowledge was high, and most (34/44, 77%) of the AYA perceived HIV testing as beneficial. However, the AYA also demonstrated some misinformation concerning HIV: an average of 67% (31/46; SD 0.474) of the participants believed that an HIV test could deliver accurate results 1 week after a potential exposure and an average of 72% (33/46; SD 0.455) believed that an HIV vaccine exists. The AYA also identified individual (“...people...are scared”), interpersonal (“it’s an awkward conversation”), and structural (“...people don’t...know where they can go”) barriers to testing. Most of the AYA indicated that they were very likely to use the demonstrated game prototype to help with getting tested for HIV (median 3.0, IQR 2.0-3.0, using a scale ranging from 0 to 3, with 3 indicating high likelihood) and strongly agreed that the game was interesting (median 5.0, IQR 5.0-5.0), fun (median 5.0, IQR 4.0-5.0), and easy to learn (median 5.0, IQR 5.0-5.0, using a scale ranging from 1 to 5, with 5 indicating strong agreement).
Conclusions
These results suggest a need for multilevel HIV testing interventions and informed the development of a mobile health intervention aiming to increase HIV knowledge and risk perception among AYA, while reducing barriers to testing at the individual and structural levels, supporting efforts to end the domestic HIV epidemic.
Keywords: youth, HIV, knowledge, testing
Introduction
HIV Among Adolescents and Young Adults in the United States
Adolescents and young adults (AYA) aged 13-24 years are disproportionately affected by HIV in the United States. Among the estimated HIV transmissions in 2016, AYA had the highest transmission rate of all age groups [1]. In 2019, AYA accounted for 21% of the new HIV infections, and young men who have sex with men (YMSM) and transgender women who identified as Black or Latinx were severely affected [2]. Approximately 50% of the AYA living with HIV in the United States are unaware of their infection and are more likely to be unaware of their infection than any other age group [2,3]. Nevertheless, once AYA are diagnosed, they often reduce their sexual risk behaviors, which limits the risk of infecting others [4-6]. In addition, AYA who are diagnosed with HIV early in the course of their infection can access antiretroviral therapy to slow disease progression and reduce mortality [4].
HIV Among AYA in Washington, District of Columbia
Just as HIV infections and diagnoses in the United States are not evenly distributed across different ages, races and ethnicities, genders, and modes of transmission, they are more concentrated in certain geographic locations than in others. The southern United States, which includes Washington, District of Columbia (DC), accounted for 53% of the new diagnoses in 2019 despite being home to just 38% of the population [7]. In DC specifically—a metropolitan area that also includes parts of Maryland, Virginia, and West Virginia—AYA are disproportionately affected by HIV, with those aged 13-24 years accounting for 21% of the new diagnoses in 2019 [8]. Furthermore, Black AYA and YMSM in DC accounted for 75% and 60%, respectively, of the new HIV diagnoses among AYA in 2019 [9]. The recently launched Ending the HIV Epidemic in the U.S. (EHE) initiative aims to end the domestic HIV epidemic by 2030, and the first strategy includes ensuring that HIV testing is widely available to diagnose infections as early as possible [10]. DC is among several localities across the nation considered geographic HIV hotspots that will be the focus of initial EHE efforts [10]. The DC-specific plan to end the HIV epidemic also includes emphasis on HIV testing and timely diagnosis [11], and DC’s Youth Sexual Health Plan [12] has the explicit goal of reducing the unintended consequences of condomless sex among AYA (eg, HIV infection) by increasing use of sexual and reproductive health services, including HIV testing.
Lack of HIV Testing Among AYA
Despite engaging in high-risk behaviors [13-19] and the existence of national guidelines that support routine HIV testing among persons aged 13-64 years [19,20], AYA do not regularly seek nor are they routinely offered testing for HIV. Barriers to HIV testing among AYA include privacy concerns, parental involvement, inconvenient clinic times, providers not assessing sexual behavior, cost, low access, and low health literacy [21-25]. Furthermore, AYA may have limited knowledge of HIV [26-29] and underestimate their risk for infection [21,25,30]. In DC, differences in perceived access to HIV education exist among AYA based on sexual orientation. According to the 2019 Youth Risk Behavior Survey (YRBS), heterosexual middle school students in DC were more likely to report either not being taught or not being sure that they were taught about HIV/AIDS in school than lesbian, gay, and bisexual middle school students [31]. YRBS data also suggest that high-risk behaviors among youth in DC differ based on sexual orientation. Among middle school and high school students who reported sexual activity on the 2019 YRBS, lesbian, gay, and bisexual students were more likely to report having condomless sex during their last sexual encounter than heterosexual students [31,32].
Potential of Mobile Health Interventions and Study Objectives
Innovative strategies to overcome these barriers and increase HIV testing among AYA include social media campaigns [33,34] and mobile health (mHealth) interventions [35,36], both of which have been endorsed by the Centers for Disease Control and Prevention (CDC) to reduce HIV risk and improve sexual health among adolescents [37]. New mHealth interventions for HIV treatment and prevention have been developed specifically for AYA in urban areas [35,36,38-42]. These interventions transcend traditional behavior modification approaches to HIV prevention and incorporate adolescent-friendly and -informed models that support the design and development of mHealth interventions. The purpose of this study is to identify sexual behaviors, HIV knowledge, HIV perceptions (eg, susceptibility and severity), and perceived barriers and facilitators to HIV testing among AYA at risk for HIV and to identify potential differences based on self-reported sexual orientation. The results from this study were used to inform the development of an mHealth intervention aiming to increase HIV testing among AYA living in DC.
Methods
Data Collection
The study was conducted as part of a larger study to determine the acceptability of using a life-and-dating simulation game to increase HIV testing among AYA; the methods have been described elsewhere [43]. The game will allow AYA to play characters that are similar to, or different from, their gender identity. The character can then spend their leisure time meeting new people and engaging in relationship scenarios—including implied sexual activity—tailored to both same-sex and opposite-sex couples. On the basis of in-game sexual activity, AYA will be shown their character’s risk of acquiring HIV and be allowed to locate nearby AYA-friendly testing locations. Guided by the Health Belief Model [44]—a widely used framework to explain and predict individual-level changes to health-related behavior [44] and to assess HIV testing uptake specifically [45-48]—we hypothesized that the game would increase perceived susceptibility to HIV infection, perceived severity of HIV infection, perceived benefits of HIV testing, motivation to test, and self-efficacy to test while decreasing perceived barriers to testing among the study participants (Figure 1).
Figure 1.
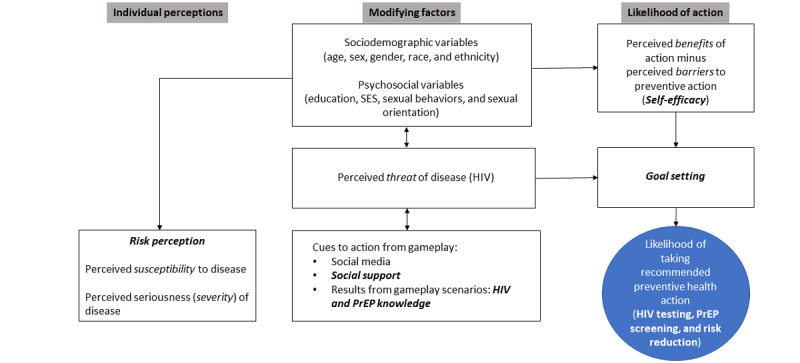
Conceptual framework for assessing HIV testing uptake among adolescents and young adults. PrEP: pre-exposure prophylaxis; SES: socioeconomic status.
From February 2017 to December 2017, HIV-negative or status-unknown AYA aged 13-24 years who were living in the DC metro area were recruited from an adolescent health center during routine visits, 2 community-based organizations, and a youth advisory council [43]. Recruitment was primarily facilitated by CT, a female researcher. Of the 52 AYA approached for the study, 6 (12%) declined to participate; the reasons for refusal included lack of time to undergo the eligibility screening process or not being available on the date of the focus group. To assess the baseline perceptions of AYA regarding HIV susceptibility and severity as well as potential benefits of, and barriers to, testing, we conducted a series of focus group discussions that lasted 50-120 minutes and were held at the adolescent health center, a local community-based organization, and a DC government building where the youth advisory council met. Focus group discussions, stratified by sexual orientation, were facilitated by ADC (a female researcher) using a semistructured focus group guide and covered the following topics: HIV knowledge, perceptions and personal experiences regarding HIV testing, and perceived barriers and facilitators to HIV testing. The focus group guide can be found in Multimedia Appendix 1.
Next, DG (a male researcher) demonstrated the game to participants and asked questions related to game acceptability. The game showed two dating scenarios: one at a house party and one at a skateboard park. DG controlled a character that had the freedom to go wherever they wanted in the 3D environment and talk to other AYA in the game by selecting from a menu of dialogue options. These conversations, combined with the player’s actions, resulted in the player’s character becoming friends, rivals, or dating partners with the people they met. Participants played the game as a group by voting on the actions and dialogue options the player character should choose in navigating dating scenarios. When the player managed to negotiate sex with another character in the game, the participants chose the kinds of sex acts the characters would engage in and whether a condom would be used. The sex acts were not depicted graphically but rather implied by fireworks, and the screen abruptly transitioned to a depiction of the risk of the sex acts chosen based on the CDC Risk Estimator Tool. The player then had the option of seeing a map of nearby HIV testing providers, with the ability to select low-cost and free options. Participants could replay the game, trying other options and seeing other outcomes.
Focus groups continued until data saturation—the point at which new data repeat data already collected [49]—was met, which occurred after 7 focus groups. Before the start of each focus group, participants completed a survey that collected information on their sociodemographic characteristics, HIV knowledge and HIV testing patterns, sexual behaviors and perceptions regarding susceptibility to HIV, self-efficacy to get tested for HIV, and barriers and benefits to HIV testing. As in the case of other research assessing HIV knowledge using a limited number of questions [50,51], HIV knowledge in this study was measured using an adapted version of the Brief HIV Knowledge Questionnaire that included 11 of the 18 questions [52]. After the game demonstration, the AYA completed a brief survey to assess game acceptability. All AYA participants were remunerated with gift cards and transportation vouchers for their participation in each focus group.
Data Analysis
All focus groups were audio recorded and professionally transcribed, and transcripts were imported into NVivo 11 (QSR International) for data analysis. Initial codes were deductively derived: BW created a codebook containing a priori codes based on the topics included in the semistructured focus group guide, and 2 coders (BW and THH) conducted independent thematic coding to link the common themes and ideas discussed among study participants in each respective focus group [53]. Next, the coders reconvened to reach intercoder agreement through reconciliation of discrepant coding. Specific themes across focus group data were developed based on patterns of shared or similar meaning identified through codes ascribed to each respondent’s feedback. Finally, final codes across focus groups and coders were compared to generate overall themes that supported the purpose of the study. In addition to focus groups, data collected from surveys were summarized using descriptive statistics in SAS 9.3 (SAS Institute Inc) by BW. Survey responses related to demographics, sexual behavior, and risk perception were stratified by self-reported sexual orientation; frequencies and percentages were used to describe categorical variables, whereas mean and range or mean and SD were used to describe continuous variables. To describe acceptability of the game prototype, survey responses were stratified by self-reported sexual orientation and median values were reported for each survey item.
Ethics Approval
Study materials were reviewed and approved by the George Washington University Institutional Review Board (IRB) (number 051602) and the Children's National Hospital IRB.
Results
AYA Demographics, Sexual Risk Behaviors, and Perceptions
Of the 46 AYA who participated in the focus groups, 30 (65%) identified as heterosexual and 16 (35%) identified as lesbian, gay, bisexual, transgender, or queer (LGBTQ; Table 1). The mean age of participants was 17.6 (SD 2.110; range 13-24) years, 85% (39/46) were Black, and 63% (29/46) were female. Most of the participants lived in DC (44/46, 96%), and 67% (30/45) had not yet graduated from high school. Higher proportions of the LGBTQ participants reported engaging in sexual activity (12/16, 75%, vs 18/30, 60%), having a history of condomless sex (11/12, 92% vs 15/18, 83%), and previous testing for HIV (13/16, 81%, vs 17/29, 59%). Most (41/44, 93%) of the participants perceived HIV infection to be severe or very severe (Table 1).
Table 1.
Demographics, HIV testing, and risk behaviors of adolescents and young adults and their peers (N=46).
| Demographics and sexual behaviors | Heterosexual (n=30)a | LGBTQb (n=16)a | Total (N=46)a | |||||||
| Age (years), mean (SD; range) | 17.1 (1.776; 13-23) | 18.6 (2.391; 15-24) | 17.6 (2.110; 13-24) | |||||||
| Gender, n (%) | ||||||||||
|
|
Male | 10 (33) | 6 (38) | 16 (35) | ||||||
|
|
Female | 20 (67) | 9 (56) | 29 (63) | ||||||
|
|
Transgender | 0 (0) | 1 (6) | 1 (2) | ||||||
| Race and ethnicity, n (%) | ||||||||||
|
|
Hispanic | 2 (7) | 1 (6) | 3 (6) | ||||||
|
|
Non-Hispanic Black | 26 (87) | 13 (81) | 39 (85) | ||||||
|
|
Non-Hispanic White | 1 (3) | 0 (0) | 1 (2) | ||||||
|
|
Other | 1 (3) | 2 (13) | 3 (6) | ||||||
| State of residence, n (%) | ||||||||||
|
|
Washington, District of Columbia | 28 (93) | 16 (100) | 44 (96) | ||||||
|
|
Maryland | 2 (7) | 0 (0) | 2 (4) | ||||||
| Highest level of education, n (%) | ||||||||||
|
|
Grade 8-11 | 23 (77) | 7c (47) | 30d (67) | ||||||
|
|
High school graduate | 6 (20) | 5c (33) | 11d (24) | ||||||
|
|
At least some college | 1 (3) | 3c (20) | 4d (9) | ||||||
| Ever tested for HIV, n (%) | 17e (58) | 13 (81) | 30d (67) | |||||||
| Location of most recent test: physician’s office, n (%) | 4f (23) | 6g (46) | 10c (33) | |||||||
| Reason for testing: offered a free test, n (%) | 8f (47) | 6g (46) | 14h (47) | |||||||
| Reason never tested: not sexually active, n (%) | 5i (50) | 0j (0) | 5g (38) | |||||||
| Ever sexually active, n (%) | 18 (60) | 12 (75) | 30 (65) | |||||||
| Condomless sex ever, n (%) | 15k (83) | 11l (92) | 26h (87) | |||||||
| Percentage of time spent... (VASm), mean (SD) | ||||||||||
|
|
Engaging in risky behavior | 8 (14) | 12 (22) | 10 (77) | ||||||
|
|
Using condoms consistently | 63 (38) | 40 (38) | 54 (39) | ||||||
| Risk perception (perceived benefit of HIV testing: beneficial or very beneficial), n (%) | 23 (76) | 11n (79) | 34o (77) | |||||||
| Perceived ease of...p, n (%) | ||||||||||
|
|
Finding a testing location | 27 (90) | 11(69) | 38 (83) | ||||||
|
|
Getting parental permission for testing | 13 (43) | 9 (56) | 22 (48) | ||||||
|
|
Paying for testing | 18 (60) | 5c (33) | 23d (51) | ||||||
|
|
Disclosing sexual orientation to health care provider or tester | 20q (69) | 7 (44) | 27d (60) | ||||||
| Likelihood of infection (VAS), mean (SD) | 13 (28) | 14 (27) | 13 (28) | |||||||
| Perceived severity of HIV infection: severe or very severe, n (%) | 29 (97) | 12n (86) | 41o (93) | |||||||
| Percentage of friends who... (VAS), mean (SD) | ||||||||||
|
|
Are sexually active | 54 (36) | 41 (36) | 50 (36) | ||||||
|
|
Engage in risky behavior | 25 (27) | 20 (27) | 23 (27) | ||||||
|
|
Use condoms | 67 (36) | 46 (35) | 60 (37) | ||||||
|
|
Have been tested for HIV | 42 (34) | 41 (39) | 42 (35) | ||||||
aTotals may not sum to N (100%) because of missing data.
bLGBTQ: lesbian, gay, bisexual, transgender, or queer.
cn=15.
dn=45.
en=29.
fn=17.
gn=13.
hn=30.
in=10.
jn=3.
kn=18.
ln=12.
mVAS: visual analog scale (0%-100%).
nn=14.
on=44.
pReporting on the combined categories of easy and very easy.
qn=19.
Regarding their perceived risk of acquiring HIV, on a scale of 0%-100%, the reported likelihood of HIV infection among heterosexual AYA (mean 13%, SD 28%) was similar to that of LGBTQ AYA (mean 14%, SD 27%). Most (34/44, 77%) of the participants perceived HIV testing to be beneficial or very beneficial (Table 1). Furthermore, most of the participants perceived finding a testing location (38/46, 83%), paying for testing (23/45, 51%), and disclosing their sexual orientation during testing (27/45, 60%) to be easy or very easy.
HIV Knowledge and Perceptions
Qualitatively, both heterosexual and LGBTQ AYA expressed an advanced understanding of HIV and of the differences between HIV and AIDS (Table 2). An LGBTQ participant explained that HIV “...attacks your immune system” and a heterosexual participant explained that AIDS “...is like the worst...it’s like after your T-cells gets to a certain amount then you have AIDS.” Both groups of AYA similarly expressed an advanced understanding of HIV prevention strategies and modes of transmission. A heterosexual participant stated of HIV prevention “if you’re going to have sex...know your partner...know their status,” and an LGBTQ participant stated that HIV could be transmitted through “exchange of fluids.” However, both groups also stated myths and misunderstandings about HIV prevention and transmission. Regarding HIV, an LGBTQ participant asked, “...can you get it from urine?” and a heterosexual participant asked, “Is there some kind of vaccine you can take?” In addition, regardless of sexual orientation, both groups held both negative and positive perceptions about HIV. A heterosexual participant shared, “It takes away your sexual life...,” whereas an LGBTQ participant felt “you still have a second chance to live...So, if you’re still alive I think that you should...say ‘I’m still here, I’m still sexy.’” On the basis of the adapted Brief HIV Knowledge Questionnaire, there were only two items for which the average number of participants responding correctly was <50%: an average of 33% (SD 0.474) of the participants knew that HIV infection could not be determined by taking an HIV test 1 week after a potential exposure and an average of 28% (SD 0.455) knew that a vaccine for HIV does not exist (Table 3).
Table 2.
Summary of focus group themes related to HIV knowledge.
| Themes and subthemes | Representative quotes | ||
| HIV knowledge | |||
|
|
General |
|
|
|
|
Prevention |
|
|
|
|
Transmission |
|
|
|
|
Myths and misunderstandings |
|
|
| Perceptions regarding HIV: severity |
|
||
aLGBTQ: lesbian, gay, bisexual, transgender, or queer.
bPrEP: pre-exposure prophylaxis.
cSTD: sexually transmitted disease.
Table 3.
Individual item means and SDs for the adapted Brief HIV Knowledge Questionnaire among adolescents and young adults.
|
|
Values, meana (SD) |
| There is a female condom that can help decrease a woman’s chance of getting HIV (Tb) | 80 (0.401) |
| People who have been infected with HIV quickly show serious signs of being infected (Fc) | 76 (0.431) |
| Having sex with more than one partner can increase a person’s chance of being infected with HIV (T) | 69 (0.465) |
| A person can get HIV from oral sex (T) | 63 (0.488) |
| A person can get HIV by sharing a glass of water with someone who has HIV (F) | 61 (0.493) |
| A person can get HIV by sitting in a hot tub or a swimming pool with a person who has HIV (F) | 61 (0.493) |
| Using Vaseline or baby oil with condoms lowers the chance of getting HIV (F) | 61 (0.493) |
| All pregnant women infected with HIV will have babies born with AIDS (F) | 61 (0.493) |
| Coughing and sneezing DO NOT spread HIV (T) | 58 (0.497) |
| Taking a test for HIV one week after having sex will tell a person if she or he has HIV (F) | 33 (0.474) |
| There is a vaccine that can stop people from getting HIV (F) | 28 (0.455) |
| Average total correct score (of 11 items) | 6.52 (2.681) |
aMean indicates the average percentage of participants who answered the question correctly.
bT: true.
cF: false.
Barriers and Facilitators to HIV Testing
During the focus group discussions, the heterosexual and LGBTQ participants described their perceptions of the benefits of HIV testing, prior experiences with HIV testing using various testing modalities, and their perceived barriers and facilitators to HIV testing (Table 4). Regarding HIV testing, a heterosexual participant felt that it should be done even if you are not sexually active: “...I still would say it’s best that you do it just so you...get into the habit of getting tested.” An LGBTQ participant thought that HIV testing should be offered on college campuses because of the risky behaviors of students: “...’cause I know...campuses...are very risky.” When describing their personal experiences with HIV testing, a heterosexual participant explained not knowing that they needed to explicitly opt out: “...I didn’t know they tested me. And so, when they took my blood to find out if I had something else...they was like ‘everything’s negative...HIV negative.’” An LGBTQ participant shared being surprised by the different options for HIV testing: “The first time I did mine it was interesting ’cause I thought you had to get the needle...I got the swab and was kinda surprised.”
Table 4.
Summary of focus group themes related to perceived barriers and facilitators to HIV testing.
| Themes | Representative quotes |
| Perceived benefits |
|
| Personal experiences |
|
| Perceived barriers to testing |
|
| Perceived facilitators to testing |
|
aLGBTQ: lesbian, gay, bisexual, transgender, or queer.
Regarding perceived barriers to HIV testing, at the individual level, the participants identified fear and a sense of invincibility among AYA. An LGBTQ participant explained: “...with us being so young we believe that we have a whole life ahead of us...some people wouldn’t want to get tested because...they want to ignore it.” At the interpersonal level, a heterosexual participant cited the lack of parental support as a potential barrier to testing: “...because my mom would be like ‘what are you doing that would warrant you to go get tested?’...And so, it’s an awkward conversation.” At the structural level, an LGBTQ participant explained that if AYA “...don’t even know where they can go,” they might not get tested for HIV. Regarding perceived facilitators to HIV testing, the participants identified factors at the individual and structural levels. An LGBTQ participant felt that, on an individual level, AYA should be intrinsically motivated to get tested: “It shouldn’t have to be a material motive...you should be willing to just go and get tested without something in it for you.” On a structural level, a heterosexual participant thought that if commercials and advertisements “...showed where the free clinics are it would help,” whereas another LGBTQ participant posited that HIV testing efforts should try “...to appeal to...people using social media...like...Facebook, Twitter, Instagram, and Snapchat...So, like you can definitely submit those sponsored ads to say you know ‘hey get tested.’”
Acceptability of Game Prototype
In addition to the engaging focus group discussions, brief surveys using Likert scales were used to evaluate acceptability of the game prototype among AYA (Table 5). On a scale of 1 to 5, with 5 indicating strong agreement, most of the participants agreed that the game was interesting (median 5.0, IQR 5.0-5.0), fun (median 5.0, IQR 4.0-5.0), and easy to learn (median 5.0, IQR 5.0-5.0). Most of the participants also liked the game environment (median 5.0, IQR 4.0-5.0), the game interface (median 5.0, IQR 5.0-5.0), the interactions with other characters in the game (median 5.0, IQR 4.0-5.0), the idea of playing games about behaviors that may be associated with HIV infection (median 5.0, IQR 5.0-5.0), and the idea of playing games about different dating scenarios (median 5.0, IQR 5.0-5.0). Participants also agreed that they would share the game with friends to help them get tested for HIV (median 5.0, IQR 4.0-5.0).
Table 5.
Acceptability of game prototype stratified by sexual orientation (N=46).
| Item | Heterosexual (n=30), median (IQR) | LGBTQa (n=16), median (IQR) | Total (N=46), median (IQR) |
| The game playing was very interestingb | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) |
| The game playing was funb | 5.0 (5.0-5.0) | 5.0 (4.0-5.0) | 5.0 (4.0-5.0) |
| It was easy to learn how to play the gameb | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) |
| I liked the art and animationb | 5.0 (4.0-5.0) | 5.0 (4.0-5.0) | 5.0 (4.0-5.0) |
| I liked the game environmentb | 5.0 (4.0-5.0) | 4.0 (4.0-5.0) | 5.0 (4.0-5.0) |
| I liked the game interfaceb | 5.0 (5.0-5.0) | 5.0 (4.0-5.0) | 5.0 (5.0-5.0) |
| I like the interactions with other characters in the gameb | 5.0 (4.0-5.0) | 5.0 (4.0-5.0) | 5.0 (4.0-5.0) |
| I like the idea of playing games about behaviors that may be associated with HIV infectionb | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) |
| I like the idea of playing games where my character can meet people and make friendsb | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) |
| I like the idea of playing games about different dating scenariosb | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) | 5.0 (5.0-5.0) |
| I would share the game with friends or people I know to help them get tested for HIVb | 5.0 (4.0-5.0) | 5.0 (4.0-5.0) | 5.0 (4.0-5.0) |
| I would play these games if I had access to themc | 3.0 (2.0-3.0) | 3.0 (3.0-3.0) | 3.0 (2.0-3.0) |
| I would recommend the games to a friendc | 3.0 (2.0-3.0) | 3.0 (2.0-3.0) | 3.0 (2.0-3.0) |
| I would be interested in playing these games in multiplayer mode with my friendsc | 3.0 (2.0-3.0) | 3.0 (2.5-3.0) | 3.0 (2.0-3.0) |
| I would use this game to help with getting tested for HIVc | 2.0 (2.0-3.0) | 3.0 (2.0-3.0) | 3.0 (2.0-3.0) |
| I would be more likely to get tested for HIV if the game determined my character to be at risk for HIV infectionc | 3.0 (2.0-3.0) | 3.0 (3.0-3.0) | 3.0 (2.0-3.0) |
| I would be more likely to get tested if the game connected me with an actual person who could help me get testedc | 3.0 (1.0-3.0) | 3.0 (2.0-3.0) | 3.0 (2.0-3.0) |
aLGBTQ: lesbian, gay, bisexual, transgender, or queer.
bResponses provided on a scale of 1 to 5: strongly agree (5), somewhat agree (4), neither agree nor disagree (3), disagree (2), strongly disagree (1).
cResponses provided on a scale of 0 to 3: very likely (3), somewhat likely (2), not at all likely (1), don’t know (0).
Using a separate Likert scale with a range of 0 to 3, with 3 indicating high likelihood, participants reported that they would play the game if it were available to them (median 3.0, IQR 2.0-3.0), they would use this game to help with getting tested for HIV (median 3.0, IQR 2.0-3.0), they would be more likely to get tested for HIV if the game determined their character to be at risk for HIV infection (median 3.0, SD 2.0-3.0), and they would be more likely to get tested if the game connected them with an actual person who could help (median 3.0, IQR 2.0-3.0).
Discussion
Principal Findings
The key findings of this study conducted among AYA in DC include a high level of engagement in sexual behaviors that increase the risk of HIV acquisition, a high level of HIV knowledge, and the identification of perceived barriers and facilitators to HIV testing at multiple levels. The findings from the study informed the development of an intervention to increase HIV testing among AYA. As in other studies, AYA in our study engaged in behaviors that might put them at risk for HIV, such as sexual activity and condomless sex [16,17,54,55], with a higher proportion of LGBTQ AYA engaging in these behaviors than heterosexual AYA [3,56]. However, the proportion of AYA in our study having ever been tested for HIV was much higher than that reported in other studies (67% vs 22%-34% in other studies) [14,16,17,54]. This may be the result of DC-wide efforts to increase HIV testing and education among AYA to curb new infections [11,57]. Furthermore, a higher proportion of LGBTQ AYA in our study had been tested for HIV than heterosexual AYA, consistent with other research [55,58].
Compared with AYA in other studies [27-29], the AYA in our study displayed relatively high HIV knowledge, and there were no differences in knowledge between LGBTQ and heterosexual AYA. Again, this may be the result of jurisdiction-wide efforts to increase HIV education among AYA. However, the participants expressed some persistent misconceptions around modes of transmission, the existence of a vaccine, and the appropriate window period for testing after a potential exposure, implying a need for continued education of AYA. The participants also perceived barriers to testing at the individual, interpersonal, and structural level, suggesting a need for multilevel interventions. Get Connected, one such intervention, is a web-based intervention that aims to reduce individual and structural barriers to HIV and sexually transmitted infection testing and pre-exposure prophylaxis access among YMSM in Philadelphia, Atlanta, and Houston by tailoring content based on individual sociodemographic characteristics, testing history, and sexual behavior and only referring participants to culturally competent, high-quality testing and pre-exposure prophylaxis sites [35].
Limitations
Our study includes several limitations that warrant discussion. First, our study used convenience sampling by recruiting from specific organizations. Thus, our findings may not be generalizable to AYA who do not routinely seek medical care, do not frequent the participating community-based organizations, and are not part of the youth advisory council. The study included a small number of focus group participants, although this is common in qualitative research. Furthermore, most of the participants identified as Black or African American. Although the racial distribution of the study could have been broader to increase the generalizability of the findings, the racial distribution of our study population reflects the high burden of, and risk for, infection among Black AYA in the United States and in DC specifically. Similarly, the generalizability of the study’s findings to AYA of other sexual orientations may be limited because most of the AYA in our study identified as heterosexual.
Implications for Research
Achieving the first strategy of the EHE initiative will depend in part on maximizing the perceived benefits of, and minimizing the perceived barriers to, HIV testing among key populations, including AYA. Toward that goal, this study provides useful information because we were able to determine the behaviors potentially placing AYA at risk for HIV, measure baseline HIV knowledge, assess perceived barriers and facilitators to HIV testing, and assess acceptability of the game prototype. These data informed the development of an mHealth intervention, a life-and-dating simulation game, tailored for, and guided by, AYA in an urban area that aims to increase the perceived susceptibility to, and knowledge of, HIV infection of AYA; increase the perceived benefits of HIV testing, motivation to test, and self-efficacy to test; and decrease the perceived barriers to testing among AYA. These aims will be achieved by displaying the consequences of unsafe sexual behavior in real time using the CDC Risk Estimator Tool while also providing a zip code testing locator and empowering messaging around testing to further facilitate access to convenient testing sites [43]. The efficacy of this intervention will be tested in a randomized controlled trial, and the results will, we hope, reduce barriers to HIV testing faced by AYA and further reduce new infections among this key population.
Acknowledgments
The research reported in this paper was fully supported by the National Institutes of Health’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (R43HD088332). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to acknowledge the providers and staff at Children’s National Hospital, the administrators of the participating community-based organizations and other organizations from which adolescents and young adults were recruited, and all the adolescents and young adults who participated in this study.
Abbreviations
- AYA
adolescents and young adults
- CDC
Centers for Disease Control and Prevention
- DC
Washington, District of Columbia
- EHE
Ending the HIV Epidemic in the U.S.
- LGBTQ
lesbian, gay, bisexual, transgender, or queer
- mHealth
mobile health
- YMSM
young men who have sex with men
- YRBS
Youth Risk Behavior Survey
Focus group guide.
Footnotes
Conflicts of Interest: DG, a principal investigator on the grant, has a stake in Media Rez consistent with the policy on small business innovation research.
References
- 1.Li Z, Purcell DW, Sansom SL, Hayes D, Hall HI. Vital signs: HIV transmission along the continuum of care - United States, 2016. MMWR Morb Mortal Wkly Rep. 2019;68(11):267–72. doi: 10.15585/mmwr.mm6811e1. doi: 10.15585/mmwr.mm6811e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Estimated HIV incidence and prevalence in the United States, 2015-2019. Centers for Disease Control and Prevention. 2021. [2021-03-29]. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-26-1.pdf .
- 3.Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Lim C, Bradford D, Yamakawa Y, Leon M, Brener N, Ethier KA. Youth risk behavior surveillance - United States, 2017. MMWR Surveill Summ. 2018;67(8):1–114. doi: 10.15585/mmwr.ss6708a1. http://europepmc.org/abstract/MED/29902162 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–53. doi: 10.1097/01.qai.0000151079.33935.79.00126334-200508010-00013 [DOI] [PubMed] [Google Scholar]
- 5.Rotheram-Borus MJ, Futterman D. Promoting early detection of human immunodeficiency virus infection among adolescents. Arch Pediatr Adolesc Med. 2000;154(5):435–9. doi: 10.1001/archpedi.154.5.435. [DOI] [PubMed] [Google Scholar]
- 6.Weinhardt LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a meta-analytic review of published research, 1985-1997. Am J Public Health. 1999;89(9):1397–405. doi: 10.2105/ajph.89.9.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diagnoses of HIV infection in the United States and dependent areas, 2019. Centers for Disease Control and Prevention. 2021. [2021-03-29]. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-updated-vol-32.pdf .
- 8.District of Columbia Department of Health. 2020. [2021-03-29]. https://dchealth.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/2020-HAHSTA-Annual-Surveillance-Report-Appendix.pdf .
- 9.District of Columbia Department of Health. 2020. [2021-03-29]. https://dchealth.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/2020-HAHSTA-Annual-Surveillance-Report.pdf .
- 10.What is ending the HIV epidemic in the U.S.? United States Department of Health and Human Services. 2019. [2021-03-29]. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview .
- 11.90/90/90/50 plan: ending the epidemic in the District of Columbia by 2020. District of Columbia Department of Health. 2016. [2021-03-29]. https://dchealth.dc.gov/page/90909050-plan-ending-epidemic-district-columbia-2020 .
- 12.Youth sexual health plan: District of Columbia 2016-2020. District of Columbia Department of Health. 2016. [2021-03-29]. https://tinyurl.com/3dhkayf3 .
- 13.Branson BM, Viall A, Marum E. Expanding HIV testing: back to the future. J Acquir Immune Defic Syndr. 2013;63 Suppl 2:S117–21. doi: 10.1097/QAI.0b013e3182986f25.00126334-201307012-00002 [DOI] [PubMed] [Google Scholar]
- 14.Inungu J, Lewis A, Mustafa Y, Wood J, O'Brien S, Verdun D. HIV testing among adolescents and youth in the United States: update from the 2009 behavioral risk factor surveillance system. Open AIDS J. 2011;5:80–5. doi: 10.2174/1874613601105010080. http://europepmc.org/abstract/MED/21915233 .TOAIDJ-5-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma M, Malcolm L, Diaz-Albertini K, Klinoff VA. HIV testing characteristics among Hispanic adolescents. J Community Health. 2016;41(1):11–4. doi: 10.1007/s10900-015-0056-7.10.1007/s10900-015-0056-7 [DOI] [PubMed] [Google Scholar]
- 16.Schnall R, Rojas M, Travers J. Understanding HIV testing behaviors of minority adolescents: a health behavior model analysis. J Assoc Nurses AIDS Care. 2015;26(3):246–58. doi: 10.1016/j.jana.2014.08.005. http://europepmc.org/abstract/MED/25283353 .S1055-3290(14)00211-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swenson RR, Rizzo CJ, Brown LK, Payne N, DiClemente RJ, Salazar LF, Vanable PA, Carey MP, Valois RF, Romer D, Hennessy M. Prevalence and correlates of HIV testing among sexually active African American adolescents in 4 US cities. Sex Transm Dis. 2009;36(9):584–91. doi: 10.1097/OLQ.0b013e3181b4704c. http://europepmc.org/abstract/MED/19661840 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Handel M, Kann L, Olsen EO, Dietz P. HIV testing among US high school students and young adults. Pediatrics. 2016;137(2):e20152700. doi: 10.1542/peds.2015-2700.peds.2015-2700 [DOI] [PubMed] [Google Scholar]
- 19.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, Clark JE, Centers for Disease Control and Prevention (CDC) Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm .rr5514a1 [PubMed] [Google Scholar]
- 20.US Preventive Services Task Force. Owens DK, Davidson KW, Krist AH, Barry MJ, Cabana M, Caughey AB, Curry SJ, Doubeni CA, Epling Jr JW, Kubik M, Landefeld CS, Mangione CM, Pbert L, Silverstein M, Simon MA, Tseng CW, Wong JB. Screening for HIV infection: US preventive services task force recommendation statement. JAMA. 2019;321(23):2326–36. doi: 10.1001/jama.2019.6587.2735345 [DOI] [PubMed] [Google Scholar]
- 21.Committee on Pediatric AIDS. Emmanuel PJ, Martinez J. Adolescents and HIV infection: the pediatrician's role in promoting routine testing. Pediatrics. 2011;128(5):1023–9. doi: 10.1542/peds.2011-1761.peds.2011-1761 [DOI] [PubMed] [Google Scholar]
- 22.Dimmitt Champion J, Harlin B, Collins JL. Sexual risk behavior and STI health literacy among ethnic minority adolescent women. Appl Nurs Res. 2013;26(4):204–9. doi: 10.1016/j.apnr.2013.06.003. http://europepmc.org/abstract/MED/23867137 .S0897-1897(13)00044-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goyal MK, Witt R, Hayes KL, Zaoutis TE, Gerber JS. Clinician adherence to recommendations for screening of adolescents for sexual activity and sexually transmitted infection/human immunodeficiency virus. J Pediatr. 2014;165(2):343–7. doi: 10.1016/j.jpeds.2014.04.009. http://europepmc.org/abstract/MED/24840761 .S0022-3476(14)00337-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hyden C, Allegrante JP, Cohall AT. HIV testing sites' communication about adolescent confidentiality: potential barriers and facilitators to testing. Health Promot Pract. 2014;15(2):173–80. doi: 10.1177/1524839913499347.1524839913499347 [DOI] [PubMed] [Google Scholar]
- 25.Peralta L, Deeds BG, Hipszer S, Ghalib K. Barriers and facilitators to adolescent HIV testing. AIDS Patient Care STDS. 2007;21(6):400–8. doi: 10.1089/apc.2006.0112. [DOI] [PubMed] [Google Scholar]
- 26.Gurvey J, Adler N, Ellen JM. Factors associated with self-risk perception for sexually transmitted diseases among adolescents. Sex Transm Dis. 2005;32(12):742–4. doi: 10.1097/01.olq.0000175385.23447.27.00007435-200512000-00006 [DOI] [PubMed] [Google Scholar]
- 27.Míguez MJ, Espinoza LA, Vargas ME, Perez C, Ergon E, Tarter R. Low HIV/AIDS knowledge among Hispanic adolescents. J AIDS Clin Res. 2015;6(7):483. doi: 10.4172/2155-6113.1000483. http://europepmc.org/abstract/MED/30627475 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swenson RR, Rizzo CJ, Brown LK, Vanable PA, Carey MP, Valois RF, DiClemente RJ, Romer D. HIV knowledge and its contribution to sexual health behaviors of low-income African American adolescents. J Natl Med Assoc. 2010;102(12):1173–82. doi: 10.1016/s0027-9684(15)30772-0. http://europepmc.org/abstract/MED/21287898 .S0027-9684(15)30772-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Udell W, Donenberg G. Remembering the basics: African American youth and HIV knowledge - brief report. J Natl Med Assoc. 2015;107(3):20–4. doi: 10.1016/S0027-9684(15)30047-X.S0027-9684(15)30047-X [DOI] [PubMed] [Google Scholar]
- 30.Murphy DA, Mitchell R, Vermund SH, Futterman D, Adolescent Medicine HIV/AIDS Research Network Factors associated with HIV testing among HIV-positive and HIV-negative high-risk adolescents: the REACH study. Reaching for Excellence in Adolescent Care and Health. Pediatrics. 2002;110(3):e36. doi: 10.1542/peds.110.3.e36. [DOI] [PubMed] [Google Scholar]
- 31.2019 youth risk behavior survey results: District of Columbia middle school survey: risk behaviors and sexual identity report. District of Columbia Office of the State Superintendent of Education. 2019. [2021-03-29]. https://osse.dc.gov/sites/default/files/dc/sites/osse/page_content/attachments/2019DCBM%20Sexual%20Identity.pdf .
- 32.2019 youth risk behavior survey results: District of Columbia high school survey: risk behaviors and sexual identity report. District of Columbia Office of the State Superintendent of Education. 2019. [2021-03-29]. https://osse.dc.gov/sites/default/files/dc/sites/osse/page_content/attachments/2019DCBH%20Sexual%20Identity.pdf .
- 33.Dowshen N, Lee S, Matty Lehman BM, Castillo M, Mollen C. IknowUshould2: feasibility of a youth-driven social media campaign to promote STI and HIV testing among adolescents in Philadelphia. AIDS Behav. 2015;19 Suppl 2(0 2):106–11. doi: 10.1007/s10461-014-0991-9. http://europepmc.org/abstract/MED/25563502 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McFarlane M, Brookmeyer K, Friedman A, Habel M, Kachur R, Hogben M. GYT: get yourself tested campaign awareness: associations with sexually transmitted disease/HIV testing and communication behaviors among youth. Sex Transm Dis. 2015;42(11):619–24. doi: 10.1097/OLQ.0000000000000361. http://europepmc.org/abstract/MED/26457487 .00007435-201511000-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauermeister JA, Golinkoff JM, Horvath KJ, Hightow-Weidman LB, Sullivan PS, Stephenson R. A multilevel tailored web app-based intervention for linking young men who have sex with men to quality care (get connected): protocol for a randomized controlled trial. JMIR Res Protoc. 2018;7(8):e10444. doi: 10.2196/10444. https://www.researchprotocols.org/2018/8/e10444/ v7i8e10444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mustanski B, Parsons JT, Sullivan PS, Madkins K, Rosenberg E, Swann G. Biomedical and behavioral outcomes of keep it up!: an eHealth HIV prevention program RCT. Am J Prev Med. 2018;55(2):151–8. doi: 10.1016/j.amepre.2018.04.026. http://europepmc.org/abstract/MED/29937115 .S0749-3797(18)31733-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kachur R, Mesnick J, Liddon N, Kapsimalis C, Habel M, David-Ferdon C, Brown K, Gloppen K, Tevendale H, Gelaude DJ, Romero L, Seitz H, Heldman AB, Schindelar J. Adolescents, technology and reducing risk for HIV, STDs, and pregnancy. Centers for Disease Control and Prevention. 2013. [2021-03-29]. https://www.cdc.gov/std/life-stages-populations/adolescents-white-paper.pdf .
- 38.Castel AD, Qasmieh S, Greenberg D, Ellenberger N, Howell TH, Griffith C, Wilbourn BC, Ganesan K, Hussein N, Ralte G, Rakhmanina N. Digital gaming to improve adherence among adolescents and young adults living with HIV: mixed-methods study to test feasibility and acceptability. JMIR Serious Games. 2018;6(4):e10213. doi: 10.2196/10213. https://games.jmir.org/2018/4/e10213/ v6i4e10213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cordova D, Alers-Rojas F, Lua FM, Bauermeister J, Nurenberg R, Ovadje L, Fessler K, Delva J, Salas-Wright CP, Youth Leadership Council The usability and acceptability of an adolescent mHealth HIV/STI and drug abuse preventive intervention in primary care. Behav Med. 2018;44(1):36–47. doi: 10.1080/08964289.2016.1189396. http://europepmc.org/abstract/MED/27223646 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones J, Dominguez K, Stephenson R, Stekler JD, Castel AD, Mena LA, Jenness SM, Siegler AJ, Sullivan PS. A theoretically based mobile app to increase pre-exposure prophylaxis uptake among men who have sex with men: protocol for a randomized controlled trial. JMIR Res Protoc. 2020;9(2):e16231. doi: 10.2196/16231. https://www.researchprotocols.org/2020/2/e16231/ v9i2e16231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kuhns LM, Garofalo R, Hidalgo M, Hirshfield S, Pearson C, Bruce J, Batey DS, Radix A, Belkind U, Jia H, Schnall R. A randomized controlled efficacy trial of an mHealth HIV prevention intervention for sexual minority young men: MyPEEPS mobile study protocol. BMC Public Health. 2020;20(1):65. doi: 10.1186/s12889-020-8180-4. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-8180-4 .10.1186/s12889-020-8180-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pendergrass T, Hieftje K, Duncan L, Fiellin L. Videogame intervention to encourage HIV testing and counseling among adolescents. Mhealth. 2020;6:26. doi: 10.21037/mhealth.2020.01.05. doi: 10.21037/mhealth.2020.01.05.mh-06-2020.01.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilbourn B, Howell TH, Castel AD, D'Angelo L, Trexler C, Carr R, Greenberg D. Development, refinement, and acceptability of digital gaming to improve HIV testing among adolescents and young adults at risk for HIV. Games Health J. 2020;9(1):53–63. doi: 10.1089/g4h.2018.0162. http://europepmc.org/abstract/MED/31560218 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 45.Dorr N, Krueckeberg S, Strathman A, Wood MD. Psychosocial correlates of voluntary HIV antibody testing in college students. AIDS Educ Prev. 1999;11(1):14–27. [PubMed] [Google Scholar]
- 46.Povinelli M, Remafedi G, Tao G. Trends and predictors of human immunodeficiency virus antibody testing by homosexual and bisexual adolescent males, 1989-1994. Arch Pediatr Adolesc Med. 1996;150(1):33–8. doi: 10.1001/archpedi.1996.02170260037005. [DOI] [PubMed] [Google Scholar]
- 47.Rosenstock IM, Strecher VJ, Becker MH. The health belief model and HIV risk behavior change. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: theories and methods of behavioral interventions. New York, NY: Plenum Press; 1994. pp. 6–24. [Google Scholar]
- 48.Thomas R, Cahill J, Santilli L. Using an interactive computer game to increase skill and self-efficacy regarding safer sex negotiation: field test results. Health Educ Behav. 1997;24(1):71–86. doi: 10.1177/109019819702400108. [DOI] [PubMed] [Google Scholar]
- 49.Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. doi: 10.1177/1525822X05279903. [DOI] [Google Scholar]
- 50.Heckman TG, Kelly JA, Sikkema K, Cargill V, Norman A, Fuqua W, Wagstaff D, Solomon L, Roffman R, Crumble D, Perry M, Winett R, Anderson E, Mercer MB, Hoffman R. HIV risk characteristics of young adult, adult, and older adult women who live in inner-city housing developments: implications for prevention. J Womens Health (Larchmt) 1995;4(4):397–406. doi: 10.1089/jwh.1995.4.397. [DOI] [Google Scholar]
- 51.Healthy Oakland teens: healthy Oakland teens description and explanation of study instrument. University of California San Francisco Department of Medicine. [2021-03-29]. https://prevention.ucsf.edu/research-project/healthy-oakland-teens-0 .
- 52.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14(2):172–82. doi: 10.1521/aeap.14.2.172.23902. http://europepmc.org/abstract/MED/12000234 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Charmaz K. Grounded theory. In: Smith JA, editor. Qualitative psychology: a practical guide to research methods. Thousand Oaks, CA: Sage Publications; 2007. [Google Scholar]
- 54.Coeytaux K, Kramer MR, Sullivan PS. HIV testing among United States high school students at the state and national level, Youth Risk Behavior Survey 2005-2011. Springerplus. 2014;3:202. doi: 10.1186/2193-1801-3-202. http://europepmc.org/abstract/MED/24855587 .944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Straub DM, Arrington-Sanders R, Harris DR, Willard N, Kapogiannis B, Emmanuel P, Futterman D, Ellen JM, Adolescent Trials Network for HIV/AIDS Interventions Correlates of HIV testing history among urban youth recruited through venue-based testing in 15 US cities. Sex Transm Dis. 2011;38(8):691–6. doi: 10.1097/OLQ.0b013e318214bb70. http://europepmc.org/abstract/MED/21758020 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mojola SA, Everett B. STD and HIV risk factors among U.S. young adults: variations by gender, race, ethnicity and sexual orientation. Perspect Sex Reprod Health. 2012;44(2):125–33. doi: 10.1363/4412512. http://europepmc.org/abstract/MED/22681428 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rakhmanina N, Messenger N, Phillips 2nd G, Teach S, Morrison S, Hern J, Payne J, Ganesan K, Castel AD. Factors affecting acceptance of routine human immunodeficiency virus screening by adolescents in pediatric emergency departments. J Adolesc Health. 2014;54(2):176–82. doi: 10.1016/j.jadohealth.2013.07.027.S1054-139X(13)00409-6 [DOI] [PubMed] [Google Scholar]
- 58.Adebayo OW, Gonzalez-Guarda RM. Factors associated with HIV testing in youth in the United States: an integrative review. J Assoc Nurses AIDS Care. 2017;28(3):342–62. doi: 10.1016/j.jana.2016.11.006.S1055-3290(16)30200-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Focus group guide.


