Abstract
Missile embolism as a consequence of gunshot wounds is a rare occurrence, and can lead to severe complications such as endocarditis, pulmonary thromboembolism and arrythmias. The correct diagnosis of bullet embolism can be challenging in an emergency care setting, often requiring a combination of clinical, radiological and surgical resources. The management of a venous missile embolism depends on characteristics such as size and location of the projectile, and must be highly individualized for each patient. In this report, a case of bullet embolism to the heart in a patient who suffered a gunshot wound to the left subclavian vein provides a backdrop for the discussion of the diagnosis and treatment of this rare ballistic injury.
Keywords: Trauma, Gunshot injury, Gunshot wound, Ballistic embolism, Bullet embolism, Missile embolism
Abbreviations: ME, Missile embolism; CT, Computerized tomography
Highlights
-
•
Missile embolism is a rare complication of gunshot wounds, usually caused by small-caliber bullets.
-
•
Most cases of missile embolism involve veins, with the projectile eventually migrating to the right ventricle or the pulmonary artery.
-
•
A projectile migrating to the heart may cause severe complications, such as endocarditis, thrombosis, pneumonia and arrythmias.
-
•
Surgical intervention is recommended for the majority of intracardiac projectiles, particularly when they are >5mm.
Introduction
Missile embolism (ME) is a rare consequence of ballistic injuries such as gunshot wounds, consisting in the traumatic penetration of a blood vessel by a foreign body (usually a bullet or pellet), which then proceeds to migrate along the trajectory of the vessel to a different part of the body. In most cases, ME results from injuries caused by small-caliber bullets with relatively low kinetic energy [1]. As the projectile loses velocity during passage through soft tissues, its kinetic energy progressively decreases [1], [2]. By the time the projectile penetrates a blood vessel, the kinetic energy of the blood flow is able to overcome the kinetic energy of the bullet, which is then able to penetrate only one wall of the blood vessel, remaining in its lumen, from where it is then propelled by the circulation to different segments of that vessel, other blood vessels or to the heart chambers [2]. ME can occur in arterial or venous blood vessels, with arterial embolization of a projectile usually causing more immediate symptoms, secondary to arterial obstruction and ischemia of the corresponding tissues [3]. Therefore, arterial emboli should always be extracted, either by endovascular treatment or open surgery [4].
Venous blood vessels are the more frequently affected by ME, with the inferior vena cava (25%), femoral veins (15%) and subclavian veins (10%) being the most common entry sites for the missile [3]. In most cases of venous ME, the projectile eventually migrates to the heart, particularly to the right-sided chambers.
Case report
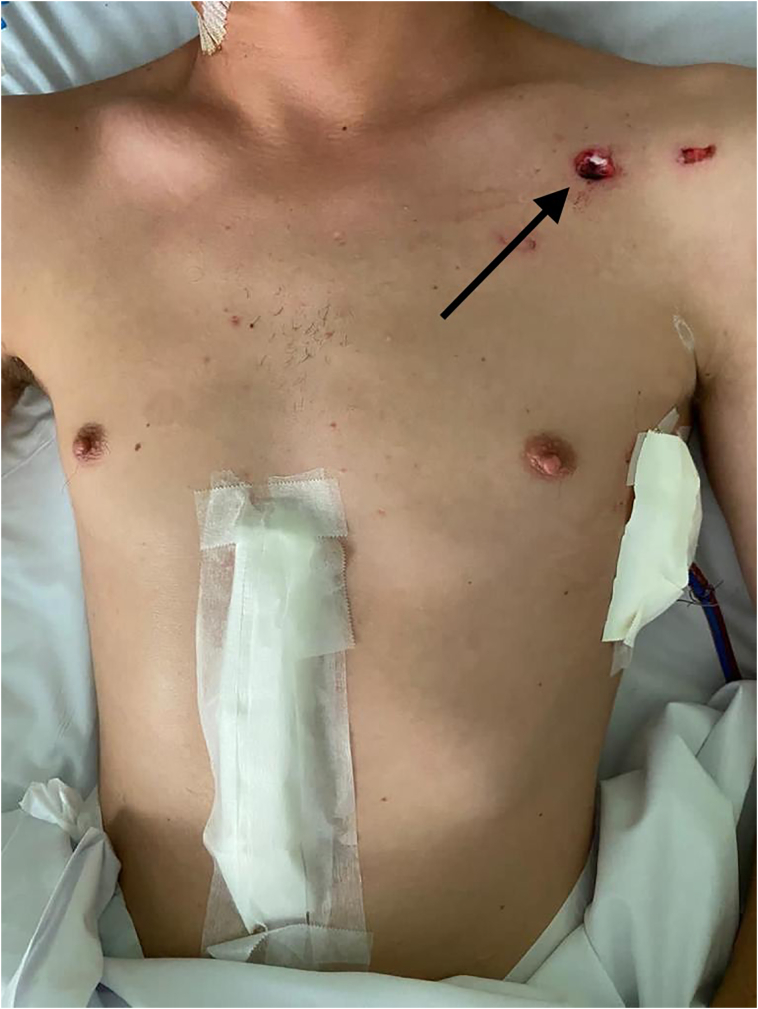
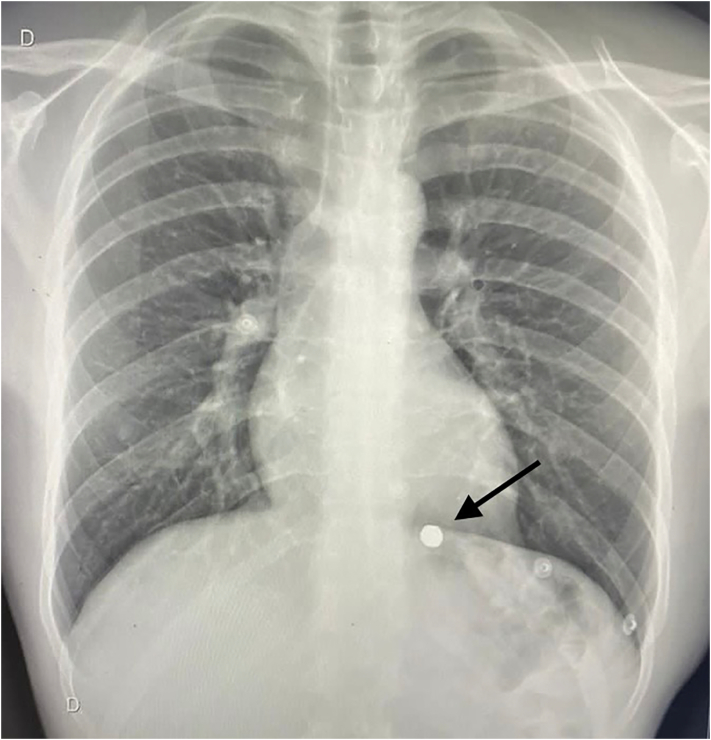
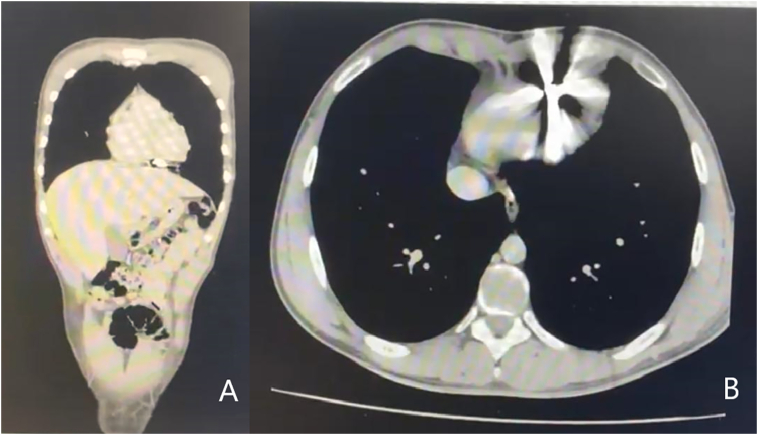
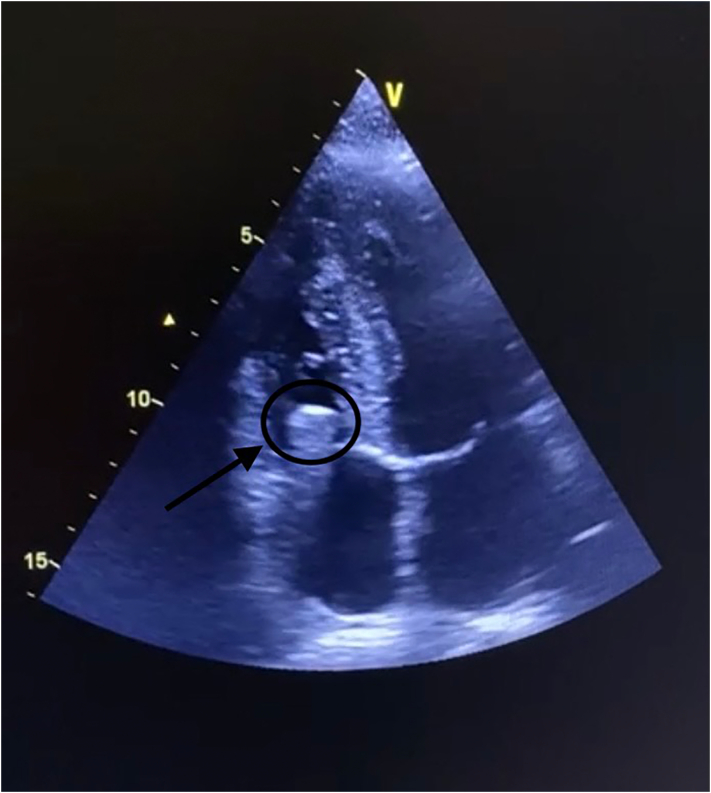
A 27-year-old male patient was brought to the emergency room of a trauma hospital after suffering a gunshot wound. At admission, the patient was alert, hemodynamically stable and had no signs of acute respiratory distress. There was a single entrance wound 1 cm below the middle portion of the left clavicle (Fig. 1). The patient reported being hit at close range by a handgun using.22 caliber ammunition, while kneeling for cover in the middle of a shootout. The projectile was fired at the patient oriented from left to right and directed towards the ground. An X-ray film showed the bullet in the mediastinum, with no signs of pneumothorax (Fig. 2). Since the patient was hemodynamically stable, a computerized tomography (CT) scan of the chest was obtained (Fig. 3), showing the projectile inside the pericardium, but its exact relation to the heart chambers was difficult to determine due to significant artifact caused by the bullet. Echocardiogram was unavailable in the emergency room at this moment. Taking in account the location of the wound and the current position of the bullet in the pericardium, the possibility of a penetrating injury to the mediastinum was considered and the patient was brought to the operating room for surgical exploration by means of a subxiphoid pericardial window. At the opening of the pericardial sac, no blood was found. Intraoperative fluoroscopy was then used to evaluate the location of the bullet, which was found to be inside the heart. The patient was maintained in close observation until the next day, when an echocardiogram was performed, which located the projectile in the right ventricle, in close relation to the tricuspid valve (Fig. 4). Due to the size of the bullet (>5 mm), the patient was transferred to a tertiary hospital, where an unsuccessful attempt of bullet removal by endovascular therapy was made. Open heart surgery with sternotomy and extracorporeal circulation was then performed, with successful removal of the bullet. Recovery from surgery was uneventful and the patient was discharged from the hospital in good conditions.
Fig. 1.
Entry wound: the bullet entry wound was located approximately 1 cm below the middle portion of the left clavicle (dark arrow).
Fig. 2.
Chest X-ray: in the chest X-ray film, the bullet (dark arrow) was apparently located in the mediastinum, with no signs of hemothorax or pneumothorax.
Fig. 3.
CT scan of the chest: in the coronal (A) and axial (B) series from the CT scan, the bullet can be seen in close relation to the heart. Significant artifact makes it difficult to point its exact location.
Fig. 4.
Echocardiogram: in the echocardiogram, the projectile (dark arrow) was located in the right ventricle, in close relation to the tricuspid valve.
Discussion
Correct localization of the projectile is of paramount importance in the treatment of ME, with X-ray usually being the first exam used due to its widespread availability. If the patient is hemodynamically stable, a CT scan may help determine the location of the missile, even if the artifact generated by a bullet can somewhat compromise the interpretation of the exam [5]. Echocardiogram and angiography may be useful in determining the location of intracardiac projectiles [5], [6]. In some cases, the correct location of the projectile can only be determined by surgical intervention, particularly in hemodynamically unstable patients or in resource-limited settings.
ME to the heart can be the result of gunshot injuries to the neck, chest, limbs or abdomen [7]. Once within the heart, a projectile may remain free within a cardiac chamber or become embedded in the myocardium [1]. A projectile in the left-sided chambers of the heart may migrate to the coronary arteries or other arteries in the body, causing ischemia and infarction. The right-sided chambers of the heart are the most commonly affected by ME, with 58% of projectiles located in the right ventricle and 32% in the pulmonary arterial tree [1], [8]. Bullets embolizing to the right ventricle are asymptomatic in most cases [7], [8], but can migrate to the pulmonary arteries, or to the left-sided chambers in the presence of a shunt [1]. The bullet may also become lodged in the tricuspid valve, causing regurgitation and thrombosis [9].
Cardiac ME can cause palpitations leading to severe anxiety (sometimes referred to as cardiac neurosis) [7], [8], endocarditis [4], intracardiac thrombosis [4], valvular incompetence [4], conduction system defects and arrhytmias [1], [8]. Migration from the right ventricle to the pulmonary artery may cause necrotizing pneumonia, formation of a bronchopleural fistula and empyema [9], [10]. Complications of cardiac ME may occur years after the trauma [4].
Surgical intervention is usually recommended for intracardiac projectiles when they are symptomatic, large in size (>5 mm), have passed through an intestinal viscus, are only partially embedded in the myocardium or are located in the left-sided chambers of the heart [1]. Removal of a missile located in the heart chambers or in the pulmonary artery can be performed by endovascular intervention, which is the treatment of choice when available, or by open cardiac surgery [9]. If feasible, endovascular removal of a projectile located in the pulmonary artery should always be attempted due to the high risk of complications associated with the migration of these projectiles [5].
Nonoperative management of intracardiac projectiles may be considered in projectiles that are asymptomatic, completely embedded in the myocardium, located in the right-sided chambers of the heart and have a size of 5 mm or less [1], [8]. The ideal combination and duration of antibiotics and anticoagulation treatment in this setting has not been properly established [1].
Conclusion
The diagnosis of ME and the correct localization of the projectile can be challenging in emergency care settings. When available, echocardiogram can be extremely helpful in the assessment of cardiac ME. While nonoperative treatment may be an option in some cases of venous ME, large projectiles lodged in the tricuspid valve, as in the case reported, must be removed by endovascular treatment or open surgery to avoid long-term complications such as endocarditis and valvular insufficiency.
Declaration of competing interest
None of the authors have any conflict of interest to disclose. There are no sources of funding to disclose for this manuscript.
References
- 1.Gandhi S.K., Marts B.C., Mistry B.M., et al. Selective management of embolized intracardiac missiles. Ann. Thorac. Surg. 1996;62:290–292. doi: 10.1016/0003-4975(96)00097-5. [DOI] [PubMed] [Google Scholar]
- 2.Ronsivalle J., Statler J., Venbrux A.C., Arepally A. Intravascular bullet migration: a report of two cases. Mil. Med. 2005;170(12):1044–1047. doi: 10.7205/milmed.170.12.1044. [DOI] [PubMed] [Google Scholar]
- 3.Kuo A.H., Gregorat A.E., Restrepo C.S., Vinu-Nair S. Systematic review of civilian intravascular ballistic embolism reports during the last 30 years. J. Vasc. Surg. 2019;70:298–306. doi: 10.1016/j.jvs.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Miller K.R., Benns M.V., Sciarretta J.D., et al. The evolving management of venous bullet emboli: a case series and literature review. Injury Int. J. Care Injured. 2011;42:441–446. doi: 10.1016/j.injury.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Stallings L.A., Newell M.A., Toschlog E.A., Thomas C.C., Kypson A.P. Right ventricular bullet embolism: diagnostic and therapeutic decisions. Injury Extra. 2013;44:64–66. doi: 10.1016/j.injury.2013.04.026. [DOI] [Google Scholar]
- 6.Elsisi I.F.H.A., Kidambi A. A shot to the heart: a rare case of cardiac embolization. Echo Res. Pract. 2018;5(1):19–21. doi: 10.1530/ERP-17-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wales L., Jenkins D.P., Smith P.L.C. Delayed presentation of right ventricular bullet embolus. Ann. Thorac. Surg. 2001;72:619–620. doi: 10.1016/s0003-4975(00)02580-7. [DOI] [PubMed] [Google Scholar]
- 8.Yoon B., Grasso S., Hofmann L.J. Management of bullet emboli to the heart and great vessels. Mil. Med. 2018;183(10):307. doi: 10.1093/milmed/usx191. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg S.R., Cassano A., Ivatury R.R. Pulmonary artery bullet emboli: to retrieve or not? A contemporary reassessment. Panam. J. Trauma Crit. Care Emerg. Surg. 2019;8(2):96–101. [Google Scholar]
- 10.Duke E., Peterson A., Erly W. Migrating bullet: a case of a bullet embolism to the pulmonary artery with secondary pulmonary infarction after gunshot wound to the left globe. J. Emerg. Trauma Shock. 2014;7(1):38–40. doi: 10.4103/0974-2700.125638. [DOI] [PMC free article] [PubMed] [Google Scholar]