Abstract
This article is one of ten reviews selected from the Annual Update in Intensive Care and Emergency Medicine 2022. Other selected articles can be found online at https://www.biomedcentral.com/collections/annualupdate2022. Further information about the Annual Update in Intensive Care and Emergency Medicine is available from https://link.springer.com/bookseries/8901.
Introduction
Accurate prognostication is a key aspect of the management of unconscious patients after cardiac arrest [1]. The focal points include not only avoiding fruitless and expensive treatment in the intensive care unit (ICU) but also needing to continue care for patients who have a realistic chance of survival but whose awakening and neurological recovery takes longer than usual. It is, of course, paramount not to withdraw care too early in patients who have a reasonable chance of full recovery. Current post-cardiac arrest care guidelines recommend a multimodal approach using a combination of clinical examination, neurophysiological investigations, such as electroencephalogram (EEG) and somatosensory evoked potentials (SSEP), radiological imaging with computed tomography (CT) or magnetic resonance imaging (MRI) of the brain, and brain injury biomarkers [1]. The strategy in unconscious patients is to use several investigative means, and if two or more investigations point toward a high risk of severe brain injury, to initiate family discussion and consider withdrawal of intensive care. Conversely, if the findings are contradictory, continuing care is recommended unless there are other reasons (e.g., comorbid conditions) for the withdrawal of care. Biomarkers have been an important part of many cardiac arrest prognostication algorithms for almost 20 years [2, 3]. The fundamental concept is that all biomarkers derived from neuronal tissue measure the severity of brain injury. However, as many patients do not survive due to multiorgan failure, severe circulatory shock, and comorbid conditions, a biomarker predicting brain injury is of limited utility in these conditions.
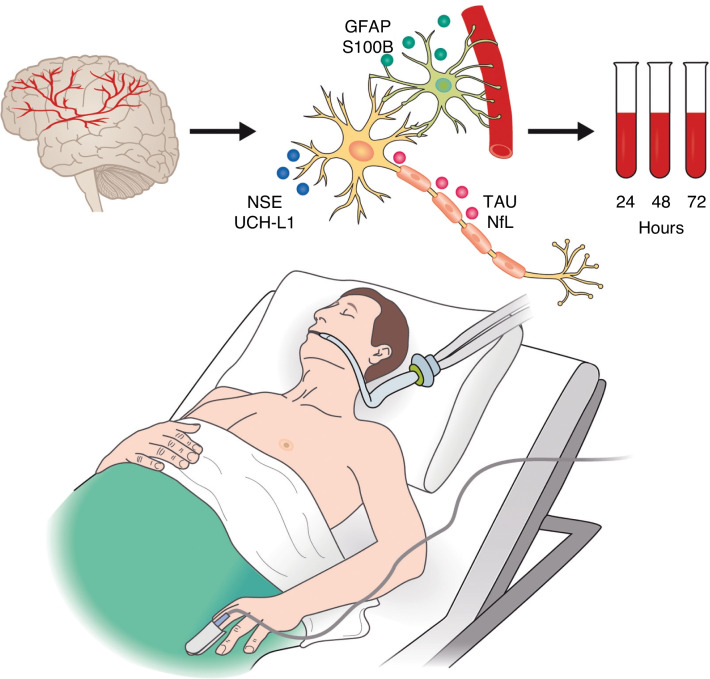
In recent years, many novel brain injury biomarkers originating from slightly different parts of the brain have been introduced (Fig. 1). A deeper understanding of these will aid clinicians’ use of brain injury biomarkers together with other means of prognostication. Compared to other investigations, biomarkers have certain advantages, as their results are, for example, not affected by sedative or pain medication or muscle relaxants. Biomarkers are easily obtained if standardized methods for determination are available. However, interpretation can be difficult, since confident and conclusive thresholds may vary, even for neuron-specific enolase (NSE), a biomarker studied in cardiac arrest for over 20 years [1]. The ideal brain injury biomarker should only be expressed in the central nervous tissue to avoid elevated levels due to other situations. For instance, several studies have shown the influence of blood sample hemolysis on NSE concentrations, which is the main disadvantage of NSE.
Fig. 1.
Central nervous system histological origin of six brain injury biomarkers studied in patients after cardiac arrest. Green dots represent biomarkers released after glial cell injury, blue dots represent biomarkers derived from injured neurons, and pink dots represent biomarkers of axonal injury. GFAP glial fibrillary acidic protein, NSE neuron-specific enolase, NfL neurofilament light, UCH-L1 ubiquitin C-terminal hydrolase-L1, S100B S100 calcium-binding protein B
Several promising novel biomarkers have been proposed and preliminary evidence has emerged: neurofilament light (NfL), ubiquitin carboxy-terminal hydro-lase L1 (UHC-L1), glial fibrillary acidic protein (GFAP), and tau protein (tau) (Fig. 1). Two studies using NfL showed an excellent ability to predict the outcome after cardiac arrest, and NfL may even replace NSE in the future [4–6]. The latest joint guidelines of the European Resuscitation Council (ERC) and the European Society of Intensive Care Medicine (ESICM) recommend against the use of S100 calcium-binding protein B (S100B) and the novel biomarkers NfL, GFAP, and tau for prognostication, given the lack of conclusive evidence [1].
In this chapter, we discuss six biomarkers—two familiar ones (NSE, S100B) and four more recently studied in relation to cardiac arrest (NfL, UCH-1, TAU, and GFAP)—focusing on their use for neurological outcome prediction in patients at risk of hypoxic brain injury after cardiac arrest. Table 1 presents a selection of recent studies on the performance of these biomarkers to predict neurological outcome after cardiac arrest. These biomarkers appear to originate histologically from slightly different parts of brain tissue, and a deeper understanding may aid the clinician in using biomarkers for determining the magnitude of brain injury in clinical practice.
Table 1.
Selected studies on the prognostic ability of six brain injury biomarkers after cardiac arrest (CA)
| Biomarker | Study | N | CA location | 24-h threshold | 48-h threshold | 72-h threshold |
|---|---|---|---|---|---|---|
| NSE ng/ml | Zandbergen, 2006 [12] | 231 | NS | 31.7 | 23.8 | 32.3 |
| AUROC | NA | NA | NA | |||
| Sensitivity (%) | NA | NA | NA | |||
| Lee, 2013 [14] | 224 | NS | 80.8 | 52.7 | NA | |
| AUROC | 0.80 | 0.90 | ||||
| Sensitivity (%) | 27 | 60 | ||||
| Larsson, 2014 [15] | 125 | OHCA/IHCA | 49 | 40 | 22 | |
| AUROC | 0.73 | 0.79 | 0.85 | |||
| Sensitivity (%) | 27 | 37 | 50 | |||
| Stammet, 2015 [16] | 686 | OHCA | 107 | 120 | 50 | |
| AUROC | 0.75 | 0.85 | 0.86 | |||
| Sensitivity (%) | 9 | 27 | 52 | |||
| Helwig, 2017 [17] | 100 | OHCA | NA | 34 | NA | |
| AUROC | 0.63 | |||||
| Sensitivity (%) | 44 | |||||
| Streitberger, 2017 [9] | 828 | OHCA | NA | NA | 85.5 | |
| AUROC | 0.90 | |||||
| sensitivity (%) | 49 | |||||
| Streitberger, 2017 [9] | 225 | IHCA | NA | NA | 1227 | |
| AUROC | 0.79 | |||||
| Sensitivity (%) | 0 | |||||
| Nakstad, 2020 [19] | 237 | OHCA | 172 | 87 | 79 | |
| AUROC | NA | NA | NA | |||
| Sensitivity (%) | 8 | 36 | 39 | |||
| S100B ng/ml | Larsson, 2014 [15] | 125 | OHCA + IHCA | 1.3 | 0.61 | 0.38 |
| AUROC | 0.78 | 0.75 | 0.83 | |||
| Sensitivity (%) | 23 | 21 | 30 | |||
| Stammet, 2017 [24] | 687 | OHCA | 2.59 | 3.67 | 1.83 | |
| AUROC | 0.80 | NA | NA | |||
| Sensitivity (%) | 10 | 5 | 5 | |||
| Duez, 2018 [23] | 115 | OHCA | 1.05 | 0.95 | 0.72 | |
| AUROC | 0.81 | 0.81 | 0.74 | |||
| Sensitivity (%) | 23 | 17 | 11 | |||
| Jang, 2019 [22] | 97 | OHCA | 0.19 | 0.16 | 0.20 | |
| AUROC | 0.93 | 0.92 | 0.86 | |||
| Sensitivity (%) | 78 | 78 | 61 | |||
| NfL pg/ml | Rana, 2013 [26] | 61 | OHCA | 321 | 405 | 309 |
| AUROC | 0.93 | 0.85 | 0.92 | |||
| Sensitivity (%) | 79 | 57 | 75 | |||
| Moseby-Knappe, 2019 [5] | 717 | OHCA | 1232 | 1539 | 1756 | |
| AUROC | 0.94 | 0.94 | 0.94 | |||
| Sensitivity (%) | 53 | 65 | 64 | |||
| Wihersaari, 2021 [4] | 112 | OHCA | 150 | 359 | 390 | |
| AUROC | 0.98 | 0.99 | 0.98 | |||
| Sensitivity (%) | 78 | 83 | 85 | |||
| UCH-L1 pg/ ml | Ebner, 2020 [36] | 717 | OHCA | 12,175 | 7945 | 9170 |
| AUROC | 0.85 | 0.87 | 0.86 | |||
| Sensitivity (%) | 4 | 9 | 1 | |||
| GFAP pg/ml | Larsson, 2014 [15] | 125 | OHCA + IHCA | 1090 | 300 | 530 |
| AUROC | 0.59 | 0.63 | 0.67 | |||
| Sensitivity (%) | 16 | 23 | 14 | |||
| Helwig, 2017 [17] | 100 | OHCA | NA | 80 | NA | |
| AUROC | 0.65 | |||||
| Sensitivity (%) | 21 | |||||
| Ebner, 2020 [36] | 717 | OHCA | 3425 | 2952 | 3581 | |
| AUROC | 0.88 | 0.88 | 0.89 | |||
| Sensitivity (%) | 17 | 19 | 12 | |||
| Tau pg/ml | Mattsson, 2017 [48] | 689 | OHCA | 874.5 | 148.8 | 72.7 |
| AUROC | 0.81 | 0.90 | 0.91 | |||
| Sensitivity (%) | 4 | 33 | 42 |
AUROC area under the receiver operating characteristic curve, CA cardiac arrest, NA not applicable, NS not specified, OHCA out-of-hospital cardiac arrest, IHCA in-hospital cardiac arrest, Nfl neurofilament light protein, S100B S100 calcium-binding protein B, GFAP glial fibrillary acidic protein, UCH-L1 ubiquitin C-terminal hydrolase L1
Neuron-Specific Enolase
NSE is a neuronal glycolytic enzyme that is abundant in the neurons of brain gray matter and involved in axonal transport [7]. NSE has a half-life of between 24 and 30 h, and its production is upregulated during ischemia and axon injuries. Extra-cerebrally, NSE is present in red blood cells (RBCs) and in thrombocytes; hence, assessing the degree of hemolysis in the blood sample is always essential, but especially when NSE is used in patients undergoing treatments that may result in hemolysis (extracorporeal membrane oxygenation [ECMO], renal replacement therapy [RRT], or use of an intra-arterial balloon pump [IABP]) [8, 9]. Additionally, neuro-endocrine cells and small cell carcinomas express NSE; thus, malignant tumors or hematologic malignancy can affect the concentration [7]. Importantly, variations in NSE levels differ between laboratories, which can influence thresholds between studies and concentrations measured in the clinical setting [10].
Studies suggest that NSE levels peak at 48–72 h after cardiac arrest, and the prognostic accuracy is also highest at 48 h [7]. The ERC/ESISCM 2021 guidelines for post-resuscitation care specify a threshold for poor prognosis of > 60 μg/l at 48 or 72 h [1]. However, there is no international consensus on the threshold [11]. Previously, a NSE concentration > 33 ng/ml at 48 h after cardiac arrest was considered to indicate poor neurological prognosis, but this was mainly based on one study by Zandbergen et al. [12], which was published in 2006 before the widespread introduction of standardized post-cardiac arrest care and targeted temperature management (TTM), which may have influenced the threshold specified in the prognostication guidelines used at that time [12, 13]. Since that study, high serum NSE levels have been demonstrated to have moderate accuracy in predicting neurological outcomes at 48–72 h after cardiac arrest with area under the receiver operating characteristic (AUROC) curves of between 0.63 and 0.90 (Table 1) [14–17]. Most studies considered in this review have been conducted on out-of-hospital cardiac arrest (OHCA) patients, but a few studies included in-hospital cardiac arrest (IHCA) patients [9, 15]. Only Streitberger et al. [9] presented the predictive accuracy separately for both cohorts, and NSE predicted outcome more accurately after OHCA than after IHCA (AUROC 0.90 vs. 0.79) in their study. As most studies do not differentiate between the causes of death, this may partly explain the discrepancy, (e.g., hypoxic brain injury may not be the most likely cause of death after IHCA [18]).
NSE has confounding sources, and it is not unusual to see high outlier values in patients who recover with good neurological outcome, which can increase the determined threshold value of poor prognosis with a 0% false positive rate to impractically high levels, also compromising the test’s sensitivity [16, 19]. In a study by Stammet et al., the threshold of poor prognosis for a 0% false positive rate at 48 h was as high as 120 ng/ml [16]. In turn, the threshold values with a 1–5% false positive rate were between 68 and 42 ng/ml, retaining moderate sensitivity (47–61%) [16]. Correspondingly, in the study by Streitberger et al. [20], the threshold for poor prognosis at 72 h with a 0% false positive rate was 85.5 ng/ml, but with a 5% false positive rate the threshold decreased to 59.2 ng/ml, simultaneously increasing the test sensitivity from 49% to 60%. As NSE’s prognostic accuracy is adequate only when used as part of a multimodal approach, it is acceptable to allow a small number of false positives to achieve at least moderate sensitivity. The smallest threshold (34 ng/ml) for poor prognosis at 48 h with a 0% false positive rate was reported in the study by Helwig et al. [17]; thus, in that study, the prognostic accuracy of NSE was rather low (AUROC 0.63). Furthermore, ascending concentration in serial measurements has been found to improve prognostic accuracy; however, the optimal sample timing is still uncertain [7, 16].
S100 Calcium-Binding Protein B
S100B is abundant in glial cells and specifically expressed in specific astrocytes surrounding the blood vessels in the brain [7, 21]. Extra-cerebrally, S100B is present in Schwann cells of the peripheral nervous system. Healthy adults express very low levels of S100B, and S100B does not move freely over an intact blood–brain barrier [21]. Of non-neuronal sources, muscle cells, adipocytes, and chondrocytes are found to express S100B, which may create a confounding source of S100B in CA patients receiving chest compressions [7, 21]. However, the half-life of S100B is only about 30 min, and compression-originated S100B possibly soon vanishes from blood [7]. S100B is considered an early biomarker after cardiac arrest, as the level usually peaks at 24 h. Four studies in the last decade examined S100B after cardiac arrest (Table 1) [15, 22–24]. In three studies, the best prognostic accuracy appeared 24 h after cardiac arrest (AUROC of between 0.78 and 0.93). In the study by Larsson et al. [15], the best accuracy was, interestingly, found at 72 h (AUROC 0.83). The thresholds to predict poor neurological outcome with a 0% false positive rate at 24 h had great variability (0.19–2.59 ng/ml). The highest threshold was reported in the largest study included in this review, that was conducted by Stammet et al. [24] with the TTM After Cardiac Arrest trial cohort. Other studies reported low sensitivities (< 24%), but Jang et al. [22] reported a sensitivity of 78%. In the study by Jang et al., the primary endpoint was 3-month neurological outcome, while in all the other studies, the outcome was assessed after a 6-month follow-up [15, 22–24]. Two of the included studies reported prognostic accuracy for both S100B and NSE, or the prognostic accuracy of NSE for the same patient cohort was reported in another manuscript: in both cases, S100B predicted the outcome better at 24 h, but, at later time points, NSE was more accurate than S100B [15, 16, 24].
Neurofilament Light
Neurofilaments (light [NfL], medium [NfM], heavy [NfH], and β-internexin), are approximately 10 nm in size, and are abundant structural scaffolding proteins exclusively expressed in neurons, predominantly within large, myelinated axons within the cerebral white matter [25]. Their function is largely unknown but hypothesized to be essential for radial growth and enabling rapid nerve conduction. Pathological processes that cause axonal damage release neurofilaments into the extracellular fluids, cerebrospinal fluid (CSF), and peripheral blood. However, even under normal circumstances, NfL is continuously released from axons in an age-dependent manner, with typical NfL reference ranges in the CSF increasing by twofold between ages 20 and 50 years and further doubling by the age of 70. A similar age-dependent increase is also seen in blood.
NfL has been extensively studied as a biomarker of neural injury in neurodegen-erative disorders, with mild increases in Alzheimer’s disease but more dynamic changes in disorders with a greater intensity of neurodegeneration (e.g., fronto-temporal dementia or amyotrophic lateral sclerosis [25]). However, the large increases in NfL in blood following hypoxic brain injury suggest that NfL may better serve as a prognostic biomarker for acute neurological injury than for chronic neurodegeneration. Studies using conventional enzyme-linked immunosorbent assay (EILSA) technology have demonstrated the large increases and predictive power of plasma neurofilaments in cardiac arrest [26, 27]. Now, semi-automated ultra-sensitive immunoassays (e.g., single molecular array [Simoa]) can quantify plasma NfL at low levels, even in healthy individuals [25].
In the Carbon dioxide, Oxygen and Mean arterial pressure After Cardiac Arrest and REsuscitation (COMACARE) trial using the Simoa platform, individuals with a poor outcome (Cerebral Performance Category [CPC] scale ≥ 3) had a median plasma NfL level > 2300 pg/ml [4]. In contrast, those with a good outcome had levels < 20 pg/ml. Consequently, NfL predicted the outcome of OHCA patients with an AUROC of 0.98 (95% CI 0.97–1.00) as early as 24 h after the event (Table 1) [4]. While admission levels of plasma NfL were elevated in individuals with subsequent poor outcomes compared to good outcomes, the considerable overlap means that NfL is unlikely to be useful at this early stage (AUROC 0.65). This study by Wihersaari et al. [4] corroborates earlier findings in a larger sample size by Moseby-Knappe et al., who also demonstrated a vastly superior prognostic performance of serum NfL in comparison to other plasma biomarkers (e.g., tau, NSE, and S100b) and clinical data in the TTM After Cardiac Arrest trial [5]. Despite these encouraging results, it has been reported that one-third of individuals with a good outcome had high levels of plasma NfL; thus, NfL has only modest specificity [28]. This leads to the conclusion that plasma NfL thresholds for normal ranges for continuing care should be applied rather than thresholds for poor outcome and terminating care.
NfL has several key advantages as a plasma biomarker. First, there is a consensus on the assay of choice (Simoa), which clinical laboratories in Sweden, the Netherlands, and France have validated for broad use in clinical laboratory practice. This gives a greater chance of thresholds being transferrable between research cohorts and, eventually, clinical routines. Furthermore, NfL in plasma is very stable, largely unaffected by preanalytical variabilities or hemolysis, and the sample can remain at room temperature > 48 h without compromising measurement quality or accuracy. In addition, an accurate measurement of NfL does not require immediate centrifugation and can even be extracted as a whole blood dry spot for longer term storage/transportation for remote setting assessment [29]. Plasma or serum NfL is also not susceptible to freeze–thaw cycling, which is useful for research settings or external laboratory testing [30]. Plasma NfL is predominately derived from the central nervous system but, however, is elevated in peripheral neuropathies [31]. However, based on the reported high levels in cardiac arrest patients with poor outcomes, this mild magnitude of change in peripheral neuropathies is unlikely to be a confounder.
Ubiquitin C-Terminal Hydrolase L1
Ubiquitin C-terminal hydrolase L1 (UCH-L1) is a 26 kDa neuronal deubiquitinase primarily expressed in neurons and neuroendocrine cells [32]. UCH-L1 is important not only for neuroaxonal stability but also for repair after brain injury [33]. Specifically, it is involved in the process of ubiquitination of proteins destined for degradation via the proteasomal pathway. Therefore, it has an essential role in the removal of oxidized or misfolded proteins in both normal and pathological conditions [34]. UCH-L1 is more commonly evaluated in traumatic brain injury (TBI), where it has been permitted for use by the U.S. Food and Drug Administration (FDA) for indicators of good outcome to avoid unnecessary CT scans following concussion [35].
Use of UCH-L1 in cardiac arrest patients has been evaluated in only two studies that were both conducted with the same patient cohort (the patient cohort from the TTM trial) [28, 36]. UCH-L1 was shown to predict poor outcome after cardiac arrest with good accuracy (AUROC of between 0.85 and 0.87), was significantly better than NSE at 24 and 48 h, and the prognostic accuracy was further improved by the addition of GFAP (AUROC of between 0.90 and 0.91) [36]. At 72 h, both UCH-L1 and NSE performed to the same degree. This is in line with the reported short half-life of UCH-L1 (< 12 h) in comparison to NSE [36, 37]. Moseby-Knappe et al. demonstrated that UCH-L1 levels were within normal ranges in 63.8% of patients with good outcome at 24 h, however this increased to 88.1% at 72 h [28]. By contrast, predicting poor outcome diminished overtime with elevated UCH-L1 above normal levels in 85.3% of poor outcome patients at 24 h but 70.3% at 72 h. Ability to predict poor outcome was inferior to NfL, Tau, and GFAP [4, 5] but ranked highly in specificity, suggesting UCH-L1 may have a role in the diagnostic challenge of cardiac arrest. The successful FDA approval of serum UCH-L1 paves the way for UCH-L1 to be used for purposes other than TBI particularly as multiple plex assays with NfL, Tau, and GFAP are available. However, further independent studies defining normal reference ranges and their added value over and above other putative biomarkers for cardiac arrest are still lacking. Lastly, given the limited number of studies available, the impact of high expression of UCH-L1 from the pancreas and kidney, as a potential confounder, has largely been unexplored.
Glial Fibrillary Acidic Protein
GFAP is a structural component of intermediate filaments in the astrocyte cytoskel-eton that is considered a highly brain-specific marker [38]. GFAP production is upregulated following ischemia, which is believed to be a neuroprotective mechanism, but can also lead to glial scarring [38]. As a structural protein, GFAP is released from damaged astrocytes and elevated levels are not in general detected in healthy individuals [7]. Serum GFAP has been found to predict neurological outcome after head trauma, and elevated blood levels have been measured after cardiac arrest, intracerebral hemorrhage, and ischemic stroke [15, 38].
To the best of our knowledge, GFAP has been investigated after cardiac arrest in six studies [15, 17, 36, 39–41]. Three studies [39–41] were conducted before the introduction of a highly sensitive method (immunoassay) to measure serum GFAP [42], and we did not include their results in this review. The accuracy of GFAP to predict neurological outcome seems to be better at 48 and 72 h after cardiac arrest compared to earlier time points, with AUROC values of between 0.65 and 0.89; see Table 1 [15, 17, 36]. The largest study included in this review, which was conducted in the TTM trial cohort by Ebner et al. [36], reported a threshold of 2952 pg/ml with a 0% false positive rate for poor prognosis 48 h after cardiac arrest, but again the sensitivity remained low (Table 1). The corresponding thresholds determined in the two other included studies were much lower (300 and 80 pg/ml), but these studies have methodological differences compared to the study by Ebner et al. Helwig et al. [17] determined the neurological outcome with a modified Glasgow Outcome Scale at 4 weeks, and a study by Larsson et al. [15] included both IHCA and OHCA patients. All the GFAP studies included in this review compared the predictive accuracy of GFAP to other biomarkers [15, 17, 36]. In the study by Larsson et al., NSE and S100B were more accurate in predicting poor neurological outcomes, and they were more sensitive compared to GFAP, with AUROC values at 48 h for NSE, S100B, and GFAP of 0.79, 0.75 and 0.63, respectively [15]. In the study by Helwig et al. [17], both NSE and GFAP showed rather modest accuracy in predicting the outcome at 48 h, and NSE was more sensitive than GFAP. In turn, in the study conducted by Ebner et al. [36], GFAP predicted the outcome more accurately at every determined time point after the arrest (at 24, 48, and 72 h) compared to NSE, but, as stated above, GFAP presented low sensitivity.
Tau Protein
Tau is a protein molecule that stabilizes the structures of microtubules in neuro-axonal processes and is mainly located in the white matter of the central nervous system [43, 44]. Ischemia causes hyperphosphorylation of tau molecules, detaching them from microtubules [45]. Detached tau molecules aggregate to insoluble masses, interrupting axonal signaling. Elevated serum tau concentrations have been reported after ischemic stroke and cardiac arrest [46–49]. Among patients with neu-rodegenerative disease (e.g., Alzheimer’s disease or Creutzfeldt-Jacob disease), elevated tau levels are present in CSF [50], but this is not reflected in blood as mild elevations are confounded by peripheral expression. Determination of accurate serum tau concentrations requires a highly sensitive immunoassay method, which is only available at specialized laboratories [42]. So far, only one large study has examined tau after cardiac arrest [48], and two other studies were small pilot studies [46, 47]. Mattsson et al. studied tau in the TTM trial cohort, and the predictive power of tau was better in the later samples (the AUROC at 24, 48, and 72 h was 0.81, 0.90, and 0.91, respectively [48]). Further, tau predicted poor neurological outcome between 24 and 72 h after cardiac arrest more accurately than NSE [48]. The thresholds for poor prognosis with a 0% false positive rate seemed high (at 48 h 148.8 pg/ml and at 72 h 72.7 pg/ml), and sensitivity remained low, but already allowing a false positive rate of 2%, the sensitivity increased above 60% and the thresholds decreased to 18.9 pg/ml at 48 h and 11.2 pg/ml at 72 h [5]. Bimodal tau release (early and late) was reported in the two pilot studies of tau and cardiac arrest; the delayed peak was absent or significantly lower in patients with good outcomes [46, 47]. Tau has a half-life of about 10 h, and late elevations in tau concentrations likely reflect ongoing neuronal injury [5].
Conclusion
Biomarkers will undoubtedly continue to be an important part of outcome prediction in patients with hypoxic brain injury after cardiac arrest. Further research will improve accuracy and may propose new strategies for the way biomarkers are used. The traditional approach of using high threshold levels to identify patients with no chance of a good functional outcome may well be complemented with a strategy of using low biomarker levels to predict a good outcome [27]. As these different biomarkers originate from different areas of the brain, it could be an option to use some of them together (e.g., one biomarker reflecting injury to gray matter, one reflecting axonal injury, and one reflecting injury to the glia). A study by Ebner et al. [36] showed that combining GFAP and UHC-L1 predicted neurological outcomes more accurately than NSE alone. Additionally, unpublished evidence suggests that high levels of tau as a marker of axonal injury identify different poor-outcome patients than those identified with GFAP, a marker of glial injury (Humaloja, personal communication October 14, 2021). It seems logical to combine several hypoxic brain injury biomarkers for improved accuracy. Whether this concept is cost-effective and accurate and whether it has a role as part of a multimodal prognostication approach should be assessed in future large-scale studies.
Acknowledgements
Not applicable.
Authors' contributions
J.H., NJ.A, and MB.S have all made equal contributions to draft and revise this narrative review. All of the authors have approved the final version of the manuscript.
Funding
Authors did not receive any funding to conduct this review. Publication costs were funded by an unrestricted research Grant. J.H. has received an unrestricted personal research Grant in 2020 and 2021 from Finska Läkaresällskapet. M.B.S. has received numerous unrestricted non-commercial research grants (Finska Läkareskällskapet, Sigrid Juselius Stiftelse, Medicinska Understödföreningen Liv och Hälsa, Helsinki University research grant, Govermental research funding (VTR), Svenska Kulturfonden, Perklen Stiftelse). The sponsors had no role in the content of this review.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable as this is a narrative review of the literature.
Consent for publication
Not applicable.
Competing interests
J.H. and NJ.A. declares no competing interests. MB.S reports speakers’ fees and travel grants from BARD Medical (Ireland) and a research grant from GE Healthcare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nolan JP, Sandroni C, Böttiger BW, et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: post-resuscitation care. Resuscitation. 2021;161:220–269. doi: 10.1016/j.resuscitation.2021.02.012. [DOI] [PubMed] [Google Scholar]
- 2.Oksanen T, Tiainen M, Skrifvars MB, Varpula T, Kuitunen A, Castrén M, Pettilä V. Predictive power of serum NSE and OHCA score regarding 6-month neurologic outcome after out-of-hospital ventricular fibrillation and therapeutic hypothermia. Resuscitation. 2009;80:165–170. doi: 10.1016/j.resuscitation.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Tiainen M, Roine RO, Pettilä V, Takkunen O. Serum neuron-specific enolase and S-100B protein in cardiac arrest patients treated with hypothermia. Stroke. 2003;34:2881–2886. doi: 10.1161/01.STR.0000103320.90706.35. [DOI] [PubMed] [Google Scholar]
- 4.Wihersaari L, Ashton NJ, Reinikainen M, et al. Neurofilament light as an outcome predictor after cardiac arrest: a post hoc analysis of the COMACARE trial. Intensive Care Med. 2021;47:39–48. doi: 10.1007/s00134-020-06218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moseby-Knappe M, Mattsson N, Nielsen N, et al. Serum neurofilament light chain for prognosis of outcome after cardiac arrest. JAMA Neurol. 2019;76:64–71. doi: 10.1001/jamaneurol.2018.3223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leithner C. Neuron specific enolase after cardiac arrest: from 33 to 60 to 100 to NFL? Resuscitation. 2021;168:234–236. doi: 10.1016/j.resuscitation.2021.09.035. [DOI] [PubMed] [Google Scholar]
- 7.Gul SS, Huesgen KW, Wang KK, Mark K, Tyndall JA. Prognostic utility of neuroinjury bio-markers in post out-of-hospital cardiac arrest (OHCA) patient management. Med Hypotheses. 2017;105:34–47. doi: 10.1016/j.mehy.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 8.Ramont L, Thoannes H, Volondat A, Chastang F, Millet M-C, Maquart FX. Effects of hemoly-sis and storage condition on neuron-specific enolase (NSE) in cerebrospinal fluid and serum: implications in clinical practice. Clin Chem Lab Med. 2005;43:1215–1217. doi: 10.1515/CCLM.2005.210. [DOI] [PubMed] [Google Scholar]
- 9.Streitberger KJ, Leithner C, Wattenberg M, et al. Neuron-specific enolase predicts poor outcome after cardiac arrest and targeted temperature management: a multicenter study on 1,053 patients. Crit Care Med. 2017;45:1145–1151. doi: 10.1097/CCM.0000000000002335. [DOI] [PubMed] [Google Scholar]
- 10.Mlynash M, Buckwalter MS, Okada A, et al. Serum neuron-specific enolase levels from the same patients differ between laboratories: assessment of a prospective post-cardiac arrest cohort. Neurocrit Care. 2013;10:161–166. doi: 10.1007/s12028-013-9867-5. [DOI] [PubMed] [Google Scholar]
- 11.Berg KM, Soar J, Andersen LW, et al. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142:S92–S139. doi: 10.1161/CIR.0000000000000893. [DOI] [PubMed] [Google Scholar]
- 12.Zandbergen EGJ, Hijdra A, Koelman JHTM, Hart AAM, Vos PE, Verbeek MM, de Haan RJ. Prediction of poor outcome within the first 3 days of postanoxic coma. Neurology. 2006;66:62–68. doi: 10.1212/01.wnl.0000191308.22233.88. [DOI] [PubMed] [Google Scholar]
- 13.Wijdicks EFM, Hijdra A, Young GB, Bassetti CL, Wiebe S. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review) Neurology. 2006;67:203–210. doi: 10.1212/01.wnl.0000227183.21314.cd. [DOI] [PubMed] [Google Scholar]
- 14.Lee BK, Jeung KW, Lee HY, Jung YH, Lee DH. Combining brain computed tomography and serum neuron specific enolase improves the prognostic performance compared to either alone in comatose cardiac arrest survivors treated with therapeutic hypothermia. Resuscitation. 2013;84:1387–1392. doi: 10.1016/j.resuscitation.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 15.Larsson IM, Wallin E, Kristofferzon ML, Niessner M, Zetterberg H, Rubertsson S. Post-cardiac arrest serum levels of glial fibrillary acidic protein for predicting neurological outcome. Resuscitation. 2014;85:1654–1661. doi: 10.1016/j.resuscitation.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 16.Stammet P, Collignon O, Hassager C, et al. Neuron-specific enolase as a predictor of death or poor neurological outcome after out-of-hospital cardiac arrest and targeted temperature management at 33°C and 36°C. J Am Coll Cardiol. 2015;65:2104–2114. doi: 10.1016/j.jacc.2015.03.538. [DOI] [PubMed] [Google Scholar]
- 17.Helwig K, Seeger F, Hölschermann H, Lischke V, Gerriets T, Niessner M, Foerch C. Elevated serum glial fibrillary acidic protein (GFAP) is associated with poor functional outcome after cardiopulmonary resuscitation. Neurocrit Care. 2017;27:68–74. doi: 10.1007/s12028-016-0371-6. [DOI] [PubMed] [Google Scholar]
- 18.Witten L, Gardner R, Holmberg M, et al. Reasons for death in patients successfully resuscitated from out-of-hospital and in-hospital cardiac arrest. Resuscitation. 2019;136:93. doi: 10.1016/j.resuscitation.2019.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakstad ER, Stær-Jensen H, Wimmer H, et al. Late awakening, prognostic factors and longterm outcome in out-of-hospital cardiac arrest—results of the prospective Norwegian Cardio-Respiratory Arrest Study (NORCAST) Resuscitation. 2020;149:170–179. doi: 10.1016/j.resuscitation.2019.12.031. [DOI] [PubMed] [Google Scholar]
- 20.Streitberger KJ, Endisch C, Ploner CJ, et al. Timing of brain computed tomography and accuracy of outcome prediction after cardiac arrest. Resuscitation. 2019;145:8–14. doi: 10.1016/j.resuscitation.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 21.Sen J, Belli A. S100B in neuropathologic states: the CRP of the brain? J Neurosci Res. 2007;85:1373–1380. doi: 10.1002/jnr.21211. [DOI] [PubMed] [Google Scholar]
- 22.Jang JH, Park WB, Lim YS, et al. Combination of S100B and procalcitonin improves prognostic performance compared to either alone in patients with cardiac arrest: a prospective observational study. Medicine (Baltimore) 2019;98:e14496. doi: 10.1097/MD.0000000000014496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duez CHV, Grejs AM, Jeppesen AN, Schrøder AD, Søreide E, Nielsen JF, Kirkegaard H. Neuron-specific enolase and S-100b in prolonged targeted temperature management after cardiac arrest: a randomised study. Resuscitation. 2018;122:79–86. doi: 10.1016/j.resuscitation.2017.11.052. [DOI] [PubMed] [Google Scholar]
- 24.Stammet P, Dankiewicz J, Nielsen N, et al. Protein S100 as outcome predictor after out-of-hospital cardiac arrest and targeted temperature management at 33 °C and 36 °C. Crit Care. 2017;21:1–10. doi: 10.1186/s13054-017-1729-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ashton NJ, Janelidze S, al Khleifat A, et al. A multicentre validation study of the diagnostic value of plasma neurofilament light. Nat Commun. 2021;12:1–12. doi: 10.1038/s41467-021-23620-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rana OR, Schröder JW, Baukloh JK, et al. Neurofilament light chain as an early and sensitive predictor of long-term neurological outcome in patients after cardiac arrest. Int J Cardiol. 2013;168:1322–1327. doi: 10.1016/j.ijcard.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 27.Rundgren M, Friberg H, Cronberg T, Romner B, Petzold A. Serial soluble neurofilament heavy chain in plasma as a marker of brain injury after cardiac arrest. Crit Care. 2012;16:R45. doi: 10.1186/cc11244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moseby-Knappe M, Mattsson-Carlgren N, Stammet P, et al. Serum markers of brain injury can predict good neurological outcome after out-of-hospital cardiac arrest. Intensive Care Med. 2021;47:984–994. doi: 10.1007/s00134-021-06481-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simrén J, Ashton NJ, Blennow K, Zetterberg H. Blood neurofilament light in remote settings: alternative protocols to support sample collection in challenging pre-analytical conditions. Alzheimers Dement (Amst) 2021;13:e12145. doi: 10.1002/dad2.12145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ashton NJ, Suárez-Calvet M, Karikari TK, et al. Effects of pre-analytical procedures on blood biomarkers for Alzheimer’s pathophysiology, glial activation, and neurodegeneration. Alzheimers Dement (Amst) 2021;13:e12168. doi: 10.1002/dad2.12168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sandelius Å, Zetterberg H, Blennow K, et al. Plasma neurofilament light chain concentration in the inherited peripheral neuropathies. Neurology. 2018;90:e518–e524. doi: 10.1212/WNL.0000000000004932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thelin EP, Zeiler FA, Ercole A, et al. Serial sampling of serum protein biomarkers for monitoring human traumatic brain injury dynamics: a systematic review. Front Neurol. 2017;8:300. doi: 10.3389/fneur.2017.00300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bishop P, Rocca D, Henley JM. Ubiquitin C-terminal hydrolase L1 (UCH-L1): structure, distribution and roles in brain function and dysfunction. Biochem J. 2016;473:2453–2462. doi: 10.1042/BCJ20160082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gong B, Leznik E. The role of ubiquitin C-terminal hydrolase L1 in neurodegenerative disorders. Drug News Perspect. 2007;20:365–370. doi: 10.1358/dnp.2007.20.6.1138160. [DOI] [PubMed] [Google Scholar]
- 35.Anderson TN, Hwang J, Munar M, Papa L, Hinson HE, Vaughan A, Rowell SE. Blood-based biomarkers for prediction of intracranial hemorrhage and outcome in patients with moderate or severe traumatic brain injury. J Trauma Acute Care Surg. 2020;89:80–86. doi: 10.1097/TA.0000000000002706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ebner F, Moseby-Knappe M, Mattsson-Carlgren N, et al. Serum GFAP and UCH-L1 for the prediction of neurological outcome in comatose cardiac arrest patients. Resuscitation. 2020;154:61–68. doi: 10.1016/j.resuscitation.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 37.Diaz-Arrastia R, Wang KKW, Papa L, et al. Acute biomarkers of traumatic brain injury: relationship between plasma levels of ubiquitin C-terminal hydrolase-l1 and glial fibrillary acidic protein. J Neurotrauma. 2014;31:19. doi: 10.1089/neu.2013.3040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hol EM, Pekny M. Glial fibrillary acidic protein (GFAP) and the astrocyte intermediate filament system in diseases of the central nervous system. Curr Opin Cell Biol. 2015;32:121–130. doi: 10.1016/j.ceb.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Kaneko T, Kasaoka S, Miyauchi T, Fujita M, Oda Y, Tsuruta R, Maekawa T. Serum glial fibrillary acidic protein as a predictive biomarker of neurological outcome after cardiac arrest. Resuscitation. 2009;80:790–794. doi: 10.1016/j.resuscitation.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 40.Mörtberg E, Zetterberg H, Nordmark J, Blennow K, Rosengren L, Rubertsson S. S-100B is superior to NSE, BDNF and GFAP in predicting outcome of resuscitation from cardiac arrest with hypothermia treatment. Resuscitation. 2011;82:26–31. doi: 10.1016/j.resuscitation.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 41.Hayashida H, Kaneko T, Kasaoka S, et al. Comparison of the predictability of neurological outcome by serum procalcitonin and glial fibrillary acidic protein in postcardiac-arrest patients. Neurocrit Care. 2009;12:252–257. doi: 10.1007/s12028-009-9318-5. [DOI] [PubMed] [Google Scholar]
- 42.Rissin DM, Fournier DR, Piech T, et al. Simultaneous detection of single molecules and singulated ensembles of molecules enables immunoassays with broad dynamic range. Anal Chem. 2011;83:2279–2285. doi: 10.1021/ac103161b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weingarten MD, Lockwood AH, Hwo SY, Kirschner MW. A protein factor essential for micro-tubule assembly. Proc Natl Acad Sci U S A. 1975;72:1858–1862. doi: 10.1073/pnas.72.5.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams DR. Tauopathies: classification and clinical update on neurodegenerative diseases associated with microtubule-associated protein tau. Intern Med J. 2006;36:652–660. doi: 10.1111/j.1445-5994.2006.01153.x. [DOI] [PubMed] [Google Scholar]
- 45.Pluta R, Ułamek-Kozioł M, Januszewski S, Czuczwar SJ. Tau protein dysfunction after brain ischemia. J Alzheimers Dis. 2018;66:429–433. doi: 10.3233/JAD-180772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Randall J, Mörtberg E, Provuncher GK, et al. Tau proteins in serum predict neurological outcome after hypoxic brain injury from cardiac arrest: results of a pilot study. Resuscitation. 2013;84:351–356. doi: 10.1016/j.resuscitation.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 47.Mörtberg E, Zetterberg H, Nordmark J, et al. Plasma tau protein in comatose patients after cardiac arrest treated with therapeutic hypothermia. Acta Anaesthesiol Scand. 2011;55:1132–1138. doi: 10.1111/j.1399-6576.2011.02505.x. [DOI] [PubMed] [Google Scholar]
- 48.Mattsson N, Zetterberg H, Nielsen N, et al. Serum tau and neurological outcome in cardiac arrest. Ann Neurol. 2017;82:665–675. doi: 10.1002/ana.25067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wunderlich MT, Lins H, Skalej M, Wallesch CW, Goertler M. Neuron-specific enolase and tau protein as neurobiochemical markers of neuronal damage are related to early clinical course and long-term outcome in acute ischemic stroke. Clin Neurol Neurosurg. 2006;108:558–563. doi: 10.1016/j.clineuro.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 50.Blennow K, Hampel H, Weiner M, Zetterberg H. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol. 2010;6:131–144. doi: 10.1038/nrneurol.2010.4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.