Abstract
Heart attacks, arrhythmias, and cardiomyopathy are all linked to the 2019 coronavirus disease (COVID-19), which has been identified as a risk factor for cardiovascular disease. Nothing can be held accountable in the current state of affairs. Undiagnosed chronic systolic heart failure (CSHF) develops when the heart’s second half of the cardiac cycle does not function properly. As a result, the heart’s blood pumping function is interrupted. Stress-induced cardiomyopathy may be caused by a variety of factors inside the body (SICM). Cytokine storm and microvascular dysfunction are among the issues. There is inflammation in the heart muscle, which may lead to stress-induced cardiomyopathy. A major part of our study is going to be devoted to understanding the effects of coronavirus on the cardiovascular system and blood vessels. A lot of time and effort has been put into figuring out the health effects of radiation exposure. The heart and circulatory system are shown to be affected by the coronavirus in this research. COVID-19 is shown to influence persons with heart disease, heart failure, arrhythmias, microvascular angiopathy, and cardiac damage in this study.
Keywords: coronavirus, heart failure, cardiac diseases, myocardial injury, arrhythmias
Introduction
Coronavirus disease (COVID-19), which is caused by the SARS-CoV-2 virus, is a dangerous and sometimes fatal disease. Viruses can spread through the air when people cough, sneeze, talk, sing, or breathe. Tiny liquid particles that come from the mouth or nose of someone who is sick can spread the virus. Particles that are small aerosols and bigger respiratory droplets are in this group. Getting the virus COVID-19 can happen if you breathe it in or touch it with eyes, nose, or mouth after it has been infected by the virus. This way, you can get the virus. People are more likely to get the virus when they are inside or in a group. This is because the virus is more likely to spread in these places than outside.
Several people have been concerned about the pandemic’s long-term effects, which has led them to worry. If people are not going to the hospital because they are afraid they will get the severe acute respiratory syndrome-coronavirus-2 virus, that could be why they are not going to the hospital for heart problems (SARS-CoV-2). Other factors, such as the stress that is put on healthcare systems, may have had an indirect effect on the outcome. The disease’s most debilitating symptom is the patient’s inability to breathe. SARS-associated pneumonia (COVID-19) and heart damage, both short-and long-term. It is needed to prioritize therapy for COVID-19.1 SARS-CoV-2, a serine protease, interacts with the angiotensin-converting enzyme 2 (ACE2) and TMPRSS2, which are found in the lungs, the gastrointestinal system, and cardiac myocytes. People with COVID-19 exposure reported heart problems, and those with heart disease in their family were more likely to pass away.2 Most patients who had CV disease prior to contracting COVID-19 have some level of acute heart injury, even in cases when there were no symptoms at the time of infection. It is critical to understand the relationship between COVID-19 and cardiovascular disease, which allows for better care for patients.3
People with or without previous cardiac problems may suffer damage to their hearts, which may cause many problems. COVID-19 has been predicted to likely cause immediate harm to the heart, most likely via a cytokine storm that causes non-ischemic myocardial injury. Many factors and stages contribute to heart deterioration and have a terrible result.4 If point-of-care cardiac ultrasonography is not available, it is unnecessary to do a complete cardiac imaging study on patients with elevated troponin levels if their clinical condition is stable Those with severe blood pressure abnormalities or ventricular arrhythmias (a kind of rapid heart rhythm) need to have more extensive consultations with cardiology specialists and may even be good candidates for clinical trials or use of experimental medications.5
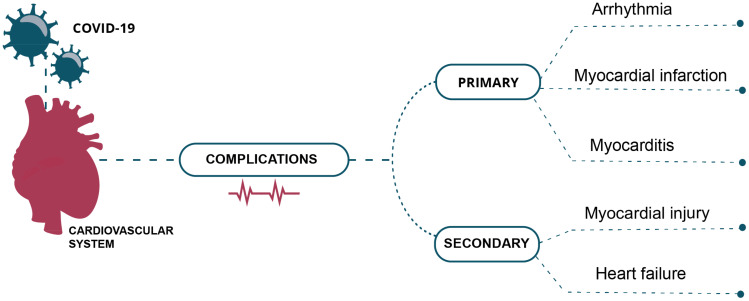
In addition to direct viral damage, the early stages of infection also trigger inflammatory cytokines and chemokines and cytotoxic immune cell responses. In the latter stages of infection, cardiac injury seems to be a result of a mix of viral damage and immune-mediated damage. A SARS-CoV-2 infection results in a complicated cytokine storm caused by a combination of host immune response factors.6 Serious problems with inflammation and the lungs may cause massive morbidity and death, but in certain cases, cardiovascular issues can also develop. If you treat patients with COVID-19,7 you should be mindful of the cardiovascular consequences while assessing and treating them. Figure 1 depicts the primary and secondary complications caused by the circulatory system.
Figure 1.
Primary and secondary complications caused by on the circulatory system.
SARS 2019 Coronavirus Disease (CODV19), caused by coronavirus 2, is a pandemic that has led to considerable morbidity and death across the world. While the virus mainly affects the respiratory system, it also causes acute myopericarditis, acute coronary syndrome, congestive heart failure, cardiogenic shock, cardiogenic shock, and cardiac arrhythmias.8 COVID-19 is caused by SARS-CoV2, a virus that penetrates cells through ACE2, which is expressed in certain organs. Emerging epidemiological data indicates that COVID-19 patients have higher illness severity and death because of cardiovascular risk factors. Patients with more serious symptoms are more prone to suffering damage to their hearts or irregular heartbeats. The exact frequency and root cause of these incidents are unknown. People have now again been anxious about coronavirus considering the COVID-19 coronavirus epidemic.9
Mechanistic details of the viral cardiac damage and hyperinflammatory syndrome, which may follow later in the course of the illness, have been given. COVID-19 is a significant threat to the public and healthcare professionals alike. Even while most individuals do not have serious or severe symptoms, it is known that around 20% of those diagnosed with COVID-19 have symptoms ranging from moderate to severe.10 Based on current research, the standard treatments for COVID-19 have been described. Considering these difficulties, further research is required to find the optimal treatment plan for individuals with COVID-19.11 The connection between COVID-19 and the cardiovascular system is direct. People with risk factors or cardiovascular disease who become infected have a greater chance of suffering illness and a poorer outcome but turning this knowledge into actionable plans is a challenge. ACE2 is the SARS-CoV-2 receptor, and it is important in inflammation and the cardiovascular system. Apart from its cytotoxic nature, SARS-CoV-2 also has powerful inflammatory and cardiovascular consequences, even causing death in previously healthy individuals. Those who suffer from cardiovascular problems are more likely to have complications and mortality, and thus they should get close attention and high-quality treatment.12 The virus enters vessels via the TMPRSS2 spike glycoprotein priming, a process that involves ACE-2. Patients still have a high risk of venous thromboembolism, even if they are taking anticoagulants. This is true even if they are taking them. This shows the need to potentially have more severe anticoagulant treatment in place, as well as regular monitoring. Investigation of D-dimer levels is needed to see if the biomarker is useful for treatment of thromboembolic consequences.13
This may tell us more about COVID-19 pathology. Patients who have COVID-19 may develop microvascular dysfunction because the disease’s inflammatory nature is mirrored in the microvasculature. COVID-19 is a laser Doppler perfusion monitor that uses local thermal hyperemia to measure systemic microcirculation. In this way, the device may assist with clinical decisions about patients by providing important information that has therapeutic and predictive consequences.14 It seems as if the inflammation is a reaction to the infection in the COVID-19ʹs cardiac tissue. In addition, COVID-19ʹs acute heart damage may be caused by virus invasion of cardiomyocytes and oxidative stress, which damage the heart muscle.15
Hypotension during treatment, severe myocardial injury, and pericardial effusion were the independent risk factors for critical disease status in patients with COVID-19. Monitoring COVID-19 patients’ vital signs and heart function is very important, especially for those who have low blood pressure during treatment, a severe heart attack, or a pericardial effusion.16 SARS-CoV-2 myocarditis is rare, but those who are sicker have a wide range of heart problems that cause myocardial damage in different ways. There are still concerns about heart disease in children (MIS-C) and adults, given that research has shown that it is possible to detect silent abnormalities in the heart on MRI scans. Acute SARS-CoV-2 myocarditis is rare, but myocardial injury is observed in many sicker patients through a variety of mechanisms.17 There are still concerns about long-term damage to the heart in children (MIS-C) and adults because of the many small, hidden problems found in cardiac MRI scans. The extra in-hospital mortality, unrelated to COVID-19 infection, has been examined in a variety of cardiovascular disorders. There has been a systematic search for studies comparing in-hospital mortality among patients admitted to the hospital with cardiovascular illness who were not infected with SARS-CoV-2. The COVID-19 pandemic increased in-hospital mortality by 62% as compared to times before the outbreak. During the COVID-19 pandemic, studies with admission rates that dropped by more than 50% saw the highest increases in mortality. There was a consistent rise in mortality across a range of cardiovascular diseases. Independent of COVID-19 co-infection, the in-hospital death rate for patients hospitalized with cardiovascular illnesses was higher than in times before the pandemic. People who were sick at the time were more likely to be admitted to the trials where admission rates fell the most.18 The aim of this review is to look at how the Corona virus has played a role in the development of several diseases that affect the heart and blood flow. Some of these diseases are myocardial damage, the effects of COVID-19 on people with congenital heart disease, heart failure, arrhythmias, microvascular angiopathy, and cardiac damage.
COVID-19 Virus Effect on the Heart
Myocardial Injury
Deficiency of oxygen to heart muscle cells results in myocardial infarction (MI), the death of heart muscle cells. COVID-19ʹs myocardial injury seems to be the result of many mechanisms. If any of the following criteria are present, they may occur in any combination. Myocardial dysfunction and respiratory failure-induced hypoxia are all symptoms of an acute illness, as are viral infiltration and subsequent myocyte death, inflammatory cytokine storms, and respiratory failure-induced hypoxia.19 Only a tiny percentage of patients with SARS-CoV-2 develop multifocal lymphocytic myocarditis, which is characterized by an increase in interstitial macrophages. There have also been reports of various sorts of heart injuries in some of those who have been treated with this drug.
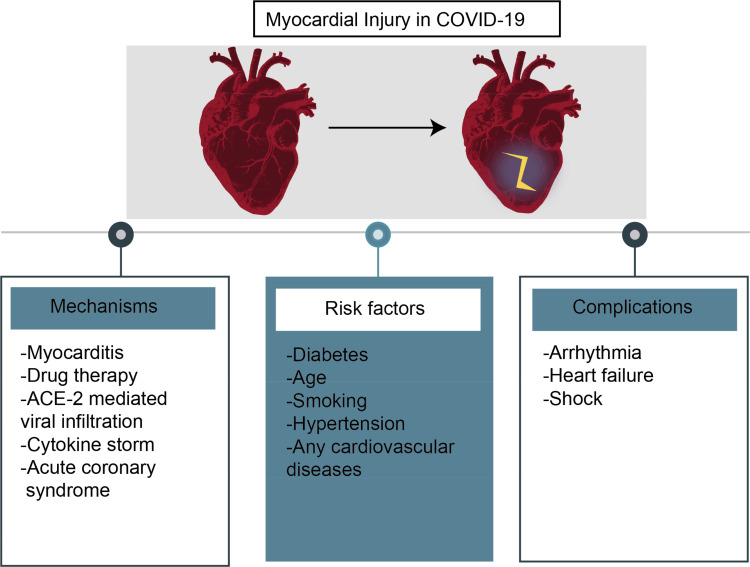
As a result, macrophage infiltration may not be caused by COVID-19. In the unfortunate event of death due to severe COVID-19, it is very unlikely that a patient’s heart has been damaged. Myocardial injury is associated with advanced age, an inflammatory response, and cardiovascular-related comorbidities,20,21 and these are all predictors of in-hospital mortality. A study suggests that multimodality imaging might help doctors better diagnose individuals with COVID-19ʹs cardiovascular difficulties and learn more about the disease’s microvascular component.22 Figure 2 depicts myocardial injury in COVID-19 as an example.
Figure 2.
An illustration of myocardial injury in COVID-19.
Individualized treatment plans may be tailored to each patient based on the amount of plaque in their arteries. CMR scanning methods should be employed as the first step in the evaluation of patients who have had an MI and in the investigation of post-accident abnormalities.23,24 Patients and researchers must be careful not to confuse the words “myocarditis,” “myocarditis,” and “myocarditis.” Imaging such as magnetic resonance imaging confirmed the presence of bilateral myocardial edema in my patient.25,26 COVID-19 may induce heart damage by myocarditis, ACS, demand ischemia, and stress cardiomyopathy.27 Some of the SARS-CoV-2-infected patients with COVID-19 were thought to have myocarditis, which caused some of their cardiac damage. Even though coronavirus-induced myocarditis is very rare, it should be noted. Pathology evaluations were given to all who were tested. More than half of the people who went through the procedure died as a result of their suffering.28
“Covid-19” was diagnosed with “purulent fulminant myopericarditis and cardiac tamponade” after an “acute coronary syndrome.” This is since they have a heart infection. A list of those who have SARSCov-2 should include those who have purulent myopericarditis, cardiac tamponade, and circulatory shock, to successfully treat the numerous complicated illnesses in the world. It has a direct effect on the heart’s cardiomyocytes, fibrosis of the interstices, hypoxia, the weakening of the coronary arteries’ plaque, and an inflammatory cytokine response. T cells have been implicated in heart disease, but they are not the sole culprits. It is important for healthcare workers to understand their own reactions to various conditions and how they manage patients.29,30
Patients with life-threatening arrhythmias that have proved hard to treat even with prescription medication should be studied more extensively for complicated mechanical circulatory support systems, particularly if they are in cardiogenic shock. Detecting and responding to problems as soon as they arise may save a great many lives and cure a great deal of illness. When assessing COVID-19 damage, heart muscle injury is employed.31,32 Heart transplant patients who had experienced cardiac trauma were the subjects of a study. The findings suggest that cardiac damage is an independent predictor of death, regardless of any comorbidities, and they show that the extra data considerably boosts predictive capacity when incorporated into regression models. If a patient’s cardiac ailment is caused by a virus, an endomyocardial biopsy may determine if immunosuppression is a therapeutic risk. In individuals with COVID-19, arrhythmias develop for unknown reasons.33,34 Lower numbers of STEMI patients were seen in the COVID-19 study, as well as increased rates of in-hospital mortality, stroke, and hemorrhage among patients getting PPCI at the ICC in Egypt. Repeat revascularization operations and recurrent infarctions also increased in frequency. According to the study, the number of individuals who suffer from heart failure or die has not changed.35
If macrophages from the lungs had carried the virus to the heart, there would have been low-grade inflammation and viruses in the afflicted myocardium.36 Even if they showed no evidence of cardiac injury, all COVID-19 patients had their troponin levels checked. By assessing troponin concentrations, it is not known whether the procedures used to determine what medication to provide to patients would work.37,38 There was a link between the pathology of cardiac troponin I and the 12.5% of COVID-19 patients who had heart disease symptoms. These patients did not have abnormal cardiac troponin I or typical ECG abnormalities, which is in keeping with the findings. People’s health appeared to be the least of their concerns in the wake of the new coronavirus of 2019. Late-stage and extra-systemic factors contributed to the patients’ poor clinical outcomes. It was determined how the COVID-19 pandemic impacted the collateral hearts of those who had an AMI during the outbreak of the disease, as well as their medical histories, clinical characteristics, and final outcomes, because they feared that hospitals were sites where people might become ill during the COVID-19 epidemic. During the pandemic, the number of AMI hospitalizations decreased significantly. The COVID-19 pandemic resulted in a greater mortality rate for patients who had a heart attack during the pandemic than those who had a heart attack before the outbreak. Information on how to manage AMI patients during an outbreak is still critical.39
Effect of COVID-19 on Congenital Heart Disease Patients
Birth defects may lead to congenital heart disease (CHD), which affects people from the moment they are born and lasts a long time. Birth defects that happen by far the most often are called “birth defects.” The ability to predict the future has been slowed down by a lot of different diseases and symptoms. People who have the gene mutation CHD-COVID-19 and who test positive for it may have trouble getting the medicines they need to treat their illnesses. COVID-19 patients with coronary artery disease (CAD) need to be studied more to better understand how CAD affects their health. As the COVID-19 virus spreads around the world’s poorest areas, people with congenital heart disease may be more at risk. Because of what you did, you are likely to think about it for a long time (ACHD). It does not look like the number of people who have ADHD is linked to how difficult their lives are because of their condition. There are a lot of different kinds of acute coronary syndrome (ACHD) and how bad their effects are. It is important for you as a patient to know that acute coronary syndrome (ACHD) can be very painful and even fatal to your health. However, there are many ways that this can happen.40,41
To keep the disease from spreading to other people in the Community, people who are sick should not leave their homes or go to work. Their own safety should also be a priority.
After leaving the hospital, a patient who has been infected with ACHD may not be able to go home. If their health does not get worse, maybe they can go home. So that they are safe at all times, experts can watch and care for them in their own homes. As soon as possible, anyone who thinks this is true should be checked out and treated in an ACHD treatment center. If you or someone you know is having trouble breathing, get them to the hospital as soon as possible.42–44 It may be hard for people with cyanotic disease or heart failure to adjust to a different place if they have to leave their old home.
In addition to how much oxygen is in the blood, the American Heart Association says that people with cyanotic heart disease should be treated based on how well their hearts work. First, doctors must figure out how much their oxygen saturation has changed from when they were healthy. Then, they can figure out how to treat the patient based on their lactate level. Because of things like acute respiratory distress syndrome (ARDS) and mechanical ventilation, the lungs might be able to get more blood and oxygen than they should.45,46 If they have had right heart failure in the past, they are more likely to have it again.
There are now more COVID-19 pandemic patients, which means that cardiologists will soon be more important than they were a few years ago. During the next few decades, this group of people is going to have a big impact on how cardiovascular diseases are treated in the United States. When they get COVID-19, people with cardiovascular disease (CAD) have a much worse chance of dying than people who do not have CAD. The best way to avoid getting infections is to use the most up-to-date methods. Infection control is very important to think about.
Algorithms are becoming more common in the medical field, and their use is rising. How likely is it that someone will get sick or hurt? You might be able to group them based on how well they are when they go to the hospital. One way a doctor or nurse might use this algorithm is to look at things like a patient’s age, psychological profile, and other things to figure out which treatment is best. People who have heart problems may be more likely to get COVID-19 infections because the severity of COVID-19 infections has gone up. People with heart problems have not been proven to be more likely to get COVID-19 infections. When this illness was first found, it was linked to a lot of different symptoms, like tiredness and headaches. You can get heart disease, diabetes, and high blood pressure all at the same time. Even if you have coronary artery disease, heart attacks and strokes are not the only things that can happen because of it (CAD).47
Heart Failure
When the heart’s ability to provide the body’s cells with oxygen and nourishment is reduced, heart failure develops. As a rule, those who have a hard time expressing empathy are to blame. Another term for this illness is congestive heart failure. More than 90% of COVID-19 patients were found to have AHF, which has been associated with a higher-than-average death rate. Patients having a prior diagnosis of COVID-19 are more likely to suffer from heart failure. The mortality rate was raised when GDMT was stopped.48 Coronavirus (COVID-19) infections are more common in people with heart failure and have a worse prognosis. COVID-19 patients with higher troponin levels were shown to have a greater risk of heart attack and muscle injury.49 More than a quarter of those polled experienced mental health issues, according to the poll. When D-dimers increase in patients with worsening respiratory symptoms but no change in imaging, the risk of pulmonary embolism increases. The use of COVID-19 in high dosages as an anticoagulant need’s additional investigation.50 Anybody may be struck down by heart failure at any time. Heart failure is very uncommon, even if you have no family history of heart disease. It was necessary to replace all of the service supplies.51,52 To better identify the impact of COVID-19 on UK HF services, researchers from the UK urged people with HF to complete a survey. COVID-19, a pandemic, had a major influence on the physical activity patterns of many HF patients and had a negative correlation with remote monitoring results.53 Those who do not see their doctor on a regular basis may benefit from telemedicine and remote monitoring.
Physicians who read this article will go away with knowledge they can immediately put to use in their clinical and practice environments. The most current position statement focuses on those with or at risk of developing cardiovascular disease or heart failure.54 (HF). Reducing emergency room visits and deaths for those with chronic heart failure may be helped by home care. During a home visit, an HF nurse specialist or doctor might gather clinical data and do blood tests. Patients with heart failure who are given COVID-19 have an extremely low likelihood of surviving the medication. CoViD-19 has been demonstrated to increase the risk of infection in patients with HF. Those with heart failure who were infected with COVID-19 died at a higher rate. The health risks for patients infected with COVID-19 and those who are not were discovered to be the same.55,56
In individuals with severe COVID-19, cardiometabolic comorbidity is frequent. COVID-19 is more likely to cause problems in patients with heart failure. One out of every four patients had long-term heart failure, and one of those patients died while still in the hospital. Heart failure and COVID-19 patients received the majority of the hospital’s resources. Because of their age, weight gain, and diabetes, they were more likely to be admitted to the hospital than younger patients. As the epidemic spreads, communities like this one that are already at high risk will need even more attention and creativity.57,58
Community heart failure care was significantly affected by the COVID-19 outbreak, and this study used a DMP to analyze this. An intimate medium has been replaced by an impersonal one, as can be observed in this instance. However, both patients and medical experts were enthusiastic about its use.59 Researchers believe that studies like this will have a substantial influence on the future of cardiology treatment through eHealth (CVD). For two reasons, it has been challenging for people with heart failure to deal with the COVID-19 epidemic. Overall, the system and strategy60 have been successfully implemented. Reformed healthcare systems were put in place throughout the globe because of the outbreak of the 2019 Coronavirus Disease pandemic. It was difficult to get to the hospital because of the social distance, the shift in resources, and the complete lockdown. The treatment stop caused harm to some heart failure patients.
Because of the AIDS crisis, healthcare reforms have been implemented. Poor treatment quality and therapy interruptions damage patients with HF. As heart failure may be lethal, coronary artery disease and the COVID-19 gene both increase the risk. COVID-19 is more likely to be administered to those who are already at high risk for serious health problems. Inflammation and coagulopathy are two instances of this kind of disorder. In both cases, heart arrhythmias are more prevalent. There is an increased risk of medication-induced arrhythmia with the use of several medications. In all circumstances, it is difficult to get and retain enough nutrition. As was to be expected, they are also suffering. Co-occurring illnesses are challenging to treat because of the interconnectivity of their symptoms. Heart failure-related inflammation and an elevated sympathetic nervous system are both possible in people with COVID-19. Coagulation issues, irregular heartbeats, and a catabolic environment may be caused by these side effects. Mortality and morbidity rates rise because of the interaction between these two systems. Long-term improvements in patient outcomes and clinical monitoring are envisaged. This year’s coronavirus epidemic poses a larger threat to people with heart failure (HF) than ever before (COVID-19).61,62 An increased risk of infection or illness is associated with high blood pressure. According to this research, COVID-19 has been linked to myocarditis. Because of this epidemic, those with heart failure who use ventricular support systems or donate organs may need further therapy.63 Medication given to patients with the LVAD, HT, or COVID-19 virus has been demonstrated to affect them.
Arrhythmias
SARS-CoV-2, while it just affects the respiratory system, is a risk factor for other bad outcomes since it may induce cardiac problems as well. Patients with COVID-19 have heart arrhythmias that occur more often in those with more advanced illness, and these arrhythmias may contribute to the problems in the patients. Arrhythmias, regarded as a major consequence of COVID-19, should be dealt with as a serious issue. The effects of COVID-19 may lead to abnormal calcium handling, which may result in cardiac arrhythmogenesis, particularly due to the alteration of various ion channels, including changes in cardiac conduction and repolarization characteristics. Additionally, anti-inflammatory medications, such as chloroquine, hydroxychloroquine, and azithromycin, that are currently being investigated as possible treatment agents for COVID-19 are unlikely to improve the condition and are more likely to extend the QT interval on the ECG, increasing the risk of arrhythmia. If the heart’s electrical activity is being monitored, then it is very important to keep a close eye on the activity and to know when arrhythmias are occurring.64
Early diagnosis and treatment are of major importance when it comes to reducing fatality rates. This article explains various pharmacological and therapeutic strategies in response to this problem. Long-term antiviral therapy for viral infections includes treatments that increase the QT interval. Arrhythmias are frequent, and it is said that they are the second most prevalent problem. Numerous explanations for the pro-arrhythmic effects of the SARS-CoV-2 infection have been posited. Many therapies have raised problems of various kinds. This research looked at the prevalence and management of arrhythmias and evaluated whether there were any problems implementing therapy. The heart may be more susceptible to arrhythmias when a patient has SARS-CoV-2. Arrhythmia risk is known to be increased, with TdP and SCD possible, by some drugs in those who already have irregular heartbeats.65
Microvascular Angiopathy
Research on the microvascular angiopathy involvement in COVID-19 is developing quickly, and new data is emerging. The broad variety of tissue pathology and clinical consequences is apparent from the existing body of information about how COVID-19-induced microvascular angiopathy may cause it. Knowing how our cells, chemistry, and illness all play together in our COVID-19 control is key. More work is required to understand the microvascular angiopathic problems associated with COVID-19, since this will help us create innovative treatments for the next global pandemic and come up with a solution.66 COVID-19 is a very virulent pandemic strain that may cause a broad range of cardiac disorders, from myocardial damage to myocardial infarction, heart failure, and fatal cardiac arrest. Patients with coronary artery disease, hypertension, diabetes mellitus, and other coagulation disorders have worse cardiovascular consequences than those without such problems. Another risk factor for pneumocystis is getting older, having a weak immune system, and having a lot of diseases that cause inflammation.67
COVID-19 infections have been connected to heart problems, which are a major cause of serious illness progression. Although a lot of effort is being spent on working out how myocardial damage happens, it’s smart to have more randomized controlled evidence. Doctors should be on the lookout for myocardial damage from COVID-19 infection, so that they may be sure to provide proper primary and secondary prophylaxis to help reduce morbidity and death. Patients with COVID-19 and prior CVD need individualized judgments on treatment choices. Individuals with severe COVID will require routine bedside echos. People with previous cardiovascular disease who arrive with either severe or subtle COVID-19 symptoms should be carefully watched. Supportive measures should be used for individuals who have particularly serious cardiac issues after COVID-19 surgery. Everybody should be encouraged to use conventional measures and social distance.68
The new virus, CVID-19, was generated by SARS-CoV2, and it’s causing a lot of illness and death. It’s an increasing health risk. Patients with COVID-19 often have CVD, which comes with a greater risk of severe illness and death. A significant portion of severe cases and patients with pre-existing CAD or heart failure suffer from myocardial damage or myocardiopathy. So even though there are some questions about how RAAS inhibitors might hurt ACE2 and how they might affect COVID-19, it is still recommended that RAAS inhibitors be used because of the data we have today. So far, only a single RCT or cohort study has shown any established therapeutic effectiveness.69,70 Individuals who suffer from CVD may benefit if there is improved knowledge of the ACE2 protein and antihypertensive medication. The COVID-19 virus could help us learn more about how recombinant ACE2 works, because a random trial on this virus is already taking place.71
Patients with COVID-19 may have life-threatening arrhythmias and refractory shock, or they may just have a modest increase in blood troponin and BNP levels. Patients must have close heart monitoring regardless of whether they take COVID-19 therapy.72 While COVID-19 affects 25% of individuals, doctors are still unsure of the virus’s pathology. Infected iPSC-derived heart cells that had been exposed to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were infected and showed strong changes in their transcriptome and morphology after they were exposed to the virus. Non-severe COVID-19 survivors with no signs of obvious cardiac abnormalities indicate that it is quite frequent. We learned that COVID-19 can cause heart problems and that our findings could help health care workers understand these problems and figure out if COVID-19 survivors need to be checked up on more often.73,74
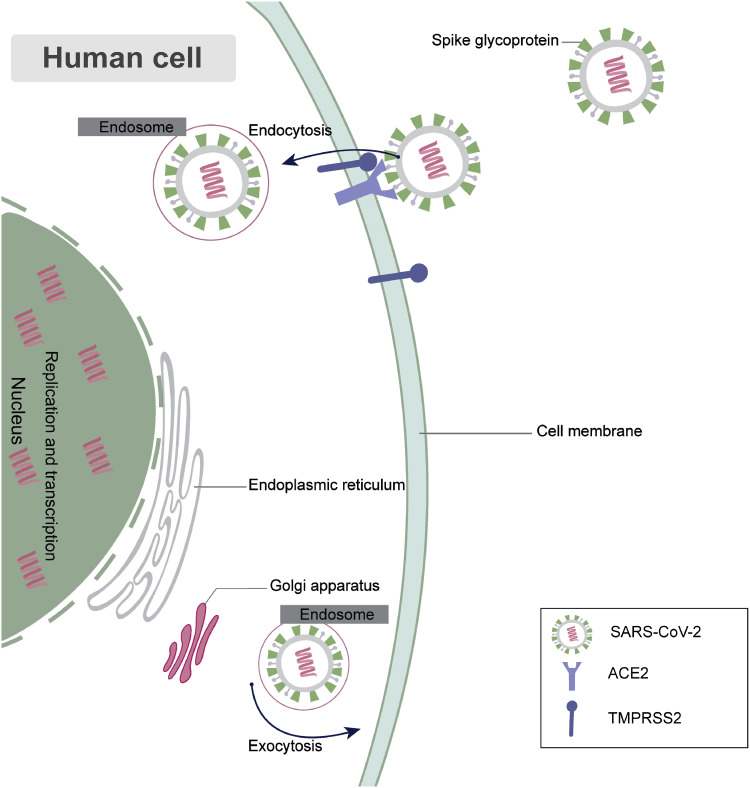
Cardiac damage is often seen in critical care patients with COVID-19, and individuals with levels of hs-cTnI higher than day 3 post-admission are expected to have a worse prognosis. At several timepoints throughout hospitalization, the persistent positive association of hs-cTnI with IL-6 and d-dimer may signify nonspecific cytokine-mediated cardiotoxicity.75–78 In addition to the myocarditis and acute coronary syndromes that were related to the viral insult, other cardiovascular symptoms were shown to have been caused by the viral infection, including acute heart failure, cardiac damage, arrhythmias, and acute pulmonary embolism. Additional research is needed to further investigate the link between SARS-CoV-2 and the heart.3,79–83 Individuals with heart disease have a high risk of negative outcomes and poor long-term prospects. It’s a sudden, infectious illness that has arisen: COVID-19. Although infections can be managed, it is necessary to plan for recurrence with additional coronaviruses and the re-emergence of COVID-19.84–87 The disease causes chronic symptoms that are prone to relapse. Additional research may be required to discover whether individuals with CVD are more likely to develop recurring COVID-19 and if there are new ways to avoid chronic inflammatory problems in patients who survived COVID-19.88 Figure 3 depicts the effect of COVID-19 on human cells.
Figure 3.
The effect of COVID-19 on the human cell.
The people in the COVID-19 study are almost certain to be dealing with severe heart disease problems. Finally, you should get yourself tested for lung disease to see if you have COVID-19, since it may be what you have. You think the treatment is essential. In addition to normal respiratory complications, patients frequently have cardiac issues and blood issues.89 Patients and doctors alike are concerned since the angiotensin-converting enzyme 2 receptor, also known as the ACE2 receptor, has been associated with severe acute respiratory syndrome coronavirus 2, the virus that is responsible for SARS. People who suffer from undiagnosed illnesses, such as heart or brain disorders, are thought to be more likely to get a highly deadly virus.90,91 ARS, which is usually caused by the coronavirus COVID-19, can cause heart problems like myocarditis and irregular heartbeats.92,93
A new study reveals that ARDS, inflammation, and cardiac stress are connected to a tremendous systemic inflammatory response that includes inflammation in the lungs and therefore plaque rupture. Heart conditions include several kinds of symptoms, and the list includes myocardial infarction, arrhythmia, clotting difficulties, and other symptoms.94 The illness, whether in itself or secondary to cardiac issues, may lead to the eventual death of the patient. These studies’ results may be significant in measuring the health of COVID-19 patients in general. The result must be examined from many angles. For the benefit of physicians, COVID-19 patients must be watched for any potential cardiac complications.95 The short-term effects of SARS-CoV-2 on the heart may lead to serious long-term issues. A real miracle for cardiac treatment lies in COVID-19.96
However, it is short on both medicine and vaccines. For people with COVID-19, doctors may use a lot of different types of care, like treatments, counseling, and advice from the internet, to make sure that their patients get the help they need, no matter how they get it. COVID-19ʹs pathology and the development of treatment and vaccine options are important to pay attention to. This will help fight the disease’s overwhelming power. COVID-19 patients have a lot of health problems and have a lot of problems, so new treatments need to be made for them.1 It’s clear from what the cardiovascular doctors are doing that they have little regard for individuals like her, because they are not offering her any kind of therapy at all.97–99 It’s still up in the air whether to use RAS inhibitors because of debates about their safety. Others in the field disagree about whether to use the medication. Because scientists have not found a link between CVD and viral replication, they cannot claim that CVD is caused by viral replication. Because severe COVID-19 is believed to be one of the most frequent complications of CVD and may happen even if there is a lack of clarity on the link between CVD and viral replication, it is often unclear whether the person will develop it or not. Even if COVID-19ʹs findings claim there is no link between RAS inhibition and RAS blockage, one has to wonder whether patients are really being refused therapy because of this.100
Cardiac Injury
Direct trauma to the heart, such as a gunshot wound, may induce blunt cardiac injury (BCI). It is far more difficult to manage cardiac damage in patients with COVID-19 syndrome (a particular disorder), and patients with COVID-19 syndrome often die in hospital.101 Patients with COVID-19 who have ACI are more likely to die, as well as develop respiratory distress syndrome (ARDS). After being admitted to the hospital, patients with COVID-19 have a two-fold greater chance of death from cardiac disease. In the midst of the outbreak, SPECT-MPI examinations experienced a considerable decrease. However, despite the constraints they faced, the number of erroneous research articles remained constant. Concerns over Corona Virus Disease’s impact on public health sparked an outbreak in 2019. There are several sectors where the virus has been known to cause issues.
COVID-19 believes that when it comes to making clinical judgments on cardiovascular therapy, there are several possibilities. The heart plays a major role in many of the body’s problems. In other words, it might be anything from a side effect of the COVID therapy, a side effect of that diagnostic device, or even the treatment itself that raises your risk of cancer. According to the research, some cardiotropic drugs were shown to be associated with a COVID-19 variation. COVID-19 should be always on the minds of cardiologists. We need to find a solution to the issue at hand. As shown in this study, the COVID-19102–104 gadget is critical in the treatment of cardiac disease.
Those who had COVID-19 injections within a week of having a fever were more likely to develop myocarditis. You may be suffering from a heart infection. People infected with COVID-19 are more likely to exhibit signs of their condition, such as those caused by the virus itself. Besides inflammation-induced heart damage, the coronavirus disease 2019 (COVID-19) also causes direct myocarditis, which is a serious complication. Postmortem observations, laboratory testing, and magnetic resonance imaging reveal that cardiac involvement is a possible outcome of COVID-19 infection.105–107 Patients who tested positive for COVID-19, hs-cTnI, upon admission and were able to provide us with sensitive assay information had a substantial influence on clinical outcomes. Individuals in exceptionally high-risk groups as well as those at the opposite end of the spectrum were identified by this method. It has the potential to both detect these individuals and forecast their future risk levels. Researchers found in the experiment that, in addition to helping them find those who had illness, they could also identify those who were at risk, those who would recover on their own, and those who would need intervention.107
Covid-19 has been related to organ failure, particularly severe organ failure, which may cause cardiac damage. As with ARDS in the rest of the body, it’s not obvious how much damage has been done to the heart. Inflammation, elevated iron levels, and clots in the heart are all symptoms of a heart attack. It is imperative that future cardiovascular disease research focuses on the several routes used by COVID-19 in treating heart disease and organ failure. Heart failure and severe arrhythmia may occur because of the spread of a virus in the body. COVID-19 patients and those who have been affected by the virus need a fundamental shift in the way hospitals operate. This alteration was brought on by the virus. Currently, only life-saving treatments are being performed. The number of STEMIs and NSTEMIs in hospitals has decreased dramatically in recent years. As a result, the quality of treatment for people with heart failure has declined. Each cardiac ailment has a similar set of symptoms. Patients’ heart health may be checked through cardiac examinations like stress echocardiography and transesophageal echocardiography, as well as guidance on how to improve their condition.108–110
Because of this, specialists have concluded that the patient is at a considerably greater risk of developing heart disease. Patients with COVID-19 and respiratory weakness are considerably more likely to be diagnosed in hospitals than those with heart failure. In this case,111 is supported by a single echo evaluation. To learn how the COVID-19 pandemic coronavirus impacts the clinical performance, anxiety level, and attitudes of cardiologists, researchers conducted a study. Keep in mind that individuals are more likely to wait until they have signs of a heart attack before seeking care. In addition to putting their lives in danger, this also has a negative impact on the economy.
For patients on ECMO, an ECMO-specific venting device may be helpful. Maintaining a normal blood pressure level while allowing the patient to prepare for surgery or a transplant will be possible with this strategy. By making patients feel unwanted, the strategy aims to keep hospitals safe. In the event of a factory closure or high levels of employee absenteeism, economic policy devises strategies to assist businesses and their employees remain productive. Efforts are being made to find a solution. In the future, cardiologists will be expected to think outside the box and come up with novel solutions to complex problems.112–114 A new list has been added to this page: “COVID-19” may be searched for in PubMed using the terms “cardiology” and “infarction”.115
People who have difficulty getting to an emergency hospital due to transportation issues are less unwell than they were in the past, despite poorer results. You never know when you are going to have an infection, so it’s important to do all you can to improve your circulation. One kind of cardiac disease known as myocardial ischemia damages the heart. Myocardial ischemia (or infarction) disrupts blood flow to the heart. Protecting the cardiovascular system is critical when influenza is in the air.116,117 Still, there is a greater chance for SARS-CoV-2 patients to have blocked arteries that lead to heart attacks and strokes. Even if all medical treatment options have been tried, this can still happen.118
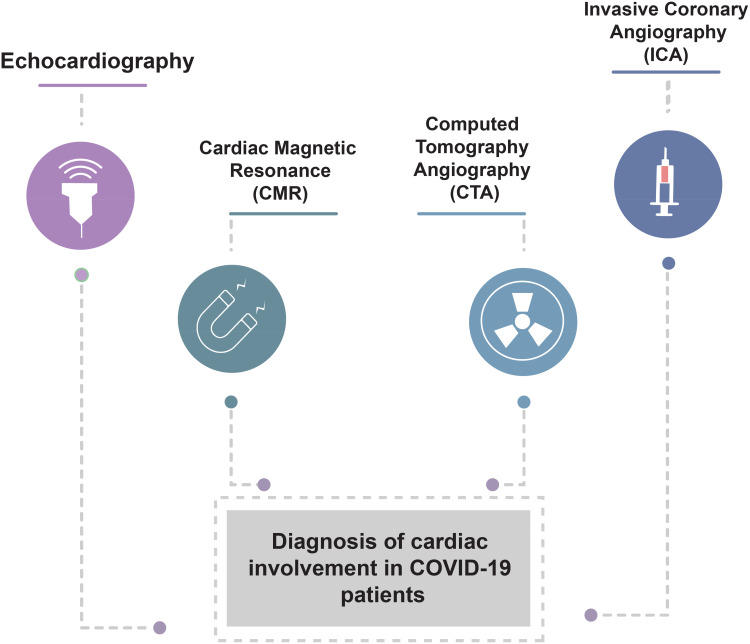
In Figure 4, the COVID-19 individuals’ cardiac involvement is seen. ICU patients are more likely to develop a condition known as acroischemia, which is caused by hardened arteries, particularly in patients with COVID-19.119 A fever, coughing, and shortness of breath are the most common signs of the sickness, but it may also bring on other, strange symptoms. Blood clots, strokes, and heart attacks are all signs of a serious clotting disorder. SARS-CoV-2 patients are concerned about hypercoagulability.120
Figure 4.
The different types of diagnosis of cardiac involvement of COVID-19 patients.
Conclusion
The SARS-CoV-2 virus causes Coronavirus disease (COVID-19), a potentially lethal viral illness. When an infected person coughs, sneezes, talks, sings, or breathes, tiny liquid particles emitted from their mouths or noses may spread viruses via the air. Particles that fall into this group include small aerosols and bigger respiratory droplets. There are several ways to acquire the virus COVID-19, including inhaling the virus from a contaminated surface or touching it with your eyes, nose, or mouth. People are more prone to getting the virus if they are inside or in large groups than if they are outdoors. Several people have expressed concern about the pandemic’s indirect effects, according to this review. There has been a decrease in the number of patients admitted to hospitals with acute cardiovascular problems, increasing the possibility that people are avoiding hospitals for fear of getting the coronavirus-2 virus that causes severe acute respiratory syndrome (SARS-CoV-2). It’s possible that other variables, like the strain on healthcare systems, influenced the result both directly and indirectly. A lot of heart problems have been linked to the drug Covid-19, like arrhythmias, heart failure, and microvascular angiopathy.
Acknowledgment
The authors are thankful to the Institute of Research and Consulting Studies at King Khalid University for supporting this research through grant number # 4-N-20/21.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Zheng Y, Ma Y, Zhang J, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiology. 2020;43:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quagliariello V, Bonelli A, Caronna A, et al. SARS-CoV-2 infection and cardioncology: from cardiometabolic risk factors to outcomes in cancer patients. Cancers. 2020;12:3316. doi: 10.3390/cancers12113316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr. 2020;14:247–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mishra A, Sahu K, George AA, Lal A. A review of cardiac manifestations and predictors of outcome in patients with COVID – 19. Heart Lung. 2020;49:848–852. doi: 10.1016/j.hrtlng.2020.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hendren NS, Drazner M, Bozkurt B, Cooper L. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;141:1903–1914. doi: 10.1161/CIRCULATIONAHA.120.047349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu H, Rhee J, Cheng P, et al. Cardiovascular complications in patients with COVID-19: consequences of viral toxicities and host immune response. Curr Cardiol Rep. 2020;22:456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Long B, Brady W, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38(7):1504–1507. doi: 10.1016/j.ajem.2020.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu J, Virani S, Alam M, Denktas A, Hamzeh I, Khalid U. Coronavirus disease‐19 and cardiovascular disease: a risk factor or a risk marker? Rev Med Virol. 2020;31. doi: 10.1002/rmv.2172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao M, Wang M, Zhang J, et al. Advances in the relationship between coronavirus infection and cardiovascular diseases. Biomed Pharmacother. 2020;127:110230. doi: 10.1016/j.biopha.2020.110230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazaridis C, Vlachogiannis NI, Bakogiannis C, et al. Involvement of cardiovascular system as the critical point in coronavirus disease 2019 (COVID-19) prognosis and recovery. Hellenic J Cardiol. 2020;61:381–395. doi: 10.1016/j.hjc.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Talasaz A, Kakavand H, Tassell BV, et al. Cardiovascular complications of COVID-19: pharmacotherapy perspective. Cardiovasc Drugs Ther. 2020;4:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barison A, Aimo A, Castiglione V, et al. Cardiovascular disease and COVID-19: les liaisons dangereuses. Eur J Prev Cardiol. 2020;27:1017–1025. doi: 10.1177/2047487320924501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts KA, Colley L, Agbaedeng T, Ellison-Hughes G, Ross M. Vascular manifestations of COVID-19 – thromboembolism and microvascular dysfunction. Front cardiovasc med. 2020;7. doi: 10.3389/fcvm.2020.598400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sabioni L, Tibiriçá E, Lamas C, Amorim GD, Lorenzo AD. Systemic microvascular dysfunction in COVID-19. Am J Cardiovasc Dis. 2020;10(4):386–391. [PMC free article] [PubMed] [Google Scholar]
- 15.Tahir F, Arif TB, Ahmed J, Malik F, Khalid M. Cardiac manifestations of coronavirus disease 2019 (COVID-19): a comprehensive review. Cureus. 2020;12:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Q, Xu L, Dai Y, et al. Cardiovascular manifestations in severe and critical patients with COVID‐19. Clin Cardiol. 2020;43:796–802. doi: 10.1002/clc.23384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kurz DJ, Eberli FR. Cardiovascular aspects of COVID-19. Swiss Med Wkly. 2020;150:w20417. doi: 10.4414/smw.2020.20417 [DOI] [PubMed] [Google Scholar]
- 18.Cannata’ A, Watson SA, Daniel A, et al. Impact of the COVID-19 pandemic on in-hospital mortality in cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. 2021. doi: 10.1093/eurjpc/zwab119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rali A, Ranka S, Shah Z, Sauer A. Mechanisms of myocardial injury in coronavirus disease 2019. Cardiac Failure Rev. 2020;6. doi: 10.15420/cfr.2020.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Basso C, Leone O, Rizzo S, et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J. 2020;41(39):3827–3835. doi: 10.1093/eurheartj/ehaa664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shi S, Qin M, Cai Y, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–2079. doi: 10.1093/eurheartj/ehaa408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Money JE, Sekaran N, Minder CM, et al. Myocardial infarction associated with regional myocardial flow deficit and normal coronary arteries in a patient with COVID-19: a case report. Cardiol Cardiovasc Med. 2020;04(06). doi: 10.26502/fccm.92920167 [DOI] [Google Scholar]
- 23.Azanza DX, Ibargüengoitia MC, Uvera SR. Cardiac computed tomography as an alternative technique in the assessment of acute myocardial ischemia in the context of COVID-19 infection. Cureus. 2020;12:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shchedrygina A, Nagel E, Puntmann V, Valbuena-Lopez S. COVID-19 myocarditis and prospective heart failure burden. Expert Rev Cardiovasc Ther. 2020;19:5–14. doi: 10.1080/14779072.2021.1844005 [DOI] [PubMed] [Google Scholar]
- 25.Mele D, Flamigni F, Rapezzi C, Ferrari R. Myocarditis in COVID-19 patients: current problems. Intern Emerg Med. 2021;1–7. doi: 10.1007/s11739-020-02494-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inciardi R, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA cardiol. 2020;5(7):819. doi: 10.1001/jamacardio.2020.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coyle J, Igbinomwanhia E, Sánchez-Nadales A, Danciu S, Chu C, Shah N. A recovered case of COVID-19 myocarditis and ARDS treated with corticosteroids, tocilizumab, and experimental AT-001. Jacc Case Rep. 2020;2:1331–1336. doi: 10.1016/j.jaccas.2020.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ho JS, Sia C, Chan M, Lin W, Wong R. Coronavirus-induced myocarditis: a meta-summary of cases. Heart Lung. 2020;49:681–685. doi: 10.1016/j.hrtlng.2020.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khatri A, Wallach F. Coronavirus disease 2019 (Covid-19) presenting as purulent fulminant myopericarditis and cardiac tamponade: a case report and literature review. Heart Lung. 2020;49(6):858–863. doi: 10.1016/j.hrtlng.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, Amanullah A. Myocardial injury and COVID-19: possible mechanisms. Life Sci. 2020;253:117723. doi: 10.1016/j.lfs.2020.117723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tam C, Cheung K, Lam S, et al. Impact of coronavirus disease 2019 (COVID‐19) outbreak on outcome of myocardial infarction in Hong Kong, China. Catheter Cardiovasc Interv. 2020;97:E194–E197. doi: 10.1002/ccd.28943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agdamag A, Edmiston J, Charpentier V, et al. Update on COVID-19 myocarditis. Medicina. 2020;56(12):678. doi: 10.3390/medicina56120678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorente-Ros A, Ruiz JM, Rincón LM, et al. Myocardial injury determination improves risk stratification and predicts mortality in COVID-19 patients. Cardiol J. 2020. doi: 10.5603/CJ.a2020.0089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19–related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17:1463–1471. doi: 10.1016/j.hrthm.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ayad S, Shenouda R, Henein M. The impact of COVID-19 on in-hospital outcomes of ST-Segment elevation myocardial infarction patients. J Clin Med. 2021;10(2):278. doi: 10.3390/jcm10020278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tavazzi G, Pellegrini C, Maurelli M, et al. Myocardial localization of coronavirus in COVID‐19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–915. doi: 10.1002/ejhf.1828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Efros O, Barda N, Meisel E, et al. Myocardial injury in hospitalized patients with COVID-19 infection—risk factors and outcomes. PLoS One. 2021;16(2):e0247800. doi: 10.1371/journal.pone.0247800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lala A, Johnson K, Russak A, et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 Infection. medRxiv. 2020;45:12–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Toscano O, Cosentino N, Campodonico J, Bartorelli AL, Marenzi G. Acute myocardial infarction during the COVID-19 pandemic: an update on clinical characteristics and outcomes. Front cardiovasc med. 2021;8. doi: 10.3389/fcvm.2021.648290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Deng Q, Hu B, Zhang Y, et al. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int J Cardiol. 2020;311:116–121. doi: 10.1016/j.ijcard.2020.03.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haiduc AA, Ogunjimi M, Shammus R, et al. COVID-19 and congenital heart disease: an insight of pathophysiology and associated risks. Cardiol Young. 2020;17:1–8. [DOI] [PubMed] [Google Scholar]
- 42.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a Modelling Study. Lancet. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan JF-W, Yuan S, Kok K-H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Radke R, Frenzel T, Baumgartner H, Diller G. Adult congenital heart disease and the COVID-19 pandemic. Heart. 2020;106:1302–1309. doi: 10.1136/heartjnl-2020-317258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diller G, Gatzoulis M, Broberg C, et al. Coronavirus disease 2019 in adults with congenital heart disease: a position paper from the ESC working group of adult congenital heart disease, and the International Society for Adult Congenital Heart Disease. Eur Heart J. 2020;24:654–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alsaied T, Aboulhosn J, Cotts T, et al. Coronavirus disease 2019 (COVID‐19) pandemic implications in pediatric and adult congenital heart disease. J Am Heart Assoc. 2020;9. doi: 10.1161/JAHA.120.017224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rey JR, Caro-Codón J, Rosillo S, et al. Heart failure in Covid‐19 patients: prevalence, incidence and prognostic implications. Eur J Heart Fail. 2020;22:2205–2215. doi: 10.1002/ejhf.1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tomasoni D, Italia L, Adamo M, et al. COVID- 19 and heart failure: from infection to inflammation and angiotensin II stimulation. Searching for evidence from a new disease. Eur J Heart Fail. 2020;22:957–966. doi: 10.1002/ejhf.1871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ullah W, Saeed R, Sarwar U, Patel RV, Fischman D. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. Jacc Case Rep. 2020;2:1379–1382. doi: 10.1016/j.jaccas.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bader F, Manla Y, Atallah B, Starling R. Heart failure and COVID-19. Heart Fail Rev. 2020;1–10. doi: 10.1007/s10741-019-09838-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sankaranarayanan R, Hartshorne-Evans N, Redmond-Lyon S, et al. The Impact of COVID-19 on the management of heart failure -A United Kingdom Patient Questionnaire Study. medRxiv. 2020;45:678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bertagnin E, Greco A, Bottaro G, et al. Remote monitoring for heart failure management during COVID-19 pandemic. Int J Cardiol. 2021;32. doi: 10.1016/j.ijcha.2021.100724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kałużna-Oleksy M, Gackowski A, Jankowska EA, et al. The patient with heart failure in the face of the coronavirus disease 2019 pandemic. Kardiologia Polska. 2020;78:618–631. [DOI] [PubMed] [Google Scholar]
- 55.Ata F, Montoro-López M, Awouda S, Elsukkar A, Badr A, Patel A. COVID-19 and heart failure: the big challenge. heart views. Off J Gulf Heart Assoc. 2020;21:187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chatrath N, Kaza N, Pabari PA, et al. The effect of concomitant COVID‐19 infection on outcomes in patients hospitalized with heart failure. ESC Heart Failure. 2020;7:4443–4447. doi: 10.1002/ehf2.13059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bhatt A, Jering KS, Vaduganathan M, et al. Clinical outcomes in patients with heart failure hospitalized with COVID-19. JACC Heart Fail. 2021;9:65–73. doi: 10.1016/j.jchf.2020.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kerr B, Pharithi R, Barrett M, et al. Changing to remote management of a community heart failure population during COVID-19 – clinician and patient perspectives’. International Journal of Cardiology.. Heart Vasc. 2020;31:456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Orso F, Migliorini M, Herbst A, et al. Protocol for telehealth evaluation and follow-up of patients with chronic heart failure during the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21:1803–1807. doi: 10.1016/j.jamda.2020.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reza N, DeFilippis E, Jessup M. Secondary impact of the COVID-19 pandemic on patients with heart failure. Circulation. 2020;34:534. [DOI] [PubMed] [Google Scholar]
- 61.Bakhsh A, Alqaseer M, Alayoubi F, et al. Health care delivery for heart failure patients during the COVID-19 pandemic; A consensus of The Saudi Heart Failure Working Group (Saudi-HF). J Saudi Heart Assoc. 2020;32:20–23. doi: 10.37616/2212-5043.1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khan E. Heart failure and COVID-19: synergism of two inflammatory conditions? Br J Community Nurs. 2021;26(1):18–25. doi: 10.12968/bjcn.2021.26.1.18 [DOI] [PubMed] [Google Scholar]
- 63.DeFilippis E, Reza N, Donald E, Givertz M, Lindenfeld J, Jessup M. Considerations for heart failure care during the COVID-19 pandemic. JACC Heart Fail. 2020;8:681–691. doi: 10.1016/j.jchf.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang Y, Wang Z, Tse G, et al. Cardiac arrhythmias in patients with COVID‐19. J Arrhythmia. 2020;36:827–836. doi: 10.1002/joa3.12405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Malaty M, Kayes T, Amarasekera A, Kodsi M, Macintyre C, Tan T. Incidence and treatment of arrhythmias secondary to coronavirus infection in humans: a systematic review. Eur J Clin Invest. 2020;51. doi: 10.1111/eci.13428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nalugo M, Schulte L, Masood M, Zayed M. Microvascular angiopathic consequences of COVID-19. Front Cardiovasc Med. 2020;8:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sattar Y, Ullah W, Rauf H, et al. COVID-19 cardiovascular epidemiology, cellular pathogenesis, clinical manifestations and management. Int J Cardiol. 2020;29:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Krittanawong C, Kumar A, Hahn J, et al. Cardiovascular risk and complications associated with COVID-19. Am J Cardiovasc Dis. 2020;10(4):479–489. [PMC free article] [PubMed] [Google Scholar]
- 69.Samidurai A, Das A. Cardiovascular complications associated with COVID-19 and potential therapeutic strategies. Int J Mol Sci. 2020;21:6790. doi: 10.3390/ijms21186790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Matsushita K, Marchandot B, Jesel L, Ohlmann P, Morel O. Impact of COVID-19 on the cardiovascular system: a review. J Clin Med. 2020;9:1407. doi: 10.3390/jcm9051407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am College Cardiol. 2020;75:2352–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dhakal B, Sweitzer N, Indik J, Acharya D, William P. SARS-CoV-2 infection and cardiovascular disease: COVID-19 heart. Heart Lung Circ. 2020;29:973–987. doi: 10.1016/j.hlc.2020.05.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pérez-Bermejo JA, Kang S, Rockwood SJ, et al. SARS-CoV-2 infection of human iPSC–derived cardiac cells reflects cytopathic features in hearts of patients with COVID-19. Sci Transl Med. 2021;13. doi: 10.1126/scitranslmed.abf7872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhou M, Wong C, Un K, et al. Cardiovascular sequalae in uncomplicated COVID-19 survivors. PLoS One. 2021;16(2):e0246732. doi: 10.1371/journal.pone.0246732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li C, Jiang J, Wang F, et al. Longitudinal correlation of biomarkers of cardiac injury, inflammation, and coagulation to outcome in hospitalized COVID-19 patients. J Mol Cell Cardiol. 2020;147:74–87. doi: 10.1016/j.yjmcc.2020.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1–8. doi: 10.1001/jamacardio.2020.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA cardiol. 2020;5:802. doi: 10.1001/jamacardio.2020.0950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cao J, Zheng Y, Luo Z, et al. Myocardial injury and COVID-19: serum hs-cTnI level in risk stratification and the prediction of 30-day fatality in COVID-19 patients with no prior cardiovascular disease. Theranostics. 2020;10:9663–9673. doi: 10.7150/thno.47980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Si D, Du B, Ni L, et al. Death, discharge and arrhythmias among patients with COVID-19 and cardiac injury. Can Med Assoc J. 2020;192:E791- E798. doi: 10.1503/cmaj.200879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bugger H, Gollmer J, Pregartner G, et al. Complications and mortality of cardiovascular emergency admissions during COVID-19 associated restrictive measures. PLoS One. 2020;15:e0239801. doi: 10.1371/journal.pone.0239801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hanfi Y, Alasnag M, Alshehri H, et al. Non-invasive cardiac imaging during the coronavirus disease 2019 (COVID-19) pandemic: a statement from the cardiac imaging working group of the Saudi Heart Association. J Saudi Heart Assoc. 2020;32:6–10. doi: 10.37616/2212-5043.1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Centurión O, Scavenius KE, García LB, Torales J, Miño L. Potential mechanisms of cardiac injury and common pathways of inflammation in patients with COVID-19. Crit Pathw Cardiol. 2020;34:456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shirazi S, Mami S, Mohtadi N, et al. Sudden cardiac death in COVID-19 patients, a report of three cases. Future Cardiol. 2020;17:113–118. doi: 10.2217/fca-2020-0082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mahenthiran AK, Mahenthiran A, Mahenthiran J. Cardiovascular system and COVID-19: manifestations and therapeutics. Rev Cardiovasc Med. 2020;21(3):399–409. doi: 10.31083/j.rcm.2020.03.124 [DOI] [PubMed] [Google Scholar]
- 85.Liao C, Chang W, Yu W, Toh H. Management of acute cardiovascular events in patients with COVID-19. Rev Cardiovasc Med. 2020;21(4):577–581. [DOI] [PubMed] [Google Scholar]
- 86.Chatzis D, Magounaki KT, Pantazopoulos I, Johnson E, Tsioufis K. COVID-19 pandemic and cardiovascular disease: where do we stand? Minerva Cardioangiol. 2020;68. doi: 10.23736/S0026-4725.20.05298-6 [DOI] [PubMed] [Google Scholar]
- 87.Wang B. Susceptibility and prognosis of COVID-19 patients with cardiovascular disease. Open Heart. 2020;7:e001310. doi: 10.1136/openhrt-2020-001310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nejadghaderi SA, Heidari A, Shakerian N, Saghazadeh A, Rezaei N. Cardiovascular system is at higher risk of affecting by COVID-19. Acta Bio Medica. 2020;91:e2020018- e2020018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Massoomi MR, Anderson RD, Ahmed MM, et al. Cardiovascular considerations for the internist and hospitalist in the COVID-19 era. Am J Med. 2020;133:1254–1261. doi: 10.1016/j.amjmed.2020.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Larson A, Savastano L, Kadirvel R, Kallmes D, Hassan A, Brinjikji W. Coronavirus disease 2019 and the cerebrovascular‐cardiovascular systems: what Do We Know So Far? J Am Heart Assoc. 2020;9. doi: 10.1161/JAHA.120.016793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Du H, Wang D, Chen C. The potential effects of DPP‐4 inhibitors on cardiovascular system in COVID‐19 patients. J Cell Mol Med. 2020;24:10274–10278. doi: 10.1111/jcmm.15674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rastogi A, Tewari P. Covid 19 and its cardiovascular effects. Ann Card Anaesth. 2020;23:401–408. doi: 10.4103/aca.aca_237_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gerc V, Masic I, Salihefendic N, Zildžić M. Cardiovascular diseases (CVDs) in COVID-19 pandemic era. Mater Sociomed. 2020;32:158–164. doi: 10.5455/msm.2020.32.158-164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bandyopadhyay D, Akhtar T, Hajra A, et al. COVID-19 pandemic: cardiovascular complications and future implications. Am J Cardiovasc Drugs. 2020;43:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sabatino J, Rosa SD, Salvo GD, Indolfi C. Impact of cardiovascular risk profile on COVID-19 outcome. A meta-analysis. PLoS One. 2020;15:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mattioli A, Puviani MB, Nasi M, Farinetti A. COVID-19 pandemic: the effects of quarantine on cardiovascular risk. Eur J Clin Nutr. 2020;3:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Li G, Saguner A, An J, et al. Cardiovascular disease during the COVID-19 pandemic: think ahead, protect hearts, reduce mortality. Cardiol J. 2020. doi: 10.5603/CJ.a2020.0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dixon D, Tassell BV, Vecchié A, et al. Cardiovascular considerations in treating patients with coronavirus disease 2019 (COVID-19). J Cardiovasc Pharmacol. 2020;75:359–367. doi: 10.1097/FJC.0000000000000836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Medzikovic L, Cunningham C, Li M, et al. Sex differences underlying preexisting cardiovascular disease and cardiovascular injury in COVID-19. J Mol Cell Cardiol. 2020;148:25–33. doi: 10.1016/j.yjmcc.2020.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yu J, Wu B, Yang J, Lei X, Shen W. Cardio-cerebrovascular disease is associated with severity and mortality of COVID-19: a systematic review and meta-analysis. Biol Res Nurs. 2020;23:258–269. doi: 10.1177/1099800420951984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kow CS, Zaidi S, Hasan S. Cardiovascular disease and use of renin-angiotensin system inhibitors in COVID-19. Am J Cardiovasc Drugs. 2020;45:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Santoso A, Pranata R, Wibowo A, Al-Farabi MJ, Huang I, Antariksa B. Cardiac injury is associated with mortality and critically ill pneumonia in COVID-19: a meta-analysis. Am J Emerg Med. 2020;43:546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Saleh SK, Oraii A, Soleimani A, et al. The association between cardiac injury and outcomes in hospitalized patients with COVID-19. Intern Emerg Med. 2020;4:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hasnie UA, Bhambhvani PG, Iskandrian A, Hage F. Prevalence of abnormal SPECT myocardial perfusion imaging during the COVID-19 pandemic. Eur J Nucl Med Mol Imaging. 2021;45:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kishor K, Marwah R, Anantharaj A, Kalra S. Cardiovigilance in COVID 19. JPMA. 2020;70(Suppl3):S77–S80. [DOI] [PubMed] [Google Scholar]
- 106.Leon-Constantin M, Maștaleru A, Abdulan I, Zota M, Cojocariu S, Mitu F. Cardiac complications in patients infected with COVID-19. Internal Med. 2020;17:55–62. doi: 10.2478/inmed-2020-0134 [DOI] [Google Scholar]
- 107.Wang H, Li R, Zhou Z, et al. Cardiac involvement in COVID-19 patients: mid-term follow up by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2021;23:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Michieli LD, Babuin L, Vigolo S, et al. Using high sensitivity cardiac troponin values in patients with SARS-CoV-2 infection (COVID-19): the Padova experience. Clin Biochem. 2021;90:8–14. doi: 10.1016/j.clinbiochem.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Metkus T, Sokoll L, Barth AS, et al. Myocardial injury in severe COVID-19 compared with non–COVID-19 acute respiratory distress syndrome. Circulation. 2020;143:553–565. doi: 10.1161/CIRCULATIONAHA.120.050543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Maier SR, Rodrigues J, Sudré MR, Dessotte C. Cardiac complications in patients with COVID-19: an integrative literature review. Aquichan. 2020;20:2043. doi: 10.5294/aqui.2020.20.4.3 [DOI] [Google Scholar]
- 111.Yasmin F, Shujauddin S, Naeem A, et al. Exploring the impact of the COVID-19 pandemic on provision of cardiology services: a scoping review. Rev Cardiovasc Med. 2021;22(1):83–95. doi: 10.31083/j.rcm.2021.01.241 [DOI] [PubMed] [Google Scholar]
- 112.Heuvel FM, Vos JL, Koop Y, et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth Heart J. 2020;28:410–417. doi: 10.1007/s12471-020-01458-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kaya Y, Bostan S, Düğeroğlu H, Özbilen M, Keskin H. The effect of COVID-19 pandemic on the anxiety levels of internal medicine physicians and practice of internal medicine clinics. J Int Health Sci Manage. 2020. doi: 10.48121/jihsam.772710 [DOI] [Google Scholar]
- 114.Bakhshi H, Gattani R, Ekanem E, et al. Ventricular septal rupture and cardiogenic shock complicating STEMI during COVID-19 pandemic: an old foe re-emerges. Heart Lung. 2020;50:292–295. doi: 10.1016/j.hrtlng.2020.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ferrari R, Pasquale GD, Rapezzi C. 2019 CORONAVIRUS: what are the implications for cardiology? Eur J Prev Cardiol. 2020;27:793–796. doi: 10.1177/2047487320918102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Grzegorowska O, Lorkowski J. Possible correlations between atherosclerosis, acute coronary syndromes and COVID-19. J Clin Med. 2020;9:3746. doi: 10.3390/jcm9113746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dash S, Dhiman A, Pandey P, Kumar A. Late presentation of acute coronary syndrome during COVID-19. Med J Dr D Y Patil Vidyapeeth. 2020;13:269–273. doi: 10.4103/mjdrdypu.mjdrdypu_209_20 [DOI] [Google Scholar]
- 118.Hatami F, Valizadeh N, Ramandi M. Emerging mechanisms for the new coronavirus-related myocardial injury and ischemia: a review of the literature. Anatolian J Cardiol. 2020;24:7–12. doi: 10.14744/AnatolJCardiol.2020.68166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zakeri AS, Jadhav A, Sullenger B, Nimjee S. Ischemic stroke in COVID-19-positive patients: an overview of SARS-CoV-2 and thrombotic mechanisms for the neurointerventionalist. J Neurointerv Surg. 2020;13:202–206. doi: 10.1136/neurintsurg-2020-016794 [DOI] [PubMed] [Google Scholar]
- 120.Alonso M, Mata-Forte T, García-León N, et al. Incidence, characteristics, laboratory findings and outcomes in acro-ischemia in COVID-19 patients. Vasc Health Risk Manag. 2020;16:467–478. doi: 10.2147/VHRM.S276530 [DOI] [PMC free article] [PubMed] [Google Scholar]