Abstract
Purpose
(Neo) adjuvant chemotherapy decreases the risk of recurrence and improves overall survival among breast cancer patients; however, delays in chemotherapy initiation are associated with adverse health outcomes. The causes of delay are complex and include interrelated social, economic, cultural, environmental, and health system factors. Project Start was a qualitative study designed to assess and identify the multilevel factors contributing to the barriers and facilitators of initiating chemotherapy.
Patients and Methods
Women diagnosed with primary invasive breast cancer who experienced ≥60 day delay in (neo) adjuvant chemotherapy initiation were included. Participants completed semi-structured interviews exploring barriers and facilitators to starting chemotherapy. Interviews were transcribed and coded to identify themes using the Sort and Sift, Think and Shift analytic approach. This analysis included thorough examination of the data by advancing through iterative analytic phases to identify core topics within and across transcripts.
Results
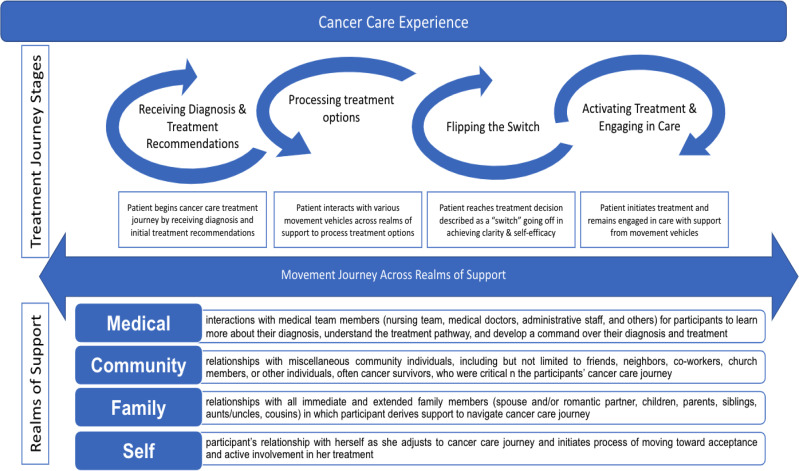
We enrolled (N=22) participants with median age at diagnosis 53.5 years (range 27–70) who identified as Latina (n=8), Black (n=5), and non-Latina White (n=9). Participants described a common chemotherapy initiation process reflecting their unique needs as they transitioned through four stages: 1) receiving diagnosis and treatment recommendations; 2) processing treatment options; 3) “Flipping the Switch”; and 4) activating treatment and engaging in care. Limited explicit insight into their chemotherapy delay was expressed. Engagement across the self-, family-, community-, and medical-realms revealed interlinked and pivotal sources of support that helped participants navigate toward initiating chemotherapy. Specifically, the overarching themes included logistical, emotional, financial, and social sources of support and the relationship of these sources of support to participants’ perceived self-efficacy to move toward initiating treatment.
Conclusion
Activating women to be engaged in the treatment process across multiple levels appeared to facilitate initiating chemotherapy. Multilevel interventions that engage the patient, family, community, and medical team may support the initiation of timely chemotherapy.
Keywords: breast cancer, care delivery, chemotherapy, treatment delay, oncology, qualitative, patient perspectives
Plain Language Summary
The use of adjuvant chemotherapy has a dramatic impact decreasing the risk of cancer recurrence and improving survival; however, delays in the administration of adjuvant chemotherapy significantly reduce this benefit. We designed Project Start to evaluate factors at the operational, medical, and personal/social level, using a semi-structured interview guide.
While the interview guide included questions addressing chemotherapy delays, explicit insight into their chemotherapy delay was rare. Participants described barriers and facilitators at the patient, family, medical, and community levels. Barriers at the patient level included patient’s hesitancy to initiate chemotherapy due to shock, fear, and denial. Within the family level, we learned of participant’s family roles (eg, caregiving, income), treatment costs, and the need for emotional support (eg, not shutting family members out). Participants sought out and relied heavily on support from their communities (eg, churches, other patients, survivors). Finally, participants described their reliance on the medical team for information, the trust needed to navigate their treatment process, and the challenge of managing information associated with their treatment. Participants also described the importance of self-efficacy to take an active role in treatment.
Findings are helping the research team inform the design of a pilot study to test the acceptability and feasibility of a patient navigation intervention aimed at reducing time to chemotherapy. Our objectives are patient-centered and have the potential to improve outcomes and reduce health disparities.
Introduction
Improvements in breast cancer treatment and early detection have resulted in decreased mortality.1 Among patients with early-stage breast cancer, chemotherapy dramatically improves outcomes; however, delays in treatment initiation may limit its benefits. Delays in administration of (neo) adjuvant chemotherapy have been associated with adverse outcomes.2 Patients who delay (neo) adjuvant chemotherapy initiation ≥60 days from the date of surgery or the date of diagnosis have been found to have a statistically significant decrease in overall survival.2–4
Evidence suggests that socially vulnerable populations, such as patients of low socioeconomic status (SES), older age, those without a partner, with non-private insurance, or who are Hispanic or African American (AA) are more likely to experience delays.3,5,6 Such disparities largely reflect numerous social, cultural, and structural obstacles to receiving healthcare services. Racial/ethnic minorities are more likely to experience poverty, be uninsured, and be burdened by the lowest levels of health literacy – all associated with diminished health outcomes.7,8 Examining the complex interaction between the health care system and social, cultural, and structural factors is needed to identify contributors to disparate delays in breast cancer treatment initiation and improve outcomes among vulnerable communities.
Project START aimed to conduct a qualitative investigation to assess and identify multilevel barriers and facilitators of initiating chemotherapy among patients with early-stage breast cancer. The purpose of this investigation was to garner a better understanding of the challenges patients experience as they navigate the process of initiating chemotherapy treatment, particularly those at an increased risk for experiencing delays, with the goal of reducing disparate health outcomes.
Materials and Methods
Study Design
Semi-structured, one-on-one interviews lasting approximately 60-minutes were conducted in-person or over the phone between the research coordinator and participants. Guided by extant literature and social determinants of health disparities in breast cancer,2,3,9 the semi-structured interview guide was developed and pilot tested by research team members with extensive qualitative experience. Interviews included a discussion of 1) attitudes and perceptions associated with chemotherapy and 2) barriers to initiation of chemotherapy (Appendix). Questions were designed to probe for the potential impact of issues at the medical, system, - and patient, levels. Compensation included a $50 gift card and parking voucher.
Participants
Female patients, English- or Spanish-speaking age ≥18, diagnosed with primary invasive breast cancer within three years of study enrollment were recruited (10/2019-10/2020) at a single academic cancer center. Patients received their first dose of adjuvant chemotherapy ≥60 days after definitive breast cancer surgery or ≥60 days after pathological diagnosis for participants treated with neoadjuvant chemotherapy. The timeframe of ≥60 days was chosen because this threshold has been shown to be related to adverse health outcomes.2–4
Participants were identified via chart review, and those meeting inclusion criteria were approached either in-person or by telephone. Detailed description of the study was provided, including a summary of the dissemination of their anonymized responses and participants signed an informed consent to participate. This study complied with the Declaration of Helsinki and was approved by the University of Texas MD Anderson Cancer Center Institutional Review Board (IRB Number: 2018-1133).
Data Collection
Sociodemographic characteristics and relevant clinical information were collected from the medical record. Health literacy, numeracy, physician trust, and social support were assessed using the 3-item-Brief Health Literacy Screener,10 3-item-Subjective Numeracy Scale,11 Interpersonal Trust in a Physician Scale,12 and the Berlin Social Support Subscale,13 respectively. Questions were administered electronically and recorded using REDCap.14 Survey items were presented visually on a tablet screen. During COVID-19 research restrictions, questions were read aloud to participants over the telephone. Audio recordings were transcribed verbatim by a professional transcription service. Professional translation services were used.
Data Analysis
Quantitative data were summarized using descriptive statistics. For the qualitative analysis, we partnered with ResearchTalk (http://www.researchtalk.com/), a leader in rigorous qualitative methodology and analysis, to use the Sort and Sift, Think and Shift analytic approach. This approach included a thorough examination of the data by advancing through “diving in” and “stepping back” iterative analytic phases.15–17 For the “diving in” phase, team members independently read four transcripts identifying powerful quotations to develop data summaries. Quotations were reviewed to create a list of core topics to monitor (coding) throughout the analysis of all project transcripts. This list featured deductive topics from the interview guide and inductive topics unearthed during the initial “diving in” phase. An episode profile (holistic depiction) was created for each transcript. Team members discussed and reviewed all transcripts and episode profiles, updating the core topics to monitor the list throughout analysis. During the “stepping back” phase, the team mined codes within the episode profiles revealing four realms, discussed in this paper, which threaded through each participant’s diagnosis and treatment journey. Data collection ended when no additional insights were identified, and repetition in the data started to occur, indicating an adequate sample size.18
Results
Participant Characteristics
We contacted 63 potentially eligible patients, of them, 22 agreed to participate (median age at diagnosis 53.5 years (range 27–70). Participants identified as: Hispanic/Latina (H/L; n=8); Black (B; n=5); and non-Latina White (NLW; n=9). Most completed interviews in English (n=15), and over half had lower educational attainment (n=12). Table 1 shows participant characteristics.
Table 1.
Sociodemographic Characteristics
| Participant Characteristics (N=22) | |
|---|---|
| Median (Range) | |
| Age at Diagnosis (years) | 53.5(27–70) |
| Chemotherapy Delay (days) | 83 (62–168) |
| N (%) | |
| Race/Ethnicity | |
| Non-Hispanic/Latina White (NHW) | 9 (40.9) |
| Latina (L) | 8 (36.4) |
| Black (B) | 5 (22.7) |
| Partner Status | |
| Partnered | 13 (59.1) |
| Not Partnered | 9 (40.9) |
| Education | |
| <Bachelors | 12 (54.5) |
| ≥Bachelors | 10 (45.5) |
| Monthly Income | |
| $0–$6000 | 14 (63.6) |
| >$6000 | 4 (18.2) |
| Prefer not to answer | 4 (18.2) |
| Health Literacy | |
| Adequate | 13 (59.1) |
| Inadequate | 9 (40.9) |
| Trust in Physician | |
| High Trust | 15 (68.2) |
| Neutral | 7 (31.8) |
| Low Trust | 0 |
| Social Support | |
| Adequate | 22 (100) |
| Inadequate | 0 |
Treatment Journey Through Cancer Care Experience
Interview analysis revealed a common four-stage journey through systemic treatment initiation across all participants: 1) Receiving diagnosis and treatment recommendations; 2) Processing treatment options; 3) “Flipping the Switch”; and 4) Activating treatment and engaging in care. Each journey was unique to the individual participant according to their needs to transition through the stages. The journey began when participants received systemic treatment recommendations. The second-stage, processing treatment options, is typically when the participant interacts with various “realms of support” to fulfill the necessary financial, emotional, logistical, and spiritual needs to achieve self-efficacy. “Flipping the Switch” is the third-stage derived from an in vivo quote coined by participant 13 as ” … the switch just went off, I was like okay, this is another thing I have to conquer” concerning her having obtained the necessary support and self-efficacy to initiate chemotherapy. Once support was established to meet individual needs, participants felt equipped to move towards the fourth- stage of activating treatment and engaging in continued care.
Realms of Support
“Flipping the Switch” appeared to be the most critical moment in the participants’ journey to initiate treatment. It is the centerpiece of our analysis reflecting the active decision of moving towards treatment initiation. This movement toward activation through the journey stages (Figure 1) was observed to occur multidimensionally across four “realms of support”: self, family, community, and medical. These realms organize the themes of our analysis and are informed by the socioecological framework to characterize key relationships that supported participants in their journeys.18,19 The various forms of support participants needed in order to achieve self-efficacy were derived from one or more “realms of support” — however, while some participants were able to readily identify their needs and establish support to continue their cancer care journey, not all participants were actively aware of the type of support they required.
Figure 1.
A four-stage journey toward treatment initiation.
To reflect the multidimensionality of our analysis, the realms below are described by incorporating participant quotes representing their movement through the treatment journey stages. The overarching themes identified from participant interviews include logistical, emotional, financial, and social support and their relationship to self-efficacy. Themes are situated within the realms to provide context and elucidate movement through the treatment journey. Additional participant quotes are included in Table 2.
Table 2.
Treatment Journey Stages and Realms of Support
| Journey Stage | Realm of Support | Direct Quote |
|---|---|---|
| Receiving Treatment Options | Self | … The whole process is scary, not understanding it; it’s a lot of going online reading about what … breast cancer is. What chemotherapy was like, and what that might look like. There were very few uplifting things about what you read; it’s all very medicinal … It did not do anything to diminish the unknown, and what the fear of all that would be like.(P20-NHW-52y) |
| Family | It was a complete imbalance in our lives, and as a marriage. Thanks to our family … that supported us and prayed for us, we were able to get through that.(P07-H/L-33y) | |
| Community | The source of information was my friends, and friends of friends … I contacted everyone I knew … so that I could talk to people who had been there-who had been through it … I only relied on people’s personal experiences, so friends, friends of friends and family members.(P01-NHW-46y) | |
| Medical | My oncologist went through it [chemo treatment plan] a couple times with me, and my nurse practitioner went through it with me as well. It was a lot of information taking in, but it was somewhat simple because they guided me through it.(P12-B-42y) | |
| Processing Treatment Options | Self | It was a little bit hard because they explain to you all the side effects that the treatment can have, but you know you have to do it in order to save your life, to get your health back … that was mostly it, the fear I had of the aggressiveness of chemotherapy. I was very scared I was not going to be able to put up with the treatments and that I was going to die, not because of the cancer but because of the chemotherapy.(P07-H/L-33y) |
| Family | … the doctor told me about the side effects, and she said, “Your hair is going to fall out, but don’t worry, it grows back.” That is what they said. I was thinking about the side effects, about my family. I did not want them to see me like that. I thought about my kids and the side effects.(P15-H/L-43y) | |
| Community | They [survivors] were a huge support, and it helped me greatly that they were there. They would say, “I went through this, I felt this, it is normal to feel this … ” They gave me all their experience so that it would be easier for me to deal with the chemotherapy.(P07-H/L-33y) | |
| Medical | … It was all overwhelming … Now if we move forward to [State Hospital] it was a completely different experience. It was much more organized, presented much more professionally, the presentation of the information left credibility to what they were telling me.(P20-NHW-52y) | |
| “Flipping the Switch” | Self | [I] started seeing God in everything and in everyone who surrounded me … I think God was everywhere, he still is. Seeing God changes everything, and I feel calm and have faith, peace, and I can move ahead.(P07-H/L-33y) |
| Family | I always got together with my sister or my husband and we decided that it was better for me to start with the chemotherapy.(P15-H/L-43y) | |
| Community | My friend kind of brought me down to, you got to think about it differently, is still kind of a choice sometime … She spoke me down enough to look at it in a different way.(P13-H/L-41y) | |
| Medical | Looking at my type of cancer … it was very aggressive, and so while I know natural remedies can work, they are normally not fast remedies. I was down, but not very long, I guess I saw it as a necessary treatment … the chemotherapy … they were recommending, historically has worked very well for the type of cancer that I have, so I just had to push through.(P12-B-42y) | |
| Activating Treatment & Engaging in Care | Self | It [chemo] is terrifying. But to me there was never a time when I said, “I’m not going to do it” because the fear of not doing it was greater than the fear of doing it. I was terrified, absolutely terrified … I was depressed, I was anxious all of the time, I cried a lot, I did not want to get out of bed, and I do not want to face the world or anyone at work. I did not want to do anything, but you have to. Well you do not have to, but for me I had to.(P01-NHW-46y) |
| Family | I was always with somebody when I was having chemotherapy … I went to the house of my husband’s mother, and she was always looking after me there. I always stayed there during the days in which I was going to experience the side effects, when I was in bed and with nausea, and she was always there with me.(P15-H/L-43yo) | |
| Community | When you see other people waiting … you have 10–15 other women going exactly thru the same thing, and we talk. We talk about it … and they will express their feelings. We might not remember our names, but when we are waiting we are a neat little group … (P02-NHW-66y) | |
| Medical | Had I not had insurance in place I may not have gone forward with it. That was another factor knowing that it was not going to be crazy expensive … so I think that make the process easier for me.(P13-H/L-41y) |
Self-Realm
The self-realm encompasses the participant’s relationship with herself as she adjusts to life with breast cancer and, ideally, moves toward acceptance and active involvement in her treatment. Movement through the treatment journey within the self-realm depended on the perception of needs and obtaining individual support to achieve self-efficacy. Participants commonly encountered shock, rejection, fear, and disbelief upon receiving chemotherapy recommendations. One participant retold her journey as “[having been] a weird experience. I kind of felt like it was not happening to me, and it was all a bad joke (Participant [P]-NHW-30 years[y])”. Emotional despair was tied to delay; for example, “If something could have been done to reduce the fear, it would have helped me in terms of reducing some of the time frame [to decision] (P20-NHW-52y).” Some women readily transitioned to processing the recommended treatment options through individual relationships with spirituality, closing gaps in knowledge, and logistical planning.
Family-Realm
This realm comprises relationships with all immediate and extended family members. Participants described how family relationships helped them move from the initial reaction to receiving treatment recommendations through processing towards treatment initiation, through the provision of spiritual, emotional, and logistical support. Activation of the family-realm was the starting point for building the necessary support network to overcome hesitation, disbelief, and/or denial and continue the treatment journey. The importance of this realm was particularly evident when a participant shared, ” … [My mom and my husband] were my second and third set of ears … we were all trying to process the information that we got that day together (P14-NHW-30y).”
Participants represented a broad range of age and family roles which were important factors to consider due to concerns of how chemotherapy would impact the family unit and not just themselves. This involved shared decision-making regarding logistical and emotional needs,
My husband and I were having discussions about starting a family around the time I was diagnosed, so I knew that I did not want to go forward with chemo, without pursuing [fertility preservation] first. (P14-NHW-30y)
For other participants, family provided a direct call to action to initiate treatment, ” … [I] got a big intervention … “Why would not I do it? … they brought up my kids, my kids [were] young at the time, “What are you going to do?” [they said] “They are still little; they need their mom (P13-H/L-41y).”
Community-Realm
The community-realm included relationships with friends, neighbors, church members, and other cancer patients/survivors, with whom the participants engaged and who were critical during the treatment journey. Participants described financial, emotional, and spiritual support from the community as crucial to “Flipping the Switch” and engaging in cancer care.
Financial support was critical when preparing for treatment, as one participant shared,
I was diagnosed, and we had no money for the extra costs for the disease. That is when the community people, the survivors … started to organize sales to get funds to help us with the gas, the food, the hotel …. (P07-H/L-33y)
Participants also described support from their church community, sharing,
We were able to find an apartment through a church group and … it was a lot cheaper than what you would find looking for yourself, so it was a huge help to us. (P01-NHW-46yo)
Emotional support was pivotal when processing diagnosis and treatment, as one participant stated,
I called my friend and then my husband … I pretty much called everybody who I was close to because I was terrified, and I wanted comfort and support. (P01-NHW-46y)
Prior to treatment, one participant shared the impact of meeting another person going through chemotherapy,
I think God put [cancer patient] in my way for one big reason, and it was so that I could start that treatment, and he taught me … He was a great support …. (P07-H/L-33y)
Moreover, participants described the importance of support from breast cancer patients and survivors,
one of my closest friends was diagnosed with breast cancer two weeks before I was … I could ask, ‘‘how was this’ [and] ‘tell me about that’, so that is kind of what I did. (P12-B-42y)
Medical-Realm
The medical-realm focused on relationships with medical team members. Communication with the medical team allowed participants to learn more about breast cancer, understand treatment pathways, and gain the necessary self-efficacy to “Flip the Switch.” Learning from the medical team was critical, as one participant described, “ … the most important thing would be communicating with your doctor and understanding every step of the process (P12-B-42y).” Participants shared the importance of seeking information, as one participant stated,
make sure you talk … with your doctors … talk to more than one doctor, talk to team members … talk to someone who can help you deal with your fears because fear is going to be there. (P01-NHW-46y)
Participants described how learning from their medical team helped them make sense of their treatment pathway, for example, “They [medical team] were very clear, they took the time to really explain everything. I had clear direction about side effects and everything (P21-B-65y).”
Discussion
Our study revealed that participants moved toward “Flipping the Switch” when they felt supported across multiple realms. Upon attaining key themes of support, participants exercised control over their care and actively participating in decision-making to initiate chemotherapy. Participants consistently described a process of identifying and seeking multiple forms of support to achieve a strong sense of self-efficacy that allowed a sense of control over their journey. This process was vital in achieving the self-efficacy needed to facilitate chemotherapy initiation. Studies show that self-efficacy is a compelling psychological strategy for patients to confront illness and its consequences,20 particularly, cancer.21,22 Our results support published literature, as achieving self-efficacy was a critical component for participants to navigate from receiving their initial systemic treatment recommendations to “Flipping the Switch” and initiating chemotherapy. The common journey among participants aligns with the decision-making process and behavior described in the Transtheoretical Model.23 The multidimensional relationship between the realms, achieving self-efficacy, “Flipping the Switch”, and initiation of cancer care revealed a complex interplay between social support and patient empowerment beyond medical care. The transition through the stages coincides with individual attainment of financial, emotional, spiritual, and logistical support. Despite all participants having expressed adequate social support via questionnaire, the delay period reflects the complexities of the cancer care journey and the need for additional support to adequately cope with cancer-related challenges and treatment initiation. Additionally, even if support was observed across the realms, unforeseen or additional medical concerns contributed to delay.
The notion of time and urgency was rarely evident in the interviews. Most participants focused more on their process to and through treatment despite targeted interview questions designed to assess delay. While most participants lacked clear insight into their delay, we observed that delay in initiating chemotherapy often aligned with unfulfilled support across four key themes: emotional, financial, logistical, and spiritual support, organized across four realms (ie, self, family, community, and medical) through the treatment pathway. These realms are consistent with various studies exploring support through the cancer care continuum.24,25
While the entirety of the cancer experience is anchored in the self-realm as participants navigate achieving self-efficacy, engagements across all realms are interlinked and contribute to optimal care. Studies have identified social support as key in decision-making and coping with cancer, with significant others, family, and community acting as sources of emotional, financial, logistical, and spiritual support.26–28 In our study, church and spirituality were strong sources of support throughout the entire journey. Spirituality provided a sense of comfort, coping, and support to fulfill emotional needs, while the church community provided emotional, but also financial and logistical support. The role of the church, spirituality, and community in the cancer care experience has been noted as a critical influence in the decision-making process, particularly among racial/ethnic minorities,29 and can serve as key instruments of support to reduce delay. Results of interventions aimed at exploring sources of support for breast cancer patients by partnering them with individuals who have dealt with similar illnesses coincide with our findings.30 Familial support in processing information and decision-making reflects the importance of social support alongside the medical-realm and may be particularly beneficial to the achievement of self-efficacy for participants with low health literacy.31
Participant interactions across the realms describe individual yet shared movement from cancer diagnosis to treatment, indicating that provision of support beyond the clinical setting is needed to empower women to “Flip the Switch”. To minimize delay in chemotherapy initiation, Srikanthan et al highlighted the importance of assisting with decision-making by providing standardized information,32 which we believe should coincide with streamlining ancillary services to coordinate care and improve outcomes. For example, decision-making regarding the impact of chemotherapy on fertility contributed to delay for some participants and required coordination of additional medical services. Much of the existing studies exploring self-efficacy within the context of cancer are limited to interventions once chemotherapy has already been initiated.33 Our results suggest that delays in chemotherapy initiation can be reduced by providing a structured system for patients to identify needs earlier in their cancer care journey and facilitate engagement with support systems appropriate to individual needs. Thus, we propose that interventions aimed at increasing patient self-efficacy as soon as patients receive diagnosis and treatment options can be beneficial. As a result, the facilitation of these interactions across the realms will empower patients to achieve to achieve self-efficacy, thus “Flipping the Switch”, and initiating treatment sooner rather than later.
Limitations
A limitation of our study is that participants were recruited from a large, academic cancer center which may limit generalizability. Despite this, approximately half of the participants identified as Black or Latina, roughly half reported less than a college degree, and about 40% had limited health literacy. While none of our participants reported distrust in their physician using the Trust in Physician Scale, this measure has demonstrated ceiling effects and may not adequately reflect the multiple constructs that contribute to trust.34 High social support observed in our participant sample may be indicate limitations of the measure used. Despite this, our research approach leveraged qualitative methodology to elucidate and capture the complexity of trust and social support. In addition, participants demonstrated limited insight into their delay. While discussed during their interview for this study, it is possible that delay was not discussed during their clinical care. Future work investigating clinical conversations regarding delay may be warranted.
Conclusion
Project Start findings demonstrate the importance of self, family, community, and medical realms to support navigation through the treatment decision-making process to chemotherapy initiation. Considering the complexities of breast cancer treatment, decreasing barriers is critical now more than ever due to unprecedented circumstances physicians and healthcare providers are experiencing. With increased challenges in cancer care delivery, additional research is needed to understand the holistic patient cancer care experience and facilitate patient engagement with support systems to mitigate treatment delays.
Acknowledgments
Findings from this manuscript were presented, in part, at the San Antonio Breast Cancer Symposium 2020.
Funding Statement
This research was supported by Conquer Cancer, The ASCO Foundation, BCRF and NIH/NCI P30CA016672. MCM is supported by Susan G. Komen SAC150061, CPRIT-RP160674. AJH is supported by R00MD011485. CM is supported by Susan G. Komen GTDR17498270 and the Duncan Family Institute.
Data Statement
The data that support the findings of this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy or ethical considerations.
Disclosure
The authors have no conflicts of interest to disclose in this work.
References
- 1.American Cancer Society. Breast Cancer Facts & Figures 2019–2020. Atlanta: American Cancer Society, Inc;2019. [Google Scholar]
- 2.de Melo Gagliato D, Lei X, Giordano SH, et al. Impact of delayed neoadjuvant systemic chemotherapy on overall survival among patients with breast cancer. Oncologist. 2020;25(9):749–757. doi: 10.1634/theoncologist.2019-0744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH. Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol. 2016;2(3):322–329. doi: 10.1001/jamaoncol.2015.3856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Melo Gagliato D, Gonzalez-Angulo AM, Lei X, et al. Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol. 2014;32(8):735–744. doi: 10.1200/JCO.2013.49.7693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet. 1999;353(9159):1119–1126. doi: 10.1016/S0140-6736(99)02143-1 [DOI] [PubMed] [Google Scholar]
- 6.Fedewa SA, Edge SB, Stewart AK, Halpern MT, Marlow NM, Ward EM. Race and ethnicity are associated with delays in breast cancer treatment (2003-2006). J Health Care Poor Underserved. 2011;22(1):128–141. doi: 10.1353/hpu.2011.0006 [DOI] [PubMed] [Google Scholar]
- 7.Sudore RL, Mehta KM, Simonsick EM, et al. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54(5):770–776. doi: 10.1111/j.1532-5415.2006.00691.x [DOI] [PubMed] [Google Scholar]
- 8.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54(2):78–93. doi: 10.3322/canjclin.54.2.78 [DOI] [PubMed] [Google Scholar]
- 9.Gerend MA, Pai M. Social determinants of Black-White disparities in breast cancer mortality: a review. Cancer Epidemiol Biomark Prev. 2008;17(11):2913–2923. doi: 10.1158/1055-9965.EPI-07-0633 [DOI] [PubMed] [Google Scholar]
- 10.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 11.McNaughton CD, Cavanaugh KL, Kripalani S, Rothman RL, Wallston KA. Validation of a short, 3-item version of the subjective numeracy scale. Med Decis Making. 2015;35(8):932–936. doi: 10.1177/0272989X15581800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37(5):1419–1439. doi: 10.1111/1475-6773.01070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulz U, Schwarzer R. Soziale Unterstützung bei der Krankheitsbewältigung: die Berliner Social Support Skalen (BSSS). [Social Support in Coping with Illness: the Berlin Social Support Scales (BSSS).]. Diagnostica. 2003;49(2):73–82. doi: 10.1026//0012-1924.49.2.73 [DOI] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fryer CS, Passmore SR, Maietta RC, et al. The symbolic value and limitations of racial concordance in minority research engagement. Qual Health Res. 2016;26(6):830–841. doi: 10.1177/1049732315575708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maietta R, Mihas P, Swartout K, Petruzzelli J, Hamilton AB. Sort and sift, think and shift: let the data be your guide an applied approach to working with, learning from, and privileging qualitative data. Qual Rep. 2021;26(6):16. [Google Scholar]
- 17.Maietta RC. State of the Art: integrating Software with Qualitative Analysis. In: Curry L, Shield R, Wetle T, editors. Applying Qualitative and Mixed Methods in Aging and Public Health Research. American Public Health Association and the Gerontological Society of America; 2006. [Google Scholar]
- 18.Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. 2021;292. 114523. [DOI] [PubMed] [Google Scholar]
- 19.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513. doi: 10.1037/0003-066X.32.7.513 [DOI] [Google Scholar]
- 20.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 21.Chirico A, Lucidi F, Merluzzi T, et al. A meta-analytic review of the relationship of cancer coping self-efficacy with distress and quality of life. Oncotarget. 2017;8(22):36800. doi: 10.18632/oncotarget.15758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.BorjAlilu S, Kaviani A, Helmi S, Karbakhsh M, Mazaheri MA. Exploring the role of self-efficacy for coping with breast cancer: a systematic review. Archives Breast Cancer. 2017;4. 42–57. [Google Scholar]
- 23.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38 [DOI] [PubMed] [Google Scholar]
- 24.Foster C, Breckons M, Cotterell P, et al. Cancer survivors’ self-efficacy to self-manage in the year following primary treatment. J Cancer Surviv. 2015;9(1):11–19. doi: 10.1007/s11764-014-0384-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelly EP, Meara A, Hyer M, Payne N, Pawlik TM. Understanding the type of support offered within the caregiver, family, and spiritual/religious contexts of cancer patients. J Pain Symptom Manage. 2019;58(1):56–64. doi: 10.1016/j.jpainsymman.2019.03.003 [DOI] [PubMed] [Google Scholar]
- 26.Adam A, Koranteng F, Galli A. Availability, accessibility, and impact of social support on breast cancer treatment among breast cancer patients in Kumasi, Ghana: a qualitative study. PLoS One. 2020;15(4):e0231691. doi: 10.1371/journal.pone.0231691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bluman LG, Rimer BK, Berry DA, et al. Attitudes, knowledge, and risk perceptions of women with breast and/or ovarian cancer considering testing for BRCA1 and BRCA2. J Clin Oncol. 1999;17(3):1040. doi: 10.1200/JCO.1999.17.3.1040 [DOI] [PubMed] [Google Scholar]
- 28.Stiggelbout A, Jansen S, Otten W, Baas-Thijssen M, Van Slooten H, Van de Velde C. How important is the opinion of significant others to cancer patients’ adjuvant chemotherapy decision-making? Support Care Cancer. 2007;15(3):319–325. doi: 10.1007/s00520-006-0149-z [DOI] [PubMed] [Google Scholar]
- 29.Johnson KS, Elbert‐Avila KI, Tulsky JA. The influence of spiritual beliefs and practices on the treatment preferences of African Americans: a review of the literature. J Am Geriatr Soc. 2005;53(4):711–719. doi: 10.1111/j.1532-5415.2005.53224.x [DOI] [PubMed] [Google Scholar]
- 30.Snyder KA, Pearse W. Crisis, social support, and the family response: exploring the narratives of young breast cancer survivors. J Psychosoc Oncol. 2010;28(4):413–431. doi: 10.1080/07347332.2010.484830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Von Wagner C, Semmler C, Good A, Wardle J. Health literacy and self-efficacy for participating in colorectal cancer screening: the role of information processing. Patient Educ Couns. 2009;75(3):352–357. doi: 10.1016/j.pec.2009.03.015 [DOI] [PubMed] [Google Scholar]
- 32.Srikanthan A, Amir E, Gupta A, Baxter N, Kennedy ED. Assisting with decision-making: how standardized information impacts breast cancer patient decisions regarding fertility trade-offs and chemotherapy. J Adolesc Young Adult Oncol. 2019;8(6):660–667. doi: 10.1089/jayao.2019.0027 [DOI] [PubMed] [Google Scholar]
- 33.Lu J, Zeng X, Liao J, et al. Effectiveness of an intervention to promote self-efficacy on quality of life of patients with nasopharyngeal carcinoma of the Zhuang tribe minority in Guangxi, China: a prospective study. Med Sci Monit. 2017;23:4077. doi: 10.12659/MSM.903205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Müller E, Zill JM, Dirmaier J, Härter M, Scholl I, Gupta V. Assessment of trust in physician: a systematic review of measures. PLoS One. 2014;9(9):e106844. doi: 10.1371/journal.pone.0106844 [DOI] [PMC free article] [PubMed] [Google Scholar]