Abstract
The coronavirus pandemic has crippled healthcare system since its outbreak in 2020, and has led to over 2.6 million deaths worldwide. Clinical manifestations of COVID-19 range from asymptomatic carrier to severe pneumonia, to life-threatening acute respiratory distress syndrome (ARDS). The early efforts of the pandemic surrounded treating the pulmonary component of COVID-19, however, there has been robust data surrounding the cardiac complications associated with the virus. This is suspected to be from a marked inflammatory response as well as direct viral injury. Arrhythmias, acute myocardial injury, myocarditis, cardiomyopathy, thrombosis, and myocardial fibrosis are some of the observed cardiac complications. There have been high morbidity and mortality rates in those affected by cardiac conditions associated with COVID-19. Additionally, there have been documented cases of patients presenting with typical cardiac symptoms who are subsequently discovered to have COVID-19 infection. In those who test positive for COVID-19, clinical awareness of the significant cardiac components of the virus is pertinent to prevent morbidity and mortality. Unfortunately, treatment and preventative measures developed for COVID-19 have been shown to be also be associated with cardiac complications. This is a comprehensive review of the cardiac complications and manifestations of COVID-19 infection in addition to those associated with both treatment and vaccination.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-COVID-2) has wreaked havoc as the deadly virus behind the COVID-19 pandemic. Over 78 million cases have been recorded in the United States with an observed 1.2% mortality rate per the analysis conducted by John Hopkins Center for System Science and Engineering.1 While the disease is often discussed in a pulmonary context, patients present and develop a variety of cardiac complications as well.2 Approximately 20%-30% of hospitalized COVID-19 patients have biochemical evidence of myocardial involvement evidenced by elevated troponin.3 Cardiac injury results from mainly COVID viral systemic effects along with direct viral cytotoxicity. The severity of illness is correlated to patients' baseline comorbidities including advanced age, diabetes, hypertension, obesity, and immunocompromised status4. With greater severity of illness comes a higher likelihood of cardiac injury, and thus more serious cardiac complications ranging from arrhythmias to myocarditis, new-onset cardiomyopathy, myocardial infarction (MI), and thromboembolism. Reported to have a cumulative incidence of 20%-40%, these cardiac presentations convey a significantly increased morbidity and mortality when associated with COVID-195. COVID-19 treatments and vaccines also have distinct cardiac side-effect profiles with many still under investigation. These, along with the infection process itself, can have long-lasting consequences on health. We aim to provide a comprehensive up to date review of the cardiac manifestations of COVID-19 infection, along with those associated with its treatment and vaccination.
Pathophysiology
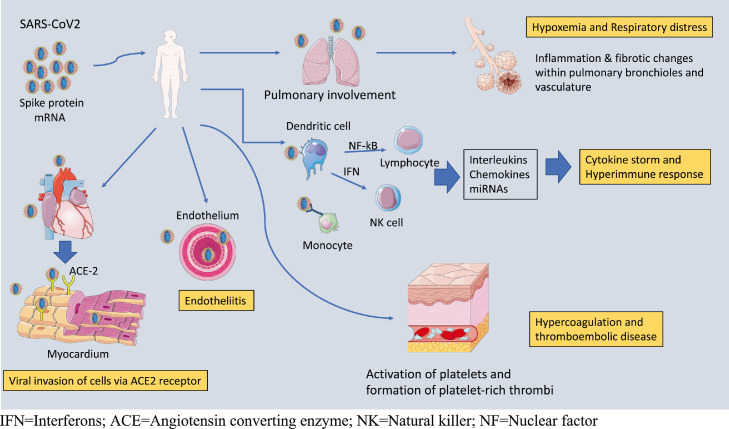
In patients with COVID-19 infection, cardiac involvement can occur indirectly or directly. There are several different mechanisms for indirect cardiac injury. Severe cases of COVID have noted a marked elevation of inflammatory cytokines and markers which may be related to viral-induced disturbances in non-coding RNAs.6 The resulting inefficient and uncontrolled systemic inflammation and cytokine storm, occurring through a hyperimmune response with inappropriate T-cell activation and markedly elevated catecholamines, can trigger arrhythmias, cardiomyopathies, plaque destabilization, and myocardial injury among other cardiac pathology.7 , 8 Along with these pro-inflammatory mediators, COVID also increases the risk for thromboembolic disease through a phenomenon of sepsis-induced coagulopathy (SIC).9 SIC is a result of the heightened immune response via cytokine storm, overstimulation of the sympathetic nervous system, and microvascular dysfunction which contribute to hypercoagulability.10 Another indirect cardiac complication includes hypoxia-driven myocardial supply-demand mismatch which results in oxidative stress on the myocardium.11
In addition to indirect mechanisms of cardiac injury, direct cardiac injury is suspected to be from entry of the virus into cardiac cells leading to endothelial disruption.12 In fact, in situ labeling of viral RNA and electron microscopy has detected viral tropism for cardiac myocytes.13 Further research and analysis led to the discovery of the interaction between viral spike protein and target cell angiotensin-converting enzyme 2 (ACE2) receptor facilitating membrane fusion.14 ACE2 receptors are found on cells of the heart, lungs, kidneys, and intestines, thereby creating a mechanism for damage of these vital organs.15 Among the highest risk factors for severe COVID-19 infection, heart disease and hypertension are thought to impart a worsened prognosis partially due to the upregulation of ACE2 found in these conditions.16 , 17
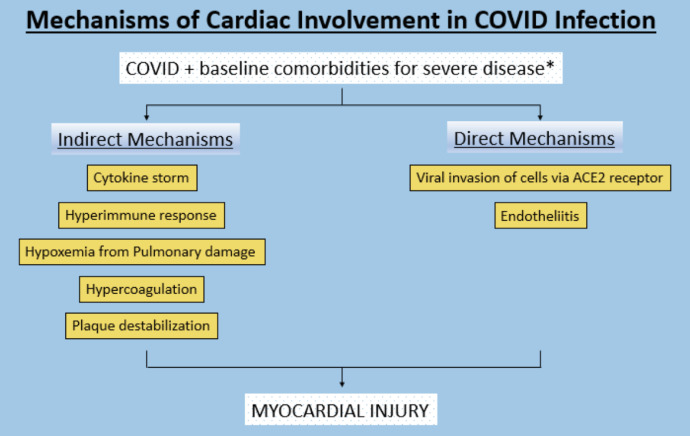
In those patients presenting with cardiac symptoms, the consequence of viral damage on myocardium has conflicting evidence. A recent analysis of intubated patients suggested that myocardial injury in COVID-related ARDS was predominantly a result of critical systemic illness and multiorgan dysfunction in the setting of advanced age and baseline comorbidities.18 Supporting evidence for this was shown in a meta-analysis from China which found that patients with cardiovascular (CV) comorbidities including hypertension and diabetes were much more likely to develop severe disease and require intensive care unit (ICU) level of care.19 They further observed that the incidence of acute cardiac injury was 13 times greater in these patients compared to those not requiring ICU care. Nevertheless, histopathological analysis has increasingly demonstrated viral invasion of endothelial tissue resulting in a COVID-19 endotheliitis with subsequent inflammation, hypoxia, and organ dysfunction.20 In light of this, a direct mechanism for cardiac injury cannot be dismissed; although the degree of influence in the overall clinical progression is still to be elucidated. The various mechanisms of cardiac involvement are summarized in Figure 1 -2 .
FIG 1.
Mechanisms of Cardiac Involvement in COVID Infection (Color version of figure is available online.)
FIG 2.
Pathophysiologic Mechanisms of Cardiac Involvement in COVID Infection (Color version of figure is available online.)
Cardiac Manifestations of COVID-19
Arrhythmias
Arrhythmias result from abnormal signaling in the setting of systemic stress or from intrinsic cardiac electrical dysregulation. Systemic stress, such as with infection, influences autonomic output to the sinoatrial and atrioventricular nodes. This cardiac electrical network can also be affected by myocardial damage and hypoxia leading to electrolyte imbalances and abnormal depolarizations. Arrhythmias in association with COVID have been found to occur in up to 10%-30% of hospitalized patients and 30%-50% of ICU patients.21 Arrhythmias alone convey significant morbidity and mortality in these patients. They are independently associated with prolonged hospitalization and duration of mechanical ventilation.21 , 22 Those with advanced age and baseline cardiac comorbidities were more prone to developing arrhythmias in the setting of COVID-19.23
Atrial arrhythmias have the highest incidence of about 60%-80% and present secondary to increased sympathetic output in the setting of infection and systemic inflammation with COVID.24 Of these arrhythmias, sinus tachycardia is most frequent followed by atrial fibrillation (AF).25 , 26 An observational study in hospitalized patients noted the incidence of AF to be directly related to the rate of myocardial injury.27 A multinational retrospective analysis of patients in early 2020 showed an increased incidence of AF associated with COVID in North America, South America, and Europe as compared to Asia, which correlated with a higher rate of comorbidities such as diabetes, hypertension, obesity, and overall CV disease in those continents28. Patients in Asia instead had a higher burden of bradyarrhythmia or AV block. In that analysis, ventricular arrhythmias defined as non-sustained ventricular tachycardia (NSVT), ventricular tachycardia (VT), or ventricular fibrillation (VF), were found to occur about 20% of the time. Interestingly, ventricular arrhythmias are rarely present at the time of death as compared to severe bradycardia or pulseless electrical activity (PEA).29 This is suggestive of severe hypoxia and critical illness being the main drivers of cardiac arrest. A multinational analysis of hospitalized COVID patients showed a pooled prevalence of ventricular arrhythmia to be 5% in the perimortem time.30 Although less frequent when present, ventricular arrhythmias significantly contributed to an increased risk of death in those patients.31 , 32
Myocardial Damage
Myocardial injury depicted via troponin elevation is a poor prognostic indicator in patients with COVID-19.33 A retrospective study of 559 patients evaluated troponin levels as a means of prognostication in COVID-19 patients. On admission, 57% of the patients had an elevated troponin level which correlated with a higher rate of ventilatory support and death (HR 1.96, 95% CI 1.15-3.37).34 Although the etiologies related to troponin elevation in these patients can extend beyond primary cardiac pathology this review will focus on primary cardiac complications surrounding myocardial damage.35
Myocarditis is caused by inflammation of the myocardium. Historically, viral infections are one of the most common causes of myocarditis.36 Myocarditis can be devastating and result in disturbances of both the electrical system and pumping function of the heart.36 , 37 Additionally, myocarditis is an established risk factor associated with increased mortality rates in patients with COVID-19 infections.38 Severe COVID-19 infections lead to a hyperinflammatory state with subsequent cytokine storm resulting in myocarditis.39 After the initial direct attack on cardiac cells through the ACE2 receptor, a subsequent secondary inflammatory response occurs augmenting cardiac injury.40 Autopsy of COVID-19 patients confirmed the presence of mononuclear cells within the myocardium and associated myocyte necrosis. Diagnosis of myocarditis can be challenging in patients presenting with acute coronary syndromes (ACS). Differentiating features are usually associated with echocardiographic evidence of global hypokinesis rather than focal wall motion abnormalities seen in ACS.41
Cardiac magnetic resonance imaging (cMRI) is the gold standard imaging modality for diagnosing myocarditis and is useful in differentiating myocarditis from other etiologies of acute chest pain.41 In those with severe COVID-19 infection, obtaining a definitive diagnosis via cMRI may not be plausible and thus the true prevalence of COVID-19 associated myocarditis is likely underestimated.42 Studies of myocardial damage in COVID-19 patients can be found in Table 1 .
TABLE 1.
Summary of studies evaluating myocardial injury, coronary ischemia, and cardiomyopathy in COVID-19 patients
| Author | Year | Study type & patients included | Measures | Outcomes/Findings |
|---|---|---|---|---|
| Buckley BJR et al.36 | November 2021 | Retrospective cohort study of 718,365 patients who tested positive for COVID | Incidence of myocarditis/pericarditis; all‐cause mortality, hospitalization, cardiac arrest, incident HF, incident AF, and acute MI in patients with & without myocarditis/pericarditis | 5% developed new myocarditis, 1.5% developed new pericarditis; increased mortality in patients with myocarditis or pericarditis compared to controls; patients with pericarditis had more CV sequalae compared to myocarditis |
| Efros O et al.34 | February 2021 | Retrospective cohort study conducted in Israel of 559 patients who tested positive for COVID | Characteristics between patients with troponin elevation vs no elevation; mortality, invasive ventilatory support, hospital stay, and acute kidney injury | Increased mortality, invasive ventilation, hospital stay and acute kidney injury significantly higher in patients with elevated troponin; predictors of elevated troponin included age, female, high Cr |
| Choudry FA et al.49 | Sept 2020 | Single-center, observational study of 115 consecutive patients admitted with confirmed STEMI | COVID vs non-COVID outcomes, comparison of bloodwork analysis; thrombus burden, Thrombolysis in Myocardial Infarction (TIMI) flow, length of hospitalization, and need for ICU admission | Patients with STEMI and COVID infection had higher levels of troponin, d-dimer, and CRP; higher rates of multivessel thrombosis and stent thrombosis; longer hospital stays and more frequent admission to ICU |
| Saad M et al.50 | October 2021 | Retrospective cohort study of 80,449 adult patients admitted with out-of-hospital or in-hospital STEMI at 509 different centers | Comparison of in-hospital mortality between COVID and non-COVID patients | Patients with diagnosis of COVID had significantly higher rates of in-hospital mortality compared with patients without COVID |
| Jabri A et al.60 | July 2020 | Retrospective cohort study of 1914 patients presenting with acute coronary syndrome who underwent angiography during COVID pandemic | Incidence of stress-induced cardiomyopathy during COVID pandemic compared with prior to COVID pandemic | Incidence of stress cardiomyopathy during COVID pandemic was significantly higher at 7.8% compared with pre-pandemic incidences of 1.5%-1.5% |
| Dweck MR et al.62 | Sept 2020 | Prospective international survey study of 1216 patients with COVID from 69 different countries | Patient characteristics, indications for echo, echocardiographic findings, and impact of echocardiography on next management | 55% of patients had abnormal echo, 15% with severe cardiac disease; in patients with no pre-existing cardiac disease (901), 46% had abnormal findings with 13% having severe disease |
STEMI, ST-segment elevation myocardial infarction, CRP, C-Reactive Protein; ICU, Intensive care unit; CV, Cardiovascular; MI, Myocardial infarction.
Coronary Ischemia
Myocardial injury is defined by the Fourth Universal Definition of MI as an elevation of troponin concentration above the 99th percentile of the upper reference limit.10.13 , 43 Myocardial injury associated with COVID-19 has been described in many clinical scenarios including acute plaque rupture, thrombosis due to hypercoagulable state, and supply and demand mismatch leading to Type II myocardial injury.13 Demand mismatch could be observed in a variety of settings including hypoxia from severe lung pathology, fever or tachycardia due to sepsis, or declining cardiac function.40 Other clinical presentations with troponin elevations include stress-induced cardiomyopathy and myocarditis.13 , 44 Diverse pathologies can lead to troponin elevation; hence, it is important to distinguish between ACS and other etiologies to ensure appropriate treatment.
In the setting of acute plaque rupture during COVID-19 infection, the mechanism is thought to be from virus-induced stress response. This is particularly noted in later stages of severe COVID-19 infection by endothelial and hemostat.13 , 45 Additionally, the virus can directly cause plaque instability and rupture through the ACE2 receptor expressed on vascular endothelial.46
Percutaneous coronary intervention remains the mainstay for treatment of ST-elevation myocardial infarction (STEMI) regardless of COVID-19 status.47 Fibrinolytic therapy should be restricted to patients with severe bilateral COVID-19 pneumonia, ARDS, or overall poor prognosis who otherwise would not survive invasive intervention.48 In those who present with non-ST elevation MI (NSTEMI), clinical decision-making in the setting of COVID-19 remains cumbersome.13 , 47 If the clinical scenario is difficult to distinguish between plaque instability vs demand mismatch, it is reasonable to initiate medical therapy and further diagnostic testing with echocardiogram and coronary CT angiogram, and risk stratification further aiding in the decision to pursue early invasive treatment strategy.13 , 48
Biochemical findings suggestive of myocardial injury lend themselves to a poor prognostic indicator. A retrospective study of 115 patients compared patients presenting with STEMI with and without concomitant COVID-19 infection.49 Results were significant for higher rates of multivessel thrombosis, in-stent thrombosis, and higher doses of heparin required to reach therapeutic levels in those with COVID-19 infection. These factors contributed to longer hospitalizations and increased morbidity and mortality. Interestingly, aside from increased troponin and D-dimer levels, the remaining laboratory findings were similar between patients who tested positive for COVID and those who tested negative.49 A retrospective study of over 80,000 patients compared out-of-hospital or in-hospital STEMI in patients with and without COVID-19.50 Results were significant for increased in-hospital mortality in patients with a concomitant diagnosis of COVID-19 compared to patients without COVID-19. This large retrospective study highlights the impact COVID-19 has on mortality from ACS. Table 1 summaries clinical trials addressing coronary ischemia in COVID-19 patients.
Cardiomyopathy
Cardiomyopathy and heart failure have been well-described CV complications in the setting of COVID-19. New-onset heart failure has been detected in as many as 25% of patients hospitalized with COVID-19, and up to 33% in critically ill patients.51 The clinical presentation can vary from compensated heart failure syndrome to cardiogenic shock.52 Etiologies include primary cardiomyopathies, stress-induced cardiomyopathies, and myocarditis resulting in cardiac dysfunction.13 , 51 The pathophysiology is thought to be from indirect myocardial injury predisposing patients to new-onset cardiomyopathy or worsening of pre-existing LV dysfunction.13 , 53
Acute lung injury and ARDS increase the afterload of the right ventricle (RV) leading to right heart strain. Eventually, RV dilatation and dysfunction can occur leading to right heart failure. Those who are intubated are initiated on a lung-protective strategy consisting of high positive end-expiratory pressure (PEEP) and low tidal volume. PEEP increases RV afterload leading to a decreased left ventricular (LV) preload while ultimately causing a decrease in cardiac output.54 The RV is particularly susceptible to changes in afterload. Small changes in pulmonary vascular resistance, especially acutely, as seen in ARDS can lead to reduced RV contractility and ultimately cardiac output.55 The aforementioned factors associated with the treatment of ARDS increase the work of the heart augmenting patients' clinical deterioration.56
A retrospective study of 191 patients with COVID-19 had a reported incidence of heart failure in 23% of patients with a mortality rate of 52% of patients with diagnosed heart failure.36 Interestingly, another retrospective study of 113 deceased patients showed that aside from ARDS and sepsis, heart failure was the second most common complication with an estimated mortality of 49%.57 Many patients who develop cardiogenic shock in the setting of COVID-19 have a high mortality rate despite maximal medical therapies. A case series in China reported an 83% mortality rate despite management with extra-corporeal membrane oxygenation ECMO.58
Takotsubo or stress-induced cardiomyopathy (SIC) is characterized by transient reduction in LV function with associated apical ballooning.59 There has been an elevated incidence of patients presenting with ACS ultimately diagnosed with SIC during the COVID-19 pandemic (7.75% during pandemic vs 1.5%-1.8% pre-pandemic), signifying an increased stress burden in the general population supporting the significant psychosocial impact of the COVID pandemic.60 Similarly, there has been a positive correlation between increased incidence of SIC in patients with COVID-19 infection, presumably from an increased catecholamine state.10 , 61 A study evaluating the incidence of SIC in COVID-19 included 1200 patients and reported 2% of the patients had concomitant SIC diagnosed by echocardiogram.62 Another study with 118 patients showed that 4.2% of patients with COVID-19 had imaging evidence consistent with SIC.10 , 63 Both studies proved SIC to have a higher incidence in COVID-19 patients than the general population.62 , 63 Treatment of SIC in COVID-19 patients mirrors the mainstay treatment for SIC with beta-blockers, ACE inhibitors or angiotensin receptor blockers. Clinical trials evaluating cardiomyopathy can be found in Table 1 .
Thrombosis
An increased risk of thromboembolic events has been reported with COVID infection.64 , 65 Briefly analyzing this in the context of Virchow's triad can help to explain the pathophysiology and identify potential treatment strategies. Severe hypoxia increases blood viscosity thus contributing to stasis and hypercoagulability. The cytokine storm and hyperimmune-related dysfunction trigger endothelial and platelet activation and dysfunction. These effects are potentiated in the setting of CV comorbidities. Despite this, acute arterial thrombotic events including stroke and ACS have been described in patients with no such comorbidities.20
A study of 3300 patients hospitalized for COVID pneumonia in the New York health system during initial peak pandemic times found that over 16% experienced a thrombotic event in the form of deep venous thrombosis (DVT), pulmonary embolism (PE), MI or stroke, which was much greater compared to the 5.9% associated with the influenza pandemic of 2009.66 Studies evaluating patients admitted to the ICU have reported up to a 30% incidence of thromboembolic events.67 Furthermore, the rate of these events was found to be greater in COVID ARDS patients as compared to non-COVID ARDS patients even after correction for confounding comorbidities.68 , 69 A small review evaluating COVID patients diagnosed with LV thrombus found that up to 20% of patients had no baseline comorbidities further underscoring the increased rate of thromboembolic complications associated with COVID infection.70 An autopsy series of COVID-19 patients showed an extensive presence of platelet-rich thrombi in the pulmonary, hepatic, renal, and cardiac microvasculature.71 Interestingly, there was an increased concentration of megakaryocytes predominantly in vascular beds of the pulmonary and cardiac systems despite patients receiving full anticoagulation. Consistent with this, a retrospective study of patients with severe COVID found a high rate of thromboembolic complications despite the use of therapeutic anticoagulation.72
Elevated concentrations of d-dimer and fibrin degradation products have been noted in COVID infection and are associated with poor prognosis.73 , 74 This has spurred an investigation into the use of therapeutic anticoagulation based on d-dimer levels. More recently in the Hep-COVID trial, therapeutic Lovenox was found to decrease the composite outcome of major thromboembolic events and death in hospitalized patients with mild to moderate COVID with very elevated D-dimer levels.75 A similar benefit was not seen in ICU patients. Although this was a small study, it shows promise for a disease-modifying treatment. This imparts an increased risk of bleeding with reports of fatal hemorrhagic events including retroperitoneal and intracranial bleeds in the setting of therapeutic anticoagulation in COVID patients.76 , 77 Prophylaxis, at the very least, is strongly recommended for all patients admitted with COVID-19 infection using low molecular heparin as the preferred option unless contraindicated.
Thrombotic events described in the setting of COVID are likely multifactorial. precipitated from endothelial dysfunction with resultant activation of platelets, recruitment of leukocytes and hyperinflammatory reaction.78, 79, 80 Additionally, patients are typically immobile leading to increased stasis and subsequent hypercoagulable state.81 Table 2 summaries studies evaluating thrombosis in COVID-19.
TABLE 2.
Summary of studies evaluating thrombosis in COVID-19 patients
| Author | Year | Study type & patients included | Measures | Outcomes/Findings |
|---|---|---|---|---|
| Bilaloglu S et al.66 | July 2020 | Retrospective analysis of 3334 patients >18yrs old admitted to NYU Langhorne hospital (ICU and non-ICU) for SARS-COVID | Risk factors for thromboembolism, thromboembolism event rate, all-cause mortality | Prior MI, CAD, and high D-dimer levels were associated with thrombotic event which occurred in 16% of patients; all-cause mortality was higher in those with thrombotic events |
| Klok FA et al.67 | April 2020 | Retrospective analysis of 184 patients admitted to ICU in Netherlands for SARS-COVID | Composite outcome and event rate of venous and arterial thromboembolic events | 31% of patients experienced thromboembolic event; pulmonary embolism was most frequent |
| Lu YF et al.69 | August 2020 | Meta-analysis of 25 observational studies on VTE (PE, DVT) incidence & therapeutic anticoagulation | Pooled incidence of VTE and relationship between therapeutic anticoagulation and mortality | Rates of VTE were >20%, higher among ICU patients; therapeutic anticoagulation not associated with decreased mortality |
| Llitjos JF et al.72 | May 2020 | Retrospective study of 26 consecutive ICU patients with COVID-19 screened for VTE | Incidence of VTE among patients on prophylactic vs therapeutic anticoagulation | Patients on prophylactic anticoagulation had higher incidence of VTE |
| Rapkiewicz et al.71 | June 2020 | Autopsy series including 7 patients who died from COVID-19 | Histopathological changes of lung, heart, kidneys, liver | Plentiful platelet-rich thrombi and megakaryocytes in all tissues even in patients with full anticoagulation |
| Spyropoulos et al.75 | October 2021 | Randomized clinical trial of 253 patients hospitalized for COVID-19 with D-dimer levels >4x normal or SIC >4 | Arterial or venous thromboembolism, death, bleeding with prophylactic vs therapeutic anticoagulation | Therapeutic LMWH reduced thromboembolic events and death compared to standard prophylaxis in patients not in ICU with high D-dimer levels (P = .004) |
ICU, Intensive care unit; MI, Myocardial infarction; CAD, Coronary artery disease; VTE, Venous thromboembolism; LMWH, Low molecular weight heparin; SIC, sepsis-induced coagulopathy score.
Myocardial Fibrosis
It has been reported that both asymptomatic and symptomatic patients can develop myocardial fibrosis in the setting of COVID infection. The pathophysiology is theorized to be from fibroblastic deposition with the myocardium, replacing the damaged myocytes. Additional mechanisms of action include a hyperinflammatory response leading to immune cell deposition within the myocardium and activation of myofibroblasts leading to fibrosis.82
Two case reports have demonstrated diffuse interstitial fibrosis in patients who reported no previous history of myocarditis with COVID and presented 3-6 months later with cardiac symptoms.83 , 84 Another study of 26 patients who had recovered from COVID demonstrated that 7 were found to have cardiac MRI findings consistent with fibrosis after developing cardiac symptoms.85 Another study evaluated 14 deceased COVID patients and found 6 of these patients had focal myocardial fibrosis. It was realized that all 6 patients had a history of MI however.79 Overall, there appears to be a connection between COVID and the development of cardiac fibrosis through the aforementioned mechanisms; however, it is difficult to establish a definitive timeline on the development of fibrosis as a result of COVID infection.
Cardiovascular Effects from Treatment/Prevention Modalities
With the acute and novel nature of the COVID-19 pandemic, a variety of medications have been trialed in search of an adequate treatment and prevention strategy. Most of the treatment modalities are medication-based and unfortunately, only a few have been shown to actually improve the clinical course. Although potentially beneficial, many of these medications have serious side-effect profiles. Summary of cardiovascular effects of COVID-19 treatment modalities can be found in Table 3 .
TABLE 3.
Cardiovascular effects associated with COVID-19 Treatment Modalities
| Drug | Mechanism of action in COVID | CV Adverse Effects |
|---|---|---|
| Hydroxychloroquine/Chloroquine | Interference in endocytic pathway Prevention of cytokine storm Prevention of pH-mediated spike protein cleavage at ACE-2R |
QT-prolongation, ventricular tachycardia, cardiac arrest |
| Remdesivir | Inhibition of viral replication, increased clearance | QTc-prolongation, bradycardia, heart block |
| Dexamethasone | Glucocorticoid-mediated anti-inflammatory effects | Heart failure exacerbation, arrythmias, electrolyte imbalance |
| Tocilizumab | Anti-inflammatory via IL-6 inhibition | QTc-prolongation |
| Baricitinib | Anti-inflammatory via JAK pathway inhibition | Arterial and venous thromboembolism |
| Nirmatrelvir and ritonavir (Paxlovid) | Anti-inflammatory via protease inhibition | Hypertension, cytochrome P450 3A4 inhibition |
| Molnuparivir | Direct-acting antiviral | Minimal |
| mRNA vaccines | mRNA encoding for viral spike protein | Myocarditis, pericarditis, POTS |
CV, Cardiovascular; ACE, Angiotensin converting enzyme; RNA, Ribonucleic acid; POTS, Postural orthostatic tachycardia syndrome.
Hydroxychloroquine/chloroquine and Azithromycin
Hydroxychloroquine and chloroquine are a mainstay for the treatment of malarial and rheumatologic diseases. Alongside azithromycin, they became a popular choice for the treatment of COVID-19 early in the pandemic due to the intrinsic antiviral and anti-inflammatory properties in conjunction with the promising results of in vitro experimentation.86, 87, 88 Despite this, high-quality evidence supporting clinical utility is sparse with more and more studies showing little efficacy.89, 90, 91 Furthermore, there may be an added harm associated with hydroxychloroquine-induced QT-prolongation and resultant arrhythmias such as Torsades de pointes, ventricular tachycardia, and cardiac arrest.91 Clinical implications of the QT-prolongation, however, have conflicting data. Several studies have shown no significant difference in arrhythmogenic events and overall outcomes.92, 93, 94 QTc prolongation tended to occur more often in COVID patients who had worsening renal disease and myocardial injury.95 Whether the harm is theoretical or not, the available evidence has not shown significant efficacy with the use of hydroxychloroquine/chloroquine with or without azithromycin and therefore it is not currently recommended for use in COVID-19 infection.
Remdesivir
Remdesivir, an RNA polymerase inhibitor, has been shown to shorten recovery time in patients hospitalized with COVID.96 It is currently approved by Food and Drug Administration (FDA) for use in these patients, and more recent data have suggested a possible role in non-hospitalized patients at high risk for COVID-19 disease progression.97 The most commonly reported side-effects include infusion site reaction, elevated liver enzymes, acute kidney injury, and hypotension.98 From a cardiac standpoint, Remdesivir has been implicated in the development of QTc prolongation, bradycardia, and even heart block.99 Case reports have noted the resolution of bradycardia and complete heart block after stopping Remdesivir.99, 100, 101
Dexamethasone
Dexamethasone is a synthetic glucocorticoid that mimics the action of steroid compounds produced in the body through strong anti-inflammatory and immunosuppressive effects via a multitude of mechanisms: (i) Decrease in leukocyte concentration and adhesion to endothelium (ii) Inhibition of phagocytosis and lysosomal degradation thereby decreasing immune cells and blocking IgE-dependent secretion of histamine and leukotrienes, and (iii) Inhibit the release of cytokines.102 Dexamethasone has been the most promising treatment modality studied and has shown to reduce mortality. High-dose corticosteroids should be used with caution in patients with cardiac comorbidities due to the potential adverse side effects such as heart failure exacerbation and arrhythmias.102
Tocilizumab
Tocilizumab is a recombinant IgG monoclonal antibody that binds to the soluble and membrane-bound receptor for IL-6, which inhibits the signaling pathway thereby decreasing the proinflammatory effects associated with IL-6.103 Tocilizumab has been shown to reduce mortality and the need for mechanical ventilation in COVID-19 patients; however, the statistical significance has varied among trials.104 , 105 Many adverse effects have been documented including the development of QT interval prolongation.105 , 106
Baricitinib
Baricitinib is a selective inhibitor of JAK-1 and JAK-2 which mediates cytokine signaling and growth factors involved in hematopoiesis, inflammation, and immune response.107 Baricitinib has been shown to significantly reduce the induction of IL-6. Approved by the FDA for use alongside Remdesivir, the combination reduces times to recovery among hospitalized COVID patients.108 Despite this, there is a dose-dependent relationship between Baricitinib and acute arterial and venous thromboembolic events.109 Baricitinib should be immediately stopped if there is concern for thromboembolism.
Paxlovid (Nirmatrlvir and Ritonavir)
Paxlovid is a combination of a protease inhibitor and HIV-1 and HIV-2 protease inhibitor (ritonavir).104 Paxlovid has been given emergency use authorization by the FDA in the treatment of COVID-19 patients with mild to moderate symptoms as an outpatient medication.110 A study showed that Paxlovid reduced the risk of hospitalization or death by 89%.111 The utilization of Paxlovid is relatively new, however, hypertension has been depicted as a common adverse effect.112 The ritonavir component of Paxlovid is a CYP3A inhibitor and can cause serious elevations of drugs metabolized by CYP3A including amiodarone.112 Post-marketing surveillance will bring to fruition any further cardiac implications associated with Paxlovid use.
Molnuparivir
Molnuparivir is an antiviral that is converted to a synthetic cytidine nucleoside inside the host's body leading to the introduction of errors introduced into the virus's genome resulting in defective viral components.113 Molnuparivir has been shown to increase time to viral clearance. In the small-scale clinical trials, Molnuparivir was very well tolerated without any noted cardiac side effects114. Post-marketing surveillance will be needed to further investigate any potential cardiac implications on a larger scale.
mRNA COVID-19 Vaccination
mRNA vaccinations were unprecedented and developed in less than 1 year after the outbreak of COVID-19 in the United States.115 After emergency use authorization, post-marketing surveillance discovered reports of myocarditis and pericarditis associated with these vaccination.116 , 117 The adjusted risk ratio for those 16-24 years of age was determined to be 0.94, and ultimately resulted in an FDA warning.115 There was a high incidence of myocarditis cases among the male population. A report from the Israeli Ministry of Health noted 1/3000 to 1/6000 men aged 16-24 developed myocarditis or pericarditis following vaccination administration118.
It is hypothesized that myocarditis occurs due to a high antibody response in a portion of the young adult population with a response similar to a multisystem inflammatory syndrome that occurs in children diagnosed with COVID-19.119 Other potential causes include vaccination induction of the innate inflammatory response between the viral protein and an unknown cardiac protein or the vaccine itself leads to cytokine activation of pre-existing immune cells in young adults who were previously infected yet had an asymptomatic presentation of COVID-19.120 , 121 Diagnosis is typically achieved through a combination of positive inflammatory markers (C-reactive protein and erythrocyte sedimentation rate), troponin elevation, electrocardiogram, echocardiogram, and cMRI.115 Typically, vaccine-induced myocarditis and pericarditis are self-limited. The long-term impact of vaccine-induced myocarditis and pericarditis are currently unknown.
Postural orthostatic tachycardia syndrome (POTS) is an autonomic condition characterized by tachycardia with associated orthostatic intolerance upon standing without accompanied hypotension.122 COVID-19 vaccinations have been associated as one of the triggers of POTS, with few case reports depicting the association between the mRNA vaccine for COVID-19 and the development of POTS post-inoculation. It has been hypothesized that POTS results from a disruption in the ACE2 receptor.123
Regardless of the risk of development of cardiovascular side effects to the COVID-19 vaccination, it is still strongly recommended to obtain a vaccine as cardiovascular side effects are rare.115
Long-term Cardiac Implications Following Recovery
Many of the cardiac complications identified with acute infection complicate the patient's clinical course and are associated with high morbidity and mortality. Those who are fortunate to survive are at risk for long-term cardiac complications. A recent study evaluated the 1-year burden in cardiovascular diseases in over 150,000 COVID-19 patients.124 An increased incidence of arrhythmias, ischemic and nonischemic cardiomyopathy, pericarditis, myocarditis, and thromboembolic disease were observed, suggesting a significant risk of cardiovascular disease in COVID-19 survivors.
As SARS-CoV-1 infection uses the same cell entry receptors as the COVID-19 virus, the cardiac complications appear similar to those seen with SARS-CoV-1.125 , 126 SARS-CoV-1 has been associated with arrhythmias, cardiomegaly, and hypotension in the acute setting with long-term follow-up studies suggesting an increased risk for cardiovascular disease including myocardial infarction, fatal coronary heart disease, atherosclerosis, and hyperlipidemia.126 There was an observed recovery in diastolic and systolic function at 30 days for a majority of SARS-CoV-1 patients. Based on the SARS-CoV-1 studies, long-term cardiac complications from COVID-19 are suggested.126 Manifestations such as cardiomyopathy may be reversible in 30-90 days post-infection; however, it is hypothesized that an increased risk for atherosclerosis and its complications may be apparent years post-infection evidenced by long-term follow-up studies for SARS-CoV-1 patients. A German study evaluated 100 recovered COVID-19 patients at a minimum of 2 weeks after diagnosis with cMRI, which revealed cardiac involvement and continued myocardial inflammation in 78% and 60% of patients respectively.127
For stress-induced cardiomyopathy, long-term follow-up is indicated to ensure recovery of ejection fraction. Prior observational studies have depicted long-term symptomology in patients with stress-induced cardiomyopathy despite resolution in ejection fraction.128 These studies were in the absence of COVID-19 as an insult however should be considered when monitoring COVID-19 survivors.
Long-term implications for patients with myocarditis in the setting of COVID-19 are unknown. However, it is important to consider complications such as atrial and ventricular arrhythmias and non-ischemic cardiomyopathy that does not recover despite optimal medical therapy in the setting of viral myocarditis.3 Case series have described autopsies that discover myocarditis as the culprit of young adults with sudden cardiac death.3 One case reported VF in a patient with myocarditis and recovered ejection fraction.129 Ventricular arrhythmias are inculpated in sudden cardiac death and therefore high-risk patients should be monitored closely.3
Children have been reported to develop a syndrome similar to Kawasaki disease referred to as multisystem inflammatory syndrome in children (MIS-C). MIS-C characteristically develops 4-6 weeks post-COVID-19 infection in which children exhibit signs of hyperinflammatory state with symptoms of diarrhea, vomiting, severe cutaneous manifestations similar to toxic shock syndrome, and multiorgan dysfunction.130 The cardiac manifestations are myocarditis, pericarditis, pericardial effusion, and coronary artery abnormalities.131 There have been case reports of MIS in adults with similar cardiac complications.132 Long-term implications are unknown.126
Long-COVID symptoms include breathlessness, palpitations, chest discomfort, fatigue, orthostatic intolerance along with a cluster of other nonspecific symptoms. These symptoms in combination with orthostatic tachycardia are referred to as POTS post-COVID-19. There have been a series of case reports depicting this manifestation.133 POTS in the absence of COVID-19 is underdiagnosed due to lack of familiarity with syndrome suggesting that post-COVID-19 patients face similar barriers to diagnosis.134 Further research is indicated to determine long-term sequelae.
Conclusion
COVID-19 can lead to a plethora of complications involving the heart, especially in patients with baseline comorbidities such as diabetes, hypertension, and obesity. An awareness of the pathophysiology and presentations of the cardiac components of COVID-19 are particularly beneficial as cardiac manifestations are associated with a significant increase in morbidity and mortality. Additionally, clinicians should be mindful of the cardiac consequences from treatment modalities and vaccination. Regardless of the cardiovascular side effects, it remains strongly recommended to receive the vaccination. For those who are COVID-19 survivors, a high clinical suspicion for the development of long-term cardiac sequelae is pertinent to ensure that improvement in quality of life and life-threatening cardiac complications can be identified and managed.
Conflict of Interest and Author Contribution
(1) All authors have participated in the work and have reviewed and agree with the content of the article; (2) None of the article contents are under consideration for publication in any other journal or have been published in any journal; (3) No portion of the text has been copied from other material in the literature; (4) I am aware that it is the authors responsibility to obtain permission for any figures or tables reproduced from any prior publications, and to cover fully any costs involved. Every author listed contributed to our work in a substantial manner. Each author's contribution is listed. (1) Conception and design: Theresa Maitz, Dominic Parfianowicz, Rahul Gupta; (2) Drafting of the manuscript and revising it critically for important intellectual content: Theresa Maitz, Dominic Parfianowicz, Ashley Vojtek, Yasotha Rajeswaran, Apurva V Vyas, Rahul Gupta: (3) Final approval of the manuscript submitted: Yasotha Rajeswaran, Apurva V Vyas, Rahul Gupta.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.University JH. 2022. COVID-19 Global map in COVID-19 dashboard by the CSSE at JHU COVID-19 Resource center. https://coronavirus.jhu.edu/map.html. [Google Scholar]
- 2.RG Vikramaditya Reddy Samala Venkata, Aedma Surya Kiran, Andrus Bruce W. Covid-19 and cardiovascular complications: pooled analysis of observational studies. Circulation. 2020;142:A15097. [Google Scholar]
- 3.Mitrani RD, Dabas N, Goldberger JJ. COVID-19 cardiac injury: Implications for long-term surveillance and outcomes in survivors. Heart Rhythm. 2020;17:1984–1990. doi: 10.1016/j.hrthm.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng S, Zhao Y, Wang F, Chen Y, Kaminga AC, Xu H. Comorbidities' potential impacts on severe and non-severe patients with COVID-19: A systematic review and meta-analysis. Medicine (Baltimore) 2021;100:e24971. doi: 10.1097/MD.0000000000024971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dy LF, Lintao RCV, Cordero CP, Cabaluna ITG, Dans LF. Prevalence and prognostic associations of cardiac abnormalities among hospitalized patients with COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11:8449. doi: 10.1038/s41598-021-87961-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aslani M, Mortazavi-Jahromi SS, Mirshafiey A. Cytokine storm in the pathophysiology of COVID-19: Possible functional disturbances of miRNAs. Int Immunopharmacol. 2021;101 doi: 10.1016/j.intimp.2021.108172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li G, Fan Y, Lai Y, et al. Coronavirus infections and immune responses. J Med Virol. 2020;92:424–432. doi: 10.1002/jmv.25685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 cytokine storm; what we know so far. Front Immunol. 2020;11:1446. doi: 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Umemura Y, Yamakawa K, Kiguchi T, Nishida T, Kawada M, Fujimi S. Hematological phenotype of COVID-19-induced coagulopathy: far from typical sepsis-induced coagulopathy. J Clin Med. 2020;9(9):2875. doi: 10.3390/jcm9092875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah RM, Shah M, Shah S, Li A, Jauhar S. Takotsubo syndrome and COVID-19: associations and implications. Curr Probl Cardiol. 2021;46 doi: 10.1016/j.cpcardiol.2020.100763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holm A, Jerkeman M, Sultanian P, et al. Cohort study of the characteristics and outcomes in patients with COVID-19 and in-hospital cardiac arrest. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-054943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shang J, Wan Y, Luo C, et al. Cell entry mechanisms of SARS-CoV-2. Proc Natl Acad Sci U S A. 2020;117:11727–11734. doi: 10.1073/pnas.2003138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dhakal BP, Sweitzer NK, Indik JH, Acharya D, William P. SARS-CoV-2 infection and cardiovascular disease: COVID-19 heart. Heart Lung Circ. 2020;29:973–987. doi: 10.1016/j.hlc.2020.05.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zamorano Cuervo N, Grandvaux N. ACE2: Evidence of role as entry receptor for SARS-CoV-2 and implications in comorbidities. Elife. 2020;9:e61390. doi: 10.7554/eLife.61390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scialo F, Daniele A, Amato F, et al. ACE2: The major cell entry receptor for SARS-CoV-2. Lung. 2020;198:867–877. doi: 10.1007/s00408-020-00408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guzik TJ, Mohiddin SA, Dimarco A, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116:1666–1687. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.RGaSKA Vikramaditya Reddy Samala Venkata. Covid-19 and hypertension: pooled analysis of observational studies. Hypertension. 2020;76:P135. [Google Scholar]
- 18.Metkus TS, Sokoll LJ, Barth AS, et al. Myocardial injury in severe COVID-19 compared with non-COVID-19 acute respiratory distress syndrome. Circulation. 2021;143:553–565. doi: 10.1161/CIRCULATIONAHA.120.050543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ranard LS, Fried JA, Abdalla M, et al. Approach to acute cardiovascular complications in COVID-19 infection. Circ Heart Fail. 2020;13 doi: 10.1161/CIRCHEARTFAILURE.120.007220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pranata R, Huang I, Raharjo SB. Incidence and impact of cardiac arrhythmias in coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Indian Pacing Electrophysiol J. 2020;20:193–198. doi: 10.1016/j.ipej.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zylla MM, Merle U, Vey JA, et al. Predictors and prognostic implications of cardiac arrhythmias in patients hospitalized for COVID-19. J Clin Med. 2021;10(1):133. doi: 10.3390/jcm10010133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zareini B, Rajan D, El-Sheikh M, et al. Cardiac arrhythmias in patients hospitalized with COVID-19: The ACOVID study. Heart Rhythm O2. 2021;2:304–308. doi: 10.1016/j.hroo.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020;41:1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garcia-Zamora S, Lee S, Haseeb S, et al. Arrhythmias and electrocardiographic findings in Coronavirus disease 2019: A systematic review and meta-analysis. Pacing Clin Electrophysiol. 2021;44:1062–1074. doi: 10.1111/pace.14247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gawalko M, Kaplon-Cieslicka A, Hohl M, Dobrev D, Linz D. COVID-19 associated atrial fibrillation: Incidence, putative mechanisms and potential clinical implications. Int J Cardiol Heart Vasc. 2020;30 doi: 10.1016/j.ijcha.2020.100631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Musikantow DR, Turagam MK, Sartori S, et al. Atrial fibrillation in patients hospitalized with COVID-19: incidence, predictors, outcomes, and comparison to influenza. JACC Clin Electrophysiol. 2021;7:1120–1130. doi: 10.1016/j.jacep.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coromilas EJ, Kochav S, Goldenthal I, et al. Worldwide survey of COVID-19-associated arrhythmias. Circ Arrhythm Electrophysiol. 2021;14 doi: 10.1161/CIRCEP.120.009458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho JH, Namazi A, Shelton R, et al. Cardiac arrhythmias in hospitalized patients with COVID-19: A prospective observational study in the western United States. PLoS One. 2020;15 doi: 10.1371/journal.pone.0244533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tan Z, Huang S, Mei K, et al. The prevalence and associated death of ventricular arrhythmia and sudden cardiac death in hospitalized patients with COVID-19: A systematic review and meta-analysis. Front Cardiovasc Med. 2021;8 doi: 10.3389/fcvm.2021.795750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beri A, Kotak K. Cardiac injury, arrhythmia, and sudden death in a COVID-19 patient. HeartRhythm Case Rep. 2020;6:367–369. doi: 10.1016/j.hrcr.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Turagam MK, Musikantow D, Goldman ME, et al. Malignant arrhythmias in patients with COVID-19: incidence, mechanisms, and outcomes. Circ Arrhythm Electrophysiol. 2020;13 doi: 10.1161/CIRCEP.120.008920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Efros O, Soffer S, Leibowitz A, et al. Risk factors and mortality in patients with pneumonia and elevated troponin levels. Sci Rep. 2020;10:21619. doi: 10.1038/s41598-020-78287-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Efros O, Barda N, Meisel E, et al. Myocardial injury in hospitalized patients with COVID-19 infection-Risk factors and outcomes. PLoS One. 2021;16 doi: 10.1371/journal.pone.0247800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim W, Whitlock R, Khera V, et al. Etiology of troponin elevation in critically ill patients. J Crit Care. 2010;25:322–328. doi: 10.1016/j.jcrc.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 36.Samidurai A, Das A. Cardiovascular complications associated with COVID-19 and potential therapeutic∼strategies. Int J Mol Sci. 2020;21 doi: 10.3390/ijms21186790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baksi AJ, Kanaganayagam GS, Prasad SK. Arrhythmias in viral myocarditis and pericarditis. Card Electrophysiol Clin. 2015;7:269–281. doi: 10.1016/j.ccep.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 38.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sawalha K, Abozenah M, Kadado AJ, et al. Systematic review of COVID-19 related myocarditis: insights on management and outcome. Cardiovasc Revasc Med. 2021;23:107–113. doi: 10.1016/j.carrev.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bandyopadhyay D, Akhtar T, Hajra A, et al. COVID-19 pandemic: cardiovascular complications and future implications. Am J Cardiovasc Drugs. 2020;20:311–324. doi: 10.1007/s40256-020-00420-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanchez Tijmes F, Thavendiranathan P, Udell JA, Seidman MA, Hanneman K. Cardiac MRI assessment of nonischemic myocardial inflammation: state of the art review and update on myocarditis associated with COVID-19 vaccination. Radiol Cardiothorac Imaging. 2021;3 doi: 10.1148/ryct.210252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mele D, Flamigni F, Rapezzi C, Ferrari R. Myocarditis in COVID-19 patients: current problems. Intern Emerg Med. 2021;16:1123–1129. doi: 10.1007/s11739-021-02635-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bielecka-Dabrowa A, Cichocka-Radwan A, Lewek J, Pawliczak F, Maciejewski M, Banach M. Cardiac manifestations of COVID-19. Rev Cardiovasc Med. 2021;22:365–371. doi: 10.31083/j.rcm2202043. [DOI] [PubMed] [Google Scholar]
- 44.Agewall S, Giannitsis E, Jernberg T, Katus H. Troponin elevation in coronary vs. non-coronary disease. Eur Heart J. 2011;32:404–411. doi: 10.1093/eurheartj/ehq456. [DOI] [PubMed] [Google Scholar]
- 45.Rusu I, Turlacu M, Micheu MM. Acute myocardial injury in patients with COVID-19: Possible mechanisms and clinical implications. World J Clin Cases. 2022;10:762–776. doi: 10.12998/wjcc.v10.i3.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tajbakhsh A, Gheibi Hayat SM, Taghizadeh H, et al. COVID-19 and cardiac injury: clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up. Expert Rev Anti Infect Ther. 2021;19:345–357. doi: 10.1080/14787210.2020.1822737. [DOI] [PubMed] [Google Scholar]
- 47.Szerlip M, Anwaruddin S, Aronow HD, et al. Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic perspectives from the Society for Cardiovascular Angiography and Interventions Emerging Leader Mentorship (SCAI ELM) members and graduates. Catheter Cardiovasc Interv. 2020;96:586–597. doi: 10.1002/ccd.28887. [DOI] [PubMed] [Google Scholar]
- 48.Welt FGP, Shah PB, Aronow HD, et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC's interventional council and SCAI. J Am Coll Cardiol. 2020;75:2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choudry FA, Hamshere SM, Rathod KS, et al. High thrombus burden in patients with COVID-19 presenting with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2020;76:1168–1176. doi: 10.1016/j.jacc.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saad M, Kennedy KF, Imran H, et al. Association between COVID-19 diagnosis and in-hospital mortality in patients hospitalized with ST-segment elevation myocardial infarction. JAMA. 2021;326:1940–1952. doi: 10.1001/jama.2021.18890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bader F, Manla Y, Atallah B, Starling RC. Heart failure and COVID-19. Heart Fail Rev. 2021;26:1–10. doi: 10.1007/s10741-020-10008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Court O, Kumar A, Parrillo JE, Kumar A. Clinical review: Myocardial depression in sepsis and septic shock. Crit Care. 2002;6:500–508. doi: 10.1186/cc1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cassidy SS, Mitchell JH. Effects of positive pressure breathing on right and left ventricular preload and afterload. Fed Proc. 1981;40:2178–2181. [PubMed] [Google Scholar]
- 55.Friedberg MK, Redington AN. Right vs left ventricular failure: differences, similarities, and interactions. Circulation. 2014;129:1033–1044. doi: 10.1161/CIRCULATIONAHA.113.001375. [DOI] [PubMed] [Google Scholar]
- 56.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vassiliki' Coutsoumbas G, Gallo P, Zagnoni S, Di Pasquale G. Long-term injury after Takotsubo syndrome (stress cardiomyopathy) Eur Heart J Suppl. 2020;22:E73–E78. doi: 10.1093/eurheartj/suaa065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jabri A, Kalra A, Kumar A, et al. Incidence of stress cardiomyopathy during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.14780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kariyanna PT, Chandrakumar HP, Jayarangaiah A, et al. Apical takotsubo cardiomyopathy in a COVID-19 patient presenting with stroke: a case report and pathophysiologic insights. Am J Med Case Rep. 2020;8:350–357. [Google Scholar]
- 62.Dweck MR, Bularga A, Hahn RT, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21:949–958. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Giustino G, Croft LB, Oates CP, et al. Takotsubo cardiomyopathy in COVID-19. J Am Coll Cardiol. 2020;76:628–629. doi: 10.1016/j.jacc.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Malas MB, Naazie IN, Elsayed N, Mathlouthi A, Marmor R, Clary B. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: A systematic review and meta-analysis. EClinicalMedicine. 2020;29 doi: 10.1016/j.eclinm.2020.100639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aktaa S, Wu J, Nadarajah R, et al. Incidence and mortality due to thromboembolic events during the COVID-19 pandemic: Multi-sourced population-based health records cohort study. Thromb Res. 2021;202:17–23. doi: 10.1016/j.thromres.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York city health system. JAMA. 2020;324:799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mehta JL, Calcaterra G, Bassareo PP. COVID-19, thromboembolic risk, and Virchow's triad: Lesson from the past. Clin Cardiol. 2020;43:1362–1367. doi: 10.1002/clc.23460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lu YF, Pan LY, Zhang WW, et al. A meta-analysis of the incidence of venous thromboembolic events and impact of anticoagulation on mortality in patients with COVID-19. Int J Infect Dis. 2020;100:34–41. doi: 10.1016/j.ijid.2020.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Philip AM, George LJ, John KJ, et al. A review of the presentation and outcome of left ventricular thrombus in coronavirus disease 2019 infection. J Clin Transl Res. 2021;7:797–808. [PMC free article] [PubMed] [Google Scholar]
- 71.Rapkiewicz AV, Mai X, Carsons SE, et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series. EClinicalMedicine. 2020;24 doi: 10.1016/j.eclinm.2020.100434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Llitjos JF, Leclerc M, Chochois C, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;18:1743–1746. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paliogiannis P, Mangoni AA, Dettori P, Nasrallah GK, Pintus G, Zinellu A. D-Dimer concentrations and COVID-19 severity: a systematic review and meta-analysis. Front Public Health. 2020;8:432. doi: 10.3389/fpubh.2020.00432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Spyropoulos AC, Goldin M, Giannis D, et al. Efficacy and safety of therapeutic-dose heparin vs standard prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with COVID-19: The HEP-COVID randomized clinical trial. JAMA Intern Med. 2021;181:1612–1620. doi: 10.1001/jamainternmed.2021.6203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Teta M, Drabkin MJ. Fatal retroperitoneal hematoma associated with Covid-19 prophylactic anticoagulation protocol. Radiol Case Rep. 2021;16:1618–1621. doi: 10.1016/j.radcr.2021.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ghani MU, Kumar M, Ghani U, Sonia F, Abbas SA. Intracranial hemorrhage complicating anticoagulant prophylactic therapy in three hospitalized COVID-19 patients. J Neurovirol. 2020;26:602–604. doi: 10.1007/s13365-020-00869-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20:389–391. doi: 10.1038/s41577-020-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Grosse C, Grosse A, Salzer HJF, Dunser MW, Motz R, Langer R. Analysis of cardiopulmonary findings in COVID-19 fatalities: High incidence of pulmonary artery thrombi and acute suppurative bronchopneumonia. Cardiovasc Pathol. 2020;49 doi: 10.1016/j.carpath.2020.107263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen J, Ye J, Li H, Xia Z, Yan H. Changes in the clinical characteristics of 62 patients who died from coronavirus disease 2019. Biomed Res Int. 2020;2020 doi: 10.1155/2020/3280908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Klok FA, Kruip M, van der Meer NJM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Farshidfar F, Koleini N, Ardehali H. Cardiovascular complications of COVID-19. JCI Insight. 2021;6(13):e148980. doi: 10.1172/jci.insight.148980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jagia P, Ojha V, Naik N, Sharma S. Myocardial fibrosis detected by cardiovascular magnetic resonance in absence of myocardial oedema in a patient recovered from COVID-19. BMJ Case Rep. 2020;13:e240193. doi: 10.1136/bcr-2020-240193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Spano G, Fischer K, Maillat C, Vicario G, Huber AT, Grani C. Delayed isolated peri-myocarditis in a Covid-19 patient with respiratory symptoms but without lung involvement. Int J Cardiovasc Imaging. 2020;36:2279–2280. doi: 10.1007/s10554-020-01943-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huang L, Zhao P, Tang D, et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13:2330–2339. doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yao X, Ye F, Zhang M, et al. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Clin Infect Dis. 2020;71:732–739. doi: 10.1093/cid/ciaa237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R. Effects of chloroquine on viral infections: an old drug against today's diseases? Lancet Infect Dis. 2003;3:722–727. doi: 10.1016/S1473-3099(03)00806-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Devaux CA, Rolain JM, Colson P, Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Singh B, Ryan H, Kredo T, Chaplin M, Fletcher T. Chloroquine or hydroxychloroquine for prevention and treatment of COVID-19. Cochrane Database Syst Rev. 2021;2 doi: 10.1002/14651858.CD013587.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kashour Z, Riaz M, Garbati MA, et al. Efficacy of chloroquine or hydroxychloroquine in COVID-19 patients: a systematic review and meta-analysis. J Antimicrob Chemother. 2021;76:30–42. doi: 10.1093/jac/dkaa403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Geleris J, Sun Y, Platt J, et al. Observational study of hydroxychloroquine in hospitalized patients with covid-19. N Engl J Med. 2020;382:2411–2418. doi: 10.1056/NEJMoa2012410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Eftekhar SP, Kazemi S, Barary M, Javanian M, Ebrahimpour S, Ziaei N. Effect of hydroxychloroquine and azithromycin on QT interval prolongation and other cardiac arrhythmias in COVID-19 confirmed patients. Cardiovasc Ther. 2021;2021 doi: 10.1155/2021/6683098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Saleh M, Gabriels J, Chang D, et al. Effect of chloroquine, hydroxychloroquine, and azithromycin on the corrected QT interval in patients with SARS-CoV-2 infection. Circ Arrhythm Electrophysiol. 2020;13 doi: 10.1161/CIRCEP.120.008662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Maneikis K, Ringeleviciute U, Bacevicius J, et al. Mitigating arrhythmia risk in hydroxychloroquine and azithromycin treated COVID-19 patients using arrhythmia risk management plan. Int J Cardiol Heart Vasc. 2021;32 doi: 10.1016/j.ijcha.2020.100685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hooks M, Bart B, Vardeny O, Westanmo A, Adabag S. Effects of hydroxychloroquine treatment on QT interval. Heart Rhythm. 2020;17:1930–1935. doi: 10.1016/j.hrthm.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of covid-19 - final report. N Engl J Med. 2020;383:1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gottlieb RL, Vaca CE, Paredes R, et al. Early remdesivir to prevent progression to severe covid-19 in outpatients. N Engl J Med. 2022;386:305–315. doi: 10.1056/NEJMoa2116846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Singh A, Kamath A. Assessment of adverse events associated with remdesivir use for coronavirus disease 2019 using real-world data. Expert Opin Drug Saf. 2021;20:1559–1564. doi: 10.1080/14740338.2021.1962846. [DOI] [PubMed] [Google Scholar]
- 99.Gupta AK, Parker BM, Priyadarshi V, Parker J. Cardiac adverse events with remdesivir in covid-19 infection. Cureus. 2020;12:e11132. doi: 10.7759/cureus.11132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gubitosa JC, Kakar P, Gerula C, et al. Marked sinus bradycardia associated with remdesivir in covid-19: a case and literature review. JACC Case Rep. 2020;2:2260–2264. doi: 10.1016/j.jaccas.2020.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Selvaraj V, Bavishi C, Patel S, Dapaah-Afriyie K. Complete heart block associated with remdesivir in covid-19: a case report. Eur Heart J Case Rep. 2021;5:ytab200. doi: 10.1093/ehjcr/ytab200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ahmed MH, Hassan A. Dexamethasone for the treatment of coronavirus disease (COVID-19): a review. SN Compr Clin Med. 2020:1–10. doi: 10.1007/s42399-020-00610-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sebba A. Tocilizumab: the first interleukin-6-receptor inhibitor. Am J Health Syst Pharm. 2008;65:1413–1418. doi: 10.2146/ajhp070449. [DOI] [PubMed] [Google Scholar]
- 104.Drozdzal S, Rosik J, Lechowicz K, et al. An update on drugs with therapeutic potential for SARS-CoV-2 (COVID-19) treatment. Drug Resist Updat. 2021;59 doi: 10.1016/j.drup.2021.100794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lan SH, Lai CC, Huang HT, Chang SP, Lu LC, Hsueh PR. Tocilizumab for severe COVID-19: a systematic review and meta-analysis. Int J Antimicrob Agents. 2020;56 doi: 10.1016/j.ijantimicag.2020.106103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ranchal P, Yates E, Gupta R, Aronow WS. Tocilizumab-associated bowel perforation in SARS-CoV-2 infection. Am J Ther. 2020 doi: 10.1097/MJT.0000000000001273. [DOI] [PubMed] [Google Scholar]
- 107.Stebbing J, Krishnan V, de Bono S, et al. Mechanism of baricitinib supports artificial intelligence-predicted testing in COVID-19 patients. EMBO Mol Med. 2020;12:e12697. doi: 10.15252/emmm.202012697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with covid-19. N Engl J Med. 2021;384:795–807. doi: 10.1056/NEJMoa2031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mogul A, Corsi K, Baricitinib McAuliffe L. The second FDA-Approved JAK inhibitor for the treatment of rheumatoid arthritis. Ann Pharmacother. 2019;53:947–953. doi: 10.1177/1060028019839650. [DOI] [PubMed] [Google Scholar]
- 110.Mahase E. Covid-19: Pfizer's paxlovid is 89% effective in patients at risk of serious illness, company reports. BMJ. 2021;375:n2713. doi: 10.1136/bmj.n2713. [DOI] [PubMed] [Google Scholar]
- 111.Wen W, Chen C, Tang J, et al. Efficacy and safety of three new oral antiviral treatment (molnupiravir, fluvoxamine and Paxlovid) for COVID-19a meta-analysis. Ann Med. 2022;54:516–523. doi: 10.1080/07853890.2022.2034936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Paxlovid for treatment of COVID-19. Med Lett Drugs Ther. 2022;64:9–10. [PubMed] [Google Scholar]
- 113.Painter WP, Holman W, Bush JA, et al. Human safety, tolerability, and pharmacokinetics of molnupiravir, a novel broad-spectrum oral antiviral agent with activity against SARS-CoV-2. Antimicrob Agents Chemother. 2021;65(5) doi: 10.1128/AAC.02428-20. e02428-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Fischer WA, 2nd, Eron JJ, Jr, Holman W, et al. A phase 2a clinical trial of molnupiravir in patients with COVID-19 shows accelerated SARS-CoV-2 RNA clearance and elimination of infectious virus. Sci Transl Med. 2022;14:eabl7430. doi: 10.1126/scitranslmed.abl7430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Das BB, Moskowitz WB, Taylor MB, Palmer A. Myocarditis and pericarditis following mRNA COVID-19 vaccination: what do we know so far? Children (Basel) 2021;8(7):607. doi: 10.3390/children8070607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ammirati E, Cavalotti C, Milazzo A, et al. Temporal relation between second dose BNT162b2 mRNA Covid-19 vaccine and cardiac involvement in a patient with previous SARS-COV-2 infection. Int J Cardiol Heart Vasc. 2021;34 doi: 10.1016/j.ijcha.2021.100774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rosner CM, Genovese L, Tehrani BN, et al. Myocarditis temporally associated with COVID-19 vaccination. Circulation. 2021;144:502–505. doi: 10.1161/CIRCULATIONAHA.121.055891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Doshi P. Covid-19 vaccines: In the rush for regulatory approval, do we need more data? BMJ. 2021;373:n1244. doi: 10.1136/bmj.n1244. [DOI] [PubMed] [Google Scholar]
- 119.Grimaud M, Starck J, Levy M, et al. Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann Intensive Care. 2020;10:69. doi: 10.1186/s13613-020-00690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Root-Bernstein R, Fairweather D. Unresolved issues in theories of autoimmune disease using myocarditis as a framework. J Theor Biol. 2015;375:101–123. doi: 10.1016/j.jtbi.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Segal Y, Shoenfeld Y. Vaccine-induced autoimmunity: the role of molecular mimicry and immune crossreaction. Cell Mol Immunol. 2018;15:586–594. doi: 10.1038/cmi.2017.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Reddy S, Reddy S, Arora M. A case of postural orthostatic tachycardia syndrome secondary to the messenger RNA COVID-19 Vaccine. Cureus. 2021;13:e14837. doi: 10.7759/cureus.14837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mustafa HI, Raj SR, Diedrich A, et al. Altered systemic hemodynamic and baroreflex response to angiotensin II in postural tachycardia syndrome. Circ Arrhythm Electrophysiol. 2012;5:173–180. doi: 10.1161/CIRCEP.111.965343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28:583–590. doi: 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jeffers SA, Tusell SM, Gillim-Ross L, et al. CD209L (L-SIGN) is a receptor for severe acute respiratory syndrome coronavirus. Proc Natl Acad Sci U S A. 2004;101:15748–15753. doi: 10.1073/pnas.0403812101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Higgins V, Sohaei D, Diamandis EP, Prassas I. COVID-19: from an acute to chronic disease? potential long-term health consequences. Crit Rev Clin Lab Sci. 2021;58:297–310. doi: 10.1080/10408363.2020.1860895. [DOI] [PubMed] [Google Scholar]
- 127.Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Scally C, Rudd A, Mezincescu A, et al. Persistent long-term structural, functional, and metabolic changes after stress-induced (Takotsubo) cardiomyopathy. Circulation. 2018;137:1039–1048. doi: 10.1161/CIRCULATIONAHA.117.031841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Prochnau D, Surber R, Kuehnert H, Heinke M, Klein HU, Figulla HR. Successful use of a wearable cardioverter-defibrillator in myocarditis with normal ejection fraction. Clin Res Cardiol. 2010;99:129–131. doi: 10.1007/s00392-009-0093-2. [DOI] [PubMed] [Google Scholar]
- 130.Ahmed M, Advani S, Moreira A, et al. Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kabeerdoss J, Pilania RK, Karkhele R, Kumar TS, Danda D, Singh S. Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: immunological mechanisms, clinical manifestations and management. Rheumatol Int. 2021;41:19–32. doi: 10.1007/s00296-020-04749-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Vogel TP, Top KA, Karatzios C, et al. Multisystem inflammatory syndrome in children and adults (MIS-C/A): Case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. 2021;39:3037–3049. doi: 10.1016/j.vaccine.2021.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Raj SR, Arnold AC, Barboi A, et al. Long-COVID postural tachycardia syndrome: an American autonomic society statement. Clin Auton Res. 2021;31:365–368. doi: 10.1007/s10286-021-00798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Dixit NM, Churchill A, Nsair A, Hsu JJ. Post-Acute COVID-19 syndrome and the cardiovascular system: what is known? Am Heart J Plus. 2021;5 doi: 10.1016/j.ahjo.2021.100025. [DOI] [PMC free article] [PubMed] [Google Scholar]