Abstract
Background:
Cannabis is widely used in the United States despite federal laws. In US states that have progressed toward legalization, there have been various reported impacts on cannabis-related emergency department (ED) visits. However, studies on the impact of legalization in Massachusetts (MA) EDs are lacking.
Methods:
Cannabinoid immunoassay (THC IA) results and cannabis-related ICD-10 codes were obtained for consecutive patient ED visits at two academic medical centers in Boston, MA over the following legalization periods (January 2012–December 2019): decriminalized (DEC), before medical dispensaries (MED BD), medical dispensaries available (MED DISP), before recreational dispensaries (REC BD) and recreational dispensaries available (REC DISP). Trends and monthly positivity rates for THC IA and ICD-10 codes were determined for these legalization periods.
Results:
There was an increase in both THC IA (p < .0001) and cannabis-related ICD-10 codes (p < .0001) in the ED as legalization progressed at both institutions. Positivity rates significantly increased by 7% for THC IA and 0.4% for ICD-10 codes. Increases in THC IA positivity were seen in females, patients aged 30–39, older adults (>59 years), and those in the highest income tertile. There was an increasing trend in amphetamine positivity and decreasing trend in opiate positivity in patients with positive THC IA. Unlike THC IA, significant trends per patient demographics were not seen with ICD-10 codes.
Conclusions:
Legalization of marijuana in MA has led to an increase in cannabis use as indicated by both increasing rates of positive THC IA results, in older adults, as well as increasing cannabis-related ICD-10 codes. Data suggest a steady increase in THC use associated with legalization that was not associated with an increase in opiate, fentanyl, or cocaine use. We recommend using ED THC IA positivity, an objective laboratory measure, to monitor THC use and the impact of state-specific progression in cannabis legalization.
Keywords: Marijuana, cannabis, tetrahydrocannabinol, urine drug screen, ICD-10, legalization
Introduction
Cannabis is one of the most widely used drugs with nearly 2.5% of the world’s population consuming cannabis and its associated compounds [1]. In the United States, up to 22 million people older than 12 years use cannabis annually. Tetrahydrocannabinol (THC) and cannabidiol (CBD) are the main psychoactive ingredients in cannabis and are the major components that act through the endocannabinoid system to address symptoms like pain, nausea, and anorexia [1]. Given empirical evidence suggesting medicinal benefit and a relatively limited side effect profile, cannabis has been legalized for medical use in 36 US states as of May 2021 [2,3]. Since June 2021, 18 of the 36 states have also legalized cannabis for recreational use [3].
Previous studies, performed in states which have approved legalization, show variable impact of legalization status on marijuana use [1,4–12]. Furthermore, the definition of cannabis use differs in published studies and may include a positive urine drug screen (UDS) for THC, self-reported marijuana use, number of calls to poison control related to marijuana, and/or positive ICD-9 or ICD-10 cannabis-related codes. Most of these studies were performed in the emergency department (ED) setting [1,4,6,8–10,12]. Levine et al. [4] reported an increase in marijuana use in ED patients, as indicated by positive UDS or self-reported marijuana use, in Arizona post-legalization of medicinal marijuana but no further increases once medical dispensaries (MED DISP) were opened. Grigorian et al. [1] also found an increase in positive UDS for marijuana in the ED post-legalization in California. Similar changes in marijuana use, ED visits and hospitalizations were seen post-legalization in Colorado, Washington, Alaska, and Oregon [8–11]. However, a study of trauma patients in Arizona reported no difference in self-reported marijuana use pre- and post-medical legalization [6] and a Canadian study showed no significant change in overall rate of ED visits with cannabis-related ICD-10 codes [12].
The clinical and operational impact of an increase in cannabis-related ED visits after legalization should be considered [1,4,8–10]. Since legalization, Colorado has reported a higher prevalence of mental health diagnoses, neuropsychiatric complaints, and burn injuries in ED patients using cannabis [9,13]. In Arizona and California, cannabis use was correlated with higher rates of trauma service activation [1,4]. Cannabis use has also been associated with adverse events, such as cyclical vomiting or cannabis-induced hyperemesis and seizures [8]. In states with more liberal regulations, additional ED resources may be required to manage patients and reduce morbidity.
Like other states, Massachusetts (MA) voters have approved legalization of cannabis use. MA voters passed medical marijuana legalization by ballot initiative in 2012 and the first dispensaries opened in 2015 [7]. In 2017, recreational use of cannabis was approved, and dispensaries began to open in late 2018. According to the 2018–2019 National Survey on Drug Use and Health (NSDUH), over 1.3 million people 12 or older had used cannabis in the past year in MA with 101,000 individuals using it for the first time. This suggested an increase in recreational use post-legalization [14]. Whitehill et al. [7] reported an increase in cannabis-related poison control calls in pediatric patients post medicinal legalization in MA. Otherwise, there are a limited number of studies on the impact of legalization of marijuana use in MA.
The primary purpose of this study was to determine trends in marijuana use in the ED at two large academic medical centers in Boston, MA.
Materials and methods
Setting
Brigham and Women’s Hospital (BWH) and Massachusetts General Hospital (MGH) are tertiary care hospitals in Boston, MA and the two founding members of Mass General Brigham (MGB) (formerly Partners Healthcare). The electronic health record (EHR) used at both institutions is Epic (Epic Healthcare Systems, Verona, WI) which was implemented on 6/1/2015 at BWH and 4/2/2016 at MGH.
BWH has an estimated 175 ED visits per day (2019 annual patient volume: 66,223), while MGH has almost double at 315 ED visits per day (2019 annual patient volume: 114,433). The overall patient populations also vary. At BWH more patients are females (p < .0001), >18 (p < .0001), Black (p < .0001), and Hispanic (p < .0001) compared to MGH. Due to the differences in the patient populations, data from each institution were analyzed separately. This study was approved by the MGB Health System Institutional Review Board.
Study description
All ED patients for which a UDS immunoassay panel or cannabinoid immunoassay screen (THC IA) was ordered during an ED visit from 1/1/2012 to 12/31/2019 were included. If multiple UDS or THC IA were ordered (0.8% of cases at both sites) during the ED visit, all results were included. At both BWH and MGH the UDS panel is ordered, per protocol, on patients with trauma team activations and patients presenting with primary behavioral health complaints. Testing is otherwise ordered at the discretion of the clinical care team. The UDS panel at BWH includes amphetamines, benzodiazepines, cannabinoids, cocaine metabolite, fentanyl, methadone, opiates, and oxycodone, while the UDS panel at MGH includes amphetamines, barbiturates, benzodiazepines, cannabinoids, cocaine metabolite, and opiates. At both BWH and MGH providers can order the panel or select individual components of the panel. The opiate assay cross reacts with morphine, codeine, hydrocodone, and hydromorphone, but not with oxycodone, oxymorphone, fentanyl, buprenorphine, or methadone. The monthly volumes of UDS panels at BWH and MGH are approximately 350/month and 775/month over the study period, respectively.
THC IA results and cannabis-related ICD-10 codes (Table 1) from the ED were obtained over multiple time periods of marijuana legalization in MA (Table 2) at both BWH and MGH. Associated demographics, such as gender, age, race, ethnicity, zip code, and results of other testing from UDS panel were also obtained. Legalization periods included decriminalized (DEC), before medical dispensaries (MED BD), medical dispensaries available (MED DISP) available, before recreational dispensaries (REC BD), and recreational dispensaries available (REC DISP) [15–19]. Qualitative urine THC IA were performed on the Roche Cobas analyzers (Roche Diagnostics, Indianapolis, IN) using the kinetic interaction of microparticles in solution (KIMS) methodology at both BWH (cutoff 50 ng/mL) and MGH (cutoff 20 ng/mL). The KIMS assay does not cross-react with CBD.
Table 1.
ICD-10 codes related to cannabis use.
| ICD10 code included | Diagnoses |
|---|---|
| F12.10, F12.12, F12.120, F12.121, F12.122, F12.129, F12.15, F12.151, F12.159, F12.18, F12.180, F12.188, F12.19, F12.2, F12.20, F12.22, F12.220, F12.221, F12.222, F12.229, F12.25, F12.250, F12.251, F12.259, F12.28, F12.280, F12.288 | Cannabis abuse and dependence |
| F12.9, F12.90, F12.92, F12.920, F12.921, F12.922, F12.929, F12.95, 12.950, F12.951, F12.959, F12.98, F12.980, F12.988, F12.99 | Cannabis use |
| T40.7 × 1, T40.7X1A, T40.7X1D, T40.7X1S, T40.7 × 2, T40.7X2A, T40.7X2D, T40.7X2S, T40.7 × 3, T40.7X3A, T40.7X3D, T40.7X3S, T40.7 × 4, T40.7X4A, T40.7X4D, T40.7X4S, T40.7 × 5, T40.7X5A, T40.7X5D, T40.7X5S | Cannabis poisoning and adverse effects |
| J66.2 | Cannabinosis |
| R11.10, R11.15 | Nausea and vomiting (cannabis hyperemesis syndrome), cyclical vomiting syndrome unrelated to migraine (based on chart review) |
Table 2.
Legalization time periods, date ranges, and urine THC immunoassay screen volumes.
| BWH | MGH | ||
|---|---|---|---|
| Time period | Date range | THC IA screen volumes | THC IA screen volumes |
| Decriminalized (DEC) | 11/4/2008–11/5/2012 | 4128 | 6459 |
| Before Medical Dispensaries (MED BD) | 11/6/2012–6/23/2015 | 12,724 | 20,799 |
| Medical Dispensaries Available (MED DISP) | 6/24/2015–7/27/2017 | 7663 | 19,603 |
| Before Recreational Dispensaries (REC BD) | 7/28/2017–11/19/2018 | 5364 | 14,390 |
| Recreational Dispensaries Available (REC DISP) | 11/20/2018–12/31/2019 | 4190 | 12,382 |
Urine cannabinoid immunoassay screen analysis
THC IA results and associated patient gender and date of birth were obtained from our laboratory information system (LIS), Sunquest (SQ; Sunquest Information Systems, Inc., Tucson, AZ) using validated reports for BWH (6/1/2015 to 12/31/2019) and MGH (1/1/2012 to 12/31/2019) and from the Research Patient Data Registry (a data repository) for BWH (1/1/2012 to 5/31/2015). BWH did not implement Sunquest until June 1, 2015 and therefore data prior to June 2015 was pulled from the validated system-wide research data repository. Age was removed from the analysis if the date of birth was unrealistic (e.g., 1900) and/or associated with an unknown patient name (e.g., “John or Jane Doe”). THC IA results and associated race, ethnicity, and zip code were obtained from the EHR between 6/1/2015 to 12/31/2019 for BWH and 4/2/2016 to 12/31/2019 for MGH. Results of other drugs in the UDS panel were obtained from the LIS for BWH (6/1/2015 to 12/31/2019 for all drugs except fentanyl, and 10/12/2016 to 12/31/2019 for fentanyl) and MGH (4/2/2016 to 12/31/2019). Fentanyl screening was added to the BWH UDS panel on 10/12/2016.
Two separate analyses were performed. First, trends in positivity for THC IA (e.g., overall positivity rate for each legalization period) over the legalization periods were determined. Trends in positivity within each demographic (gender, age, race, ethnicity, and income) were also determined over the legalization periods. Second, the 25th, median, 75th percentile for THC IA positivity rate per month was calculated for each legalization period (DEC, MED BD, MED DISP, REC BD, and REC DISP) at BWH and MGH.
The number and percentage of males and patients falling into the following age categories (<18, 18–29, 30–39, 40–49, 50–59, and >59 years) with positive THC IA in each legalization period was calculated. Self-reported race was divided into White, Black, Asian, American Indian, Native Hawaiian, other and, unavailable (this included patients who reported their race as Hispanic) and number and percentages with positive THC IA in each legalization period were calculated. Ethnicity was divided into Hispanic, not Hispanic, or unavailable, and, like race, the number and percentages with positive THC IA in each of the legalization periods were calculated.
MA zip codes were available for most patients with THC IA testing performed during their ED encounter (93% and 92% for BWH and MGH, respectively). Based on the median household annual income for each zip code [20], three tertiles were defined: tertile 1 included zip codes with the lowest median annual incomes from $13,666 to $62,037 (n = 7494 at BWH and n = 15,477 at MGH); tertile 2 included zip codes with median annual incomes from $62,091 to $82,950 (n = 4870 at BWH and n = 10,507 at MGH); and tertile 3 included zip codes with the highest median annual incomes, from $83,149 to $203,009 (n = 3,666 at BWH and n = 10,895 at MGH). The number and percentage of patients with positive THC IA in each of the tertiles per legalization period was determined.
In patients with a positive THC IA result in MED DISP, RED BD, and REC DISP, the results for other drugs in the UDS panel (components of the UDS panel at BWH and MGH were stated previously) were determined. Trends in other drug positivity over the legalization period were analyzed.
A two-dimensional heatmap was created using 300 random patients from both BWH and MGH. Only patients with at least one positive THC IA during any of the legalization periods were included. THC IA results per time period were categorized as no testing performed, zero positive, one positive, and ≥ two positive. Patients were sorted to display all patients with a positive result in a specific time period together.
ICD-10 code analysis
ICD-10 codes were obtained from the EHR from 10/1/2015 (the date of mandated conversion from ICD-9 to ICD-10) to 12/31/2019 for BWH and from 4/2/2016 (the date of conversion to new EHR) to 12/31/2019 for MGH. All ICD-10 codes associated with an ED visit in which a UDS panel or THC IA screen was ordered were obtained. Table 1 lists the ICD-10 codes that were considered positive for cannabis-related use [21]. Due to the lack of specificity of R11.10 and R11.15, chart review was performed (N.T., S.U., S.M.) for all cases with R11.10 or R11.15 in the absence of another cannabis-related code to determine if the patients’ symptoms and/or diagnosis were related to cannabis use. Cases with the following cannabis-related ICD-10 codes were not categorized as positive: F12.21 (Cannabis dependence, in remission) and T40.7, T40.7, T40.7X, T40.7 × 6, T40.7X6A, T40.7X6D, T40.7X6S (codes associated with underdosing of Cannabis).
First, trends in positivity for THC ICD-10 (e.g., overall positivity rate for each legalization period) over the legalization periods were determined. Trends in positivity within each demographic (gender, age, race, ethnicity, and income) were also determined over the legalization periods. Second, the 25th, median, 75th percentile for ICD-10 code positivity rate per month was calculated for MED DISP, REC BD, and REC DISP time periods at BWH and MGH.
Statistics
Monthly THC IA and ICD-10 positivity rates and patient demographics were compared between legalization periods using the Pearson’s chi-squared (χ2) test for categorical outcomes, the Fisher’s exact test for categorical outcomes when cell counts were <5, and the Wilcoxon rank-sum test for non-normally distributed continuous variables.
Logistic regression with positivity as the dependent variable and time period as a categorical predictor was used to assess trends in THC IA positivity or ICD-10 codes over legalization periods. The analysis was adjusted for gender, age, race, and ethnicity and the significance of a linear trend was tested by examining contrasts of marginal linear predictions with a post-estimation command. Further, trend analysis was performed to determine any differences in gender, age, race, ethnicity, income tertiles, and drug positivity for both THC IA and ICD-10 codes over the legalization periods.
Based on the sample size of this investigation, the minimum % increase in the dichotomous outcomes that could be detected as statistically significant – in any comparison – was 5%, assuming a power of 0.80 and an alpha level of 5%.
Analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC) and STATA version SE15 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). R version 3.5.3 (R Core Team 2013, Vienna, Austria. URL http://www.R-project.org/) was used for data retrieval from LIS and EHR, analysis, and figure creation. The packages used included RODBC 1.3–16, readxl 1.3.1, plyr 1.8.6, tidyverse 1.3.0, gtools 3.8.2, ggpubr 0.4.0, scales 1.1.0, and gridextra 2.3.
Results
Urine cannabinoid immunoassay screen
Table 2 shows the volume of THC IA screens at BWH and MGH per legalization period. Patient demographics are shown in Table 3.
Table 3.
Demographics for all ED patients with THC IA testing at BWH and MGH.
| Category | Demographic | DEC | MED BD | MED DISP | REC BD | REC DISP | p Value |
|---|---|---|---|---|---|---|---|
| BWH gender | Male, N (%) | 2270 (54.5%) | 6828 (53.7%) | 4109 (53.6%) | 2885 (53.8%) | 2206 (52.7%) | .323 |
| BWH age | Age, median (IQR) | 46 (25) | 47 (26) | 47 (30) | 49 (31) | 49 (31) | .0001 |
| BWH race | White, N (%) | – | – | 4448 (58.0%) | 3146 (58.7%) | 2431 (58.0%) | .751 |
| Black, N (%) | – | – | 1768 (23.1%) | 1159 (21.6%) | 965 (23.0%) | .108 | |
| Asian, N (%) | – | – | 153 (2.0%) | 137 (2.6%) | 100 (2.4%) | .091 | |
| American Indian, N (%) | – | – | 21 (0.3%) | 29 (0.5%) | 13 (0.3%) | .037 | |
| Native Hawaiian, N (%) | – | – | 5 (0.07%) | 3 (0.06%) | 1 (0.02%) | .635 | |
| Other, N (%) | – | – | 671 (8.8%) | 482 (9.0%) | 384 (9.2%) | .745 | |
| Unavailable, N (%) | – | – | 597 (7.8%) | 408 (7.6%) | 296 (7.1%) | .355 | |
| BWH ethnicity | Not Hispanic, N (%) | – | – | 6064 (79.1%) | 4357 (81.2%) | 3382 (80.7%) | .008 |
| Hispanic, N (%) | – | – | 1195 (15.6%) | 797 (14.9%) | 653 (15.6%) | .467 | |
| Unavailable, N (%) | – | – | 404 (5.3%) | 210 (3.9%) | 155 (3.7%) | <.0001 | |
| MGH gender | Male, N (%) | 3798 (58.8%) | 12,342 (59.3%) | 11,781 (60.1%) | 8550 (59.4%) | 7363 (59.5%) | .347 |
| MGH age | Age, median (IQR) | 40 (27) | 39 (27) | 40 (28) | 42 (28) | 42 (28) | .0001 |
| MGH race | White, N (%) | – | – | 9656 (72.3%) | 10,367 (72.0%) | 8827 (71.3%) | .181 |
| Black, N (%) | – | – | 1427 (10.7%) | 1566 (10.9%) | 1399 (11.3%) | .274 | |
| Asian, N (%) | – | – | 407 (3.1%) | 431 (3.0%) | 366 (3.0%) | .912 | |
| American Indian, N (%) | – | – | 52 (0.4%) | 35 (0.2%) | 49 (0.4%) | .048 | |
| Native Hawaiian, N (%) | – | – | 6 (0.04%) | 9 (0.06%) | 6 (0.05%) | .793 | |
| Other, N (%) | – | – | 886 (6.6%) | 1182 (8.2%) | 1075 (8.7%) | <.0001 | |
| Unavailable, N (%) | – | – | 924 (6.9%) | 800 (5.6%) | 660 (5.3%) | <.0001 | |
| MGH ethnicity | Not Hispanic, N (%) | – | – | 11,268 (84.4%) | 12,073 (83.9%) | 10,258 (82.9%) | .004 |
| Hispanic, N (%) | – | – | 1551 (11.6%) | 1743 (12.1%) | 1550 (12.5%) | .081 | |
| Unavailable, N (%) | – | – | 539 (4.0%) | 574 (4.0%) | 574 (4.6%) | .016 |
The bolded values are those with significant p values <0.05.
Overall, there was an increasing number of positive THC IA results at both BWH (p<.0001) and MGH (p<.0001) as legalization progressed. Furthermore, at BWH, the monthly positivity rates for each legalization time period increased from 18.0% in DEC (n=716) to 18.3% in MED BD (n=2327) to 21.4% in MED DISP (n=1629) to 23.2% (n=1220) in REC BD to 25.1% (n=1049) in REC DISP (Figure 1(A)). All p values between time-periods were <.0001, except for DEC to MED BD (p=.537), DEC to MED DISP (p=.002), MED BD to MED DISP (p=.0003), MED DISP to REC BD (p=.134), and REC BD to REC DISP (p=.071) (Supplemental Table 1).
Figure 1.
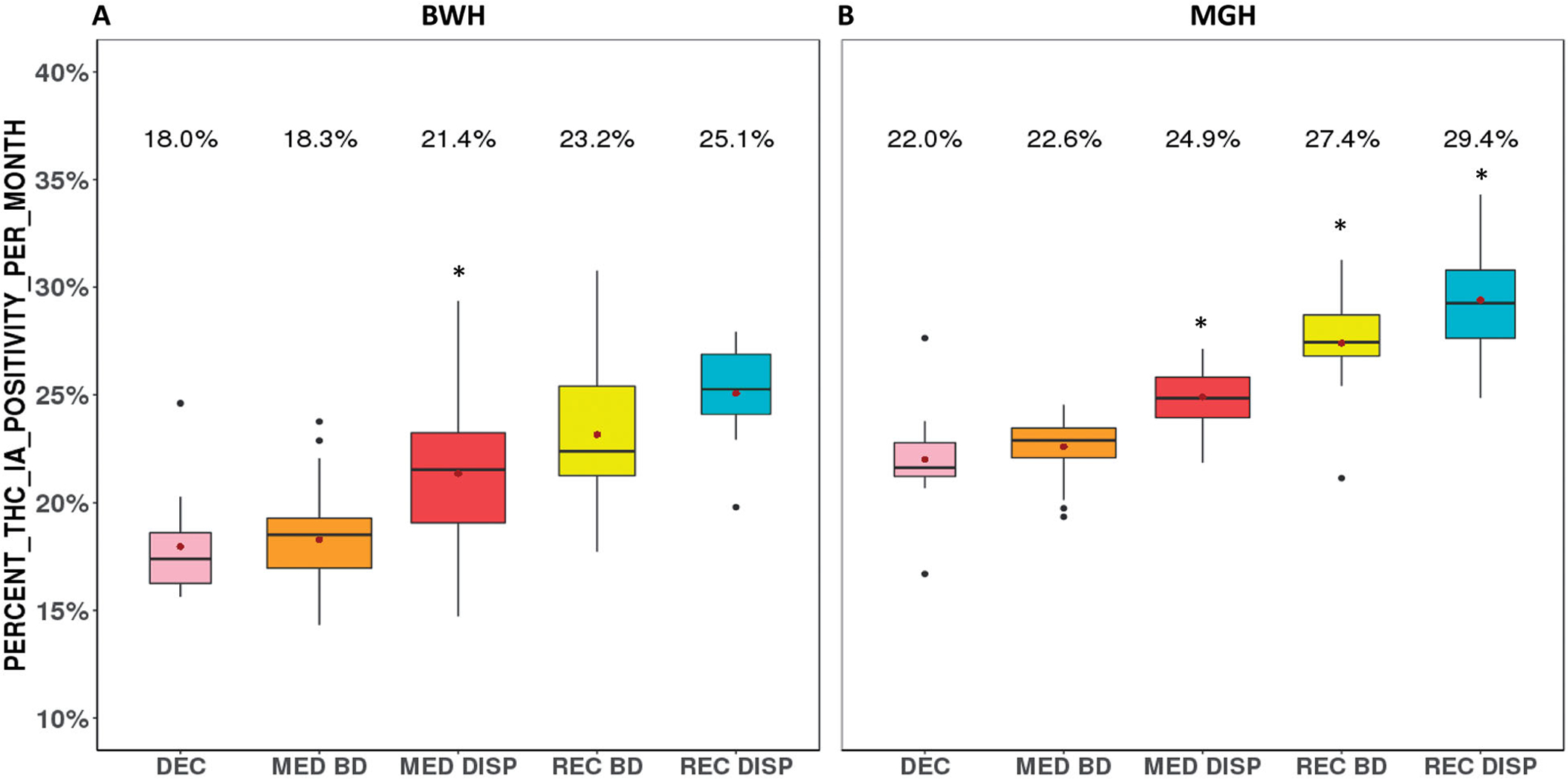
Rates of monthly THC IA positivity in ED as legalization progresses. The median, 25th and 75th percentile for monthly THC IA positivity is plotted for A) BWH and B) MGH from 2012 to 2019 for each time period of legalization. Where, from left to right, DEC = decriminalized; MED BD = before medical dispensaries; MED DISP = medical dispensaries available; REC BD = before recreational dispensaries; REC DISP = recreational dispensaries available. The mean positivity per month is displayed and indicated by the central point (●) and a significant change from the previous time period is indicated by the asterisk (*).
The THC IA positivity rates were higher for MGH as compared to BWH for all legalization periods (all p<.0001 with the exception of BWH DEC to MGH DEC (p=.002) and BWH REC BD to MGH REC BD (p=.0002) (Supplemental Table 2), but similarly increased from 22.0% (n=1393) in DEC to 22.6% (n=4706) in MED BD to 24.9% (4875) in MED DISP to 27.4% (n=3947) in REC BD to 29.4% (n=3673) in REC DISP (Figure 1(B)). All p values were <.0001, except for DEC to MED BD (p=.171), DEC to MED DISP (p=.0002), DEC to REC BD (p=.0001), and REC BD to REC DISP (p=.040) (Supplemental Table 1).
Certain demographics contributed more significantly to the increasing rates of THC IA positivity (Table 4). The positivity rate in females increased at both BWH (p=.002) and MGH (p=.003). There was also an increase in positivity in patients aged 30–39 (p<.0001 at BWH and MGH), aged 50–59 (p<.0001 MGH only), and aged >59 (p<.0001 at BWH and MGH) (Figure 2, Table 4). A decrease in positivity was seen in patients <18 (p<.0001 at MGH only), aged 18–29 (p<.0001 at BWH and MGH), aged 40–49 (p=.010 at BWH only), and aged 50–59 (p=.009 at BWH only) (Figure 2, Table 4). At MGH there was a decrease in positivity in White patients (p=.001) and non-Hispanic patients (p=.009) and increase in positivity in Hispanic patients (p=.009) and patient in income tertile 3 (the highest income) (p=.038). There were no significant trends in different races, ethnicities, or income tertiles at BWH (Table 4).
Table 4.
THC IA positivity at BWH and MGH as a function of gender, age, race, ethnicity, and income.
| Category | Demographic | DEC | MED BD | MED DISP | REC BD | REC DISP | p Value (trend) |
|---|---|---|---|---|---|---|---|
| BWH gender | Male, N (%) | 486 (67.9%) | 1443 (62.0%) | 980 (60.2%) | 728 (59.7%) | 631 (60.2%) | .002 |
| BWH age | <18, N (%) | 5 (0.7%) | 9 (0.4%) | 6 (0.4%) | 4 (0.3%) | 4 (0.4%) | .423 |
| 18–29, N (%) | 309 (43.2%) | 862 (37.0%) | 653 (40.1%) | 418 (34.3%) | 309 (29.5%) | <.0001 | |
| 30–39, N (%) | 126 (17.6%) | 525 (22.6%) | 394 (24.2%) | 302 (24.8%) | 297 (28.3%) | <.0001 | |
| 40–49, N (%) | 129 (18.0%) | 394 (16.9%) | 232 (14.2%) | 182 (14.9%) | 152 (14.5%) | .010 | |
| 50–59, N (%) | 115 (16.1%) | 403 (17.3%) | 217 (13.3%) | 183 (15.0%) | 143 (13.6%) | .009 | |
| >59, N (%) | 32 (4.5%) | 133(5.7%) | 111(6.9%) | 124(10.2%) | 137(13.2%) | <.0001 | |
| BWH race | White, N (%) | – | – | 767 (51.7%) | 572 (51.0%) | 545 (55.8%) | .068 |
| Black, N (%) | – | – | 520 (35.0%) | 378 (33.7%) | 307 (31.4%) | .066 | |
| Asian, N (%) | – | – | 17 (1.2%) | 18 (1.6%) | 16 (1.6%) | .283 | |
| American Indian, N (%) | – | – | 4 (0.3%) | 5 (0.5%) | 4 (0.4%) | .531 | |
| Native Hawaiian, N (%) | – | – | 2 (0.1%) | 2 (0.2%) | 0 (0.0%) | .380 | |
| Other, N (%) | – | – | 174 (11.7%) | 147 (13.1%) | 105 (10.8%) | .582 | |
| Unavailable, N (%) | – | – | 145 (8.9%) | 98 (8.0%) | 72 (6.9%) | <.0001 | |
| BWH ethnicity | Not Hispanic, N (%) | – | – | 1221 (79.1%) | 917 (78.9%) | 828 (81.9%) | .113 |
| Hispanic, N (%) | – | – | 322 (20.9%) | 245 (21.1%) | 183 (18.1%) | .113 | |
| Unavailable,N (%) | – | – | 86 (5.3%) | 58 (4.8%) | 38 (3.6%) | <.0001 | |
| BWH income | Tertile 1 (lowest), N (%) | – | – | 844(54.9%) | 622(54.1%) | 490 (50.9%) | .065 |
| Tertile 2, N (%) | – | – | 441(28.7%) | 343 (29.9%) | 288 (29.9%) | .468 | |
| Tertile 3 (highest), N (%) | – | – | 253 (16.5%) | 184 (16.0%) | 184 (19.1%) | .116 | |
| BWH other drug positivity | Amphetamine, N (%) | – | – | 124(7.6%) | 112 (9.2%) | 125 (11.9%) | <.0001 |
| Benzodiazepine, N (%) | – | – | 305 (18.7%) | 229 (18.8%) | 208 (19.8%) | .502 | |
| Cocaine, N (%) | – | – | 357 (21.9%) | 287 (23.5%) | 229 (21.8%) | .929 | |
| Fentanyl, N (%) | – | – | 163 (23.3%) | 278 (22.8%) | 235 (22.4%) | .667 | |
| Methadone, N (%) | – | – | 75 (4.6%) | 54 (4.4%) | 58 (5.5%) | .320 | |
| Opiates, N (%) | – | – | 306 (18.8%) | 159 (13.0%) | 126 (12.0%) | <.0001 | |
| Oxycodone, N (%) | – | – | 83 (5.1%) | 65 (5.3%) | 51 (4.9%) | .831 | |
| MGH gender | Male, N (%) | 981 (70.4%) | 3234 (68.7%) | 3349 (68.7%) | 2669 (67.6%) | 2442 (66.5%) | .003 |
| MGH age | <18, N (%) | 82 (5.9%) | 277 (5.9%) | 197 (4.0%) | 138 (3.5%) | 156 (4.3%) | <.0001 |
| 18–29, N (%) | 628 (45.1%) | 1876 (39.9%) | 1774 (36.4%) | 1307 (33.1%) | 1108 (30.2%) | <.0001 | |
| 30–39, N (%) | 270 (19.4%) | 1072 (22.8%) | 1227 (25.2%) | 1025 (26.0%) | 998 (27.2%) | <.0001 | |
| 40–49, N (%) | 230 (16.5%) | 774 (16.5%) | 756 (15.5%) | 645 (16.3%) | 606 (16.5%) | .904 | |
| 50–59, N (%) | 136 (9.8%) | 516 (11.0%) | 642 (13.2%) | 547 (13.9%) | 488 (13.3%) | <.0001 | |
| >59, N (%) | 45(3.2%) | 182 (3.9%) | 275 (5.7%) | 281 (7.1%) | 313(8.5%) | <.0001 | |
| MGH race | White, N (%) | – | – | 2366 (76.0%) | 2813 (75.3%) | 2522 (72.6%) | .001 |
| Black, N (%) | – | – | 470 (15.1%) | 583 (15.6%) | 576 (16.6%) | .099 | |
| Asian, N (%) | – | – | 58 (1.9%) | 63 (1.7%) | 61 (1.8%) | .750 | |
| American Indian, N (%) | – | – | 18 (0.6%) | 13 (0.4%) | 20 (0.6%) | .971 | |
| Native Hawaiian, N (%) | – | – | 2 (0.06%) | 5 (0.1%) | 0 (0.0%) | .287 | |
| Other, N (%) | – | – | 199 (6.4%) | 257 (6.9%) | 297 (8.5%) | .001 | |
| Unavailable, N (%) | – | – | 248 (7.4%) | 213 (5.4%) | 197 (5.4%) | <.0001 | |
| MGH ethnicity | Not Hispanic, N (%) | – | – | 2840 (88.2%) | 3339 (88.9%) | 3010(86.2%) | .009 |
| Hispanic, N (%) | – | – | 379 (11.8%) | 419 (11.2%) | 482 (13.8%) | .009 | |
| Unavailable, N (%) | – | – | 142 (4.2%) | 189 (4.8%) | 181 (4.9%) | .166 | |
| MGH income | Tertile 1 (lowest), N (%) | – | – | 1323(43.0%) | 1503 (41.0%) | 1385 (41.0%) | .115 |
| Tertile 2, N (%) | – | – | 874 (28.4%) | 1027(28.0%) | 944 (28.0%) | .697 | |
| Tertile 3 (highest), N (%) | – | – | 881 (28.6%) | 1135 (31.0%) | 1048(31.0%) | .038 | |
| MGH other drug positivity | Amphetamine, N (%) | – | – | 336 (10.0%) | 444 (11.3%) | 429 (11.7%) | .025 |
| Barbiturate, N (%) | – | – | 73 (2.2%) | 64 (1.6%) | 76 (2.1%) | .792 | |
| Benzodiazepine, N (%) | – | – | 880 (26.2%) | 873 (22.1%) | 769 (20.9%) | <.0001 | |
| Cocaine, N (%) | – | – | 840 (25.0%) | 1092 (27.7%) | 917 (25.0%) | .914 | |
| Opiates, N (%) | – | – | 457 (13.6%) | 383 (9.7%) | 287 (7.8%) | <.0001 |
The bolded values are those with significant p values <0.05.
Figure 2.
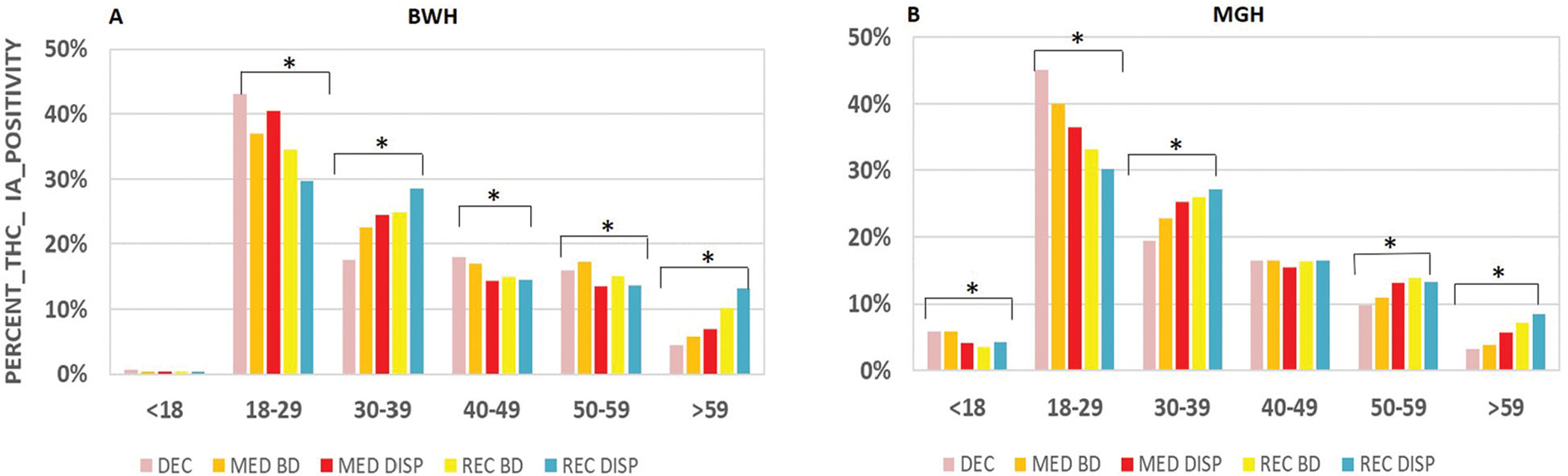
Trends in THC IA positivity in different age groups as legalization progresses. The percentage of positive THC IA results per legalization period per age groups is plotted for A) BWH and B) MGH. Where, from left to right, DEC = decriminalized; MED BD = medical before dispensaries; MED DISP = medical dispensaries available; REC BD = recreational before dispensaries; REC DISP = recreational dispensaries available. An asterisk (*) indicates a significant trend across the legalization periods.
Patients positive for THC were also positive for other drugs, most commonly benzodiazepines, cocaine, and fentanyl (Figure 3, Table 4). There was an increasing number of patients positive for both THC and amphetamine at BWH (p<.0001) and MGH (p=.025) and decreasing number of patients positive for both THC and opiates at BWH (p<.0001) and MGH (p<.0001) over the latter three legalization periods (MED DISP, REC BD, and REC DISP). MGH also had a decreasing number of patients positive for both THC and benzodiazepines (p<.0001).
Figure 3.
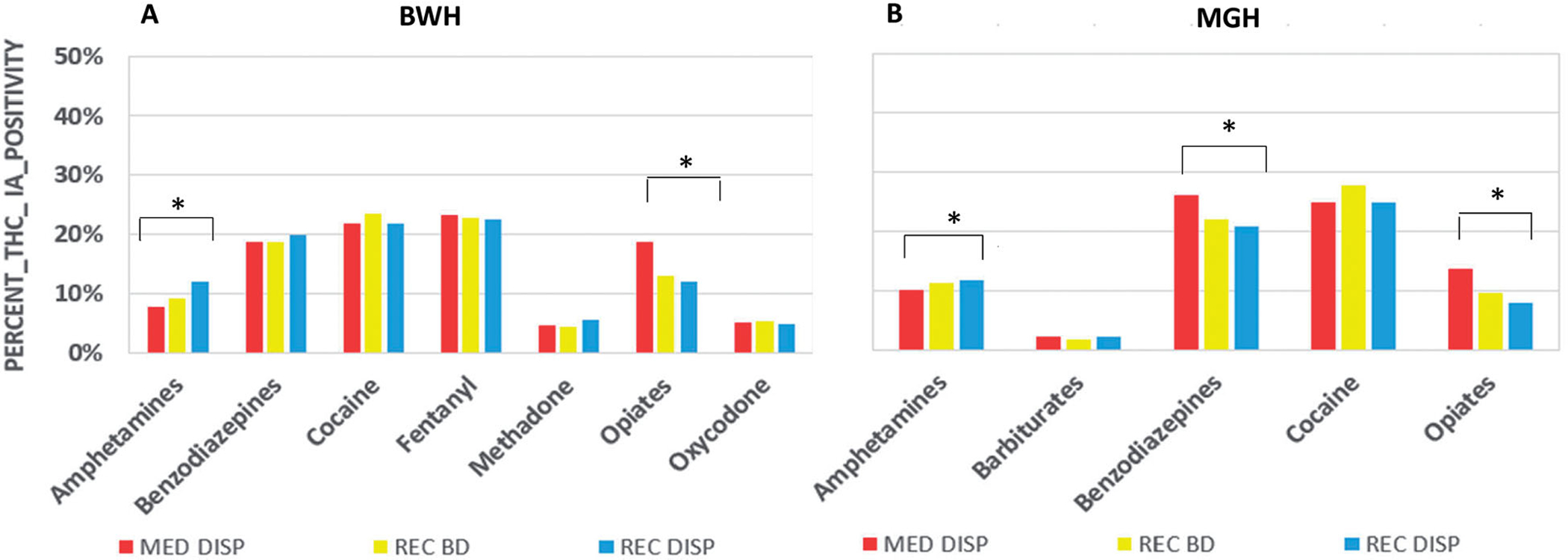
Trends in other drug positivity as legalization progresses. The percentage of positive results for other drugs in the UDS panel per legalization period is plotted for A) BWH and B) MGH. Where, from left to right, MED DISP = medical dispensaries available; REC BD = before recreational dispensaries; REC DISP= recreational dispensaries available. An asterisk (*) indicates a significant trend across the legalization periods.
Heatmap analysis
The patterns of positivity were similar at BWH and MGH (Figure 4). The heatmap revealed two common patterns. First, many patients have their first and only positive THC IA in a specific time period suggesting that individuals are increasing use after legalization in MA. The time periods vary but it is more common for patients to have their only positive THC IA in MED BD or MED DISP. Second, there are patients who were repeatedly and consistently positive throughout most of the periods. Further, most patients with more than one positive THC IA tended to be positive in other legalization periods.
Figure 4.
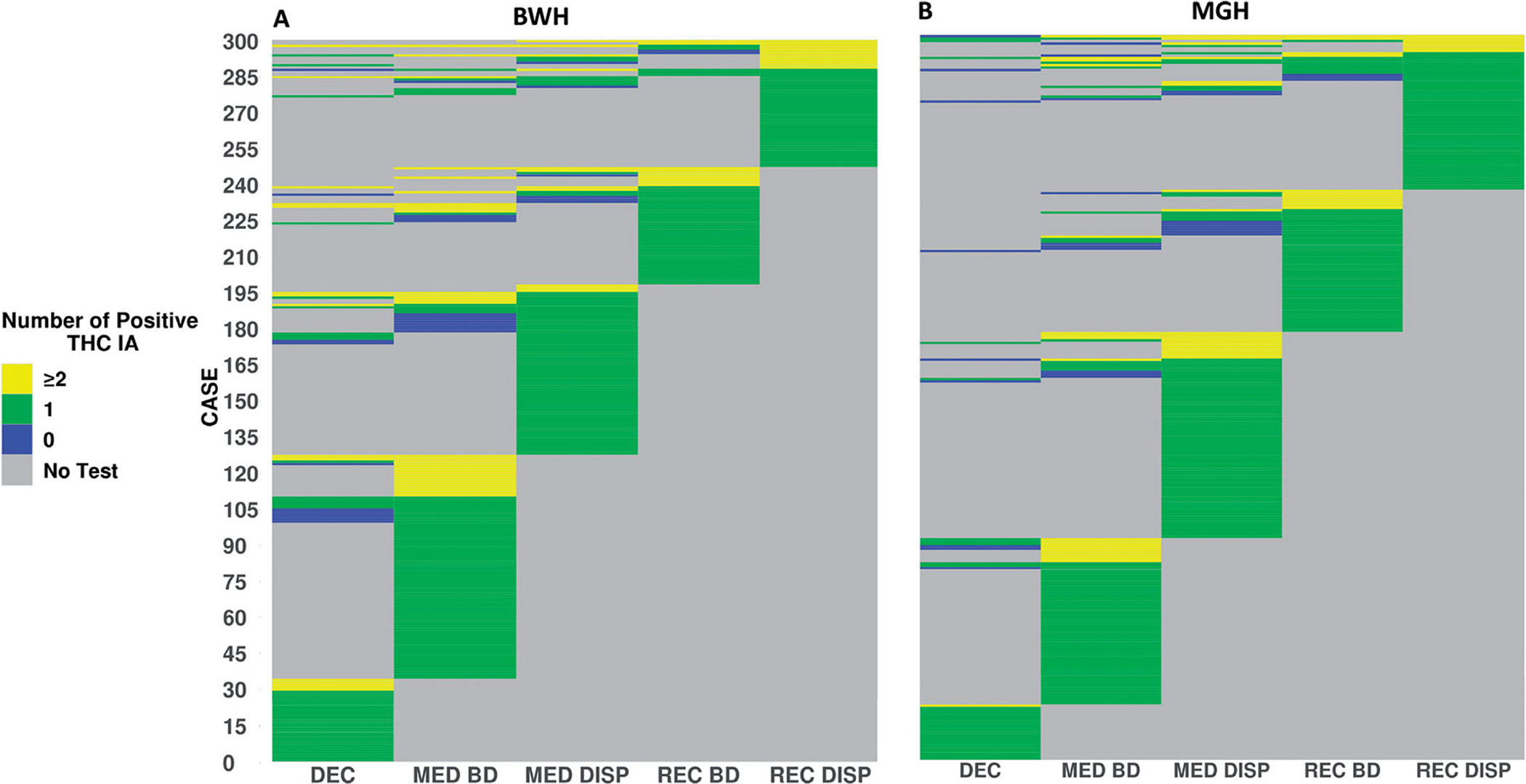
Heatmap of THC IA positivity per patient as legalization progresses. THC IA results from 300 random patients from A) BWH and B) MGH are plotted. Gray indicates that no THC IA testing was performed during the legalization period. Blue, green, and yellow indicate zero, one, ≥ two positive THC IA results, respectively. DEC: decriminalized; MED BD: before medical dispensaries; MED DISP: medical dispensaries available; REC BD: before recreational dispensaries; REC DISP: recreational dispensaries available.
Cannabis-related ICD-10 codes
Overall, there was an increase in number of cannabis-related ICD-10 codes at both BWH (p=.006) and MGH (p<.0001) per legalization period. Furthermore, monthly ICD-10 positivity rates at BWH increased from 0.6% (n=38) to 0.8% (n=39) to 1.0% (n=43) (Figure 5(A)). The p values for BWH were as follows: MED DISP to REC BD (p=.496), REC BD to REC DISP (p=.171), and MED DISP to REC DISP (p=.013) (Supplemental Table 1).
Figure 5.
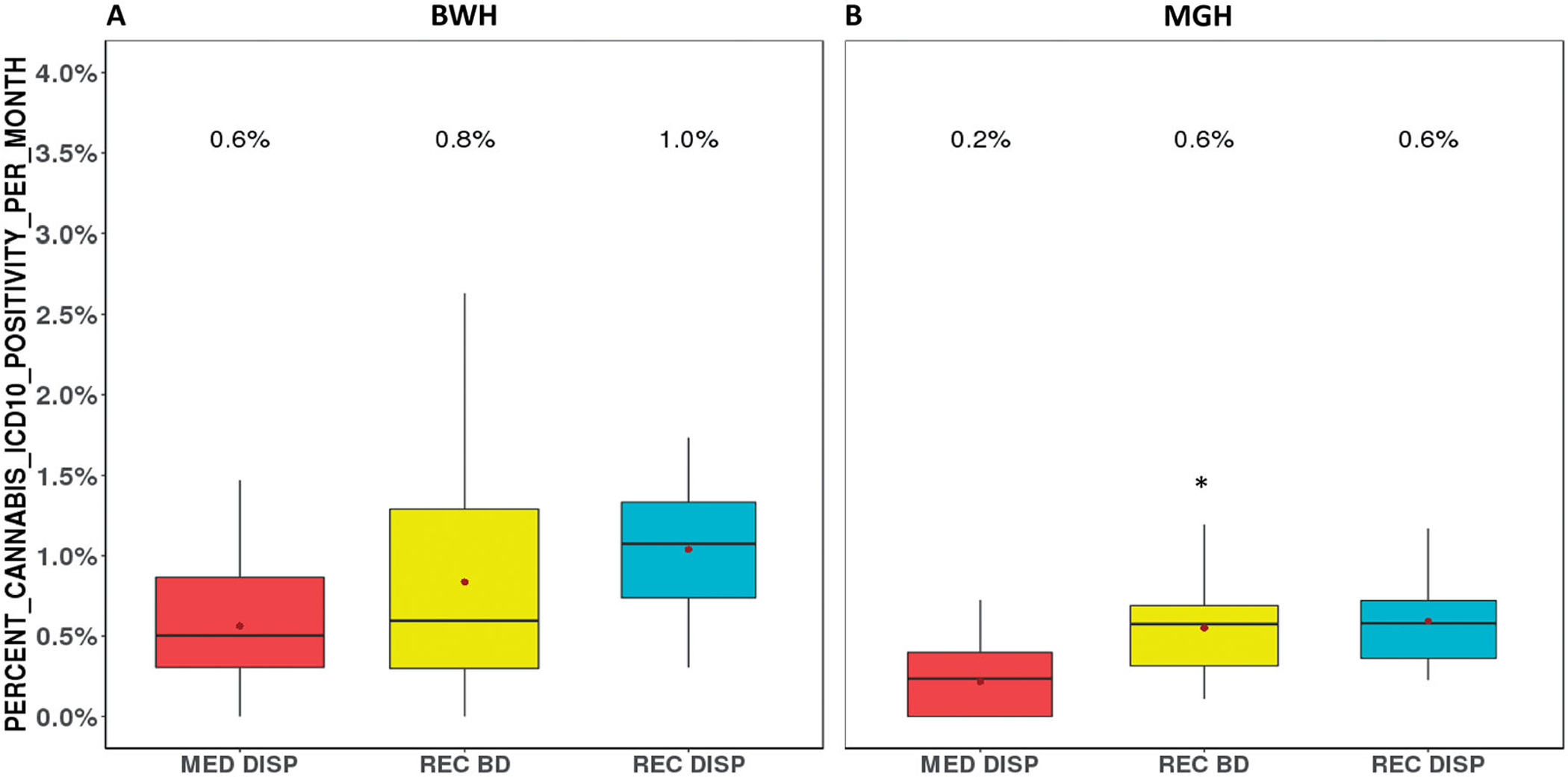
Rates of monthly THC ICD-10 positivity in ED as legalization progresses. The median, 25th and 75th percentile for monthly THC ICD-10 positivity is plotted for A) BWH and B) MGH from 2015 to 2019 (BWH) and 2016 to 2019 (MGH) for each time period of legalization. Where, from left to right, MED DISP = medical dispensaries available; REC BD = before recreational dispensaries; REC DISP= recreational dispensaries available. The mean positivity per month is displayed and indicated by a central point (●) and a significant difference from previous time period is indicated by an asterisk (*).
The ICD-10 code positivity rate was significantly higher at BWH (BWH MED DISP vs. MGH MED DISP (p=.006), BWH REC BD vs. MGH REC BD (p=.007), and BWH REC DISP vs. MGH REC DISP (p=.009) (Supplemental Table 2), but similarly increased from 0.2% (n=28) to 0.6% (n=74) to 0.6% (n=71) at MGH (Figure 5(B)). Significant differences were seen between MED DISP and REC BD (p=.008) and MED DISP and REC DISP (p=.002) at MGH (Supplemental Table 1). The difference between REC BD and REC DISP (p=.736) was not significant.
There were a limited number of significant increasing and decreasing trends in THC ICD-10 codes and results differed between BWH and MGH (Table 5). At BWH there was a decrease in positive cannabis-related ICD-10 codes in Blacks (p=.025) and in patients in income tertile 1 (lowest) (p=.040). The only significant trend at MGH was a decrease in patients aged 18–29 (p=.006).
Table 5.
ICD-10 positivity at BWH and MGH as function of gender, age, race, ethnicity, and income.
| Category | Demographic | MED DISP | REC BD | REC DISP | p Value (trend) |
|---|---|---|---|---|---|
| BWH gender | Male, N (%) | 15 (39.5%) | 20 (51.3%) | 24 (55.8%) | .147 |
| BWH age | <18, N (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | – |
| 18–29, N (%) | 21 (55.3%) | 12 (30.8%) | 16 (38.1%) | .132 | |
| 30–39, N (%) | 7 (18.4%) | 11 (28.2%) | 14 (33.3%) | .137 | |
| 40–49, N (%) | 5 (13.2%) | 2 (5.1%) | 5 (11.9%) | .881 | |
| 50–59, N (%) | 2 (5.3%) | 7 (18.0%) | 4 (9.5%) | .577 | |
| >59, N (%) | 3 (7.9%) | 7 (18.0%) | 3 (7.1%) | .876 | |
| BWH race | White, N (%) | 9 (25.7%) | 11 (32.4%) | 17 (41.5%) | .147 |
| Black, N (%) | 21 (60.0%) | 16 (47.1%) | 14 (34.2%) | .025 | |
| Asian, N (%) | 1 (2.9%) | 1 (2.9%) | 2 (4.9%) | .633 | |
| American Indian, N (%) | 0 (0.0%) | 0 (0.0%) | 1 (2.4%) | .254 | |
| Native Hawaiian, N (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | – | |
| Other, N (%) | 4 (11.4%) | 6 (17.7%) | 7 (15.5%) | .512 | |
| Unavailable, N (%) | 3 (7.9%) | 5 (12.8%) | 2 (4.7%) | .570 | |
| BWH ethnicity | Not Hispanic, N (%) | 30 (81.1%) | 26 (68.4%) | 30 (69.8%) | .273 |
| Hispanic, N (%) | 7 (18.9%) | 12 (31.6%) | 13 (30.2%) | .273 | |
| Unavailable, N (%) | 1 (2.6%) | 1 (2.6%) | 0 (0.0%) | .348 | |
| BWH income | Tertile 1 (lowest), N (%) | 26 (70.3%) | 24 (63.2%) | 20 (47.6%) | .040 |
| Tertile 2, N (%) | 10 (27.0%) | 9 (23.7%) | 16 (38.1%) | .270 | |
| Tertile 3 (highest), N (%) | 1 (2.7%) | 5 (13.2%) | 6 (14.3%) | .097 | |
| MGH gender | Male, N (%) | 14 (50.0%) | 50 (67.6%) | 36 (50.7%) | .540 |
| MGH age | <18, N (%) | 6 (21.4%) | 20 (27.0%) | 22 (31.0%) | .335 |
| 18–29, N (%) | 17 (60.7%) | 39 (52.7%) | 24 (33.8%) | .006 | |
| 30–39, N (%) | 0 (0.0%) | 9 (12.2%) | 9 (12.7%) | .116 | |
| 40–49, N (%) | 4 (14.3%) | 2 (2.7%) | 7 (9.9%) | .926 | |
| 50–59, N (%) | 1 (3.6%) | 3 (4.1%) | 6 (8.5%) | .253 | |
| >59, N (%) | 0 (0.0%) | 1 (1.4%) | 3 (4.2%) | .157 | |
| MGH race | White, N (%) | 18 (69.2%) | 48 (68.6%) | 42 (64.6%) | .612 |
| Black, N (%) | 3 (11.5%) | 11 (15.7%) | 9 (13.9%) | .892 | |
| Asian, N (%) | 1 (3.9%) | 1 (1.4%) | 0 (0.0%) | .139 | |
| American Indian, N (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | – | |
| Native Hawaiian, N (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | – | |
| Other, N (%) | 4 (15.4%) | 10 (14.3%) | 14 (21.5%) | .349 | |
| Unavailable, N (%) | 2 (7.1%) | 4 (5.4%) | 6 (8.5%) | .671 | |
| MGH ethnicity | Not Hispanic, N (%) | 19 (76.0%) | 57 (83.8%) | 46 (69.7%) | .241 |
| Hispanic, N (%) | 6 (24.0%) | 11 (16.2%) | 20 (30.3%) | .241 | |
| Unavailable, N (%) | 3 (10.7%) | 6 (8.1%) | 5 (7.0%) | .565 | |
| MGH income | Tertile 1 (lowest), N (%) | 13 (48.2%) | 32 (46.4%) | 32 (51.6%) | .667 |
| Tertile 2, N (%) | 7 (25.9%) | 15 (21.7%) | 15 (24.2%) | .959 | |
| Tertile 3 (highest), N (%) | 7 (25.9%) | 22 (31.9%) | 15 (24.2%) | .666 |
The bolded values are those with significant p values <0.05.
Discussion
We report an increase in positivity in both THC IA and cannabis-related ICD-10 codes at our hospital EDs as legalization has progressed in Boston, MA. Positivity rates increased by 7% for THC IA and 0.4% for ICD-10 codes across both institutions. However, the percentage of positivity in THC IA differed significantly between our two institutions across all five periods of legalization.
To our knowledge, this is the first and longest duration study to determine THC IA positivity rates across five major time periods of legalization, including before and after the opening of dispensaries, at two large hospital EDs. Importantly, the analysis occurs over the span of 8 years allowing us to accurately determine dynamic trends as well as positivity rates between legalization periods. Most other studies focus on the latter and only determine changes between one or two legalization periods as opposed to the five analyzed in our study.
Although positivity rates were significantly higher at MGH, trends in positivity and patient populations responsible for increasing positivity were similar at both institutions. Adult patients in their 20s aging into their 30s with continued use could explain the increase seen in patients aged 30–39 years. Older adults also had increasing use; a pattern seen nationwide [22]. The increase in older adults may be explained by the “baby-boomer” generation (born 1946–1964) retiring and re-engaging in recreational drug use. Older patients are also more likely to have chronic disease, depression, anxiety, loss of appetite or weight loss, sleeping disorders, and cancer-related illnesses which are common indications for medicinal cannabis use [22]. Interestingly, we did not find many significant and consistent trends in THC IA positivity by race, ethnicity, or level of income. At MGH, there was an increase in positivity in Hispanic patients and patients in the highest income tertile; the latter suggesting the legalization may be a driver for use in wealthier patients. However, no significant trends were seen at BWH making it difficult to generalize our findings.
Marijuana is frequently referred to as a “gateway” drug and opponents of marijuana legalization are concerned that its legalization will increase the use of illicit drugs, such as heroin, cocaine, and fentanyl. Epidemiological data demonstrate that there is considerable variation among cannabis use and its relationship to other substances of abuse [23]. Post-legalization in Arizona, patients who used cannabis were 2.3 times more likely to have a positive UDS for cocaine or amphetamines and 1.57 times more likely to be positive for ethanol (>80 mg/dL) [4]. However, in Louisiana the increasing prevalence of both marijuana and opiate, as determined by positive UDS, was unrelated to legalization [24]. At our institutions, the increase in THC IA positivity was not associated with increasing rates of cocaine, fentanyl, or opiate use suggesting that THC is not a “gateway” drug. In fact, opiate use (e.g., morphine and codeine) decreased at both institutions. Similar to the study by Levine et al. [4], there was an increase in amphetamine use at both BWH and MGH but the etiology of increased amphetamine detection is unclear. One plausible explanation may be that there was an increasing distribution of prescription amphetamines used to treat medical illnesses [25]. Another explanation may be the increasing rates of methamphetamine use in MA over the study period [26]. Benzodiazepine use decreased at MGH but, for unclear reasons, did not change at BWH.
A 2-dimensional heatmap, to our knowledge, has not been used previously to display THC use patterns and provided unique insight. According to the heatmap, there is no one particular stage of legalization responsible for the increase in THC use. The additional patients’ positive in MED BD and MED DISP may be explained by the longer time window for those legalization periods. Instead, there is a steady increase unrelated to the type of legalization (e.g., medical or recreational) or availability of dispensaries; a finding also seen in Arizona [4]. These steady increases may be due to changes in an individuals’ legal risk tolerance at certain legalization periods. For some patients, legalization of medical marijuana may be sufficient to justify their recreational use as they perceive minimal risk. Further, the heatmap reveals a group of patients that are “frequent ED users” and consistently positive throughout many legalization periods.
Similar to other studies, the positivity rates for ICD-10 codes were low [12] with BWH increasing from 0.6 to 1.0% and MGH increasing from 0.2 to 0.6%. Baraniecki et al. [12] reported a positivity rate of 0.6% in the ED over a 12-month period. The small numbers make it challenging to identify significant trends in positivity in specific demographics. Unlike THC IA, the rates of ICD-10 positivity were significantly higher at BWH suggesting a different threshold for utilizing cannabis-related ICD-10 codes at each institution. Although ICD-10 codes should be more reflective of acute THC intoxication or associated side effects, the subjectivity of ICD-10 codes and relatively low use suggest that THC IA may be a better indicator of cannabis use in patients presenting to the ED.
ED operations and resources will likely be impacted by the steady the increase in cannabis use associated with legalization. In addition, the potency of marijuana has increased dramatically over the past several decades which may lead to more acute intoxications and long- term side effects [27,28]. Edible marijuana is also commonly ingested, particularly in adolescents. However, cannabis use in patients <18 years decreased significantly at MGH and did not change at BWH. States that have progressed toward legalization should be prepared to manage an increasing number of ED patients with cannabis-associated cyclical vomiting or hyperemesis, trauma, neuropsychiatric disorders, and burn injuries. Hospital admission rates may also increase because of cannabis-related ED visits. Based on our study, EDs should not necessarily anticipate an increase in use of illicit drugs in patients concomitantly using THC.
Limitations
Our study was performed at two large academic medical centers in Boston, MA and while it demonstrated important regional differences in THC use, this may not be generalizable throughout the state or nationally. It is important to consider that we did not exclude patients on drugs, such as dronabinol, efavirenz, or pantoprazole which may rarely cause false-positive THC IA results. Furthermore, the THC IA used for clinical testing does not detect CBD or synthetic cannabinoids and would not reflect the use of these drugs in our patient population, as opposed to more general ICD-10 coding. Further, UDS are unable to determine which patients were intoxicated or impaired with marijuana during their ED visit. The half-life of cannabinoids in urine ranges from 4 to 27 d and depends on multiple factors including frequency and amount of use [1]. For several data points (e.g., ICD-10, race, and ethnicity), we were not able to obtain data prior to the new EHR implementation. We did not analyze serum toxicology results (e.g., ethanol). The UDS panels were also different at BWH and MGH and our conclusions on fentanyl, oxycodone, and methadone were based on BWH data, albeit a large dataset. Finally, we used different cutoffs for urine THC IA at BWH and MGH which may explain significantly higher positivity rates at MGH. However, the patterns of positivity were similar suggesting the use of different cutoffs had minimal impact on the conclusions.
Conclusion
Legalization of marijuana in MA has led to an increase in cannabis use as indicated by both increasing rates of positive THC IA results, particularly in older adults, as well as increasing cannabis-related ICD-10 codes. To our knowledge, this is the first and longest duration study to determine THC IA positivity rates across five major time periods of legalization in MA at two large hospital EDs. Data suggest a steady increase in THC use, as opposed to a spike associated with a certain legalization status, that was not associated with an increase in opiates, fentanyl, or cocaine use. Based on our study results, we recommend using THC IA positivity, an objective laboratory measure, to monitor THC use and the impact of state-based progression in cannabis legalization on ED resources and patient outcomes. Further, it is important to monitor THC IA positivity over several years and multiple legalization periods to accurately determine these dynamic trends and impact on patients presenting to EDs.
Supplementary Material
Funding
This work was supported by National Institutes of Health. PRC/TBE funded by NIH R44DA051106. PRC is funded by NIH K23DA044874, the Hans and Mavis Lopater Psychosocial Foundation and Defense Advanced Research Projects Agency.
Footnotes
Supplemental data for this article can be accessed here.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Grigorian A, Lester E, Lekawa M, et al. Marijuana use and outcomes in adult and pediatric trauma patients after legalization in California. Am J Surg. 2019;218(6):1189–1194. [DOI] [PubMed] [Google Scholar]
- [2].Aggarwal SK, Carter GT, Sullivan MD, et al. Medicinal use of cannabis in the United States: historical perspectives, current trends, and future directions. J Opioid Manag. 2009;5(3):153–168. [DOI] [PubMed] [Google Scholar]
- [3].NCSL.org. [Internet]. Washington (DC): NCSL; [cited 2021. Aug 11]. Available from: https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx [Google Scholar]
- [4].Levine M, Jontz A, Dabrowski P, et al. Prevalence of marijuana use among trauma patients before and after legalization of medical marijuana: the Arizona experience. Subst Abus. 2021;42(3): 366–371. [DOI] [PubMed] [Google Scholar]
- [5].Hammond CJ, Chaney A, Hendrickson B, et al. Cannabis use among US adolescents in the era of marijuana legalization: a review of changing use patterns, comorbidity, and health correlates. Int Rev Psychiatry. 2020;32(3):221–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Claudius IA, Jontz A, Levine M, et al. Marijuana self-report compared with testing in trauma patients before and after legalization. Clin Toxicol. 2020;58(8):801–803. [DOI] [PubMed] [Google Scholar]
- [7].Whitehill JM, Harrington C, Lang CJ, et al. Incidence of pediatric cannabis exposure among children and teenagers aged 0 to 19 years before and after medical marijuana legalization in Massachusetts. JAMA Netw Open. 2019;2(8):e199456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Roberts B Legalized cannabis in Colorado emergency departments: a cautionary review of negative health and safety effects. West J Emerg Med. 2019;20(4):557–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hall KE, Monte AA, Chang T, et al. Mental health–related emergency department visits associated with cannabis in Colorado. Bird SB, editor. Acad Emerg Med. 2018;25(5):526–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Wang GS, Davies SD, Halmo LS, et al. Impact of marijuana legalization in Colorado on adolescent emergency and urgent care visits. J Adolesc Health. 2018;63(2):239–241. [DOI] [PubMed] [Google Scholar]
- [11].Cerdá M, Mauro C, Hamilton A, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2020;77(2):165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Baraniecki R, Panchal P, Malhotra DD, et al. Acute cannabis intoxication in the emergency department: the effect of legalization. BMC Emerg Med. 2021;21(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Monte AA, Zane RD, Heard KJ. The implications of marijuana legalization in Colorado. JAMA. 2015;313(3):241–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].SAMHSA.gov. [Internet]. Rockville (MD): SAMHSA; [cited 2021. Aug 2]. Available from: https://www.samhsa.gov/data/report/2018-2019-nsduh-state-specific-tables [Google Scholar]
- [15].Boston.com. [Internet]. Boston (MA): The Boston Globe; [cited 2021. Sep 2]; Available from: http://archive.boston.com/news/local/articles/2008/11/05/voters_approve_marijuana_law_change/ [Google Scholar]
- [16].Boston.com. [Internet]. Boston (MA): The Boston Globe; [cited 2021. Sep 2]. Available from: https://www.boston.com/uncategorized/noprimarytagmatch/2012/11/06/massachusetts-voters-approve-ballot-measure-to-legalize-medical-marijuana/ [Google Scholar]
- [17].Lazar K, Staff VHG, Correspondent G, et al. At Salem medical marijuana dispensary, a sense of relief - The Boston Globe [Internet]. BostonGlobe.com. 2015. Jun 24 [cited 2021 Sep 2]; Metro:[about 5 screens]. Available from: https://www.bostonglobe.com/metro/2015/06/24/patients-line-first-medical-marijuana-dispensary-opens/ocV8KMa9oVpYNvAhZwhqWJ/story.html [Google Scholar]
- [18].Boston.com. [Internet]. Boston (MA): The Boston Globe; [cited 2021. Sep 2]. Available from: https://www.boston.com/news/politics/2017/07/28/charlie-baker-signs-bill-making-changes-to-marijuana-law/ [Google Scholar]
- [19].Boston.com. [Internet]. Boston (MA): The Boston Globe; [cited 2021. Sep 2]. Available from: https://www.boston.com/news/local-news/2018/11/20/massachusetts-recreational-marijuana-dispensaries-opening-day/ [Google Scholar]
- [20].USA.com. [Internet]. Basking Ridge (NJ): USA.com; [cited 2021. Aug 2]. Available from: http://www.usa.com/rank/massachusetts-state-median-household-income-zip-code-rank.htm [Google Scholar]
- [21].DenverPublicHealth.org. [Internet]. Denver (CO): Denver Public Health and Denver Department of Public Health and Environment; [cited 2021. Aug 11]. Available from: https://www.denverpublichealth.org/-/media/dph-files-and-docs/health-info-and-reports/mj-trendanalysis-2012-2017-final-branded.pdf [Google Scholar]
- [22].Han BH, Sherman S, Mauro PM, et al. Demographic trends among older cannabis users in the United States, 2006–13. Addict Abingdon Engl. 2017;112(3):516–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Jorgensen C, Wells J. Is marijuana really a gateway drug? A nationally representative test of the marijuana gateway hypothesis using a propensity score matching design. J Exp Criminol. 2021. [Internet]. [cited 2021 Aug 11]; Available from: 10.1007/s11292-021-09464-z. [DOI] [Google Scholar]
- [24].Korneeva N, Cvek U, Leskova A, et al. Urine drug screen trends from 1998 through 2011 among emergency department patients treated in a university teaching hospital. Toxicol Commun. 2018; 2(1):24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Piper BJ, Ogden CL, Simoyan OM, et al. Trends in use of prescription stimulants in the United States and territories, 2006 to 2016. PLoS One. 2018;13(11):e0206100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wakeman S, Flood J, Ciccarone D. Rise in presence of methamphetamine in oral fluid toxicology tests among outpatients in a large healthcare setting in the northeast. J Addict Med. 2021; 15(1):85–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Cash MC, Cunnane K, Fan C, et al. Mapping cannabis potency in medical and recreational programs in the United States. PLoS One. 2020;15(3):e0230167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Chandra S, Radwan MM, Majumdar CG, et al. New trends in cannabis potency in USA and Europe during the last decade (2008–2017). Eur Arch Psychiatry Clin Neurosci. 2019;269(1): 5–15. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


