Abstract
Objective:
Interpersonal negative life events (NLEs) have been linked to risk for suicidal thoughts and behaviors. However, little is known about how this risk is conferred over the short term and the mechanisms linking interpersonal NLEs to suicide risk, particularly in adolescents. This study used an intensive longitudinal design to examine thwarted belongingness with family and friends as potential mechanisms linking interpersonal NLEs to suicidal thoughts.
Method:
Forty-eight adolescents (Mage = 14.96 years; 64.6% female, 77.1% White), who recently received acute psychiatric care for suicide risk, were followed intensely for 28 days after discharge. Smartphone-based ecological momentary assessment was used to measure presence of interpersonal NLEs at the day level, fluctuations in thwarted belongingness with family and friends (separately) within day, and fluctuations in suicidal thoughts within day. A multi-level structural equation model was utilized to examine family thwarted belongingness and friend thwarted belongingness as parallel mediators in the relationship between interpersonal NLEs and next-day suicidal thoughts.
Results:
Significant direct effects were observed between interpersonal NLEs and family thwarted belongingness, family thwarted belongingness and suicidal thoughts, and friend thwarted belongingness and suicidal thoughts. In addition, family, but not friend, thwarted belongingness significantly mediated the association between interpersonal NLEs and next-day suicidal thoughts.
Conclusions:
Interpersonal NLEs predicted greater suicidal thoughts over the short term (next day) in high-risk adolescents. Findings suggest how interpersonal NLEs may confer risk for suicidal thoughts—by reducing feelings of family belongingness. Future research is needed to examine how modifying belongingness may reduce suicide risk in adolescents.
Keywords: adolescent, belongingness, ecological momentary assessment, stress, suicide ideation
Suicidal thoughts and behaviors (STBs) are a major public health concern among adolescents. STBs are related to significant academic and social impairment (Copeland et al., 2017; Foley et al., 2006) and confer risk for suicide death (Ribeiro et al., 2016). Suicidal thoughts typically begin during the transition to adolescence and rates increase significantly during this developmental period (Nock et al., 2008; Nock et al., 2013). Moreover, for about a third of adolescents, escalation from suicidal thoughts to suicide attempts (i.e., deliberate, self-inflicted injury with at least some intent to die; Silverman et al., 2007) will occur within one to two years after the onset of suicidal thoughts (Glenn et al., 2017; Nock et al., 2008; Nock et al., 2013). Recent estimates from the Centers for Disease Control and Prevention’s 2019 Youth Risk Behavior Survey suggest that approximately 19% of high school students thought about suicide in the past year and 9% attempted suicide at least once (Ivey-Stephenson et al., 2020). Alarmingly, STB-related hospitalizations have doubled for youth over the past decade (Plemmons et al., 2018).
Effective suicide prevention for youth will require a range of upstream (i.e., build protective factors) and downstream (i.e., crisis intervention) approaches (JED Foundation, 2017; Suicide Prevention Resource Center, 2020). To enhance downstream suicide prevention approaches, the field needs knowledge about when youth are most at risk and what factors may be modifiable during this time to reduce risk. Although considerable research has aimed to identify potential suicide risk factors (Franklin et al., 2017), this work has been limited in its examination of short-term risk factors and high-risk periods (Glenn & Nock, 2014). For instance, one of the highest risk periods for suicidal behavior and suicide-related rehospitalizations is the month following discharge from psychiatric hospitalization (Chung et al., 2017). This also is a time period with significant fluctuations in suicide ideation among adolescents (Prinstein et al., 2008). However, far less is known about how risk is conferred during the post-hospitalization period. One factor that has been related to suicide risk, and may help to clarify risk processes during this time, is the presence of negative life events (NLEs), specifically interpersonal NLEs.
Interpersonal negative life events and suicide risk
NLEs have been linked to risk for STBs across the lifespan (Liu & Miller, 2014). The range of NLEs that have been associated with STBs can be broadly categorized as either interpersonal (e.g., loss, difficulties or conflict with family, friends, and romantic partners) or non-interpersonal events (e.g., health, financial, legal). This distinction between interpersonal and non-interpersonal NLEs is important given research indicating that interpersonal NLEs are robustly related to suicide risk (Bagge et al., 2013; Brent et al., 1993; Liu & Miller, 2014; Stewart et al., 2019). Among adolescents, interpersonal NLEs related to family (e.g., conflict, rejection), peers (e.g., rejection, exclusion, victimization), and romantic partners (e.g., relationship break-ups) are the most strongly linked to STBs (Beautrais et al., 1997; Cheek, Goldston, et al., 2020; Fergusson et al., 2000; Holt et al., 2015).
Interpersonal NLEs may play a particularly important role in adolescents’ risk for STBs, due to the socioemotional changes that normatively occur during this developmental period. Specifically, adolescence is marked by significant changes in social salience and peer relationships, including increased desire for affiliation and belonging with peers, as well as greater sensitivity to social evaluation and rejection (Crone & Dahl, 2012; Crosnoe & Johnson, 2011; Powers et al., 2013; Santor et al., 2000; Somerville, 2013). There also is a normative increase in parent-child conflict as adolescents develop increased autonomy and their own identity, separate from that of their parents (Crosnoe & Johnson, 2011; Laursen & Collins, 2009).
To date, most studies examining the link between interpersonal NLEs and STBs have been cross-sectional or examined the association over long follow-up periods (Cheek, Reiter-Lavery, et al., 2020)—a limitation of most suicide risk factor research (Franklin et al., 2017). However, growing evidence suggests that interpersonal NLEs may confer risk for STBs over the short term. For instance, longitudinal studies indicate that interpersonal NLEs are common in the month prior to a suicide attempt in adults (Yen et al., 2005) and adolescents (Cheek, Goldston, et al., 2020). Even more proximal to suicidal behavior, one study using an intensive Timeline Followback methodology with adults found that interpersonal NLEs were more common on the day a suicide attempt occurred, compared to the day before, when all distal risk factors were the same for that individual, but they did not attempt suicide (Bagge et al., 2013). In addition, a recent daily diary study (i.e., one daily assessment) with adults found that NLEs (both interpersonal and non-interpersonal) were contemporaneously related to greater suicidal thoughts that day (Franz et al., 2021). Greater temporal resolution comes from an ecological momentary assessment (EMA) study with adults finding that family NLEs, but not general NLEs, predicted greater suicide ideation that day (Husky et al., 2017). However, this level of temporal sensitivity (i.e., examining how NLEs relate to STB risk over the subsequent hours and day) has not been examined in youth.
Although there is some evidence linking interpersonal NLEs to suicide risk in adolescents, significant gaps still exist. First, as noted above, research in youth has examined these associations over long periods of time, such as assessment of lifetime NLEs or predicting subsequent STBs over months to years (Cheek, Reiter-Lavery, et al., 2020). Therefore, far less is known about how interpersonal NLEs relate to STBs over short time periods. Second, whereas there is some research exploring factors that may moderate the impact of NLEs on suicidal thoughts among adults (e.g., greater reappraisal and expressive suppression decrease risk for suicidal thoughts among those who experience stress; Franz et al., 2021), these mechanisms are understudied and poorly understood, particularly among adolescents. Elucidating these risk mechanisms has implications for understanding the development of STBs, as well as informing effective intervention and prevention efforts. Notably, this line of research is consistent with the National Institute of Mental Health’s experimental therapeutics approach (Gordon, 2017), which aims to identify factors that cause and maintain psychopathology to directly intervene on those mechanisms to improve clinical outcomes.
Belongingness and the link between interpersonal NLEs and suicide risk
Belongingness, or connectedness, may be one potential mediator, or mechanism, by which interpersonal NLEs confer risk for STBs in adolescents. The ability to satisfy our basic psychological need to form social connections and to belong has significant implications for health and well-being (Baumeister & Leary, 1995). Connectedness has been conceptualized to include subjective (i.e., feeling satisfied in interpersonal relationships and social groups) and structural components (i.e., social networks and integration; Holt-Lunstad et al., 2017; Townsend & McWhirter, 2005; Whitlock et al., 2014). Although connectedness/belongingness has not been examined in longitudinal research as a mechanism linking interpersonal NLEs to STBs, there is converging research to suggest that it may, at least partially, mediate this association. Separate research literatures have found that: (1) interpersonal NLEs lead to reduced connectedness/thwarted belongingness, (2) reduced connectedness/thwarted belongingness is related to increased risk for STBs, and (3) loneliness mediates (in cross-sectional research) the association between interpersonal stress and a range of negative outcomes. Each will be discussed briefly in turn.
First, several lines of research indicate that interpersonal NLEs lead to social disconnection or reduced belonging. Studies using lab-based social rejection paradigms have found that rejection reduces feelings of belongingness and social connection (Gerber & Wheeler, 2009; Hartgerink et al., 2015), including among early adolescents (Ruggieri et al., 2013). Experiences of social rejection in the real world also impact belongingness among youth. Parental and peer rejection, including peer victimization, lead to feelings of loneliness among adolescents (Asher & Paquette, 2003; Baker & Bugay, 2011; Ferguson & Zimmer-Gembeck, 2014). In addition, online experiences of ostracism or rejection can negatively impact youth’s sense of belonging and connectedness (Allen et al., 2014).
Second, conceptual and empirical work have linked thwarted belongingness, or reduced connectedness, to greater risk for STBs. Building on early sociological theories of suicide positing the key role of social disintegration (Durkheim, 1897/1951), contemporary theories of suicide include thwarted belongingness, or reduced connectedness, as important factors leading individuals down the pathway to suicidal behavior (Klonsky & May, 2015; O’Connor & Kirtley, 2018; Van Orden et al., 2010). There also is empirical evidence linking thwarted belongingness and social disconnection to risk for STBs (Stewart et al., 2017; Whitlock et al., 2014). Disruptions in social connectedness (family, peers, school) have been found to increase risk for STBs in youth, and greater social connectedness reduces risk for STBs in youth (e.g., Czyz et al., 2012; Foster et al., 2017; Gunn et al., 2018; Whitlock et al., 2014). Family connectedness (often operationalized as parent/caregiver involvement, degree of attachment, and quality of supportive relationship) has demonstrated a consistent association with STB risk; reduced family connection increases risk (e.g., Ackard et al., 2006; Arria et al., 2009; Fotti et al., 2006; Kerr et al., 2006) and greater connection reduces risk (e.g., Cuesta et al., 2021; Steiner et al., 2019; Xiao & Lindsey, 2021). The link between peer connectedness (e.g., degree of peer support, relationship strength) and STB risk has been more mixed. Some studies have found that peer connectedness buffers risk for STBs (e.g., Czyz et al., 2012; Kia et al., 2021; Massing-Schaffer et al., 2020), whereas others do not find this association or find that peer connections may increase risk (e.g., Arango et al., 2016; Kaminski et al., 2010; Kerr et al., 2006). Peers may increase risk by promoting STB engagement, either through their own behaviors or attitudes supporting STBs (Whitlock et al., 2014). Studies comparing these relationships have found that family, compared to peer, connections demonstrate a more robust role in reducing risk for STBs among youth (De Luca et al., 2012; Fotti et al., 2006; Kaminski et al., 2010).
Notably, several studies using intensive retrospective and prospective designs have found that reduced belongingness (sometimes conceptualized specifically as loneliness) relates to STBs over the short term. For instance, using an intensive Timeline Followback interview methodology with adults, one study found greater feelings of loneliness reported in the hours, specifically the six hours, prior to a suicide attempt (Bagge et al., 2017). Further support comes from recent intensive longitudinal studies. EMA studies with adults have found that thwarted belongingness (or loneliness) relates to greater suicidal thoughts contemporaneously (Hallensleben et al., 2019; Kleiman et al., 2017) and prospectively (Kyron et al., 2018). Further, in the only study with adolescents, Czyz et al. (2019) utilized a daily diary study (i.e., one daily assessment) with high-risk adolescents (n = 34; 652 total observations), hospitalized for suicide risk, during the post-hospitalization period. Lower social connectedness was significantly related to same-day suicide ideation frequency, duration, and urges (Czyz et al., 2019). In addition, the interaction between lower connectedness and either hopelessness or burdensomeness predicted next-day suicide ideation frequency and duration.
The third, and final, piece of evidence comes from work suggesting that lack of social connection may mediate the association between interpersonal NLEs and negative mental health outcomes. For example, loneliness has been found to mediate the association between interpersonal stress and psychological distress in adults (Aanes et al., 2010), and the association between peer victimization and depressive symptoms in adolescents (Baker & Bugay, 2011). Moreover, in an adult outpatient sample, thwarted belongingness mediated the link between bullying and suicide ideation (Brailovskaia et al., 2020). This finding is consistent with the interpersonal theory of suicide (Van Orden et al., 2010), which posits that thwarted belongingness is a mediator between NLEs and suicide ideation. Although promising, a major limitation of this prior mediation research is that all studies were cross-sectional and therefore unable to establish the temporal precedence needed for mediation (Cole & Maxwell, 2003).
Taken together, there is considerable evidence suggesting that reduced social connectedness, or thwarted belongingness, may help to explain how interpersonal NLEs increase risk for STBs in youth. However, this mechanism has not been examined directly in prior longitudinal research with adolescents.
Current Study
The current study aims to fill a significant gap in previous research by examining how thwarted belongingness with family and friends may temporally mediate the association between interpersonal NLEs and suicidal thoughts in a high-risk adolescent sample. First, we predicted that interpersonal NLEs would relate prospectively to lower belongingness (i.e., greater thwarted belongingness) with both family and friends. Second, we hypothesized that thwarted belongingness with family and friends would prospectively lead to greater suicidal thoughts. Finally, we predicted that thwarted belongingness (with family and friends) would temporally mediate the association between interpersonal NLEs and suicidal thoughts.
Method
This study was part of a larger project examining short-term risk factors for suicidal thoughts in adolescents during the high-risk post-discharge period. The method for this project has been described in detail in a prior paper (Glenn et al., 2021). A brief overview of methods related to the current study are summarized below.
Participants
Participants were recruited from an urban academic medical center in the northeastern U.S. Adolescents, ages 12–18 years, were eligible for this study if they had recently received acute psychiatric care (i.e., psychiatric emergency department, inpatient care, partial hospitalization) for suicide risk (i.e., suicide attempt, suicide ideation with intent and/or a plan) and were transitioning to outpatient care at the site’s medical center (for risk and safety monitoring reasons: Glenn et al., 2021). All adolescents (regardless of age) were enrolled with one parent or legal guardian (referred to collectively as Parents) within two weeks following the adolescent’s discharge from acute psychiatric care. Adolescents were ineligible for the following reasons: inability to provide assent/consent (due to severe cognitive impairment, current manic or psychotic state), unwillingness to complete the study procedures (e.g., smartphone-based EMA), or concerns for their safety (i.e., imminent risk for suicide or violence). Of those initially referred (i.e., any adolescent receiving acute psychiatric care), 39% were eligible for the current study; of those eligible, 65% enrolled in the study.1 Out of the full (n = 53) sample (Glenn et al., 2021), the first five adolescents were excluded because they did not receive the same questions about momentary suicidal thoughts as the rest of the sample. These questions were revised after the fifth participant was enrolled. Therefore, only 48 adolescents were included in the current paper because they received the same four questions about momentary suicidal thoughts (see Measures). Major sociodemographic and clinical characteristics for this sample are presented in Table 1.
Table 1.
Major sociodemographics, psychiatric disorders, and suicidal thoughts and behaviors in the adolescent sample (n=48).
| Sociodemographics | |
|---|---|
| Age (years): M (SD) | 14.96 (1.60) |
| Gender Identity: % (n/N) | |
| Female | 64.6% (31/48) |
| Male | 16.7% (8/48) |
| Nonbinary1 | 18.8% (9/48) |
| Race and Ethnicity: % (n/N) | |
| White | 77.1% (37/48) |
| Black/African American | 8.3% (4/48) |
| American Indian/Alaskan Native | 2.1% (1/48) |
| Multi-racial | 10.4% (5/48) |
| Hispanic/Latinx2 | 13.6% (6/44) |
| Sexual Orientation: % (n/N) | |
| Heterosexual | 41.7% (20/48) |
| Gay or Lesbian | 6.3% (3/48) |
| Bisexual | 31.3% (15/48) |
| Pansexual | 6.3% (3/48) |
| Asexual | 4.2% (2/48) |
| Unsure | 10.4% (5/48) |
| Annual Household Income: % (n/N)3 | |
| < $29,000 | 4.2% (2/48) |
| $30,000 – $69,000 | 31.3% (15/48) |
| $70,000 – $99,000 | 35.4% (17/48) |
| > $100,000 | 18.8% (9/48) |
| Prefer not to report | 10.4% (5/48) |
| Current Major Psychiatric Disorders4: % (n/N) | |
| Anxiety disorder | 93.5% (43/46) |
| Attention-deficit hyperactivity disorder | 27.9% (12/43) |
| Bipolar disorder | 6.5% (3/46) |
| Disruptive behavior disorder | 25.0% (11/44) |
| Eating disorder | 20.9% (9/43) |
| Major depressive disorder | 82.6% (38/46) |
| Obsessive compulsive disorder | 9.3% (4/43) |
| Posttraumatic stress disorder | 20.0% (9/45) |
| Psychotic symptoms | 7.0% (3/43) |
| Substance use disorder | 8.7% (4/46) |
| Suicidal Thoughts and Behaviors and Non-Suicidal Self-Injury | |
| Lifetime: | |
| Suicide ideation: % (n/N) | 100% (48/48) |
| Suicide attempt: % (n/N) | 85.4% (41/48) |
| Multiple attempts5: | 61.0% (25/41) |
| NSSI: % (n/N) | 81.3% (39/48) |
| # NSSI methods6: M (SD) | 2.11 (0.89) |
| Past year: | |
| Suicide ideation: % (n/N) | 100% (48/48) |
| Suicide attempt: % (n/N) | 78.7% (37/47) |
| Multiple attempts5: | 51.4% (19/37) |
| NSSI: % (n/N) | 77.1% (37/48) |
| Past month: | |
| Suicide ideation: % (n/N) | 91.7% (44/48) |
| Suicide attempt: % (n/N) | 31.3% (15/48) |
| NSSI: % (n/N) | 58.3% (28/48) |
NSSI=nonsuicidal self-injury
Nonbinary includes adolescents identifying as transgender, nonbinary, or agender.
Four adolescents did not report their ethnicity.
Annual household income was reported by parents/guardians.
Anxiety disorder includes any of the following current disorders: panic disorder, agoraphobia, social anxiety disorder, specific phobia, or generalized anxiety disorder; Attention-deficit hyperactivity disorder includes any of the following current subtypes: inattentive only, hyperactive/impulsive only, or combined; Bipolar disorder includes current bipolar I or II disorder; Disruptive behavior disorder includes current conduct disorder or oppositional defiant disorder; Eating disorder includes current anorexia nervosa or bulimia nervosa; Substance use disorder includes current alcohol use disorder or substance (drug) use disorder. Given time constraints, not all disorder modules were administered to all participants resulting in missing data.
Out of those with a history of suicide attempts, the percentage who reported more than one suicide attempt in the specified time period.
Among adolescents reporting lifetime NSSI, the average number of NSSI methods used over their lifetime.
Procedure
Study procedures were approved by the University of Rochester’s Institutional Review Board (RSRB00066408). Adolescents and one parent were enrolled in the study from September 2017 to July 2019. Prior to study initiation, adolescents provided assent (12–17 year-olds) or consent (18 year-olds), and parents provided permission for their child (12–17 year-olds) or consent for their own participation (for 18 year-olds). There were two main phases relevant to the current study: (1) baseline assessment with the adolescent and their parent, within two weeks of discharge from acute psychiatric care, and (2) a 28-day EMA period following the baseline, for the adolescent only.
Phase 1 Baseline.
The baseline assessment included a series of interviews and questionnaires for the adolescent and parent (details below). The baseline concluded with an orientation to the smartphone-based EMA application (described in Phase 2 EMA) and a review of the adolescent’s most recent safety plan (created with their clinical team) for use during crisis in the EMA phase of the study. For the baseline assessment, adolescents and parents were each compensated $25/hour (maximum of $75 each).
Background sociodemographic and diagnostic information.
At baseline, adolescents provided their own demographic information (age, gender identity, race, ethnicity, sexual orientation) and parents provided information about family socioeconomic status (see Table 1). To characterize the sample, adolescents’ major psychiatric disorders were assessed using the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-Kid)—a brief, fully structured diagnostic interview that has demonstrated good psychometric properties in adolescents (Duncan et al., 2018). In the current study, adolescents and parents were interviewed separately and current psychiatric diagnoses were determined by integrating adolescent and parent reports (see Table 1).
Suicidal thoughts and behaviors, and self-injury.
Adolescents’ suicide ideation and attempts (i.e., lifetime, past year, and past month) were assessed, from the adolescent, with the Columbia-Suicide Severity Rating Scale (C-SSRS; (Posner et al., 2011)). As needed, parents separately provided missing details about their adolescents’ suicidal behavior (e.g., lethality of, and medical treatment received for, a suicide attempt). The C-SSRS has been validated in adolescents (Brent et al., 2009; Gipson et al., 2015). To assess history of nonsuicidal self-injury (NSSI), a supplemental form based on the Self-Injurious Thoughts and Behaviors Interview (SITBI; (Nock et al., 2007)) was used. Prevalence of STBs and NSSI over adolescents’ lifetime, past year, and past month are presented in Table 1.
Phase 2 Ecological momentary assessment (EMA).
The EMA period was for 28 days following the baseline assessment. Several types of EMA surveys were utilized in this project. This study will focus on two types of surveys:
Interval-contingent surveys were completed at a fixed time each evening (ICPM), around the adolescent’s bedtime (tailored to each adolescent’s schedule to increase adherence). After receiving the survey prompt, adolescents were given two hours (one hour before and one hour after specified bedtime) to complete each survey. During the EMA period, participants completed an average of 16.42 ICPM surveys (SD = 8.46, range = 2–28). The median ICPM completion time was 1 minute 16 seconds. In these surveys, adolescents indicated whether a range of interpersonal NLEs occurred that day (see Measures).
Signal-contingent (SC), or random, surveys were completed multiple, 3–6, times each day. After receiving the survey prompt, adolescents were given 30 minutes to complete each survey. The window to complete surveys was based on each adolescent’s availability, which provided more time on some days than others (leading to a range of 3–6 available surveys). Adolescents were not prompted to complete surveys during weekday school hours. Although several SC prompts were offered each day, adolescents were only required to complete three SC surveys daily to receive full compensation. During the EMA period, participants completed an average of 62.36 SC surveys (SD = 31.03, range = 6–116).2 The median completion time for these surveys was 3 minutes 25 seconds. In these surveys, adolescents responded to prompts about momentary belongingness with family and friends and suicidal thoughts (see Measures).
EMA surveys were completed on adolescents’ iOS or Android smartphones (i.e., either their personal phone or one loaned to them by the researchers) using a HIPAA-compliant smartphone application specifically designed for mobile EMA research (www.metricwire.com). During the 28-day EMA period, adolescents were compensated with a $25 Amazon gift card for each week they completed at least 75% of the EMA surveys. The constructs assessed in these surveys are described below and the specific questions included in each survey are provided in Table 2.
Table 2.
Ecological momentary assessment items utilized to assess interpersonal negative life events (predictor), thwarted belongingness with family and friends (mediators), and suicidal thinking (outcome).
| Interpersonal negative life events |
|---|
| Instructions: Did any of the following happen to you today? Select all that apply. |
| 1. Events with a family member: |
| Argument with a family member |
| Criticized by a family member |
| Ignored by a family member |
| A family member cancelled plans |
| A family member broke a promise to you |
| There were arguments among your family members |
| 2. Events with a friend or peer: |
| Argument with a friend/peer/someone else around your age |
| Criticized by a friend/peer/someone else around your age |
| Ignored by a friend/peer/someone else around your age |
| A friend/peer/someone else around your age cancelled plans |
| A friend/peer/someone else around your age broke a promise to you |
| You were bullied while you were at school |
| You were bullied online |
| You were bullied somewhere other than school or online |
| 3. Events with a significant other/romantic partner: |
| Argument with a significant other/romantic partner |
| Criticized by a significant other/romantic partner |
| Ignored by a significant other/romantic partner |
| Significant other/romantic partner cancelled plans |
| Significant other/romantic partner broke a promise to you |
| You broke up with your significant other/romantic partner |
| Significant other/romantic partner broke up with you |
| Significant other/romantic partner cheated or was unfaithful to your relationship |
| 4. Stressful events with others: |
| Argument with a teacher/principal/authority figure |
| Argument with someone else |
| Other stressful event(s)1 (Please describe: ____________) |
| 1 See Supplement 1 for information about how “other” stressful life events were coded. |
| Thwarted Belongingness |
| Instructions: The following questions ask you to think about yourself and other people. Please base your responses on how you feel right now. |
| Scale: 0=Not at all true for me, 1=Somewhat true, 2=Quite a bit true, 3=Very much true for me. |
| Family belongingness items (items scored so higher values indicate greater thwarted belonging) |
| 1. My family cares about me (reverse scored) |
| 2. I feel disconnected from my family |
| 3. I feel that I can turn to my family in times of need (reverse scored) |
| 4. I am close to my family (reverse scored) |
| Friend belongingness items (items scored so higher values indicate greater thwarted belonging) |
| 1. My friends care about me (reverse scored) |
| 2. I feel disconnected from my friends |
| 3. I feel that I can turn to my friends in times of need (reverse scored) |
| 4. I am close to my friends (reverse scored) |
| Suicidal Thoughts | ||
|---|---|---|
| Variable | Question | Scale |
| Suicide desire | “How intense is your desire to kill yourself right now?” | 0=Absent/no desire, 1=Present, but not at all intense to 5=Extremely intense |
| Suicide intent | “How strong is your intent to kill yourself right now?” | 0=Absent/no intent, 1=Present but not at all strong to 5=Extremely strong |
| Ability to keep self safe | “How able are you to keep yourself safe right now?” | 1=I definitely CAN keep myself safe
to 5=I definitely CANNOT keep myself safe |
| Desire for life | “How strong is your desire to live right now?” | 1=Very strong
to 5=Very weak |
Measures
Interpersonal negative life events (predictor).
At the end of each day (ICPM survey), adolescents indicated whether a range of interpersonal NLEs occurred that day. The list of interpersonal NLEs provided was based on the Life Events Scale for Children (LES-C; Coddington, 1972), and assessed a range of interpersonal experiences, such as arguments/disagreements, disappointments, rejection, loss, humiliation/embarrassment, and victimization (see Table 2). Events were clustered based on the relationship to the adolescent: family, friends/peers, significant other/romantic partner, or others (e.g., teacher, authority figure, someone else who did not fit into any of these categories). Adolescents were able to indicate (with checkboxes) all events that occurred that day (yes/no). A “none of the above” option was provided for each cluster (coded as 0). Finally, a write in “other stressful life event” option was provided. “Other” events were reviewed by both the first and last author to determine whether these free responses were interpersonal NLEs that should be included in the analyses. A list of coding decisions is provided in Supplement 1. In the current sample, 89.6% of adolescents reported an interpersonal NLE occurred during the EMA period (total NLEs between-person M = 13.63; SD = 15.35): 79.2% of the full sample reported a family NLE, 64.6% reported a peer NLE, 37.5% reported a romantic partner NLE, and 47.9% reported an interpersonal NLE with someone else. For the current study, the frequency of total interpersonal NLEs was utilized as the primary predictor (see Table 3).
Table 3.
Descriptive information about major study variables.
| Variable | M | SD | ICC (95% CI) |
|---|---|---|---|
| NLE Total | 0.80 | 1.36 | 0.44 [0.35–0.56] |
| NLE family | 0.44 | 0.94 | 0.31 [0.23–0.43] |
| NLE peer | 0.22 | 0.76 | 0.52 [0.43–0.63] |
| NLE romantic partner | 0.07 | 0.32 | 0.25 [0.17–0.36] |
| NLE others | 0.05 | 0.23 | 0.11 [0.07–0.17] |
| INQ family 1 | 0.84 | 0.98 | 0.70 [0.61–0.78] |
| INQ family 2 | 1.33 | 1.05 | 0.67 [0.58–0.76] |
| INQ family 3 | 1.38 | 1.09 | 0.78 [0.71–0.85] |
| INQ family 4 | 1.27 | 1.06 | 0.76 [0.68–0.83] |
| INQ friend 1 | 0.80 | 0.97 | 0.72 [0.64–0.80] |
| INQ friend 2 | 1.06 | 1.01 | 0.68 [0.59–0.77] |
| INQ friend 3 | 1.09 | 1.02 | 0.68 [0.59–0.77] |
| INQ friend 4 | 0.92 | 0.97 | 0.69 [0.60–0.77] |
| Suicide desire | 0.65 | 1.03 | 0.46 [0.37–0.58] |
| Suicide intent | 0.27 | 0.62 | 0.45 [0.36–0.57] |
| Ability to keep self safe | 1.30 | 0.49 | 0.45 [0.36–0.57] |
| Desire for life | 2.71 | 1.25 | 0.70 [0.62–0.79] |
ICC=intraclass correlation (higher ICC=more variability between vs. within person), INQ=interpersonal needs questionnaire, M=mean, NLE=interpersonal negative life event, SD=standard deviation.
Note. Correlations between major study variables are presented in Supplement 2.
Thwarted belongingness (mediator).
Belongingness with family and friends was assessed multiple times each day in the SC surveys using a subset of belongingness items from the Interpersonal Needs Questionnaire (INQ; Van Orden et al., 2012). The INQ is a self-report measure developed to assess thwarted belongingness and perceived burdensomeness related to the interpersonal theory of suicide (Van Orden et al., 2012), and has demonstrated good psychometric properties in adolescents (Hill et al., 2020). Items from the INQ have been adapted to measure belongingness in prior EMA studies with adults (Hallensleben et al., 2019; Kyron et al., 2018) and a daily diary study with adolescents (Czyz et al., 2019). For the current study, a subset of INQ belongingness items was adapted to assess belongingness with family and friends separately. Specifically, four belongingness items (included on the full INQ-25, as well as briefer INQ-15 and INQ-12 versions; Hill et al., 2015)) were modified from “other people” to ask about either “family” or “friends” to specifically assess belongingness with these individuals. Items were rates on a scale from 0 = Not at all true for me to 3 = Very true for me (specific items are provided in Table 2). For the current study, family thwarted belongingness and friend thwarted belongingness were examined as separate latent constructs (see Table 3).
Suicidal thoughts (outcome).
During the multiple SC surveys daily, adolescents reported their momentary suicidal thoughts, using four items adapted from prior EMA studies with adolescents (Nock et al., 2009) and adults (Kleiman et al., 2017). These questions assessed current (at that moment) suicide desire, suicide intent, ability to keep oneself safe, and desire for life (specific items are provided in Table 2). All items were rated on a 0–5 scale with higher scores indicating greater suicidal thoughts. We created a latent variable consisting of these four items (see Table 3). Given the high-risk sample included in the current study, adolescents’ responses to these questions were monitored daily to assess their risk and ensure their safety (consistent with guidelines for conducting EMA research with high-risk youth; Bai et al., 2021; Nock et al., 2021). Appropriate steps were taken to keep adolescents safe during this assessment study (additional details about the risk and safety monitoring protocol are reported in Glenn et al., 2021).
Data preparation and analysis
The study included 2,733 total observations over 945 days of data (M = 2.89 surveys per person per day; SD = 1.33). Correlations between major study variables (within-person and between-person) are provided in Supplement 2.
Missing data.
EMA data were missing at the survey level (i.e., a survey was not completed) rather than at the item level (i.e., all items in a single survey were completed). The current study utilized the prior day’s ICPM survey to predict the next day’s SC responses. If an ICPM survey was missing, that day’s data were not included in the model, because the predictor was missing for that day. If a next-day SC survey was missing (i.e., mediator: belongingness, outcome: suicidal thoughts), other SC surveys from that day were included in the model. If all SCs were missing the next day (following an ICPM), or all but one (since we were using two consecutive SCs for mediation), that day’s data were not included in the model. The configuration of our missing data involved a completely missing survey rather than a missing item from an otherwise complete survey. This type of missingness is expected in multi-level modelling (effectively only leading to unevenly spaced data) and is not something that can be imputed.
Analytic strategy.
Overview.
We conducted a multi-level structural equation model (SEM) in lavaan in R, which examined (1) family thwarted belongingness and (2) friend thwarted belongingness as parallel mediators in the relationship between interpersonal NLEs and suicidal thoughts. We created latent variables for (1) family thwarted belongingness, (2) friend thwarted belongingness, and (3) suicidal thoughts. All three latent variables consisted of the four observed variables representing each construct. Total number of interpersonal NLEs was measured as a unitary construct and thus was specified in the model as an observed variable. We unfortunately were unable to examine NLEs by category given the co-occurrence of family and peer NLE, and the unequal occurrence of NLEs. Specifically, of the days when a peer NLE was reported, 40% of days co-occurred with a family NLE. And, of the days when a family NLE was reported, 20% of days co-occurred with a peer NLE. Therefore, it is hard to disentangle the unique effects of these NLE categories.
Temporality and hierarchical structure.
Given that we were testing a mediational model, it was important to establish temporality (Cole & Maxwell, 2003). Accordingly, we included interpersonal NLEs as a day-level variable. Next-day thwarted belongingness and suicidal thoughts were measured at the momentary level multiple times daily, and therefore belongingness could be measured at the time point prior to suicidal thoughts at the within-day level. In summary, our model included interpersonal NLEs from the prior day (day 1), friend/family thwarted belongingness at the current day (day 2) at time T, and suicidal thoughts at the current day (day 2) at time T+1 (i.e., examination of full mediation). Multi-level SEM includes, and estimates, all direct and indirect effects in the same model. As is common in SEM mediation approaches, we did not examine direct effects prior to testing the main model. Testing direct effects first is not a requirement if there is theoretical rationale for examining mediation, effect sizes may be small (recognition that proximal associations will be larger than distal ones), or suppression is possible (Shrout & Bolger, 2002).
Centering.
We utilized latent variable centering (Asparouhov & Muthén, 2019), which involves estimating two simultaneous structural equation models: (1) a within-person model, which is the model testing our primary hypotheses, as described above and (2) a between-person model that includes the between-person means for the variables at the within-person level. This decomposes the variance and thus allows us to examine the within-person effects in our model (where our hypothesized effects of interest are) separate from any between-person effects. Given our focus on within-person, time-varying processes, we primarily report and discuss the within-person component of the model.
Model fit.
To assess model fit, we used several common indicators (Schreiber et al., 2006). First, we used the comparative fit index (CFI), which compares the hypothesized model to a “null” model with the worst possible fit. Larger CFIs indicate a better fitting model (i.e., one that differs more to a null model). CFI should be > .95. We also report the Tucker-Lewis Index (TLI), which compares the chi-square of the hypothesize model to the chi-square of the null model. It is highly correlated with and interpreted similarly to the CFI. Next, we used root mean square error of approximation (RMSEA), which compares the hypothesized model to one with “perfect” fit. Smaller RMSEA values indicate a model closer to one with perfect fit. RMSEA should be < .08. We do not report the traditional chi-square/degrees of freedom fit metric given that it is problematic in large samples, which is the case for our level 1 sample size (Shi et al., 2019).
Results
Measurement model
When conducting individual measurement models for the latent variables, model fit was acceptable. The two-factor (family and friends) thwarted belongingness latent variables had excellent fit: RMSEA = .039 (90% CI = .033 to .045), CFI = .975, TLI = .959. The suicidal thoughts latent variable had relatively poorer, but still acceptable fit: RMSEA = .134 (90% CI = .111 to .158), CFI = .968, TLI = .806. For parsimony, we report the factor loadings in the main SEM in Figure 1 (thinner grey paths) instead of in a separate measurement model-only figure. The loadings were nearly identical in measurement-only models as in the full structural model: across all three latent variables, the observed variables significantly loaded onto their respective factors (all ps < .001).
Figure 1.
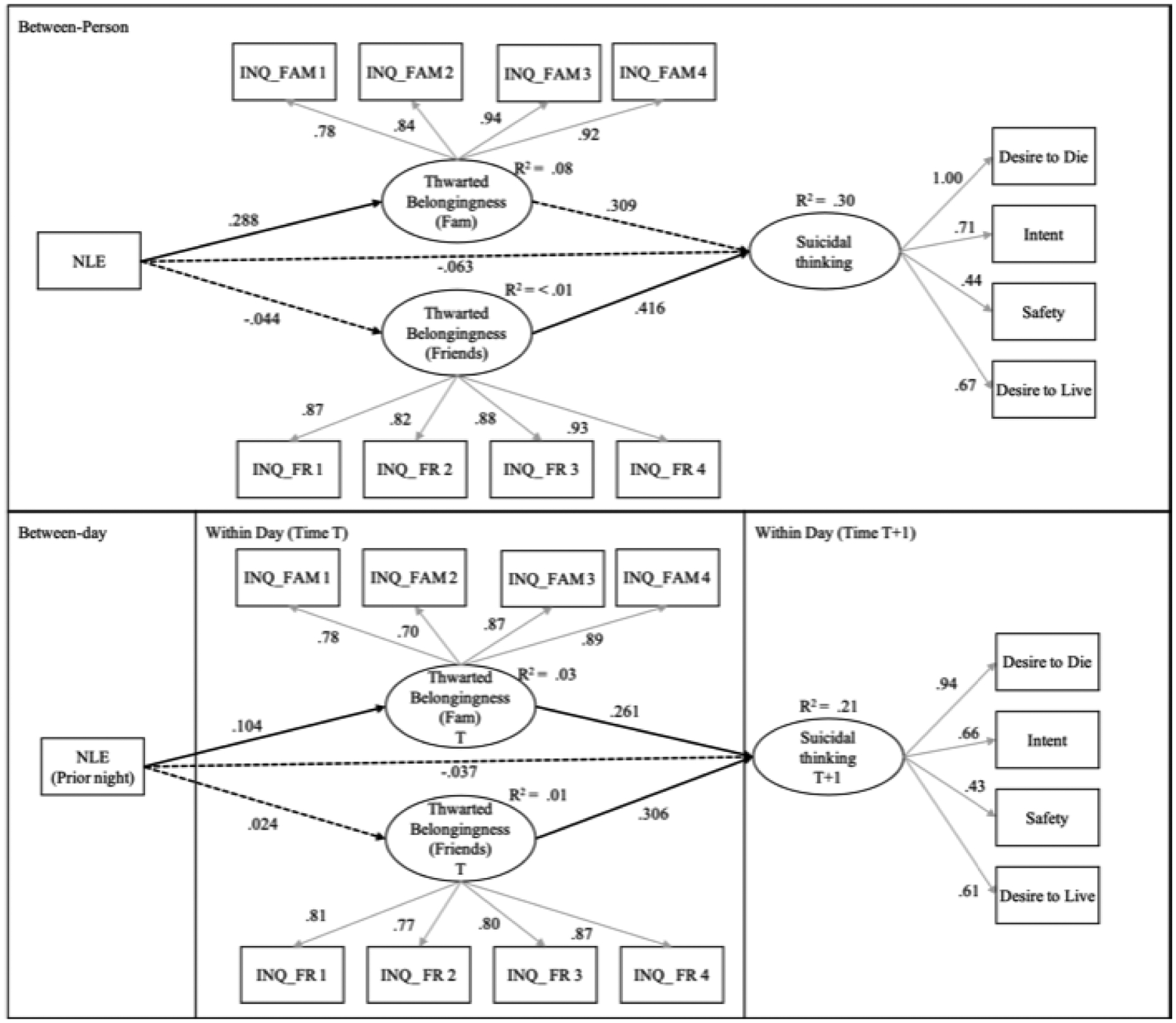
Results of the multi-level structural equation model testing family thwarted belongingness and friend thwarted belongingness as mediators of the association between interpersonal negative life events (NLEs) and next-day suicidal thinking.
INQ=interpersonal needs questionnaire; NLE=frequency of interpersonal negative life events; T=time 1 (EMA survey), T+1=time 2 (subsequent EMA survey)
Note. Standardized estimates shown. Grey lines=measurement model, Black lines=structural models. Solid lines=significant at p < .05, dashed lines=not significant. The covariances between the family and friend latent variables are not shown for clarity purposes but reported here. Between-person level: β=.07, p=.303, within-person level: β=.17, p<.001.
Structural model
The structural model had acceptable fit (RMSEA = .091 [90% CI = .087 to .095)], CFI = .856, TLI = .815). The thicker, black paths in Figure 1 represent the structural model. There were significant direct effects (solid black lines) in the within-person model between interpersonal NLEs and family thwarted belongingness, between family thwarted belonginess and suicidal thoughts, and between friend thwarted belongingness and suicidal thoughts.
Indirect effects (mediation)
The indirect effect, within-person effect, through family thwarted belongingness was significant (β = 0.048, se = 0.006, p < .001). The indirect effect through friend thwarted belongingness was not significant (β = 0.005, se = 0.006, p = .392).3
Discussion
The current study increases understanding of how interpersonal negative life events (NLEs) relate to suicidal thoughts in adolescents over the short term. There are three major findings from this research. First, interpersonal NLEs were significantly related to next-day suicidal thoughts in high-risk adolescents during the 28 days following discharge from acute psychiatric care. Second, thwarted belongingness with family mediated the link between interpersonal NLEs and next-day suicidal thoughts. Third, thwarted belongingness with friends did not mediate the association between interpersonal NLEs and next-day suicidal thoughts in youth, although friend thwarted belongingness did relate to next-day suicidal thoughts. Each finding will be discussed in turn.
First, this research provides greater temporal resolution of the association between interpersonal NLEs and suicidal thoughts in youth. Consistent with prior research in adults (Bagge et al., 2013; Franz et al., 2021; Husky et al., 2017; Yen et al., 2005) and adolescents (Cheek, Goldston, et al., 2020), interpersonal NLEs predicted greater suicidal thoughts over the short term. Although prior studies in adults have examined this association over the course of hours (up to one day; Bagge et al., 2013; Franz et al., 2021; Husky et al., 2017), this is the first EMA study in youth to indicate that interpersonal NLEs predict increased suicidal thoughts the next day. Notably, this association was significant when NLEs were used to predict next-day suicidal thoughts (in order to establish temporal precedence; Kraemer et al., 1997), suggesting the robustness of these effects for youth.
Second, thwarted belongingness with family mediated the association between interpersonal NLEs and suicidal thoughts. Specifically, interpersonal NLEs predicted greater next-day thwarted belongingness with family, family thwarted belongingness predicted greater suicidal thoughts later in the day, and family thwarted belongingness mediated the association between interpersonal NLEs and suicidal thoughts. Given the intensive longitudinal design and ability to examine full temporal mediation, these findings significantly extend prior cross-sectional research on the mediating role of belongingness (Brailovskaia et al., 2020). Further, these results align with previous longitudinal research, including a prior EMA study with adults indicating the unique role of family stressors on suicidal thoughts (Husky et al., 2017), and research in adolescents indicating that parental stressors, such as parental rejection, are significantly associated with STBs (Cheek, Reiter-Lavery, et al., 2020). The importance of belongingness with family is also evidenced by research indicating that family connectedness is a protective factor for youth (Cuesta et al., 2021; Steiner et al., 2019; Xiao & Lindsey, 2021). Notably, family connectedness may buffer STB risk for high-risk clinical (i.e., previously hospitalized) youth (Czyz et al., 2012), as well as youth minoritized based on their race and ethnicity (e.g., O’Donnell et al., 2004), or sexual orientation and gender identity (e.g., Ryan et al., 2010). In fact, family connectedness has been most consistently and robustly linked to reduced risk for STBs (Whitlock et al., 2014).
Third, unlike family, thwarted belongingness with friends did not mediate the association between interpersonal NLEs and suicidal thoughts. Thwarted belongingness with friends was related to greater suicidal thoughts later in the day. However, interpersonal NLEs did not directly relate to thwarted belongingness with friends the next day, nor did thwarted belongingness with friends mediate the association between interpersonal NLEs and suicidal thoughts. This finding is somewhat surprising given the important role that peers play for adolescents (Crone & Dahl, 2012; Somerville, 2013), and consistent research indicating that peer relationship difficulties are linked with STBs (Cheek, Reiter-Lavery, et al., 2020). There are several interpretations of these results. One interpretation is that friend belongingness does not play a mediating role like family belongingness. Prior research on the link between peer connections and STBs suggests that these associations are complicated: although peers can provide social support and protection against STBs, peers can also increase STB risk if they also engage in suicidal behavior (social contagion) or hold STB-promoting attitudes (Whitlock et al., 2014). It is important to note that this sample was enrolled in the study within two weeks after discharge from acute psychiatric care. During this post-discharge period, family may play a more important role for adolescents than their friends (e.g., Kerr et al., 2006)), or adolescents may simply have more interaction with family than friends during this time (e.g., the sample reported more family NLEs than friend/peer NLEs). An alternative interpretation is that the study was not designed to measure the temporal course of how interpersonal NLEs impact belongingness with friends. For instance, if the impact on friend belongingness was shorter (i.e., within day, rather than between day measured in this study) or longer (more than one day), it would not be captured in the current study. Replication is needed to examine if, and for whom, friend belongingness may play a role in the link between interpersonal NLEs and suicidal thoughts in youth.
Clinical Implications
These findings have several implications for clinical practice. First, they suggest that interpersonal NLEs are proximal risk factors for suicidal thoughts, leading to greater suicidal thoughts over a relatively short time period (i.e., the following day). These findings provide additional empirical support for the assessment of interpersonal NLEs for youth in risk assessment protocols (Linehan et al., 2012; Pisani et al., 2016). Second, this study indicates one way in which interpersonal NLEs may confer risk for STBs in youth. Not all stressors, and not even all interpersonal stressors, will increase STB risk for youth. Findings suggest that an interpersonal NLE may increase risk for adolescents to the degree that it makes them feel like they do not belong, specifically with family. Clinically, this provides additional guidance about how interpersonal stressors might impact adolescents and suggests additional details to assess their impact. Third, and finally, these findings have implications for downstream suicide prevention approaches, by indicating which factors may be proximally related, and treatment targetable, to reduce suicide risk. To reduce the likelihood of some interpersonal NLEs (e.g., arguments with parents), youth may benefit from enhancing interpersonal effectiveness skills including communication and problem-solving (e.g., Rathus & Miller, 2014). Notably, a review of evidence-based treatments for STBs among youth (Glenn et al., 2019) suggests that effective interventions include a central family component, such as family skills training (e.g., family communication). In addition, findings suggest that modifying belongingness, for those who have experienced an interpersonal NLE, may reduce suicide risk. Greater connectedness to others (family, peers, school, community) relates to reduced risk for STBs (Whitlock et al., 2014), even during the high-risk post-hospitalization period (e.g., Czyz et al., 2012). Interventions and preventions that aim to increase social connection have shown some effectiveness for reducing suicide ideation in adults (Comtois et al., 2019; Wyman et al., 2020). Clinicians also may consider addressing the cognitive vulnerabilities and self-blaming attributions that can follow interpersonal stressors leading youth to feel like they do not belong (e.g., Graham & Juvonen, 1998; Schacter et al., 2015). Future research is needed to identify if, and how, belongingness can be modified in adolescents to reduce suicidal thoughts and risk for suicidal behaviors.
Limitations and Future Directions
Limitations of this study provide directions for future research. First, this study focused on interpersonal NLEs, given their relevance for youth, and specific mediators of interest. However, we were unable to examine interpersonal NLEs by category (e.g., family, peer), and how the impact of interpersonal NLEs compares to non-interpersonal NLEs over this high-risk period, which are important directions for future research. Second, this study focused on thwarted belongingness as one specific mechanism linking interpersonal NLEs to suicidal thoughts, but there are likely other potential mediators that may play a role (e.g., Franz et al., 2021). Third, this study examined one temporal association given the structure of the data. That is, NLEs were measured at the day level; therefore, to assume temporal precedence, they could only be used to predict next-day factors. However, the negative impact of these events is likely experienced within the same day (e.g., Chaudhury et al., 2017). Future research would benefit from utilizing alternative study designs that examine the immediate impact of these events, such as burst designs that can assess factors repeatedly in the hours following an event (Sliwinski, 2008). Finally, although the study was well-powered for within-person analyses, and our multi-level SEM model incorporated person-level means, we did not have the power for between-person analyses to examine specific individual differences in overall effects. Thus, we were underpowered to examine how effects may be moderated by demographic differences in the sample (such as gender identity, and race/ethnicity). An important direction for future research will be to examine this mechanism among minoritized youth given the high risk of STBs (Lindsey et al., 2019; The Trevor Project, 2021) and interpersonal NLEs (e.g., discrimination) uniquely experienced by these populations (Benner et al., 2018; The Trevor Project, 2021).
Summary
This study found some support for belongingness as a potential mechanism linking interpersonal NLEs to suicidal thoughts among youth. Findings indicate that thwarted belongingness with family, but not friends, mediated the association between interpersonal NLEs and next-day suicidal thoughts among high-risk adolescents following discharge from acute psychiatric care. Belongingness may be a promising target for youth who experience interpersonal stressors to reduce their risk for suicide.
Supplementary Material
Acknowledgements
Funding Statement:
This research was supported in part by a grant from the American Foundation for Suicide Prevention (YIG-1-054-16), funding from the National Institute of Mental Health (L30 MH101616), and pilot funding from the University of Rochester Medical Center.
This study was approved by the University of Rochester’s Institutional Review Board (RSRB00066408).
The authors would like to thank the following members of the research team for their assistance with this project: Linda Alpert-Gillis PhD, Yeates Conwell MD, Wilfred Pigeon PhD, Jaclyn Kearns MA, John (Kai) Kellerman, Angela Santee, and all the research assistants who helped with data collection and risk monitoring. In addition, the authors thank Kim Van Orden PhD for assistance modifying the belongingness measure for the current study. Finally, the authors would like to thank the adolescents and their families who volunteered to participate in this research, as well as Michael Scharf, MD, Claudia Blythe, and the clinical team in Pediatric Behavioral Health & Wellness at the University of Rochester Medical Center for their support with this research.
Footnotes
At the time of eligibility screening, only adolescents’ age and gender were available. Enrolled and unenrolled adolescents did not differ in age (t[80] = −0.12, p = .902) or gender (χ2[2, N = 82] = 1.05, p = .591).
Because the number of total SC prompts varied across adolescents depending on the number of days enrolled in the study and number of daily prompts (based on each adolescent’s availability), survey completion is reported as raw numbers instead of percentages.
When testing alternative models with only one mediator at a time, the interpretation was the same: family thwarted belongingness was a significant mediator, but friend thwarted belongingness was not.
Conflicts of Interest: Author CG receives royalties from UpToDate, and RL is a consultant for Relmada Therapeutics. The other authors have no conflicts of interest to disclose.
References
- Aanes MM, Mittelmark MB, & Hetland J (2010). Interpersonal stress and poor health. European Psychologist, 15(1), 3–11. [Google Scholar]
- Ackard DM, Neumark-Sztainer D, Story M, & Perry C (2006). Parent–child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine, 30(1), 59–66. [DOI] [PubMed] [Google Scholar]
- Allen KA, Ryan T, Gray DL, McInerney DM, & Waters L (2014). Social media use and social connectedness in adolescents: The positives and the potential pitfalls. The Educational and Developmental Psychologist, 31(1), 18–31. [Google Scholar]
- Arango A, Opperman KJ, Gipson PY, & King CA (2016). Suicidal ideation and suicide attempts among youth who report bully victimization, bully perpetration and/or low social connectedness. Journal of Adolescence, 51, 19–29. [DOI] [PubMed] [Google Scholar]
- Arria AM, O’Grady KE, Caldeira KM, Vincent KB, Wilcox HC, & Wish ED (2009). Suicide ideation among college students: A multivariate analysis. Archives of Suicide Research, 13(3), 230–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asher SR, & Paquette JA (2003). Loneliness and peer relations in childhood. Current Directions in Psychological Science, 12(3), 75–78. [Google Scholar]
- Asparouhov T, & Muthén B (2019). Latent variable centering of predictors and mediators in multilevel and time-series models. Structural Equation Modeling: A Multidisciplinary Journal, 26(1), 119–142. [Google Scholar]
- Bagge CL, Glenn CR, & Lee H-J (2013). Quantifying the impact of recent negative life events on suicide attempts. Journal of Abnormal Psychology, 122(2), 359–368. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Littlefield AK, & Glenn CR (2017). Trajectories of affective response as warning signs for suicide attempts: An examination of the 48 hours prior to a recent suicide attempt. Clinical Psychological Science, 5(2), 259–271. [Google Scholar]
- Bai S, Babeva KN, Kim MI, & Asarnow JR (2021). Future directions for optimizing clinical science & safety: ecological momentary assessments in suicide/self-harm research. Journal of Clinical Child & Adolescent Psychology, 50(1), 141–153. [DOI] [PubMed] [Google Scholar]
- Baker OE, & Bugay A (2011). Peer victimization and depressive symptoms: The mediation role of loneliness. Procedia-Social and Behavioral Sciences, 30, 1303–1307. [Google Scholar]
- Baumeister RF, & Leary MR (1995). The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Interpersonal Development, 117(3), 497–529. [PubMed] [Google Scholar]
- Beautrais AL, Joyce PR, & Mulder RT (1997). Precipitating factors and life events in serious suicide attempts among youths aged 13 through 24 years. Journal of the American Academy of Child & Adolescent Psychiatry, 36(11), 1543–1551. [DOI] [PubMed] [Google Scholar]
- Benner AD, Wang Y, Shen Y, Boyle AE, Polk R, & Cheng Y-P (2018). Racial/ethnic discrimination and well-being during adolescence: A meta-analytic review. American Psychologist, 73(7), 855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brailovskaia J, Ujma M, Friedrich S, & Teismann T (2020). Thwarted belongingness and perceived burdensomeness mediate the association between bullying and suicide ideation. Crisis, 41(2), 136–140. [DOI] [PubMed] [Google Scholar]
- Brent DA, Greenhill LL, Compton S, Emslie G, Wells K, Walkup JT, Vitiello B, Bukstein O, Stanley B, & Posner K (2009). The Treatment of Adolescent Suicide Attempters study (TASA): predictors of suicidal events in an open treatment trial. Journal of the American Academy of Child & Adolescent Psychiatry, 48(10), 987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Baugher M, Roth C, Balach L, & Schweers J (1993). Stressful life events, psychopathology, and adolescent suicide: A case control study. Suicide and Life‐Threatening Behavior, 23(3), 179–187. [PubMed] [Google Scholar]
- Chaudhury SR, Galfalvy H, Biggs E, Choo T-H, Mann JJ, & Stanley B (2017). Affect in response to stressors and coping strategies: an ecological momentary assessment study of borderline personality disorder. Borderline Personality Disorder and Emotion Dysregulation, 4(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheek SM, Goldston DB, Erkanli A, Massing-Schaffer M, & Liu RT (2020). Social rejection and suicidal ideation and attempts among adolescents following hospitalization: A prospective study. Journal of Abnormal Child Psychology, 48(1), 123–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheek SM, Reiter-Lavery T, & Goldston DB (2020). Social rejection, popularity, peer victimization, and self-injurious thoughts and behaviors among adolescents: A systematic review and meta-analysis. Clinical Psychology Review, 101936. [DOI] [PubMed] [Google Scholar]
- Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, & Large MM (2017). Suicide rates after discharge from psychiatric facilities: A systematic review and meta-analysis. JAMA Psychiatry, 74(7), 694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coddington RD (1972). The significance of life events as etiologic factors in the diseases of children: II. A study of a normal population. Journal of Psychosomatic Research, 16(3), 205–213. [DOI] [PubMed] [Google Scholar]
- Cole DA, & Maxwell SE (2003). Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112(4), 558–577. [DOI] [PubMed] [Google Scholar]
- Comtois KA, Kerbrat AH, DeCou CR, Atkins DC, Majeres JJ, Baker JC, & Ries RK (2019). Effect of augmenting standard care for military personnel with brief caring text messages for suicide prevention: a randomized clinical trial. JAMA Psychiatry, 76(5), 474–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Goldston DB, & Costello EJ (2017). Adult associations of childhood suicidal thoughts and behaviors: a prospective, longitudinal analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56(11), 958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crone EA, & Dahl RE (2012). Understanding adolescence as a period of social–affective engagement and goal flexibility. Nature Reviews Neuroscience, 13(9), 636–650. [DOI] [PubMed] [Google Scholar]
- Crosnoe R, & Johnson MK (2011). Research on adolescence in the twenty-first century. Annual Review of Sociology, 37, 439–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuesta I, Montesó‐Curto P, Metzler Sawin E, Jiménez‐Herrera M, Puig‐Llobet M, Seabra P, & Toussaint L (2021). Risk factors for teen suicide and bullying: An international integrative review. International Journal of Nursing Practice, e12930. [DOI] [PubMed] [Google Scholar]
- Czyz EK, Horwitz AG, Arango A, & King CA (2019). Short‐term change and prediction of suicidal ideation among adolescents: a daily diary study following psychiatric hospitalization. Journal of Child Psychology and Psychiatry, 60(7), 732–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czyz EK, Liu Z, & King CA (2012). Social connectedness and one-year trajectories among suicidal adolescents following psychiatric hospitalization. Journal of Clinical Child & Adolescent Psychology, 41(2), 214–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Luca SM, Wyman P, & Warren K (2012). Latina adolescent suicide ideations and attempts: Associations with connectedness to parents, peers, and teachers. Suicide and Life‐Threatening Behavior, 42(6), 672–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan L, Georgiades K, Wang L, Van Lieshout RJ, MacMillan HL, Ferro MA, Lipman EL, Szatmari P, Bennett K, & Kata A (2018). Psychometric evaluation of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Psychological Assessment, 30(7), 916. [DOI] [PubMed] [Google Scholar]
- Durkheim E (1897/1951). Suicide: A study in sociology. Free Press. (Original work published 1897). [Google Scholar]
- Ferguson S, & Zimmer-Gembeck MJ (2014). Associations of parental and peer rejection with preadolescents’ loneliness: emotional sensitivities as mediators. Journal of Relationships Research, 5, 1–11. [Google Scholar]
- Fergusson DM, Woodward LJ, & Horwood LJ (2000). Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine, 30(1), 23–39. [DOI] [PubMed] [Google Scholar]
- Foley DL, Goldston DB, Costello EJ, & Angold A (2006). Proximal psychiatric risk factors for suicidality in youth: The Great Smoky Mountains Study. Archives of General Psychiatry, 63(9), 1017–1024. [DOI] [PubMed] [Google Scholar]
- Foster CE, Horwitz A, Thomas A, Opperman K, Gipson P, Burnside A, Stone DM, & King CA (2017). Connectedness to family, school, peers, and community in socially vulnerable adolescents. Children and Youth Services Review, 81, 321–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fotti SA, Katz LY, Afifi TO, & Cox BJ (2006). The associations between peer and parental relationships and suicidal behaviours in early adolescents. The Canadian Journal of Psychiatry, 51(11), 698–703. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, & Nock MK (2017). Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. [DOI] [PubMed] [Google Scholar]
- Franz PJ, Kleiman EM, & Nock MK (2021). Reappraisal and Suppression Each Moderate the Association Between Stress and Suicidal Ideation: Preliminary Evidence From a Daily Diary Study. Cognitive Therapy and Research, 1–8.34177004 [Google Scholar]
- Gerber J, & Wheeler L (2009). On being rejected: A meta-analysis of experimental research on rejection. Perspectives on Psychological Science, 4(5), 468–488. [DOI] [PubMed] [Google Scholar]
- Gipson PY, Agarwala P, Opperman KJ, Horwitz A, & King CA (2015). Columbia-suicide severity rating scale: predictive validity with adolescent psychiatric emergency patients. Pediatric Emergency Care, 31(2), 88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Esposito EC, Porter AC, & Robinson DJ (2019). Evidence base update of psychosocial treatments for self-injurious thoughts and behaviors in youth. Journal of Clinical Child & Adolescent Psychology, 48(3), 357–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Kleiman EM, Kearns JC, Santee AC, Esposito EC, Conwell Y, & Alpert-Gillis L (2021). Feasibility and acceptability of intensive ecological momentary assessment in high-risk suicidal youth during the post-hospitalization period. Journal of Clinical Child and Adolescent Psychology. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Lanzillo EC, Esposito E, Santee AC, Nock MK, & Auerbach RP (2017). Examining the course of suicidal and nonsuicidal self-injurious thoughts and behaviors in outpatient and inpatient adolescents. Journal of Abnormal Child Psychology, 45(5), 971–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, & Nock MK (2014). Improving the short-term prediction of suicidal behavior. American Journal of Preventive Medicine, 47(3), S176–S180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon J (2017). An experimental therapeutic approach to psychosocial interventions. NIMH Director’s Message. https://www.nimh.nih.gov/about/director/messages/2017/an-experimental-therapeutic-approach-to-psychosocial-interventions [Google Scholar]
- Graham S, & Juvonen J (1998). Self-blame and peer victimization in middle school: an attributional analysis. Developmental Psychology, 34(3), 587. [DOI] [PubMed] [Google Scholar]
- Gunn III JF, Goldstein SE, & Gager CT (2018). A longitudinal examination of social connectedness and suicidal thoughts and behaviors among adolescents. Child and Adolescent Mental Health, 23(4), 341–350. [DOI] [PubMed] [Google Scholar]
- Hallensleben N, Glaesmer H, Forkmann T, Rath D, Strauss M, Kersting A, & Spangenberg L (2019). Predicting suicidal ideation by interpersonal variables, hopelessness and depression in real-time. An ecological momentary assessment study in psychiatric inpatients with depression. European Psychiatry, 56(1), 43–50. [DOI] [PubMed] [Google Scholar]
- Hartgerink CH, Van Beest I, Wicherts JM, & Williams KD (2015). The ordinal effects of ostracism: A meta-analysis of 120 Cyberball studies. PloS one, 10(5), e0127002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill RM, Mellick W, Alvis L, Dodd CG, Do C, Buitron V, Sharp C, Pettit JW, & Kaplow JB (2020). Performance of the interpersonal needs questionnaire in adolescent clinical samples: Confirmatory factor analyses and evaluation of measurement invariance. Suicide and Life‐Threatening Behavior, 50(6), 1214–1222. [DOI] [PubMed] [Google Scholar]
- Hill RM, Rey Y, Marin CE, Sharp C, Green KL, & Pettit JW (2015). Evaluating the Interpersonal Needs Questionnaire: Comparison of the reliability, factor structure, and predictive validity across five versions. Suicide and Life‐Threatening Behavior, 45(3), 302–314. [DOI] [PubMed] [Google Scholar]
- Holt MK, Vivolo-Kantor AM, Polanin JR, Holland KM, DeGue S, Matjasko JL, Wolfe M, & Reid G (2015). Bullying and suicidal ideation and behaviors: a meta-analysis. Pediatrics, 135(2), e496–e509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Robles TF, & Sbarra DA (2017). Advancing social connection as a public health priority in the United States. American Psychologist, 72(6), 517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husky M, Swendsen J, Ionita A, Jaussent I, Genty C, & Courtet P (2017). Predictors of daily life suicidal ideation in adults recently discharged after a serious suicide attempt: a pilot study. Psychiatry Research, 256, 79–84. [DOI] [PubMed] [Google Scholar]
- Ivey-Stephenson AZ, Demissie Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, Lowry R, & Brown M (2020). Suicidal Ideation and Behaviors Among High School Students—Youth Risk Behavior Survey, United States, 2019. MMWR supplements, 69(1), 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JED Foundation. (2017). JED’S Comprehensive Approach to Mental Health Promotion and Suicide Prevention.
- Kaminski JW, Puddy RW, Hall DM, Cashman SY, Crosby AE, & Ortega LA (2010). The relative influence of different domains of social connectedness on self-directed violence in adolescence. Journal of Youth and Adolescence, 39(5), 460–473. [DOI] [PubMed] [Google Scholar]
- Kerr DC, Preuss LJ, & King CA (2006). Suicidal adolescents’ social support from family and peers: Gender-specific associations with psychopathology. Journal of Abnormal Child Psychology, 34(1), 99–110. [DOI] [PubMed] [Google Scholar]
- Kia H, MacKinnon KR, Abramovich A, & Bonato S (2021). Peer support as a protective factor against suicide in trans populations: A scoping review. Social Science & Medicine, 114026. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, & May AM (2015). The three-step theory (3ST): A new theory of suicide rooted in the “ideation-to-action” framework. International Journal of Cognitive Therapy, 8(2), 114–129. [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, & Kupfer DJ (1997). Coming to terms with the terms of risk. Archives of General Psychiatry, 54(4), 337–343. [DOI] [PubMed] [Google Scholar]
- Kyron MJ, Hooke GR, & Page AC (2018). Daily assessment of interpersonal factors to predict suicidal ideation and non-suicidal self-injury in psychiatric inpatients. Journal of Consulting and Clinical Psychology, 86(6), 556. [DOI] [PubMed] [Google Scholar]
- Laursen B, & Collins WA (2009). Parent-child relationships during adolescence. In Lerner RM & Steinberg L (Eds.), Handbook of adolescent psychology: Contextual influences on adolescent development (pp. 3–42). John Wiley & Sons, Inc.. [Google Scholar]
- Lindsey MA, Sheftall AH, Xiao Y, & Joe S (2019). Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics, 144(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, & Ward-Ciesielski EF (2012). Assessing and managing risk with suicidal individuals. Cognitive and Behavioral Practice, 19(2), 218–232. [Google Scholar]
- Liu RT, & Miller I (2014). Life events and suicidal ideation and behavior: A systematic review. Clinical Psychology Review, 34(3), 181–192. [DOI] [PubMed] [Google Scholar]
- Massing-Schaffer M, Nesi J, Telzer EH, Lindquist KA, & Prinstein MJ (2020). Adolescent peer experiences and prospective suicidal ideation: the protective role of online-only friendships. Journal of Clinical Child & Adolescent Psychology, 1–12. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, & Lee S (2008). Suicide and suicidal behavior. Epidemiologic Reviews, 30(1), 133–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-Injurious Thoughts and Behaviors Interview: development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kleiman EM, Abraham M, Bentley K, Brent DA, Buonopane RJ, …, & Pearson J (2021). Consensus statement on ethical & safety practices for conducting digital monitoring studies with those at risk of suicidal and related behaviors. Psychiatric Research and Clinical Practice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ, & Sterba S (2009). Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118(4), 816–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor RC, & Kirtley OJ (2018). The integrated motivational–volitional model of suicidal behaviour. Philosophical Transactions of the Royal Society B: Biological Sciences, 373(1754), 20170268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell L, O’Donnell C, Wardlaw DM, & Stueve A (2004). Risk and resiliency factors influencing suicidality among urban African American and Latino youth. American Journal of Community Psychology, 33(1–2), 37–49. [DOI] [PubMed] [Google Scholar]
- Pisani AR, Murrie DC, & Silverman MM (2016). Reformulating suicide risk formulation: from prediction to prevention. Academic Psychiatry, 40(4), 623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plemmons G, Hall M, Doupnik S, Gay J, Brown C, Browning W, Casey R, Freundlich K, Johnson DP, & Lind C (2018). Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics, 141(6), e20172426. [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, …, & Shen S (2011). The Columbia–Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry, 168(12), 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers KE, Somerville LH, Kelley WM, & Heatherton TF (2013). Rejection sensitivity polarizes striatal–medial prefrontal activity when anticipating social feedback. Journal of Cognitive Neuroscience, 25(11), 1887–1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, & Spirito A (2008). Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of Consulting and Clinical Psychology, 76(1), 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathus JH, & Miller AL (2014). DBT skills manual for adolescents. Guilford Publications. New York, NY. [Google Scholar]
- Ribeiro J, Franklin J, Fox KR, Bentley K, Kleiman EM, Chang B, & Nock MK (2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychological Medicine, 46(2), 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggieri S, Bendixen M, Gabriel U, & Alsaker F (2013). Cyberball: The impact of ostracism on the well-being of early adolescents. Swiss Journal of Psychology, 72(2), 103. [Google Scholar]
- Ryan C, Russell ST, Huebner D, Diaz R, & Sanchez J (2010). Family acceptance in adolescence and the health of LGBT young adults. Journal of Child and Adolescent Psychiatric Nursing, 23(4), 205–213. [DOI] [PubMed] [Google Scholar]
- Santor DA, Messervey D, & Kusumakar V (2000). Measuring peer pressure, popularity, and conformity in adolescent boys and girls: Predicting school performance, sexual attitudes, and substance abuse. Journal of Youth and Adolescence, 29(2), 163–182. [Google Scholar]
- Schacter HL, White SJ, Chang VY, & Juvonen J (2015). “Why me?”: Characterological self-blame and continued victimization in the first year of middle school. Journal of Clinical Child & Adolescent Psychology, 44(3), 446–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiber JB, Nora A, Stage FK, Barlow EA, & King J (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research, 99(6), 323–338. [Google Scholar]
- Shi D, Lee T, & Maydeu-Olivares A (2019). Understanding the model size effect on SEM fit indices. Educational and Psychological Measurement, 79(2), 310–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, & Bolger N (2002). Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods, 7(4), 422. [PubMed] [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, & Joiner TE Jr (2007). Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 2: Suicide-related ideations, communications, and behaviors. Suicide and Life-threatening Behavior, 37(3), 264–277. [DOI] [PubMed] [Google Scholar]
- Sliwinski MJ (2008). Measurement‐burst designs for social health research. Social and Personality Psychology Compass, 2(1), 245–261. [Google Scholar]
- Somerville LH (2013). The teenage brain: Sensitivity to social evaluation. Current Directions in Psychological Science, 22(2), 121–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiner RJ, Sheremenko G, Lesesne C, Dittus PJ, Sieving RE, & Ethier KA (2019). Adolescent connectedness and adult health outcomes. Pediatrics, 144(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JG, Shields GS, Esposito EC, Cosby EA, Allen NB, Slavich GM, & Auerbach RP (2019). Life stress and suicide in adolescents. Journal of Abnormal Child Psychology, 47(10), 1707–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SM, Eaddy M, Horton SE, Hughes J, & Kennard B (2017). The validity of the interpersonal theory of suicide in adolescence: A review. Journal of Clinical Child & Adolescent Psychology, 46(3), 437–449. [DOI] [PubMed] [Google Scholar]
- Suicide Prevention Resource Center. (2020). A Comprehensive Approach to Suicide Prevention. https://www.sprc.org/effective-prevention/comprehensive-approach
- The Trevor Project. (2021). 2021 National Survey on LGBTQ Youth Mental Health. West Hollywood, CA: The Trevor Project. [Google Scholar]
- Townsend KC, & McWhirter BT (2005). Connectedness: A review of the literature with implications for counseling, assessment, and research. Journal of Counseling & Development, 83(2), 191–201. [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, & Joiner TE Jr (2012). Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychological Assessment, 24(1), 197–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE Jr (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock J, Wyman PA, & Moore SR (2014). Connectedness and suicide prevention in adolescents: Pathways and implications. Suicide and Life‐Threatening Behavior, 44(3), 246–272. [DOI] [PubMed] [Google Scholar]
- Wyman PA, Pisani AR, Brown CH, Yates B, Morgan-DeVelder L, Schmeelk-Cone K, Gibbons RD, Caine ED, Petrova M, & Neal-Walden T (2020). Effect of the Wingman-Connect upstream suicide prevention program for Air Force personnel in training: A cluster randomized clinical trial. JAMA Network Open, 3(10), e2022532–e2022532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y, & Lindsey MA (2021). Adolescent social networks matter for suicidal trajectories: disparities across race/ethnicity, sex, sexual identity, and socioeconomic status. Psychological Medicine, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S, Pagano ME, Shea MT, Grilo CM, Gunderson JG, Skodol AE, McGlashan TH, Sanislow CA, Bender DS, & Zanarini MC (2005). Recent life events preceding suicide attempts in a personality disorder sample: findings from the collaborative longitudinal personality disorders study. Journal of Consulting and Clinical Psychology, 73(1), 99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


