Abstract
Background: The development of preventive measures and promotion of healthcare delivery systems for disease management is dependent on detecting the incidence rates of the diseases and important risk factors. The current study aimed to determine some epidemiological indices and trends of the human brucellosis incidence in Iran between 2009 and 2017.
Study design: A descriptive cross-sectional study.
Methods: In the current study, online data were gathered from all cases of brucellosis who were potentially or definitely diagnosed and registered in medical centers, hospitals, laboratories, and private clinics in all districts of Iran. Epidemiologic questionnaires were used to collect data on demographic and background characteristics, risk factors, high-risk behaviors, and lab test results, respectively, based on the national brucellosis control plan.
Results: A total of 138,448 cases of brucellosis have been studied in Iran from 2009 to 2017. The highest (25.89) and the lowest (12.07) incidence rates were observed in 2014 and 2009, respectively. In this nine-year study, the highest incidences were reported in the Hamadan, Lorestan, Kurdistan, and Kermanshah provinces. The cumulative percentages of the disease were estimated for different variables at the following rates: by gender: 57.9% for males; by age groups: 36.2% and 16.7% for the 25-44 and16-24 years age groups, respectively; by occupation: 33.2% for housewives; and by residential area: 75.7% for rural residents.
Conclusions: Based on the obtained results, although the incidence of human brucellosis in Iran has declined since 2015, the number of cases has remained high.
Keywords: Epidemiology, Human brucellosis, Infectious diseases, Iran, Malta fever
Introduction
B rucella is a small gram-negative, facultative intracellular, severely aerobic, and resilient bacteria that cause brucellosis (zoonosis) in cows, sheep, goats, and humans 1 . Based on differences in the main hosts and their pathogenicity, Brucel la is classified into six species. B. abortus causes bovine brucellosis that gives rise to undulant fever (brucellosis) in humans. However, this disease can also be caused by B. melitensis, B. suis, and B. canis 2,3 . Human brucellosis presents a wide range of clinical symptoms and is difficult to diagnose due to its similarity to other diseases 4 . Brucellosis poses an occupational hazard to those in contact with infected animals. A non-occupational source of this disease can be the consumption of fresh unpasteurized dairy products 5 . Other than its serious physical complications, this disease is one of the most challenging factors for economic development in many countries. Upon acquiring the disease, the patients become dependent on others for performing their daily activities due to body weakness which imposes a financial burden on the patient, family, and healthcare system 6 .
The annual reported incidence of new cases of brucellosis is 500,000 cases globally. The prevalence of brucellosis in some countries exceeds 10 cases per 100,000 population. Nevertheless, the reported incidence is lower than the actual rate since for every reported case, there are 26 undiagnosed cases. In endemic regions, the incidence rate ranges from less than 0.03 to more than 200 per 100,000 population. Many regions in the world, such as the Middle East (including Iran), Africa, Latin America, Central Asia, and the Mediterranean region are still considered the endemic areas for brucellosis 7 . In terms of the incidence of brucellosis, Iran ranks fourth in the world and first in the Eastern Mediterranean region 7,8 . One systematic review reported an annual incidence of brucellosis among Middle Eastern countries ranging from 0.73 to 149.54 per 100,000 population. The results of a study conducted in Iran by Mirzanejad et al. (2017) indicated that the incidence of brucellosis ranged from 7.00 to 276.42 per 100,000 population over 18 years 9 .
Brucellosis has become a health priority in different regions of Iran due to the outcomes of the disease on public health and the patient’s social functioning and numerous problems in controlling the disease 10,5 . The development of preventive measures and promotion of healthcare delivery systems for disease management depends on detecting the incidence and prevalence rates as well as important risk factors of brucellosis.
The current study was conducted to determine some of the epidemiological indices and the trend of human brucellosis incidence in Iran between 2009 and 2017.
Methods
The current study was a descriptive cross-sectional one. All cases of brucellosis that were potentially or definitely diagnosed were gathered online from medical centers, hospitals, laboratories, and private clinics in all districts of Iran.
Data were collected via epidemiologic questionnaires, based on the National Brucellosis Control Plan. These questionnaires consisted of three parts:
The first part included items related to demographic and background characteristics, such as age, gender, occupation, and residential area.
The second part included items on risk factors and high-risk behaviors, including the history of contact with livestock, history of livestock vaccination, history of unpasteurized dairy products consumption, type of contact with livestock in the past 18 months, and month of being infected with the disease.
The third part involved items on lab test results, such as the results of the Wright, Coombs Wright, and 2-Mercaptoethanol (2-ME) tests.
The procedure was as follows:
Suspected cases (based on epidemiologic evidence and disease symptoms) were identified and referred to the laboratory by a physician.
Serum samples from the referred cases were prepared in each provincial lab. The Rose Bengal Plate Test (RBPT), as the most common screening test for brucellosis, was first performed on the samples. Next, Wright’s Standard Tube Agglutination Test was performed on samples that were positive by RBPT to confirm the result and determine the titer. Eventually, the 2-ME test was performed on every sample that tested positive in both the RBPT and Wright’s test to measure the immunoglobulin G (IgG) titer as an indicator of the active phase of brucellosis. Following the National Brucellosis Control Plan, a titer of ≥1.40 in the 2-ME test was used as the diagnostic criteria for brucellosis in this study 11 . The laboratory data included in the analysis were based on the Wright and 2-ME tests performed on the serum samples and extracted as titers.
The patients’ characteristics were registered by physicians in the questionnaires with items on demographic and background characteristics, risk factors, and high-risk behaviors, and then reported to the district health center.
All data were registered in the brucellosis report form that was available in all urban health centers and sent to the district health centers through an online portal system.
Complementary data were registered in the epidemiologic examination sheets in the portal system of the district health centers. The data were then sent to the Deputies of Health in the provincial universities of medical sciences.
The disease cases were reported to the Communicable Diseases Center (CDC) of the Ministry of Health and Medical Education by the aforementioned Deputies of Health in each provincial medical university.
The data collected and registered through the previous steps were acquired by the researchers after obtaining the permission from the CDC authority. The data were analyzed using SPSS software (Version 18) and reported afterward. The data were analyzed using descriptive statistical methods and presented by frequencies and percentages. The incidence rates were estimated and reported (yearly) per every 100,000 persons in populations at risk.
The permission for using the national database and records was granted by the Iranian Center for Communicable Diseases Control, Ministry of Health and Medical Education, Tehran, Iran (NO: 304/1309).
Results
A total of 138,448 cases of brucellosis have been studied in Iran from 2009 to 2017.
The cumulative estimated percentages of disease for different variables were as follows: by gender: 57.9% for males; by age: 36.2% and 16.7% for the 25-44 and 16-24-year age groups; and by residential area: 75.7% for rural residents. The cumulative percentages of disease cases based on a positive history of livestock vaccination were 42.2%, 48.8% among those who kept their livestock near their residential area in the previous 18 months, and 28.5% for the consumption of unpasteurized dairy products, such as milk and cheese. Furthermore, throughout the study years, the participants reported a history of contact with livestock (Table 1).
Table 1. Distribution of the relative frequencies of the population with brucellosis based on the studied variables .
| Variable | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |||||||||
| Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | |
| Gender | ||||||||||||||||||
| Male | 4876 | 55.1 | 5811 | 55.4 | 7246 | 56.9 | 9238 | 57.6 | 11446 | 59.9 | 11869 | 58.8 | 11556 | 58.4 | 8970 | 58.4 | 9157 | 57.7 |
| Female | 3969 | 44.9 | 4674 | 44.6 | 5501 | 43.1 | 6360 | 39.7 | 7349 | 38.5 | 8327 | 41.2 | 8247 | 41.6 | 6384 | 41.6 | 6705 | 42.3 |
| Age | ||||||||||||||||||
| <15 | 1153 | 13 | 1528 | 14.6 | 1758 | 13.8 | 2173 | 13.6 | 2585 | 13.5 | 2738 | 13.6 | 2397 | 12.1 | 1811 | 11.8 | 1915 | 12.1 |
| 16 - 24 | 182 | 20.7 | 2098 | 20 | 2545 | 19.9 | 2960 | 18.5 | 3449 | 18.1 | 3383 | 16.8 | 2910 | 14.7 | 2036 | 13.3 | 1916 | 12.1 |
| 25 – 44 | 2965 | 33.5 | 3467 | 33.1 | 4332 | 33.9 | 5447 | 34 | 6511 | 34.1 | 7701 | 38.1 | 7696 | 38.9 | 5889 | 38.4 | 6063 | 38.2 |
| 45 - 54 | 1370 | 15.5 | 1590 | 15.2 | 1938 | 15.2 | 2126 | 13.3 | 2585 | 13.5 | 2935 | 14.5 | 3152 | 15.9 | 2579 | 16.8 | 2639 | 16.6 |
| 55< | 1530 | 17.3 | 1802 | 17.2 | 2192 | 17.2 | 2509 | 15.6 | 2958 | 15.5 | 3439 | 17 | 3648 | 18.4 | 3039 | 19.8 | 3329 | 21 |
| Residential area | ||||||||||||||||||
| Rural | 6898 | 78 | 8099 | 77.2 | 10250 | 80.3 | 12472 | 77.8 | 14482 | 75.8 | 15799 | 78.2 | 15135 | 76.4 | 11404 | 74.3 | 1879 | 74.9 |
| Urban | 1947 | 22 | 2386 | 22.8 | 2515 | 19.7 | 3252 | 20.3 | 4070 | 21.3 | 4214 | 20.9 | 4418 | 22.3 | 3464 | 122.6 | 3667 | 23.1 |
| Nationality | ||||||||||||||||||
| Iranian | 8785 | 99.3 | 10395 | 99.1 | 12631 | 66.1 | 15877 | 83.1 | 18934 | 99.1 | 20022 | 99.1 | 19643 | 97.3 | 15212 | 99.1 | 15660 | 98.7 |
| Afghan | 58 | 0.7 | 86 | 0.8 | 130 | 0.7 | 157 | 0.8 | 165 | 0.9 | 165 | 0.8 | 145 | 0.7 | 129 | 0.8 | 181 | 1.1 |
| Pakistani | 1 | 0 | 2 | 0 | 1 | 0 | - | 2 | 0 | - | - | - | 12 | 0.1 | ||||
| Iraqi | 1 | 0 | 2 | 0 | 2 | 0 | 1 | 0 | - | 6 | 0 | 10 | 0 | 7 | 0 | - | ||
| History of contact with livestock | ||||||||||||||||||
| No | 2248 | 25.4 | 1896 | 18.1 | 2047 | 16 | 2334 | 14.6 | 2889 | 15.1 | 4052 | 20.1 | 2436 | 12.3 | 2177 | 14.2 | 2585 | 16.3 |
| Yes | 6179 | 69.9 | 7929 | 75.6 | 10427 | 81.7 | 12392 | 77.3 | 14664 | 76.8 | 16144 | 79.9 | 15559 | 78.6 | 11721 | 76.3 | 11915 | 75.1 |
| History of livestock vaccination | ||||||||||||||||||
| Yes | 2301 | 26 | 5112 | 48.8 | 7153 | 56 | 8459 | 52.8 | 10405 | 54.5 | 7393 | 36.6 | 7340 | 37.1 | 5136 | 33.51 | 5380 | 33.9 |
| No | 814 | 9.2 | 2533 | 24.2 | 2968 | 23.3 | 3881 | 24.2 | 4672 | 24.5 | 12803 | 63.4 | 5168 | 26.1 | 3648 | 23.8 | 3799 | 24 |
| Unclear | 18 | 0.2 | - | - | 616 | 3.8 | 997 | 5.2 | - | 2852 | 14.4 | 2789 | 18.2 | 3079 | 19.4 | |||
| History of consuming unpasteurized dairy products | ||||||||||||||||||
| Milk | 3516 | 39.8 | 3244 | 30.9 | 4317 | 33.8 | 219 | 1.4 | 30501 | 18.3 | 4276 | 21.21 | 5914 | 29.9 | 4459 | 29 | 4756 | 30 |
| Cheese | 1063 | 12 | 1205 | 11.5 | 1403 | 11 | 39 | 0.2 | 1296 | 6.8 | 1310 | 6.5 | 1587 | 8 | 1162 | 7.6 | 1168 | 7.4 |
| Whipped cream | 69 | 0.8 | 68 | 0.6 | 113 | 0.9 | 5 | 0 | 95 | 0.5 | 44 | 0.2 | 88 | 0.4 | 59 | 0.4 | 69 | 0.4 |
| Butter | 38 | 0.4 | 59 | 0.6 | 92 | 0.7 | 4 | 0 | 78 | 0.4 | 97 | 0.5 | 104 | 0.5 | 75 | 0.5 | 59 | 0.4 |
| Colostrum | 91 | 1 | 160 | 1.5 | 190 | 1.5 | 7 | 0 | 225 | 1.2 | 551 | 2.7 | 299 | 1.5 | 196 | 1.3 | 248 | 1.6 |
| Kaymak | 95 | 1.1 | 264 | 2.5 | 138 | 1.1 | 48 | 0.3 | 170 | 0.9 | 153 | 0.8 | 123 | 0.6 | 166 | 1.1 | 225 | 1.4 |
| Milk and cheese | 3122 | 35.3 | 3748 | 35.7 | 4410 | 34.5 | 284 | 1.8 | 4113 | 21.5 | 7407 | 36.7 | 6346 | 32 | 4918 | 32 | 5058 | 31.9 |
| Ice cream | 45 | 0.5 | 87 | 0.8 | 115 | 0.9 | 5 | 0 | 117 | 0.6 | 155 | 0.8 | 202 | 1 | 139 | 0.9 | 246 | 1.6 |
| None | 174 | 2 | - | - | - | - | - | - | - | - | ||||||||
| Unclear | 231 | 2.6 | - | - | - | - | - | 39 | 0.2 | - | 33 | 0.2 | ||||||
| Type of contact with livestock during the last 18 months | ||||||||||||||||||
| Keeping the animal near one’s residential area | 304 | 3.4 | 1774 | 16.9 | 5617 | 44 | 9362 | 58.4 | 12157 | 63.6 | 10382 | 51.4 | 13483 | 68.1 | 9666 | 63 | 4859 | 30.6 |
| Contact with live animals | 3756 | 42.5 | 3206 | 30.6 | 1447 | 11.3 | 1194 | 7.4 | 2235 | 11.7 | 3217 | 15.9 | 13837 | 1658 | 10.8 | 5724 | 36.1 | |
| Contact with birth secretions and/or the aborted fetus | 682 | 7.7 | 1210 | 11.5 | 2121 | 16.6 | 12.6 | 7.5 | - | - | - | - | 34 | 0.2 | ||||
| Slaughtering the animal | 100 | 1.1 | 659 | 6.3 | 887 | 6.9 | 380 | 2.4 | - | - | 326 | 1.6 | 257 | 1.7 | 1128 | 7.1 | ||
| Contact with the animal corpse and its secretions after its slaughtering | 507 | 5.7 | 708 | 6.8 | 42 | 0.3 | 56 | 0.3 | 305 | 1.6 | 1999 | 7.9 | 218 | 1.1 | 36 | 0.2 | 69 | 0.4 |
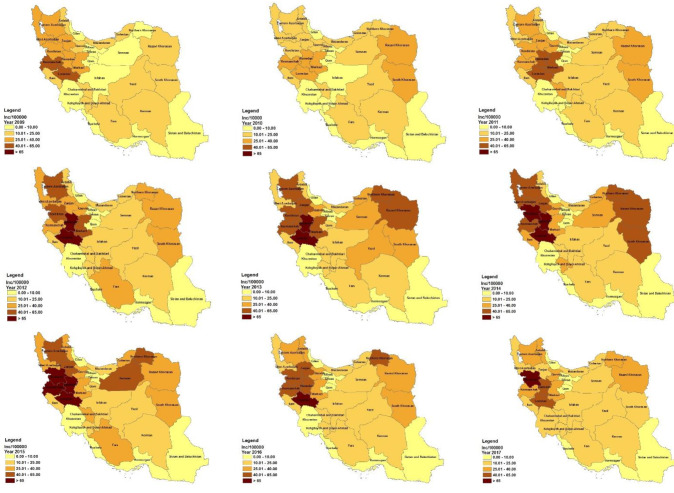
In most of the years studied, the highest numbers of cases of brucellosis were observed in June, July, and August (Figure 1).
Figure 1.
The trend in the numbers of cases of brucellosis according to the month of disease presentation
Based on the results of the present study, the highest number of brucellosis cases during the nine-year study period occurred among farmer-ranchers (4,196), housewives (6,503), and students (2,253), in 2011, 2015, and 2014 respectively.
Based on Wright’s serology, examination of the brucellosis frequency showed that most patients had titers of 1.160 and 1.320 by the Wright and Coombs’ Wright tests (positive cut-off≥1:160), respectively. Furthermore, most patients had titers of 1.80 for the 2-ME test.
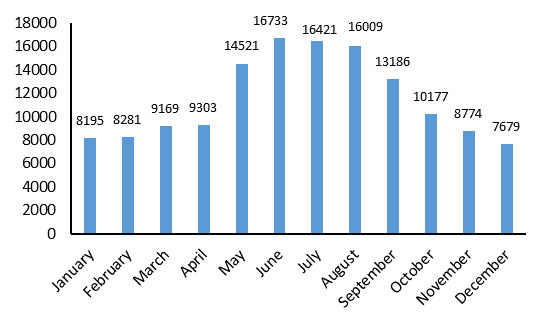
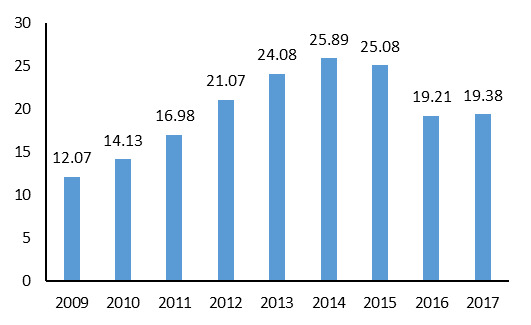
The highest frequency (72.8%) of individuals seropositive for brucellosis by the 2-Mercaptoethanol test was observed in 2016. The highest (25.89 per 100,000 population) and lowest (12.07 per 100,000 population) incidence rates were observed in 2014 and 2009, respectively. Based on the nine-year examination of brucellosis, the highest incidence rates were observed in the Hamedan, Lorestan, Kordestan, and Kermanshah provinces (Figure 2, Table 2). The geographical distribution of brucellosis in Iran between 2009 and 2017 is illustrated in Figure 3.
Figure 2.
The trend of brucellosis incidence in 100,000 population, 2009-2017
Table 2. Frequency and incidence rate of human brucellosis by province .
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | ||||||||||
| Province | Number | Incidence rate | Number | Incidence rate | Number | Incidence rate | Number | Incidence rate | Number | Incidence rate | Number | Incidence rate | Number | Incidence rate | Number | Incidence rate | Number | Incidence rate |
| Eastern Azerbaijan | 937 | 31.27 | 750 | 24.68 | 1063 | 34.50 | 1767 | 56.69 | 1785 | 56.61 | 1628 | 51.03 | 1426 | 44.18 | 1082 | 33.13 | 1237 | 37.31 |
| Ardabil | 210 | 16.93 | 185 | 14.87 | 186 | 14.89 | 183 | 14.60 | 255 | 20.28 | 253 | 20.05 | 506 | 39.98 | 428 | 33.68 | 440 | 33.18 |
| Isfahan | 62 | 1.30 | 366 | 7.60 | 511 | 10.47 | 653 | 13.25 | 954 | 19.17 | 835 | 16.62 | 807 | 15.91 | 763 | 14.89 | 722 | 13.57 |
| Khuzestan | - | - | 387 | 8.64 | 333 | 7.34 | 337 | 7.37 | 439 | 9.61 | 316 | 6.81 | 343 | 7.34 | 282 | 5.98 | 542 | 10.87 |
| Ilam | 116 | 21.16 | 93 | 16.75 | 115 | 20.62 | 126 | 22.41 | 135 | 23.83 | 151 | 26.44 | 139 | 24.15 | 109 | 18.78 | 129 | 20.87 |
| Mazandaran | 316 | 10.86 | 441 | 14.77 | 435 | 14.15 | 565 | 18.14 | 522 | 16.54 | 356 | 11.13 | 412 | 12.71 | 422 | 12.85 | 450 | 13.69 |
| Bushehr | 3 | .3 | 10 | .9 | 28 | 2.71 | 31 | 2.93 | 33 | 3.04 | 56 | 5.04 | 36 | 3.16 | 42 | 3.61 | 34 | 3.11 |
| South Khorasan | 141 | 21.63 | 244 | 37.13 | 194 | 29.28 | 172 | 25.19 | 248 | 35.26 | 415 | 57.28 | 235 | 31.49 | 197 | 25.62 | 144 | 19.79 |
| West Azerbaijan | 108 | 27.45 | 626 | 16.92 | 797 | 21.39 | 1315 | 34.96 | 563 | 14.82 | 1696 | 44.23 | 1325 | 34.22 | 934 | 23.88 | 739 | 21.79 |
| Fars | 580 | 12.91 | 664 | 14.61 | 944 | 20.53 | 1302 | 28.02 | 1166 | 24.82 | 1165 | 24.54 | 1248 | 26 | 970 | 19.99 | 850 | 17.15 |
| Tehran | 186 | 1.57 | 160 | 1.33 | 185 | 1.51 | 248 | 2 | 317 | 2.51 | 348 | 2.71 | 531 | 4.07 | 381 | 2.87 | 327 | 2.01 |
| Kerman | 520 | 18.43 | 451 | 15.66 | 421 | 14.32 | 476 | 15.95 | 580 | 19.15 | 509 | 16.56 | 599 | 19.21 | 502 | 15.86 | 579 | 18.44 |
| Chaharmahal and Bakhtiari | 104 | 11.81 | 135 | 15.21 | 257 | 28.70 | 223 | 24.62 | 201 | 21.94 | 221 | 23.86 | 275 | 29.35 | 135 | 14.24 | 137 | 13.84 |
| Northern Khorasan | 60 | 7.10 | 136 | 15.80 | 206 | 23.74 | 256 | 29.53 | 347 | 40.06 | 404 | 46.69 | 402 | 46.51 | 380 | 44.2 | 326 | 35.47 |
| Sistan and Baluchistan | 72 | 2.90 | 188 | 7.49 | 154 | 6.07 | 112 | 4.33 | 162 | 6.16 | 98 | 3.66 | 82 | 3 | 92 | 3.31 | 161 | 5.22 |
| Razavi Khorasan | 1208 | 20.72 | 1702 | 28.79 | 1957 | 32.64 | 2143 | 35.24 | 2606 | 42.26 | 2508 | 40.10 | 2231 | 35.17 | 1900 | 29.52 | 2608 | 39.30 |
| Semnan | 49 | 7.97 | 97 | 15.58 | 117 | 18.53 | 125 | 19.38 | 220 | 33.40 | 209 | 31.06 | 284 | 41.32 | 138 | 19.46 | 133 | 19.33 |
| Kermanshah | 841 | 43.83 | 721 | 37.32 | 773 | 39.73 | 746 | 38.29 | 1058 | 54.31 | 1241 | 63.66 | 1381 | 70.79 | 841 | 43.07 | 734 | 38.33 |
| Qazvin | 200 | 16.98 | 198 | 16.64 | 313 | 26.04 | 322 | 26.48 | 362 | 29.43 | 448 | 36 | 494 | 39.24 | 411 | 32.26 | 349 | 26.9 |
| Qom | 40 | 3.60 | 74 | 6.55 | 79 | 6.85 | 74 | 6.27 | 142 | 11.77 | 92 | 7.45 | 158 | 12.51 | 80 | 6.19 | 37 | 2.86 |
| Golestan | 263 | 15.46 | 285 | 16.39 | 199 | 11.19 | 344 | 19.16 | 590 | 32.54 | 525 | 28.66 | 507 | 27.40 | 447 | 23.92 | 364 | 18.48 |
| Gilan | 40 | 1.63 | 69 | 2.79 | 66 | 2.66 | 76 | 3.05 | 66 | 2.63 | 60 | 2.39 | 92 | 3.65 | 95 | 3.75 | 78 | 2.95 |
| Lorestan | 831 | 47.79 | 638 | 36.53 | 845 | 48.16 | 1159 | 66.02 | 1277 | 72.69 | 1759 | 100.06 | 2035 | 115.68 | 1420 | 80.65 | 1176 | 62.33 |
| Markazi | 461 | 33.20 | 444 | 31.68 | 599 | 42.36 | 735 | 51.87 | 596 | 41.97 | 510 | 35.84 | 542 | 38.09 | 432 | 30.22 | 437 | 28.40 |
| Alborz | - | - | 26 | 11.13 | 77 | 3.19 | 84 | 3.40 | 162 | 6.40 | 136 | 5.25 | 138 | 5.20 | 131 | 4.82 | 242 | 8.74 |
| Kordistan | 415 | 28.21 | 354 | 23.86 | 536 | 36.64 | 762 | 51.15 | 976 | 64.33 | 1584 | 102.52 | 1319 | 83.83 | 972 | 60.63 | 1250 | 80.16 |
| Kohgiluyeh and Boyer-Ahmad | 116 | 17.88 | 59 | 9.02 | 61 | 9.26 | 68 | 10.16 | 88 | 12.94 | 191 | 27.65 | 130 | 18.52 | 146 | 20.47 | 111 | 15.8 |
| Hormozgan | 32 | 2.12 | 37 | 2.40 | 17 | 1.07 | 22 | 1.36 | 28 | 1.69 | 18 | 1.06 | 15 | .86 | 29 | 1.63 | 25 | 1.42 |
| Hamedan | 436 | 25.12 | 586 | 33.55 | 835 | 47.48 | 1144 | 65.20 | 1498 | 85.57 | 1681 | 96.23 | 1305 | 74.87 | 882 | 50.74 | 894 | 50.44 |
| Yazd | 142 | 13.65 | 130 | 12.29 | 170 | 15.82 | 135 | 12.42 | 281 | 25.55 | 166 | 14.92 | 215 | 19.10 | 154 | 13.52 | 171 | 13.81 |
| Zanjan | 256 | 25.73 | 229 | 22.78 | 290 | 28.55 | 312 | 30.47 | 446 | 43.21 | 617 | 59.30 | 591 | 56.35 | 549 | 51.91 | 435 | 40.02 |
| Total | 8845 | 12.07 | 10485 | 14.13 | 12765 | 16.98 | 16035 | 21.07 | 19103 | 24.80 | 20196 | 25.89 | 19803 | 25.08 | 15354 | 19.21 | 15862 | 19.38 |
Figure 3.
Geographical distribution of brucellosis in Iran between 2009 and 2017.
Discussion
A total of 138,448 cases of brucellosis were observed over the nine-year study period. The incidence rate of the disease ranged from 12.07 to 25.89. An increasing trend was observed until 2014, which may have been due to the public’s lack of awareness of preventive measures, consequences of consuming unpasteurized dairy products, lack of livestock vaccination, issues related to the statistical system, and absence of accurate registration of data in the portal system for diseases during these years.
Esmaeili et al. suggested that a number of cases were undiagnosed, particularly in poor and remote provinces. However, the performance of the health surveillance system has improved in recent years in Iran. With the expansion of the healthcare system, one would expect the number of reported cases to increase 12 . Nevertheless, the results of the present study indicates a declining trend in the disease from 2015 until 2017. This decline may be attributed to increased awareness about the modes of disease transmission and preventive measures through the education of ranchers and those in contact with raw livestock products. Furthermore, the increased vaccination coverage of lambs and care of infected and suspected cases of livestock can contribute to the prevention of disease spread in the community. Compared to the incidence rates of brucellosis in some countries (not exceeding 10 cases per 100,000 population), the results of this study indicate that the disease is endemic in Iran. In endemic regions, the incidence rate ranges from 0.03 to 200 cases per 100,000 population. However, for every reported case there may be 26 undiagnosed cases indicating that the incidence rate of the disease may be much higher 13,14 . Based on the results of the study conducted by Rostami et al. (2015) on 1,698 patients across 30 provinces in Iran, the estimated mean incidence of brucellosis was 29.83 per 100,000 population 15 . Despite the observation of a declining trend in recent years, the geographical location of Iran and its adjacency to endemic countries, such as Iraq, Pakistan, and Afghanistan are important risk factors for the re-emergence and spread of brucellosis. Although high-quality veterinary services have been delivered to these countries to control animal diseases, the danger of the disease spreading from country to country still persists 12 .
Based on the results of the present study, the rate of brucellosis has remained high in Iran in recent years (at least in some provinces, such as Razavi Khorasan and Kordestan). Inaccurate laboratory diagnostics might be an important reason for the persistently high rate of brucellosis in Iran. False-negative cases during culturing, tubal agglutination, and the higher antibody titers among ordinary people in endemic regions have led to the reduced efficiency of these methods. The failure to use molecular methods or other diagnostic techniques in many medical centers and laboratories across the country further complicates the diagnosis of the disease. Other than the absence of appropriate and alternative verification methods, there are limiting diagnostic factors, such as the low quality of kits available in the market and the absence of a comprehensive seroepidemiologic study that can determine the diagnostic level of specific antibodies through serological techniques 16,17 .
The results of this nine-year study indicated the highest incidence rates in the provinces of Hamedan, Lorestan, Kordestan, and Kermanshah in Iran. The classification conducted in 2010 showed that among all provinces, Kermanshah, Lorestan, Kordestan, and Hamedan had the highest incidence rates of brucellosis. These provinces fall in the ‘very high’ category 13,18 , indicating that, despite the steps taken to control the disease, the incidence rates have remained high. Health policy-makers need to plan for public education (particularly during months in which the probability of incidence is higher), expand livestock vaccination, continually assess disease control programs and follow-ups, and address administrative issues.
According to the obtained results, the disease is mostly present in males. This finding is concordant with those of other studies conducted across Iran’s provinces 15,11-21 . Nevertheless, throughout the years of this study, the percentages of cases of disease remained similar in both genders. In this respect, Azizi et al. (2010) believe that since women work alongside men in such occupations as ranching and farming, the number of cases is high among women as well. Moreover, women are in contact with the causative agent and can inhale it while milking the animals and cleaning their shelters 22 . Incorrect habits of food consumption among the Iranian society, such as the consumption of meat products and offal with insufficient cooking due to inadequate information on the routes of disease transmission may also contribute to the increase in the number of brucellosis cases in both genders.
The highest percentages of cases were observed in the 16-24 and 25-44 years age groups. This may be explained by these age groups’ occupational exposures and involvement in ranching, farming, butchering, and slaughtering livestock. Most studies conducted in Iran have also reported the highest number of brucellosis cases among adolescent and young adult age groups 18,2,2 . According to Zeinalian Dastjerdi et al. (2012), given the risk of contact with infected animals and their products, the mean age of the affected cases was 31.3 years 23 . Nevertheless, other studies have reported a peak of cases in the age group older than 50 years 20 .
In this study, the most common mode of infection was through the consumption of unpasteurized dairy products, such as milk and cheese. Keeping livestock in residential areas and contact with live animals were the main routes of transmission. Based on numerous reports, the dominant route of Brucella transmission to humans is through the digestive tract (i.e., the consumption of unpasteurized dairy products, such as fresh milk and other milk-derived products, particularly whipped cream and ice cream, which contain high levels of the bacteria) 13 . Moreover, consistent with the literature, the highest number of cases were observed in rural areas 12,24-25 .
The highest numbers of cases were observed in the second and third months of spring and the first month of summer. According to Golshani et al. (2017), the incidence of brucellosis increases during spring and summer as the ranchers are in direct contact with aborted fetuses, and infected dairy products are consumed 10 . The global seasonal pattern of brucellosis indicates that the disease is more common in the first half of the year, during the animal reproduction period 24 . The seasonal pattern of brucellosis in Iran was also assessed in a meta-analysis, which reported the highest prevalence in the spring and summer and the lowest prevalence during the autumn and winter months 24 .
It was observed that housewives were most affected by the disease since they worked alongside men and were responsible for milking animals. Moreover, they lived in a contaminated environment and inhaled the causative agent due to the adjacency of their residential areas to animal shelters, which exposed them to the disease. Farmer-ranchers have the second most common occupation affected by brucellosis. Brucellosis is usually considered an occupational disease, as it is most commonly observed among slaughterhouse workers, veterinary doctors, laboratory technicians, hunters, farmers, and ranchers 26 .
Conclusions
Although brucellosis has witnessed a declining trend in Iran since 2015, the number of infected cases has remained high. Given the high number of recurrent cases 27 , changes in the epidemiologic pattern of the disease, and clinical factors, research should focus on the epidemiologic cases of the disease in different regions of Iran. Male gender, adolescent and young adult age groups, housewives and farmer-rancher occupations, and warm seasons of the year are probable risk factors for brucellosis in humans. Advanced surveillance systems that are focused on probable risk factors can effectively protect against the disease. Comprehensive measures need to be taken to control the routes of disease transmission from domesticated animals and their products to humans. Preventive measures must also be taken by health officials and health service providers. In this regard, the following measures are recommended:
Frequent visits must be made to restaurants and dining halls across the city as well as various centers responsible for the distribution, storage, and supply of raw livestock products, such as centers providing red and white meat, chain stores, centers supplying poultry products, and butcheries.
The Brucella test must be conducted on animals and positive cases must be slaughtered in industrial and semi-industrial cattle farms.
Given the high number of cases among men and housewives, educating these people on disease prevention in contact with animals can help control the disease. Such measures as the provision of education on the significance of the correct handwashing procedure with soap and water, application of gloves and face masks in contact with affected livestock and when cleaning the affected livestock’s shelter, and proper air conditioning can all prevent infection in these individuals.
Given the increased number of cases during the spring and summer months, education, therapeutic interventions, and screening should be increased during the seasons in which disease transmission is higher.
The culture of consuming pasteurized dairy products should be institutionalized in society to achieve this goal. The Department of Education and Health Networks can play significant roles in schools and across urban and rural areas, respectively.
The provision of continuous education through health service providers and mass media campaigns are required to raise awareness about the modes of disease transmission, symptoms, and methods of disease prevention.
The expansion of intersectoral collaborations among veterinary clinics, governorates, prefectures, village administrators, non-governmental organizations, teachers, and all classes of society (particularly journalists, etc.) are strategies to reduce the incidence of the disease. Education on the significance of vaccinating livestock and the introduction of centers providing this service, especially to rural inhabitants, are indicated as well.
Acknowledgments
The authors would like to thank the personnel at the urban and rural health centers and all those who helped to register and collect the data.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this study.
Funding
This study was not financially supported by any governmental, private, or non for profit organization or institute.
Authors’ contributions
F.GH. and F.N. wrote the manuscript; H.E., A.N., and F.K. collected the data and reviewed/edited the manuscript; F.GH. and F.N. contributed to the discussion section and reviewed/edited the manuscript, and F.GH. collected the data and contributed to the discussion section.
Highlights
A total of 138,448 cases of brucellosis were studied in Iran from 2009 to 2017.
The highest (25.89) and the lowest (12.07) incidence rate was observed in 2014 and 2009, respectively.
The highest incidence rates were reported in Hamadan, Lorestan, Kurdistan, and Kermanshah provinces.
Citation: Norouzinezhad F, Erfani H, Norouzinejad A, Ghaffari F, Kaveh F. Epidemiological Characteristics and Trend in the Incidence of Human Brucellosis in Iran from 2009 to 2017. J Res Health Sci. 2021; 21(4): e00535.
References
- 1.Seleem MN, Boyle SM, Sriranganathan N. Brucellosis: a re-emerging zoonosis. Vet Microbial. 2010;140(3-4):392–8. doi: 10.1016/j.vetmic.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 2. Silva T, Costa EA, Paixão TA, Tsolis RM, Santos RL. Laboratory animal models for brucellosis research. BioMed Research International. 2011. [DOI] [PMC free article] [PubMed]
- 3.Assadi M, Siyadatpanah A, Soufiani KB, Mobayyen H, Sadighbayan K, Asadi J. et al. Brucellosis in Iran: a literature review. J Am Sci. 2013;9(3):203–8. [Google Scholar]
- 4.Hashtarkhani S, Akbari M, Jarahi L, Etminani K. Epidemiological characteristics and trend of incidence of human brucellosis in Razavi Khorasan province. Medical Journal of Mashhad University of Medical Sciences. 2015;58(9):531–8. [Google Scholar]
- 5.Blasco JM, Molina-Flores B. Control and eradication of Brucella melitensis infection in sheep and goats. Vet Clin North Am Food Anim Pract. 2011;27(1):95–104. doi: 10.1016/j.cvfa.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Maleki F, RafieManesh H, Abbasi-Ghahramanloo A, Ghadimi N, Kousha A, Safiri S. Epidemiological characteristics of human brucellosis in Shahin Dezh, western Azarbaijan, Iran, 2008-2012. Archives of Clinical Infectious Diseases. 2015;10(1):e22279. [Google Scholar]
- 7.Mohammadian M, Mohammadian HA. Epidemiological characteristics and incidence rate of brucellosis over a period of 14 years in the Tiran-Karvan Township, Isfahan, Iran. Journal of Isfahan Medical School. 2014;32(293):1103–9. [Google Scholar]
- 8.Soleimani A, Alizadeh S, Farshad MS, Kusha A, Mohamdzadeh M, Haghiri L. et al. Descriptive Epidemiology of Human Brucellosis in East Azerbaijan, 2001-2009. Medical Journal of Tabriz University of Medical Sciences & Health Services. 2012;34(1):63–9. [Google Scholar]
- 9.Mirnejad R, Jazi FM, Mostafaei S, Sedighi M. Epidemiology of brucellosis in Iran: A comprehensive systematic review and meta-analysis study. Microb Pathog. 2017;109:239–47. doi: 10.1016/j.micpath.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Golshani M, Buozari S. A review of Brucellosis in Iran: Epidemiology, Risk Factors, Diagnosis, Control, and Prevention. Iran Biomed J. 2017;21(6):349–59. doi: 10.18869/acadpub.ibj.21.6.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zeinali M SM, Haj rasuliha H National Guideline for Brucellosis Control. Tehran: Raz Nahan Publishing; 2012.
- 12.Esmaeili H. Brucellosis in Islamic republic of Iran. J Med Bacteriol. 2015;3(3-4):47–57. [Google Scholar]
- 13.Fallah Rostami F, Borzoueisileh S, Ebrahimpour S. An overview of brucellosis epidemic in Iran. Crescent Journal of Medical and Biological Sciences. 2016;3(1):35–6. [Google Scholar]
- 14.Yang X, Skyberg JA, Cao L, Clapp B, Thornburg T, Pascual DW. Progress in Brucella vaccine development. Front Biol. 2013;8(1):60–77. doi: 10.1007/s11515-012-1196-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rostami H, Tavana AM, Tavakoli HR, Tutunchian M. Prevalence study of brucellosis in Iranian military forces during 2001-2009. Journal of Health Policy and Sustainable Health. 2015;2(2):191–4. [Google Scholar]
- 16.Hajia M, Jazi FM. Looking Again at the Diagnosis of Brucellosis Difficulties in Iran. Iran J Med Microbiol. 2018;12:68–77. [Google Scholar]
- 17.Hajia M. The Challenges in Diagnosis of Brucellosis Serological Tests and Available Approaches. Iran J Med Microbiol. 2018;12(1):1–5. [Google Scholar]
- 18.Sofian M, Aghakhani A, Velayati AA, Banifazl M, Eslamifar A, Ramezani A. Risk factors for human brucellosis in Iran: a case–control study. Int J Infect Dis. 2008;12(2):157–61. doi: 10.1016/j.ijid.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 19.Farahani S, Shahmohamadi S, Navidi I, Sofian S. An investigation of the epidemiology of brucellosis in Arak City, Iran, (2001-2010) J Arak Uni Med Sci. 2012;14(7):49–54. [Google Scholar]
- 20.Ramezani Avval Riabi H, Razmara H. Epidemiological Feature of the Human Brucellosis Prevalence in People in Southern Cities of Khorasan Razavi, Iran. Zahedan Journal of Research in Medical Sciences. 2017;19(4):e7911. [Google Scholar]
- 21. Azizi F, Hatami H, Janghorbani M. Epidemiology and control of common diseases in Iran. Tehran, Eshtiagh Pub; 2007.
- 22.Pakzad R, Barati M, Moludi J, Barati H, Pakzad I. Epidemiology of Brucellosis in the North and North-West Iran. Paramedical Sciences and Military Health. 2016;11(1):17–23. [Google Scholar]
- 23.Dastjerdi MZ, Nobari RF, Ramazanpour J. Epidemiological features of human brucellosis in central Iran, 2006–2011. Public Health. 2012;126(12):1058–62. doi: 10.1016/j.puhe.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Moosazadeh M, Abedi G, Kheradmand M, Safiri S, Nikaeen R. Seasonal pattern of brucellosis in Iran: A systematic review and meta-analysis. Iranian Journal of Health Sciences. 2016;4(1):62–72. [Google Scholar]
- 25.Mostafavi E, Asmand M. Trend of brucellosis in Iran from 1991 to 2008. Iranian Journal of Epidemiology. 2012;8(1):94–101. [Google Scholar]
- 26. Corbel MJ. Brucellosis in humans and animals. Geneva: WHO; 2006.
- 27.Nematollahi S, Ayubi E, Karami M, Khazaei S, Shojaeian M, Zamani R. et al. Epidemiological characteristics of human brucellosis in Hamadan Province during 2009–2015: results from the National Notifiable Diseases Surveillance System. Int J Infect Dis. 2017;61:56–61. doi: 10.1016/j.ijid.2017.06.002. [DOI] [PubMed] [Google Scholar]