Abstract
Background
Emerging literature has documented heat‐related impacts on child health, yet few studies have evaluated the effects of heat among children of different age groups and comparing emergency department (ED) and hospitalisation risks.
Objectives
To examine the differing associations between high ambient temperatures and risk of ED visits and hospitalisations among children by age group in New York City (NYC).
Methods
We used New York Statewide Planning and Research Cooperative System (SPARCS) data on children aged 0–18 years admitted to NYC EDs (n = 2,252,550) and hospitals (n = 228,006) during the warm months (May‐September) between 2005 and 2011. Using a time‐stratified, case‐crossover design, we estimated the risk of ED visits and hospitalisations associated with daily maximum temperature (Tmax) for children of all ages and by age group.
Results
The average Tmax over the study period was 80.3°F (range 50°, 104°F). Tmax conferred the greatest risk of ED visits for children aged 0–4, with a 6‐day cumulative excess risk of 2.4% (95% confidence interval [CI] 1.7, 3.0) per 13°F (ie interquartile range) increase in temperature. Children and adolescents 5–12 years (0.8%, 95% CI 0.1, 1.6) and 13–18 years (1.4%, 95% CI 0.6, 2.3) are also sensitive to heat. For hospitalisations, only adolescents 13–18 years had increased heat‐related risk, with a cumulative excess risk of 7.9% (95% CI 2.0, 14.2) per 13°F increase in Tmax over 85°F.
Conclusions
This urban study in NYC reinforces that young children are particularly vulnerable to effects of heat, but also demonstrates the sensitivity of older children and adolescents as well. These findings underscore the importance of focussing on children and adolescents in targeting heat illness prevention and emergency response activities, especially as global temperatures continue to rise.
Keywords: ambient temperature, children and adolescents, climate‐sensitive exposures, emergency department visits, heat risk, hospitalisations, New York City, urban environments
Synopsis.
1. Study question
Are higher ambient temperatures associated with increased risk of emergency department visits and hospitalisations among children from 0 to 18 years and across different age groups?
2. What's already known
Emerging literature has documented heat‐related impacts on child health. As most prior studies have examined heat impacts among infants and young children under age 4 years, our knowledge of heat impacts remains limited across the age range of childhood and adolescence.
3. What this study adds
Using a time‐stratified, case‐crossover design, we found that higher warm‐season ambient temperatures are associated with increased risk of emergency department visits and hospitalisations among children from 0 to 18 years. These findings demonstrate that young children, as well as older children and adolescents, are sensitive to heat effects.
1. BACKGROUND
Hot weather is associated with considerable morbidity. 1 Children may be uniquely vulnerable to the adverse impact of heat due to physiological and developmental factors; 2 , 3 they have greater body surface‐to‐volume ratio and lesser ability to regulate core body temperature, are more prone to behaviours that increase exposure (eg outdoor play) and are less able to self‐care compared to adults. 4 , 5 Higher summertime average temperatures, as well as more frequent, more intense, longer heat waves, are projected for the future. 6 , 7 , 8 Thus, increases in ambient temperatures because of climate change represent a major threat to children's health. 9 As such, addressing the impact of elevated temperatures on child morbidity is an important public health concern. 2 , 9 , 10 Children living in urban areas—where the majority and a growing proportion of the global population reside 11 —are exposed to higher temperatures during the day and the night, due to the urban heat island effect. 12 New York City (NYC) is the most populated city in the United States (US), with a high population density that further amplifies heat‐related health impacts. NYC has already experienced rising temperatures, and hotter temperatures are expected in the coming decades. 6
Emerging literature has documented heat‐related impacts on child health. 13 , 14 , 15 , 16 For example, Schinasi et al. 14 observed that higher minimum daily temperatures conferred a greater mortality risk among infants younger than 12 months in Philadelphia. Another study reported that a higher maximum temperature was associated with increased risk of emergency department visits among children 0 to 4 years in NYC. 13 While most studies have examined heat impact among infants and children under age 4 years, our knowledge of heat impacts remains limited across the age range of childhood and adolescence. Only a few studies have evaluated the effects of heat exposure on all‐age children, 13 , 14 , 15 , 16 and, of these, even fewer have evaluated effects comparing emergency department and hospitalisation risks among different age groups of children. We investigate the associations between high ambient temperatures and emergency department (ED) visits and hospitalisations among children and adolescents and to identify vulnerable subpopulations of heat susceptibility. We hypothesised that temperature would increase the risk of ED visits and hospitalisations among children and that younger children would have greater susceptibility to heat compared to older children and adolescents.
2. METHODS
2.1. Health data
We used all ED visit (outpatient) and hospitalisation (inpatient) records for children aged 0 to 18 years in NYC from 2005 to 2011 New York Statewide Planning and Research Cooperative System (SPARCS). SPARCS is a comprehensive, statewide, all‐payer administrative database that collects patient‐level data from all hospital ED visits and inpatient stays. 17 We restricted the analysis to NYC ED visits and hospitalisations that occurred during the warm months of 2005–2011 (May to September), because we were interested in studying the effect of hot temperature on child morbidity, 13 and this restriction allowed us to avoid the complexity of modelling associations with both hot and cold temperatures. SPARCS data included the date, month and year of each ED visit and hospitalisation. Each record in SPARCS represented a single ED visit or hospitalisation; no distinction was made between an initial visit and recurrent admission as records are not linked. We examined ED visits and hospitalisations as separate outcomes.
2.2. Climate exposure data
We downloaded data on daily maximum temperature, minimum temperature and mean temperature recorded by the four meteorological stations in the NYC area (JFK International Airport, LaGuardia Airport, Central Park, Newark International Airport; Figure S1) from the National Oceanic and Atmospheric Administration (NOAA) National Climate Data Center (NCDC). 18 We chose to use temperature data from LaGuardia Airport as a single site was most parsimonious and prior work had demonstrated high correlation between the stations (rs > 0.93). 19 We chose to use maximum temperature as our main exposure variable because it was tightly correlated with minimum temperature (r = 0.87) and mean temperature (r = 0.97) at this spatial resolution, and it provided the best fit for heat‐health models in children in several prior studies. 13 , 20 , 21 We calculated relative humidity (RH) from mean temperature and dew point temperature using the standard NOAA equation. 22 We linked the daily maximum temperature and RH data to each ED visit and inpatient hospitalisation based on the date of the visit.
2.3. Statistical analysis
We conducted a time‐stratified, case‐crossover study 23 to evaluate associations between ambient temperatures and the risk of ED visits and hospitalisations. For every child 0–18 years of age who had an ED visit or hospital admission, we defined each date of visit as a case day. We used a time‐stratified strategy to identify control days based on same day of the week within the same month of the year, resulting in 3 or 4 control days per case. 24 For example, if a child had an ED visit on a Friday in August 2011, then we compared the temperature on that day with the temperature on all other Fridays in August 2011. By selecting control days on the same day of the week as the case day and within the same month, the analysis adjusts for long‐term time trends, seasonality and day of week. 14 Confounding by individual‐level characteristics such as age, sex, race/ethnicity and socioeconomic position is inherently adjusted for, since cases serve as their own controls by design. 23
We used conditional logistic regression models to estimate associations between temperature and ED visits or hospitalisations among children. Rather than analysing temperature at separate lags, we used the distributed lag non‐linear models (DLNMs) to account for the delayed and possible non‐linear effects of temperature on the risk of ED visits and hospitalisations. 25 We selected a lag period of 6 days for the effect of daily maximum temperature (Tmax; lag 0 to lag 5), where lag 0 day corresponds to the case or control day. We selected these lag periods a priori, based on previous research showing that the heat effects on child morbidity are relatively acute, with the most adverse effects of heat apparent within several days. 26 We used a constrained linear structure for the lag‐response function to improve the precision in estimating the distributed lag curve. 27 In preliminary analyses, we first estimated the association between Tmax and ED visits and hospitalisations by modelling Tmax as a continuous term, using natural cubic splines with 3 degrees of freedom (df). We selected the degrees of freedom after comparing the model fit statistics (ie Akaike information criterion) of several alternative parameterisations (4, 5 and 6 df). We controlled for RH using a natural spline with 3 df, as humidity can increase physiological heat stress particularly when the temperature is high leading to increased morbidity. 28 We developed separate models for the two outcomes (ED visits and hospitalisations), and we used the results of these models to select the best functional form of Tmax to include in the main analyses.
After examining the shape of the temperature‐response associations from the preliminary spline term model results (Figures 1 and 2), we ran our main analysis using a modified linear modelling approach to maximise interpretability. Specifically, we ran the main analyses with Tmax parameterised as a linear term for ED visits models. For hospitalisation models, we ran Tmax as a piecewise linear term, coded as zero for temperatures less than 85°F, and as Tmax minus 85°F, at or above 85°F, for days on which Tmax exceeded 85°F. The piecewise approach has been used in previous analyses to quantify associations of temperature exposures with health outcomes and is appropriate for parameterising the effect of an exposure which is linear above a threshold value. 14 We chose the threshold by visual inspection of plots on the association between temperature and hospitalisations. A temperature of 85°F represents the 75th percentile of the distribution of Tmax, and it allowed us to evaluate increases in heat‐related risk above a meaningful high temperature threshold, while retaining a sufficient sample size for estimation. We estimated the excess risk of ED visits per interquartile range (IQR, 13°F) increase in Tmax, as well as the excess risk of hospitalisations per 13°F increase in Tmax over 85°F. We reported the excess risk of ED visit and hospitalisations accumulated over lag days 0 to 5 (referred to as the ‘cumulative’ lag), as well as at individual lag days.
FIGURE 1.
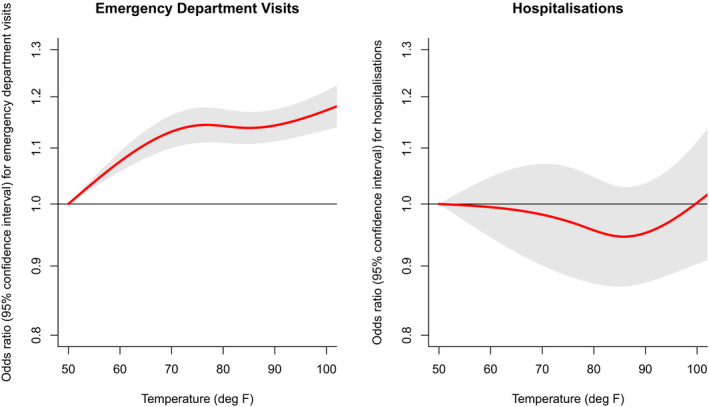
Odds ratio (ORs) and 95% confidence intervals of emergency department visits and hospitalisations associated with daily maximum temperature, relative to the reference temperature (50°F), cumulative over lag days 0–5 [Colour figure can be viewed at wileyonlinelibrary.com]
FIGURE 2.
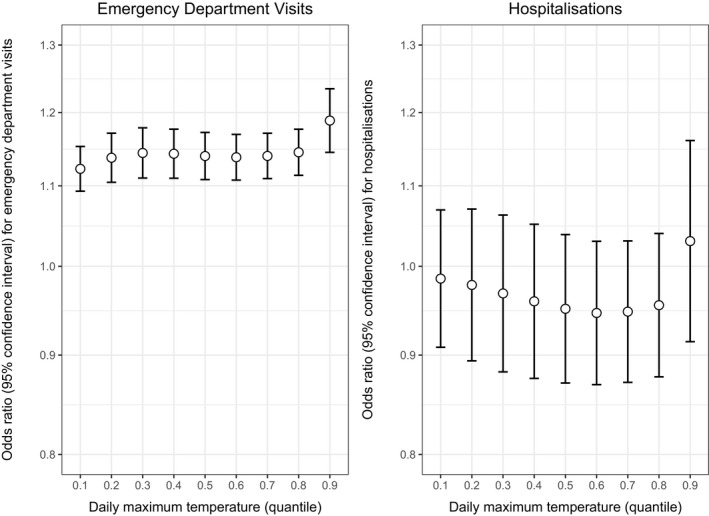
Odds ratio (ORs) and 95% confidence intervals of emergency department visits and hospitalisations across quantiles of daily maximum temperature, relative to the reference temperature (50°F), cumulative over lag days 0–5
To examine effect modification of heat vulnerability by age, we stratified the analysis by three age groups (0–4, 5–12 and 13–18 years). While the analyses of ED visits among children 0–4 years overlap with a prior publication from our team, 13 the current study expands on that work by evaluating the effect of heat exposure on both ED visits and hospitalisations and adds additional age groups of children and adolescents up to 18 years of age. We also examined variations in the associations of Tmax with ED visits and hospitalisations by stratifying analyses by categories of sex (male and female), race/ethnicity (Hispanic, non‐Hispanic White, non‐Hispanic Black, non‐Hispanic Other) and six specific diagnostic categories (general symptoms, injury, respiratory illness, viral and ear infections, heat‐related illness and digestion‐related illness).
To test the sensitivity of our results to the choice of temperature metrics, we reran the main analyses using minimum temperature and maximum heat index, a metric reflecting perceived temperature based on maximum temperature and relative humidity. 22 All statistical analyses were conducted using the R statistical software version 4.0.2 (R Core Team 2015) with the ‘dlnm’ and ‘coxph’ packages. 29
2.4. Ethics approval
Institutional review boards at Icahn School of Medicine at Mount Sinai, Drexel University and the University at Pittsburgh approved this study.
3. RESULTS
In New York City, there were 2,252,500 ED visits and 228,006 hospitalisations for children aged 0–18 years from May through September between 2005 and 2011 (Table 1). The largest proportion of ED visits occurred among children 0 to 4 years (44.6%), followed by children 5 to 12 years (31.0%) and adolescents 13–18 years (24.5%). Among inpatient hospitalisations, 42.7% were among children 0 to 4 years, followed by adolescents 13–18 years (33.2%) and children 5–12 years (27.4%). Just under half of the children were female (47.0% ED visits and 48.4% hospitalisations). Roughly two‐thirds of the patients were either Hispanic (32.4% ED visits and 30.6% hospitalisations) or non‐Hispanic Black (33.1% ED visits and 30.6% hospitalisations). The range of maximum temperatures over the study period was 50°F to 104°F, with a mean of 80.3°F (standard deviation = 9.1°F, IQR = 13°F). The average relative humidity was 62.4% (range 28.5, 93.2).
TABLE 1.
Descriptive statistics of New York City emergency department visits and hospitalisations from May to September, 2005–2011
| Characteristics | Emergency department visits (n = 2,252,550) | Hospitalisations (n = 228,006) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Age (years) | ||||
| 0–4 | 1,003,993 | 44.6 | 97,430 | 42.7 |
| 5–12 | 697,221 | 31.0 | 54,972 | 27.4 |
| 13–18 | 551,336 | 24.5 | 75,604 | 33.2 |
| Female sex | 1,059,675 | 47.0 | 110,336 | 48.4 |
| Race/ethnicity | ||||
| Hispanic | 729,618 | 32.4 | 69,661 | 30.6 |
| Non‐Hispanic Black | 746,141 | 33.1 | 70,854 | 31.1 |
| Non‐Hispanic Other | 526,818 | 23.4 | 48,593 | 21.3 |
| Non‐Hispanic White | 240,617 | 10.7 | 36,607 | 16.1 |
| Unknown | 9156 | 0.4 | 2291 | 1.0 |
3.1. ED visits
In our main ED visit models with maximum temperature parameterised as a linear term (Table 2), a 13°F (IQR) increase in Tmax was associated with a 6‐day cumulative excess risk of 1.6% (95% CI 1.2, 2.1) of ED visits for children of all ages. We observed elevated risk of ED visits associated with Tmax on lag days 0 through 3, peaking at lag day 0. Tmax was associated with a decreased risk on lag days 4 and 5, possibly showing a partial offset of ED visits, similar to the harvesting effect seen in some mortality studies. 30 , 31 , 32
TABLE 2.
Per cent excess risk and 95% confidence intervals for emergency department visits per 13°F increase in overall daily maximum temperature over lags 0–5 days for children aged 0–18 years living in New York City, 2005–2011, overall and by age groups
| Lag day | Overall (0–18 years) | Age 0–4 years | Age 5–12 years | Age 13–18 years |
|---|---|---|---|---|
| Lag0 | 1.06 (0.90, 1.23) | 1.23 (0.99, 1.48) | 0.93 (0.64, 1.22) | 0.91 (0.58, 1.24) |
| Lag1 | 0.75 (0.63, 0.86) | 0.89 (0.73, 1.06) | 0.61 (0.41, 0.81) | 0.64 (0.41, 0.87) |
| Lag2 | 0.43 (0.35, 0.51) | 0.56 (0.44, 0.67) | 0.29 (0.16, 0.43) | 0.37 (0.22, 0.52) |
| Lag3 | 0.11 (0.04, 0.19) | 0.22 (0.11, 0.33) | −0.02 (−0.15, 0.11) | 0.10 (−0.05, 0.25) |
| Lag4 | −0.20 (−0.31, −0.09) | −0.12 (−0.28, 0.05) | −0.33 (−0.53, −0.14) | −0.17 (−0.39, 0.05) |
| Lag5 | −0.52 (−0.68, −0.36) | −0.45 (−0.69, −0.21) | −0.65 (−0.93, −0.36) | −0.44 (−0.76, −0.11) |
| Cumulative | 1.63 (1.21, 2.06) | 2.35 (1.71, 3.00) | 0.83 (0.08, 1.59) | 1.42 (0.56, 2.28) |
All models adjusted for relative humidity using a national spline with 3 degrees of freedom.
Age‐stratified analyses showed cumulative heat effects for each age group, with the strongest heat vulnerability observed for children 0–4 years, followed by children 13–18 years and children 5–12 years (Table 2). Specifically, the cumulative per cent excess risk per 13°F increase in Tmax was 2.4% (95% CI 1.74, 3.0) for children 0–4 years, 0.8% (95% CI 0.8, 1.6) for children 5–12 years and 1.4% (95% CI 0.6, 2.3) for children 13–18 years. Tmax conferred excess risks of ED visits on lag days 0 to 2 for all‐age groups and on lag day 3 for children aged 0–4 years.
Table S3 shows the cumulative excess risk in ED visits in association with Tmax, stratified by sex, race/ethnicity and specific diagnostic categories. We found that the risk of ED visits was elevated for both sexes, with a greater risk for girls than for boys; the risk of ED visits was elevated for non‐Hispanic White, Hispanic and non‐Hispanic Other subgroups and was nonsignificant for non‐Hispanic Black; and the risk of ED visits was elevated for heat‐specific, general symptoms and injury diagnostic codes, but decreased for digestive, viral and ear, and respiratory illness.
3.2. Hospitalisations
In our main hospitalisation models with Tmax parameterised as a piecewise linear term above the threshold of 85°F (Table 3), we observed an elevated risk of hospitalisations in association with higher Tmax only on lag day 0 for children of all ages. Specifically, a 13°F (IQR) increase in same‐day Tmax above 85°F was associated with 1.2% (95% CI 0.1, 2.4) higher odds of hospitalisation. Tmax was not associated with hospitalisations on subsequent lag days.
TABLE 3.
Per cent excess risk and 95% confidence intervals for hospitalisations per 13°F increase in daily maximum temperature over 85°F over lags 0–5 days for children aged 0–18 years living in New York City, 2005–2011, overall and by age groups
| Lag day | Overall (0–18 years) | Age 0–4 years | Age 5–12 years | Age 13–18 years |
|---|---|---|---|---|
| Lag0 | 1.24 (0.05, 2.44) | 1.40 (−0.42, 3.26) | −0.81 (−3.22, 1.66) | 2.45 (0.41, 4.53) |
| Lag1 | 0.82 (−0.02, 1.67) | 0.72 (−0.57, 2.02) | −0.69 (−2.41, 1.05) | 1.98 (0.54, 3.44) |
| Lag2 | 0.40 (−0.19, 1.00) | 0.04 (−0.87, 0.96) | −0.57 (−1.79, 0.66) | 1.51 (0.49, 2.54) |
| Lag3 | −0.01 (−0.60, 0.58) | −0.63 (−1.54, 0.28) | −0.45 (−1.67, 0.78) | 1.05 (0.03, 2.07) |
| Lag4 | −0.43 (−1.26, 0.41) | −1.30 (−2.56, −0.02) | −0.33 (−2.05, 1.41) | 0.58 (−0.83, 2.02) |
| Lag5 | −0.84 (−2.00, 0.34) | −1.96 (−3.73, −0.17) | −0.21 (−2.63, 2.26) | 0.12 (−1.87, 2.15) |
| Cumulative | 1.17 (−2.14, 4.60) | −1.76 (−6.68, 3.41) | −3.04 (−9.53, 3.92) | 7.91 (1.99, 14.18) |
All models adjusted for relative humidity using a natural spline with 3 degrees of freedom.
When stratified by age group, Tmax conferred excess risks for hospitalisations in adolescents aged 13–18 years only, on lag days 0 through 3, with the highest excess risk observed on lag day 0 (2.5%, 95% CI 0.4, 4.5). Tmax above 85°F was not associated with elevated risks of hospitalisations in children 0–4 or 5–12 years. When stratified by sex, race/ethnicity and specific diagnostic categories, we did not observe increased risks for hospitalisation for any of these subgroups (Table S3).
3.3. Sensitivity analysis
To test the sensitivity of our results to the choice of temperature metrics, we reran the main analyses using heat index (Table S1) and minimum temperature (Table S2). Results were similar to our main findings except that heat index was not associated with hospitalisation on lag day 0 for children of all ages and that minimum temperature was associated with a decreased cumulative risk for ED visits for children of all ages and ages 5–12 and 13–18, with an elevated risk for ED visits observed only on lags 0–1, as compared to lags 0–3 for Tmax, for children of all ages.
4. COMMENT
4.1. Principal findings
In New York City, we observed greater risks of ED visits and inpatient hospitalisations associated with high daily maximum temperatures during warm seasons between 2005 and 2011 among children from 0 to 18 years. For ED visits, young children aged 0–4 years were the most susceptible to the adverse effects of high temperatures, but children and adolescents aged 5–12 years and 13–18 years were also sensitive to heat effects. For hospitalisations, only adolescents aged 13–18 years showed increased heat‐related risks. These findings contribute to our understanding of the differential effects of heat on children by age group, highlighting young children, as well as older children and adolescents, as subpopulations sensitive to the adverse health impacts of climate change, but in potentially different ways reflective of different social protections and risk behaviours. Our findings could have important clinical counselling implications for adolescents involved in warm‐season sports and outdoor work or other activities.
4.2. Strengths of the study
This study has several strengths, including our examination of heat susceptibility across age groups, the use of a large administrative data set capturing citywide ED visits and hospitalisations, and a case‐crossover study design that inherently adjust for all time‐invariant confounders. The findings underscore the importance of focussing on children and adolescents in targeting heat illness prevention and emergency response activities, especially as high temperatures become more frequent and intense. Although the effect sizes of ambient temperatures are very small, a small increase in the risk of morbidity among children is of serious public health concern. Our findings carry important clinical and anticipatory guidance implications around heat exposure to a wide range of care providers who participate in the care of children, including primary care and emergency service. For example, paediatric healthcare professionals have an important role in anticipatory guidance around heat‐health risk and teaching about appropriate hydration and exposure guidelines. In addition, public health planning and design strategies should target resources to provide safe, thermally comfortable, accessible and age‐appropriate spaces (eg schoolyards, urban parks, playgrounds, sports fields) to reduce the heat impact of extreme heat on children. 33 School physical education programmes and sports teams should monitor youth participating in outdoor sports to ensure proper sport clothing, adequate hydration and sufficient rest and recovery time between repeats of high‐intensity physical activities in the heat. 34
4.3. Limitations of the data
First, while heat can exacerbate a wide range of medical conditions, 1 with cross‐sectional data, we cannot rule out the possibility that children and their families have a greater proclivity to seek care for discretionary problems when the temperature is high. Future research may focus on heat‐related conditions and investigate mechanisms by which high temperatures affect heat‐related vulnerability among children and adolescents and whether the risks differ across age groups. Second, we did not examine effect modification by individual characteristics such as family socioeconomic conditions, insurance status, disease severity, medication use, healthcare needs, neighbourhood social and built environments, and housing features. In particular, children from socioeconomically disadvantaged families and deprived neighbourhoods may be more likely to live in physical and social conditions vulnerable to heat impacts (eg due to a lack of air conditioning, non‐nutritious diet, and inadequate sanitation systems that increase dehydration). Further research exploring socioeconomic variations of heat susceptibility would help identify subgroups of children who are most adversely affected by heat and inform effective, targeted interventions. Third, due to data limitation, we did not explore spatial variations in heat exposure in the analyses despite potential differential heat exposures due to micro‐urban heat islands within the city. Previous studies have found substantial spatial variations in temperature within NYC, with hotter temperatures found in low‐income, high‐poverty neighbourhoods. 35 , 36 Further studies are needed to leverage more spatially resolved exposures and geocoded data on neighbourhood socioeconomic and environmental conditions to explore spatial heterogeneity in temperature impacts and examine heat‐related health disparities. Further, these findings may not be generalisable to rural areas. While the urban heat island effect can increase risk in cities, populations in rural areas may also have heat‐health risks, 37 which warrants more work to understand burden on rural paediatric populations. Fourth, the data set did not permit us to distinguish primary and recurrent visits. However, to inform how repeated visits may influence the interpretability of our results, we have previously examined the number of repeated addresses in the data set and found that less than 5% are repeated. 38 Fifth, we had access to the SPARCS data for 2005–2011 for the main project, although data for more recent years are available. It is possible that the risk associations seen during this earlier time period differ from present, and while no long‐term trend studies exist for paediatric morbidity and heat, we know from long‐term trend studies of heat and mortality that over the last decade the risk association has not significantly changed—likely due to relatively stable air conditioning access over recent years. 39
4.4. Interpretation
Consistent with our team's prior findings, we found an association between daily maximum temperature and ED visits among children aged 0–4 years on lag days 0–3. 13 We extended our prior work by showing increased heat risks for ED visits among older children and adolescents as well, although with smaller effect sizes. Our findings are consistent with our current understanding of the physiologic age‐related susceptibility. 15 , 40 , 41 Younger children have a greater body surface‐to‐volume ratio which increases dermal fluid loss risk during hot days and exercise, while their ability to regulate core body temperature and self‐care (hydration and proper clothing) is still immature compared to older children, adolescents and adults. 5 We also observed decreased risk of ED visits on lag days 4 and 5, which may point to potential offsetting effects where increased ED visits on the first three days following a hot day would be partially offset by a reduction in ED visits on a later day. However, the absolute magnitude of the lower risk seen on lag days 4 and 5 was smaller than the absolute magnitudes of the elevated risk on the first three days suggesting a net, cumulative increased risk from heat.
Although we found an increased risk of hospitalisations associated with a higher same‐day daily maximum temperature over 85°F among children overall, when stratified by age groups, it was only significant among adolescents 13–18 years, not among children 0–4 or 5–12 years. Our findings add to the scarce literature that focusses on associations between heat and morbidity among adolescents. 15 This finding suggests potentially different mechanisms of how heat is associated with health risks for young children compared to adolescents manifesting subsequently in different healthcare utilisation patterns. Adolescents may have increased exposure to outdoor temperatures because they spend more time playing outdoors and in transit on public transportation in NYC than younger children, increasing their vulnerability to high temperatures. 15 Adolescent athletes in particular may face greater health risks when practicing or competing in heat, as long periods of recurring high‐intensity activity patterns can exacerbate thermal and cardiovascular strain, leading to heat illness. 34 , 42
The lag structure of temperature effects on ED visits and hospitalisations found in this study is consistent with prior studies that reported relatively acute lag effects of heat among children. 26 In this study, the effects of high temperature peaked on the same day, and lasted for three days for ED visits, and were only significant on the same day for hospitalisations. While ED cases are generally considered to be less severe and more acute than hospitalisation, 26 our data show that ED visits are sensitive to the impact of high temperatures with associations that endure over multiple days. We also show that high temperatures confer elevated risks for ED visits, but not hospitalisations, for specific sex, racial/ethnic and diagnostic subgroups, suggesting that evaluating ED visits could provide valuable information on subpopulations most vulnerable to heat and potentially also mechanism. Some prior studies suggest that heat waves or temperatures exceeding a certain heat threshold increase the risk of morbidity. 43 In this study, we observed a linear effect of maximum temperature on the risk of ED visits, and a threshold of 85°F (29.4℃) for the heat effect on hospitalisations, suggesting that not only just extreme heat, but warm temperatures more generally, could confer health risks for children.
4.5. Conclusions
In conclusion, this study expands our understanding of heat‐health risks to children and the heterogeneity across age groups. While all‐age children have increased risk of ED visits, adolescents are at increased risk of severe health consequences relative to younger children which warrants tailored risk messaging by providers to their patients and caregivers.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
Supporting information
Supporting information
ACKNOWLEDGEMENT
Research reported in this publication was supported by the National Institute of Environmental Health Sciences (R01ES030717). The funder/sponsor did not participate in the work.
Niu L, Herrera MT, Girma B, et al. High ambient temperature and child emergency and hospital visits in New York City. Paediatr Perinat Epidemiol.2022;36:36–44. 10.1111/ppe.12793
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from New York State (NYS) Statewide Planning and Research Cooperative System (SPARCS). Restrictions apply to the availability of these data, which were used under license for this study. Data are available from https://www.health.ny.gov/statistics/sparcs/ with the permission of NYS SPARCS.
REFERENCES
- 1. Hajat S, Kosatky T. Heat‐related mortality: a review and exploration of heterogeneity. J Epidemiol Commun Health. 2010;64(9):753‐760. [DOI] [PubMed] [Google Scholar]
- 2. Sheffield PE, Landrigan PJ. Global climate change and children's health: threats and strategies for prevention. Environ Health Perspect. 2011;119(3):291‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ahdoot S, Pacheco SE. Global climate change and children’s health. Pediatrics. 2015;136(5):e1468. [DOI] [PubMed] [Google Scholar]
- 4. Kim JJ. Ambient air pollution: health hazards to children. Pediatrics. 2004;114(6):1699‐1707. [DOI] [PubMed] [Google Scholar]
- 5. Smith CJ. Pediatric thermoregulation: considerations in the face of global climate change. Nutrients. 2019;11(9):2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li T, Horton RM, Kinney P. Future projections of seasonal patterns in temperature‐related deaths for Manhattan. Nat Clim Chang. 2013;3:717‐721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meehl GA, Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science. 2004;305(5686):994‐997. [DOI] [PubMed] [Google Scholar]
- 8. Grotjahn R, Huynh J. Contiguous US summer maximum temperature and heat stress trends in CRU and NOAA Climate Division data plus comparisons to reanalyses. Sci Rep. 2018;8(1):1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shea KM. Global climate change and children's health. Pediatrics. 2007;120(5):e1359‐e1367. [DOI] [PubMed] [Google Scholar]
- 10. Watts N, Adger WN, Agnolucci P, et al. Health and climate change: policy responses to protect public health. The Lancet. 2015;386(10006):1861‐1914. [DOI] [PubMed] [Google Scholar]
- 11. United Nations . World urbanization prospects: the 2018 revision. United Nations Publications; 2019. [Google Scholar]
- 12. Heaviside C, Macintyre H, Vardoulakis S. The Urban Heat Island: implications for health in a changing environment. Curr Environ Health Rep. 2017;4(3):296‐305. [DOI] [PubMed] [Google Scholar]
- 13. Sheffield PE, Herrera MT, Kinnee EJ, Clougherty JE. Not so little differences: variation in hot weather risk to young children in New York City. Public Health. 2018;161:119‐126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schinasi LH, Bloch JR, Melly S, Zhao Y, Moore K, De Roos AJ. High ambient temperature and infant mortality in Philadelphia, Pennsylvania: A case‐crossover study. Am J Public Health. 2020;110(2):189‐195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xu Z, Hu W, Su H, et al. Extreme temperatures and paediatric emergency department admissions. J Epidemiol Community Health. 2014;68(4):304‐311. [DOI] [PubMed] [Google Scholar]
- 16. Iñiguez C, Schifano P, Asta F, Michelozzi P, Vicedo‐Cabrera A, Ballester F. Temperature in summer and children's hospitalizations in two Mediterranean cities. Environ Res. 2016;150:236‐244. [DOI] [PubMed] [Google Scholar]
- 17. Statewide Planning and Research Cooperation System (SPARCS) . New York State Department of Health website. https://www.health.ny.gov/statistics/sparcs/. Published 2015. Accessed May 17, 2020.
- 18. NOAA National Centers for Environmental Information . Climate data online. https://www.ncdc.noaa.gov/cdo‐web/. Published 2020. Accessed May 16, 2020, 2020.
- 19. Metzger KB, Ito K, Matte TD. Summer heat and mortality in New York City: how hot is too hot? Environ Health Perspect. 2010;118(1):80‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barnett AG, Tong S, Clements AC. What measure of temperature is the best predictor of mortality? Environ Res. 2010;110(6):604‐611. [DOI] [PubMed] [Google Scholar]
- 21. Winquist A, Grundstein A, Chang HH, Hess J, Sarnat SE. Warm season temperatures and emergency department visits in Atlanta, Georgia. Environ Res. 2016;147:314‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Anderson GB, Bell ML, Peng RD. Methods to calculate the heat index as an exposure metric in environmental health research. Environ Health Perspect. 2013;121(10):1111‐1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Maclure M. The case‐crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133(2):144‐153. [DOI] [PubMed] [Google Scholar]
- 24. Janes H, Sheppard L, Lumley T. Case‐crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology. 2005;16(6):717‐726. [DOI] [PubMed] [Google Scholar]
- 25. Buteau S, Goldberg MS, Burnett RT, et al. Associations between ambient air pollution and daily mortality in a cohort of congestive heart failure: Case‐crossover and nested case‐control analyses using a distributed lag nonlinear model. Environ Int. 2018;113:313‐324. [DOI] [PubMed] [Google Scholar]
- 26. Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120(1):19‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gasparrini A, Armstrong B, Kenward MG. Distributed lag non‐linear models. Stat Med. 2010;29(21):2224‐2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gao J, Sun Y, Lu Y, Li L. Impact of ambient humidity on child health: a systematic review. PLoS One. 2014;9(12):e112508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gasparrini A. Distributed lag linear and non‐linear models in R: the package dlnm. J Stat Software. 2011;43(8):1. [PMC free article] [PubMed] [Google Scholar]
- 30. Kouis P, Kakkoura M, Ziogas K, Paschalidou AΚ, Papatheodorou SI. The effect of ambient air temperature on cardiovascular and respiratory mortality in Thessaloniki, Greece. Sci Total Environ. 2019;647:1351‐1358. [DOI] [PubMed] [Google Scholar]
- 31. Baccini M, Kosatsky T, Biggeri A. Impact of summer heat on urban population mortality in Europe during the 1990s: an evaluation of years of life lost adjusted for harvesting. PLoS One. 2013;8(7):e69638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease: the effects of temperature and humidity. Epidemiology. 2004;15(6):755‐761. [DOI] [PubMed] [Google Scholar]
- 33. Fjørtoft I. Landscape as playscape: The effects of natural environments on children's play and motor development. Children Youth Environ. 2004;14(2):21‐44. [Google Scholar]
- 34. Falk B, Dotan R. Temperature regulation and elite young athletes. Med Sport Sci. 2011;56:126‐149. [DOI] [PubMed] [Google Scholar]
- 35. Huang G, Zhou W, Cadenasso ML. Is everyone hot in the city? Spatial pattern of land surface temperatures, land cover and neighborhood socioeconomic characteristics in Baltimore, MD. J Environ Manage. 2011;92(7):1753‐1759. [DOI] [PubMed] [Google Scholar]
- 36. Hoffman JS, Shandas V, Pendleton N. The effects of historical housing policies on resident exposure to intra‐urban heat: A study of 108 US urban areas. Climate. 2020;8(1):12. [Google Scholar]
- 37. Bernhard MC, Kent ST, Sloan ME, Evans MB, McClure LA, Gohlke JM. Measuring personal heat exposure in an urban and rural environment. Environ Res. 2015;137:410‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sheffield PE, Shmool JLC, Kinnee EJ, Clougherty JE. Violent crime and socioeconomic deprivation in shaping asthma‐related pollution susceptibility: a case‐crossover design. J Epidemiol Community Health. 2019;73(9):846‐853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Petkova EP, Gasparrini A, Kinney PL. Heat and mortality in New York City since the beginning of the 20th century. Epidemiology (Cambridge, Mass). 2014;25(4):554‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nastos PT, Paliatsos AG, Papadopoulos M, Bakoula C, Priftis KN. The effect of weather variability on pediatric asthma admissions in Athens, Greece. J Asthma. 2008;45(1):59‐65. [DOI] [PubMed] [Google Scholar]
- 41. Knowlton K, Rotkin‐Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Persp. 2009;117(1):61‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Committee on Sports Medicine and Fitness . Climatic heat stress and the exercising child and adolescent. Pediatrics. 2000;106(1):158. [PubMed] [Google Scholar]
- 43. Gronlund CJ, Berrocal VJ, White‐Newsome JL, Conlon KC, O’Neill MS. Vulnerability to extreme heat by socio‐demographic characteristics and area green space among the elderly in Michigan, 1990–2007. Environ Res. 2015;136:449‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information
Data Availability Statement
The data that support the findings of this study are available from New York State (NYS) Statewide Planning and Research Cooperative System (SPARCS). Restrictions apply to the availability of these data, which were used under license for this study. Data are available from https://www.health.ny.gov/statistics/sparcs/ with the permission of NYS SPARCS.


