Abstract
Context
Too many people living with chronic kidney disease are opting for and starting on hospital‐based dialysis compared to a home‐based kidney replacement therapy. Dialysis services are becoming financially unsustainable.
Objective
This study aimed to assess the efficacy of coproductive research in chronic kidney disease service improvement to achieve greater sustainability.
Design
A 2‐year coproductive service improvement study was conducted with multiple stakeholders with the specific intention of maximizing engagement with the national health kidney services, patients and public.
Setting and Participants
A national health kidney service (3 health boards, 18 dialysis units), patients and families (n = 50), multidisciplinary teams including doctors, nurses, psychologists, social workers, and so forth (n = 68), kidney charities, independent dialysis service providers and wider social services were part of this study.
Findings
Coproductive research identified underutilized resources (e.g., patients on home dialysis and social services) and their potential, highlighted unmet social care needs for patients and families and informed service redesign. Education packages were reimagined to support the home dialysis agenda including opportunities for wider service input. The impacts of one size fits all approaches to dialysis on specialist workforce skills were made clearer and also professional, patient and public perceptions of key sustainability policies.
Discussion and Conclusions
Patient and key stakeholders mapped out new ways to link services to create more sustainable models of kidney health and social care. Maintaining principles of knowledge coproduction could help achieve financial sustainability and move towards more prudent adult chronic kidney disease services.
Patient or Public Contribution
Involved in developing research questions, study design, management and conduct, interpretation of evidence and dissemination.
Keywords: coproduction, dialysis, family, kidney disease, patient, service improvement study, sustainability
Abbreviations
- WRCN
Welsh Renal Clinical Network
- MDTs
Multi Disciplinary Teams
- UHD
Unit Haemodialysis also referred to as hospital‐based dialysis
- NICE
National Institute for Health and Care Excellence
- PD
Peritoneal Dialysis
- HHD
Home Haemodialysis
- KRT
Kidney Replacement Therapy
- BAME
Black, Asian, Minority, Ethnic
- WKRU
Wales Kidney Research Unit
1. BACKGROUND
At least 10% of the global population is estimated to have chronic kidney disease (CKD). 1 Kidney disease has a major impact on global health both in terms of mortality and disease burden, with these numbers increasing year on year. 2 , 3 , 4 , 5 In 2010, more than 2.6 million people received a kidney replacement treatment (KRT—the collective name for either a transplant or dialysis), and numbers are projected to more than double by 2030, with the biggest increase coming from low‐ and middle‐income countries. 6 People who have developed kidney failure very often have multiple comorbidities, 7 are older, more frail, more deprived 8 , 9 and disease progression is not easily predicted. 10 They can rely on multiple health and social care services for their care and support. 11 While KRTs have been available for decades in high‐income countries, overall, little is known about the optimal way to coordinate, finance and regulate people with CKD from diagnosis, access to KRT and their overall care and support. 12
There are three main options available when a person goes into kidney failure: transplant, dialysis and supportive care without dialysis (sometimes called conservative management). Dialysis can occur in a hospital setting called unit haemodialysis (UHD) undertaken three times a week for 4 hour sessions at a time, or at home. If a person chooses home dialysis, there are generally two types of dialysis (peritoneal dialysis and home haemodialysis) available (depending on clinical suitability), both of which can be administered during the day or overnight depending on people's preferences and outcomes. National Institute for Health and Care Excellence (NICE) guidelines estimate that a minimum of 30% of the current dialysis population in the United Kingdom could be on home dialysis. NICE guidance also acknowledges the substantial impact that the different treatments will have on lifestyle and that people's values and preferences must be taken into account when presenting KRT options to them and their family. 13 Further background to the development of home therapies and global trends is presented in File S1.
1.1. Sustainability and the Welsh National Health Service context
Wales is one of the four devolved nations of the United Kingdom, with a devolved healthcare system and a population of around 3 million. The incidence and prevalence of CKD are higher in Wales than in the rest of the United Kingdom, affecting 6%–8% of the Welsh population (around 200,000 people). 14 More than 3000 people are currently on KRT in Wales, with this number increasing year on year. 15 In 2017, Wales had higher numbers of people start on home therapies and higher numbers of people currently on home therapies compared to the UK average (Box 1). For the first time in 10 years, commissioners of kidney services in Wales (Welsh Renal Clinical Network) were forced to request a net increase in investment from NHS Wales to sustain the dialysis service for increasing numbers of people. This exponential increase is considered unsustainable as money is finite and too many people are unnecessarily opting for more expensive UHD.
BOX 1. Summary percentages of the Welsh population starting and currently on dialysis compared to the UK average 2017 16 .
1.
| Wales | UK | |
| Percentage of people to start on home therapies | 23% | 21.6% |
| Percentage of prevalent dialysis patients on home dialysis | 20.3% | 16.8% |
The National Health Service (NHS) adopts the well‐established ‘Three Pillars of Sustainability: Social, Economic and Environmental’ model across all its health service improvement strategies and agendas for change. 17 In Wales, the Wellbeing of Future Generations (Wales) Act 2015 18 and the Social Services and Wellbeing (Wales) Act 2014 19 provide the key policy contexts for all health and social care including three pillar plans for more sustainable services. The underpinning healthcare policy in Wales is Prudent Healthcare, 20 which specifically recognizes the interdependence of specific challenges in creating more sustainable health and social care services. Examples of prudent healthcare plans include ‘A Healthier Wales’ 21 which puts care and support at home at the heart of service improvement developments, 22 long‐term ambitions for health and social care systems to work together and, where possible, to shift services out of hospitals into the communities. 23
A key principle of prudent healthcare is coproduction, defined as ‘a way of working whereby citizens and decision makers, or people who use services, family, carers and service providers work together to create a decision or service which works for them all’. 24 Since the implementation of prudent healthcare in 2014, Welsh policy makers encourage coproduction as the default way of working and are increasingly asking that the evidence which informs decision making is coproduced. 19 , 25 , 26 Increasing the number of people on home dialysis in Wales is a prudent healthcare policy. 20
1.2. Coproduction in sustainable health services contexts
In a research context, coproduction is broadly defined as ‘an approach in which researchers, practitioners and the public work together, sharing power and responsibility from the start to the end of the project, including the generation of knowledge’. 27 Coproduction is becoming more common, and new models of coproduction and methods of assessment are constantly being developed. 28 , 29 , 30 Recent coproductive health research reports on the capacity of coproduction to increase impact, facilitate knowledge translation, identify underused or unrecognized resources (people, services, networks), improve information and education processes by tailoring to individual need and support overall health improvement initiatives. 31 , 32 , 33 , 34 Increases in the breadth of examples of coproductive health services research have also highlighted challenges to coproduction. These include costs, resources, training, time, cultural differences and misunderstandings of what is (and is not) coproductive research. 35 , 36 , 37 , 38 , 39 , 40 , 41 Increasingly, however, health research is turning to the global contexts of coproduction, recognizing the potential value (in health service and policy contexts) while at the same time addressing known barriers and new challenges. 33 , 34 , 36 , 42 , 43 , 44
Previous attempts to address low uptake of home dialysis have centred around shared decision making (SDM), specifically, the Making Good Decisions In Collaboration (MAGIC) model developed for the UK NHS. 45 MAGIC provides a template based on ‘choice, option, decision talk’ to help professionals implement SDM in clinical settings and explains the patient's experience as a journey from uninformed to informed through building rapport, mutual respect and active listening. SDM is widely recognized as best practice, and yet has been shown to be problematic to implement across the relevant healthcare settings as the necessary systems, infrastructures and wider support networks (e.g., well designed and validated decision support aids, patient empowerment, clinician training, culture shifts and system bureaucracies) are either not available or not working in ways that promote SDM models of care. SDM is also a key principle of prudent healthcare that has been implemented across international health contexts and policies, for example, the ‘1000 Lives Improvement’ programme, 47 and changing the law in consent for organ donation. 48
2. METHODS
2.1. Study context
We conducted a study with two elements—a health service improvement element and an empirical element that included an analysis of epidemiological big data, costs of dialysis modalities and a qualitative study of patient and carer perspectives. In this paper, we specifically focus on the health service improvement element and the coproductive methods and outcomes, which were deployed to help answer a specific coproductive research question: Can coproduction lead to more sustainable adult CKD services in Wales? This question was predefined by the funder as part of a themed national health and social care funding call under the umbrella of research for the patient and public benefit scheme. The question was interpreted for this study as ‘assessing the efficacy of coproduction to better understand the barriers to home dialysis and map alternate pathways’. Full details of the overall study are available in the published protocol. 49 We summarize the overall study in Figure 1 and at the same time highlight the specific health service improvement and coproduction elements that this paper focusses on. The objective of this study was to ‘assess the efficacy of co‐productive research in chronic kidney disease service improvement to achieve greater sustainability’. The core research team were multidisciplinary and included academics from health services and systems research, health economists, the lead kidney nurse for Wales, kidney service commissioners, nephrologists and people living with kidney disease.
Figure 1.
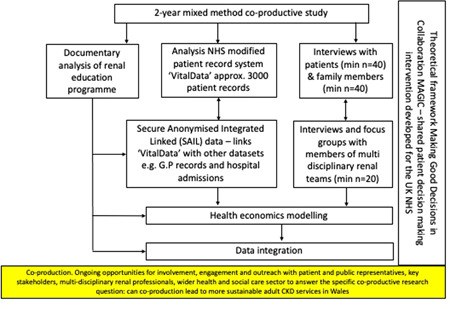
Overall study diagram, highlighting the coproductive elements and the focus of this paper
2.2. Settings and participants
This was a 2‐year coproductive study (October 18–20). The following were either key partners or settings in the study: kidney services covering all kidney healthcare in Wales (Figure 2), commissioners of welsh kidney services—Welsh Renal Clinical Network (WRCN), kidney third sector services (Paul Popham Fund, Kidney Care UK, Kidney Wales), wider third sector services (e.g., Carers Wales, Citizens Advice, Care and Repair Cymru, Action for Elders), local councils and local authorities in Wales, industry (independent dialysis service providers Baxter, B. Braun, Fresenius), social service commissioners in Wales, people living with kidney disease, their family members and close friends. Overall numbers of participants from the all‐Wales NHS kidney team workforce are summarized in Box 2. As a coproductive study, all people living with kidney disease in Wales and their families were eligible for inclusion in the study. We used a purposive sampling frame to achieve a maximum‐variation sample. People were invited by healthcare professionals and kidney charities to participate in the various coproductive elements of the study. Healthcare professionals included those most directly involved in dialysis decision making and care (e.g., specialist nurses and nephrologists) and included the wider multidisciplinary team to ensure that the whole kidney service was represented.
Figure 2.

Map of kidney services across Wales
BOX 2. Overall numbers of NHS kidney multidisciplinary teams, patients and family members who contributed to the coproduction.
1.
| Clinical consultants | n = 12 |
| Nurses and nurse managers, including predialysis education specialists, home therapies specialists and transplant specialists | n = 30 |
| Allied health professionals, including psychologists, dieticians, occupational therapists, physiotherapists, pharmacists | n = 20 |
| Specialist renal social workers, counsellors and additional specialist services, for example, youth workers | n = 6 |
| People living with kidney disease including family members from across Wales on various kidney replacement therapies and people who had yet to start dialysis | n = 50 |
2.3. Coproduction
Specific coproduction principles that focussed on sustainability were adapted from Norstrom et al., 50 who produced a set of four general principles to underpin high‐quality knowledge coproduction for sustainability research. These principles were then used to map the coproduction processes throughout the study and acted as the theoretical framework (Box 3). The broad aim was to assess the efficacy of coproductive research in a health service improvement study. In this context, that translated to better understanding of the barriers to home dialysis and mapping of alternate pathways. The goal was to cocreate a new vision for home dialysis services and achieve greater sustainability.
BOX 3. Principles for knowledge coproduction in sustainability research 50 .
1.
Context‐based: The process should be grounded in an understanding of how a challenge emerged, how it is affected by its particular social, economic, political and ecological contexts and the different beliefs and needs of those affected by it.
Pluralistic: The process should explicitly recognize a range of perspectives, knowledge and expertise and consider gender, ethnicity and age in development.
Goal‐oriented: The process should articulate clearly defined, shared and meaningful goals that are related to the challenge at hand.
Interactive: The process should allow for ongoing learning among actors, active engagement and frequent interactions.
We also embedded the six UK standards for public involvement into the study (inclusive opportunities, working together, support and learning, governance, communications and impact) to ensure that coproduction was at the centre of all research activities and processes throughout. The UK standards are mapped against the full range of coproductive activities in this study with examples in File S2. All of the coproductive patient and public involvement was conceptualized as a partnership. Coproductive partners were coproducing and interpreting the research together and as such were fully informed of their roles and expectations in invitations. No formal consent procedures were required as they were not research participants.
We present the purpose of coproduction mapped onto the principles of knowledge coproduction in sustainability research in Table 1. Table 1 also includes an ‘interactive co‐production activity log’ with details of the meetings, events and engagements including numbers who attended with a breakdown of kidney professionals, the public and people living with kidney disease over the 2‐year timeframe of the study. We offered travel and any out‐of‐pocket expenses for people with kidney disease and the public to attend any coproductive events or meetings organized by the research team. Coapplicants who were people with kidney disease were paid a rate in line with the national standards for PPI throughout the study. 51
Table 1.
Principles of knowledge coproduction mapped against coproductive elements and clarifying their purpose
| Principles of knowledge coproduction mapped against key components of the study, of which coproduction was essential | ||||||
|---|---|---|---|---|---|---|
| Purpose | Context‐based methods | Pluralistic methods | Goal‐orientated methods | Interactivea (see coproduction interaction log below for further details) | ||
| 1 | Creating a vision of a more sustainable adult kidney service in Wales | There were two main purposes to this activity: (1) To unpick the key elements of the current renal service that were unsustainable from the perspective of coproductive partners and (2) highlight some of the ways in which existing services and resources could be reconfigured or redesigned to support a future sustainable renal service | Academic members of the research team with PPI input produced a framework with the headings; ‘what is currently unsustainable in adult kidney services’, ‘what does good look like’, ‘how can coproduction help’ and ‘what is difficult to achieve through co‐production’. The headings were then linked to the various perspectives: people living with kidney disease; family members; multi‐disciplinary health and social care professionals; NHS; industry; government; third sector; and wider social contexts (Table 2) | The table was then shared with all the multiple key stakeholders for their input. This included NHS specialist; nephrologists, transplant physicians, social workers, physiotherapists, dieticians, clinical psychologists, counsellors, youth workers and specialist nurses; commissioners; Industry and independent service providers; renal third sector service providers; wider third sector services; social service commissioners; people living with kidney disease; family members and close friends; and the public | The table presented current challenges and potential consequences in tandem with the vision for what good looks like; this included immediate challenges to the Welsh renal service such as overspending, as well as wider challenges outside of NHS secondary renal care, such as overall population health and deprivation. The template presented problems alongside their ‘ideal’ solution and how the multiple audiences could help achieve the solution, in particular, how people living with kidney disease could influence change. As the table grew, we extracted elements that were more relevant to specific groups (e.g., social services) and presented specific problems, ideal solutions and novel ideas for coproduction back to the stakeholders who would be most affected by any changes | We shared the list at specifically curated coproductive meetings with the multidisciplinary teams in North and South Wales, which included patients and family members; operational engagements led by the NHS such as quarterly all Wales Specialist Nurse meetings; and Renal third sector partner events such as transplant cafes. We also shared via small group face‐to‐face meetings with specific members of the MDTs, visits to dialysis units and centres, non‐kidney‐related events (e.g., the festival of social sciences in North Wales and research festivals in Wales National Museum). We shared via email, telephone and face‐to‐face correspondence with patients and later over zoom meetings and curated webinars following the COVID‐19 outbreak. People inputted directly into the table by writing into it, group and individual face‐to‐face feedback, emails and by reviewing the materials directly with academic members of the research team. People often fed back informally following presentations and events throughout the study. We used post it notes, traffic light systems (green = good, amber = don't know/irrelevant, red = bad) and paper cut outs to facilitate the mappings |
| 2 | Coproductive redesigning of service pathways in adult chronic kidney disease | The purpose of this coproductive activity was to gain an understanding of the current renal service pathways, how they connect and interact and to design new pathways that could potentially address the sustainability issues as seen from the multiple perspectives. This particular component was deemed essential by key stakeholders (especially commissioners) to address the overall research question, set by a research funding scheme designed to focus on health service improvement and demonstrate impact in the short to medium term | The original draft of the service improvement pathway/‘pathways to home’ were designed by the lead renal nurse for Wales, also a study coapplicant who had extensive knowledge of the current state of Welsh renal services and were very knowledgeable about wider UK and global contexts and service improvement initiatives. The initial drafting also had patient input (Figure 3) | The pathways were shared with the NHS multidisciplinary teams, in particular, the specialist renal nurses in predialysis and home therapies; professionals allied to medicine including physiotherapists, dieticians and clinical psychologists; renal social workers and youth workers; and people living with kidney disease, family members, renal third sector CEOs and staff working for renal charities and volunteer peer‐to‐peer support workers—many of whom were either living with kidney disease or a family member of someone with kidney disease | Sharing included a preamble, with the current service pathway as a backdrop. This helped to highlight gaps in terms of what the service did not currently have, and then move onto potentials for improvement across the multiple service pathways. The before and after snap shots helped set out the vision for what renal services could look like at a fairly high level across Wales and to more easily present this in relevant ways to the multiple stakeholders for their input | Academic members of the research team attended quarterly NHS specialist nurse meetings, quarterly professionals allied to medicine meetings (which were also attended by patients and renal third sector partners) and worked with renal charity partners to set up specially coordinated zoom meetings to present to people living with kidney disease, family members and charity provider executives. Webinars were produced and made available online and promoted on social media for people to refer and feedback into via comments, telephone, zoom and face‐to‐face meetings |
| 3 | Coproductive Review of education materials and processes | The purpose was to gain a better understanding of the predialysis education programme across Wales, how it was delivered, by whom and to better understand any variations in practice and uptake of home dialysis | Specialist predialysis nurses are primarily responsible for explaining the available treatment options (using various education materials) to people who will need a renal replacement therapy and their family. They also support people while transitioning to starting dialysis or moving to a different treatment and managing symptoms with conservative care and liaise with the multidisciplinary teams (including consultants) about patient care. There are around 15 working across five renal centres in Wales. Despite education processes looking broadly similar across centres on paper, reviews of the number of people on home dialysis varied significantly: only one centre was achieving the national guidelines of 30% on home dialysis | The research team invited the lead nurse to come and present at a specially coordinated coproductive multidisciplinary meeting (with patients and family members in their service also attending) and explain how their service worked and what they felt they were doing differently to everybody else. Academic members of the research team were also invited (following a study update at an NHS quarterly meeting) to attend a house visit with a specialist nurse (from a different centre) to observe their initial conversations with a person needing RRT and their family members | Early on, we explained the aims of the study and highlighted the crucial role that the predialysis specialist nurses played in the research and their role in supporting patients. In this instance, the research team were especially keen to find out more about the potential impacts that the different service configurations had on the uptake of home dialysis, as well as how nurses were delivering education in terms of their priorities and practices | The lead nurse presentation was followed by a question and answer session to an MDT room of practitioners from different services, patients and family members. Having patients and family members attend who were under that particular service care also enabled them to talk about their recent experiences and views on the barriers to home therapies from their perspectives. The field visit to the predialysis persons' home with their family was in itself highly interactive—academic members of the research team and the predialysis nurse were able to converse in detail informally about their education processes and practices as a whole and with that particular family following the consultation |
| 5 | Coproductive review of patient and public attitudes to costs | The purpose was to learn more about public attitudes to the costs of renal healthcare and services to better understand if and how costs are considered in patient and clinical decision making and how the conceptualization of costs could be framed and apportioned to health and social services in a sustainability context looking forward | Nobody knew the actual costs of RRTs in Wales. Previous estimates were outdated and likely to be inaccurate. Wider literature provided little up‐to‐date insights in terms of NHS spend, especially in home haemodialysis. Hidden costs for example job loss, part‐time working, childcare, housing modifications and family impacts such as switching to full‐time carers were scarcely reported. There were various perspectives on costs; however, it was widely assumed within the NHS that hospital or unit dialysis was the most expensive but we knew little about public understandings, attitudes and perceptions of costs of dialysis | Academic members of the research team approached patients and the public to ask about their views on dialysis costs, potential savings and perceptions of shifting services between health and social care. We also approached social services commissioners in Wales to learn from their perspectives | The costs of dialysis services are increasing globally. The coproduction aimed to learn about views and perceptions of the costs of different RRTs in Wales, and specifically how people felt about suggested models for cost savings from the multiple stakeholder perspectives | Academic members of the research team attended several nonkidney disease‐related public events such as hosting a market stall at St. David's Day parade, presenting at All Wales involving people festival and attending local community group meetings with BAME individuals and groups to enhance opportunities for learning and interactive feedback with the public in Wales. We also attended the National Transplant games in Newport and the Welsh Renal Clinical Networks Renal Roadshow with a banner and preamble of the most recent evidence of costs of dialysis. We delivered presentations at kidney patient‐led conferences and meetings to discuss costs and gather perspectives, with larger and smaller groups of kidney patients over 18 months |
| Coproduction log | |||||||
|---|---|---|---|---|---|---|---|
| PPI and professional outreach and engagement dialysis options and choices | |||||||
| Event | Type of activity | Type of PPI | Date | Total number of attendees | Total number of renal profs | Number of public members | Number of patients |
| Give the name of the event, in brief | Please specify the main type of activity | Please specify if: involvement, engagement outreach | Please select from the dropdown menu | Give the total number of attendees | Give the total number of attendees | Give the number of lay/public members attending event | Give the number of patients attending the event |
| Presentation to CNS nurses CKD meeting, llandrinod wells, 26.11.18 | Presentation | Involvement | 26.11.18 | 15 | 14 | 1 | 1 |
| Presentation to home therapies nurses, llandrinod, 07.12.18 | Presentation | Involvement | 07.12.18 | 12 | 11 | 3 | 3 |
| Presentation to BAME group Wyndam Day Centre Riverside, 30.11.18 | Presentation | Engagement | 30.11.18 | 12 | 0 | 12 | 12 |
| Presentation to patient focus group, Cardiff WKRU 06.11.18 | Presentation | Involvement | 06.11.18 | 7 | 3 | 1 | 3 |
| Stand HCRW AGM all | Stand | Outreach | 25.10.18 | 100 | 8 | 10 | 2 |
| Presentation at WKRU AGM Swansea 28.11.18 | Presentation | Engagement | 28.11.18 | 50 | 38 | 12 | 10 |
| Attendance. Community‐powered health supporting better outcomes for all ages | Attendance | Engagement | 23.10.18 | 25 | 2 | 15 | 5 |
| Attendance Castle Bingo Newport Rd | Attendance | Engagement | 06.11.18 | 5 | 0 | 5 | 5 |
| Presentation National Home Therapies Group | Presentation | Involvement | 07.12.18 | 20 | 17 | 2 | 2 |
| Presentation kidney clinical community England | Presentation | Engagement | 10.12.18 | 12 | 10 | 2 | 1 |
| Presentation Clinicians Morriston internal meeting group | Presentation | Engagement | 20.12.18 | 7 | 7 | 0 | 0 |
| Presentation ABMU CNSs Morriston | Presentation | Engagement | 08.01.19 | 4 | 4 | 0 | 0 |
| Presentation C&V CNSs C&V | Presentation | Involvement | 16.01.19 | 5 | 5 | ||
| Presentation Renal Business meeting Morristion | Presentation | Engagement | 22.01.19 | 19 | 19 | ||
| Update Presentation National Home Therapies Road show | Talk | Engagement | 25.01.19 | 12 | 12 | ||
| Meeting Race Council Cymru | Meeting | Outreach | 29.01.19 | 1 | 1 | ||
| Presentation to CNS nurses North Wales | Presentation | Engagement | 05.02.19 | 6 | 6 | ||
| Catch up C&V CNSs Nurses | Meeting | Involvement | 14.01.19 | 5 | 5 | ||
| Glan Clwyd Renal Patient Support Group | Presentation | Engagement | ######### | 8 | 1 | 7 | 7 |
| Meeting Swansea CNSs/shared care nurses | Meeting | Involvement | 19.02.19 | 3 | 3 | ||
| Meeting lead Renal Nurse | Meeting | Involvement | 22.02.19 | 1 | 1 | ||
| Reference Group meeting | Meeting | Involvement | ######### | 14 | 5 | 1 | 1 |
| Glan Clwyd Renal Unit | Meeting | Coproduction | ######### | 4 | 0 | 4 | |
| St David's Day Parade, St Davids Pembrokeshire | Stand | Involvement/outreach | 3.0319 | 40 | 0 | 40 | 5 |
| Ysbyty Gwynedd Renal Unit | Meeting | Coproduction | ######### | 3 | 3 | 0 | 0 |
| Attendance 'co‐producing research' how do we share power NIHR | Attendance | Engagement | 12.03.19 | 70 | 0 | 30 | 10 |
| Public Health Wales 2019 conference | Poster Presentation | Engagement | 13.03.19 | 100 | 0 | 20 | 10 |
| National Home Therapies Group | Meeting | Involvement | 29.04.19 | 20 | 18 | 2 | 2 |
| CNO conference presentation | Presentation | Engagement | 08.05.19 | 20 | 2 | 2 | 2 |
| Dialysis Options and Choices Key stakeholder meeting | Meeting | Involvement | 15.05.19 | 20 | 12 | 2 | 6 |
| Paul Popham Conference presentation and stand | Presentation/stand | Involvement/engagement | 17.05.19 | 40 | 20 | 5 | 20 |
| CHEME Bangor University Invited Seminar | Presentation | Engagement | 14.05.19 | 15 | 0 | 15 | 1 |
| Meeting Kidney Research UK | Meeting | Engagement | 26.06.19 | 4 | 0 | 2 | 1 |
| Renal Roadshow Morriston | Stand | Involvement | 04.07.19 | 40 | 20 | 10 | 10 |
| National Home Therapies Meeting | meeting | Involvement | 12.07.19 | 30 | 27 | 2 | 1 |
| HCRW Lets Talk Research Annual Involving People Conference | Presentation | Engagement | 27.07.19 | 50 | 50 | 50 | 2 |
| Transplant Games Newport | Stand | Outreach | 28.07.19 | 100 | 0 | 100 | 50 |
| Meeting with‐ Lead Nurse/Directorate manager | Meeting | Involvement | 12.08.19 | 1 | 1 | ||
| Meeting‐ Kidney Wales patient advocate | Meeting | Involvement | 15.08.19 | 1 | 1 | ||
| Visit Carmarthen Dialysis Unit | Stand | Engagement | 29.08.19 | 7 | 7 | ||
| Visit Llandrindod Dialysis Unit | Stand | Engagement | 30.08.19 | 6 | 6 | ||
| Presentation and meeting with Paul Popham Befrienders | Meeting | Involvement | 12.09.19 | 10 | 2 | 8 | |
| Third wider stakeholder meeting | Meeting | Involvement | 18.09.19 | 30 | 18 | 8 | 4 |
| Presentation National Home Therapies Group | Presentation | Involvement | 20.09.19 | 15 | 12 | 1 | 3 |
| HCRW annual conference—Collaboration and Partnerships | Presentation | Engagement | 03.10.19 | 50+ | 50+ | 1 Kidney patient was a co presenter | |
| National Audit Presentation | 04.10.19 | ||||||
| Cardiff and Vale R&D conference presentation | Presentation | Engagement | 15.10.19 | 40+ | 40+ | ||
| Attendance at National Health and Wellbeing Professionals Group | Meeting | Involvement | 22.10.19 | 10 | 10 | ||
| Presentation at Festival of Social Sciences 'Social Prescribing Network Event, Bangor, Bangor University | Presentation/stand | Involvement | 07.11.19 | 25 | 0 | 23 | 1 |
| Workshop with Paul Popham Befrienders, Swansea | Workshop | Involvement | 12.11.19 | 9 | 0 | 1 | 8 |
| Research findings mapping roadmaps | Meeting/presentation | Involvement | 13.11.19 | 5 | 1 | 4 | |
| National CKD meeting | Meeting/presentation | Involvement | 22.11.19 | 13 | 9 | 2 | 2 |
| Coproduction meeting on home therapies | Meeting/presentation | Involvement | 25.11.19 | 35 | 12 | 10 | 13 |
| Field visit with CKD nurse to home | Field work | Involvement | 27.11.19 | 1 | 1 | ||
| Conservative Management meeting ACP | Meeting | Engagement | 28.11.19 | 8 | 6 | 2 | |
| Transplant café Swansea | Meeting/presentation | Involvement | 13.12.19 | 12 | 4 | 1 | 7 |
| Patient meeting | Meeting | Involvement | 13.01.20 | 2 | 1 | ||
| Transplant café Cardiff | Meeting | Involvement | 15.01.20 | 9 | 3 | 1 | 5 |
| Renal peer review training | Meeting | Involvement | 17.01.20 | 30 | 28 | 2 | |
| Befriender steering committee | Meeting | Involvement | 23.01.20 | 9 | 5 | 3 | 1 |
| Home therapies café | Meeting | Involvement | 07.02.20 | 9 | 6 | 3 | |
| National home therapies group | Meeting | Involvement | 10.02.20 | 15 | 13 | 2 | |
| National CKD meeting | Meeting | Involvement | 21.02.20 | 12 | 10 | 2 | |
| WKRU AGM | Meeting/presentation | Involvement | 27.07.20 | 80 | 60 | 10 | 10 |
| Video of patient presentation shown on YouTube over world kidney day describing his live donor journey | Video | Involvement | 12.03.20 | Over 100 views online | |||
| Types of events (hosted/organized by Infrastructure group) | |||||||
| Seminar | |||||||
| Conference | |||||||
| Workshop | |||||||
| Open‐lab | |||||||
| Open‐office | |||||||
| Presentation | |||||||
Abbreviations: CNS, clinical nurse specialist; MDT, multidisciplinary team; RRT, renal replacement therapy; WKRU, Wales Kidney Research Unit.
We offered travel and any out‐of‐pocket expenses for patients and the public to attend any coproductive events or meetings organized by the research team. Coapplicants who were patients were paid a rate in line with the national standards for PPI throughout the study. 56
There were four specific components of the health improvement study, of which coproduction was fundamental to address:
-
1.
To create a vision of a more sustainable adult kidney service in Wales,
-
2.
To redesign service pathways in adult CKD,
-
3.
To review patient education materials and processes and
-
4.
To better understand patient and public attitudes towards the costs of kidney care and services.
In the following section, we summarize how and what data were collected and analysed for each coproductive element, and how data were used to achieve the intended outcomes.
-
1.
To create a vision of a more sustainable adult kidney service in Wales.
-
Data collection
The multidisciplinary research team, which included people with kidney disease, produced a framework with the headings ‘what is currently unsustainable in adult kidney services’, ‘what does good look like’, ‘how can co‐production help’ and ‘what is difficult to achieve through co‐production’. The headings were then linked to the various perspectives: people living with kidney disease, family members, multidisciplinary health and social care professionals, NHS, independent dialysis service providers, government, third sector and wider social contexts (Table 2).
People with kidney disease worked with the research team to cocreate Table 2. They had input across every perspective by identifying sustainability issues and inputting into potential solutions through coproduction as well as helping produce subheadings to ensure that all elements of the wider services were included. To facilitate this, the research team arranged two specifically curated coproductive meetings with the multidisciplinary teams in North (25 November 2019) and South Wales (15 May 2019). We contacted the predialysis nurse specialists for each team and asked them to send out invites to people living with kidney disease and their families. We prepared a brief poster advertising the meeting and requested that people get in touch either by phone or email to book their places. We also invited nephrologists, predialysis nurse specialists and representatives from independent dialysis service providers (Baxter, B.braun, Fresenius) via email. Members of the research team are part of the Wales Kidney Research Unit, and these stakeholders were known to the academic team; those who were not immediately known were contacted by NHS members of the research team. Kidney charity representatives were also invited.
To bolster these specifically curated meetings, the evolving framework in Table 2 was shared with stakeholders across Wales from November 2018 to March 2020 (16 months) to provide their input. Members of the research team attended regular meetings and events hosted by the coproductive partners, for example, operational engagements led by the NHS such as quarterly all‐Wales specialist nurse meetings and kidney third sector partner support events such as ‘transplant cafes’. Members of the research team who were patients also gathered anonymized information by speaking to patients in their roles as peer support workers and feeding information back to the research team throughout the data collection window.
Data analysis
List of key events and attendees
North Wales curated meeting: Total n = 30, n = 18 renal professionals (nephrologists, kidney specialist nurses), n = 8 family members, n = 4 people with kidney disease
South Wales curated meeting: Total n = 20, n = 12 renal professionals (nephrologists, social workers, youth workers, specialist nurses), n = 2 family member, n = 2 people with kidney disease, n = 4 kidney industry partners.
Transplant cafés: Total n = 21, n = 7 renal professionals (specialist nurses, social workers clinical psychologists), n = 12 people with kidney disease, n = 2 industry partners.
Table 2.
How can coproduction improve the sustainability of kidney services in Wales
| What is unsustainable (and barriers to sustainability) in the current adult CKD service in Wales | What does a sustainable kidney service look like for adult CKD services in Wales. ‘What does good look like?’ | What can be changed through coproduction? | |
|---|---|---|---|
| People living with kidney disease (PLKD) | |||
| Decision making |
|
|
|
| Demographics |
|
|
|
| Social contexts and services |
|
|
|
| Expectations versus reality |
|
|
|
| Family members, close friends, unpaid carers | |||
| Influences and concerns |
|
|
|
| Professionals: Multidisciplinary teams | |||
| Bias |
|
|
|
| Variation in practices |
|
|
|
| Staffing and training |
|
|
|
| Organizations: NHS, Wales Renal Clinical Network (WRCN), Kidney Charities, Independent Service Providers (ISPs), Welsh Government | |||
| Configuration of services |
|
|
|
| Limited resources |
|
|
|
| Policy contexts |
|
|
|
| Clinical recommendations |
|
|
|
| Outside secondary care including early‐stage CKD, the public, wider health and social care services | |||
| Overall Health literacy |
|
|
|
| Population |
|
|
|
| Wider service configurations |
|
|
|
| Research |
|
|
|
| Culture |
|
|
|
| Public perceptions and attitudes |
|
|
– Kidney charities can work with wider charity providers and Public HealthWales to support raising awareness of ESRD treatments. |
Abbreviations: ACP, advance care plan; CKD, chronic kidney disease; ESRD, end stage renal disease; GP, general practitioner; HHD, home haemodialysis; ISP, independent service provider; MDT, multidisciplinary team; NHS, National Health Service; NICE, National Institute for Health and Care Excellence; PIP, personal independent payment; PLKD, people living with kidney disease; QOL, quality of life; RRT, renal replacement therapy; SDM, shared decision making; UHD, hospital‐based dialysis; WG, Welsh Government; WRCN, Wales Renal Clinical Network
The research team reviewed Table 2 together at their weekly core team meetings and discussed and further refined the evolving content. The team hosted a specifically co‐ordinated data analysis meeting (13 November 2019) with selected wider stakeholders including people with kidney disease who were becoming increasingly knowledgeable on the sustainability issues. Table 2 was cleaned, and each sustainability element was summarized and sense‐checked by the multidisciplinary research team and people living with kidney disease and presented as a final stand‐alone sustainability table (Table 2).
-
2.
To redesign service pathways in adult CKD
-
Data collection
The original draft of the service improvement pathway 'pathways to home' (Figure 3) was designed by the lead kidney nurse for Wales, also a study coapplicant and expert in the current state of Welsh kidney services. The initial drafting also had patient input from representatives of the WKRU.
The research team worked to ensure that the draft pathways were shared with representatives from the full NHS MDTs; the specialist renal nurses in predialysis and home therapies, professionals allied to medicine including physiotherapists, dieticians and clinical psychologists, kidney social workers and youth workers, people living with kidney disease, family members, kidney third sector CEOs and staff working for kidney charities, and volunteer peer‐to‐peer support workers—many of whom were either living with kidney disease or a family member of someone with kidney disease. This took place over 16 months from March 2019 to June 2020.
We did this by sharing the first drafts of the pathways at quarterly NHS specialist nurse meetings and quarterly professionals allied to medicine meetings (which were also attended by patients and kidney third sector partners). The research team also worked with kidney charity partners to set up specially coordinated Zoom meetings to present to people living with kidney disease, family members and charity provider executives. These Zoom meetings were developed into webinars, which were made available online on YouTube and promoted on social media (Twitter, Facebook, mailing lists) for people to refer and feedback into via comments, telephone and email communications. This process continued over 15 months at face‐to‐face and virtual meetings until no new options or additions were forthcoming and there was a sense of data saturation.
Data analysis
Figure 3.

Draft service improvement documents ‘Pathways to Home’
Analysis was integrated into the development of the pathways from the outset. We presented the current service pathway as a backdrop and then asked what needed to/should be added to improve uptake of home therapies. Each engagement event was an opportunity for refinement and clarification from the multiple perspectives. This helped to highlight gaps in terms of what the service did not currently have and then move onto possibilities for improvement across the multiple service pathways. The before and after snap shots helped set out the vision for what kidney services could look like at a fairly high level across Wales and to more easily present this in relevant ways to the multiple stakeholders for their input.
Summary of key events and attendees
All Wales National Home Therapies meeting (29.04.19): Total n = 20, n = 18 renal professionals (kidney specialist nurses, nurse managers and directorate managers), n = 1 family member and kidney charity representative, n = 1 people with kidney disease
Presentation and meeting with Kidney patient ‘befrienders’ via kidney charity (12.09.19): Total n = 10, n = 2 family members, n = 8 people with kidney disease
All Wales Health and Wellbeing reference group (22.10.19): total n = 10, n = 9 renal professionals (dieticians, social workers, physiotherapies, psychologists) n = 1 kidney charity provider.
-
3.
To review patient education materials and processes
-
Data collection
There were around 15 specialist nurses working across five kidney centres in Wales. We contacted each centre lead nurse and requested that they collate their current paper‐based education materials and send to the research team. We developed a simple pro forma education flow chart and requested that the nurses fill it in to illustrate their current education practice, from initial conversation through to making a choice of RRT. We also requested that all Wales figures for numbers of people on home dialysis from the WRCN were shared. The research team then invited the lead nurse of the only centre that was achieving the national guidelines of 30% of patients on home dialysis to come and present at a specially co‐ordinated coproductive multidisciplinary meeting (with people with kidney disease and family members in their service also attending) and explain how their service worked. Academic members of the research team were also invited (following a study update at an NHS quarterly meeting) to attend a house visit with a specialist nurse (from a different centre) to observe their initial conversations with a person needing renal replacement therapy and their family members.
Data analysis
After the materials were collected, the research team reviewed their content alongside a review of the numbers of people on home dialysis across Wales by region and centre and presented the review as well as examples of education materials back to a group of professionals, people with kidney disease and family members for their input. Despite education processes looking broadly similar across centres, on paper, the review of the number of people on home dialysis varied significantly (File S3). The lead nurse presentation was followed by a question‐and‐answer session to an MDT room of practitioners from different services, people with kidney disease and family members to ask more about why their service appeared to be overachieving. People with kidney disease and family members were also invited to share their recent experiences of predialysis education and expressed their views on the barriers to home therapies from their perspectives. The field visit to the pre‐dialysis person's home with their family was followed by a detailed discussion with the nurse, a report and presentation of findings to the research team at core team meetings.
Summary of key events and list of attendees
National Chronic Kidney Disease specialist nurse meeting (22.11.19): Total n = 13, n = 9 kidney professionals (specialist kidney nurses), n = 2 family member, n = 2 people with kidney disease
Presentation from home therapies teams (25.11.19): Total n = 35, n = 12 kidney professionals (specialist nurses, nephrologists, social workers), n = 10 family members, n = 13 people with kidney disease
Field visit with CKD nurse to home consultation (27.11.19) total n = 3, n = 1 specialist kidney nurse, n = 1 family member, n = 1 person living with kidney disease
Visits to dialysis Units across Wales (25.02.19, 29.08.19, 30.08.19) total n = 17 people with kidney disease
-
4.
To better understand patient and public attitudes towards the costs of kidney care and services
-
Data collection
Academic members of the research team attended nonkidney disease‐related public events during the 18‐month data collection window of the study. This included hosting a market stall at the St. David's Day parade, presenting at the all Wales Involving people festival and attending local community group meetings with Black Asian Minority Ethnic individuals and groups to enhance opportunities for learning and interactive feedback with the public in Wales including minority and underrepresented groups. We attended the National Transplant games in Newport and the WRCNs ‘Renal Roadshow’ with a banner and preamble to introduce the topic of treatment option costs to the public and invite their opinion. We delivered presentations at kidney patient‐led conferences and meetings to discuss costs and gather perspectives with larger and smaller groups of kidney patients. We also approached social services commissioners in Wales to learn from their perspectives and invited commissioners to a specially co‐ordinated meeting on Zoom to discuss the sustainability of kidney services.
Data analysis
Analysis was built into the discussions with members of the public. We asked about their perceptions of costs and asked them to list which treatments they felt were the most to the least expensive. This was followed by opinions on service configurations and, in particular, if and how they felt social services could support a home‐first agenda. Field notes were collected from each engagement and presented back to the research team at core meetings for discussion.
Summary of key events and list of attendees
St David's Day parade Pembrokeshire (01.03.19): Total n = 40 members of the public
Bangor University Centre for Health Economics invited seminar (14.05.20): Total n = 15 members of the public
‘Renal Roadshowz’ West Wales (04.07.19): Total n = 40, n = 20 kidney professionals (specialist nurses, physiotherapists, dieticians, pharmacists), n = 10 family members, n = 10 kidney patients
Workshop with kidney ‘befrienders' (12.11.19): Total n = 9, n = 1 family members, n = 8 people living with kidney disease
‘Home therapies café’ (07.02.20) total 9, n = 6 people with kidney disease, n = 3 family members.
3. FINDINGS
-
1.
Creating a vision of a more sustainable adult kidney service in Wales
People living with kidney disease could play a potentially vital role in addressing specific sustainability issues (such as professional confidence in having perceived difficult conversations e.g., Advance Care Planning) all the way through to policy contexts and updating clinical practice (Table 2, What can be changed through coproduction). Involving people living with kidney disease and available peer‐to‐peer support networks earlier to help explain the benefits of home dialysis, alleviate concerns and empower people to make informed decisions about future tailored treatment plans could encourage more people to opt for home dialysis (Table 2, Decision making).
There needed to be more options to ‘try home dialysis out’ such as dedicated home training areas without any perceived burdens such as wait times including ‘nocturnal hotels’. The visibility of home‐based dialysis needed to increase across Wales and throughout the service (Table 2, Configuration of services).
The clear and known barriers to people opting for home dialysis, for example, needling, home reconfigurations, living alone, etc could be eliminated with creative and personalized approaches from the MDTs. We frequently found that factors listed as barriers were not particularly difficult or problematic to address or overcome such as worries about self‐administration of treatment, perceived inconveniences of home reconfigurations or perceived time saving of hospital dialysis (Table 2, Influences and concerns). Social care services needed to be better integrated with kidney health services to directly address where the NHS was picking up areas of unmet need, which might be better placed elsewhere. Healthcare services needed to recognize that CKD is a lifelong condition and that the service needs to be able to adapt to people as they progress through their life as well as their disease condition (Table 2, Social contexts and services).
-
2.
Redesigning service pathways in adult CKD, pathways to home
Required modifications to existing care pathways clearly showed that there needed to be more defined pathways for people ‘to get home’ and more quickly (Figure 3). The pathways highlighted areas where the service was potentially picking up areas of unmet need that might be best placed elsewhere; for example, patients on a conservative management pathway were currently being managed by specialist dialysis nurses and potentially missing out on wider palliative care services.
We observed a lack of support services for both patients and family members in these cases (clinical, psycho/social, wider social care support) and uncertainty within the renal teams with how best to manage them as a result.
New stepped stages in the pathway introduced opportunities for more MDT input, patient‐led support interventions and signposting to wider third sector and social services across all pathways. This could help reduce or prevent patients being siloed or treated solely on the basis of their current kidney treatment. It would also seek to eliminate service configurations that saw people finding themselves by default on unit/hospital dialysis with no clear alternate pathways (Figure 3, New pathways).
Pathways not clearly associated with home dialysis, for example, transplant were having an influence on people opting for or currently on UHD. For example, most people awaiting transplant in Wales are on UHD, but we know that most transplants will eventually fail and that patients rarely decide to switch dialysis modalities (Table 2, Decision making). These new pathways included more clear definitions and acknowledgement of the multiple ‘pre‐transplant dialysis’ pathways and their potential influence on getting onto home dialysis.
-
3.
Review of patient education materials and processes
We found that the attitudes of professionals had a huge influence on uptake of home dialysis, and there was variation in perceived barriers to home dialysis and how people felt they could overcome them. The clinical nurse specialists enthusiasm for home dialysis and a very connected service both in practice (they work in the same offices) and in behaviour (all of the team felt no barrier was too high to overcome to get people on home dialysis) helped to create a culture of a home‐first service. Many of these nurses even felt that the national targets were too low. They also expressed concern that It was too easy for people to opt for UHD nowadays, and that the pathway had become the norm rather than the exception in Wales. This particular team had developed over time a home dialysis‐led service with problem‐solving approaches to known barriers to home dialysis (e.g., needling, living alone, space, home reconfigurations, safety etc.), of which they were very proud. Close working relationships and up‐to‐date expertise in the various dialysis treatments helped create a culture that questioned the status quo and a desire to change it (presentation from home therapies teams (25.11.19)).
Paper‐based education (based largely on describing dialysis and kidney disease) was having little impact. Patients rarely read the resources provided. Family members did, but this only exasperated patient and family member concerns and increased worry. There was also little evidence of resources especially developed for family members. In service configurations with high numbers of patients on home dialysis, the family were given equal attention by professionals and managed alongside, but separate to patients (field visit with CKD nurse to home consultation (27.11.19)).
Professionals rarely, if ever, used predesigned paper‐based education materials as part of their conversations. They preferred to rely on their own expertise and rapport with the patient. During the study, some professionals began to reconsider what ‘education materials’ actually mean and how they can support a home therapies agenda. This began by shifting the purpose of education away from explaining dialysis and more towards showcasing living well on dialysis. People going through kidney replacement therapy education will always have a consultant and specialist nurse to manage their care and will have access to a wider MDT for more specific needs. Education programmes are needed to help and support these roles, signpost to their expertise and then fill gaps in professional knowledge, for example, lived experiences as told by patients. Peer‐led networks and opportunities to interact with more patients on home dialysis were considered essential, as was removing and decommissioning any information and literature that did not talk to a home‐first agenda (Table 2, Variation in practice).
While most professionals said that they supported home therapies, there was variation in perceived barriers to home therapies and how people felt they could overcome them. This was exacerbated by a lack of clear processes for ‘escalation’ for complex cases such as sudden and unexpected change of mind, decisions that were firmly against clinical (and family) advice or cases where there was disagreement (amongst professionals) as to what treatment to recommend (Table 2, Bias).
Finally, we also observed that a standard model of dialysis was deskilling some of the specialist workforce, for example, up‐to‐date knowledge of various types of dialysis, confidence in (re)approaching families who initially declined home dialysis or changed their minds and overall experience in communication techniques including SDM (Table 2, Staffing and training).
-
4.
Patient and public attitudes to costs of health services
There were substantial gaps in peoples' understandings of the costs of dialysis treatments as well as mixed views about shifting or reconfiguring costs. While in general patients and members of the public understood that NHS services cost money, they had not previously thought about the different costs of various treatments. People were very surprised to learn about potential variations in costs and the potential savings. Very few people had previously considered the fact that the NHS might be picking up unmet social care needs, which were in turn having a substantial impact on NHS finances. Once members of the public and patients were made aware that the potential savings were substantial; they felt that everything possible should be done to realize cost savings and develop more sustainable services (Table 2, Policy contexts).
We also observed clearly that policy contexts designed to develop and create more fair, equitable and parity to public health service spending were not well understood. Sometimes, discussions about costs and service reconfiguration were met with suspicion and an overall perception that potential saving was equated to cost‐cutting. Responses to shifting costs between services were mixed. The public generally supported the idea of shifting costs from social services to health, but not the other way around. The public perception was that social services were stretched to an upper limit and would be unable to cope with any costs newly attributed to social services. Social service workers, volunteers and commissioners initially struggled to see some of the unmet social care needs that the NHS was picking up and the potential costs of this. Their immediate reactions were that dialysis is a primary healthcare need, and they did not necessarily see the potential benefits of a more integrated health and social service package of care to pick up very clear unmet social care needs, for example, isolation and loneliness (Table 2, Outside secondary care).
Costs were never a consideration when discussing and recommending treatment options to patients. Professionals do not routinely discuss costs and have limited knowledge of NHS costs, spending, commissioning and service design. Importantly, we saw that professionals did not feel at all comfortable talking about costs and service configurations in front of patients and actively avoided talking about real barriers in terms of service delivery in general with patients (Table 2, Limited resources).
4. DISCUSSION
4.1. Main findings
This study highlighted the effects of the unsustainable service on the multiple stakeholders. This included an unhelpful standardized model of care for all people with kidney disease, a default position to UHD as the norm and a deskilling of some specialist key roles. Key stakeholders—people on home therapies—are essential to understanding sustainability contexts and developing new service pathways, and their input remains essential to realizing the outcomes and ambitions of any coproduced outcomes. More integrated health and social care kidney services have the potential to lead to a more financially sustainable NHS (reducing NHS burden by reconfiguring services out of hospitals and more towards home), but this needs to be underpinned with a shared vision from professionals in key influencing roles if models of care are to switch from acute to long‐term sustainable care packages. A significant gap was the lack of understanding (from the multiple perspectives) of dialysis monetary value—how much various services cost and how they are delivered. Policy contexts (e.g., value‐based and prudent healthcare) were not well understood; generally, people understood potential service improvement initiatives as a cost‐cutting measure and could see (at least initially) little potential benefits to them. Many healthcare professionals did not immediately connect potential impacts of UHD on long‐term patient outcomes, especially nonclinical impacts, for example, restrictions on travel, work, childcare and lifestyle. Many had never heard of the policy contexts or were unclear as to how these related to them.
4.2. Meaning of this study in relation to other research
As with previous research, we found that local practices or perhaps more accurately ‘individual personalities’ influence the uptake of home dialysis and help explain some of the observed variation between centres. 52 , 53 , 54 This study went a step further in terms of realizing how these individuals can be (re)imagined as a resource—key influencers to change—at the multiple levels from practice through to policy.
Generally, previous research into kidney health service improvement has a high focus on clinical outcomes. 55 More recent health service improvement initiatives have focussed on encouraging people already on UHD to have a more proactive role in their dialysis and increase opportunities for self‐care. 56 In this study, the coproductive approach set within the context of sustainability—and not just the clinical benefits of home dialysis—supported key stakeholders to unpick on their own terms what they saw as barriers to home therapies and ways to achieve more sustainable services.
The coproductive outcomes in this study reinforce the assertions of Elwyn et al. 23 that SDM on its own does nothing.Interventions intended to bring about change need appropriate infrastructures, training and multiple linked networks to realize their aims. The coproductive approaches in this study have helped to identify what resources are already available and where additional investments may be needed. This contributes to the growing literature around global coproduction practice and value.
4.3. Implications for clinicians and policymakers
Increasing the number of people on home dialysis is a global health priority. The UK NICE first recognized the benefits of home dialysis more than 20 years ago; 57 yet, unit/hospital dialysis continues to increase. Lord Nigel Crisp (independent Member of the House of Lords), in a recent letter to the BMJ, highlighted that ‘UK health and care system, like all others in the West, is still largely using a 20th century acute care model of service delivery to meet 21st century needs’ and put forward seven factors necessary to contribute to sustainability (1. Efficiency and effectiveness of health and care provision, 2. Availability of well‐trained health and care workers, 3. Costs and economic benefits, 4. Health and resilience of the population, 5. Contribution of carers and informal networks of care, 6. Integration of policy and practice with other sectors and building healthy and health creating communities and 7. Public and political acceptability and support), highlighting that two in particular need more emphasis—economic benefits and multisectoral partnerships. This study unpacked key issues within all seven factors (Table 2), and by utilizing a coproductive approach, highlighted the ways in which the current service was working contradictorily to prudent healthcare and created a new vision for what a good adult CKD service looks like in Wales. 58
Commitment is needed from all the multiple stakeholders to develop networks and opportunities for meaningful knowledge coproduction and ways to sustain it. This includes working more closely and more frequently with people living with kidney disease, their family and networks of support. As of April 2020, there were 292 people on various types of home dialysis in Wales. This group are potentially one of the biggest untapped resources that can influence changes in attitudes and culture towards a home‐led service and actually support (rather than compete with) the wider health and social care agenda towards prudent healthcare.
Knowledge gained from this study includes the coproduced vision of more sustainable services, improved pathways to home dialysis and opportunities for greater integration of social care services and highlights ways to more proactively involve people with kidney disease more directly in service reconfiguration. This learning and the methods to coproduce it have the potential for transferability to similarly configured global healthcare systems. Redesigned pathways may even be more easily adapted outside of Wales, which has an older, sicker and more deprived population than other countries, and health literacy is generally low. Although additional account may need to be taken of country‐specific social care systems and the ways in which they currently integrate with health services to make best and better use of existing resources.
4.4. Strengths and weaknesses of the study
This is the first all‐Wales co‐productive study to address the sustainability of adult CKD health and social care services from direct and indirect key stakeholder perspectives. We believe that this is the first application of the principles for knowledge coproduction in sustainability research in kidney health research and can be built upon in future research, quality improvement and service development initiatives. 50 The study was limited to Wales, which has a predominantly white population, and it was not able to account for extraordinary events, for example, COVID‐19 (data collection completed just before the pandemic), although many feel that COVID‐19 has simply provided a stark reminder of the unsustainability of the NHS in general in its current guise and the need to keep people living well and at home. Finally, this study was not designed to measure any specific outcomes of sustainability, but rather the potential of coproduction to improve sustainability for the multiple stakeholders.
4.5. Unanswered questions and future research
The question can coproduction lead to more sustainable adult CKD services in Wales was the focus of this study. In this context, we have only been able to partially answer it. We do not know explicitly whether coproduction will lead to greater sustainability of kidney services as this was not conceptualized as a longitudinal study to monitor behaviour change over time. For this, more research is needed over a longer period, with a larger and more diverse population to build upon the work outlined in this study, which includes templates on ways to work coproductively with NHS MDTs, kidney charities and people living with kidney disease. The NHS now needs to implement the new clinical pathways and embrace the transformational roadmap to change that was co‐produced with patients. 44 Going forward, it will be important to evaluate the outcomes of coproductive research and processes using routine data collection methods, for example, routinely collected patient data, health economics modelling, patient‐reported outcome measures and patient‐reported experience measures.
5. CONCLUSION
Coproductive research helped start a conversation between key stakeholders and researchers about sustainability. Much more needs to be done to increase the overall understanding of NHS financial and service structures to ensure that this is not a barrier in any future coproduction. Coproduction has the capacity to identify and reverse unintended consequences of health service systems that have (almost always) grown based on perceived immediate need, with little evidence basis and over a very long time. More case studies are needed to provide exemplars of what key policy contexts look like in health service delivery to realize the ambitions of prudent healthcare at scale.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Leah Mc Laughlin led on coproductive activities, conceptualized the coproduction and drafted the manuscript. Gail Williams co led on coproductive activities, drafted key service redesign pathways, produced home therapies reports, undertook data analysis and data integration and reviewed the manuscript. Gareth Roberts developed the overall study design, co led on some coproductive activities and reviewed the manuscript. David Dallimore contributed to the design of coproductive activities, supported overall coproduction, contributed to data analysis and data integrated and reviewed the manuscript. David Fellowes contributed to data analysis and data integration, and reviewed the manuscript. Joanne Popham provided key coproductive support to deliver objectives, key understanding of configuration of peer support workers and reviewed the manuscript. Joanna Charles supported the coproduction of some activities and supported sharing of interim findings. James Chess developed the overall study design, and supported data integration and analysis. Sarah Hirst Williams provided key understanding of NHS home therapy service configurations, coproduced data and reviewed the manuscript. Jonathan Mathews supported the overall coproductive activities, coordinated multiple group meetings, provided data sets and reviewed the manuscript. Judith Stone provided key coproductive support to deliver objectives, key understanding of charity providers configurations and their potential influences and reviewed the manuscript. Teri Howells supported the overall study design and supported coproductive development. Teri sadly passed away before this study was completed. Linzi Isaac supported the coproduction of activities, supported sharing interim findings with UK patients and reviewed the manuscript. Jane Noyes oversaw coproductive activities, conceptualized the coproduction and drafted the manuscript.
ETHICS STATEMENT
This study was approved by Wales REC 5. REC No. 19/WA0020. IRAS ID: 255387.
Supporting information
Supporting information.
Supporting information.
Supporting information.
ACKNOWLEDGEMENTS
The authors would like to thank all the NHS Kidney health and social care professionals working across Wales, including: Consultants—Sian Griffin, Ruth Benzimra, Sarah Browne, Kieron Donovan, Helen Jefferies, Mat Davies, Mahdi Jibani, Soma Meran, Ashraf Mikhail, Siva Shrikanth, Michael Stephens, Nicki Pease; NHS Renal Managers—Claire Main, Lisa Higginson, Jennifer Ann Williams, Ruth Glover, Meryl Webb Jones; Predialysis nurses in: Cardiff (Nerys Thomas, Alison Pritchard, Annwen Goodland, Justine Aggett); Swansea (Lynda Thomas, Nicola Medicke, Amanda Rees); Bangor (Dawn Hails, Donna Jones, Emma Davies, Jane Powell); Glan Clwyd (Anna Jolley, Ruth Glover); Wrexham (Angie Monk, Jacqui Jones, Kerry Burlison, Sally Griffiths).Home Therapy Teams in Cardiff (Clare Porter, Francis Robinson, Sally Jones, Shirley Huerta); Swansea; Bangor (Julie Moxley, Sara Baker); Glan Clwyd (Melanie Hayward, Nicola Roberts, Karen Davies); Wrexham (Sandie Coleclough, Gail Oldfield Jones, Hayley Water House). Dialysis NHS Technical Services—Andrew long, Jim Blackie, Specialist Renal Social Workers—Caron Jones, Jayne Davis, Andrew Barnett, Laura McGuinness; Renal Pharmacists—Chris Brown, Owain Brookes; Dieticians—Emma Catling, Harriet Williams, Anne Williams, Elizabeth Wynne, Ffion Hughes, Laura Eilbeck, Sarah Gooda; Physiotherapists—Louise Kennedy, Clare Weekes; Psychologists—Kate Shakespeare, Paul Gardner, Beth Parry Jones, Catherine O Leary, Amy Howells, Caroline Anderson, Louise Evans, Misbah gladwyn‐khan; Counsellors—Maria Nunan; Youth Workers—Shaun Thomas. The Welsh Renal Clincial Network Manager: Susan Spence. The Welsh Renal Clinical Network Specialist Staff: Jennifer Holmes, Helen Harris, Richard Davies; Renal Registrars: Karen Brown, Carmen Mallett; Industry B.braun: Jane Doherty. Baxter; Jonathan Florence; The Paul Popham Fund Counsellor: Hayleigh IsaacThe Paul Popham Fund Peer to peer support workers including; Geraint John, Patricia Ann Hill, Melanie Pickman, Penny Turner, Helen Jones, Joseph Townsend, Amanda Tully, Julie Jones, Roger Bambridge, Lynda Griffiths, Jamie de Lloyd Bowen, Michael Stacey, Margaret Susan Parry, Brian Hill Fiona Akpinar, Robin Simpson. Kidney Wales Patient Advocates—Brett Dowds and Shaun Ruck. Kidney Care UK Advocacy Officer—Francesca Teasdale. Dialysis Unit Managers—Toni Hamlett, Tracy Owen, Lisa Davies, David West. Commissioners Social Services ADSS CYMU—Jayne Davis, Louise Sweeney. Wider third sector services—Carers Wales, Action for Elders, Care and Repair Cymru, Citizens advice. Local councils—Gwynedd, Carmarthenshire. Bangor University School of Sport—Jamie MacDonald, Jennifer Cooney Bangor University School of Health Economics; Rhiannon Tudor Edwards, Ned Hartfiel, Joanna Charles. Wales Kidney Research Unit (WKRU) Manager—Chantal Colmont. Director WKRU—Donald Fraser.Patient Representatives and Members of WKRU Eexecutive Board—Gloria Owens and Janet Williams. Finally a special thank to all people living with kidney disease across Wales and family and friends who contributed to this work by attending events, sharing your views and participating in interviews and focus groups.This study was funded by Health and Care Research Wales, Research for Patient and Public Benefit Scheme. This study was supported by WKRU.
Mc Laughlin L, Williams G, Roberts G, et al. Assessing the efficacy of coproduction to better understand the barriers to achieving sustainability in NHS chronic kidney services and create alternate pathways. Health Expect. 2022;25:579‐606. 10.1111/hex.13391
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the Supporting Information Material of this article.
REFERENCES
- 1.Global Facts: About Kidney Disease. National Kidney Foundation. Accessed July 6, 2020. https://www.kidney.org/kidneydisease/global-facts-about-kidney-disease#_ENREF_1
- 2. Coresh J. Update on the burden of CKD. J Am Soc Nephrol. 2017;28(4):1020‐1022. 10.1681/ASN.2016121374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jha V, Modi GK. Getting to know the enemy better—the global burden of chronic kidney disease. Kidney Int. 2018;94(3):462‐464. 10.1016/j.kint.2018.05.009 [DOI] [PubMed] [Google Scholar]
- 4. Fraser SDS, Roderick PJ. Kidney disease in the Global Burden of Disease Study 2017. Nat Rev Nephrol. 2019;15(4):193‐194. 10.1038/s41581-019-0120-0 [DOI] [PubMed] [Google Scholar]
- 5. Bikbov B, Purcell CA, Levey AS, et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10225):709‐733. 10.1016/S0140-6736(20)30045-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end‐stage kidney disease: a systematic review. Lancet. 2015;385(9981):1975‐1982. 10.1016/S0140-6736(14)61601-9 [DOI] [PubMed] [Google Scholar]
- 7. Abdel‐Kader K, Unruh ML, Weisbord SD. Symptom burden, depression, and quality of life in chronic and end‐stage kidney disease. Clin J Am Soc Nephrol. 2009;4(6):1057‐1064. 10.2215/CJN.00430109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nguyen NTQ, Cockwell P, Maxwell AP, Griffin M, O'Brien T, O'Neill C. Chronic kidney disease, health‐related quality of life and their associated economic burden among a nationally representative sample of community dwelling adults in England. PLoS One. 2018;13:e0207960. 10.1371/journal.pone.0207960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crews DC, Bello AK, Saadi G. Burden, access, and disparities in kidney disease. Brazilian J Med Biol Res. 2019;52(3), 10.1590/1414-431x20198338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Anderson S, Halter JB, Hazzard WR, et al. Prediction, progression, and outcomes of chronic kidney disease in older adults. J Am Soc Nephrol. 2009;20(6):1199‐1209. 10.1681/ASN.2008080860 [DOI] [PubMed] [Google Scholar]
- 11. Luyckx VA, Tonelli M, Stanifer JW. The global burden of kidney disease and the sustainable development goals. Bull World Health Organ. 2018;96(6):414‐422C. 10.2471/BLT.17.206441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chronic Kidney Disease. Accessed July 6, 2020. https://www.theisn.org/focus/ckd#publications
- 13.Recommendations, Renal replacement therapy and conservative management, Guidance, NICE. Accessed June 12, 2020. https://www.nice.org.uk/guidance/ng107/chapter/Recommendations#indications-for-starting-dialysis
- 14. Network WR . Renal Services in Wales 2016–2020 DELIVERY PLAN; 2016. Accessed October 11, 2019. http://www.wales.nhs.uk/sites3/Documents/773/Renal_Disease_Quality_Delivery_Plan1.pdf
- 15. UK Renal Registry . Audit Portal. Accessed October 11, 2019. https://www.renalreg.org/datasets/audit-portal/
- 16. UK Renal Registry. UK Renal Registry 21st Annual Report—data to 31/12/2017, Bristol, UK. 2019. Accessed June 12, 2020. https://www.renalreg.org/publications-reports/
- 17. Purvis B, Mao Y, Robinson D. Three pillars of sustainability: in search of conceptual origins. Sustain Sci. 2019;14(3):681‐695. 10.1007/s11625-018-0627-5 [DOI] [Google Scholar]
- 18. Future Generations Act . Future Generations Commissioner for Wales. Accessed June 15, 2020. https://futuregenerations.wales/about-us/future-generations-act/
- 19. Government Welsh . SOCIAL SERVICES AND WELL‐BEING (WALES) ACT 2014. Www.Ccwales.Org.Uk/Getting‐in‐on‐the‐Act‐Hub/ #GetTheAct The Main Principles Underpinning the Act: Voice and Control, Prevention and Early Intervention, Well‐Being, Co‐Production and Multi Agency. 2014. Accessed May 30, 2020. https://socialcare.wales/cms_assets/hub-downloads/Principles-Resource-Guide_March-17.pdf
- 20. Prudent Healthcare Securing Health and Well‐Being for Future Generations . Wales Securing Health and Well‐Being for Future Generations 2 Focusing Collective National Action around 3 Main Areas. Accessed June 15, 2020. www.prudenthealthcare.wales
- 21. Welsh Government . Social Services and Wellbeing (Wales) Act 2014; 2014. Accessed October 31, 2019. http://www.legislation.gov.uk/anaw/2014/4/pdfs/anaw_20140004_en.pdf
- 22. Welsh Government . Care and support at home, a summary of the five year strategic plan 2017–2022; 2017. Accessed October 31, 2019. https://socialcare.wales/cms_assets/file-uploads/Plan-on-a-page-English.pdf
- 23. WHO . Donation and transplantation; 2013. Accessed February 11, 2020. https://www.who.int/transplantation/donation/en/
- 24.Valuing Our Health Chief Medical Officer for Wales. Annual Report 2018/19. https://gov.wales/sites/default/files/publications/2019-05/valuing-our-health.pdf
- 25. Spencer M, Dineen R, Phillips A, et al. Tools for improvement 1000 Lives co‐producing services/co creating health. Accessed May 30, 2020. www.1000livesi.wales.nhs.uk
- 26.Co‐production Network for Wales. Accessed May 30, 2020. https://copronet.wales/
- 27.Guidance on co‐producing a research project. Accessed August 7, 2020. https://www.invo.org.uk/posttypepublication/guidance-on-co-producing-a-research-project/
- 28. Realpe A, Wallace LM. What is co‐production? Identify, Innovate, Demonstrate Encourage.
- 29. Batalden M, Batalden P, Margolis P, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25(7):509‐517. 10.1136/bmjqs-2015-004315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Graffigna G, Barello S, Palamenghi L, Lucchi F. “Co‐production Compass” (COCO): an analytical framework for monitoring patient preferences in co‐production of healthcare services in mental health settings. Front Med. 2020;7:279. 10.3389/fmed.2020.00279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vennik FD, van de Bovenkamp HM, Putters K, Grit KJ. Co‐production in healthcare: rhetoric and practice. Int Rev Adm Sci. 2016;82(1):150‐168. 10.1177/0020852315570553 [DOI] [Google Scholar]
- 32. De Rosis S, Pennucci F, Noto G, Nuti S. Healthy living and co‐production: evaluation of processes and outcomes of a health promotion initiative co‐produced with adolescents. Int J Environ Res Public Health. 2020;17(21):1‐19. 10.3390/ijerph17218007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Oliver BJ, Batalden PB, Dimilia PR, et al. COproduction VALUE creation in healthcare service (CO‐VALUE): an international multicentre protocol to describe the application of a model of value creation for use in systems of coproduced healthcare services and to evaluate the initial feasibility, utility and acceptability of associated system‐level value creation assessment approaches. BMJ Open. 2020;10(10):37578. 10.1136/bmjopen-2020-037578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Redman S, Greenhalgh T, Adedokun L, Staniszewska S, Denegri S. Co‐production of knowledge: the future. BMJ. 2021;372:n434. 10.1136/bmj.n434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Williams O, Sarre S, Papoulias SC, et al. Lost in the shadows: reflections on the dark side of co‐production. Heal Res Policy Syst. 2020;18(1):43. 10.1186/s12961-020-00558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tembo D, Hickey G, Montenegro C, et al. Effective engagement and involvement with community stakeholders in the co‐production of global health research. BMJ. 2021;372:n178. 10.1136/bmj.n178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Broom A, Parker R, Raymond S, et al. The (co)production of difference in the care of patients with cancer from migrant backgrounds. Qual Health Res. 2020. 2020;30(11):1619‐1631. 10.1177/1049732320930699 [DOI] [PubMed] [Google Scholar]
- 38. Filipe A, Renedo A, Marston C. The co‐production of what? Knowledge, values, and social relations in health care. PLoS Biol. 2017;15(5):2001403. 10.1371/journal.pbio.2001403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Palumbo R, Manna R. What if things go wrong in co‐producing health services? Exploring the implementation problems of health care co‐production. Policy Soc. 2018;37(3):368‐385. 10.1080/14494035.2018.1411872 [DOI] [Google Scholar]
- 40. Oliver K, Kothari A, Mays N. The dark side of coproduction: do the costs outweigh the benefits for health research? Health Res Policy Syst. 2019;17(1):33. 10.1186/s12961-019-0432-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Noyes J, Mclaughlin L, Morgan K, et al. Designing a co‐productive study to overcome known methodological challenges in organ donation research with bereaved family members. Health Expect. 2019;22(4):824‐835. 10.1111/hex.12894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Turk E, Durrance‐Bagale A, Han E, et al. International experiences with co‐production and people centredness offer lessons for covid‐19 responses. BMJ. 2021;372:m4752. 10.1136/bmj.m4752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fusco F, Marsilio M, Guglielmetti C. Co‐production in health policy and management: a comprehensive bibliometric review. BMC Health Serv Res. 2020;20(1):1‐16. 10.1186/s12913-020-05241-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Increasing the impact of health research through co‐production of knowledge. World Health Organisation; 2021. Accessed February 23, 2021. https://www.bmj.com/co-producing-knowledge
- 45. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361‐1367. 10.1007/s11606-012-2077-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glyn Elwyn: Expecting too much of “patient decision aids.” Accessed August 12, 2020. https://blogs.bmj.com/bmj/2019/12/02/glyn-elwyn-expecting-too-much-of-patient-decision-aids/
- 47.Improvement 1000 Lives. 1000 Lives Improvement—Making Choices Together.
- 48. Noyes J, McLaughlin L, Morgan K, et al. Short‐term impact of introducing a soft opt‐out organ donation system in Wales: before and after study. BMJ Open. 2019;9(4):025159. 10.1136/bmjopen-2018-025159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Roberts G, Chess JA, Howells T, et al. Which factors determine treatment choices in patients with advanced kidney failure? A protocol for a co‐productive, mixed methods study. BMJ Open. 2019;9(10):e031515. 10.1136/bmjopen-2019-031515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Norström AV, Cvitanovic C, Löf MF, et al. Principles for knowledge co‐production in sustainability research. Nat Sustain. 2020;3(3):182‐190. 10.1038/s41893-019-0448-2 [DOI] [Google Scholar]
- 51. UK Standards for Public Involvement . NIHR Central Commissioning Facility, Patient and Public Involvement Team NCCF. 2019. Accessed February 19, 2020. https://sites.google.com/nihr.ac.uk/pi-standards/home
- 52. Jain AK, Blake P, Cordy P, Garg AX. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23(3):533‐544. 10.1681/ASN.2011060607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Struijk DG. Peritoneal dialysis in western countries. Kidney Dis. 2015;1(3):157‐164. 10.1159/000437286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Macgregor MS, Agar JWM, Blagg CR. Home haemodialysis‐international trends and variation. Nephrol Dial Transpl. 2006;21:1934‐1945. 10.1093/ndt/gfl093 [DOI] [PubMed] [Google Scholar]
- 55. Ebah L, Hanumapura P, Waring D, et al. A multifaceted quality improvement programme to improve acute kidney injury care and outcomes in a large teaching hospital. BMJ Qual Improv Reports. 2017;6(1):96‐104. 10.1136/bmjquality.u219176.w7476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. The Health Foundation . My improvement journey: renal care. Accessed June 11, 2021. https://www.health.org.uk/news-and-comment/blogs/my-improvement-journey-renal-care
- 57. (APPKG) TAPPKG . A HOME DIALY SISMANIFESTO. 2. Accessed June 23, 2020. https://www.kidney.org.uk/Handlers/Download.ashx?IDMF=ffca233b-27c8-4bbd-ae3d-1d3cad97cd6c
- 58. Crisp N. What would a sustainable health and care system look like? BMJ. 2017;358:358. 10.1136/bmj.j3895 [DOI] [PubMed] [Google Scholar]
- 59. Misra M, Phadke GM. Historical milestones in peritoneal dialysis. Contrib Nephrol. 2019;197:1‐8. 10.1159/000496301 [DOI] [PubMed] [Google Scholar]
- 60. St. George's Kidney Patients Association . History of the kidney disease treatment. Accessed July 8, 2020. https://www.sgkpa.org.uk/main/history-of-the-kidney-disease-treatment
- 61. DaVita Kidney Care . History of home hemodialysis. Accessed July 8, 2020. https://www.davita.com/treatment-services/home-hemodialysis/history-of-home-hemodialysis
- 62. Blagg CR. A brief history of home hemodialysis. Adv Ren Replace Ther. 1996;3(2):99‐105. 10.1016/S1073-4449(96)80048-3 [DOI] [PubMed] [Google Scholar]
- 63. Chandna SM, Schulz J, Lawrence C, Greenwood RN, Farrington K. Is there a rationale for rationing chronic dialysis? A hospital based cohort study of factors affecting survival and morbidity. BMJ. 1999;318(7178):217‐223. 10.1136/bmj.318.7178.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Blagg CR. The early history of dialysis for chronic renal failure in the United States: a view from Seattle. Am J Kidney Dis. 2007;49(3):482‐496. 10.1053/j.ajkd.2007.01.017 [DOI] [PubMed] [Google Scholar]
- 65. Wing AJ. Can we meet the real need for dialysis and transplantation? Br Med J. 1990;301(6757):885‐886. 10.1136/bmj.301.6757.885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Dialysis Patient Citizens Education Center . History and overview of home hemodialysis. Accessed July 8, 2020. https://www.dpcedcenter.org/news-events/news/history-and-overview-of-home-hemodialysis/
- 67.Dialysis in the UK in 1959. History of Nephrology. Accessed July 8, 2020. http://historyofnephrology.blogspot.com/2009/02/dialysis-in-uk-in-1959.html
- 68. Institute of Medicine (US) Committee for the Study of the Medicare End‐Stage Renal Disease Program . Structure of the provider community. In: Rettig RA, Levinsky NG, eds. Kidney Failure and the Federal Government. National Academies Press; 1991. [PubMed] [Google Scholar]
- 69. Fisher DJ, Johnson DB, Farrow SC. Dialysis and transplantation: the national picture over the next five years. Br Med J. 1972;3(5828):686‐690. 10.1136/bmj.3.5828.686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Wing AJ. Why don't the British treat more patients with kidney failure? BMJ. 1983;287(6400):1157‐1158. 10.1136/bmj.287.6400.1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. UKKA . Renal Units in the UK—The Renal Association. Accessed July 8, 2020. https://renal.org/information-resources/renal-units-in-the-uk/
- 72. Dobson R. Kidney patients should get more care from nurse practitioners and have dialysis closer to home. BMJ. 2007;334(7587):226. 10.1136/bmj.39111.705162.db [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Vinson AJ, Perl J, Tennankore KK. Survival comparisons of home dialysis versus in‐center hemodialysis: a narrative review. Can J Kidney Health Dis. 2019;6:1‐7. 10.1177/2054358119861941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Maruyama Y, Higuchi C, Io H, et al. Comparison of peritoneal dialysis and hemodialysis as first renal replacement therapy in patients with end‐stage renal disease and diabetes: a systematic review. Ren Replace Ther. 2019;5(1):44. 10.1186/s41100-019-0234-7 [DOI] [Google Scholar]
- 75. Baboolal K, Mcewan P, Sondhi S, Spiewanowski P, Wechowski J, Wilson K. The cost of renal dialysis in a UK setting‐a multicentre study. Nephrol Dial Transpl. 2008;23:1982‐1989. 10.1093/ndt/gfm870 [DOI] [PubMed] [Google Scholar]
- 76. Eriksson JK, Neovius M, Jacobson SH, Elinder CG, Hylander B. Healthcare costs in chronic kidney disease and renal replacement therapy: a population‐based cohort study in Sweden. BMJ Open. 2016;6(10):e012062. 10.1136/bmjopen-2016-012062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Rydell H, Ivarsson K, Almquist M, Segelmark M, Clyne N. Improved long‐term survival with home hemodialysis compared with institutional hemodialysis and peritoneal dialysis: a matched cohort study. BMC Nephrol. 2019;20(1):52. 10.1186/s12882-019-1245-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Surendra NK, Abdul Manaf MR, Hooi LS, et al. Cost utility analysis of end stage renal disease treatment in Ministry of Health dialysis centres, Malaysia: hemodialysis versus continuous ambulatory peritoneal dialysis. PLoS One. 2019;14(10):e0218422. 10.1371/journal.pone.0218422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Jansz TT, Noordzij M, Kramer A, et al. Survival of patients treated with extended‐hours haemodialysis in Europe: an analysis of the ERA‐EDTA Registry. Nephrol Dial Transpl. 2020;35:488‐495. 10.1093/ndt/gfz208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. ERA‐EDTA Registry . ERA‐EDTA Registry Annual Report 2017. Amsterdam UMC, location AMC, Department of Medical Informatics, Amsterdam, the Netherlands, 2019. 2017. Accessed June 12, 2020. https://era-edta-reg.org/files/annualreports/pdf/AnnRep2017.pdf
- 81. US Renal Data System . Annual Data Report: Epidemiology of Kidney Disease in the United States Executive Summary; 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The data that support the findings of this study are available in the Supporting Information Material of this article.


