Abstract
Introduction
Healthcare inequalities and ethnicity are closely related. Evidence has demonstrated that patients from ethnic minority groups are more likely to report a long‐term illness than their white counterparts; yet, in some cases, minority groups have reported poorer adherence to prescribed medicines and may be less likely to access medicine services. Knowledge of the barriers and facilitators that impact ethnic minority access to medicine services is required to ensure that services are fit for purpose to meet and support the needs of all.
Methods
Semistructured interviews with healthcare professionals were conducted between October and December 2020, using telephone and video call‐based software. Perspectives on barriers and facilitators were discussed. Interviews were audio‐recorded and transcribed verbatim. Reflexive thematic analysis enabled the development of themes. QSR NVivo (Version 12) facilitated data management. Ethical approval was obtained from the Newcastle University Faculty of Medical Sciences Ethics Committee.
Results
Eighteen healthcare professionals were interviewed across primary, secondary and tertiary care settings; their roles spanned medicine, pharmacy and dentistry. Three themes were developed from the data regarding the perceived barriers and facilitators affecting access to medicine services for ethnic minority patients. These centred around patient expectations of health services; appreciating cultural stigma and acceptance of certain health conditions; and individually addressing communication and language needs.
Conclusion
This study provides much‐needed evidence relating to the barriers and facilitators impacting minority ethnic communities when seeking medicine support. The results of this study have important implications for the delivery of person‐centred care. Involving patients and practitioners in coproduction approaches could enable the design and delivery of culturally sensitive and accessible medicine services.
Patient or Public Contribution
The Patient and Public Involvement and Engagement (PPIE) group at Newcastle University had extensive input in the design and concept of this study before the research was undertaken. Throughout the work, a patient champion (Harpreet Guraya) had input in the project by ensuring that the study was conducted, and the findings were reported, with cultural sensitivity.
Keywords: BAME, ethnic minority, ethnicity, medicine review, medicine services, prescribing safety
1. INTRODUCTION
Disparities within healthcare provision have been widely discussed in recent literature, 1 , 2 , 3 with the coronavirus‐19 pandemic shedding further light on inequalities in access to healthcare across the globe. 4 , 5 , 6 Healthcare inequalities and ethnicity are closely related, and yet, patients from ethnic minority groups have not been involved in health and social care research to the same extent as those from predominantly white groups. 7 Evidence has shown that individuals from minority ethnic backgrounds report poorer general health when compared to their white counterparts. 8 In addition, evidence has also demonstrated that patients from ethnic minority groups are more likely to report a long‐term illness than their white counterparts. 9 Yet, these patients are reportedly less likely to engage in regular medicine reviews and have reported poorer adherence to prescribed medications to manage long‐term illness. 10 , 11
Regular reviews of patient medications, which include high‐quality information at the point of prescribing and considerations around deprescribing inappropriate medicines, are essential to support medicine effectiveness and prescribing safety. 12 , 13 , 14 Medicine review services delivered in primary care settings (like New Medicine Services conducted by community pharmacists or structured medicine reviews performed by general practice pharmacists) are one method that exists within the United Kingdom's National Health Service (NHS). 15 , 16 , 17 The focus of such services centres on improving the clinical effectiveness of medicines being taken, by addressing issues relating to medicine optimization and medicine adherence. 18 , 19 , 20 The economic effectiveness of these interventions has also recently been explored, where Elliott et al. 21 suggested that New Medicine Services would deliver better patient outcomes than normal practice at reduced costs to the health service in the long term. It is important to consider the accessibility of these services for patients to access and use these effectively, in particular, those patients from ethnic minority groups. 22
Variation in healthcare access can be associated with social and cultural determinants creating inequality for ethnic minority patient groups. 23 In previous medical literature across the globe, reduced access to healthcare for ethnic minority populations has been well reported, 8 , 24 , 25 , 26 and groups have been previously referred to as medically underserved across a range of health conditions. 27 , 28 , 29 In recent studies, patients from minority ethnic groups were reported less likely to access and attend medicine‐based services. 30 For example, Eh et al. found that Chinese immigrants who had stronger beliefs in the effectiveness of traditional Chinese medications were less likely to be adherent to prescribed medication 31 ; a systematic review by Alhomoud et al. highlighted the paucity of research that examines medicine‐related needs for ethnic minority patient groups, 32 and Latif et al. reported on the low level of evidence of underrepresented ethnic minority groups engaging in medicine‐related research, 33 as well as the inequitable access to healthcare services, including pharmacies. 29 Gaining knowledge of the barriers and facilitators that impact ethnic minority groups accessing medicine services is required to ensure that services are fit for purpose to meet and support the medicine‐centred needs of all patient populations.
In the United Kingdom, as demonstrated in other countries, the growth of various ethnic communities and linguistic groups, each with their own cultural traits and health profiles, presents a complex challenge to healthcare practitioners and policy makers in terms of achieving equitable access to healthcare. To shed light on the inequalities that impact the accessibility of medicine services, a greater understanding is required about the perceptions of healthcare professionals involved in the delivery of the services. By sharing the views of this cohort of healthcare professionals, this study aims to go beyond the existing patient‐centred research to better learn about ways to improve access for minority groups themselves. Limited studies are available that apply this lens, with even fewer focusing on the challenges of medicine‐specific contexts. 10 , 25 , 34 This study investigates the details surrounding the barriers and facilitators to access for these patient groups and seeks to build on existing evidence to ask the following question: ‘What do healthcare professionals believe are the barriers and facilitators for patients of minority ethnic groups when accessing medicines services?’
2. MATERIALS AND METHODS
2.1. Recruitment and sampling
The consolidated criteria for reporting qualitative research (COREQ) checklist were followed for this study, according to EQUATOR guidelines (see Supporting Information File, Item 1). 35 Immediately before study commencement, COVID‐19 restrictions were enforced across the United Kingdom. This meant that the planned face‐to‐face recruitment and data collection could no longer be undertaken in person. Instead, an amendment to University Ethics meant that participant recruitment could be conducted using remote methods. Purposive sampling was used to recruit participants from a range of healthcare professional groups, who were of mixed in terms of age ranges, ethnic backgrounds, clinical expertise and years of experience. Publicly available data were used to access email addresses, and all participants were invited to participate via an email invitation (which included a study information sheet and consent form). Participants who expressed an interest and provided their informed written consent were enrolled into the study. No prior relationship was established between the researcher and participants before study commencement or recruitment. Participants were also given the opportunity to ask questions before signing the consent form and were informed that they were free to withdraw from the study at any time. Inclusion criteria were as follows: participants working in a UK‐based healthcare professional role and those who perform medicine review services as part of their professional role.
2.2. Semistructured interviews
In depth, semistructured interviews were conducted by one researcher (M. E., a female undergraduate researcher with experience of qualitative research) between October and December 2020. Interviews were conducted with participants over the telephone or by using video call‐based software, such as Zoom® and Microsoft Teams®; all participants were offered the choice of which platform they prefer. The semistructured interview topic guide was developed based on two pilot interviews and covered key issues identified within the current literature focusing on ethnic minority groups (see the Supporting Information File, Item 2). 8 , 24 , 25 , 36 These issues included participants' experiences of performing medicine review services with ethnic minority patient groups and their perceptions of barriers and facilitators that may impact the service. Interviews were conducted until theoretical data saturation was reached, that is, upon author consensus that subsequent interviews yielded no new information. 37 , 38 , 39
2.3. Data analysis
All interviews were audio‐recorded and transcribed verbatim by one researcher (M. E.). All data were anonymized at the point of transcription; participants did not provide comments on the transcripts or feedback on the results. A reflexive thematic analysis approach was performed by two researchers (M. E., a student pharmacist, and A. R., a pharmacist and qualitative researcher). Following reflexive thematic analysis processes, as defined by Braun and Clarke, 39 , 40 each interview was transcribed and analysed before conducting the next. Constant comparison guided an iterative process of data collection and analysis. Data familiarization was achieved through close and detailed reading of the transcripts. Initial descriptive codes were identified in a systematic manner across the data set. The codes were grouped into common coding patterns, which aided the development of analytic themes from the data. Themes were reviewed, refined and named once coherent and distinctive. If agreement was not reached between the two authors performing the data analysis, discussion and consensus were sought from the wider research team (A. H. and A. T., both experienced qualitative researchers and healthcare professionals). Interview field notes (maintained by M. E.) enhanced the reflective process. NVivo (version 12) software facilitated the data management processes throughout. When sharing participant quotes in this study, nonidentifiable pseudonyms have been used to ensure confidentiality, for example, Participant A, Participant B, and so forth.
2.4. Ethical approval
The study received full ethical approval from the Newcastle University Faculty of Medical Sciences Ethics Committee, with an ethical reference number of 5314/2020.
3. RESULTS
Eighteen participants were recruited and interviewed as part of this study (there were no refusals to partake, participant dropouts or repeat interviews). The characteristics of the healthcare professional participants are described in Table 1. The average age of the participants was 38 years (SD: 11.97), and the most common healthcare professional group interviewed was pharmacists (n = 9, 50%). Eleven interviews were conducted over the telephone and seven were performed using the video call‐based software, Zoom®.
Table 1.
Participant characteristics
| Participant | Sex (M/F) | Age range (years) | Interview format | Healthcare professional role | Ethnicity |
|---|---|---|---|---|---|
| 1 | F | 60–69 | Video‐call | Paediatric consultant | Indian |
| 2 | F | 50–59 | Telephone | GP pharmacist | White |
| 3 | F | 30–39 | Telephone | Registrar | Arab |
| 4 | F | 50–59 | Video‐call | Paediatrician | Arab |
| 5 | F | 30–39 | Telephone | GP pharmacist | Indian |
| 6 | F | 30–39 | Telephone | GP | Indian |
| 7 | F | 30–39 | Telephone | Registrar | White |
| 8 | F | 20–29 | Telephone | Hospital pharmacist | Black |
| 9 | F | 30–39 | Telephone | Community pharmacist | Pakistani |
| 10 | F | 40–49 | Video‐call | Hospital pharmacist | White |
| 11 | F | 20–29 | Video‐call | S/S pharmacist | White |
| 12 | M | 40–49 | Video‐call | GP | White |
| 13 | F | 20–29 | Telephone | Community pharmacist | Bengali |
| 14 | F | 20–29 | Telephone | Care home pharmacist | Arab |
| 15 | F | 30–39 | Video‐call | Hospital pharmacist | White |
| 16 | M | 60–69 | Video‐call | Respiratory consultant | Arab |
| 17 | F | 20–29 | Telephone | Dentist | White |
| 18 | M | 30–39 | Telephone | GP | White |
Abbreviations: F, female; GP, general practitioner; GP pharmacist, pharmacist working in a GP surgery; M, male; Registrar, specialist doctor who has received advanced training in a specialist field of medicine; S/S pharmacist, split sector pharmacist (working in hospital and a GP surgery).
Three key themes were developed from the data to highlight the perceived barriers and facilitators that affect access to medicine review services for ethnic minority patients. These themes centred around (1) healthcare professionals bridging the cultural divide; (2) appreciating cultural stigma and acceptance of certain health conditions; and (3) addressing communication and language needs on an individualized basis (as demonstrated in Figure 1). Each of these themes is discussed in turn and participant perspectives and recommendations are shared throughout as anonymized interview quotes.
Figure 1.
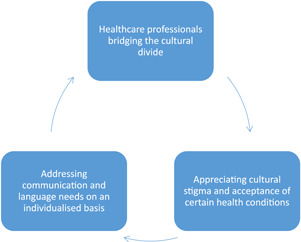
Barriers and facilitators that affect access to medicine services for ethnic minority patients
3.1. Theme 1: Healthcare professionals bridging the cultural divide
Participants discussed how certain cultural expectations and fundamental understanding of what the UK healthcare system provides can pose as barriers to accessing care. One general practitioner (GP) described their understanding as follows: ‘general practice isn't a specialty that exists in every country, so some people don't really know our role’ (Participant 18). They reflected that patient expectations of health services can be better understood when healthcare professionals have appreciation of other cultures. Cultural competency awareness can act as a facilitator to remove this barrier and support patient understanding to get the most out of their healthcare. One participant stated ‘making sure if somebody prefers a female GP, there is a female GP available and just being more culturally aware’ (Participant 12). They also felt that, although healthcare professionals are ‘generally more aware of (differences in cultures) than they were in the past’, they recognized ‘that it is still a barrier for some patients’ (Participant 12).
if they (healthcare professionals) are struggling to understand that person, or if they don't understand their background, then they are not going to cater their treatment towards what's best for them… it would be good to have teaching sessions about different cultures… ethical dilemmas and how different faiths and different ethnicities might deal with these. (Participant 14)
By improving patient familiarity with the NHS and health services, barriers to accessibility and unmanaged expectations can be overcome. One participant discussed the importance of recognizing those patients who ‘are unlikely to be familiar with the NHS’ and providing additional support if ‘they don't know how to access services, and maybe don't know how prescription system works or how to go to the pharmacy’ (Participant 12). Factors such as ‘how long they've been in the UK, whether they were born in the UK and whether they recently arrived in the UK’ were all discussed as barriers that may impact a person's understanding and expectations relative to their health (Participant 12).
One participant also discussed a wider, system‐level approach to overcome accessibility barriers for patients of ethnic minorities. Perceptions were shared about the need to separately view ‘patients who have arrived here within the last two or three years or asylum seekers’ from those who ‘have grown up here or their families have grown up here’, on the basis that the ‘key difference is whether or not you understand how the system works and how to access medicines services’ (Participant 12). By appreciating the immigration history of individual patients, healthcare professionals can work to break the barriers relating to the accessibility of medicine review services and strive for equality. By gaining an understanding of a person's cultural beliefs and expectations, healthcare professionals and policy makers can ensure the design and delivery of medicine review services that are culturally acceptable and adaptable.
if you've only recently arrived then you might be used to a different healthcare system, maybe either a private healthcare system or no healthcare system, depending where you come from. (Participant 12)
3.2. Theme 2: Appreciating cultural stigma and acceptance of certain health conditions
Participants shared their perceptions of barriers to accessing medicine services that exist as a consequence of cultural beliefs of ethnic minority communities, in particular, the diagnosis and treatment of certain physical and mental health conditions. One participant reflected on their prior experience of ‘giving bad news… it's lung cancer’ to minority ethnic patients from the Middle East. This participant felt that ‘people from the Middle East, it's very difficult for them to accept such bad news… to a degree (where) sometimes the families are trying to protect the patient and “say don't tell him the diagnosis”’, which, in turn, affected the patient's engagement with treatment (Participant 16). Another participant, who specialized in paediatric health, discussed similar experiences relating to barriers that exist from the cultural beliefs of accepting a diagnosis and treatment for a child with Autism. This participant described seeing this ‘more in ethnic minorities… they are not acknowledging that problem of their child’ (Participant 4). In particular, the participant discussed the impact that cultural barriers can have around the ‘stigma that accompanies’ a diagnosis, as well as the traditional cultural beliefs that ethnic minority groups may have towards certain health conditions. As a consequence, access to appropriate medicines and care were delayed.
a parent who refused my diagnosis that the child has Autism… the mum requested not to share it with the school and to take the diagnosis off (the child's medical records). I said I can't take the diagnosis off because it has been done, what I can do is not to share the letter with the school it's your right… and if you change your mind, I'm quite happy to see you again. What happened is six months later, because the school refused to give the right support, because he doesn't have the right diagnosis, the mum came and asked for help. So, the challenges are sometimes the cultural beliefs. (Participant 4)
In a similar way, participants reflected on a cultural barrier that has impacted discussions on mental health conditions within ethnic minority communities, when compared to their white counterparts. One participant, who worked as a GP in a highly populated Romanian and South‐East Asian area, described seeing patients from ethnic minorities ‘suppress their symptoms’ of depression and anxiety due to cultural beliefs of shame and embarrassment (Participant 6). This participant went on to explain how these cultural behaviours can later manifest as generic physical pain, which is more difficult to treat and manage.
(patients) often go to see a GP and say ‘I've got aches and pains here, I've got this, I've got that’ like there's always non‐specific symptoms… depression, anxiety—they aren't really recognised, they just say that you need to crack on, it doesn't really exist. What they often do is suppress the symptoms… they're not recognizing it. (Participant 6)
Similar views were shared by participants working in other healthcare specialties, where it was recognized that age and underlying cultural beliefs may play a role in acceptance and support‐seeking when it came to a person's mental health. One participant, with experience of working as a GP for asylum seeker groups, stated that ‘older patients are less likely to come to the GP… I'm thinking particularly around mental health (where) older patients would be less likely to see the GP compared to younger patients… I'm thinking specifically in an older, immigrant population’ (Participant 12). From their experience, this participant stated that patients from ethnic minority groups were ‘less likely to present with a mental health problem but actually, sometimes they come with a physical problem and when you dig down into it, you realise that there's mental health problems underlying it… and there's an under‐diagnosis of dementia and cognitive problems in some minority populations too’ (Participant 12). Another reason given for this was associated with thoughts of ‘other causes for their mental health’ symptoms, often rooted in religious or spiritual beliefs that would not respond to medical treatment (Participant 12).
I'm thinking about a patient from Malawi, where they had um… particular sort of symptoms that they and their family had attributed to witchcraft or just spiritual beliefs… (if) my symptoms are caused by witchcraft then a tablet isn't going to fix that problem… or like, seeing a therapist isn't going to fix that problem. (Participant 12)
3.3. Theme 3: Addressing communication and language needs on an individualized basis
All healthcare professionals who were interviewed remarked on the existing barriers of communication and language when patients from ethnic minority groups access medicine services. Participants discussed the need for inclusive medicine‐specific resources, like leaflets, that could be produced in multiple languages to overcome barriers and better support patient understanding about their medicines. One participant reflected on their experience with language and communication barriers whilst working as a GP for asylum seekers, and reported ‘not being able to access other resources that are available (is) obviously a problem from the NHS… we don't provide resources in a wide range of languages, and we expect that patients will be able to educate themselves about things’ (Participant 12). Another GP discussed steps already being taken in their locality around communicating ‘public health messages amongst the communities, which we do try and do here in [name of city] for different community groups… making sure it's published in lots of different languages’ to bridge communication gaps (Participant 18).
Limitations in communication also meant that some participants felt that they were unable to give the full medication counselling or advice, compared to the amount they would provide to patients who were fluent in English. Participants considered this to negatively impact medicine issues including prescribing safety and poor treatment adherence, if patients were not fully aware of the medicine rationale and importance of medicine‐taking.
If I said to someone you need to take that daily, ‘just one daily’, then that's it. That's different to if I had a conversation with them explaining ‘why you need to take that, if you don't take that then this is the route you are looking at, if you do take it you are looking at a better quality of life’… making the patient understand from your perspective, getting them to see a long‐term picture. If you've got a communication barrier, you can't take them through that (Participant 9)
Another participant acknowledged the importance of wider messages of communication across cultures, where the way in which symptoms are described in one culture may not translate into another community or language.
Sometimes the way that we describe symptoms… we have a particular way, and maybe in the UK or in Europe describing certain some mental health symptoms… (the descriptions) they maybe don't translate into the communities or other languages. You know when we talk about mental health, we use lots of euphemisms and lots of idioms, and they can be mistranslated and maybe people from a different background have a different understanding of how to describe their symptoms… it can get lost (Participant 12)
Other means of translation, including NHS‐based interpreter services, were widely discussed in the interviews. The availability of interpreter services appeared to vary between healthcare settings and locations across the United Kingdom. While some participants praised current services where, ‘if you need an interpreter, they can generally be readily available’ (Participant 14), other participants discussed difficulties in service availability or not meeting the individual needs of patients. One hospital registrar stated that ‘if the language is a very specific dialect… it's very hard to get someone to translate’ (Participant 7). Another participant reflected on the impact that interpreter services can have when facilitating a person‐centred consultation, where ‘all of your conversation should be directed to the patient… but when it goes to a third party that makes the interaction probably not as personable as it would be otherwise’ (Participant 10).
Some participants reflected on strategies that they have used in attempts to bridge the language gap, if interpreters were unavailable. Reliance on ‘a family member who understands English. (I) communicate with them and they can translate for me’ was often discussed (Participant 8). Participants acknowledged the integral role that family members can play within minority ethnic cultures. In their experience of working as a pharmacist conducting medicine reviews, one participant discussed benefits for patients of ‘South Asian background or Arab background… (they are) more likely to have more input from their children and so, sometimes, actually it makes it a lot easier to do things like medicines reconciliations because you know there's someone there who is looking after them and so you can go through (the medicines) with them’ (Participant 14). However, in certain instances, participants believed translation by family members to be inappropriate, for instance, ‘if it's a medicine for an intimate or sensitive subject, they may not be too keen to discuss that with a family member’ (Participant 2).
Clear communication about medicines was recognized as a significant barrier by participants; however, facilitators to overcome this were also considered. One participant described the use of digital translator devices in their community pharmacy‐based consultations, where ‘Google translate’ was previously used ‘so that I know, whatever I'm saying, they're understanding it properly’ if they or other staff members did not speak the same language as the patient (Participant 13). A hospital pharmacist stated that they ‘found this pharmacy website that created a label in the language that the patient speaks’ as a specific way to support ethnic minority patients being discharged from hospital (Participant 8). This participant also discussed the development of ‘NHS approved’ digital translator technologies that could offer practitioners the same degree of flexibility and ease when discussing and reviewing a patient's medicines, while being more reputable than other digital alternatives (Participant 8).
Accounting for additional time pressures in appointments for patients with translation requirements was a recognized facilitator to manage communication and language barriers. Participants raised concerns that adequate time was often not allocated to adequately address patient needs. One GP spoke about strategies implemented within their surgery to facilitate appointments for ethnic minority patients with translator requirements, thus supporting meaningful medicine‐specific discussions.
We try to book a double appointment if we had an interpreter… if they've got limited English, it's difficult for them to access services, so when they do, then they often have lots of problems that they want to discuss… I would want to know that I've got enough time to deal with the issues properly. (Participant 12).
4. DISCUSSION
This study builds on the limited evidence base that focuses on healthcare professional perspectives when delivering medicine reviews for patients from ethnic minority groups. By collecting the perspectives of healthcare professionals who are involved in the delivery of medicine reviews, this study sheds light on the existing barriers and enablers that affect service accessibility in a bid to improve the quality and delivery of culturally competent, person‐centred care across all patient populations.
A consistent finding across interviews was that participants identified differences in cultural backgrounds between healthcare professionals and patients to be a key contributor to inequalities when accessing healthcare and medicine‐specific services. A lack of cultural understanding and cultural competence by healthcare professionals can have severe implications for patient care. This is echoed by previous work 24 , 41 that instils the importance of recognizing that individuals have diverse identities. To achieve culturally competent care, the cultures of care recipients and healthcare providers are of significance. 25 Involving the patient and the healthcare professional in coproduction approaches may be a useful strategy to overcome this barrier and develop and refine a targeted intervention to support access to medicine services for minority ethnic patients. It is apparent that, to be of the best use for patients and professionals, any such intervention should be designed with a holistic, culturally sensitive and culturally competent approach. 10
Results from this study echo previous studies in demonstrating that certain health conditions, in particular mental health issues, still carry a stigma within ethnic minority communities that causes barriers to seeking medical help and adhering to medication‐based treatment. 42 , 43 The EMPIRIC study by Weich et al. demonstrated that particular ethnic groups (middle‐aged Irish and Pakistani men, and older Indian and Pakistani women) had significantly higher rates of mental health disorders than their white counterparts. 44 The 2007 adult psychiatric morbidity survey also found that individuals from nonwhite ethnicities were less likely to consult healthcare professionals about their mental health and thus less likely to be prescribed medications like antidepressants to manage their symptoms. 45 Ethnic minority patients were also more likely to be diagnosed with severe mental illness and, therefore, receive higher doses of medication. 46 Factors such as cultural, religious or spiritual beliefs should be considered and better integrated into clinical assessments. 47 For instance, developing a greater awareness of potential cultural barriers that may arise with patients from ethnic minority groups should be a priority. 48 , 49 , 50 , 51 , 52 , 53 Thus, healthcare professionals may be better equipped with strategies to overcome them to facilitate better and equal access to appropriate medicine review and supportive care. 48 , 54 , 55 , 56 , 57
Communication is an important prerequisite for successful healthcare access and outcomes. 58 Due to the presence of a language barrier, studies have reported that ethnic minority patients with limited English demonstrate lower rates of medication adherence, make fewer visits to healthcare professionals, have reduced understanding of their conditions and treatment and develop increased medical complications. 11 , 59 Language barriers mean that patients may lack the ability to express themselves and may feel embarrassed to seek medical advice, further hindering the ability to communicate and build a rapport between the healthcare professional and the patient. 60 , 61 The use of an independent translator could circumvent the language barrier issue. 62 The study by Karliner et al. found that professional interpreters were associated with improved quality of care and reduced differentials in access to care. 63 Participants in this study also cited the importance of translators as a facilitator for minority patient access; however, they also cited the challenges associated with accessing interpreters in a timely manner to support consultations. The lack of availability of interpreters in pharmacy‐based settings has been a recognized source of patient safety concern in the wider literature, 64 , 65 with Chauhan et al. reporting low English‐language proficiency as a contributor to increased risk of patient safety events for ethnic minority populations. 59 In the absence of interpreters, participants of this study discussed reliance on other methods to communicate, such as Google® translate. In other studies, such situations were associated with limited quality‐of‐care communications and a lack of information transfer, including medication changes and counselling. 66 , 67 By encountering a language barrier where an interpreter may also not be available, healthcare professionals could find themselves providing the patient with limited information regarding their medication in the scope that the patient can understand. As a result, this may lead to reduced condition comprehension, medicine adherence and a poorer long‐term prognosis. 68 , 69 The opportunity to use written multilingual prescription labels has been researched in the recent literature 70 ; however, considerations should be made for those patients who communicate in non‐English languages verbally, rather than in written format.
Eighteen participants were purposively sampled and interviewed in this study to include a range of experiences across different roles and settings, who routinely engage in the provision of medicine services. However, we acknowledge that there are some limitations in this study. The addition of other healthcare professional groups (such as nurses) may have provided additional insight. Many participants themselves were from minority ethnic backgrounds, and thus were able to provide in‐depth, first‐hand insight with cultural appreciation. There was no representation from East Asian participants, which may have conveyed alternative perspectives in the data. The intended method of in‐person data collection was impacted by the COVID‐19 pandemic. Although video call‐based software can replicate face‐to‐face interviews in the ability to respond to verbal and nonverbal cues, 71 , 72 there are some disadvantages to note with this interview technique. 73 User familiarity and comfort of use may have resulted in the higher number of telephone‐based interviews with participants. 74 This study includes the perspectives of healthcare professionals involved in the delivery of medicine services to patients from ethnic minority groups. What remains to be better examined is the perceptions of patients themselves, to understand their lived experiences of accessing medicine services. Future studies should seek to utilize coproduction approaches that involve patients from underrepresented ethnic minority groups alongside healthcare professionals. 75 Latif et al. described coproduction approaches as a reflective opportunity for community pharmacy professionals to review services offered to medically underserved groups, including those from ethnic minority backgrounds. 33 Previous studies have also implemented coproduction approaches to tailor health services to the needs and preferences of service users. 76 , 77 , 78 Done in partnership with patient representatives from the communities being researched, coproduction can better extend the understanding of the lived experiences of ethnic minority groups in terms of accessibility. As a result, further investigation may enable the recognition and resolution of barriers and facilitators that would enable improved accessibility and inclusivity for ethnic minority communities.
5. CONCLUSION
Acknowledging the barriers and facilitators to ethnic minority groups is an important step towards ensuring equality in access to medicine services. Before this study, limited data existed that explored the perspectives of healthcare professionals involved in delivering medicine review services, particularly in relation to barriers and facilitators affecting ethnic minority patient access. This study seeks to address this gap and provides much‐needed evidence implicating the delivery of person‐centred care and considering changes based on a systems‐level and an individualized person level. Coproduction approaches should be adopted to support better understanding of ethnic minority cultures and thus inform the design and delivery of culturally sensitive, medicine review services. Findings from this qualitative study should be used alongside patient‐informed research to work to achieve equal access to medicine services for all.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Supporting information
Supporting information.
ACKNOWLEDGEMENTS
The authors wish to acknowledge and thank the participants who were interviewed as part of this study, without whom, this study would not have been possible. We would also like to thank Harpreet Guraya, Laura Sile and Thorrun Govind for their support in proof‐reading the manuscript and ensuring that the study was conducted (and the findings were reported) with cultural sensitivity. This study was supported by the National Institute of Health Research (NIHR) Applied Research Collaboration (ARC) for the North East and North Cumbria (NENC). This study did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors. This study was supported by the National Institute of Health Research (NIHR) Applied Research Collaboration (ARC) for the North East and North Cumbria (NENC). The National Institute for Health Research (NIHR) is the nation's largest funder of health and care research and provides the people, facilities and technology that enable research to thrive.
Robinson A, Elarbi M, Todd A, Husband A. A qualitative exploration of the barriers and facilitators affecting ethnic minority patient groups when accessing medicine review services: perspectives of healthcare professionals. Health Expect. 2022;25:628‐638. 10.1111/hex.13410
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Aspinall PJ & Jacobsen B. Ethnic disparities in health and health care: a focused review of the evidence and selected examples of good practice: executive summary. 2004. https://kar.kent.ac.uk/id/eprint/7769
- 2. Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. J Gen Intern Med. 2002;17(6):477‐486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666‐668. [PMC free article] [PubMed] [Google Scholar]
- 4. Razai MS, Kankam HK, Majeed A, Esmail A, Williams DR. Mitigating ethnic disparities in covid‐19 and beyond. BMJ. 2021;372:m4921. [DOI] [PubMed] [Google Scholar]
- 5. Lassale C, Gaye B, Hamer M, Gale CR, Batty GD. Ethnic disparities in hospitalisation for COVID‐19 in England: The role of socioeconomic factors, mental health, and inflammatory and pro‐inflammatory factors in a community‐based cohort study. Brain Behav Immun. 2020;88:44‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan D, Sze S, Minhas JS, et al. The impact of ethnicity on clinical outcomes in COVID‐19: a systematic review. EClinicalMedicine. 2020;23:100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smart A, Harrison E. The under‐representation of minority ethnic groups in UK medical research. Ethn Health. 2017;22(1):65‐82. [DOI] [PubMed] [Google Scholar]
- 8. Nazroo JY, Falaschetti E, Pierce M, Primatesta P. Ethnic inequalities in access to and outcomes of healthcare: analysis of the Health Survey for England. J Epidemiol Community Health. 2009;63(12):1022‐1027. [DOI] [PubMed] [Google Scholar]
- 9. Evandrou M, Falkingham J, Feng Z, Vlachantoni A. Ethnic inequalities in limiting health and self‐reported health in later life revisited. J Epidemiol Community Health. 2016;70(7):653‐662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gault I, Pelle J, Chambers M. Co‐production for service improvement: developing a training programme for mental health professionals to enhance medication adherence in Black, Asian and Minority Ethnic Service Users. Health Expect. 2019;22(4):813‐823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van Rosse F, Suurmond J, Wagner C, de Bruijne M, Essink‐Bot M‐L. Role of relatives of ethnic minority patients in patient safety in hospital care: a qualitative study. BMJ Open. 2016;6(4):e009052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Institute for Health and Care Excellence (NICE). Clinical Guideline (CG76) . Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. 2009. https://www.nice.org.uk/guidance/cg76 [PubMed]
- 13. Clyne B, Bradley MC, Smith SM, et al. Effectiveness of medicines review with web‐based pharmaceutical treatment algorithms in reducing potentially inappropriate prescribing in older people in primary care: a cluster randomized trial (OPTI‐SCRIPT study protocol). Trials. 2013;14(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jain S, Upadhyaya P, Goyal J, et al. A systematic review of prescription pattern monitoring studies and their effectiveness in promoting rational use of medicines. Perspect Clin Res. 2015;6(2):86‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nazar H, Nazar Z, Portlock J, Todd A, Slight SP. A systematic review of the role of community pharmacies in improving the transition from secondary to primary care. Br J Clin Pharmacol. 2015;80(5):936‐948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lenander C, Elfsson B, Danielsson B, Midlöv P, Hasselström J. Effects of a pharmacist‐led structured medication review in primary care on drug‐related problems and hospital admission rates: a randomized controlled trial. Scand J Prim Health Care. 2014;32(4):180‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khera S, Abbasi M, Dabravolskaj J, Sadowski CA, Yua H, Chevalier B. Appropriateness of medications in older adults living with frailty: impact of a pharmacist‐led structured medication review process in primary care. J Prim Care Community Health. 2019;10:2150132719890227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Threapleton C, Kimpton JE, Carey IM, et al. Development of a structured clinical pharmacology review for specialist support for management of complex polypharmacy in primary care. Br J Clin Pharmacol. 2020;86(7):1326‐1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wright DJ, Maskrey V, Blyth A, et al. Systematic review and narrative synthesis of pharmacist provided medicines optimisation services in care homes for older people to inform the development of a generic training or accreditation process. Int J Pharm Pract. 2020;28(3):207‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Odeh M, Scullin C, Hogg A, Fleming G, Scott MG, McElnay JC. A novel approach to medicines optimisation post‐discharge from hospital: pharmacist‐led medicines optimisation clinic. Int J Clin Pharm. 2020;42(4):1036‐1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Elliott RA, Boyd MJ, Tanajewski L, et al. ‘New Medicine Service': supporting adherence in people starting a new medication for a long‐term condition: 26‐week follow‐up of a pragmatic randomised controlled trial. BMJ Qual Saf. 2020;29(4):286‐295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Thomson K, Hillier‐Brown F, Walton N, Bilaj M, Bambra C, Todd A. The effects of community pharmacy‐delivered public health interventions on population health and health inequalities: a review of reviews. Prev Med. 2019;124:98‐109. [DOI] [PubMed] [Google Scholar]
- 23. Barnard H, Turner C. Poverty and Ethnicity: A Review of Evidence. Joseph Rowntree Foundation; 2011. [Google Scholar]
- 24. Szczepura A. Access to health care for ethnic minority populations. Postgrad Med J. 2005;81(953):141‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. van Eechoud IJ, Grypdonck M, Beeckman D, Van Lancker A, Van Hecke A, Verhaeghe S. Oncology health workers' views and experiences on caring for ethnic minority patients: a mixed method systematic review. Int J Nurs Stud. 2016;53:379‐398. [DOI] [PubMed] [Google Scholar]
- 26. Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national patient survey. BMC Fam Pract. 2010;11(1):1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McFadden A, Siebelt L, Gavine A, et al. Gypsy, Roma and Traveller access to and engagement with health services: a systematic review. Eur J Public Health. 2018;28(1):74‐81. [DOI] [PubMed] [Google Scholar]
- 28. Marmot M. The health gap: the challenge of an unequal world. Lancet. 2015;386(10011):2442‐2444. [DOI] [PubMed] [Google Scholar]
- 29. Latif A, Mandane B, Ali A, Ghumra S, Gulzar N. A qualitative exploration to understand access to pharmacy medication reviews: views from marginalized patient groups. Pharmacy. 2020;8(2):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bancroft S, Attar‐Zadeh D, Heading C, Shah U. BAME patients less likely to take up community pharmacy services in North West London. Pharm J. 2020;304:7938. [Google Scholar]
- 31. Eh K, McGill M, Wong J, Krass I. Cultural issues and other factors that affect self‐management of Type 2 Diabetes Mellitus (T2D) by Chinese immigrants in Australia. Diabetes Res Clin Pract. 2016;119:97‐105. [DOI] [PubMed] [Google Scholar]
- 32. Alhomoud F, Dhillon S, Aslanpour Z, Smith F. Medicine use and medicine‐related problems experienced by ethnic minority patients in the United Kingdom: a review. Int J Pharm Pract. 2013;21(5):277‐287. [DOI] [PubMed] [Google Scholar]
- 33. Latif A, Tariq S, Abbasi N, Mandane B. Giving voice to the medically under‐served: a qualitative co‐production approach to explore patient medicine experiences and improve services to marginalized communities. Pharmacy (Basel). 2018;6(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Elkan R, Avis M, Cox K, et al. The reported views and experiences of cancer service users from minority ethnic groups: a critical review of the literature. Eur J Cancer Care (Engl). 2007;16(2):109‐121. [DOI] [PubMed] [Google Scholar]
- 35. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349‐357. [DOI] [PubMed] [Google Scholar]
- 36. Priebe S, Sandhu S, Dias S, et al. Good practice in health care for migrants: views and experiences of care professionals in 16 European countries. BMC Public Health. 2011;11(1):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Urquhart C. Grounded Theory for Qualitative Research: A Practical Guide. Sage; 2012. [Google Scholar]
- 38. Birks M, Mills J. Grounded Theory: A Practical Guide. Sage; 2015. [Google Scholar]
- 39. Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 2019;11(4):589‐597. [Google Scholar]
- 40. Braun V, Clarke V. What can “thematic analysis” offer health and wellbeing researchers? Int J Qual Stud Health Well‐Being. 2014;9:26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Vydelingum V. Nurses' experiences of caring for South Asian minority ethnic patients in a general hospital in England. Nurs Inq. 2006;13(1):23‐32. [DOI] [PubMed] [Google Scholar]
- 42. Linney C, Ye S, Redwood S, et al. “Crazy person is crazy person. It doesn't differentiate”: an exploration into Somali views of mental health and access to healthcare in an established UK Somali community. Int J Equity Health. 2020;19(1):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bhui K, Halvorsrud K, Nazroo J. Making a difference: ethnic inequality and severe mental illness. Br J Psychiatry. 2018;213(4):574‐578. [DOI] [PubMed] [Google Scholar]
- 44. Weich S, Nazroo J, Sproston K, et al. Common mental disorders and ethnicity in England: the EMPIRIC study. Psychol Med. 2004;34(8):1543‐1551. [DOI] [PubMed] [Google Scholar]
- 45. Cooper C, Bebbington P, McManus S, et al. The treatment of Common Mental Disorders across age groups: results from the 2007 Adult Psychiatric Morbidity Survey. J Affect Disord. 2010;127(1‐3):96‐101. [DOI] [PubMed] [Google Scholar]
- 46. Bansal N, Bhopal R, Netto G, Lyons D, Steiner MF, Sashidharan SP. Disparate patterns of hospitalisation reflect unmet needs and persistent ethnic inequalities in mental health care: the Scottish health and ethnicity linkage study. Ethn Health. 2014;19(2):217‐239. [DOI] [PubMed] [Google Scholar]
- 47. Dein S, Bhui KS. At the crossroads of anthropology and epidemiology: current research in cultural psychiatry in the UK. Transcult Psychiatry. 2013;50(6):769‐791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Levkovich I, Rodin D, Shinan‐Altman S, Alperin M, Stein H. Perceptions among diabetic patients in the ultra‐orthodox Jewish community regarding medication adherence: a qualitative study. BMC Public Health. 2021;21(1):1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Duke N, Wigley W. Literature review: the self‐management of diet, exercise and medicine adherence of people with type 2 diabetes is influenced by their spiritual beliefs. J Diabetes Nurs. 2016;20(5):184‐190. [Google Scholar]
- 50. Shahin W, Kennedy GA, Stupans I. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Prefer Adherence. 2019;13:1019‐1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Penn C, Watermeyer J, Evans M. Why don't patients take their drugs? The role of communication, context and culture in patient adherence and the work of the pharmacist in HIV/AIDS. Patient Educ Couns. 2011;83(3):310‐318. [DOI] [PubMed] [Google Scholar]
- 52. Curtis E, Jones R, Tipene‐Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health. 2019;18(1):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Latif A, Waring J, Chen LC, et al. Supporting the provision of pharmacy medication reviews to marginalised (medically underserved) groups: a before/after questionnaire study investigating the impact of a patient–professional co‐produced digital educational intervention. BMJ Open. 2019;9(9):e031548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Peeters B, Van Tongelen I, Duran Z, et al. Understanding medication adherence among patients of Turkish descent with type 2 diabetes: a qualitative study. Ethn Health. 2015;20(1):87‐105. [DOI] [PubMed] [Google Scholar]
- 55. Daher M, Chaar B, Saini B. Impact of patients' religious and spiritual beliefs in pharmacy: from the perspective of the pharmacist. Res Social Adm Pharm. 2015;11(1):e31‐e41. [DOI] [PubMed] [Google Scholar]
- 56. Ahmed S, Lee S, Shommu N, Rumana N, Turin T. Experiences of communication barriers between physicians and immigrant patients: a systematic review and thematic synthesis. Patient Exp J. 2017;4(1):122‐140. [Google Scholar]
- 57. Shahin W, Kennedy GA, Cockshaw W, Stupans I. The role of medication beliefs on medication adherence in Middle Eastern refugees and migrants diagnosed with hypertension in Australia. Patient Prefer Adherence. 2020;14:2163‐2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hadziabdic E, Heikkilä K, Albin B, Hjelm K. Problems and consequences in the use of professional interpreters: qualitative analysis of incidents from primary healthcare. Nurs Inq. 2011;18(3):253‐261. [DOI] [PubMed] [Google Scholar]
- 59. Chauhan A, Walton M, Manias E, et al. The safety of health care for ethnic minority patients: a systematic review. Int J Equity Health. 2020;19(1):1‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Maura J, de Mamani AW. Mental health disparities, treatment engagement, and attrition among racial/ethnic minorities with severe mental illness: a review. J Clin Psychol Med Settings. 2017;24(3):187‐210. [DOI] [PubMed] [Google Scholar]
- 61. Richardson A, Thomas VN, Richardson A. “Reduced to nods and smiles”: experiences of professionals caring for people with cancer from black and ethnic minority groups. Eur J Oncol Nurs. 2006;10(2):93‐101. discussion 102‐105. [DOI] [PubMed] [Google Scholar]
- 62. Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255‐299. [DOI] [PubMed] [Google Scholar]
- 63. Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727‐754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Westberg SM, Sorensen TD. Pharmacy‐related health disparities experienced by non–English‐speaking patients: impact of pharmaceutical care. J Am Pharm Assoc. 2005;45(1):48‐54. [DOI] [PubMed] [Google Scholar]
- 65. Schwappach DL, Massetti CM, Gehring K. Communication barriers in counselling foreign‐language patients in public pharmacies: threats to patient safety? Int J Clin Pharm. 2012;34(5):765‐772. [DOI] [PubMed] [Google Scholar]
- 66. Kaufert JM, Putsch RW. Communication through interpreters in healthcare: ethical dilemmas arising from differences in class, culture, language, and power. J Clin Ethics. 1997;8:71‐87. [PubMed] [Google Scholar]
- 67. Hadziabdic E, Hjelm K. Arabic‐speaking migrants' experiences of the use of interpreters in healthcare: a qualitative explorative study. Int J Equity Health. 2014;13(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Crane JA. Patient comprehension of doctor‐patient communication on discharge from the emergency department. J Emerg Med. 1997;15(1):1‐7. [DOI] [PubMed] [Google Scholar]
- 69. Jaeger FN, Pellaud N, Laville B, Klauser P. Barriers to and solutions for addressing insufficient professional interpreter use in primary healthcare. BMC Health Serv Res. 2019;19(1):753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Zargarzadeh AH, Law AV. Access to multilingual prescription labels and verbal translation services in California. Res Social Adm Pharm. 2011;7(4):338‐346. [DOI] [PubMed] [Google Scholar]
- 71. Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using Zoom videoconferencing for qualitative data collection: perceptions and experiences of researchers and participants. Int J Qual Methods. 2019;18:1609406919874596. [Google Scholar]
- 72. Lobe B, Morgan D, Hoffman KA. Qualitative data collection in an era of social distancing. Int J Qual Methods. 2020;19:1609406920937875. [Google Scholar]
- 73. Upadhyay UD, Lipkovich H. Using online technologies to improve diversity and inclusion in cognitive interviews with young people. BMC Med Res Methodol. 2020;20(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid‐19. BMJ. 2020;368:m998. [DOI] [PubMed] [Google Scholar]
- 75. Redman S, Greenhalgh T, Adedokun L, Staniszewska S, Denegri S, Co‐production of Knowledge Collection Steering Committee . Co‐production of knowledge: the future. BMJ. 2021;372:n434. https://www.bmj.com/content/372/bmj.n434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ. 2015;350:g7714. [DOI] [PubMed] [Google Scholar]
- 77. Robert G, Donetto S, Williams O. Co‐designing healthcare services with patients. In: Loeffler E, Bovaird T, eds. The Palgrave Handbook of Co‐Production of Public Services and Outcomes. Springer International Publishing; 2021:313‐333. [Google Scholar]
- 78. Palmer VJ, Weavell W, Callander R, et al. The Participatory Zeitgeist: an explanatory theoretical model of change in an era of coproduction and codesign in healthcare improvement. Med Humanit. 2019;45(3):247‐257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


