Abstract
Background
There is still no consensus regarding the role of laparoscopy in trauma cases. The purpose of this paper is to assess the value of diagnostic and therapeutic laparoscopy for patients with blunt or penetrating abdominal trauma by performing a systematic review and meta-analysis.
Methods
PubMed, Embase, and the Cochrane library were systemically searched for the randomized controlled trials (RCTs) and non-RCT comparative studies on effectiveness and safety of laparoscopy vs. laparotomy for the two authors independently performed the search, data extraction, and quality assessment.
Results
A total of 5,517 patients were enrolled in 23 eligible studies that were published in English. Meta-analysis results suggest that there is no significant difference in the incidence of missed injury and mortality between abdominal trauma patients receiving laparoscopy and those receiving laparotomy. Concerning postoperative complications, compared with patients in the open surgery group, those in the laparoscopy group are at a similar risk of intra-abdominal abscesses, thromboembolism, and ileus, while there is a decreased incidence of wound infection and pneumonia. Besides, patients in the laparoscopy group experience shorter hospitalization times and procedure times. For most outcomes, the sensitivity analysis yielded similar results to the primary analysis.
Conclusion
Laparoscopic surgery is a practical alternative to laparotomy for appropriate patients. The decision to perform laparoscopy should be based on the experience of the surgeon and the resources available.
Keywords: abdominal trauma, laparoscopy, laparotomy, systematic review, meta-analysis
Introduction
Trauma is the fourth leading cause of death in the overall population, while it is the main cause of death during the first half of the human life span (1). Besides, 9~14.9% of all trauma cases involve the abdomen (2). Abdominal trauma is one of the preventable causes of death in polytrauma patients (3), and laparotomy has traditionally been considered as the standard treatment (4). However, since laparotomy is associated with morbidity ranging from 20 to 40% (5–7), it may be preferable to avoid unnecessary laparotomies. In haemodynamically stable conditions and conducted by experienced surgeons, laparoscopy is an effective and safe in the management of abdominal trauma patients (8). Advances of imaging technology and selective non-operative management have led to a decrease in non-therapeutic laparotomy for haemodynamically stable patients (9–11). Studies have also shown that since the introduction of the laparoscopy procedure, the rate of non-therapeutic laparotomy has further decreased (7, 12). Moreover, as a diagnostic or therapeutic tool, laparoscopy involves less pain and results in a shorter hospital stays and faster recovery times than laparotomy. Although the feasibility and benefits of diagnostic and therapeutic laparoscopy in selected haemodynamically stable trauma patients have already been demonstrated, a widely accepted consensus has not yet been reached (8, 13). Soon after the laparoscopy procedure was introduced, several systematic reviews (14–16) summarizing its value for penetrating or blunt abdominal trauma were published. Subsequently, a series of papers (7, 8, 12, 17–21) were published addressing a wide range of possibilities for the application of laparoscopy in abdominal trauma. In this review, we integrated newly published studies with previous evidence to comprehensively compare the effectiveness and safety of laparoscopy with laparotomy on penetrating or blunt abdominal trauma.
Methods
This study was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement (22).
Search Strategy
We searched PubMed, Embase, and the Cochrane Library for comparative studies on the effectiveness and safety of laparoscopy vs. laparotomy for the management of abdominal trauma up to 30th June 31, 2021. The Medical Subject Headings (MeSH) including “laparoscopy,” “abdominal injuries,” as well as free text words like “laparoscop*,” “minimal* invasive,” “abdom*,” “injur*,” “wound*,” “stab*,” “shot*,” “shoot*,” “lacerat*,” “trauma*,” “penetrat*,” and “blunt*,” in combination with the Boolean operators “AND” and “OR.” Besides, we also searched the references listed in all the articles that were initially selected. The Appendix in the Supplementary Materials gives details of the search strategies.
Study Selection and Data Abstraction
Comparative studies that were published in English, and focused on the comparison of laparoscopy and laparotomy for the management of abdominal trauma were included. We excluded studies where the full text was not available, those that focused on children (age <18 years), and ones that did not select laparotomy as a comparator, or did not report on outcomes predefined in his review. The selection process of the relevant literature was conducted independently by two researchers (JW and LC), and any disagreements were resolved through discussion or by consulting a third author (SZ). Primary outcomes included missed injury, mortality, and postoperative complications such as wound infection, abscess formation, bowel obstruction or ileus, pneumonia, and thromboembolism. Additionally, the secondary outcomes encompassed procedure time, length of hospital stay, and re-operation. Two researchers (JW and LC) independently extracted the following information: (1) features of studies including the first author, published year, country, study design, study period, intervention, sample size, and rate of conversion to open surgery; (2) characteristics of patients including age, gender, injury severity score, abbreviated injury scale/ abdominal trauma index, and percentage of haemodynamic stable patients; (3) outcomes.
Quality Assessment of the Eligible Studies
The bias risk of the eligible RCTs was assessed using Cochrane Collaboration's tool (23) for assessing the risk of bias in randomized trials, which includes the following seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. Each of the seven domains could be rated as having potentially high, unclear, or low risk of bias (24). The Newcastle-Ottawa Scale (NOS) was also applied to assess the quality of cohort studies. Three dimensions contributed to the overall quality score, including selection assessment of the exposed and unexposed cohort, comparability of the two cohorts, and outcome assessment. We graded the quality of cohort studies as high (≥8 stars), moderate (4–7 stars), or low (<4 stars), with a third person (SZ) resolving any disagreements.
Statistical Analysis
Where possible, data analysis was based on the intention-to-treat principle for each study that was included, and we performed meta-analyses using Review Manager version 5.3.5 (Cochrane Collaboration) (25). We assessed the heterogeneity between studies using Cochran's Q test and the I2 statistics. Results were interpreted as either low (I2 = 0–40%), moderate (I2 = 30–60%), substantial (I2 = 50–90%) or high heterogeneity (I2 = 75–100%) (23, 26). We also calculated risk difference (RD) with a 95% confidence interval (CI) for the dichotomous outcomes, and the mean differences (MD) with 95% CI for continuous data. Subgroup analyses were performed according to the study design (prospective vs. retrospective), injury mechanism (penetrating vs. blunt abdominal trauma), and the purpose of laparoscopy use (diagnosis vs. treatment) for primary outcomes. A random effects model was applied in the primary analysis, whereas fixed effects models were used for sensitivity analysis. Furthermore, a sensitivity analysis was performed by removing the studies one by one. Additionally, meta-analyses were performed on only the high-quality studies. A qualitative description was performed for studies that were not suitable for quantitative data synthesis, and potential publication bias was assessed using funnel plots. P < 0.05 were considered statistically significant.
Results
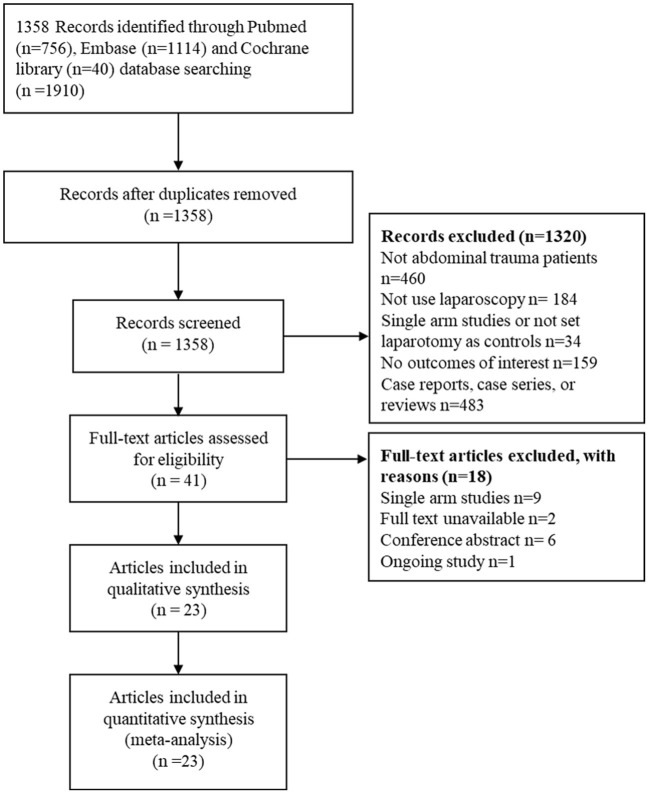
The literature search initially identified 1, 358 papers, of which 41 studies were eligible for the full-text screening process, and 23 studies (7, 8, 12, 17–21, 27–41) were included in the meta-analysis. The PRISMA flow diagram is illustrated in Figure 1.
Figure 1.
The PRISMA flow diagram for literature screening.
The 23 studies encompassed one RCT (30), two prospective observational studies (29, 35) and 20 retrospective observational studies (7, 8, 12, 17–21, 27, 28, 31–34, 36–41). Four (33, 34, 37, 41) of the 20 retrospective observational studies were based on controlled before and after study designs, while the remainder were comparative/parallel studies. Nine (7, 8, 12, 18, 19, 21, 36, 39, 40) of the 23 studies were focussed on therapeutic laparoscopy or reported separately on diagnostic laparoscopy. A total of 5,517 individual patients were involved in the study, with 2,594 patients enrolling in the laparoscopy group, and 2,923 patients in the laparotomy group. All but one study (17) reported the conversion rate from laparoscopy to laparotomy, with an average value of 25.0% (range from 0 to 45.1%). The patient age varied from 26 to 57 years, with a 76.9% male population. Besides, the age did not differ significantly between the two intervention groups. Seventeen studies (7, 8, 12, 18, 19, 21, 27, 30–32, 34, 36–41) reported the severity of the condition evaluated by the injury severity score, new injury severity score, or abbreviated injury scale/abdominal trauma index, while the six other studies (17, 20, 28, 29, 33, 35) did not specify the severity scores at all. Additionally, in two studies, there was a significant difference in disease severity between the laparoscopy and laparotomy groups (12, 32). Almost all reports involved only haemodynamically stable patients, except for two studies (33, 39), which included a certain percentage of haemodynamically unstable patients. The basic characteristics of the studies and the patients involved in the meta-analysis are presented in Tables 1, 2.
Table 1.
Characteristics of the included studies.
| References | Region | Study type | Study period | Intervention | Sample size | Conversion to open, n (%) |
|---|---|---|---|---|---|---|
| Shams and Elyasi (17) | Iran | Retrospective observational study | 1 year | Laparoscopy | 18 | NR |
| Laparotomy | 22 | |||||
| Birindelli et al. (19) | Italy | Retrospective observational study | Jan 2013 to Dec 2017 | Laparoscopy | 16 | 3 (19.0%) |
| Laparotomy | 32 | |||||
| Obaid et al. (18) | USA | Retrospective observational study | Jan 2017 to Dec 2017 | Laparoscopy | 177 | 13 (7.3%) |
| Laparotomy | 354 | |||||
| Gao et al. (8) | China | Retrospective observational study | Jan 2013 to Dec 2017 | Laparoscopy | 54 | 4 (7.4%) |
| Laparotomy | 54 | |||||
| Lin et al. (12) | Taiwan | Retrospective observational study | Jan 2006 to Dec 2015 | Laparoscopy | 126 | 9 (7.1%) |
| Laparotomy | 139 | |||||
| Chakravartty et al. (7) | UK | Retrospective observational study | Jan 2004 to Jan 2014 | Laparoscopy | 25 | 1 (4.0%) |
| Laparotomy | 25 | |||||
| Trejo-Ávila et al. (20) | Mexico | Retrospective observational study | Jan 2013 to May 2016 | Laparoscopy | 19 | 1 (5.3%) |
| Laparotomy | 19 | |||||
| Huang et al. (21) | USA | Retrospective observational study | Jan 2011 to Dec 2014 | Laparoscopy | 11 | 0 (0%) |
| Laparotomy | 41 | |||||
| Lim et al. (40) | South Korea | Retrospective observational study | Jan 2006 to Aug 2012 | Laparoscopy | 41 | 9 (18%) |
| Laparotomy | 55 | |||||
| Chestovich et al. (39) | USA | Retrospective observational study | Jan 2008 to Dec 2013 | Laparoscopy | 94 | 15 (16.0%) |
| Laparotomy | 96 | |||||
| Liao et al. (38) | Taiwan | Retrospective observational study | Jan 2010 to Jan 2013 | Laparoscopy | 15 | 1 (6.7%) |
| Laparotomy | 20 | |||||
| Lee et al. (37) | Taiwan | Retrospective observational study | Jun 2003 to Jun 2006; Jul 2007 to Jun 2010 | Laparoscopy | 57 | 2 (3.5%) |
| Laparotomy | 47 | |||||
| Karateke et al. (35) | Turkey | Prospective non-randomized study | Jun 2010 to Jul 2011 | Laparoscopy | 26 | 9 (34.6%) |
| Laparotomy | 26 | |||||
| Khubutiya et al. (36) | Russia | Retrospective observational study | 2000 to 2011 | Laparoscopy | 328 | 130 (37.3%) |
| Laparotomy | 280 | |||||
| Lin et al. (34) | Taiwan | Retrospective observational study | Jan 1998 to Jan 2003; Jan 2003 to Dec 2007 | Laparoscopy | 48 | 1 (2.1%) |
| Laparotomy | 38 | |||||
| Cherkasov et al. (33) | Russia | Retrospective observational study | 1997 to 2003 | Laparoscopy | 1332 | 356 (26.7%) |
| Laparotomy | 1363 | |||||
| Cherry et al. (32) | USA | Retrospective observational study | Jan1999 to Dec 2001 | Laparoscopy | 92 | 36 (39.1%) |
| Laparotomy | 64 | |||||
| Miles et al. (31) | USA | Retrospective observational study | Jul 1999 to Jul 2002 | Laparoscopy | 22 | 9 (40.9%) |
| Laparotomy | 154 | |||||
| Omori et al. (41) | Japan | Retrospective observational study | Jan1993 and Dec1997; Jan 1998 to Jan 2000 | Laparoscopy | 11 | 1 (9.1%) |
| Laparotomy | 13 | |||||
| Leppäniem and Haapiainen (30) | Finland | RCT | May 1997 to Jan 2002 | Laparoscopy | 20 | 9 (45.0%) |
| Laparotomy | 23 | |||||
| DeMaria et al. (29) | USA | Prospective observational study | Nov 1991 to Sep 1993 | Laparoscopy | 31 | 14 (45.1%) |
| Laparotomy | 23 | |||||
| Mutter et al. (28) | France | Retrospective observational study | Feb 1990 to Jan 1996 | Laparoscopy | 17 | 4 (23.6%) |
| Laparotomy | 18 | |||||
| Marks et al. (27) | USA | Retrospective observational study | Jan 1992 to Sep 1994 | Laparoscopy | 14 | 4 (28.6%) |
| Laparotomy | 19 |
NR, not report.
Table 2.
Characteristics of the included patients.
| References | Population | Intervention | Age (y)* | Male, n (%) | ISS | New ISS | AIS/ATI | Haemodynamically stable (%) |
|---|---|---|---|---|---|---|---|---|
| Shams and Elyasi (17) | PAT | Laparoscopy | 33.4 ± 15.1 | 26 (65.0) | NR | NR | NR | 100.0% |
| Laparotomy | 27.8 ± 7.9 | NR | NR | NR | 100.0% | |||
| Birindelli et al. (19) | Splenic trauma | Laparoscopy | Mean 47 | 10 (62.5) | 24 | NR | NR | 100.0% |
| Laparotomy | Mean 50 | 22 (68.8) | 20 | NR | NR | 100.0% | ||
| Obaid et al. (18) | TDI | Laparoscopy | 36 ± 17 | 136 (76.8) | 17 (10–22) | NR | 2 (1–3) | 100.0% |
| Laparotomy | 35 ± 16 | 280 (79.1) | 17 (9–21) | NR | 2 (1–2) | 100.0% | ||
| Gao et al. (8) | PAT, BAT | Laparoscopy | 39.1 ± 15.3 | 41 (75.9) | 5.39 ± 2.72 | NR | NR | 100.0% |
| Laparotomy | 42.5 ± 13.6 | 42 (77.8) | 4.67 ± 2.56 | NR | NR | 100.0% | ||
| Lin et al. (12) | BAT | Laparoscopy | 38.5 ± 18.0 | 80 (63.5) | 18.9 ± 8.5 | NR | 3.3 ± 0.6 | 100.0% |
| Laparotomy | 35.2 ± 16.2 | 99 (71.2) | 23.3 ± 9.9 | NR | 3.7 ± 0.7 | 100.0% | ||
| Chakravartty et al. (7) | AT | Laparoscopy | 33 (14–62) | 21 (84.0) | 16 (4–34) | NR | NR | 100.0% |
| Laparotomy | 26 (16–58) | 23 (92.0) | 16 (3–29) | NR | NR | 100.0% | ||
| Trejo-Ávila et al. (20) | PAT, BAT | Laparoscopy | 25.5 ± 7.7 | 17 (89.5) | NR | NR | NR | 100.0% |
| Laparotomy | 30.9 ± 10.9 | 19 (100.0) | NR | NR | NR | 100.0% | ||
| Huang et al. (21) | BAT | Laparoscopy | Mean 47.2 | 6 (54.5) | Mean 21.6 | NR | Mean 3.4 | 100.0% |
| Laparotomy | Mean 49.1 | 30 (73.2) | Mean 28.6 | NR | Mean 3.8 | 100.0% | ||
| Lim et al. (40) | AT | Laparoscopy | 53.8 ± 15.7 | NR | 9.3 ± 3.6 | NR | 3.2 ± 1.4 | 100.0% |
| Laparotomy | 57.2 ± 15.6 | 9.1 ± 2.8 | NR | 3.2 ± 0.9 | 100.0% | |||
| Chestovich et al. (39) | PAT | Laparoscopy | 28 (22–42)a/ 29 (23–37)b |
82 (87.2) | 1 (1–3)a/ 1 (1–3)b |
1 (1–3)a/9 (4–15)b | 1 (1–1)a/ 2 (2–3)b |
100.0% |
| Laparotomy | 31 (23–42)a/ 30 (22–40)b |
88 (91.7) | 8 (4–13) a/ 9 (4–12)b |
1 (1–3)a/ 13 (5–20)b |
1 (1–1)a/ 3 (2–3)b |
97.9% | ||
| Liao et al. (38) | PAT, BAT | Laparoscopy | 44.4 ± 13.8 | 10 (66.7) | 11.5 ± 6.7 | NR | NR | 100.0% |
| Laparotomy | 44.1 ± 16.2 | 25 (83.3) | 11.8 ± 5.1 | NR | NR | 100.0% | ||
| Lee et al. (37, 38) | BAT | Laparoscopy | 38.0 ± 19.4 | 37 (64.9) | 17.6 ± 8.2 | NR | NR | 100.0% |
| Laparotomy | 33.6 ± 15.9 | 37 (78.7) | 20.2 ± 6.9 | NR | NR | 100.0% | ||
| Karateke et al. (35) | PAT | Laparoscopy | 33.2 ± 9.2 | 45 (86.5) | NR | NR | NR | 100.0% |
| Laparotomy | 35.2 ± 10.6 | NR | NR | NR | 100.0% | |||
| Khubutiya et al. (36) | PAT, BAT | Laparoscopy | 34.5 ± 14c/ 35.8 ± 3.5d |
273 (78.4) | 14.6 ± 0.7c/ 9.8 ± 0.5d |
NR | NR | 100.0% |
| Laparotomy | 33.5 ± 2.5c/ 36.5 ± 2.3d |
220 (78.6) | 14.9 ± 0.7c /6.4 ± 0.2d | NR | NR | 100.0% | ||
| Lin et al. (34) | abdominal stab wounds | Laparoscopy | 41.1 ± 14.3 | NR | 4.3 ± 4.8 | NR | 3.9 ± 4.7 | 100.0% |
| Laparotomy | 43.8 ± 11.6 | NR | 5.7 ± 5.0 | NR | 5.1 ± 5.5 | 100.0% | ||
| Cherkasov et al. (33) | PAT | Laparoscopy | NR | NR | NR | NR | NR | 8.7% of total patients |
| Laparotomy | NR | NR | NR | NR | NR | |||
| Cherry et al. (32) | PAT | Laparoscopy | 29.4 ± 1.2 | NR | 5.5 ± 0.6 | NR | NR | 100.0% |
| Laparotomy | 29.1 ± 1.4 | NR | 9.0 ± 0.8 | NR | NR | 100.0% | ||
| Miles et al. (31) | PAT | Laparoscopy | Mean 32.8 | 171 (81.8) | Mean 13.6 | NR | NR | 100.0% |
| Laparotomy | Mean 6.4 | NR | NR | 100.0% | ||||
| Omori et al. [41 | BAT | Laparoscopy | 50.6 ± 18.2 | 8 (72.7) | 11.8 ± 5.8 | NR | NR | 100.0% |
| Laparotomy | 45.9 ± 13.6 | 9 (69.2) | 14.4 ± 5.7 | NR | NR | 100.0% | ||
| Leppäniemi and Haapiainen (30) | Stab wounds | Laparoscopy | 39 ± 11 | 16 (85) | 6 ± 3 | 8 ± 6 | 9 ± 9 | 100.0% |
| Laparotomy | 41 ± 13 | 21 (91) | 8 ± 5 | 9 ± 7 | 6 ± 6 | 100.0% | ||
| DeMaria et al. (29) | Abdominal stab wounds | Laparoscopy | NR | NR | NR | NR | NR | 100.0% |
| Laparotomy | NR | NR | NR | NR | NR | 100.0% | ||
| Mutter et al. (28) | Abdominal stab wounds | Laparoscopy | 34 (17–62) | 32 (91.4) | NR | NR | NR | 100.0% |
| Laparotomy | NR | NR | NR | 100.0% | ||||
| Marks et al. (27) | PAT | Laparoscopy | 30.5 ± 2.4 | NR | 2.4 ± 0.6 | NR | NR | 100.0% |
| Laparotomy | 31.2 ± 2.2 | NR | 3.2 ± 0.7 | NR | NR | 100.0% |
PAT, penetrating abdominal trauma; BAT, Blunt abdominal trauma; TDI, Traumatic diaphragmatic injury; ISS, injury severity score; AIS, abbreviated injury scale; ATI, abdominal trauma index; NR, not reported.
Presented as mean ± standard deviation, median (range) or median (interquartile range).
Diagnostic laparoscopy.
Therapeutic laparoscopy.
Blunt abdominal trauma.
PAT, penetrating abdominal trauma.
Quality Assessment of the Included Studies
Although the only RCT (30) we reviewed did not implement the blinding method, the author specified random sequence generation and allocation concealment. With respect to incomplete outcome data and selective reporting, the RCT demonstrated a low risk of bias. Since blinding was not possible due to the nature of the surgical interventions, we deemed this RCT as a high-quality study. The quality of the selected cohort studies assessed by the NOS was moderate-to-high, although around half of the included studies (12, 17, 21, 28, 29, 31–33, 35, 36) did not describe in detail the methods used to avoid bias in the comparability domain. The details of the quality assessment are presented in Supplementary Tables S1, S2.
Meta-Analysis Results
Missed Injury
A total of 19 studies (8, 12, 18, 20, 27–35, 37–41) (5,327 patients) reported the cases of missed injury. In the laparoscopy arm, which resulted in 13 missed injuries in the laparoscopy group and 46 in the laparotomy group. The difference between the two groups (0.52vs 1.64%) was not statistically significant [RD −0.00, 95%CI (−0.00, 0.00), p = 0.90] (see Figure 2). The I2 statistic for heterogeneity among studies was 4%, suggesting low heterogeneity.
Figure 2.
Forest plot of the comparison of laparoscopy vs. laparotomy for abdominal trauma, outcome: missed injury. M-H, Mantel-Haenszel; CI, confidence interval.
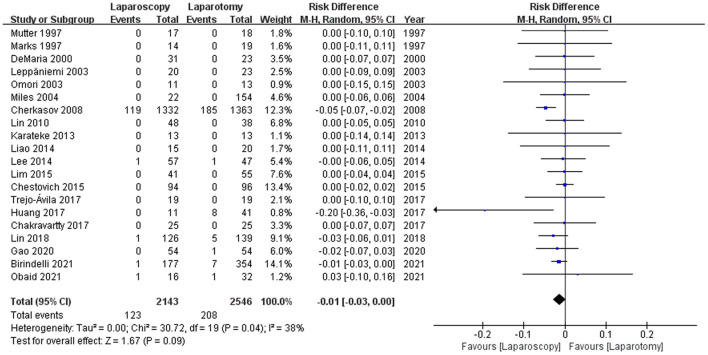
Mortality
Of the 23 studies, 20 (8, 12, 18–21, 27–31, 33–35, 37–41) reported mortalities. Overall, there were 123 mortalities in the laparoscopy group and 208 in the laparotomy group. There was no significant disparity in the incidence of mortality between the groups [5.74 vs. 8.17%, RD −0.01, 95%CI (−0.03, 0.00), p = 0.09], with moderate heterogeneity (I2 = 38%; see Figure 3).
Figure 3.
Forest plot of the comparison of laparoscopy vs. laparotomy for abdominal trauma, outcome: mortality. M-H, Mantel-Haenszel; CI, confidence interval.
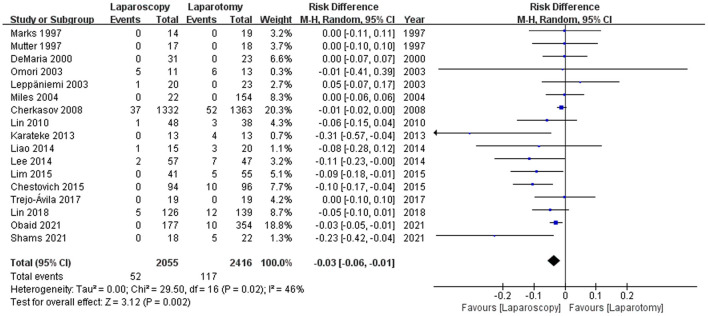
Wound Infection
Regarding complications, wound infections were reported by 17 studies (12, 17, 18, 20, 27–31, 33–35, 37–41), and the wound infection rate was 52 of 2055 (2.53%) patients in the laparoscopy group and 117 of 2,416 (4.84%) patients in the laparotomy group. Patients who underwent laparoscopy had a substantially lower incidence of wound infection than those in the laparotomy group [RD −0.03, 95%CI (−0.06, −0.01), p = 0.002] (see Figure 4). Heterogeneity among the studies was moderate (I2 = 46%).
Figure 4.
Forest plot of the comparison of laparoscopy vs. laparotomy for abdominal trauma, outcome: wound infection. M-H, Mantel-Haenszel; CI, confidence interval.
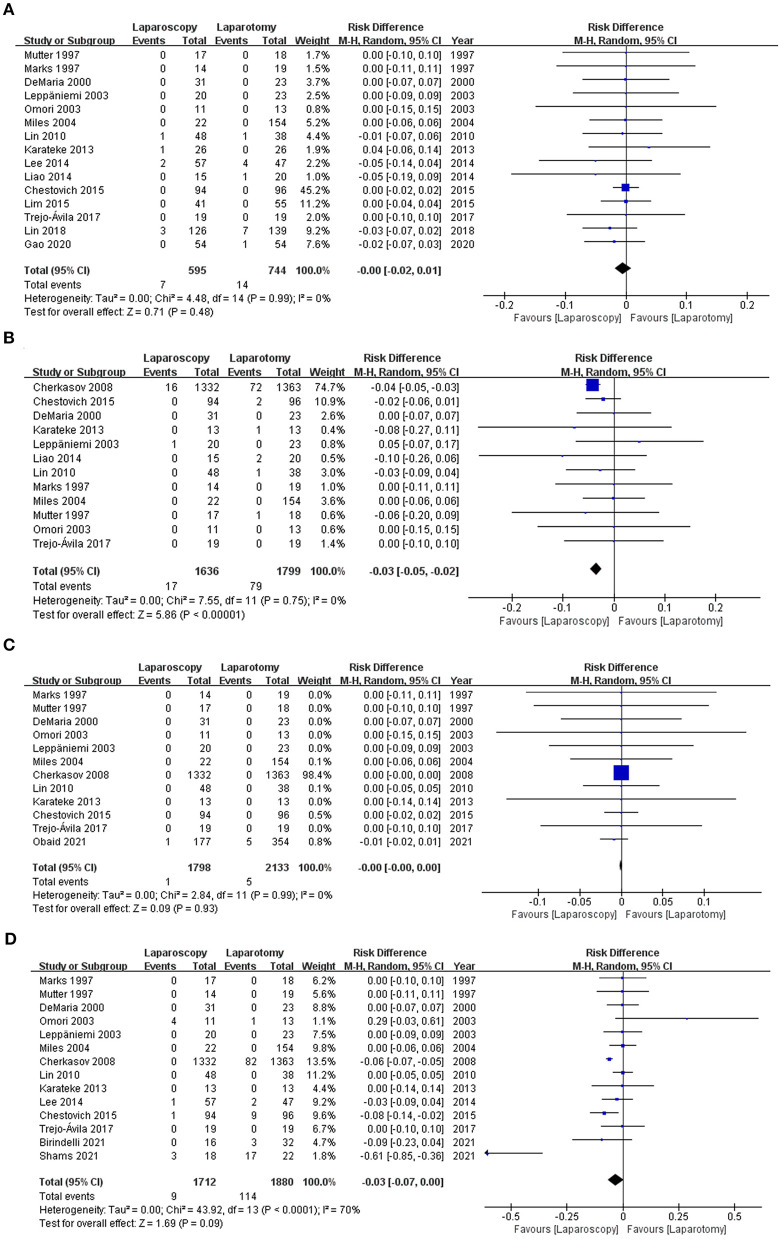
Intra-Abdominal Abscess
Of the 23 studies, 15 (8, 12, 20, 27–31, 34, 35, 37–41) of them including 1,339 patients, evaluated intra-abdominal abscesses. Seven patients treated with laparoscopy developed abscesses, compared with 14 patients in the laparotomy group. Both groups had similar rates of abscesses [1.18 vs. 1.88%, RD −0.00, 95% CI (−0.02, 0.01), p = 0.48] (see Figure 5A), and there was no significant heterogeneity across the studies (I2 = 0%).
Figure 5.
Forest plot of the comparison of laparoscopy vs. laparotomy for abdominal trauma, outcome: (A) intra-abdominal abscess; (B) pneumonia; (C) thromboembolism; (D) bowel obstruction or ileus. M-H, Mantel-Haenszel; CI, confidence interval.
Pneumonia
Twelve studies (20, 27–31, 33–35, 38, 39, 41), involving 1,636 patients in the laparoscopy group and 1,799 patients in the laparotomy group, investigated the incidence of pneumonia. Pneumonia occurred 17 times within the laparoscopy group and 79 times in the laparotomy group, indicating a substantially higher incidence rate for patients who underwent laparotomy [1.04 vs. 4.39%, RD −0.03, 95% CI (−0.05, 0.02), p < 0.00001]. There was no statistical heterogeneity among the studies (I2 = 0%; see Figure 5B).
Thromboembolism
Twelve studies (18, 20, 27–31, 33–35, 39, 41) examined thromboembolism, and only one reported that thromboembolism was occurred in both groups. The pooled analysis indicated that the proportion of thromboembolism was comparable between the two groups [0.05 vs. 0.23%, RD −0.00, 95% CI (−0.00, −0.00), p = 0.93], and there was no heterogeneity (I2 = 0%; see Figure 5C).
Bowel Obstruction or Ileus
There were 14 studies (17, 19, 20, 27–31, 33–35, 37, 39, 41) that reported data on bowel obstruction or ileus. Compared to patients in the laparotomy group, there was a lower incidence of ileus in the laparoscopy group (0.53 vs. 6.06%). However, the difference was not statistically significant in a pooled analysis [RD −0.03, 95% CI (−0.07, −0.00), p = 0.09]. Heterogeneity analyses suggested substantial heterogeneity across the studies (I2 = 70%; see Figure 5D).
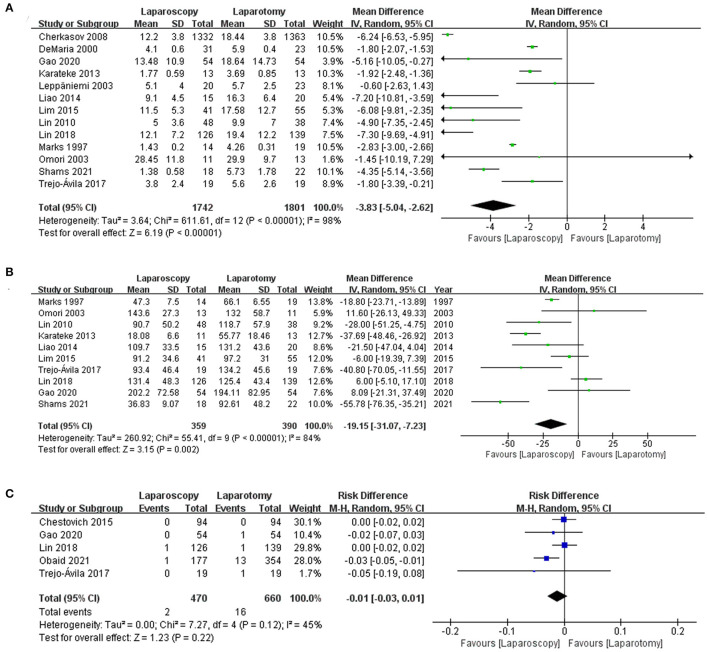
Length of Stay
All of the included studies considered the length of stay of patients with abdominal trauma. However, only 13 studies (8, 12, 17, 20, 27, 29, 30, 33–35, 38, 40, 41) of them were included in the quantitative synthesis. Meta-analysis results suggested that the length of stay of patients who underwent laparoscopy was significantly shorter than those who underwent laparotomy [MD −3.83, 95% CI (−5.04, −2.62) days, p < 0.00001], there was high heterogeneity (I2 = 98%; see Figure 6A). Eight (7, 18, 28, 31, 32, 36, 37, 39) of the ten remaining studies whose data was not suitable for quantitative synthesis were consistent with the above results, while the findings of two studies (19, 21) did not favor the above results.
Figure 6.
Forest plot of the comparison of laparoscopy vs. laparotomy for abdominal trauma, outcome: (A) the length of stay; (B) procedure time; (C) re-operation. IV, Inverse variance; CI, confidence interval.
Procedure Time
Of the 14 studies (8, 12, 17, 19–21, 27, 34, 35, 37, 38, 40, 41) that provided details of the procedure time, ten studies (8, 12, 17, 20, 27, 34, 35, 38, 40, 41) including 749 patients could be synthesized quantitatively. By comparing the operation conditions of two groups of patients, results from the meta-analysis showed that the procedure time of the laparoscopy was significantly shorter than laparotomy [MD −19.15, 95% CI (−31.07, −7.23) min, p = 0.002] (see Figure 6B). Nevertheless, heterogeneity among the studies was high (I2 = 84%). One (37) of the four studies that were performed qualitatively concurred with the above meta-analysis results. However, the three remaining studies (7, 19, 21) suggested that patients in laparoscopy group experienced a significantly longer procedure time compared with those in laparotomy.
Re-operation
Five studies (8, 12, 18, 20, 39) comprising 1,130 patients reported the rate of re-exploration, and the pooled analysis indicated that the rate of re-exploration did not differ significantly between the two groups [0.43 vs. 2.42%, RD −0.01, 95% CI (−0.03, 0.01), p = 0.22]. Besides, there was moderate heterogeneity (I2 = 45%; see Figure 6C).
Subgroup Analyses and Sensitivity Analyses
There was no statistical difference between subgroups based on study design, injury mechanism, and the purpose of laparoscopy use for primary outcomes (see Supplementary Tables S3–S5). Using fixed effects models did not substantially alter the results of any outcomes except for mortality, ileus, and re-operation (see Supplementary Table S6). Besides, sensitivity analyses indicated that the pooled results of mortality and pneumonia were varied after excluding the studies one by one. Concerning mortality, the results changed significantly when the study of Chestovich et al. (39) was removed [6.00 vs. 8.49%, RD −0.02, 95% CI (−0.03, −0.00), p = 0.02, I2 = 19%]. Moreover, the heterogeneity disappeared after removing the study of Cherkasov et al. (33) (from 41 to 0%), without causing a significant change in the pooled estimate. Besides, the results became statistically insignificant in the meta-analysis of pneumonia [0.33 vs. 1.61%, RD −0.01, 95% CI (−0.04, −0.01), p = 0.20] after removing the study of Cherkasov et al. (33), although there was still a lower trend toward laparoscopy. Also, inter-study heterogeneity was insignificant (I2 = 0%). After removing the study of Shams and Elyasi (17), the inter-study heterogeneity fell significantly (from 71 to 44%) for ileus. Additionally, the pooled results of high-quality studies (7, 8, 18–20, 27, 34, 37–40) were consistent with the results of the primary analyses for all outcomes except pneumonia (see Supplementary Table S7). Here, the difference in the risk of pneumonia became insignificant in the comparison of laparoscopy vs. laparotomy [0.48 vs. 2.35%, RD −0.02, 95% CI (−0.05, −0.01), p = 0.20, I2 = 0%]. Unfortunately, the sensitivity analyses did not reveal the source of high heterogeneity of length of stay and procedure time.
Publication Bias
The funnel plot of each outcome assessing the risk of publication bias showed symmetric distribution, indicating an absence of publication bias.
Discussion
The results of this study demonstrate that there is no significant difference in the incidence of missed injury and mortality between abdominal trauma patients receiving laparoscopy and those receiving laparotomy. Regarding postoperative complications, compared with patients in the laparotomy group, patients in the laparoscopy group have a similar risk of undergoing re-exploration or developing intra-abdominal abscesses, thromboembolism, and ileus, but there is a decreased incidence of wound infection and pneumonia. Besides, patients in the laparoscopy group experienced shorter hospitalization and procedure times.
Our results are largely consistent with previous reviews (15, 16). However, it was worth mentioning that there were two advantages in our study. First, we added several pieces of evidence from literature and comprehensively analyzed the value of diagnostic and therapeutic laparoscopy for patients with penetrating vs. blunt abdominal trauma. Moreover, this study conducted detailed subgroup analyses and found that there was no statistical difference between subgroups based on study design, injury mechanism, and the purpose of laparoscopy use. Finally, the findings demonstrated that therapeutic laparoscopy can serve as a safe and effective alternative in hemodynamically stable patients with abdominal trauma.
In this review, about one-quarter of all patients who had been recommended for laparoscopy needed to convert to laparotomy, with various conversion rates in all of the included studies. This is probably because the ability to conduct laparoscopy depends on hospital resources and the surgical skills of the surgeon (20). Another factor that may influence the results is that, different hospitals adopt various policies, and some centers recommend routine open surgery while others conduct laparoscopy in comparable patients (4, 7, 42, 43). Additionally, we noted that conversion rates are lower now than they were a decade ago, perhaps due to technological improvements in laparoscopic instruments and the accumulation of procedural experience. Also, with the advance in both laparoscopic experience and surgical techniques, the rate of missed injury has declined from 13 to 0.12%, a similar rate to its open surgery counterpart (44, 45). In this review, we calculated the overall rate of missed injury was 0.52% in the laparoscopy group, which was lower than the 3.2% reported by a review published in 2013 (46).
Laparoscopy benefits patients by significantly reducing peri-operative complications and hospital stays, improving quality of life, and accelerating their return to normal activities. Wound infection was the most commonly encountered complication in this review, with an overall incidence of 2.53% in the laparoscopy group, which was far lower than laparotomy. This is consistent with other studies that showed fewer wound infections following laparoscopic procedures, such as appendectomy (47) and cholecystectomy (48, 49). This could be due to the reduced surgical stress and tissue trauma that is imposed on the patient as a result of the minimally invasive approach. Multiple factors have been reported to be involved in this process, including less surgical trauma, a smaller incision, earlier mobilization, less postoperative pain, a less pronounced proinflammatory response than open surgery, and better preservation of the systemic immune function (50–52). The decreased incidence of pneumonia in patients with laparoscopy should be taken cautiously because of the inconsistencies between primary and sensitivity analysis. The inclusion of Cherkasov's study (33) may be responbile for the significant results. In the study (33), only 8% of the patients were haemodynamically stable, indicating that laparoscopy seemed to reduce the incidence of pneumonia in haemodynamically unstable patients. Also, sensitivity analyses did not support the robustness of results of the primary analyses for incidence of ileus. Given the significant heterogeneity between studies, the random-effects model was more appropriate because it provided a more conservative and reliable estimate of pooled RD. Coupled with the negative results of the pooled analysis of high-quality studies, we believed that there is no significant difference between the two surgical modes concerning the incidence of ileus. Finally, we found that laparoscopy is related to a decrease in the length of stay by approximately 4 days, and was close to the value of 5 days reported in the previous systematic review (15). Although there was high heterogeneity among the included studies, and we were not able to identify the source of heterogeneity, we still considered that the results were credible due to the consistency across all sensitivity analyses.
There are several limitations in this study that should be highlighted. First, only one of the studies included in our review was an RCT, and a majority of the studies were retrospective. These studies inherently contain a greater potential for misinterpretations than RCTs. However, because of the small number of trauma patients requiring surgical intervention, designing prospective comparative studies or RCTs may be difficult from an ethical or logistical perspective (7). Moreover, several studies included in this review were from historical cohorts of abdominal trauma, and the management methods do not correspond with current practice. Nonetheless, our study was not powered to see differences between the subgroups stratified by study designs. Second, some outcomes were not clearly defined, such as the differentiation between wound infection and intra-abdominal abscess. If a study reported organ space infection, that is technically an intra-abdominal abscess. However, there is no way to definitively distinguish between the two outcomes, so we could only assume that the determination of intra-abdominal abscess was correct when performing the quantitative synthesis. Finally, the experience of surgeon and trauma center infrastructure are important factors for assessing the laparoscopic operations, but a half of the included studies did not specify the experience of laparoscopic trauma surgeons and the volume of trauma centers. This makes it difficult to evaluate the performance bias by stratification.
Conclusion
Laparoscopic surgery is a reasonable alternative to open surgery for the appropriate patients, but the intervention should be performed by the experienced surgeons in well-equipped health care facilities. However, more well-organized RCTs are required to verify the value of laparoscopy for diagnosing and treating abdominal trauma.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
SZ and KW proposed the conception or study design. JW and LC performed literature search and screening and risk of bias assessment. JW wrote the manuscript. JL, BZ, WW, WZ, YG, and CB were responsible for data analysis. YH and SQ revised the manuscript. All authors agree to be responsible for all aspects of the work and finally approved the version to be published.
Funding
This study was supported by Foundation of Emergency Medical Association of Anhui Province (FY2019-098).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.817134/full#supplementary-material
References
- 1.Rhee P, Joseph B, Pandit V, Aziz H, Vercruysse G, Kulvatunyou N, et al. Increasing trauma deaths in the United States. Ann Surg. (2014) 260:13–21. 10.1097/SLA.0000000000000600 [DOI] [PubMed] [Google Scholar]
- 2.Smith J, Caldwell E, D'Amours S, Jalaludin B, Sugrue M. Abdominal trauma: a disease in evolution. ANZ J Surg. (2005) 75:790–4. 10.1111/j.1445-2197.2005.03524.x [DOI] [PubMed] [Google Scholar]
- 3.Parajuli P, Kumar S, Gupta A, Bansal VK, Sagar S, Mishra B, et al. Role of laparoscopy in patients with abdominal trauma at level-i trauma center. Surg Laparosc Endosc Percutan Tech. (2018) 28:20–5. 10.1097/SLE.0000000000000379 [DOI] [PubMed] [Google Scholar]
- 4.Ozkan OV, Justin V, Fingerhut A, Uranues S. Laparoscopy in abdominal trauma. Curr Trauma Rep. (2016) 2:238–46. 10.1007/s40719-016-0067-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma. (1995) 38:350–6. 10.1097/00005373-199503000-00007 [DOI] [PubMed] [Google Scholar]
- 6.Sosa JL, Baker M, Puente I, Sims D, Sleeman D, Ginzburg E, et al. Negative laparotomy in abdominal gunshot wounds: potential impact of laparoscopy. J Trauma. (1995) 38:194–7. 10.1097/00005373-199502000-00007 [DOI] [PubMed] [Google Scholar]
- 7.Chakravartty S, Sarma DR, Noor M, Panagiotopoulos S, Patel AG. Laparoscopy has a therapeutic role in the management of abdominal trauma: a matched-pair analysis. Int J Surg. (2017) 44:21–5. 10.1016/j.ijsu.2017.05.035 [DOI] [PubMed] [Google Scholar]
- 8.Gao Y, Li S, Xi H, Bian S, Zhang K, Cui J, et al. Laparoscopy versus conventional laparotomy in the management of abdominal trauma: a multi-institutional matched-pair study. Surg Endosc. (2020) 34:2237–42. 10.1007/s00464-019-07013-4 [DOI] [PubMed] [Google Scholar]
- 9.Goodman CS, Hur JY, Adajar MA, Coulam CH. How well does CT predict the need for laparotomy in hemodynamically stable patients with penetrating abdominal injury? a review and meta-analysis. AJR Am J Roentgenol. (2009) 193:432–7. 10.2214/AJR.08.1927 [DOI] [PubMed] [Google Scholar]
- 10.Lamb CM, Garner JP. Selective non-operative management of civilian gunshot wounds to the abdomen: a systematic review of the evidence. Injury. (2014) 45:659–66. 10.1016/j.injury.2013.07.008 [DOI] [PubMed] [Google Scholar]
- 11.Durso AM, Paes FM, Caban K, Danton G, Braga TA, Sanchez A, et al. Evaluation of penetrating abdominal and pelvic trauma. Eur J Radiol. (2020) 130:109187. 10.1016/j.ejrad.2020.109187 [DOI] [PubMed] [Google Scholar]
- 12.Lin HF, Chen YD, Chen SC. Value of diagnostic and therapeutic laparoscopy for patients with blunt abdominal trauma: a 10-year medical center experience. PLoS ONE. (2018) 13:e0193379. 10.1371/journal.pone.0193379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koganti D, Hazen BJ, Dente CJ, Nguyen J, Gelbard RB. The role of diagnostic laparoscopy for trauma at a high-volume level one center. Surg Endosc. (2021) 35:2667–70. 10.1007/s00464-020-07687-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ki YJ, Jo YG, Park YC, Kang WS. The efficacy and safety of laparoscopy for blunt abdominal trauma: a systematic review and meta-analysis. J Clin Med. (2021) 10:1853. 10.3390/jcm10091853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hajibandeh S, Hajibandeh S, Gumber AO, Wong CS. Laparoscopy versus laparotomy for the management of penetrating abdominal trauma: a systematic review and meta-analysis. Int J Surg. (2016) 34:127–36. 10.1016/j.ijsu.2016.08.524 [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Xiang Y, Wu N, Wu L, Yu Z, Zhang M, et al. A comparison of laparoscopy and laparotomy for the management of abdominal trauma: a systematic review and meta-analysis. World J Surg. (2015) 39:2862–71. 10.1007/s00268-015-3212-4 [DOI] [PubMed] [Google Scholar]
- 17.Shams M, Elyasi A. Comparison of diagnostic laparoscopy and exploratory laparotomy in the management of patients with penetrating abdominal trauma. J Babol Univ Medical Sci. (2021) 23:222–8. [Google Scholar]
- 18.Obaid O, Hammad A, Bible L, Ditillo M, Castanon L, Douglas M, et al. Open versus laparoscopic repair of traumatic diaphragmatic injury: a nationwide propensity-matched analysis. J Surg Res. (2021) 268:452–8. 10.1016/j.jss.2021.07.022 [DOI] [PubMed] [Google Scholar]
- 19.Birindelli A, Martin M, Khan M, Gallo G, Segalini E, Gori A, et al. Laparoscopic splenectomy as a definitive management option for high-grade traumatic splenic injury when non operative management is not feasible or failed: a 5-year experience from a level one trauma center with minimally invasive surgery expertise. Updates Surg. (2021) 73:1515–31. 10.1007/s13304-021-01045-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trejo-Ávila ME, Valenzuela-Salazar C, Betancourt-Ferreyra J, Fernández-Enríquez E, Romero-Loera S, Moreno-Portillo M. Laparoscopic versus open surgery for abdominal trauma: a case-matched study. J Laparoendosc Adv Surg Tech A. (2017) 27:383–7. 10.1089/lap.2016.0535 [DOI] [PubMed] [Google Scholar]
- 21.Huang GS, Chance EA, Hileman BM, Emerick ES, Gianetti EA. Laparoscopic splenectomy in hemodynamically stable blunt trauma. JSLS. (2017) 21: e2017.00013. 10.4293/JSLS.2017.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane. (2021). Available online at: www.training.cochrane.org/handbook (accessed November 17, 2021).
- 24.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Review Manager (RevMan) . [Computer Program]. Version 5.3. Copenhagen, DTNCC. The Cochrane Collaboration (2014). [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marks JM, Youngelman DF, Berk T. Cost analysis of diagnostic laparoscopy vs laparotomy in the evaluation of penetrating abdominal trauma. Surg Endosc. (1997) 11:272–6. 10.1007/s004649900342 [DOI] [PubMed] [Google Scholar]
- 28.Mutter D, Nord M, Vix M, Evrard S, Marescaux J. Laparoscopy in the evaluation of abdominal stab wounds. Digest Surg. (1997) 14:39–42. 10.1159/00017250919095102 [DOI] [Google Scholar]
- 29.DeMaria EJ, Dalton JM, Gore DC, Kellum JM, Sugerman HJ. Complementary roles of laparoscopic abdominal exploration and diagnostic peritoneal lavage for evaluating abdominal stab wounds: a prospective study. J Laparoendosc Adv Surg Tech A. (2000) 10:131–6. 10.1089/lap.2000.10.131 [DOI] [PubMed] [Google Scholar]
- 30.Leppäniemi A, Haapiainen R. Diagnostic laparoscopy in abdominal stab wounds: a prospective, randomized study. J Trauma. (2003) 55:636–45. 10.1097/01.TA.0000063000.05274.A4 [DOI] [PubMed] [Google Scholar]
- 31.Miles EJ, Dunn E, Howard D, Mangram A. The role of laparoscopy in penetrating abdominal trauma. JSLS. (2004) 8:304–9. [PMC free article] [PubMed] [Google Scholar]
- 32.Cherry RA, Eachempati SR, Hydo LJ, Barie PS. The role of laparoscopy in penetrating abdominal stab wounds. Surg Laparosc Endosc Percutan Tech. (2005) 15:14–7. 10.1097/01.sle.0000153732.70603.f9 [DOI] [PubMed] [Google Scholar]
- 33.Cherkasov M, Sitnikov V, Sarkisyan B, Degtirev O, Turbin M, Yakuba A. Laparoscopy versus laparotomy in management of abdominal trauma. Surg Endosc. (2008) 22:228–31. 10.1007/s00464-007-9550-z [DOI] [PubMed] [Google Scholar]
- 34.Lin HF, Wu JM, Tu CC, Chen HA, Shih HC. Value of diagnostic and therapeutic laparoscopy for abdominal stab wounds. World J Surg. (2010) 34:1653–62. 10.1007/s00268-010-0485-5 [DOI] [PubMed] [Google Scholar]
- 35.Karateke F, Özdogan M, Özyazici S, Daş K, Menekşe E, Gülnerman YC, et al. The management of penetrating abdominal trauma by diagnostic laparoscopy: a prospective non-randomized study. Ulus Travma Acil Cerrahi Derg. (2013) 19:53–7. 10.5505/tjtes.2013.40799 [DOI] [PubMed] [Google Scholar]
- 36.Khubutiya MS, Yartsev PA, Guliaev AA, Levitsky VD, Tlibekova MA. Laparoscopy in blunt and penetrating abdominal trauma. Surg Laparosc Endosc Percutan Tech. (2013) 23:507–12. 10.1097/SLE.0b013e3182937c37 [DOI] [PubMed] [Google Scholar]
- 37.Lee PC, Lo C, Wu JM, Lin KL, Lin HF, Ko WJ. Laparoscopy decreases the laparotomy rate in hemodynamically stable patients with blunt abdominal trauma. Surg Innov. (2014) 21:155–65. 10.1177/1553350612474496 [DOI] [PubMed] [Google Scholar]
- 38.Liao CH, Kuo IM, Fu CY, Chen CC, Yang SJ, Ouyang CH, et al. Gasless laparoscopic assisted surgery for abdominal trauma. Injury. (2014) 45:850–4. 10.1016/j.injury.2013.10.041 [DOI] [PubMed] [Google Scholar]
- 39.Chestovich PJ, Browder TD, Morrissey SL, Fraser DR, Ingalls NK, Fildes JJ. Minimally invasive is maximally effective: diagnostic and therapeutic laparoscopy for penetrating abdominal injuries. J Trauma Acute Care Surg. (2015) 78:1076–83; discussion 1083–5. 10.1097/TA.0000000000000655 [DOI] [PubMed] [Google Scholar]
- 40.Lim KH, Chung BS, Kim JY, Kim SS. Laparoscopic surgery in abdominal trauma: a single center review of a 7-year experience. World J Emerg Surg. (2015) 10:16. 10.1186/s13017-015-0007-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Omori H, Asahi H, Inoue Y, Tono C, Irinoda T, Saito K. Selective application of laparoscopic intervention in the management of isolated bowel rupture in blunt abdominal trauma. J Laparoendosc Adv Surg Tech A. (2003) 13:83–8. 10.1089/109264203764654696 [DOI] [PubMed] [Google Scholar]
- 42.Lin HF, Chen YD, Lin KL, Wu MC, Wu CY, Chen SC. Laparoscopy decreases the laparotomy rate for hemodynamically stable patients with blunt hollow viscus and mesenteric injuries. Am J Surg. (2015) 210:326–33. 10.1016/j.amjsurg.2014.11.009 [DOI] [PubMed] [Google Scholar]
- 43.Cocco AM, Bhagvan S, Bouffler C, Hsu J. Diagnostic laparoscopy in penetrating abdominal trauma. ANZ J Surg. (2019) 89:353–6. 10.1111/ans.15140 [DOI] [PubMed] [Google Scholar]
- 44.Matsevych O, Koto M, Balabyeki M, Aldous C. Trauma laparoscopy: when to start and when to convert? Surg Endosc. (2018) 32:1344–52. 10.1007/s00464-017-5812-6 [DOI] [PubMed] [Google Scholar]
- 45.Koto MZ, Matsevych OY, Motilall SR. The role of laparoscopy in penetrating abdominal trauma: our initial experience. J Laparoendosc Adv Surg Tech A. (2015) 25:730–6. 10.1089/lap.2015.0042 [DOI] [PubMed] [Google Scholar]
- 46.O'Malley E, Boyle E, O'Callaghan A, Coffey JC, Walsh SR. Role of laparoscopy in penetrating abdominal trauma: a systematic review. World J Surg. (2013) 37:113–22. 10.1007/s00268-012-1790-y [DOI] [PubMed] [Google Scholar]
- 47.Zhang J, Wang M, Xin Z, Li P, Feng Q. Updated evaluation of laparoscopic vs. open appendicectomy during pregnancy: a systematic review and meta-analysis. Front Surg. (2021) 8:720351. 10.3389/fsurg.2021.720351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhao JJ, Syn NL, Chong C, Tan HL, Ng JYX, Yap A, et al. Comparative outcomes of needlescopic, single-incision laparoscopic, standard laparoscopic, mini-laparotomy, and open cholecystectomy: a systematic review and network meta-analysis of 96 randomized controlled trials with 11,083 patients. Surgery. (2021) 170:994–1003. 10.1016/j.surg.2021.04.004 [DOI] [PubMed] [Google Scholar]
- 49.Kurtulus I, Culcu OD, Degerli MS. Which is more effective: laparoscopic or open partial cholecystectomy? J Laparoendosc Adv Surg Tech A. (2021). 10.1089/lap.2021.0300. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 50.Boni L, Benevento A, Rovera F, Dionigi G, Di Giuseppe M, Bertoglio C, et al. Infective complications in laparoscopic surgery. Surg Infect. (2006) 7(Suppl. 2):S109–11. 10.1089/sur.2006.7.s2-109 [DOI] [PubMed] [Google Scholar]
- 51.Shabanzadeh DM, Sørensen LT. Laparoscopic surgery compared with open surgery decreases surgical site infection in obese patients: a systematic review and meta-analysis. Ann Surg. (2012) 256:934–45. 10.1097/SLA.0b013e318269a46b [DOI] [PubMed] [Google Scholar]
- 52.Gupta A, Watson DI. Effect of laparoscopy on immune function. Br J Surg. (2001) 88:1296–306. 10.1046/j.0007-1323.2001.01860.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.