Abstract
Background:
US policy efforts have focused on reducing rural-urban health inequities. However, it is unclear whether gaps in care and outcomes remain among older adults with acute cardiovascular conditions.
Objective:
To evaluate rural-urban differences in procedural care and mortality for acute myocardial infarction (AMI), heart failure (HF), and ischemic stroke.
Methods:
Retrospective cross-sectional study of Medicare fee-for-service beneficiaries aged ≥65 years with acute cardiovascular conditions from 2016 to 2018. Cox proportional hazards model with random hospital intercepts were fit to examine the association of presenting to a rural (vs. urban) hospital and 30- and 90-day patient-level mortality.
Results:
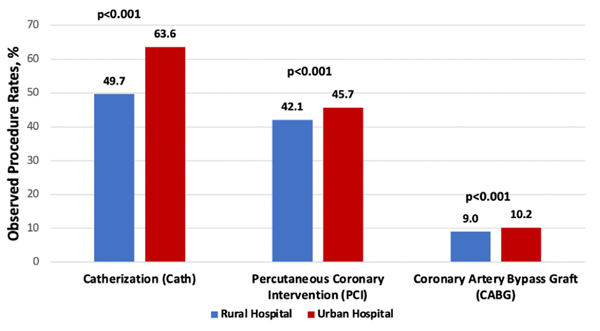
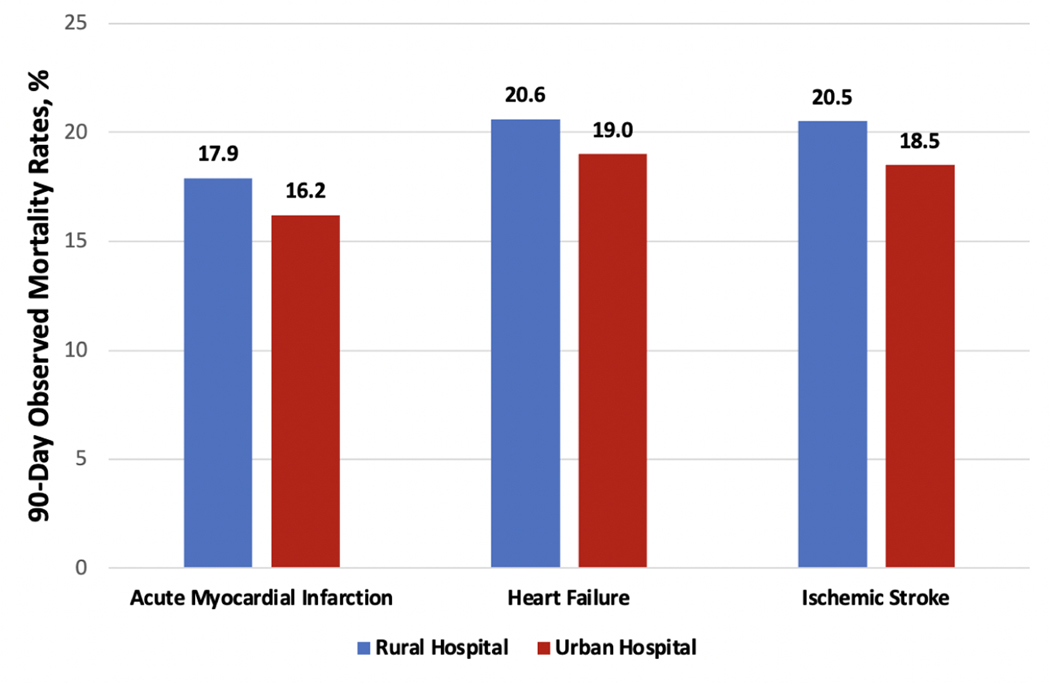
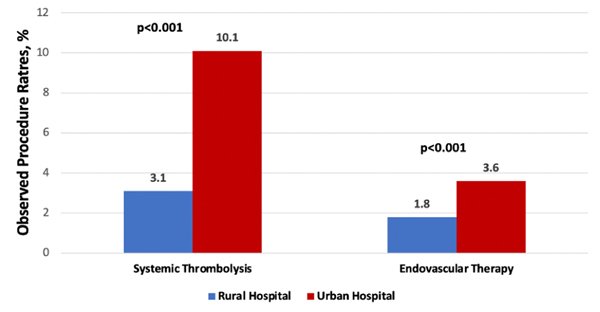
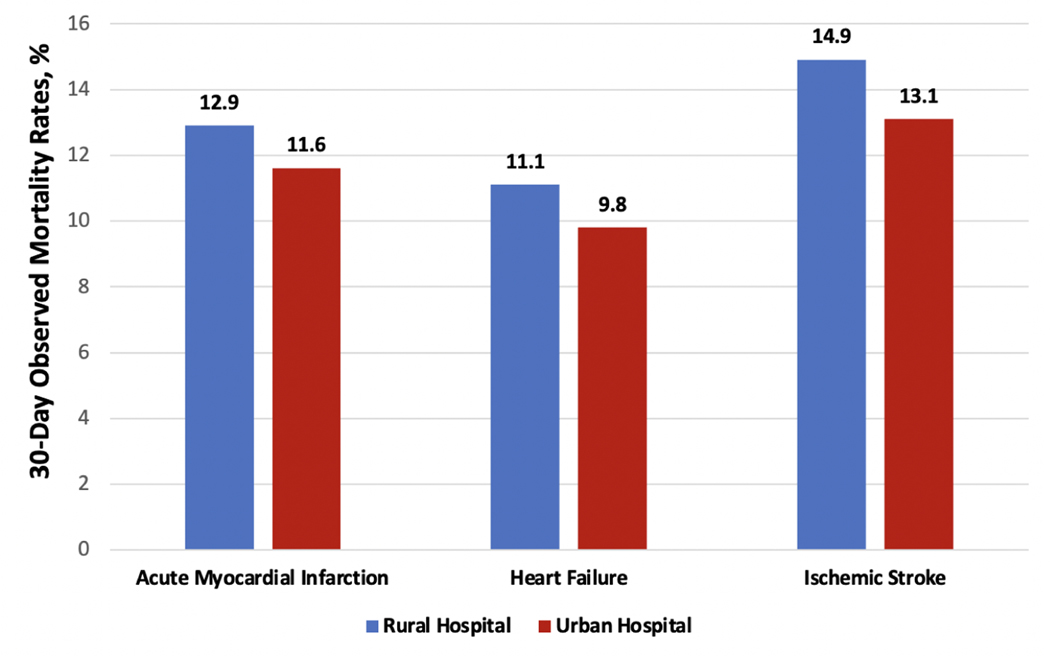
There were 2,182,903 Medicare patients hospitalized with AMI, HF, or ischemic stroke from 2016–2018. Patients with AMI were less likely to undergo cardiac catherization (49.7% vs. 63.6%, p<0.001), PCI (42.1% vs. 45.7%, p<0.001) or CABG (9.0% vs. 10.2%, p<0.001) within 30 days at rural vs. urban hospitals. Thrombolysis rates (3.1% vs. 10.1%, p<0.001) and endovascular therapy (1.8% vs. 3.6%, p<0.001) for ischemic stroke were lower at rural hospitals. After adjustment for demographics and clinical comorbidities, the 30-day mortality hazard ratio (HR) was significantly higher among patients presenting to rural hospitals for AMI (HR 1.10, 95% CI 1.08–1.12), HF (1.15, 95% CI 1.13–1.16), and ischemic stroke (1.20, 95% CI 1.18–1.22), with similar patterns at 90 days. These differences were most pronounced for the subset of critical access hospitals that serve remote, rural areas.
Conclusions:
Clinical, public health, and policy efforts are needed to improve rural-urban gaps in care and outcomes for acute cardiovascular conditions.
Keywords: Rural health, Myocardial infarction, Heart Failure, Stroke, Cardiovascular, Health disparities
Condensed Abstract
In this national study of Medicare beneficiaries aged 65 years or older in the US, there were significant rural-urban differences in procedural care and mortality for AMI, HF, and ischemic stroke between 2016 and 2018. Patients initially presenting to rural hospitals were less likely to receive important procedures and treatments for AMI and ischemic stroke. Mortality at 30- and 90-days was significantly higher among beneficiaries presenting to rural hospitals for all three conditions compared to urban hospitals. These differences were most pronounced for the subset of critical access hospitals that serve remote, rural areas. Policy and clinical efforts are urgently needed to improve rural-urban gaps in care delivery and outcomes for acute cardiovascular conditions.
Introduction
In the United States, cardiovascular mortality rates are higher in rural areas compared with urban areas. (1, 2) Rural residents face numerous challenges that affect their cardiovascular health, including poor access to healthcare services for urgent conditions and lower quality care. (3) For acute cardiovascular conditions in particular, data from the early 2000s suggest that older adults admitted to rural hospitals have higher mortality rates than their urban counterparts. (4–8) Although public health and policy efforts to improve rural health have intensified over the past decade, recent studies suggest that the gap in population-level cardiovascular mortality has widened between rural and urban areas of the US. (9–12) However, less is known about whether these patterns, at least in part, reflect ongoing disparities in hospital-level care for acute cardiovascular conditions, including acute myocardial infarction and stroke. (3) Rural adults hospitalized with cardiovascular conditions may receive lower quality hospital care and may also face increasing barriers in access to critical post-acute and rehabilitative care services after discharge due to declining rural healthcare infrastructure. (13–15) Regional systems of care and transfer protocols that rapidly route rural patients to better-resourced urban centers have proliferated, but it is unclear whether gaps in the delivery of time-sensitive procedural care remain. (16, 17) In addition, more than 130 rural hospitals have closed since 2010, and rural adults may therefore now have worse access to timely care for emergent conditions such as acute myocardial infarction and stroke. (18–21) Given these patterns, there is an urgent need to understand current differences in care and outcomes for patients hospitalized with cardiovascular conditions in rural vs. urban areas, to inform clinical and policy strategies that aim to reduce rural-urban health inequities.
Therefore, in this study, we aimed to answer three questions. First, did treatment patterns and mortality differ for Medicare beneficiaries initially presenting to rural vs. urban hospitals with acute myocardial infarction, heart failure, or ischemic stroke between 2016 and 2018? Second, were these patterns related to differences in hospital resources/capabilities and the delivery of procedural care? And third, were rural-urban differences in mortality more pronounced in specific geographic regions of the United States?
Methods
Institutional review board approval, including waiver of the requirement for participant informed consent, was provided by Beth Israel Deaconess Medical Center.
Study Population
We used 100% Medicare Provider Analysis and Review files to identify individuals aged 65 years or older enrolled in Medicare fee-for-service (FFS) between January 1, 2016 and December 31, 2018 with a primary discharge diagnosis of acute myocardial infarction, heart failure, or ischemic stroke. The study cohorts were defined with International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes used in the publicly reported measures. (22) Medicare denominator files were used to obtain information on demographic characteristics, patient-level poverty (defined by dual enrollment in Medicare and Medicaid), and mortality. (23) If a patient had more than one hospitalization for a given condition during the study period, the earliest event was selected. We linked transfers into a single episode of care. Outcomes were attributed to the first (transfer-out) hospital where patients presented. In other words, if a patient initially presented to a rural hospital and was then transferred to an urban hospital, treatments and outcomes were attributed to the rural hospital. Using the Medicare Institutional Outpatient files, we were able to link patients who were initially in Emergency Department (ED) or observation stays with their subsequent inpatient stays. The time zero for these patients started from the ED or observation stays.
Patient Characteristics
Patient characteristics included demographics (age, sex, race/ethnicity), dual-enrollment status, and clinical comorbidities. We obtained patient’s clinical comorbidities from two sources: 1) inpatient data based on the Elixhauser Comorbidity algorithm to identify comorbidities during the year prior to the index hospitalization and 2) the Chronic Condition Data Warehouse (CCW), to identify 27 common chronic conditions present one year prior to the index hospitalization. The CCW data gathers patient chronic conditions based on all available sources of the Medicare claims. (24, 25) Race/ethnicity was classified based on self-report using categories specified by Medicare at the time of Medicare enrollment. Race/ethnicity was included as a covariate in the analysis because it is associated with mortality.
Definition of Rural and Urban Hospitals
To classify rural and urban hospitals, we used the 2010 rural-urban commuting area (RUCA) codes to identify whether a hospital was located in a rural or urban area. (26) Specifically, we assigned a hospital to the rural group if it was located in an area with a RUCA code equal to 4 or greater (eTable 1), consistent with prior studies. (26–28) Hospital characteristics were obtained from the 2018 American Hospital Association Survey data.
Outcomes
The primary outcomes were 1) 30-day all-cause mortality rates and 2) 90-day all-cause mortality rates for acute myocardial infarction, heart failure, or ischemic stroke. We also evaluated cardiac catheterization and revascularization rates (percutaneous coronary intervention (PCI), coronary artery bypass graft surgery (CABG)) for acute myocardial infarction within 30 days of presentation and treatment rates (thrombolysis, endovascular therapy) for ischemic stroke (eTable 2).
Statistical Analysis
Baseline characteristics of Medicare patients with acute myocardial infarction, heart failure, or ischemic stroke at rural vs. urban hospitals were compared using two-sided t-tests and chi-squared tests. We then fit a Cox proportional hazards model with random hospital intercepts to examine the unadjusted the association between presenting to a rural (vs. urban) site and patient-level 30- and 90-day mortality for acute myocardial infarction (overall, non-STEMI, and ST-elevation MI), heart failure, and ischemic stroke. We then adjusted for patient demographics (age, sex, race/ethnicity, and poverty) and clinical comorbidities. Our multivariable adjusted model allowed us to account for individual risk factors and make inferences at the patient level about the association of presenting to a rural hospital with clinical outcomes, and represent our main findings. We then performed a mediation analysis that included additional variables in our models, including those that reflect hospital resources and capabilities (nurse staffing levels, presence of an intensive care unit, cardiology services) as well as treatment/procedure rates (e.g. PCI/CABG within 30 days of presentation for myocardial infarction), to understand whether these factors contributed to observed differences in rural vs. urban outcomes. We also repeated Cox model for 30-day all-cause readmissions for patients initially admitted for heart failure, and accounted for competing risk of death using the Fine and Gray method. (29) We also included an interaction term in our models for race (white vs. non-white), site of presentation (rural vs. urban hospital), and outcomes. As a sensitivity analysis, we repeated our main analyses after excluding patients who were transferred (because the rate at which patients are transferred out is higher at rural hospitals). (30)
Additional Analyses
We performed several additional analyses. First, we examined geographic differences in the rural-urban association with clinical outcomes, by repeating our main analysis stratified by U.S. Census bureau regions. Second, within rural areas, we compared critical access vs. non-critical access rural hospitals. Hospitals eligible to become a critical access site must have 25 or fewer acute care inpatient beds, generally be located more than 35 miles from another hospital, and provide 24/7 emergency care services. (31) We performed this analysis because critical-access sites represent a subset of rural hospitals that deliver care to particularly remote communities and receive cost-based reimbursement to ensure their viability.
Statistical tests were 2-sided at a significance level of 0.05. Analyses were performed using SAS, version 9.4 64-bit (SAS Institute Inc., Cary, North Carolina). The study followed the guidelines for cohort studies, described in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies.
Results
Baseline Characteristics
The study cohort included 2,182,903 Medicare fee-for-service beneficiaries across 4,488 hospitals, of which 2,375 were urban and 2,113 rural sites. There were 578,437 Medicare beneficiaries who were hospitalized for acute myocardial infarction, 1,031,522 for heart failure, and 572,944 for ischemic stroke, of which 98,878 (17.1%), 183,277 (17.8%), and 89,922 (15.7%) presented to a rural hospital (Table 1).
Table 1.
Baseline Characteristics of Medicare Beneficiaries with Cardiovascular Conditions at Rural and Urban Hospitals
| Acute Myocardial Infarction | Heart Failure | Ischemic Stroke | ||||
|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | Rural | Urban | |
| Total (n) | 98878 | 479559 | 183277 | 848245 | 89922 | 483022 |
| Age (mean, SD) | 77.8 (8.8) | 77.1 (8.7) | 80.7 (8.9) | 80.2 (9.3) | 79.8 (8.8) | 79.3 (8.9) |
| Female | 45.4 | 43.5 | 53.0 | 52.0 | 55.1 | 54.5 |
| Race | ||||||
| White | 90.6 | 84.1 | 87.3 | 81.2 | 88.8 | 80.8 |
| Black | 4.7 | 8.6 | 6.9 | 12.1 | 7.2 | 12.1 |
| Other | 4.7 | 7.3 | 5.8 | 6.7 | 4.0 | 7.1 |
| Cardiovascular Conditions | ||||||
| Atrial fibrillation | 10.9 | 11.1 | 31.5 | 33.2 | 15.7 | 16.5 |
| Diabetes | 44.3 | 47.3 | 52.1 | 54.3 | 40.7 | 43.1 |
| Hypertension | 85.3 | 85.6 | 88.5 | 89.4 | 91.8 | 93.2 |
| Hyperlipidemia | 57.9 | 60.9 | 67.4 | 71.2 | 55.4 | 58.8 |
| Ischemic heart disease | 48.3 | 49.7 | 61.7 | 63.3 | 38.8 | 39.6 |
| Peripheral vascular disease | 14.9 | 16.8 | 15.4 | 18.2 | 8.6 | 10.2 |
| History of AMI | 2.5 | 2.6 | 3.8 | 3.7 | 1.5 | 1.5 |
| History of stroke/TIA | 5.3 | 5.8 | 6.8 | 7.8 | 9.9 | 11.2 |
| History of congestive heart failure | 28.4 | 28.6 | 64.0 | 64.3 | 30.3 | 30.4 |
| Valvular heart disease | 3.5 | 4.4 | 8.7 | 11.8 | 11.0 | 13.1 |
| Other Conditions | ||||||
| Anemia | 35.5 | 40.1 | 54.2 | 61.1 | 29.6 | 34.5 |
| Alzheimer’s and Dementia | 13.7 | 12.7 | 18.6 | 18.4 | 19.4 | 19.6 |
| Chronic kidney disease | 32.1 | 35.1 | 50.4 | 54.2 | 29.8 | 32.0 |
| Chronic obstructive pulmonary disease | 19.8 | 16.7 | 32.4 | 29.2 | 15.8 | 14.0 |
| Chronic pulmonary disorders | 28.9 | 26.5 | 44.1 | 42.7 | 17.8 | 16.6 |
| Electrolyte/fluid disorders | 32.7 | 36.7 | 46.8 | 52.7 | 22.6 | 24.7 |
| Hip/pelvic fracture | 1.0 | 0.8 | 1.6 | 1.5 | 1.2 | 1.2 |
| Hypothyroidism | 16.2 | 16.0 | 22.6 | 22.4 | 17.4 | 17.4 |
| Liver disease | 1.9 | 2.5 | 3.1 | 4.4 | 1.0 | 1.4 |
| Lymphoma | 0.7 | 0.8 | 1.1 | 1.6 | 0.5 | 0.7 |
| Metastatic cancer | 1.4 | 1.5 | 1.5 | 1.9 | 1.3 | 1.9 |
| Obesity | 16.1 | 17.5 | 22.7 | 24.9 | 8.8 | 10.0 |
| Other neurological disorders | 12.1 | 11.3 | 14.5 | 13.6 | 0.3 | 0.5 |
| Pulmonary circulation disorders | 0.4 | 0.5 | 1.2 | 1.5 | 0.6 | 0.8 |
| Rheumatoid arthritis/ osteoarthritis | 35.6 | 34.5 | 43.8 | 42.9 | 36.1 | 35.5 |
| Solid tumor w/o metastases | 2.6 | 3.0 | 3.3 | 3.8 | 2.0 | 2.2 |
| Length of stay (mean, SD) | 4 (4.2) | 5 (5.4) | 4 (3.2) | 5 (4.9) | 4 (3.7) | 5 (4.9) |
| Disposition | ||||||
| Home | 53.6 | 54.8 | 42.7 | 42.4 | 26.9 | 27.7 |
| Home-care | 11.7 | 14.2 | 18.7 | 23.5 | 11.0 | 13.0 |
| Intermediate care or Skilled nursing facility | 13.5 | 13.6 | 20.1 | 20.8 | 27.2 | 23.5 |
SD, standard deviation; AMI, acute myocardial infarction; TIA, transient ischemic attack. Select other comorbidities are shown.
Medicare beneficiaries with acute myocardial infarction at rural hospitals, compared with urban hospitals, were older (mean [SD] age, 77.8 [8.8] vs. 77.1 [8.7] years), more likely to be female (45.4% vs. 43.5%), more likely to be White (90.6% vs. 84.1%), and less likely to be Black adults (4.7% vs. 8.6%) (Table 1). These patterns were similar for patients with heart failure and ischemic stroke. Clinical comorbidities for patients at rural vs. urban sites are also shown in Table 1.
Treatment Patterns
Medicare beneficiaries at rural hospitals were less likely to receive procedural care than those in urban areas. For acute myocardial infarction, beneficiaries admitted to rural hospitals were less likely to undergo cardiac catheterization (49.7% vs. 63.6%, p<0.001), PCI (42.1% vs. 45.7%, p<0.001) and/or CABG (9.0% vs. 10.2%, p<0.001) within 30 days of initial presentation. Among beneficiaries with ischemic stroke, those at rural hospitals were less likely to undergo thrombolysis (3.1% vs. 10.1%, p<0.001) and endovascular therapy (1.8% vs. 3.6%, p<0.001) (Central Figure A, B).
Central Figure.
Observed Procedure and Mortality Rates for Acute Cardiovascular Conditions at Rural vs. Urban Hospitals
A. Procedures for Acute Myocardial Infarction
B. Procedures for Ischemic Stroke
C. 30-Day Mortality Rates
D. 90-Day Mortality Rates
Observed Procedure and Mortality Rates for Acute Cardiovascular Conditions at Rural vs. Urban Hospitals. (A) Procedure rates for acute myocardial infarction, (B) Procedure rates for ischemic stroke, (C) 30-day morality rates, and (D) 90-day mortality rates among Medicare beneficiaries age 65 years or older at rural (blue) vs. urban (red) hospitals are shown in the figure above. Procedures for acute myocardial infarction that were performed within 30-days of initial presentation were included in order to capture care that may have been delivered after transfer to another hospital. Procedure rates for acute myocardial infarction and ischemic stroke were higher at urban hospitals compared to rural hospitals. Observed 30- and 90-day mortality rates were higher at rural hospitals compared to urban hospitals.
30- and 90-Day Mortality
Observed mortality rates within 30 days of initial presentation was higher among beneficiaries at rural (vs. urban) hospitals for all three cardiovascular conditions (acute myocardial infarction 12.9% vs. 11.6%, p<0.001; heart failure 11.1% vs. 9.8%, p<0.001; ischemic stroke 14.9% vs. 13.1%, p<0.001). These patterns were similar for 90-day mortality (acute myocardial infarction 17.9% vs. 16.2%, p<0.001; heart failure 20.6% vs. 19.0%, p<0.001; ischemic stroke 20.5% vs. 18.5%, p<0.001) (Central Figure C, D and eTable 3A).
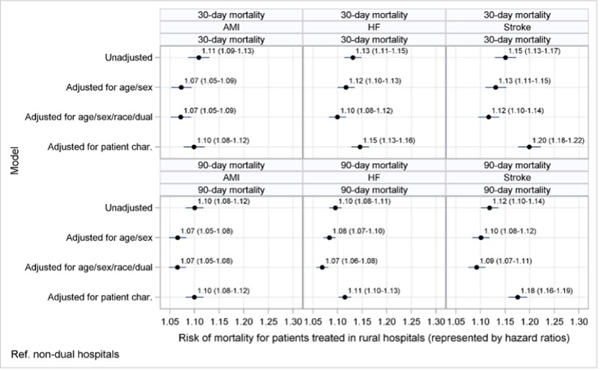
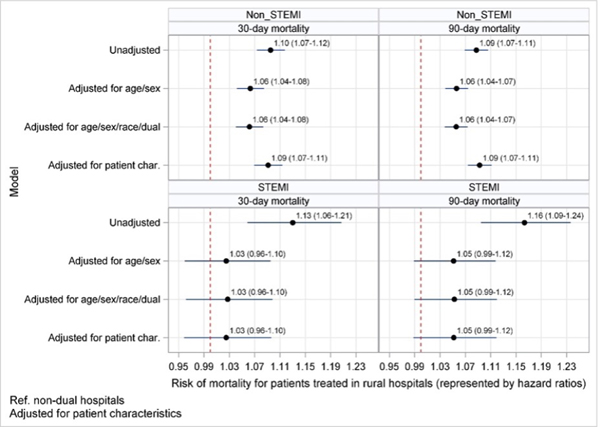
After adjusting for demographics (age, sex, race, and poverty) and clinical comorbidities, mortality at 30 days among patients presenting to a rural hospital with acute myocardial infarction was higher than those at urban hospitals (hazard ratio [HR] 1.10, 95% confidence interval [CI] 1.08–1.12) (Figure 1A). Among those presenting with non-STEMI, 30-day mortality was higher at rural hospitals (HR 1.09, 95% CI 1.07–1.11). However, 30-day mortality for patients presenting with STEMI was similar at both rural and urban hospitals (HR 1.03, 95% CI 0.96–1.10) (Figure 1B). Thirty-day mortality was also higher for patients with heart failure at rural vs. urban hospitals (HR 1.15, 95% CI 1.13–1.16). However, 30-day all-cause readmission rates after a heart failure hospitalization did not differ between these sites (HR 0.99, 95% CI 0.98–1.00). Among those with ischemic stroke, 30-day mortality was higher at rural sites (HR 1.20, 95% CI 1.18–1.22). Mortality at 90 days was higher for all three cardiovascular conditions for beneficiaries at rural hospitals (acute myocardial infarction, HR 1.10, 95% CI 1.08–1.12; heart failure, HR 1.11, 95% CI 1.10–1.13; ischemic stroke, HR 1.18; 95% CI 1.16–1.19) (Figure 1A). The addition of hospital resource variables and procedure rates to our models did not significantly attenuate the observed association for acute myocardial infarction (30-day HR 1.08, 95% CI 1.06–1.10; 90-day HR 1.08, 95% CI 1.06–1.10) or ischemic stroke (30-day HR 1.19, 95% CI 1.16–1.21; 90-day HR 1.16, 95% CI 1.14–1.18). Across most conditions and outcomes, the interaction between race, site of presentation, and outcomes was significant (eTable 4). Additionally, in our sensitivity analysis that excluded patients who were transferred in or out of a hospital, mortality patterns were similar for all conditions (eFigure 1).
Figure 1.
Mortality Among Older Adults with Cardiovascular Conditions at Rural vs. Urban Hospitals
A. Acute Myocardial Infarction, Heart Failure, Ischemic Stroke
B. Non-STEMI and STEMI
Mortality Among Older Adults at Rural vs. Urban Hospitals for Cardiovascular Conditions. Hazard ratios for mortality among older adults at rural vs. urban Hospitals for (A) acute myocardial infarction, heart failure, ischemic stroke and (B) non-STEMI and STEMI. The figures show multivariable adjusted hazard ratios (with 95% confidence intervals) for mortality at 30- and 90-days among Medicare beneficiaries 65 years or older with acute cardiovascular conditions whom initially presented to a rural hospital compared with those at urban hospitals (reference group). Cox proportional hazards models adjusted for age, sex, race, dual enrollment, and clinical comorbidities. When compared to urban hospitals, 30- and 90-day mortality at rural hospitals was higher for all conditions (except STEMI).
Geographic Variation
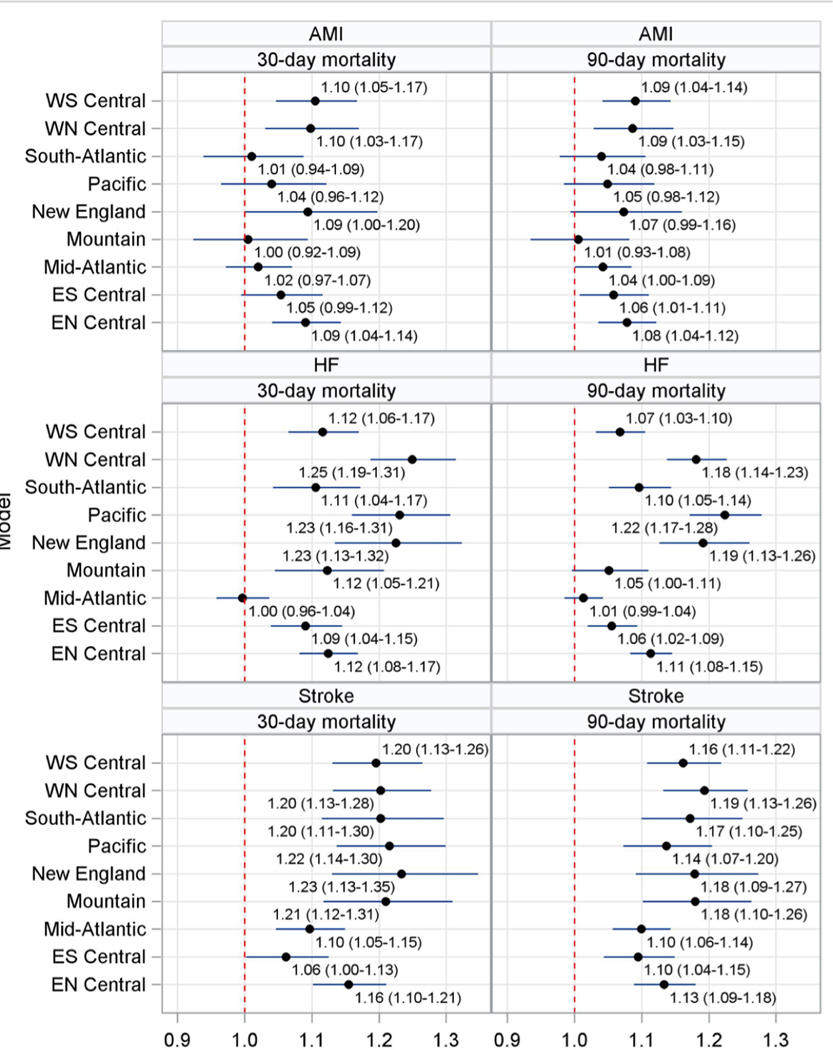
The rural-urban gap in 30- and 90-day risk-adjusted mortality varied across US Census Bureau regions (Figure 2). Mortality rates for acute myocardial infarction were higher at rural compared with urban hospitals in several regions, but similar in the New England, Mid-Atlantic, South-Atlantic, Mountain, and East South-Central regions. For ischemic stroke, mortality rates at rural hospitals were higher than at urban hospitals in all US regions. For heart failure, rural mortality was higher in all regions except the Mid-Atlantic.
Figure 2. Mortality Among Older Adults with Cardiovascular Conditions at Rural vs. Urban Hospitals across U.S. Regions.
Mortality Among Older Adults with Cardiovascular Conditions at Rural vs. Urban Hospitals across U.S. Regions. The figure shows multivariable adjusted hazard ratios (with 95% confidence intervals) for mortality at 30 and 90 days among Medicare beneficiaries age 65 years or older with acute cardiovascular conditions (acute myocardial infarction, heart failure, ischemic stroke) at rural hospitals compared with those at urban hospitals (reference group) by U.S. Census Bureau Regions. Cox proportional hazards models adjusted for age, sex, race, dual enrollment, and clinical comorbidities. The West North Central region (Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota and South Dakota) generally had the largest rural-urban gap in 30 and 90-day mortality rates for all three cardiovascular conditions.
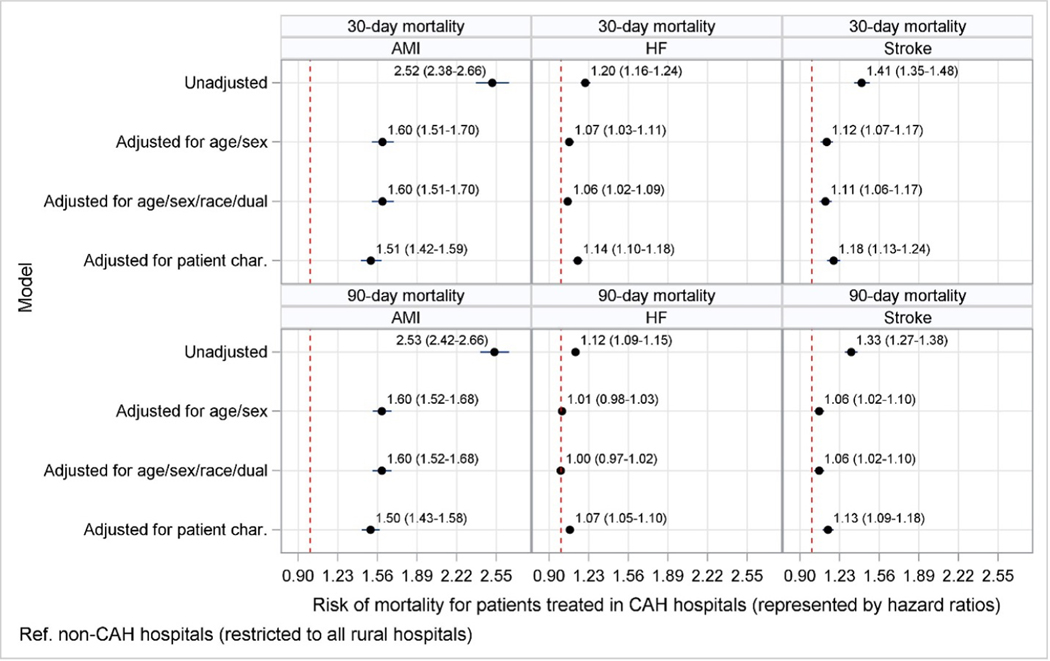
Critical Access vs. Non-Critical Access Hospitals in Rural Areas
Of the 2,113 rural hospitals, 1,331 were critical access and 782 were non-critical-access sites. Medicare beneficiaries with acute myocardial infarction at critical access hospitals, compared with those at non-critical access hospitals, were substantially less likely to undergo PCI/CABG within 30 days (3.7% vs. 53.6%, p<0.001). Similarly, patients hospitalized for ischemic stroke at critical access sites were less likely to receive thrombolysis and/or endovascular therapy (0.36% vs. 5.4%, p<0.001) (eFigure 2). There were substantial differences in observed 30-day mortality rates between critical access and non-critical access hospitals for acute myocardial infarction (27.6% vs. 12.1%, p<0.001), heart failure (12.6% vs. 10.7%, p<0.001), and ischemic stroke (19.4% vs. 14.3%, p<0.001) (eTable 3B). After risk-adjustment (age, sex, race, and poverty, clinical comorbidities), the hazard ratio for mortality at 30 days was higher among patients at critical access sites across all 3 conditions (acute myocardial infarction, HR 1.31, 95% CI 1.231.40; heart failure, HR 1.12, 95% CI 1.08–1.17; ischemic stroke, HR 1.17, 95% CI 1.11–1.24) (Figure 3). These patterns were similar at 90 days.
Figure 3. Mortality at Critical Access vs. Non-Critical Access Rural Hospitals.
Mortality at Critical Access vs. Non-Critical Access Rural Hospitals. The figure shows multivariable adjusted hazard ratios (with 95% confidence intervals) for mortality at 30 and 90 days among Medicare beneficiaries age 65 years or older with acute cardiovascular conditions whom initially presented to a critical access hospital compared to those at non-critical access hospitals (reference group) in rural areas. Cox proportional hazards models adjusted for age, sex, race, dual enrollment, and clinical comorbidities. Thirty and ninety-day mortality were higher at critical access rural hospitals than non-critical access rural hospitals for all acute cardiovascular conditions. Among patients presenting to critical access rural hospitals for AMI, HF, and stroke, 13.9%, 25.4%, and 21.1% were transferred to another hospital, while at non-critical access rural hospitals, 5.4%, 18.5%, and 12.5% of patients were transferred, respectively.
Discussion
In this national study of Medicare beneficiaries age 65 years or older with acute myocardial infarction, heart failure, and ischemic stroke, mortality at 30 and 90 days was significantly higher among those presenting to rural hospitals compared to those at urban hospitals. Patients at rural sites were less likely to receive important treatments, such as thrombolysis or endovascular treatment for ischemic stroke. In addition, there was marked geographic variation in the rural-urban gap in mortality for cardiovascular conditions across the US.
Despite significant public health and policy efforts to reduce rural-urban health inequities, our findings highlight that large gaps in clinical outcomes for acute cardiovascular conditions remain in the United States. Early studies of the Medicare population, prior to 2010, reported lower quality of care and higher 30-day mortality rates for cardiovascular conditions in rural compared with urban areas. (4–8) Although the federal government has implemented rural initiatives that aim to improve the delivery and quality of care, rural hospitals closures have increased over the last decade. (19, 32, 33) As a result, rural adults increasingly face challenges in accessing hospital care, including longer travel times and delays in emergency medical services and treatment, which adversely affect outcomes for emergent conditions. (11, 20, 21, 34) Our finding that rural-urban disparities varied markedly across U.S. regions indicates that geographically-targeted, public health strategies may be needed to improve care delivery for acute cardiovascular conditions in rural areas.
We also found differences in the intensity of care at rural vs. urban hospitals. Despite substantial investment in the development of stroke systems of care and the growth in telemedicine services that provide rapid access to stroke specialists, rates of thrombolysis and endovascular therapy for ischemic stroke were markedly lower at rural sites, consistent with recent studies. (17, 35–38) These findings may reflect rural-urban gaps in tele-stroke services, secondary to financial constraints, lack of high-speed internet, and regulatory barriers. (35, 36, 39) Previous studies have found that small, rural, and critical access hospitals, which are the most likely to benefit from telestroke capabilities, and less likely to offer these services. (35, 40, 41) Interestingly however, these treatment differences did not explain the rural-urban gap in stroke mortality. One potential explanation for this finding is that patients who present to rural hospitals with stroke may be more likely to be ineligible for these treatments. It is also possible that these treatment gaps meaningfully impact outcomes not measured in our study, including morbidity, functional status, and disability. Although we found that patients presenting to rural hospitals were also less likely to undergo revascularization within 30 days of admission than those at urban hospitals, the absolute difference was small (PCI 42% vs. 46%). Interestingly, STEMI mortality rates did not significantly differ among those initially presenting to rural compared with urban hospitals rural hospitals; however, non-STEMI mortality rates were higher at rural hospitals. Collectively, these findings suggest that concerted public health initiatives, such as the implementation of region systems of care, have likely helped facilitate the timely transfer of patients with STEMI from rural hospitals to those with PCI/CABG capabilities. (40) These advances have likely been counterbalanced by the rise in rural hospital closures, which have led to delays in access to time-sensitive procedural care for patients with myocardial infarction, and contributed to higher mortality rates. (18, 42)
Within rural areas, we observed stark differences in care between critical access sites that serve remote communities compared with non-critical access rural hospitals. For example, less than 5% of patients hospitalized with acute myocardial infarction at critical access rural sites underwent revascularization within 30 days, compared with nearly one-half of those hospitalized at non-critical access rural sites. These disparities were even more pronounced for ischemic stroke. Perhaps due to these differences in treatment, mortality rates were markedly worse at critical access hospitals. Our findings parallel studies of critical access hospitals prior to 2010, and suggest that no progress has been made in improving outcomes for urgent cardiovascular conditions at these sites over the last decade. (4–6) Greater policy attention is needed to increase resources and improve quality of care at critical access hospitals, which provide much-needed access to care for many rural Americans.
Beyond inpatient care, patients hospitalized with acute cardiovascular conditions often benefit from close follow-up and care during the vulnerable period after discharge. Post-acute care facilities located in rural areas may provide lower quality of care compared to those in urban areas, and rural patients may face barriers in accessing other important types of care, such as cardiac rehabilitation. (15, 43) In addition, rural areas have experienced a decline in primary care physicians and specialists, which may make access to follow-up care after discharge more difficult. (13, 44) These challenges, coupled with worse access to cardiac rehabilitation and important rehabilitative services after stroke may contribute to worse outcomes in rural areas and may disproportionally impact minorities. (11, 14, 15, 45)
This study has several limitations. First, our analysis focused on the Medicare fee-for-service population and did not include beneficiaries enrolled in Medicare Advantage, who comprise one-third of the Medicare population. As national claims data for the Medicare Advantage enrollees become increasingly available, understanding rural-urban care for this population will be an important area for future research. Second, we used administrative claims data, which do not include detailed information about laboratory values, vital signs, and medical therapy during hospitalization. These data could provide additional insights on why mortality rates are higher in rural areas. Third, because we rely on claims data for risk-adjustment, it is possible that unmeasured clinical factors (e.g., blood pressures at time of admission, frailty) contribute, at least in part, to differences in outcomes between rural and urban hospitals. Fourth, recent evidence suggest that critical access hospitals submit fewer inpatient codes than other hospitals, which may affect comparisons of outcomes. (46) However, we used a comprehensive approach to risk-adjustment that included hospital diagnoses codes and pre-existing comorbidities ascertained from both inpatient and outpatient visits during the prior year. Fifth, our study does not account for patient preferences. It is possible that some beneficiaries initially seen at rural hospitals elected to not be transferred to an urban hospital for procedural care. Sixth, we used the 2010 Rural-Urban Commuting Area Codes to identify rural and urban areas and were unable to account for minor urbanization or de-urbanization that may have occurred after this time period.
Conclusions
In the United States, older adults presenting to rural hospitals with urgent cardiovascular conditions (acute myocardial infarction, heart failure, and ischemic stroke) were less likely to receive important therapeutic procedures and experienced higher 30- and 90-day mortality rates than their urban counterparts. Procedure rates were substantially lower and mortality rates much worse at the subset of critical access hospitals that serve remote, rural communities. In addition, there was marked geographic variation in rural-urban disparities for cardiovascular conditions across the US. Despite efforts to improve rural healthcare in the US, our findings suggest that large gaps in care delivery and outcomes for acute myocardial infarction, heart failure, and ischemic stroke remain.
Supplementary Material
Perspectives.
Competency in Systems-Based Practice:
Older adults presenting to rural hospitals with acute myocardial infarction, decompensated heart failure, or ischemic stroke are less likely to receive therapeutic interventions and experience higher 30- and 90-day mortality rates than those managed in urban facilities. There is marked geographic variation across the nation in rural-urban disparities for patients with these acute cardiovascular conditions.
Translational Outlook:
Policy changes and clinical efforts are urgently needed to reduce rural-urban inequities in care for patients with acute cardiovascular conditions.
Acknowledgments
Disclosures:
Dr. Emefah Loccoh receives research support from the Sarnoff Cardiovascular Research Fellowship. Dr. Joynt Maddox receives research support from the National Heart, Lung, and Blood Institute (R01HL143421) and National Institute on Aging (R01AG060935). Dr. Yeh receives research support from the National Heart, Lung and Blood Institute (R01HL136708 and R01HL157530) and the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology and receives personal fees from Biosense Webster, grants and personal fees from Abbott Vascular, AstraZeneca, Boston Scientific, and Medtronic, outside the submitted work.
Dr. Wadhera receives research support from the National Heart, Lung, and Blood Institute (K23HL148525) at the National Institutes of Health. He currently serves as a consultant for Abbott, outside the submitted work. All other authors have no disclosures.
Funding:
National Heart, Lung, and Blood Institute (K23HL148525) at the National Institutes of Health.
Role of the Funder/Sponsor:
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations:
- CABG
coronary artery bypass grafting
- PCI
percutaneous coronary intervention
- CCW
chronic conditions data warehouse
- RUCA
rural-urban commuting area
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Garcia MC, Faul M, Massetti G, et al. Reducing potentially excess deaths from the five leading causes of death in the rural United States. MMWR Surveill. Summ 2017;66:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cross SH, Mehra MR, Bhatt DL, et al. Rural-urban differences in cardiovascular mortality in the US, 1999–2017. JAMA 2020;323:1852–1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrington RA, Califf RM, Balamurugan A, et al. Call to action: rural health: a presidential advisory from the American Heart Association and American Stroke Association. Circulation 2020;141:e615–e644. [DOI] [PubMed] [Google Scholar]
- 4.Joynt KE, Harris Y, Orav EJ, Jha AK. Quality of care and patient outcomes in critical access rural hospitals. Jama 2011;306:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. 30-Day risk-standardized mortality and readmission rates after ischemic stroke in critical access hospitals. Stroke 2012; 43:2741–2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joynt KE, Orav EJ, Jha AK. Mortality rates for medicare beneficiaries admitted to critical access and non–critical access hospitals, 2002–2010. JAMA 2013;309:1379–1387. [DOI] [PubMed] [Google Scholar]
- 7.Sheikh K, Bullock C. Urban-rural differences in the quality of care for Medicare patients with acute myocardial infarction. Arch. Intern. Med 2001;161:737–743. [DOI] [PubMed] [Google Scholar]
- 8.Baldwin L-M, Chan L, Andrilla CHA, Huff ED, Hart LG. Quality of care for myocardial infarction in rural and urban hospitals. J. Rural Health 2010;26:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah NS, Carnethon M, Lloyd-Jones DM, Khan SS. Widening rural-urban Cardiometabolic mortality gap in the United States, 1999 to 2017. J. Am. Coll. Cardiol 2020;75:3187–3188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nambiar L, LeWinter MM, VanBuren PC, Dauerman HL. Decade-long temporal trends in US hypertension-related cardiovascular mortality. J. Am. Coll. Cardiol 2020;75:2644–2646. [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal R, Chiu N, Loccoh EC, Kazi DS, Yeh RW, Wadhera RK. Rural-Urban Disparities: Diabetes, Hypertension, Heart Disease, and Stroke Mortality Among Black and White Adults, 1999–2018. J Am. Coll. Cardiol 2021:77:1480–1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cross SH, Califf RM, Warraich HJ. Rural-Urban Disparity in Mortality in the US From 1999 to 2019. JAMA 2021;325:2312–2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern. Med 2019;179:506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burke RE, Jones CD, Coleman EA, Falvey JR, Stevens-Lapsley JE, Ginde AA. Use of post-acute care after hospital discharge in urban and rural hospitals. Am. J. Accountable Care 2017;5:16. [PMC free article] [PubMed] [Google Scholar]
- 15.Valencia HE, Savage PD, Ades PA. Cardiac rehabilitation participation in underserved populations. J. Cardiopulm. Rehabil. Prev 2011;31:203–210. [DOI] [PubMed] [Google Scholar]
- 16.Jollis JG, Al-Khalidi HR, Roettig ML, et al. Regional systems of care demonstration project: American Heart Association Mission: lifeline STEMI systems accelerator. Circulation 2016;134:365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song S, Saver J. Growth of regional acute stroke systems of care in the United States in the first decade of the 21st century. Stroke 2012;43:1975–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gujral K, Basu A. Impact of rural and urban hospital closures on inpatient mortality. National Bureau of Economic Research; 2019. [Google Scholar]
- 19.174 Rural hospital closures: January 2005–present (132 since 2010)—Sheps Center. 2020. Available at: https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospitalclosures/
- 20.Miller KE, James HJ, Holmes GM, Van Houtven CH. The effect of rural hospital closures on emergency medical service response and transport times. Health Serv. Res 2020;55:288–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCarthy S, Moore D, Smedley WA, et al. Impact of Rural Hospital Closures on Health-Care Access. J. Surg. Res 2021;258:170–178. [DOI] [PubMed] [Google Scholar]
- 22.Mortality Measures Methodology. Available at: https://qualitynet.cms.gov/inpatient/measures/mortality/methodology. Accessed September 21, 2021.
- 23.Wadhera RK, Wang Y, Figueroa JF, Dominici F, Yeh RW, Maddox KEJ. Mortality and hospitalizations for dually enrolled and nondually enrolled Medicare beneficiaries aged 65 years or older, 2004 to 2017. Jama 2020;323:961–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med. Care 1998:8–27. [DOI] [PubMed] [Google Scholar]
- 25.Chronic Conditions Data Warehouse. Available at: https://www2.ccwdata.org/web/guest/home/. Accessed September 21, 2021.
- 26.Version 2.0 Rural-Urban Commuting Areas (RUCAs) Code Descriptions. Available at: https://depts.washington.edu/uwruca/RUCACodeDes2.pdf.
- 27.Redmond N, Richman J, Gamboa CM, et al. Perceived stress is associated with incident coronary heart disease and all cause mortality in low but not high income participants in the Reasons for Geographic and Racial Differences in Stroke Study. J. Am. Heart Assoc 2013;2: e000447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilcock AD, Zachrison KS, Schwamm LH, Uscher-Pines L, Zubizarreta JR, Mehrotra A. Trends among rural and urban Medicare beneficiaries in care delivery and outcomes for acute stroke and transient ischemic attacks, 2008–2017. JAMA Neurol. 2020;77:863–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc 1999;94:496–509. [Google Scholar]
- 30.Bennett KJ, Probst JC, Bullard JC, Crouch E. The importance of rural hospitals: transfers and 30-day readmissions among rural residents and patients presenting at rural hospitals. Popul. Health Manag 2019;22:120–126. [DOI] [PubMed] [Google Scholar]
- 31.Critical Access Hospitals (CAHs) Overview - Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/topics/critical-access-hospitals. Accessed September 21, 2021.
- 32.Rural Health Council | CMS. Available at: https://www.cms.gov/About-CMS/AgencyInformation/OMH/equity-initiatives/rural-health/rural-health-council. Accessed September 21, 2021.
- 33.Rural Community Hospital Demonstration | CMS Innovation Center. Available at: https://innovation.cms.gov/innovation-models/rural-community-hospital. Accessed September 21, 2021.
- 34.O’Hanlon CE, Kranz AM, DeYoreo M, Mahmud A, Damberg CL, Timbie J. Access, Quality, And Financial Performance Of Rural Hospitals Following Health System Affiliation. Health Aff. Proj. Hope 2019;38:2095–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Richard JV, Wilcock AD, Schwamm LH, et al. Assessment of telestroke capacity in US hospitals. JAMA Neurol. 2020;77:1035–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Silva GS, Farrell S, Shandra E, Viswanathan A, Schwamm LH. The status of telestroke in the United States: a survey of currently active stroke telemedicine programs. Stroke 2012;43:2078–2085. [DOI] [PubMed] [Google Scholar]
- 37.Gorelick PB. Primary and comprehensive stroke centers: history, value and certification criteria. J. Stroke 2013;15:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hammond G, Luke AA, Elson L, Towfighi A, Joynt Maddox KE. Urban-rural inequities in acute stroke care and in-hospital mortality. Stroke 2020;51:2131–2138. [DOI] [PubMed] [Google Scholar]
- 39.Zachrison KS, Richard JV, Mehrotra A. Paying for Telemedicine in Smaller Rural Hospitals: Extending the Technology to Those Who Benefit Most. In: JAMA Health Forum.Vol 2. American Medical Association, 2021:e211570–e211570. [DOI] [PubMed] [Google Scholar]
- 40.Jacobs AK. Regional systems of care for patients with ST-elevation myocardial infarction: being at the right place at the right time. Am Heart Assoc; 2007. [DOI] [PubMed] [Google Scholar]
- 41.Wilcock AD, Schwamm LH, Zubizarreta JR, et al. Reperfusion treatment and stroke outcomes in hospitals with telestroke capacity. JAMA Neurol. 2021;78:527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramesh T, Gee E. Rural Hospital Closures Reduce Access to Emergency Care. Cent. Am. Prog. Wash, DC 2019. [Google Scholar]
- 43.Kosar CM, Loomer L, Ferdows NB, Trivedi AN, Panagiotou OA, Rahman M. Assessment of rural-urban differences in postacute care utilization and outcomes among older US adults. JAMA Netw. Open 2020;3:e1918738–e1918738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnston KJ, Wen H, Joynt Maddox KE. Lack of access to specialists associated with mortality and preventable hospitalizations of rural Medicare beneficiaries. Health Aff. (Millwood) 2019;38:1993–2002 [DOI] [PubMed] [Google Scholar]
- 45.Koifman J, Hall R, Li S, et al. The association between rural residence and stroke care and outcomes. J. Neurol. Sci 2016;363:16–20. [DOI] [PubMed] [Google Scholar]
- 46.Kosar CM, Loomer L, Thomas KS, White EM, Panagiotou OA, Rahman M. Association of Diagnosis Coding With Differences in Risk-Adjusted Short-term Mortality Between Critical Access and Non–Critical Access Hospitals. Jama 2020;324:481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.