Abstract
Mechanical ventilation (MV) is an essential life support method for patients with acute respiratory distress syndrome (ARDS), which is one of the most common critical illnesses with high mortality in the intensive care unit (ICU). A lung-protective ventilation strategy based on low tidal volume (LTV) has been recommended since a few years; however, as this did not result in a significant decrease of ARDS-related mortality, a more optimal ventilation mode was required. Airway pressure release ventilation (APRV) is an old method defined as a continuous positive airway pressure (CPAP) with a brief intermittent release phase based on the open lung concept; it also perfectly fits the ARDS treatment principle. Despite this, APRV has not been widely used in the past, rather only as a rescue measure for ARDS patients who are difficult to oxygenate. Over recent years, with an increased understanding of the pathophysiology of ARDS, APRV has been reproposed to improve patient prognosis. Nevertheless, this mode is still not routinely used in ARDS patients given its vague definition and complexity. Consequently, in this paper, we summarize the studies that used APRV in ARDS, including adults, children, and animals, to illustrate the settings of parameters, effectiveness in the population, safety (especially in children), incidence, and mechanism of ventilator-induced lung injury (VILI) and effects on extrapulmonary organs. Finally, we found that APRV is likely associated with improvement in ARDS outcomes, and does not increase injury to the lungs and other organs, thereby indicating that personalized APRV settings may be the new hope for ARDS treatment.
Keywords: Acute respiratory distress syndrome, Airway pressure release ventilation, Ventilator-induced lung injury, Outcome, Organ protection
Introduction
Mechanical ventilation (MV) is an essential life support approach used for patients with acute respiratory distress syndrome (ARDS).[1] However, it may potentiate lung damage due to regional alveolar overstretch and/or repetitive alveolar collapse with shearing (atelectrauma).[2] The low tidal volume (LTV) ventilation strategy was developed 20 years ago; since then, many MV strategies have aimed to reduce ventilator-induced lung injury (VILI) and assumed that alveoli behave elastically, up to an elastic load limit, based on the elastin/collagen interaction.[3], [4] However, alveoli actually behave as a viscoelastic system, where alveolar recruitment and collapse depend not only on the amount of pressure applied to the lung but also on the time during which the pressure is applied, especially during lung injury.[5], [6]
Based on the above knowledge, airway pressure release ventilation (APRV), first described in 1987 by Stock et al.,[7] is defined as a continuous positive airway pressure (CPAP) with a brief intermittent release phase, allowing the release of only partial lung volume and spontaneous breathing (SB) throughout the high level of pressure,[7], [8] where the user can independently control inspiratory and expiratory time, and is based on the open lung concept.[9], [10] Despite its theoretically attractive advantages over other conventional MV modes, APRV is not routinely used in daily clinical practice but rather only used in patients with acute lung injury (ALI)/ARDS as rescue therapy.[11] Because the methodologies of APRV vary greatly and the conclusions from related studies are still controversial, we tried to explain the rationale of APRV, and update the application of APRV in ARDS and summarize its effects on other organs.
Definition and Rationale of APRV
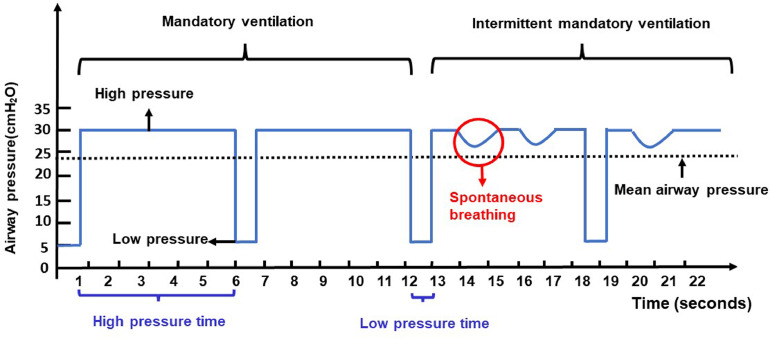
The original definition of APRV includes simple CPAP with a brief release to low-level positive end-expiratory pressure (PEEP).[7] It is characterized by the application of an inverse inspiratory–expiratory (I:E) ratio.[12] Based on the definition, APRV has four basic parameters, namely: high-level pressure (the pressure of CPAP, Phigh); low-level pressure (PEEP or Plow); high-pressure time (Thigh); and low-pressure time (Tlow), where Thigh and Tlow form a respiratory cycle. As such, both mandatory breath and spontaneous breath are allowed, and SB can occur at Phigh and Plow [Figure 1]. Oxygenation is mainly determined by Phigh, Thigh, and the fraction of inspired oxygen (FiO2). Ventilation is determined by the frequency with which Phigh releases to Plow, the gap between Phigh and Plow, and the proportion of SB.[8], [13]
Figure 1.
Pressure (longitudinal axis) and time (horizontal axis) curve in APRV. Two mandatory breaths (without SB, switched by time) and two intermittent mandatory breaths (with SB, triggered by flow or pressure, switched by both time and SB) are shown. Black arrows represent high pressure (Phigh), low pressure (Plow), and mean airway pressure (Pmean). Red arrow represents SB. Blue fontin the horizontal axis represents high pressure time (Thigh) and low-pressure time (Tlow).
APRV: Airway pressure release ventilation; SB: Spontaneous breathing.
In some studies, APRV is called biphasic positive airway pressure ventilation (BIPAP); however, these two are distinct. APRV and BIPAP are time-triggered, pressure-limited, and time-cycled and allow unrestricted SB both during and between mandatory breaths, thus benefiting from active inhalation and exhalation servo valves. The biggest difference between these two modes is the I:E ratio.[13], [14] APRV typically uses various time ratios for Thigh and Tlow ranging from 1:1 to 9:1, with the most common being inverse I:E ratios, while this is not the case for BIPAP.[14] Furthermore, Tlow is usually controlled within 1.5 s, even <0.65 s in APRV mode, but there is no limit in BIPAP.[14], [15]
Application of APRV in ARDS
ARDS is a serious clinical condition with a high incidence and mortality, characterized by an increased permeability of the alveolar-capillary barrier.[16] The current understanding of the lung-protective ventilation strategy to minimize VILI is to “open the lung and keep it open”.[17], [18] Usually, the open lung concept consists of recruitment maneuvers (RMs) for re-inflating the collapsed lung tissue, and a high PEEP for keeping the lung open and avoiding cyclic opening and closing of alveoli to prevent injury.[19], [20], [21] Existing evidence has indicated that RMs combined with PEEP can improve oxygenation on the third day in ARDS patients and reduce the length of hospital stay. However, it has no beneficial effect on mortality.[22], [23] As previously mentioned, APRV is an open lung approach based on the principles of open lung strategy (OLS).
A prolonged inspiratory time of high pressure in APRV and nearly continuous RM provides an alternative open lung approach. Maintaining open lung pressure (Phigh) for a prolonged period promotes recruitment of slowly opening alveoli and gives unstable lung units enough time to fill and balance the volume due to the collateral ventilation.[24] In addition, Tlow is also an important reason for preventing alveolar collapse in some studies, where Tlow was even reduced to as little as 0.2 s.[25] The short release terminates expiratory flow early, permitting only partial discharge of lung capacity, thus causing auto-PEEP and preventing instability.[24] Consequently, APRV is considered an alternative, life-saving approach in patients with ARDS.
APRV in adults with ALI/ARDS
During the first few years of its use, APRV was not usually employed as a primary ventilation mode, but was considered an alternative approach for patients with ALI/ARDS refractory to conventional MV.[11] We reviewed the studies (case reports were not included) comparing APRV and conventional MV in adults with ALI/ARDS [Table 1]. Most were crossover studies (i.e., switching from assist/control ventilation [A/CV] or synchronized intermittent mandatory ventilation [SIMV] to APRV) and randomized controlled trials (RCTs) with a small sample size (from n = 22 to n = 138).[8], [26], [27], [28] However, the different studies used different settings, which indicate the inconsistency and complexity of ARPV. Most of the studies reported that APRV could improve oxygenation compared to other modes and showed that APRV could improve hemodynamics and respiratory system compliance, reduce peak inspiratory pressure (PIP), airway pressure, plateau pressure (Pplat), and the need for paralysis and sedation.[8], [29], [30], [31] No studies proved that APRV could improve the mortality of patients with ARDS; nevertheless, it was associated with a reduction of the duration of intensive care unit (ICU) stays and incidence of progression to extracorporeal membrane oxygenation (ECMO).[26], [31], [32], [33]
Table 1.
Application of ARPV in adults with ALI/ARDS.
| Authors | Year | Country | Study design | Comparison | Sample size | APRV settings |
Main findings and outcomes |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phigh | Thigh | Plow | Tlow | Oxygenation | Respiratory mechanics | Hemodynamics | VILI | Outcomes | ||||||
| Varpula et al.[43] | 2003 | Finland | RCT | APRV vs. SIMV-PC/PS | 45 | <35 cm H2O or UIP | Produce 12 pressure shifts per minute | Titrated according to PV-curve | Allow expiratory flow to decay to zero | Increased | Reduced Pplat | NA | NA | NA |
| Varpula et al.[78] | 2004 | Finland | RCT | APRV vs. SIMV-PC/PS | 58 | <35 cm H2O or UIP | 4.0 s | Titrated according to PV-curve | 1.0 s | Similar | Reduced inspiratory pressure | Similar | NA | Similar mortality andventilator free days |
| Li et al.[29] | 2016 | China | RCT | APRV vs. SIMV | 52 | 30 cm H2O | 4.0–8.0 s | 0 cm H2O | 0.4–0.8 s | Increased | Reduced PIP | Improved | Similar | Decreased the duration of MV and ICU stay, survival rate, and days without organ failure were similar |
| Song et al.[28] | 2016 | China | RCT | APRV vs. SIMV + PEEP | 22 | UIP | 4.0 s | LIP | 1.0 s | Increased | Increased Pmean | Similar | Might exacerbate VILI | NA |
| Zhou et al.[8] | 2017 | China | RCT | APRV vs. LTV | 138 | Pplat | RR:10–14/min | 5 cm H2O | ≥50% PEF | Increased | Reduced Pplat, improved respiratory compliance | Improved | Similar | Reduced the duration of MV and ICU stay |
| Liu et al.[32] | 2009 | Japan | Retrospective study | APRV vs. SIMV | 58 | 30–35 cm H2O | 2.5–3.5 s | 0 cm H2O | RR:12–15/min | Increased | NA | NA | Similar | A trend toward lower mortality in ICU |
| Yoshida et al.[79] | 2009 | Japan | Retrospective study | APRV vs. LTV | 18 | <30 cm H2O | 4 s | 0 cm H2O | 50–75% PEF | Increased | Similar | Improved | Decrease atelectasis | NA |
| Lim et al.[26] | 2016 | Australia | Retrospective study | APRV vs. CV | 50 | NA | NA | NA | NA | Increased | NA | NA | Decreased barotrauma | Reduced incidence of ECMO |
| Räsänen et al.[27] | 1991 | America | Crossover | APRV vs. CV | 50 | NA | NA | NA | 1.5 s | Similar | Reduced PIP | NA | NA | NA |
| Sydow et al.[80] | 1994 | Germany | Crossover | APRVvs. VC-IRV | 18 | 15–30 cm H2O | 2–4 s | 5 cm H2O | 0.5–0.7 s | Similar | Reduced PIP | NA | NA | NA |
| Kaplan et al.[30] | 2001 | America | Crossover | APRV vs. IRV-PCV | 12 | 75% PIP | 4.5 s | NA | 0.8 | Similar | Reduced PIP and Pmean | Improved | NA | NA |
| Dart et al.[81] | 2005 | America | Crossover | APRV vs. CV | 46 | Slight increase in the mean airway pressure | 3–4 s | 0 cm H2O | 40–50% PEF | Increased | Reduced PIP | NA | NA | NA |
| Rozé et al.[45] | 2017 | France | Case series | APRV + ECMO | 8 | ≤28 cm H2O | 1.0 s | ≥10 cm H2O | RR:12/min | NA | NA | NA | NA | May reduce the time under MV after ECMO |
| Lee et al.[44] | 2020 | Singapore | Case series | APRV + PP | 5 | NA | NA | NA | NA | Increased | NA | NA | NA | NA |
ALI: Acute lung injury; APRV: Airway pressure release ventilation; ARDS: Acute respiratory distress syndrome; CV: Conventional ventilation; ECMO: Extracorporeal membrane oxygenation; ICU: Intensive care unit; LIP: Lower inflection point; LTV: Low tidal volumeventilation; MV: Mechanical ventilation; MV: Mechanicalventilation; NA: Not available; PEEP: Positive end expiratory pressure; PEF: Peak expiratory flow; PEFR: Peak expiratory flow rate; Phigh: High pressure; PIP: Inspiratory peak pressure; Plow: Low pressure; Pmean: Mean airway pressure; PP: Prone position; Pplat: Platpressure; PV-curve: Pressure-volume curve; RCT: Randomized controlled study; RR: Releaserate; SIMV: Synchronized intermittent mandatory ventilation; SIMV-PC/PS: Synchronized intermittent mandatory ventilation-pressure control/pressure support; Thigh: High pressure time; Tlow: Low pressure time; UIP: Upper inflection point; VC-IRV: Volume control- inverse ratio ventilation; VILI: Ventilator induced lunginjury.
Whether coronavirus disease 2019 (COVID-19) infection is a typical manifestation of ARDS is still controversial,[34], [35], [36] but the main pathology of COVID-19 including cytokine storm and excessive inflammation is similar to traditional ARDS.[37], [38], [39] Recently, Mahmoud et al.[40] found that APRV may improve oxygenation, alveolar ventilation, and CO2 clearance in patients with COVID-19 and refractory hypoxemia. Moreover, Zorbas et al.[41] urged caution with the use of APRV in patients with COVID-19.
APRV combined prone position (PP)/ECMO in adults with ALI/ARDS
Research on combined APRV and PP has been limited to two case reports and one prospective RCT.[42], [43], [44] These studies reported that combining the two modalities resulted in a greater improvement in oxygenation. Varpula et al.[42] first discovered that APRV combined with the PP was feasible in the most severe ARDS, and a prospective RCT conducted 2 years later confirmed these results,[43] Lee et al.[44] reported five ARDS cases where APRV and PP were used and found that APRV could be safely used in the PP in a subtype of ARDS patients with improving oxygenation.
ECMO treatment for severe ARDS patients is also a current research focus, and there are few related studies on APRV MV mode under ECMO. Rozé et al.[45] reported eight cases of ARDS under ECMO, demonstrating that moderate SB with APRV was feasible while maintaining the tidal volume in an ultra-protective range without complications after ECMO.
APRV in children with ALI/ARDS
It is known that the philological characteristics of the respiratory system of adults and children are distinct.[46] Apart from considering the disease itself, the setting of the ventilator is always based on age, especially for children. Therefore, it is necessary to differentiate the use of APRV in children with ARDS. Although theoretically, APRV has many potential therapeutic benefits for pediatric ARDS patients, the safety concerns should be explored. Until 2020, the evidence for the application of APRV in children was insufficient; apart from a few retrospective studies and case reports, only one RCT compared LTV lung protective ventilation and APRV in children with ARDS [Table 2]. In 2001, Schultz et al.[47] compared APRV and SIMV for the treatment of pediatric ARDS and found that APRV provided similar ventilation, oxygenation, mean airway pressure, hemodynamics, and patient comfort as SIMV. Similarly, a recent RCT found that APRV was associated with a trend toward higher mortality than the conventional LTV.[48] However, because this study had unbalanced baseline characteristics and non-personalized initial parameter settings, its results are worthy of further verification.
Table 2.
Application of ARPV in children with ALI/ARDS.
| Authors | Year | Country | Study design | Comparison | Sample size | APRV settings |
Main findings and outcomes |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Phigh | Thigh | Plow | Tlow | Oxygenation | Respiratory mechanics | Hemodynamics | VILI | Outcome | ||||||
| Lalgudi et al.[48] | 2018 | India | RCT | APRV vs. LTV | 52 | 1–2 cm H2O above the Pplat (not to exceed 30 cm H2O) | 4 s | 0 cm H2O | Around 75% PEF | Increased | Increased Pmean | Similar | Similar | A trend toward higher mortality |
| Ning et al.[50] | 2020 | China | Retrospective study | APRV vs. HFOV | 47 | Pmean | NA | 0 cm H2O | 1/2–3/4 of PEF | NA | NA | NA | NA | Similar of survival |
| Schultz et al.[47] | 2001 | America | Crossover | APRV vs. SIMV | 15 | NA | NA | NA | NA | Similar | Reduced PIP and Pplat, Similar Pmean | Similar | NA | NA |
| Kamath et al.[82] | 2010 | America | Crossover | APRV vs. CV | 12 | Pplat or PIP | Higher than Tlow | PEEP | Higher than Tlow | Increased | Increased Pmean | Similar | NA | NA |
| Yehya et al.[51] | 2013 | America | Crossover | APRV vs. HFOV | 104 | Pmean | NA | 0 cm H2O | 50–75% PEF | NA | NA | NA | NA | Similar of survival |
| Yener and Udurgucu[83] | 2020 | Turkey | Crossover | APRV vs. CV | 30 | NA | NA | 0 cm H2O | Prevents end-expiratory pressure from reaching zero | Increased | Reduced PIP, increased Pmean | NA | NA | NA |
| Kawaguchi et al.[84] | 2015 | Japan | Case series | APRV | 13 | Pplat | 3.0–5.0 s | 0 cm H2O | 0.2–0.6 s | Similar | Increased Pmean | Similar | NA | NA |
ALI: Acute lung injury; APRV: Airway Pressure Release Ventilation; ARDS: Acute respiratory distress syndrome; CV: Conventional ventilation; HFOV: High frequency oscillatory ventilation; LTV: Low tidal volume; NA: Not available; PEEP: Positive end expiratory pressure; PEF: Peak expiratory flow; PEFR: Peak expiratory flow rate; Phigh: High pressure; PIP: Inspiratory peak pressure; Plow: Low pressure; Pmean: Mean airway pressure; Pplat: Platpressure; RCT: Randomized controlled study; SIMV: Synchronized intermittent mandatory ventilation; Thigh: High pressure time; Tlow: Low pressure time; VILI: Ventilator induced lung injury.
High-frequency oscillatory ventilation (HFOV), which was first developed to treat respiratory distress syndrome in neonates, is considered a very effective treatment in children with ARDS.[49] Ning et al.[50] retrospectively compared HFOV and APRV in the treatment of patients with moderate-to-severe ARDS and found that oxygenation at 48 h was improved with HFOV and APRV application, but no significant difference in the survival rates was noted in either group; this finding was consistent with that of Yehya et al.[51]'s study. Hence, more studies are needed to illustrate the therapeutic effect and safety for pediatric patients.
APRV in animal models with ALI/ARDS
Since 2000, 32 animal studies on APRV reported parameter setting and lung injury comparison with conventional ventilation (CV) modes, including 20 swine models, 5 rat models, 3 dog models, and 1 rabbit model [Supplementary Table 1]. There are three common methods for ARDS model establishment: (1) oleic acid injection, (2) saline lung lavage, and (3) ischemia-reperfusion and peritoneal sepsis. Most studies indicated that SB during APRV can improve oxygenation, decreases respiratory work, and redistribute ventilation to the dependent lung area, thereby reducing VILI.[52], [53], [54], [55], [56], [57], [58] Most studies compared CV modes and APRV in the animal ALI model and found that APRV had lower lung injury histological scores and could reduce cytokine mRNA expressions in lung tissue and reduce tumor necrosis factor (TNF)-a, interleukin (IL)−8, and IL-6 in the bronchoalveolar lavage fluid (BALF).[56], [58], [59], [60] Moreover, APRV was reported to preserve surfactant concentrations of proteins A and B, which were associated with a lower incidence of basilar collapse.[61], [62]
APRV and VILI
Although various lung-protective ventilation strategies such as LTV and high PEEP or respiratory physiological guiding titration of PEEP (also known as optimal PEEP) or combining lung recruitment maneuver have been developed in recent years, it is still difficult to prevent VILI.[63] Moreover, because alveolar volume change is viscoelastic in nature, there is a time lag between the time point of the airway pressure applied or removed and the time point at which alveoli open or collapse.[64] These data indicated that to minimize VILI, the MV strategies must open and stabilize the lung by appropriately applying the pressure/time profile. A few experiments with the expiratory time titrated to target end-expiration at 75% of the peak expiratory flow (PEF) in APRV demonstrated high effectiveness by recruiting/stabilizing alveoli and preventing VILI.[54], [61], [62], [65]
Only a few studies have focused on VILI in humans; the majority of them have been conducted on animals. Roy et al.[61] found that early preventative MV with APRV blocked ARDS development, preserved surfactant proteins, and reduced pulmonary inflammation. They proposed that the injury prevention mechanism is related to preserving alveolar epithelial and endothelial integrity. Their conclusion was inconsistent with the results of Emr et al.[62] In this research, APRV blocked early drivers of lung injury, preventing ARDS, but improved endothelial permeability and maintained the concentrations of surfactant proteins A and B. In vivo microscopy demonstrated that compared with the A/CV, APRV significantly improved alveolar patency and stability. Another study also found that decreased Tlow to achieve a termination of peak expiratory flow rate (PEFR) equal to 75% of the PEFR could reduce alveolar microstrain and improve alveolar recruitment.[56], [57] These results were consistent with the study of Kollisch-Singule, who found that decreased Tlow was associated with large alveoli and greater alveolar air space occupancy, resulting in the least conducting airway μ-strain.[66]
Effects of APRV on Extrapulmonary Organs
Patients with ARDS rarely die of hypoxia and/or hypercapnia but often have multiple organ system dysfunction syndromes, which increase mortality.[67] This suggests that in the treatment of ARDS, attention should also be given to extrapulmonary organs. APRV-related studies focusing on extrapulmonary organs mainly include the heart, brain, and kidney.
Heart
Preclinical and clinical studies have shown that increasing SB in APRV can improve hemodynamic function and lower the demand for vasopressor support.[29], [30], [31], [68] Lewis's study demonstrated that during SB of APRV, the peak and average airway pressures decreased on the original high basis, resulting in decreased intrathoracic transmission pressure and decreased central venous pressure in patients with ALI/ARDS.[30] Reduced intrathoracic pressure enhances the venous reflux, thereby enhancing cardiac function, while reducing the need for a vasopressor to support mean arterial pressure and oxygen delivery (DO2).[29] Finally, use of APRV is associated with improvement of cardiopulmonary function including increased cardiac index (CI) and DO2 and decreased venous admixture (QVA/QT).[31]
Brain
In 2012, Marik et al.[69]. showed that APRV can be safely and effectively applied to patients with severe neurological diseases and can increase cerebral blood flow without increasing intracranial pressure (ICP), which was confirmed in a similar study by Fletcher et al.[70] in 2018. Similarly, Edgerton et al.[71] retrospectively studied the effects of APRV in 15 patients with traumatic brain injury. In this study, ICP did not significantly change after the transition to APRV. These data clearly show that the ventilation strategy of increasing mean airway pressure has little effect on ICP. However, Fletche et al.[70] verified the effect of APRV on the brain in a pig model and found that APRV was associated with increased cerebral ischemia and the risk increased over time.
Kidney
The analysis of risk factors for acute kidney injury (AKI) in patients with ARDS showed that ARDS did not significantly affect the occurrence of AKI.[72], [73] Specifically, no correlation was found between MV parameters and AKI changes. In their prospective study, Hering et al.[74] evaluated the effects of APRV on renal perfusion and renal function in patients with ALI/ARDS. They found that SB with APRV was related to the improvement of renal hemodynamics and function. However, renal perfusion and function did not improve once there was no SB during APRV ventilation.
Other organs
There are limited studies to explore the effect of APRV on other organs. Hering et al.[75] found that APRV with SB could increase intestinal blood flow in a pig model of ARDS. One case study reported that APRV could be a useful rescue therapy in pediatric hepatopulmonary syndrome.[76] However, APRV was not significantly associated with an improvement in hepatic arterial blood flow in the pig model.[77] Therefore, further studies are needed to provide more evidence of the effect of APRV on other organs.
Conclusions
Based on clinical and experimental data, APRV has been indicated to have many physiological benefits for patients with ARDS and those at risk of developing ARDS because it can improve oxygenation and hemodynamic function, perform alveolar recruitment, preserve SB, and decrease VILI, while not increasing the side effects on the function of extrapulmonary organs, which is highly consistent with the concept of ARDS treatment. However, evidence regarding the efficacy and safety of APRV is still insufficient for patients with ARDS, especially for children. Moreover, given the complicated and non-specific parameters, APRV has still not found widespread clinical application. Furthermore, because ARDS has many phenotypes, each associated with different pathophysiological changes, future well-organized, large-scale, multicenter RCTs are needed to validate the effect of APRV in patients with ARDS based on the pathophysiology, to clarify which specific subgroups of patients could benefit from APRV.
Funding
This work was supported by the National Natural Science Foundation of China (gereral program, Grant No. 81,873,929).
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Managing Editor: Jingling Bao
Footnotes
Given his role as Editorial Board Member, Prof. Yan Kang had no involvement in the peer-review of this article and has no access to information regarding its peer-review. Prof. Dechang Chen who is the co-editor-in-chief took the responsibility for peer-review progress and made the final decision.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jointm.2022.02.003.
Contributor Information
Jing Yang, Email: yjingscu@163.com.
Yan Kang, Email: Kangyan@scu.edu.cn.
Appendix. Supplementary materials
References
- 1.Fan E., Del Sorbo L., Goligher E.C., Hodgson C.L., Munshi L., Walkey A.J., et al. An official American thoracic society/European society of intensive care medicine/society of critical care medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 2.Kuchnicka K., Maciejewski D. Ventilator-associated lung injury. Anaesthesiol Intensive Ther. 2013;45(3):164–170. doi: 10.5603/ait.2013.0034. [DOI] [PubMed] [Google Scholar]
- 3.Meade M.O., Cook D.J., Guyatt G.H., Slutsky A.S., Arabi Y.M., Cooper D.J., et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):637–645. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 4.Gattinoni L., Protti A., Caironi P., Carlesso E. Ventilator-induced lung injury: the anatomical and physiological framework. Crit Care Med. 2010;38(10 Suppl):S539–S548. doi: 10.1097/CCM.0b013e3181f1fcf7. [DOI] [PubMed] [Google Scholar]
- 5.Allen G.B., Pavone L.A., DiRocco J.D., Bates J.H., Nieman G.F. Pulmonary impedance and alveolar instability during injurious ventilation in rats. J Appl Physiol. 2005;99(2):723–730. doi: 10.1152/japplphysiol.01339.2004. [DOI] [PubMed] [Google Scholar]
- 6.Albert S.P., DiRocco J., Allen G.B., Bates J.H., Lafollette R., Kubiak B.D., et al. The role of time and pressure on alveolar recruitment. J Appl Physiol. 2009;106(3):757–765. doi: 10.1152/japplphysiol.90735.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Downs J.B., Stock M.C. Airway pressure release ventilation: a new concept in ventilatory support. Crit Care Med. 1987;15(5):459–461. doi: 10.1097/00003246-198705000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Zhou Y., Jin X., Lv Y., Wang P., Yang Y., Liang G., et al. Early application of airway pressure release ventilation may reduce the duration of mechanical ventilation in acute respiratory distress syndrome. Intensive Care Med. 2017;43(11):1648–1659. doi: 10.1007/s00134-017-4912-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lachmann B. Open up the lung and keep the lung open. Intensive Care Med. 1992;18(6):319–321. doi: 10.1007/bf01694358. [DOI] [PubMed] [Google Scholar]
- 10.Amato M.B., Barbas C.S., Medeiros D.M., Schettino Gde P., Lorenzi Filho G., Kairalla R.A., et al. Beneficial effects of the “open lung approach” with low distending pressures in acute respiratory distress syndrome. A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med. 1995;152(6 Pt 1):1835–1846. doi: 10.1164/ajrccm.152.6.8520744. [DOI] [PubMed] [Google Scholar]
- 11.Dries D.J., Marini J.J. Airway pressure release ventilation. J Burn Care Res. 2009;30(6):929–936. doi: 10.1097/BCR.0b013e3181bfb84c. [DOI] [PubMed] [Google Scholar]
- 12.Chatburn R.L. Understanding mechanical ventilators. Expert Rev Respir Med. 2010;4(6):809–819. doi: 10.1586/ers.10.66. [DOI] [PubMed] [Google Scholar]
- 13.Hess D.R., Kacmarek R.M. McGraw Hill Education, Medical Publishing Division; New York: 2014. Essentials of mechanical ventilation; pp. 84–85. [Google Scholar]
- 14.Daoud E., Farag H., Chatburn R. Airway pressure release ventilation: what do we know? Respir Care. 2012;57(2):282–292. doi: 10.4187/respcare.01238. [DOI] [PubMed] [Google Scholar]
- 15.Seymour C., Frazer M., Reilly P., Fuchs B. Airway pressure release and biphasic intermittent positive airway pressure ventilation: are they ready for prime time? J Trauma. 2007;62(5):1298–1308. doi: 10.1097/TA.0b013e31803c562f. discussion 308–9. [DOI] [PubMed] [Google Scholar]
- 16.Yadav H., Thompson B.T., Gajic O. Fifty years of research in ARDS. Is acute respiratory distress syndrome a preventable disease? Am J Respir Crit Care Med. 2017;195(6):725–736. doi: 10.1164/rccm.201609-1767CI. [DOI] [PubMed] [Google Scholar]
- 17.Jain S.V., Kollisch-Singule M., Sadowitz B., Dombert L., Satalin J., Andrews P., et al. The 30-year evolution of airway pressure release ventilation (APRV) Intensive Care Med Exp. 2016;4(1):11. doi: 10.1186/s40635-016-0085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mallory P., Cheifetz I. A comprehensive review of the use and understanding of airway pressure release ventilation. Expert Rev Respir Med. 2020;14(3):307–315. doi: 10.1080/17476348.2020.1708719. [DOI] [PubMed] [Google Scholar]
- 19.Nieman G., Al-Khalisy H., Kollisch-Singule M., Satalin J., Blair S., Trikha G., et al. A physiologically informed strategy to effectively open, stabilize, and protect the acutely injured lung. Front Physiol. 2020;11:227. doi: 10.3389/fphys.2020.00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borges J., Okamoto V., Matos G., Caramez M., Arantes P., Barros F., et al. Reversibility of lung collapse and hypoxemia in early acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;174(3):268–278. doi: 10.1164/rccm.200506-976OC. [DOI] [PubMed] [Google Scholar]
- 21.Fan E., Wilcox M., Brower R., Stewart T., Mehta S., Lapinsky S., et al. Recruitment maneuvers for acute lung injury: a systematic review. Am J Respir Crit Care Med. 2008;178(11):1156–1163. doi: 10.1164/rccm.200802-335OC. [DOI] [PubMed] [Google Scholar]
- 22.Cui Y., Cao R., Wang Y., Li G. Lung recruitment maneuvers for ARDS patients: a systematic review and meta-analysis. Respiration. 2020;99(3):264–276. doi: 10.1159/000501045. [DOI] [PubMed] [Google Scholar]
- 23.Lu J., Wang X., Chen M., Cheng L., Chen Q., Jiang H., et al. An open lung strategy in the management of acute respiratory distress syndrome: a systematic review and meta-analysis. Shock. 2017;48(1):43–53. doi: 10.1097/shk.0000000000000822. [DOI] [PubMed] [Google Scholar]
- 24.Rose L. Clinical application of ventilator modes: ventilatory strategies for lung protection. Aust Crit Care. 2010;23(2):71–80. doi: 10.1016/j.aucc.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 25.Frawley P.M., Habashi N.M. Airway pressure release ventilation and pediatrics: theory and practice. Crit Care Nurs Clin North Am. 2004;16(3):337–348. doi: 10.1016/j.ccell.2004.04.003. viii. [DOI] [PubMed] [Google Scholar]
- 26.Lim J., Litton E., Robinson H., Das Gupta M. Characteristics and outcomes of patients treated with airway pressure release ventilation for acute respiratory distress syndrome: a retrospective observational study. J Crit Care. 2016;34:154–159. doi: 10.1016/j.jcrc.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Räsänen J., Cane R.D., Downs J.B., Hurst J.M., Jousela I.T., Kirby R.R., et al. Airway pressure release ventilation during acute lung injury: a prospective multicenter trial. Crit Care Med. 1991;19(10):1234–1241. doi: 10.1097/00003246-199110000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Song S., Tian H., Yang X., Hu Z. [The clinical effect of airway pressure release ventilation for acute lung injury/acute respiratory distress syndrome]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2016;28(1):15–21. 10.3760/cma.j.issn.2095-4352.2016.01.004. [DOI] [PubMed]
- 29.Li J.Q., Li N., Han G.J., Pan C.G., Zhang Y.H., Shi X.Z., et al. Clinical research about airway pressure release ventilation for moderate to severe acute respiratory distress syndrome. Eur Rev Med Pharmacol Sci. 2016;20(12):2634–2641. [PubMed] [Google Scholar]
- 30.Kaplan L.J., Bailey H., Formosa V. Airway pressure release ventilation increases cardiac performance in patients with acute lung injury/adult respiratory distress syndrome. Crit Care. 2001;5(4):221–226. doi: 10.1186/cc1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Putensen C., Zech S., Wrigge H., Zinserling J., Stüber F., Von Spiegel T., et al. Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med. 2001;164(1):43–49. doi: 10.1164/ajrccm.164.1.2001078. [DOI] [PubMed] [Google Scholar]
- 32.Liu L., Tanigawa K., Ota K., Tamura T., Yamaga S., Kida Y., et al. Practical use of airway pressure release ventilation for severe ARDS – a preliminary report in comparison with a conventional ventilatory support. Hiroshima J Med Sci. 2009;58(4):83–88. [PubMed] [Google Scholar]
- 33.Hanna K., Seder C.W., Weinberger J.B., Sills P.A., Hagan M., Janczyk R.J. Airway pressure release ventilation and successful lung donation. Arch Surg. 2011;146(3):325–328. doi: 10.1001/archsurg.2011.35. [DOI] [PubMed] [Google Scholar]
- 34.Gattinoni L., Coppola S., Cressoni M., Busana M., Rossi S., Chiumello D. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201(10):1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gattinoni L., Chiumello D., Rossi S. COVID-19 pneumonia: ARDS or not? Crit Care. 2020;24(1):154. doi: 10.1186/s13054-020-02880-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chiumello D., Busana M., Coppola S., Romitti F., Formenti P., Bonifazi M., et al. Physiological and quantitative CT-scan characterization of COVID-19 and typical ARDS: a matched cohort study. Intensive Care Med. 2020;46(12):2187–2196. doi: 10.1007/s00134-020-06281-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim C.H. SARS-CoV-2 evolutionary adaptation toward host entry and recognition of receptor O-acetyl sialylation in virus-host interaction. Int J Mol Sci. 2020;21(12):4549. doi: 10.3390/ijms21124549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jose R.J., Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. 2020;8(6):e46–e47. doi: 10.1016/s2213-2600(20)30216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Merad M., Martin J.C. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(6):355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mahmoud O., Patadia D., Salonia J. Utilization of airway pressure release ventilation as a rescue strategy in COVID-19 patients: a retrospective analysis. J Intensive Care Med. 2021;36(10):1194–1200. doi: 10.1177/08850666211030899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zorbas J.S., Ho K.M., Litton E., Wibrow B., Fysh E., Anstey M.H. Airway pressure release ventilation in mechanically ventilated patients with COVID-19: a multicenter observational study. Acute Crit Care. 2021;36(2):143–150. doi: 10.4266/acc.2021.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Varpula T., Pettilä V., Nieminen H., Takkunen O. Airway pressure release ventilation and prone positioning in severe acute respiratory distress syndrome. Acta Anaesthesiol Scand. 2001;45(3):340–344. doi: 10.1034/j.1399-6576.2001.045003340.x. [DOI] [PubMed] [Google Scholar]
- 43.Varpula T., Jousela I., Niemi R., Takkunen O., Pettilä V. Combined effects of prone positioning and airway pressure release ventilation on gas exchange in patients with acute lung injury. Acta Anaesthesiol Scand. 2003;47(5):516–524. doi: 10.1034/j.1399-6576.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 44.Lee S.J., Lee Y., Kong A., Ng S.Y. Airway pressure release ventilation combined with prone positioning in acute respiratory distress syndrome: old tricks new synergy: a case series. A A Pract. 2020;14(8):e01231. doi: 10.1213/XAA.0000000000001231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rozé H., Richard J.M., Thumerel M., Ouattara A. Spontaneous breathing (SB) using airway pressure-release ventilation (APRV) in patients under extracorporeal-membrane oxygenation (ECMO) for acute respiratory distress syndrome (ARDS) Intensive Care Med. 2017;43(12):1919–1920. doi: 10.1007/s00134-017-4892-z. [DOI] [PubMed] [Google Scholar]
- 46.Dong M., Cheng J., Wang B., Zhou Y., Kang Y. Airway pressure release ventilation: is it really different in adults and children? Am J Respir Crit Care Med. 2019;200(6):788–789. doi: 10.1164/rccm.201901-0179LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schultz T.R., R.A.T.-Costarino A.T.J., Durning S.M., Napoli L.A., Schears G., Godinez R.I., et al. Airway pressure release ventilation in pediatrics. Pediatr Crit Care Med. 2001;2(3):243–246. doi: 10.1097/00130478-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 48.Lalgudi Ganesan S., Jayashree M., Chandra Singhi S., Bansal A. Airway pressure release ventilation in pediatric acute respiratory distress syndrome. A randomized controlled trial. Am J Respir Crit Care Med. 2018;198(9):1199–1207. doi: 10.1164/rccm.201705-0989OC. [DOI] [PubMed] [Google Scholar]
- 49.Froese A.B., Kinsella J.P. High-frequency oscillatory ventilation: lessons from the neonatal/pediatric experience. Crit Care Med. 2005;33(3 Suppl):S115–S121. doi: 10.1097/01.ccm.0000155923.97849.6d. [DOI] [PubMed] [Google Scholar]
- 50.Ning B., Liang L., Lyu Y., Yu Y., Li B. The effect of high-frequency oscillatory ventilation or airway pressure release ventilation on children with acute respiratory distress syndrome as a rescue therapy. Transl Pediatr. 2020;9(3):213–220. doi: 10.21037/tp-19-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yehya N., Topjian A.A., Lin R., Berg R.A., Thomas N.J., Friess S.H. High frequency oscillation and airway pressure release ventilation in pediatric respiratory failure. Pediatr Pulmonol. 2014;49(7):707–715. doi: 10.1002/ppul.22853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Neumann P., Wrigge H., Zinserling J., Hinz J., Maripuu E., Andersson L., et al. Spontaneous breathing affects the spatial ventilation and perfusion distribution during mechanical ventilatory support. Crit Care Med. 2005;33(5):1090–1095. doi: 10.1097/01.ccm.0000163226.34868.0a. [DOI] [PubMed] [Google Scholar]
- 53.Hering R., Zinserling J., Wrigge H., Varelmann D., Berg A., Kreyer S., et al. Effects of spontaneous breathing during airway pressure release ventilation on respiratory work and muscle blood flow in experimental lung injury. Chest. 2005;128(4):2991–2998. doi: 10.1378/chest.128.4.2991. [DOI] [PubMed] [Google Scholar]
- 54.Roy S., Habashi N., Sadowitz B., Andrews P., Ge L., Wang G., et al. Early airway pressure release ventilation prevents ARDS – a novel preventive approach to lung injury. Shock. 2013;39(1):28–38. doi: 10.1097/SHK.0b013e31827b47bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kollisch-Singule M., Emr B., Smith B., Roy S., Jain S., Satalin J., et al. Mechanical breath profile of airway pressure release ventilation: the effect on alveolar recruitment and microstrain in acute lung injury. JAMA Surg. 2014;149(11):1138–1145. doi: 10.1001/jamasurg.2014.1829. [DOI] [PubMed] [Google Scholar]
- 56.Arrindell E.L., Krishnan R., van der Merwe M., Caminita F., Howard S.C., Zhang J., et al. Lung volume recruitment in a preterm pig model of lung immaturity. Am J Physiol Lung Cell Mol Physiol. 2015;309(10):L1088–L1092. doi: 10.1152/ajplung.00292.2015. [DOI] [PubMed] [Google Scholar]
- 57.Kollisch-Singule M., Jain S.V., Satalin J., Andrews P., Searles Q., Liu Z., et al. Limiting ventilator-associated lung injury in a preterm porcine neonatal model. J Pediatr Surg. 2017;52(1):50–55. doi: 10.1016/j.jpedsurg.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 58.Han G.J., Li J.Q., Pan C.G., Sun J.X., Shi Z.X., Xu J.Y., et al. Experimental study of airway pressure release ventilation in the treatment of acute respiratory distress syndrome. Exp Ther Med. 2017;14(3):1941–1946. doi: 10.3892/etm.2017.4718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xia J., Sun B., He H., Zhang H., Wang C., Zhan Q. Effect of spontaneous breathing on ventilator-induced lung injury in mechanically ventilated healthy rabbits: a randomized, controlled, experimental study. Crit Care. 2011;15(5):R244. doi: 10.1186/cc10502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Albert S., Kubiak B.D., Vieau C.J., Roy S.K., DiRocco J., Gatto L.A., et al. Comparison of “open lung” modes with low tidal volumes in a porcine lung injury model. J Surg Res. 2011;166(1):e71–e81. doi: 10.1016/j.jss.2010.10.022. [DOI] [PubMed] [Google Scholar]
- 61.Roy S., Sadowitz B., Andrews P., Gatto L.A., Marx W., Ge L., et al. Early stabilizing alveolar ventilation prevents acute respiratory distress syndrome: a novel timing-based ventilatory intervention to avert lung injury. J Trauma Acute Care Surg. 2012;73(2):391–400. doi: 10.1097/TA.0b013e31825c7a82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Emr B., Gatto L.A., Roy S., Satalin J., Ghosh A., Snyder K., et al. Airway pressure release ventilation prevents ventilator-induced lung injury in normal lungs. JAMA Surg. 2013;148(11):1005–1012. doi: 10.1001/jamasurg.2013.3746. [DOI] [PubMed] [Google Scholar]
- 63.Ak A.K., Anjum F. StatPearls. Treasure island. StatPearls Publishing; FL: 2021. Ventilator-induced lung injury (VILI) https://pubmed.ncbi.nlm.nih.gov/33085391/ [PubMed] [Google Scholar]
- 64.Slutsky A.S., Ranieri V.M. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–2136. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 65.Roy S.K., Emr B., Sadowitz B., Gatto L.A., Ghosh A., Satalin J.M., et al. Preemptive application of airway pressure release ventilation prevents development of acute respiratory distress syndrome in a rat traumatic hemorrhagic shock model. Shock. 2013;40(3):210–216. doi: 10.1097/SHK.0b013e31829efb06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kollisch-Singule M., Emr B., Smith B., Ruiz C., Roy S., Meng Q., et al. Airway pressure release ventilation reduces conducting airway micro-strain in lung injury. J Am Coll Surg. 2014;219(5):968–976. doi: 10.1016/j.jamcollsurg.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Menk M., Estenssoro E., Sahetya S.K., Neto A.S., Sinha P., Slutsky A.S., et al. Current and evolving standards of care for patients with ARDS. Intensive Care Med. 2020;46(12):2157–2167. doi: 10.1007/s00134-020-06299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ge H., Lin L., Xu Y., Xu P., Duan K., Pan Q., et al. Airway pressure release ventilation mode improves circulatory and respiratory function in patients after cardiopulmonary bypass, a randomized trial. Front Physiol. 2021;12 doi: 10.3389/fphys.2021.684927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Marik P.E., Young A., Sibole S., Levitov A. The effect of APRV ventilation on ICP and cerebral hemodynamics. Neurocrit Care. 2012;17(2):219–223. doi: 10.1007/s12028-012-9739-4. [DOI] [PubMed] [Google Scholar]
- 70.Fletcher J.J., Wilson T.J., Rajajee V., Davidson S.B., Walsh J.C. Changes in therapeutic intensity level following airway pressure release ventilation in severe traumatic brain injury. J Intensive Care Med. 2018;33(3):196–202. doi: 10.1177/0885066616669315. [DOI] [PubMed] [Google Scholar]
- 71.Edgerton C.A., Leon S.M., Hite M.A., Kalhorn S.P., Scott L.A., Eriksson E.A. Airway pressure release ventilation does not increase intracranial pressure in patients with traumatic brain injury with poor lung compliance. J Crit Care. 2019;50:118–121. doi: 10.1016/j.jcrc.2018.11.034. [DOI] [PubMed] [Google Scholar]
- 72.Darmon M., Clec'h C., Adrie C., Argaud L., Allaouchiche B., Azoulay E., et al. Acute respiratory distress syndrome and risk of AKI among critically ill patients. Clin J Am Soc Nephrol. 2014;9(8):1347–1353. doi: 10.2215/cjn.08300813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Han H., Li J., Chen D., Zhang F., Wan X., Cao C. A clinical risk scoring system of acute respiratory distress syndrome-induced acute kidney injury. Med Sci Monit. 2019;25:5606–5612. doi: 10.12659/msm.915905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hering R., Peters D., Zinserling J., Wrigge H., von Spiegel T., Putensen C. Effects of spontaneous breathing during airway pressure release ventilation on renal perfusion and function in patients with acute lung injury. Intensive Care Med. 2002;28(10):1426–1433. doi: 10.1007/s00134-002-1442-z. [DOI] [PubMed] [Google Scholar]
- 75.Hering R., Viehöfer A., Zinserling J., Wrigge H., Kreyer S., Berg A., et al. Effects of spontaneous breathing during airway pressure release ventilation on intestinal blood flow in experimental lung injury. Anesthesiology. 2003;99(5):1137–1144. doi: 10.1097/00000542-200311000-00021. [DOI] [PubMed] [Google Scholar]
- 76.Jenkins J.K., Gebergzabher Y.D., Island E.R., Habashi N., Hauser G.J. Use of airway pressure release ventilation in a child with refractory hepatopulmonary syndrome after liver transplantation. Pediatr Transplant. 2013;17(3):E81–E87. doi: 10.1111/petr.12058. [DOI] [PubMed] [Google Scholar]
- 77.Hering R., Bolten J.C., Kreyer S., Berg A., Wrigge H., Zinserling J., et al. Spontaneous breathing during airway pressure release ventilation in experimental lung injury: effects on hepatic blood flow. Intensive Care Med. 2008;34(3):523–527. doi: 10.1007/s00134-007-0957-8. [DOI] [PubMed] [Google Scholar]
- 78.Varpula T., Valta P., Niemi R., Takkunen O., Hynynen M., Pettilä V.V. Airway pressure release ventilation as a primary ventilatory mode in acute respiratory distress syndrome. Acta Anaesthesiol Scand. 2004;48(6):722–731. doi: 10.1111/j.0001-5172.2004.00411.x. [DOI] [PubMed] [Google Scholar]
- 79.Yoshida T., Rinka H., Kaji A., Yoshimoto A., Arimoto H., Miyaichi T., et al. The impact of spontaneous ventilation on distribution of lung aeration in patients with acute respiratory distress syndrome: airway pressure release ventilation versus pressure support ventilation. Anesth Analg. 2009;109(6):1892–1900. doi: 10.1213/ANE.0b013e3181bbd918. [DOI] [PubMed] [Google Scholar]
- 80.Sydow M., Burchardi H., Ephraim E., Zielmann S., Crozier T.A. Long-term effects of two different ventilatory modes on oxygenation in acute lung injury. Comparison of airway pressure release ventilation and volume-controlled inverse ratio ventilation. Am J Respir Crit Care Med. 1994;149(6):1550–1556. doi: 10.1164/ajrccm.149.6.8004312. [DOI] [PubMed] [Google Scholar]
- 81.Dart B.W., Maxwell R.A., Richart C.M., Brooks D.K., Ciraulo D.L., Barker D.E., et al. Preliminary experience with airway pressure release ventilation in a trauma/surgical intensive care unit. J Trauma. 2005;59(1):71–76. doi: 10.1097/00005373-200507000-00010. [DOI] [PubMed] [Google Scholar]
- 82.Kamath S.S., Super D.M., Mhanna M.J. Effects of airway pressure release ventilation on blood pressure and urine output in children. Pediatr Pulmonol. 2010;45(1):48–54. doi: 10.1002/ppul.21058. [DOI] [PubMed] [Google Scholar]
- 83.Yener N., Udurgucu M. Airway pressure release ventilation as a rescue therapy in pediatric acute respiratory distress syndrome. Indian J Pediatr. 2020;87(11):905–909. doi: 10.1007/s12098-020-03235-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kawaguchi A., Guerra G.G., Duff J.P., Ueta I., Fukushima R. Hemodynamic changes in child acute respiratory distress syndrome with airway pressure release ventilation: a case series. Clin Respir J. 2015;9(4):423–429. doi: 10.1111/crj.12155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.