Abstract
Purpose:
Childhood and adult adversities occur more frequently among women and persons of colour, possibly influencing racial/ethnic disparities in substance use behaviours. This study investigates how childhood and adult adversities cluster together by race/ethnicity and how these adversity clusters predict binge drinking, tobacco, e-cigarette, and marijuana use in women.
Methods:
Latent class analysis (LCA) was used in a combined sample from the 2015 and 2018 Minnesota College Student Health Survey to identify clusters of childhood adversities plus highly correlated adult adversities among Asian, Black, Latina, and White women aged 18-25. The LCA method allowed unique clusters of adversity to emerge from these data, stratified by race/ethnicity. Each substance use outcome was regressed on each adversity cluster across each race/ethnicity group.
Results:
A seven-cluster model was selected for White women, a five-cluster model for Black women, and four-cluster models for Asian and Latina women. Differences across racial/ethnic clusters included the presence of a lifetime sexual assault only cluster in the White, Black, and Asian women that did not exist among Latina women. Across all racial/ethnic groups and substance use outcomes, the high adversity cluster exhibited the greatest risk. Significant racial/ethnic disparities were observed across several substance use behaviours; these were narrowed substantially among women with fewer adversities.
Conclusions:
In this study, subtyping women according to their histories of adversity revealed differences in substance use risk. The reduced substance use disparities found among those with lower adversities suggest that prevention of adversities may advance health equity.
Keywords: adverse childhood experiences (ACEs), alcohol, substance use, race/ethnicity, latent class analysis, women
1.0. Background
1.1. Substance use in young adulthood
Consistent evidence of short and long-term negative effects of substance use in adolescence and young adulthood has made ongoing surveillance, research, and prevention efforts focused on substance use during college an important public health priority (Schulenberg et al., 2019). Initiation of substance use during college increases the risk for continued use into adulthood and associated social and behavioural health consequences (Caldeira KM et al., 2012; Jennison, 2004). Substance use, inclusive of alcohol, tobacco, and marijuana use, are highest among young adults aged 18-22 and higher in college-enrolled young adults than their non-enrolled peers (Schulenberg et al., 2019). Excessive substance use during college increases the risk of poor academic performance and reduces long-term employment opportunities and lifetime earnings (Arria et al., 2013; Caldeira et al., 2008; Meda et al., 2017). The prevalence of tobacco use through e-cigarettes has also been on the rise among young adults (Schulenberg et al., 2019). Identifying risk and protective factors for substance use in college can help to identify those who may benefit from targeted intervention and may provide insight into potential prevention interventions.
Adverse childhood experiences (ACEs) have been identified as potential risk factors for substance use. ACEs include exposure to maltreatment (e.g., abuse, neglect) and household dysfunction (e.g., domestic violence, parental substance use) (Felitti et al., 1998). Research on the association between ACEs and substance use behaviours have often used cumulative frequency scores (summing the number of different ACEs) (Allem et al., 2015; Anda et al., 1999; Dube et al., 2003; Mersky & Janczewski, 2018). These studies have consistently demonstrated an overall dose-response relationship between the cumulative impact of ACEs and increased use of tobacco, alcohol, and illicit drug use in adulthood (Anda et al., 1999, 2006; Dube et al., 2003; Ford et al., 2010). A criticism of this approach is the assumption that each adversity experience contributes equally to a given health outcome and largely ignores the patterning and co-occurrence of exposures concerning substance use outcomes. This critique is important because children who experience ACEs commonly experience more than one type of ACE (Finkelhor, 2009; Ford et al., 2010). For example, a study using combined data from the 2011-2014 Behavioral Risk Factor Surveillance System (BRFSS) found that 61.6% of participants reported exposure to one ACE while 34.6% reported exposure to three or more ACEs (Merrick et al., 2018). One alternative to the cumulative frequency score approach is to use Latent Class Analysis (LCA) to empirically identify patterns or "clusters" of exposure to types of ACEs (Hajat et al., 2020; Rebbe et al., 2017; Shin et al., 2018). Studies applying the LCA approach have demonstrated mixed findings, with one study indicating childhood exposure to parental substance use and parental incarceration predicting higher rates of tobacco use compared to other ACEs (Hajat et al., 2020). Another study of young adults, found the high and multiple ACEs clusters (including the highest prevalence of emotional abuse, neglect, and adult experience of IPV victimization) had the strongest association with alcohol-related problems and tobacco use (Shin et al., 2018).
Exposure to ACEs during childhood are associated with adult adversities such as intimate partner violence (IPV) (Montalvo-Liendo et al., 2015; Young-Wolff et al., 2013) and sexual assault in adulthood (Ports et al., 2016; Widom et al., 2014). A life course approach considers the continuum of adversities experienced during childhood and early adulthood and provides a more holistic understanding of the compounding impacts of these stressors and their associations with negative health behaviours. In particular, exposure to childhood and early adult adversities confers an increased risk of a range of behavioural health problems, including substance use (Kobulsky et al., 2018; Mersky et al., 2013; Shin et al., 2018) which becomes more prominent during college (Schulenberg et al., 2019). However, few studies have used LCA to derive clusters of combined childhood and adult adversities and examined how these are related to substance use (Shin et al., 2018).
Despite methodological advances in understanding the impacts of ACEs on adult health outcomes, several research gaps remain. The first limitation of the existing literature is a dearth of analyses assessing how adversity–substance use associations may differ by race/ethnicity. Because of racial and ethnic social stratification, different racial and ethnic groups appear to experience different patterns and prevalence of childhood and adult adversity (Ahern et al., 2016; Maguire-Jack et al., 2019; Merrick et al., 2018). Second, much of the existing literature focuses only on the association of ACEs and substance use behaviours and does not incorporate early adult adversities that may impact substance use trajectories. Applying a life course perspective may reveal adversity types that are most predictive of substance use during college. This study applies LCA to investigate the patterning of exposure to childhood and early adult adversities to examine how these patterns are related to substance use behaviours, during the critical developmental period of emerging adulthood in a cohort of racial/ethnically diverse women attending 2- and 4-year colleges.
The overarching goal of this study is to provide insight into which adversity profiles confer higher risk to better target prevention and student mental health services. The primary objectives are: 1) identify the patterning of childhood and adult adversities stratified by race/ethnicity using LCA and 2) examine the predicted rates of tobacco, e-cigarette, marijuana, and binge drinking as predicted by membership in a unique adversity cluster generated in stratified race/ethnicity groups. This study focused on women because of their higher exposure to adversities.
2.0. Methods
2.1. Data
Data were combined from the 2015 (N=12,220) and 2018 (N=10,579) Minnesota College Student Health Surveys (CSHS). The CSHS is an annual surveillance system that recruits a random sample of undergraduate and graduate students from institutional enrolment lists in up to 17 participating 2-year and 4-year public and private colleges in Minnesota. Survey methodology is documented elsewhere (Health and Health-Related Behaviors 2015 College Student Health Survey Report. Minneapolis, MN, 2015; Health and Health-Related Behaviors 2018 College Student Health Survey Report, 2018). Briefly, students are randomly invited through multiple mailings and emails. Previous research using these data found that adversity clusters in the overall sample of women replicated well across the CSHS 2015 and 2018 surveys, providing a rationale for combining the datasets to maximize power to conduct race/ethnicity-stratified analyses (Santaularia et al., 2021). In addition, these two survey years were chosen because they contained the same set of adversity and substance use measures and were less likely to have repeat responders given they were three years apart. The current study restricted analyses to emerging adult women aged 18 to 25, yielding an analytical sample of 9,310 participants.
2.2. Measures
2.2.1. Childhood adversities
Childhood adversities were assessed using the 11-question ACEs questionnaire from the Behavioral Risk Factor Surveillance System (BRFSS) (Centers for Disease Control and Prevention, 2015). Specific items are described in Appendix 1. Childhood emotional abuse and childhood physical abuse were assessed with one question each. Three questions were used to assess different types of childhood sexual abuse, including (1) being touched by, (2) forced to touch, or (3) forced into sex by someone at least five years older. Endorsement of any of these items was counted as an experience of sexual abuse. Six forms of childhood household dysfunction were assessed with one question each, including: household mental illness, household alcohol problems, household drug use, incarcerated household member, parental divorce/separation, and witnessed family violence. All nine childhood adversity measures were operationalized as dichotomous variables (Merrick et al., 2018) as described in Appendix 1.
2.2.2. Adult adversities
Adult adversities measures included lifetime and past 12-month sexual assault, intimate partner emotional abuse, and intimate partner physical abuse. There were two sexual assault questions. These two questions asked about actual or attempted sexual intercourse and attempted or actual non-consensual or forced touching. To maintain adequate cell sizes, these responses were combined to create an adult sexual assault variable. The adult adversity past 12 months and lifetime questions were combined to create three yes/no ever-experienced sexual assault, intimate partner emotional abuse, and intimate partner physical abuse variables for analysis. Full details of variable and cluster formation for lifetime adversities are described in Appendix 2.
2.2.3. Race/Ethnicity
Race/ethnicity (Asian, Black, Latina, or White) was self-identified on the CSHS and is used to approximate a combination of historical, social, and systemic factors that shape health and opportunity in the United States (Jones, 2001). Differences attributed to different races/ethnicities in this study are not biologically meaningful. Instead, they capture important differences in the way people of different races/ethnicities experience intergenerational barriers and opportunities in the United States and their manifestation in the patterning across lifetime adversities and substance use behaviours (Manly, 2006).
2.2.4. Substance Use
Tobacco smoking, e-cigarette use, and marijuana use were defined as engaging in each of these behaviours, respectively, at any time during the past 12 months. Binge drinking was defined as having five or more drinks in a single sitting in the past two weeks (Schulenberg et al., 2019). These measures are consistent with annual prevalence and binge drinking measures from the Monitoring the Future study (Schulenberg et al., 2019) .
2.2.5. Sociodemographic Variables
Several sociodemographic variables were included as potential confounders that are highly correlated with race/ethnicity and/or also predict substance use. Parental educational attainment was defined as the highest education of any parent, stepparent, or adult caretaker, dichotomized into bachelor's degree or more education versus less education. Survey respondents' post-secondary school type was defined as being currently enrolled in either a 2-year or 4-year college. Age was dichotomized as 18-20 or 21-25 years old as 21 is the legal drinking age in the United States.
2.3. Statistical analyses
To identify race/ethnicity group-specific clusters of adult and child adversities, LCA was performed using all 12 child and adult adversity indicator variables, stratified by race/ethnicity categories. For each racial/ethnic group, a one-cluster model was fit first, then clusters were added one at a time until the fit and/or interpretability worsened. Standard criteria (the sample size-adjusted a-BIC, AIC, Vuong- Lo-Mendell-Rubin (VLMR) likelihood ratio test, and entropy) were used to determine the number of LCA clusters and to evaluate model fit and precision (Nylund et al., 2007). Smaller a-BIC and AIC values indicated a better fit. Significant VLMR values indicated that the k cluster model was a better fit than the k-1 cluster model. Entropy values closer to 1.00 indicated more precision. The best model optimized fit criteria and had a meaningful qualitative interpretation of clusters. Mplus (Version 8.4, Los Angeles, CA: Muthén & Muthén) was used for analysis. A full description and results of the LCA cluster selection and formation are noted in Appendices 2 and 3. After identifying meaningful clusters, we assessed how each of the substance use behaviours differed across clusters. We used the distal outcome procedure and the three-step Bolck-Croon-Hagenaars (BCH) (Nylund et al., 2007) approach to regress each substance use behaviour on clusters, within each race/ethnic group, adjusting for potential confounders. We then estimated predicted probabilities of each substance use behaviour for each cluster, within each race/ethnicity group, estimated at the mean of the covariate levels. The distal outcome procedure and the BCH approach handled missingness with listwise deletion in the outcome and covariate measures (Wang & Wang, 2020).
3.0. Results
3.1. Descriptive statistics
Table 1 provides demographic and substance use characteristics of the women in our sample. The most prevalent substance use behaviours were binge drinking and marijuana use. Overall, substance use behaviours were more common in White and Latina students compared to Black and Asian students. For example, 28% of White women and 23% of Latinas reported binge drinking, compared to 17% of Asian and 12% of Black women. Marijuana use was highest among Latinas (22%), followed by White (15%), Black (13%), and Asian (8%) students. Tobacco use was highest among Latina women (13%) and White women (11%) compared to Black (8%) and Asian 6%) women. Finally, e-cigarette use was highest among Latina (11%) and White (8%) compared to Black (8%) and Asian (6%) women.
Table 1.
Sample characteristics
| Asian | Black | Latina | White | |||||
|---|---|---|---|---|---|---|---|---|
| (n=940) | (n=437) | (n=453) | (n=7448) | |||||
| n | % | n | % | n | % | n | % | |
| Social Demographics | ||||||||
| Age, years | ||||||||
| <21 | 463 | 49% | 244 | 56% | 261 | 58% | 4028 | 54% |
| >=21 | 477 | 51% | 194 | 44% | 192 | 42% | 3430 | 46% |
| College Type | ||||||||
| 4-year college | 808 | 86% | 309 | 71% | 334 | 75% | 6156 | 83% |
| 2-year college | 127 | 14% | 124 | 29% | 114 | 25% | 1264 | 17% |
| Educational attainment | ||||||||
| Some high school - associates degree | 402 | 47% | 256 | 61% | 276 | 63% | 2768 | 38% |
| Bachelor's degree or more | 455 | 53% | 161 | 39% | 163 | 37% | 4604 | 62% |
| Substance Use Behaviors | ||||||||
| Tobacco | ||||||||
| yes | 54 | 6% | 36 | 8% | 59 | 13% | 761 | 10% |
| no | 885 | 94% | 401 | 92% | 393 | 87% | 6687 | 90% |
| E-cigarettes | ||||||||
| yes | 48 | 5% | 13 | 3% | 48 | 11% | 581 | 8% |
| no | 892 | 95% | 423 | 97% | 405 | 89% | 6860 | 92% |
| Binge Drinking | ||||||||
| yes | 158 | 17% | 52 | 12% | 103 | 23% | 2090 | 28% |
| no | 781 | 83% | 384 | 88% | 350 | 77% | 5344 | 72% |
| Marijuana | ||||||||
| yes | 77 | 8% | 56 | 13% | 201 | 22% | 1150 | 15% |
| no | 860 | 92% | 380 | 87% | 350 | 77% | 6287 | 85% |
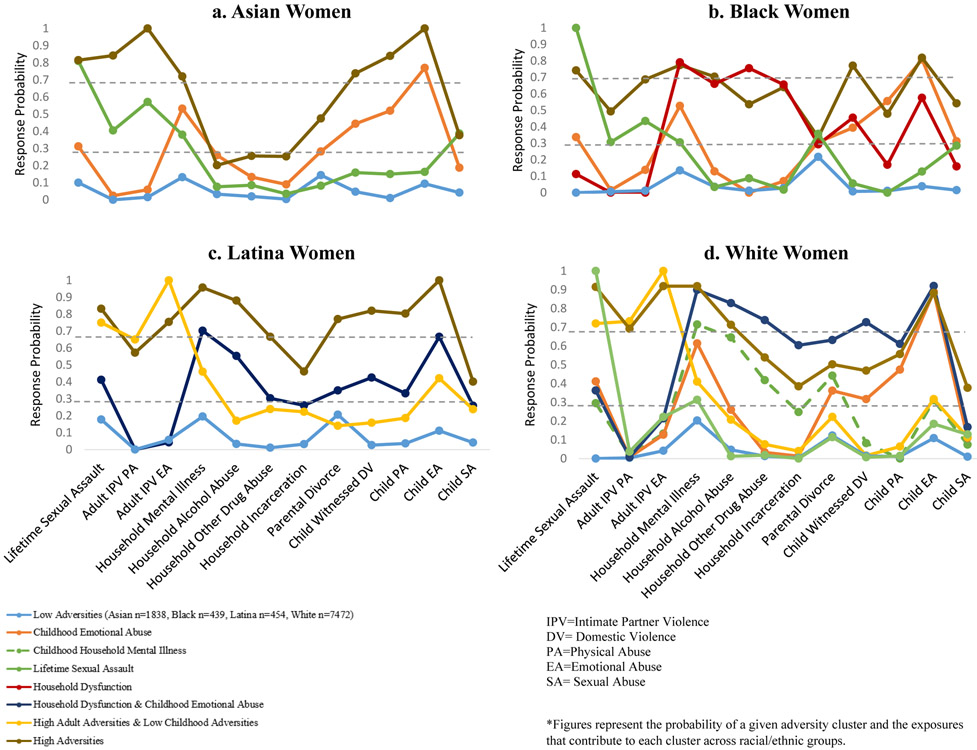
3.2. Clusters of adversities by race/ethnicity
LCA identified meaningful clusters for all race/ethnicity groups. Among White participants, the largest sample (n=7448), a 7-cluster solution, was identified, while a 5-cluster solution was chosen for Black participants, and 4-cluster models were identified for Asian and Latina participants. All race/ethnicity groups had a low adversity cluster and a high adversity cluster. A lifetime sexual assault cluster and childhood emotional abuse cluster were present across all racial/ethnic groups except among Latina participants. The White and Latina groups both contained a high adult and low childhood adversity cluster, while Black and Asian groups did not. A household dysfunction cluster was identified only among Black participants. A household mental illness cluster was identified only among White participants.
3.3. Lifetime adversities and substance use
Results are presented as predicted probabilities (PPs), which can be interpreted as the average probability of substance use for women belonging to a specific adversity cluster, after accounting for the influence of covariates.
3.3.1. Tobacco
As shown in Table 2, adversity clusters were predictive of tobacco use across all racial/ethnic groups. For all groups, tobacco use was lowest for women in the low adversity cluster (Asian PP=2% [95% CI: 1%-4%]; Black PP=4% [95% CI: 1%-7%]; White PP=5% [95% CI: 4%-5%]); Latina PP=7% [95% CI: 3%-11%]. Likewise, for all groups, tobacco use was highest in the high adversity cluster (Black PP=17% [95% CI: 7%-27%]; Asian PP=21% [95% CI: 9%-32%]; White PP=21% [95% CI: 17%-25%]; Latina PP=33% [95% CI: 15%-50%]) Probabilities were notably high for Latina (PP=17% [95% CI: 9%-24%]) and White (PP=20% [95% CI: 17%-21%]) women in the high adult and low childhood adversity cluster; this cluster did not exist for Asian and Black women.
Table 2.
Predicted probability of tobacco, e-cigarette, binge drinking, and marijuana use across adversity clusters by race/ethnicity
| Asian | 95% CI | Black | 95% CI | Latina | 95% CI | White | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Tobacco | ||||||||
| 1-Low Adversities | 0.02 | 0.01-0.04 | 0.04 | 0.01-0.07 | 0.07 | 0.03-0.11 | 0.05 | 0.04-0.05 |
| 2- Childhood Emotional Abuse | 0.05 | 0.02-0.08 | 0.09 | 0.03-0.15 | * | * | 0.11 | 0.09-0.13 |
| 3-Household Mental Illness | * | * | * | * | * | * | 0.12 | 0.10-0.14 |
| 4- Lifetime Sexual Assault | 0.08 | 0.04-0.12 | 0.12 | 0.02-0.21 | * | * | 0.09 | 0.08-0.11 |
| 5- Household Dysfunction | * | * | 0.13 | 0.03-0.23 | * | * | * | * |
| 6-Household Dysfunction and Child Emotional Abuse | * | * | * | * | 0.14 | 0.08-0.20 | 0.16 | 0.11-0.20 |
| 7-High Adult Adversities & Low Childhood Adversities | * | * | * | * | 0.17 | 0.09-0.24 | 0.20 | 0.17-0.24 |
| 8- High Adversities | 0.21 | 0.09-0.32 | 0.17 | 0.07-0.27 | 0.33 | 0.15-0.50 | 0.21 | 0.17-0.25 |
| E-Cigarette Use | ||||||||
| 1-Low Adversities | 0.03 | 0.01-0.05 | 0.00 | 0.00-0.01 | 0.07 | 0.03-0.11 | 0.04 | 0.04-0.05 |
| 2- Childhood Emotional Abuse | 0.05 | 0.03-0.08 | 0.02 | 0.00-0.05 | * | * | 0.10 | 0.08-0.12 |
| 3-Household Mental Illness | * | * | * | * | * | * | 0.09 | 0.07-0.10 |
| 4- Lifetime Sexual Assault | 0.10 | 0.05-0.15 | 0.03 | −0.01-0.08 | * | * | 0.07 | 0.05-0.8 |
| 5- Household Dysfunction | * | * | 0.04 | −0.02-0.11 | * | * | * | * |
| 6-Household Dysfunction and Child Emotional Abuse | * | * | * | * | 0.11 | 0.06-0.16 | 0.08 | 0.05-0.11 |
| 7-High Adult Adversities & Low Childhood Adversities | * | * | * | * | 0.11 | 0.05-0.18 | 0.13 | 0.10-0.16 |
| 8- High Adversities | 0.10 | 0.02-0.18 | 0.08 | 0.00-0.16 | 0.15 | 0.02-0.29 | 0.16 | 0.12-0.20 |
| Binge Drinking | ||||||||
| 1-Low Adversities | 0.12 | 0.09-0.16 | 0.07 | 0.03-0.11 | 0.18 | 0.12-0.24 | 0.24 | 0.22-0.26 |
| 2- Childhood Emotional Abuse | 0.16 | 0.12-0.20 | 0.17 | 0.09-0.24 | * | * | 0.28 | 0.25-0.31 |
| 3-Household Mental Illness | * | * | * | * | * | * | 0.31 | 0.28-0.34 |
| 4- Lifetime Sexual Assault | 0.21 | 0.14-0.28 | 0.06 | −0.01-0.13 | * | * | 0.30 | 0.28-0.33 |
| 5- Household Dysfunction | * | * | 0.17 | 0.05-0.29 | * | * | * | * |
| 6-Household Dysfunction and Child Emotional Abuse | * | * | * | * | 0.24 | 0.17-0.32 | 0.28 | 0.22-0.34 |
| 7-High Adult Adversities & Low Childhood Adversities | * | * | * | * | 0.26 | 0.17-0.35 | 0.36 | 0.32-0.40 |
| 8- High Adversities | 0.36 | 0.24-0.49 | 0.27 | 0.14-0.40 | 0.41 | 0.22-0.59 | 0.31 | 0.26-0.35 |
| Marijuana | ||||||||
| 1-Low Adversities | 0.04 | 0.02-0.07 | 0.05 | 0.02-0.08 | 0.13 | 0.08-0.18 | 0.08 | 0.07-0.09 |
| 2- Childhood Emotional Abuse | 0.09 | 0.05-0.12 | 0.13 | 0.06-0.20 | * | * | 0.18 | 0.15-0.20 |
| 3-Household Mental Illness | * | * | * | * | * | * | 0.18 | 0.16-0.21 |
| 4- Lifetime Sexual Assault | 0.12 | 0.07-0.17 | 0.19 | 0.08-0.31 | * | * | 0.18 | 0.16-0.19 |
| 5- Household Dysfunction | * | * | 0.11 | 0.10-0.30 | * | * | * | * |
| 6-Household Dysfunction and Child Emotional Abuse | * | * | * | * | 0.27 | 0.19-0.34 | 0.23 | 0.18-0.29 |
| 7-High Adult Adversities & Low Childhood Adversities | * | * | * | * | 0.33 | 0.23-0.43 | 0.27 | 0.23-0.31 |
| 8- High Adversities | 0.15 | 0.05-0.25 | 0.35 | 0.20-0.50 | 0.28 | 0.12-0.44 | 0.32 | 0.27-0.36 |
Data does not exist for this class
Adjusted for age, parent education & 2 or 4 year school
All estimates have been rounded to two significant digits
3.3.2. E-cigarette use
Predicted e-cigarette use was much lower than tobacco use across all groups. Predicted probabilities for e-cigarette use was lowest for women in the in low adversity cluster (Black PP=0% [95% CI: 0%-1%]; Asian PP=3% [95% CI: 1%-5%]; White PP=4% [95% CI: 4%-5%]; Latina PP=7% [95% CI: 3%-11%]). E-cigarette use was highest in the high adversity cluster (Black PP=8% [95% CI: 0%-16%]; Asian PP=10% [95% CI: 2%-18%]; Latina PP=15% [95% CI: 2%-29%]; White PP=16% [95% CI: 12%-20%]).
3.3.3. Binge drinking
Overall, race/ethnicity was more strongly associated with binge drinking than adversity cluster, with White students exhibiting the highest prevalence regardless of adversity. Predicted probabilities for binge drinking for women were, on average, lowest in the low adversity cluster (Black PP=7% [95% CI: 3%-11%]; Asian PP=12% [95% CI: 9%-16%]; Latina PP=18% [95% CI: 12%-24%]; White PP=24% [95% CI: 22%-25%]). Across the high adversity cluster, predicted binge drinking was higher across all groups (Asian PP=27% [95% CI: 14%-40%]; White PP=31% [95% CI: 26%-35%]; Asian PP=36% [95% CI: 24%=49%]; Latina PP=41% [95% CI: 22% - 59%]). White (PP=35% [95% CI: 32%-40%]) and Latina (PP=26% [95% CI: 17%-32%]) women in the high adult adversities and low childhood adversities cluster had similarly high predicted probabilities of binge drinking.
3.3.4. Marijuana
Predicted marijuana use was comparatively higher across all races/ethnicities than either tobacco or e-cigarette use but lower than binge drinking. Predicted probabilities of marijuana use were lowest in the low adversity cluster (Asian PP=4% [95% CI: 2%-7%]; Black PP=5% [95% CI: 2%-18]; White PP=8% [95% CI: 7%-9%]; Latina PP=13% [95% CI: 8%-18%]). Predicted marijuana use was, on average, highest across the high adversity cluster (Asian PP=15% [95% CI: 5%-25%]; Latina PP=28% [95% CI: 12%-44%]; White PP=28% [95% CI: 12%-44%] Black PP=35% [95% CI: 20%-50%]). Similar to tobacco use and binge drinking, high levels of predicted marijuana use were associated with the high adult adversities and low childhood adversities cluster in White (PP=27% [95% CI: 23%-31%] and Latina (PP=33% [95% CI: 23%-43%]) women.
4.0. Discussion
We explored whether different clusters of adversity predicted the likelihood of tobacco, e-cigarette, binge drinking, and marijuana use in racial/ethnically diverse young adults enrolled in post-secondary education in Minnesota. Using LCA as the method of analysis allowed the frequency and patterning of adversities in our sample of young adult women to shape the cluster creation within each racial/ethnic group. Ultimately, eight distinct clusters emerged across the four included racial/ethnic groups. Only the low adversity and high adversity clusters were consistent across all racial/ethnic groups, but most clusters existed across at least two groups. Notably, most clusters identified in the smaller race/ethnicity groups overlapped with clusters identified in the large White group. This suggests that the larger number of clusters in the White race/ethnicity may reflect their greater sample size allowing for detection of smaller clusters, rather than fundamental differences in adversity experiences across groups. However, in a few cases unique clusters emerged in the smaller racial/ethnic groups. For example, the household dysfunction cluster was found only in Black, and the high adult, low childhood adversities cluster was found in the Latina and White but not in the Black and Asian groups.
Our findings are consistent with earlier studies using both the cumulative risk score (Allem et al., 2015; Anda et al., 1999; Mersky et al., 2013) and LCA approaches (Hajat et al., 2020; Mersky et al., 2013; Shin et al., 2018). In the latter studies, clusters characterized by multiple types of adversities were associated with greater substance use than clusters characterized by single or no adversities, similar to our results. This pattern is evident even within tobacco and e-cigarette use, which had the lowest prevalence of use across all racial/ethnic groups.
Nationally, the rate of marijuana use across female college students is approximately 42% (Schulenberg et al., 2019), indicating that across race/ethnicity and adversity groups, the predicted rates of marijuana use are lower in our sample compared to a national sample of college-enrolled women. Despite our overall lower predicted prevalence of marijuana use, differences exist across adversity clusters with women in the low adversity cluster having between 4%-13% predicted use compared to nearly one-third of women in the highest adversity groups considering both childhood and early adult adversities. This finding indicates that research considering additional and mutually reinforcing adversities deepen our understanding of how these experiences shape substance use behaviours into later adulthood (Finkelhor et al., 2013; Liu et al., 2018; Ports et al., 2016; Shin et al., 2018).
Binge drinking was the most common substance abuse behaviour among White, Latina, and Asian students. Binge drinking is an especially prevalent substance abuse behaviour in the American Midwest (Schulenberg et al., 2019). This finding is important because much of the existing literature does not describe racial/ethnic differences in binge drinking patterns among women, who, on average, binge drink less than their male counterparts (Krieger et al., 2018). A small number of previous studies investigated the prevalence of binge drinking in Asian and Hispanic college students (LaBrie et al., 2012; Shields et al., 2016; Wechsler et al., 2002). However, we know of no studies that have examined how exposure to adversities may predict this behaviour by racial/ethnic group. Thus, the current study adds to the existing literature by describing the patterning of this behaviour by individuals' underlying history of adversities. Our findings suggest that Latina and Asian students with a higher prevalence of lifetime adversities binge drink at similar levels to White students, suggesting that adversities may be as important as race/ethnicity in shaping binge drinking behaviour.
Overall, findings of this study emphasize the importance of preventing adversities. Preventing exposure to childhood and adult adversities, and bolstering mechanisms for resilience, could potentially not only improve health outcomes in the near term, but also reduce future potential for violence victimization. Childhood and adult adversities are examples of how the social, economic, and environmental conditions in which people grow and develop shape quality of life and health outcomes for individuals and communities. These factors are also referred to as social determinants of health (Braveman & Gottlieb, 2014; Compton & Shim, 2015). Policy prevention strategies aimed at reducing adversity-related health disparities are therefore rooted reducing inequalities in income, housing, and educational attainment (Marmot, 2005; Metzler et al., 2017).
Specific examples of programs including family home visiting (Chartier et al., 2017) and school-based programs (Fortson et al., 2016) have demonstrated their effectiveness in building resilience and reducing the impacts of childhood adversities. Family home visiting is an evidence-based intervention strategies that may decrease hospitalizations due to childhood maltreatment (Chartier et al., 2017) Early childhood school-based interventions, such as universal prekindergarten or Headstart are effective strategies in reducing abuse and child welfare encounters (Green et al., 2014). Programs such as these, promote safe, nurturing environments that build resilience and coping strategies and reduce the likelihood of intergenerational experiences of violence and adversity (Merrick & Guinn, 2018).
Both adult adversities included in this analysis concerned gender-based violence. College campuses have initiated prevention efforts to create safer campus communities, yet campus sexual assault and IPV remain prevalent. (Campus Sexual Violence: Statistics ∣ RAINN, 2020; Cantor et al., 2020). Among students who have experienced adversities, prevention and resilience interventions could aid in reducing substance use on campus. Trauma-informed care creates a space for survivors of sexual assault or IPV to process re-traumatization in the context of past adversities or traumas and promotes positive coping techniques (Yoshimura & Campbell, 2016). Additionally, campus-based services designed to support survivors should take a race-conscious and intersectional approach to treatment that centres the experience of students with diverse identities (Crenshaw, 1990; Harris et al., 2021) . Finally, campus-based substance use prevention interventions should acknowledge social determinants of health, as well as social and environmental factors that influence help-seeking behaviour among racial/ethnic minority students exposed to adverse experiences (Srivastav et al., 2020).
4.1. Limitations
Our findings should be viewed in light of several limitations. First, our sample, while relatively racially diverse, was roughly 79% White. The large sample of White students likely permitted more nuanced cluster formation in White female students compared to Black, Asian, and Latina students. Second, college students are a select population of individuals who have chosen to pursue post-secondary education. While our sample includes students in both two- and four-year educational institutions in Minnesota and is likely more socioeconomically diverse than studies of 4-year college and university students only, our findings may not be generalizable to a broader population. Third, our experiences with childhood and adult adversities and substance use behaviours were self-reported. Fourth, while the timing of childhood and adult exposure to sexual assault were reported in separate questions, this outcome was collapsed to maintain adequate cell size for analysis. Fifth, the CSHS had overall response rates of 32% and 37% in 2015 and 2018, respectively which, although not optimal, are similar to response rates across other surveys of young adults (American College Health Association, 2015). Survey responses are subject to recall and social desirability bias. Nonetheless, assessing the occurrence of lifetime adversities in a large epidemiologic sample is difficult without retrospective reporting, thus these methods are the standard in this type of research. Finally, the ACEs index was developed in a medical context and does not capture a range of race, place, poverty, and historical and structural factors that disproportionately, negatively impact children and families who identify as Black, Indigenous and/or people of colour (Bruner, 2017). Finally, the present analyses assumed that substance use behaviours were preceded by adult adversities, an assumption that cannot be tested in this cross-sectional study.
4.2. Conclusion
There is little debate that substance use during college can lead to problematic health outcomes. However, discerning who is most at risk and identifying what predictors place students at high risk remains an open question. Comparatively few studies have considered how exposures to childhood and adult adversities vary by race/ethnicity and the extent to which these exposures predict substance use behaviours across racial/ethnic groups. The results of this study have implications for understanding the types of exposures that may place female racial/ ethnic minority students at increased risk for substance use behaviours during college. Of particular note are the consistently high rates of substance use behaviours in those with high adversities, across all racial/ethnic groups. In many cases, adversity history appeared to be at least as predictive of substance use as racial/ethnic background. Addressing lifetime adversities in substance use interventions could potentially improve effectiveness of efforts to prevent and mitigating risks of alcohol, marijuana, and tobacco use. Additionally, campus services that respond to reports of sexual assault, intimate partner violence, or stalking can provide additional referral services for women who may be at higher risk of increased substance use subsequent to their adversity experience. Experiencing different types of childhood and early adult adversity can put individuals on a trajectory of poorer health outcomes; however, those outcomes are not foregone conclusions. Future research should consider the efficacy of early intervention strategies to prevent ACEs and build resilience in children, which, in turn, can reduce the likelihood of exposure to early adult adversities and associated negative health outcomes. College is a critical developmental period where individuals begin to make their own decisions regarding their health and health risks. Detection and acknowledgement are the first steps in preventing negative outcomes from adverse experiences. There is a window of opportunity, during the college years for education, peer support and, when necessary, clinical intervention to transform downward trajectories into positive adaptive behaviour.
Role of Funding Sources
The authors gratefully acknowledge support from the Minnesota Population Center (P2C HD041023 & T32HD095134) funded through a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD).
Declarations of Interest:
This study was funded by Grant R21DK117466 from the National Institute for Diabetes and Digestive and Kidney Diseases (NIDDK)
Appendix
Appendix 1.
Indicator question and response coding
| Child Adversities | Variable Name | Question | Response Options | Coded Response |
|---|---|---|---|---|
| Childhood emotional abuse | How often did a parent or adult in your home ever swear at you, insult you, or put you down? | Never | No | |
| Once | No | |||
| More than once | Yes | |||
| Childhood physical abuse | How often did a parent or adult in your home ever hit, beat, kick, or physically hurt you in anyway? Do not include spanking. | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Childhood sexual abuse | How often did anyone at least 5 years older than you or an adult, ever touch you sexually? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Childhood sexual abuse | How often did anyone at least 5 years older than you or an adult, try to make you touch them sexually? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Childhood sexual abuse | How often did anyone at least 5 years older than you or an adult, force you to have sex? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Household mental illness | Did you live with anyone who was depressed, mentally ill, or suicidal? | Yes | Yes | |
| No | No | |||
| Don't know/Not sure | Missing | |||
| Household alcohol abuse | Did you live with anyone who was a problem drinker or alcoholic? | Yes | Yes | |
| No | No | |||
| Don't know/Not sure | Missing | |||
| Household drug abuse | Did you live with anyone who used illegal street drugs or who abused prescription medications? | Yes | Yes | |
| No | No | |||
| Don't know/Not sure | Missing | |||
| Incarcerated household member | Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility? | Yes | Yes | |
| No | No | |||
| Don't know/Not sure | Missing | |||
| Parental divorce/ separation | Were your parents separated or divorced? | Yes | Yes | |
| No | No | |||
| Parents never married | No | |||
| Don't know/Not sure | Missing | |||
| Witnessed family violence | How often did your parents or adults in your home ever slap, hit, kick, punch or beat each other up? | Never | No | |
| Once | Yes | |||
| More than once | Yes | |||
| Adult Adversities | Lifetime sexual assault | Have you experienced actual or attempted sexual intercourse without your consent or against your will? | Yes-within the past 12 months | Yes |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No | |||
| Lifetime sexual assault | Have you experienced actual or attempted sexual touching without your consent or against your will? | Yes-within the past 12 months | Yes | |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No | |||
| Adult Intimate partner physical abuse | Have you been slapped, kicked or pushed by your significant other or spouse/partner? | Yes-within the past 12 months | Yes | |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No | |||
| Adult Intimate partner emotional abuse | Have you been hurt by threats, "put-downs", or yelling from your significant other or spouse/partner? | Yes-within the past 12 months | Yes | |
| No-within the past 12 months | No | |||
| Yes- within your lifetime | Yes | |||
| No- within your lifetime | No |
Appendix 2.
Cluster formation by race/ethnicity
Appendix 3.
Fit statistics for the class formation by race/ethnicity
| Number of Classes |
Log- likelihood |
Adjusted BIC |
AIC | Entropy | Vuong-Lo-Mendell- Rubin p-value |
|---|---|---|---|---|---|
| 2015 & 2018 Black Women Sample (N=438) | |||||
| 1 | −2605.262 | 5245.428 | 5234.524 | 1 | |
| 2 | −2298.822 | 4670.362 | 4647.644 | 0.792 | 0.002 |
| 3 | −2232.804 | 4576.138 | 4541.607 | 0.784 | 0.0003 |
| 4 | −2191.635 | 4531.614 | 4485.27 | 0.824 | 0.2247 |
| 5 | −2158.379 | 4502.917 | 4444.758 | 0.833 | 0.3352 |
| 6 | −2138.152 | 4500.275 | 4430.303 | 0.849 | 0.0882 |
| 2015 & 2018 Asian Women Sample (N=940) | |||||
| 1 | −4527.201 | 9098.442 | 9078.402 | 1 | |
| 2 | −4128.23 | 8348.208 | 8306.459 | 0.742 | 0 |
| 3 | −4042.903 | 8225.264 | 8161.806 | 0.775 | 0.0003 |
| 4 | −3988.769 | 8164.705 | 8079.538 | 0.789 | 0.0039 |
| 5 | −3936.568 | 8108.013 | 8001.136 | 0.795 | 0.2186 |
| 2015 & 2018 Latina Women Sample (N=453) | |||||
| 1 | −2816.242 | 5667.791 | 5656.484 | 1 | |
| 2 | −2534.075 | 5141.707 | 5118.151 | 0.777 | 0 |
| 3 | −2467.217 | 5046.24 | 5010.435 | 0.818 | 0.0017 |
| 4 | −2414.632 | 4979.318 | 4931.263 | 0.812 | 0.0105 |
| 5 | −2389.858 | 4968.02 | 4907.717 | 0.824 | 0.2856 |
| 2015 & 2018 White Women Sample (N=7,458) | |||||
| 1 | −39664.957 | 79398.785 | 79353.914 | 1 | |
| 2 | −35822.863 | 71789.207 | 71695.726 | 0.776 | 0 |
| 3 | −34946.427 | 70110.945 | 69968.854 | 0.804 | 0 |
| 4 | −34465.685 | 69224.072 | 69033.37 | 0.759 | 0.005 |
| 5 | −34154.398 | 68676.109 | 68436.796 | 0.767 | 0 |
| 6 | −33984.996 | 68411.914 | 68123.991 | 0.76 | 0 |
| 7 | −33884.444 | 68285.421 | 67948.888 | 0.785 | 0.0011 |
| 8 | −33792.441 | 68176.025 | 67790.881 | 0.769 | 0.0137 |
Note: Final solutions are in bold. AIC=Akaike information criterion; BIC=Bayesian information criterion
Footnotes
Disclosure Statement No potential competing interest was reported by the authors
Ethics Approval: All authors listed on this manuscript have agreed to the listed authorship order and to submission of the manuscript in this form. Neither this manuscript nor one with substantially similar content under our authorship has been published or is being considered for publication elsewhere. The University of Minnesota’s Institutional Review Board Human Subject’s Committee approved all study protocols and all procedures performed with the study’s participants were in accordance with the ethical standards of the Institution and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All listed co-authors are aware that this manuscript is being submitted to the International Journal of Injury Control and Safety Promotion.
Consent to participate: None required. Our study is a secondary analysis of anonymously collected data, deemed exempt by our University's IRB.
Availability of Data: Requests for data can be made to Katherine Lust, PhD at Boynton Health Services lustx001@umn.edu
Availability of Code: All analyses were carried out in MPlus; code can be provided upon request.
CRediT author statement
Jessica K. Friedman: Writing- Original Draft, Writing- Review & Editing, Visualization N. Jeanie Santaularia: Formal Analysis, Writing- Review & Editing Dunia Dadi Writing- Review & Editing Darin J. Erickson: Methodology, Supervision Katherine Lust: Data Curation, Writing- Review & Editing, and Susan M. Mason: Writing- Review & Editing, Conceptualization, Supervision, Funding acquisition
References
- Ahern J, Karasek D, Luedtke AR, Bruckner TA, & van der Laan MJ (2016). Racial/Ethnic Differences in the Role of Childhood Adversities for Mental Disorders Among a Nationally Representative Sample of Adolescents. Epidemiology (Cambridge, Mass.), 27(5), 697–704. 10.1097/EDE.0000000000000507 [DOI] [PubMed] [Google Scholar]
- Allem JP, Soto DW, Baezconde-Garbanati L, & Unger JB (2015). Adverse childhood experiences and substance use among Hispanic emerging adults in Southern California. Addictive Behaviors, 50, 199–204. 10.1016/j.addbeh.2015.06.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College Health Association. (2015). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2015. American College Health Association. https://www.acha.org/documents/ncha/NCHA-II_WEB_SPRING_2015_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf [Google Scholar]
- Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, Williamson DF, & Giovino GA (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA, 282(17), 1652–1658. 10.1001/jama.282.17.1652 [DOI] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, & Giles WH (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232061/pdf/nihms340170.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Garnier-Dykstra LM, Cook ET, Caldeira KM, Vincent KB, Baron RA, & O’Grady KE (2013). Drug use patterns in young adulthood and post-college employment. Drug and Alcohol Dependence, 127(1–3), 1–3. 10.1016/j.drugalcdep.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P, & Gottlieb L (2014). The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Reports, 129, 19–31. 10.1177/00333549141291S206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruner C (2017). ACE, Place, Race, and Poverty: Building Hope for Children. ACAP Academic Pediatrics, 17(7), S123–S129. 10.1016/j.acap.2017.05.009. [DOI] [PubMed] [Google Scholar]
- Caldeira KM, Arria AM, O’Grady KE, Vincent KB, & Wish ED (2008). The occurrence of cannabis use disorders and other cannabis-related problems among first-year college students. Addictive Behaviors, 33(3), 397–411. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2247439/pdf/nihms38443.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldeira KM, O’Grady KE, Vincent KB, & Arria AM. (2012). Marijuana use trajectories during the post-college transition: Health outcomes in young adulthood. Drug and Alcohol Dependence, 125(3), 267–275. 10.1016/j.drugalcdep.2012.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campus Sexual Violence: Statistics ∣ RAINN. (2020). https://www.rainn.org/statistics/campus-sexual-violence [Google Scholar]
- Cantor D, Fisher B, Chibnall SH, Townsend R, Lee H, Thomas G, Bruce C, Association of American U, & Westat I (2020). Report on the AAU campus climate survey on sexual assault and sexual misconduct. /z-wcorg/. https://www.aau.edu/uploadedFiles/AAU_Publications/AAU_Reports/Sexual_Assault_Campus_Survey/Report%20on%20the%20AAU%20Campus%20Climate%20Survey%20on%20Sexual%20Assault%20and%20Sexual%20Misconduct.pdf [Google Scholar]
- Centers for Disease Control and Prevention, N. C. for C. D. P. and H. P., Division of Population Health. (2015). BRFSS Prevalence & Trends Data. https://www.cdc.gov/brfss/brfssprevalence/
- Chartier MJ, Brownell MD, Isaac MR, Chateau D, Nickel NC, Katz A, Sarkar J, Hu M, & Taylor C (2017). Is the Families First Home Visiting Program Effective in Reducing Child Maltreatment and Improving Child Development? Child Maltreatment, 22(2), 121–131. 10.1177/1077559517701230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, & Shim RS (2015). The Social Determinants of Mental Health. FOCUS, 13(4), 419–425. 10.1176/appi.focus.20150017 [DOI] [Google Scholar]
- Crenshaw K (1990). Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanford Law Review, 43(6), 1241–1300. https://heinonline.org/HOL/P?h=hein.journals/stflr43&i=1257 [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, & Anda RF (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics, 111(3), 564–572. 10.1542/peds.111.3.564 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Finkelhor D (2009). Childhood Victimization: Violence, Crime, and Abuse in the Lives of Young People. 10.1093/acprof:oso/9780195342857.001.0001 [DOI] [Google Scholar]
- Finkelhor D, Shattuck A, Turner H, & Hamby S (2013). Improving the adverse childhood experiences study scale. Archives of Pediatrics and Adolescent Medicine, 167(1), 70–75. 10.1001/jamapediatrics.2013.420 [DOI] [PubMed] [Google Scholar]
- Ford JD, Elhai JD, Connor DF, & Frueh BC (2010). Poly-Victimization and Risk of Posttraumatic, Depressive, and Substance Use Disorders and Involvement in Delinquency in a National Sample of Adolescents. Journal of Adolescent Health, 46(6), 545–552. 10.1016/j.jadohealth.2009.11.212 [DOI] [PubMed] [Google Scholar]
- Fortson BL, Klevens J, Merrick MT, Gilbert LK, Alexander SP, Atlanta GA. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (U.S.). Division of Violence Prevention., & National Center for Injury Prevention and Control (U.S.). Division of Violence Prevention. (2016). Preventing child abuse and neglect: A technical package for policy, norm, and programmatic activities. https://www.cdc.gov/violenceprevention/pdf/can-prevention-technical-package.pdf. [Google Scholar]
- Green BL, Ayoub C, Bartlett JD, Von Ende A, Furrer C, Chazan-Cohen R, Vallotton C, & Klevens J (2014). The effect of Early Head Start on child welfare system involvement: A first look at longitudinal child maltreatment outcomes. Children and Youth Services Review, 42, 127–135. 10.1016/j.childyouth.2014.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A, Nurius P, & Song C (2020). Differing trajectories of adversity over the life course: Implications for adult health and well-being. Child Abuse and Neglect, 102. Scopus. 10.1016/j.chiabu.2020.104392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JC, Karunaratne N, & Gutzwa JA (2021). Effective Modalities for Healing from Campus Sexual Assault: Centering the Experiences of Women of Color Undergraduate Student Survivors. Harvard Educational Review, 91(2), 248–272. 10.17763/1943-5045-91.2.248 [DOI] [Google Scholar]
- Health and Health-Related Behaviors 2015 College Student Health Survey Report. Minneapolis, MN. (2015). https://boynton.umn.edu/sites/boynton.umn.edu/files/2018-02/MNPostsecondaryStudents_CSHSReport_2015.pdf [Google Scholar]
- Health and Health-Related Behaviors 2018 College Student Health Survey Report. (2018). https://boynton.umn.edu/sites/boynton.umn.edu/files/2019-09/CSHS-2018-Minnesota-Post-secondary.pdf [Google Scholar]
- Jennison KM (2004). The short-term effects and unintended long-term consequences of binge drinking in college: A 10-year follow-up study. American Journal of Drug and Alcohol Abuse, 30(3), 659–684. 10.1081/ADA-200032331 [DOI] [PubMed] [Google Scholar]
- Jones CP (2001). Invited Commentary: “Race,” Racism, and the Practice of Epidemiology. American Journal of Epidemiology, 154(4), 299–304. 10.1093/aje/154.4.299 [DOI] [PubMed] [Google Scholar]
- Kobulsky JM, Yoon S, Bright CL, Lee G, & Nam B (2018). Gender-Moderated Pathways From Childhood Abuse and Neglect to Late-Adolescent Substance Use. Journal of Traumatic Stress, 31(5), 654–664. 10.1002/jts.22326 [DOI] [PubMed] [Google Scholar]
- Krieger H, Young CM, Anthenien AM, & Neighbors C (2018). The epidemiology of binge drinking among college-age individuals in the United States. Alcohol Research: Current Reviews, 39(1), 23–30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6104967/pdf/arcr-39-1-e1_a04.pdf [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Ehret PJ, Hummer JF, & Prenovost K (2012). Poor adjustment to college life mediates the relationship between drinking motives and alcohol consequences: A look at college adjustment, drinking motives, and drinking outcomes. Addictive Behaviors, 37(4), 379–386. 10.1016/j.addbeh.2011.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu SR, Kia-Keating M, & Nylund-Gibson K (2018). Patterns of adversity and pathways to health among White, Black, and Latinx youth. Child Abuse & Neglect, 86, 89–99. 10.1016/j.chiabu.2018.09.007 [DOI] [PubMed] [Google Scholar]
- Maguire-Jack K, Lanier P, & Lombardi B (2019). Investigating Racial Differences in Clusters of Adverse Childhood Experiences. American Journal of Orthopsychiatry, 90(1). 10.1037/ort0000405 [DOI] [PubMed] [Google Scholar]
- Manly JJ (2006). Deconstructing Race and Ethnicity: Implications for Measurement of Health Outcomes. Medical Care, 44(11), S10–S16. 10.1097/01.mlr.0000245427.22788.be [DOI] [PubMed] [Google Scholar]
- Marmot M (2005). Social determinants of health inequalities. Lancet, 365(9464), 1099–1104. 10.1016/s0140-6736(05)74234-3 [DOI] [PubMed] [Google Scholar]
- Meda SA, Gueorguieva RV, Pittman B, Rosen RR, Aslanzadeh F, Tennen H, Leen S, Hawkins K, Raskin S, Wood RM, Austad CS, Dager A, Fallahi C, & Pearlson GD (2017). Longitudinal influence of alcohol and marijuana use on academic performance in college students. PLOS ONE, 12(3), e0172213. 10.1371/journal.pone.0172213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick MT, Ford DC, Ports KA, & Guinn AS (2018). Prevalence of Adverse Childhood Experiences from the 2011-2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatrics, 172(11), 1038–1044. Scopus. 10.1001/jamapediatrics.2018.2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick MT, & Guinn AS (2018). Child Abuse and Neglect: Breaking the Intergenerational Link. American Journal of Public Health, 108(9), 1117–1118. 10.2105/AJPH.2018.304636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, & Janczewski CE (2018). Racial and ethnic differences in the prevalence of adverse childhood experiences: Findings from a low-income sample of U.S. women. Child Abuse & Neglect, 76, 480–487. 10.1016/j.chiabu.2017.12.012 [DOI] [PubMed] [Google Scholar]
- Mersky JP, Topitzes J, & Reynolds AJ (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the U.S. Child Abuse & Neglect, 37(11), 917–925. 10.1016/j.chiabu.2013.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzler M, Merrick MT, Klevens J, Ports KA, & Ford DC (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review, 72, 141–149. Scopus. 10.1016/j.childyouth.2016.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montalvo-Liendo N, Fredland N, McFarlane J, Lui F, Koci AF, & Nava A (2015). The Intersection of Partner Violence and Adverse Childhood Experiences: Implications for Research and Clinical Practice. Issues in Mental Health Nursing, 36(12), 989–1006. 10.3109/01612840.2015.1074767 [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Ports KA, Ford DC, & Merrick MT (2016). Adverse childhood experiences and sexual victimization in adulthood. Child Abuse and Neglect, 51, 313–322. Scopus. 10.1016/j.chiabu.2015.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebbe R, Nurius PS, Ahrens KR, & Courtney ME (2017). Adverse childhood experiences among youth aging out of foster care: A latent class analysis. Children and Youth Services Review, 74, 108–116. 10.1016/j.childyouth.2017.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santaularia NJ, Baker MR, Erickson D, Frazier P, Laska MN, Lust K, & Mason SM (2021). Classes of lifetime adversity in emerging adult women and men and their associations with weight status. Preventive Medicine, 146, 106455–106455. 10.1016/j.ypmed.2021.106455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME, & University of Michigan, I. for S. R. (2019). Monitoring the Future National Survey Results on Drug Use, 1975-2018. Volume II, College Students & Adults Ages 19-60. Institute for Social Research. University of Michigan. http://www.isr.umich.edu. [Google Scholar]
- Shields JD, Archiopoli AM, Bentley JM, Weiss D, Hoffmann J, White JM, Sharp MK, Hong Z, & Kimura M (2016). Binge-Drinking Attitudes and Behaviors Among Hispanic and Non-Hispanic College Students: Suggestions for Tailoring Health Campaign Messages. Hispanic Journal of Behavioral Sciences, 38(2), 243–263. 10.1177/0739986316633436 [DOI] [Google Scholar]
- Shin SH, McDonald SE, & Conley D (2018). Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addictive Behaviors, 78, 187–192. 10.1016/j.addbeh.2017.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastav A, Strompolis M, Moseley A, & Daniels K (2020). The Empower Action Model: A Framework for Preventing Adverse Childhood Experiences by Promoting Health, Equity, and Well-Being Across the Life Span. Health Promotion Practice, 21(4), 525–534. 10.1177/1524839919889355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, & Wang X (2020). Structural equation modeling applications using Mplus. doi: 10.1002/9781118356258. [DOI] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, & Lee H (2002). Trends in College Binge Drinking During a Period of Increased Prevention Efforts. Journal of American College Health, 50(5), 203. 10.1080/07448480209595713 [DOI] [PubMed] [Google Scholar]
- Widom CS, Czaja S, & Dutton MA (2014). Child abuse and neglect and intimate partner violence victimization and perpetration: A prospective investigation. Child Abuse Negl. Child Abuse and Neglect, 38(4), 650–663. /z-wcorg/. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4035378/pdf/nihms540880.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshimura CG, & Campbell KB (2016). Interpersonal Violence and Sexual Assault: Trauma-Informed Communication Approaches in University Counseling Centers. Journal of College Student Psychotherapy, 30(4), 300–312. 10.1080/87568225.2016.1221720 [DOI] [Google Scholar]
- Young-Wolff KC, Hellmuth J, Jaquier V, Swan SC, Connell C, & Sullivan TP (2013). Patterns of Resource Utilization and Mental Health Symptoms Among Women Exposed to Multiple Types of Victimization: A Latent Class Analysis. Journal of Interpersonal Violence, 28(15), 3059–3083. 10.1177/0886260513488692 [DOI] [PMC free article] [PubMed] [Google Scholar]