Abstract
Objectives
To report the characteristics of vaccine-hesitant individuals in a French-speaking adult population in the context of the SARS-CoV-2 pandemic; and to identify predictors of hesitancy about Covid-19-related vaccines.
Methods
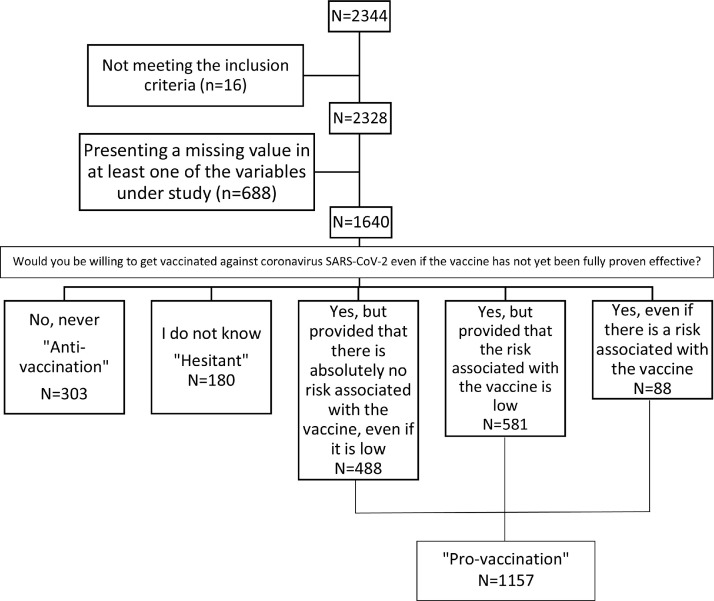
Between April and May 2020, 1640 French-speaking adults participating in an online cohort were classified according to their attitudes towards vaccination as: “hesitant”, “anti-vaccination”, and “pro-vaccination”. Descriptive statistics, univariate multinomial regression models and multivariate analyses were compiled and carried out.
Results
At the time of inclusion, compared to pro-vaccination participants, hesitant participants were more frequently females (p=0.044), not annually vaccinated against flu (p=0.026), less optimistic about the discovery of a treatment against Covid-19 in a few months (p<0.001), less ready to undergo this treatment (p<0.001), presenting less trust in the ability of public health authorities to control the pandemic (p=0.036) and reporting lower scores on knowledge-related scales (p values from <0.001 to 0.002). Univariate analyses confirmed these results with odds ratios ranging from 1.51 [1.05-2.17] to 2.19 [1.56-3.07]. In the multivariate models, the remaining variables associated with hesitant compared to pro-vaccination attitudes were discovery of a treatment against Covid-19 in a few months (OR=2.57 [1.73-3.81]), being ready to undergo this treatment (OR=7.07 [4.89-10.22]), digital vaccine literacy (OR=1.70 [1.14-2.54]) and general health literacy (OR=1.49 [1.03-2.15]).
Discussion
In a continuum of relative acceptance of Covid-19-related vaccines, hesitant individuals were situated in between the behaviours and characteristics of pro-vaccination and anti-vaccination groups. While their characteristics were in line with the literature, this study was the first to report data on health literacy, digital vaccine literacy and capacity to detect fake news associated with vaccine hesitancy.
Conclusions
While failing to identify straightforward predictors, findings suggest that continued education and communication campaigns focused on improving vaccine literacy, particularly among women younger than 35 years, could heighten the proportion of persons accepting vaccination.
Keywords: Vaccine hesitancy, Cohort, Profiling, Covid-19
Résumé
Objectifs
Décrire les caractéristiques des personnes hésitantes vis-à-vis de la vaccination dans une population adulte francophone dans le contexte de la pandémie de SARS-CoV-2, et identifier les déterminants de l'hésitation vis-à-vis des vaccins contre la Covid-19.
Méthodes
1 640 adultes francophones participant à une cohorte en ligne, entre avril et mai 2020, ont été classés en fonction de leur attitude vis-à-vis de la vaccination : "hésitant", "anti-vaccination" et "pro-vaccination". Les données ont été analysées à l'aide de statistiques descriptives, de modèles de régression multinomiale univariés et d'analyses multivariées.
Résultats
Au moment de l'inclusion, par rapport aux pro-vaccination, les hésitants étaient plus souvent des femmes (p=0,044), moins vaccinés contre la grippe chaque année (p=0,026), moins optimistes quant à la découverte d'un traitement contre la Covid-19 dans quelques mois (p<0,001), moins prêts à prendre ce traitement (p<0,001), présentaient une moindre confiance dans les autorités de santé publique pour contrôler la pandémie (p=0,036) et rapportaient des scores plus faibles sur les échelles de connaissances (valeurs p de <0,001 à 0,002). Les analyses univariées ont confirmé ces résultats avec des odds ratios (OR) variant de 1,51 [1,05-2,17] à 2,19 [1,56-3,07]. Dans les modèles multivariés, les variables associées à l'hésitation par rapport aux pro-vaccination étaient la découverte d'un traitement contre la Covid-19 dans quelques mois (OR=2,57 [1,73-3,81]), le fait d'être prêt à prendre ce traitement (OR=7,07 [4,89-10,22]), la littératie vaccinale digitale (OR=1,70 [1,14-2,54]) et la littératie générale en santé (OR=1,49 [1,03-2,15]).
Discussion
Les attitudes des hésitants se situaient entre les comportements et les attitudes des groupes pro-vaccination et anti-vaccination. Leurs caractéristiques étaient conformes à la littérature, mais cette étude était la première à rapporter des données sur la littératie en matière de santé et des vaccins dans le numérique, et la capacité à détecter les fake news associées à l'hésitation en matière de vaccins.
Conclusions
Sans identifier de déterminants spécifiques, les résultats suggèrent que la mise en place de campagnes d'éducation et de communication axées sur l'amélioration de la littératie sur les vaccins, en particulier chez les femmes de moins de 35 ans, pourrait réduire le nombre d'hésitants.
Mots clés: Hésitation vaccinale, Cohorte, Profil, Covid-19
1. Introduction
Vaccine hesitancy is defined as delay in acceptance or refusal of vaccination despite availability of vaccination services [1]. This phenomenon is particularly prominent in France, where about 40 % of the population questions the effectiveness of vaccines [2,3]. By way of comparison, in Nordic countries, only 27 % of the population think vaccines are unsafe [4]. Studies have reported that considering vaccines as ineffective or unsafe is associated with higher vaccine hesitancy and lower vaccine uptake [2,5]. Seasonal flu shots are relatively low in France, largely inferior to the World Health Organisation (WHO) recommendations : one French citizen out of two has not been vaccinated against influenza [2]. In comparison, 61 % of the German population and 67.5 % of the Italian population think the seasonal influenza vaccination is important and consequently get vaccinated [6]. As regards compulsory vaccination, French vaccine hesitancy is likewise high, with parents representing the most hesitant portion of the general population (73 %), while 93 % of parents in Spain are pro-vaccination [7]. In the same line of thought, doubts about the effectiveness and safety of Covid-19-related vaccines are now being diffused worldwide [8]. Furthermore, some people may feel unconcerned, and do not consider vaccination as a priority [6,9]. Their attitude may induce vaccine hesitancy and consequently limit vaccine uptake.
There exist several identified factors determining vaccine hesitancy, including Covid-19 vaccines [10]. Personal characteristics such as sex, age, comorbidities, having children, and self-rated health are known to impact vaccine-related decision-making [11]. Furthermore, false beliefs and misconceptions about vaccination can be fuelled by information obtained through Internet sources [9]. Elevated literacy skills, time invested in extensive research [12,13] and ability to detect fake news can also contribute to rational decision-making on vaccination [14,15]. On the other hand, distrust in public authorities during vaccine-related controversies and scepticism generated by the unusually rapid development of vaccines against coronavirus SARS-CoV-2 can favour vaccine hesitancy [16]. Over recent months, no less than three vaccines have shown satisfactory efficacy and are currently administered in different population groups throughout the world. And yet, when vaccination against the coronavirus started early in 2021 in France, some people continued to express reluctance [16,17]. This trend is in line with worldwide hesitancy about these new vaccines [17].
Delineating in the French population the profile of those who are hesitant about SARS-CoV-2 vaccination can help to tailor the format and contents of communication campaigns and policy initiatives designed to promote Covid-19 vaccination. This is a pivotal upcoming challenge.
The objectives of this study were (1) to report the characteristics of vaccine-hesitant individuals in a French-speaking adult population in the context of the SARS-CoV-2 pandemic ; and (2) to identify predictors of hesitancy about Covid-19-related vaccines. Comparison between hesitant and pro-vaccination groups was sought out insofar as the ultimate aim of the study was to present the factors that could induce the hesitant group to accept vaccination.
2. Methods
2.1. The CONFINS cohort
The CONFINS cohort study (www.confins.org) was initiated on the 8th of April 2020 to monitor French-speaking people's well-being and mental health during the Covid-19 lockdown. The cohort was online-based and participation was voluntary. Participants were recruited through social media posts, press releases, podcasts, TV programs and mailing were. The sole eligibility criterion was being aged 18+. For the purposes of this study only, we excluded subjects who had declared “other” for the sex variable since there were only 16 of them (0.7 %). Wishing to attain sufficient statistical power, we also excluded those reporting missing data on at least one variable in the analyses. A sensitivity analysis tested result robustness and enhanced understanding of the relationships between outcome and exposure variables. Data covered the period culminating on May 10th, one day before the end of the first lockdown in France.
The CONFINS questionnaire contained 77 items drawn up by several researchers through different stages of drafts and reviews. Participants completed the online survey after reading the written consent form and explicitly agreeing to participate. The cohort was approved by the French Committee for the Protection of Individuals (Comité de Protection des Personnes - CPP, nr. 46-2020) and the French National Agency for Data Protection (Commission Nationale Informatique et Libertés - CNIL, nr. MLD/MFI/AR205600), and data were stored and analyzed according to the General Data Protection Regulation (EU GDPR). The study was conducted in accordance with the Declaration of Helsinki.
2.2. Outcome measure : defining the hesitant population
In order to characterise the group of hesitant subjects, we formulated the question : “Would you be willing to get vaccinated against coronavirus SARS-CoV-2 even if the vaccine has not yet been fully proven effective ? ”. Response modalities were : “No, never” ; “Yes, even if there is a risk associated with the vaccine” ; “Yes, but provided that the risk associated with the vaccine is low” ; “Yes, but provided that there is absolutely no risk associated with the vaccine, even if it is low” ; “I don't know”. We allocated the answer “No, never” to the “anti-vaccination group”, the answer “I do not know” to the “hesitant group” and the three “Yes” modalities to the “pro-vaccination” group.
2.3. Covariates : predictors of vaccine hesitancy
Sociodemographic and medical data included sex ; age ; marital status ; having children ; being a student ; studying or working in the health domain ; self-perceived health (using the WHO standardized questionnaire, “How is your health in general ? ” : very good/good/fair/bad/very bad) ; and lifelong medical history (at least of the following : cardiovascular disease, hypertension, diabetes, chronic digestive disease, cancer, asthma or other respiratory disease, mental illness, other). We asked whether participants updated themselves on vaccination and whether they were annually vaccinated against the flu.
We also asked specific questions on Covid-19 : degree of concern about Covid-19 as a health issue (categories : 1-2 “low concern”, 3 “medium concern” and 4-5 “high concern”) ; perceived dangerousness of Covid-19 (categories : 0-3 “low dangerousness”, 4-6 “medium dangerousness” and 7-10 “high dangerousness) ; agreeing that the epidemic will last several months and that our lives will be durably strongly affected (no vs yes) ; trust in the discovery of a treatment (no, yes, I do not know) ; ready to take a treatment against Covid-19 that has yet to be conclusively proven effective (no never, yes, I do not know) ; and trust in public authorities to control the pandemic (categories : 0-3 “low trust”, 4-6 “medium trust” and 7-10 “high trust”).
To evaluate knowledge and literacy, we used four tools : 1) General health literacy (GHL) on the 5th dimension of the Health Literacy Questionnaire (HLQ), i.e. critical literacy [13,18] measured through 5 items with the following categories : “bad GHL” (0-9) and “good GHL” (10-15) ; 2) Scale on knowledge and beliefs about vaccination containing 6 items scored in the following categories : “bad” (6-18) and “good” (19-30) ; 3) Digital vaccine literacy (DVL), which contained 7 items with the following categories : “bad DVL” (7-20) and “good DVL” (21-33) ; and 4) Capacity to detect Covid-19-related fake news with the categories : “bad capacity to detect fake news” (0-5) and “good capacity to detect fake news” (6-8). Means and standard deviations were reported for all tools which are presented in the Supplementary Material.
The STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) guidelines were followed.
2.4. Statistical analyses
“Hesitant”, “anti-vaccination” and “pro-vaccination” groups were described according to sociodemographic characteristics, variables relating to Covid-19 and knowledge-related scores, showing numbers and percentages for qualitative variables and means plus standard deviations ( ± SD) for quantitative variables. We then made univariate comparisons of “hesitant” to the other two groups using Chi2 independence tests for categorical variables and comparison of means (t-test if normal law) with verification of the homoscedasticity of variances beforehand. We created univariate multinomial regression models, with the "pro-vaccination" group as the reference category, in order to study the association between characteristics of vaccine hesitancy and the likelihood of being in "hesitant" or "anti-vaccination" groups. This choice of statistical modelling enabled comparison between “anti-vaccination” and “hesitant” groups versus “pro-vaccination” individuals and observation of trends toward differentiation between “anti-vaccination” and “hesitant” individuals. Lastly, we performed multivariate analyses in which all study variables were included in an initial multinomial regression model. In order to identify the odds ratios related to the degree of vaccine acceptance, a stepwise top-down procedure was applied. Interactions with a p-value > 0.25 were removed from the model ; the covariates were then removed one by one until all p-values in the model were below the statistical significance level of 0.05, except for variables that could potentially be confounding factors. We obtained a final multivariate multinomial regression model. Data were analyzed using SAS® version 9.3.
2.5. Missing values
We considered that some data were missing at random, i.e. MAR (Missing At Random) type (see Figure 1 below, n=688). A multiple imputation method using chained equations (MICE) was consequently performed as a sensitivity analysis concerning the entire sample. With complete data, the variables present in the final regression models and with missing data could be imputed. The validity of the imputation was checked by comparing the observed data with the missing data of the indicator variables used for imputation of missing data. In addition, Rubin's three diagnostic parameters were checked : low relative increase in variance, a fraction of missing information lower than the proportion of missing values and relative efficiency close to 100 % [19]. In the end, missing values concerned the following variables : age, being a student, scale on knowledge and beliefs about vaccination, capacity to detect fake news scale and general health literacy scale. Twenty-three categorical variables (22 for exposure, e.g., sex, age, and one for vaccine hesitancy) were initially used (Table 1 ). Following which, 15 were retained in the final model. We chose an imputation number of 20, which corresponded to satisfactory values of Rubin's diagnostic parameters.
Figure 1.
Study flowchart
Table 1.
Sociodemographic characteristics of the three study groups (N=1640)
| Hesitant (N=180) |
Anti-vax (N=303) |
p-valueα | Pro-vax (N=1157) |
p-valueβ | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Sex | 0.489 | 0.044 | ||||||
| Male | 31 | 17.2 | 45 | 14.9 | 278 | 24.0 | ||
| Female | 149 | 82.8 | 258 | 85.1 | 879 | 76.0 | ||
| Age (years) | 0.079 | 0.743 | ||||||
| 18-34 | 149 | 82.8 | 268 | 88.4 | 969 | 83.8 | ||
| ≥ 35 | 31 | 17.2 | 35 | 11.6 | 188 | 16.2 | ||
| Marital status | 0.218 | 0.121 | ||||||
| Couple | 93 | 51.7 | 174 | 57.4 | 669 | 57.8 | ||
| Single | 87 | 48.3 | 129 | 42.6 | 488 | 42.2 | ||
| Having children | 0.358 | 0.630 | ||||||
| No | 156 | 86.7 | 271 | 89.4 | 987 | 85.3 | ||
| Yes | 24 | 13.3 | 32 | 10.6 | 170 | 14.7 | ||
| Student | 0.283 | 0.303 | ||||||
| No | 65 | 36.1 | 95 | 31.4 | 373 | 32.2 | ||
| Yes | 115 | 63.9 | 208 | 68.6 | 784 | 67.8 | ||
| Study or work in health domain | 0.008 | 0.092 | ||||||
| No | 113 | 62.8 | 225 | 74.3 | 649 | 56.1 | ||
| Yes | 67 | 37.2 | 78 | 25.7 | 508 | 43.9 | ||
| Self-perceived health | 0.594 | 0.117 | ||||||
| Bad | 30 | 16.7 | 45 | 14.9 | 144 | 12.4 | ||
| Good | 150 | 83.3 | 258 | 85.1 | 1013 | 87.6 | ||
| Lifelong medical history* | 0.803 | 0.191 | ||||||
| No | 87 | 48.3 | 150 | 49.5 | 499 | 43.1 | ||
| Yes | 93 | 51.7 | 153 | 50.5 | 658 | 56.9 | ||
| Up-to-date vaccination | 0.003 | 0.526 | ||||||
| No | 6 | 3.3 | 27 | 8.9 | 61 | 5.3 | ||
| Yes | 162 | 90.0 | 236 | 77.9 | 1015 | 87.7 | ||
| I do not know | 12 | 6.7 | 40 | 13.2 | 81 | 7.0 | ||
| Being vaccinated against flu each year | <0.001 | 0.026 | ||||||
| No | 137 | 76.1 | 274 | 90.4 | 785 | 67.8 | ||
| Yes | 43 | 23.9 | 29 | 9.6 | 372 | 32.2 | ||
: p-value for the comparison hesitant vs anti-vax ; β : p-value for the comparison hesitant vs pro-vax
At least one among the following : cardiovascular disease, hypertension, diabetes, chronic digestive disease, cancer, asthma or other respiratory disease, mental illness, other
3. Results
3.1. Characteristics of hesitant individuals compared to pro-vaccination and anti-vaccination individuals
A total of 2344 individuals completed the CONFINS questionnaire : 16 were excluded since they declared “other” for gender, a number that was too small to be taken into account in the analyses ; and 688 presented at least one missing value among the variables of interest. All in all, there were 1640 full cases (Figure 1).
Based on an a priori classification, we observed that 11.0 % were “hesitant” (180/1640), 70.5 % “pro-vaccination” (1157/1640), and 18.5 % “anti-vaccination” (303/1640). Concerning socio-demographic characteristics, compared to “pro-vaccination”, “hesitant” individuals were more frequently females (p=0.044) and less vaccinated against flu each year (p=0.026). However, when compared to “anti-vaccination”, they were more vaccinated against flu each year (p<0.001). Details are given in Table 1.
As far as specific questions about Covid-19 are concerned, compared to “pro-vaccination”, “hesitant” individuals were less optimistic about the discovery of a treatment against Covid-19 in a few months (p<0.001), less ready to undergo a treatment against Covid-19 with low risk (p<0.001), and manifested less trust in public health authorities to control the pandemic (4.7, SD ± 2.3 vs 5.1, SD ± 2.5, p=0.036). Compared to “anti-vaccination”, “hesitant” individuals were more optimistic about discovery of a treatment (p<0.001), more willing to undergo a treatment (p<0.001) and had more trust in public authorities to control the pandemic (p=0.019). Details are in Table 1S in the Supplementary Material.
When looking at knowledge-related scores, compared to “pro-vaccination”, “hesitant” participants presented lower scores on all scales, i.e., knowledge and beliefs about vaccination (21.9, SD ± 2.9 vs 22.3, SD ± 2.4, p<0.001), digital vaccine literacy (21.7, SD ± 2.8 vs 22.7, SD ± 2.4, p<0.001), capacity to detect fake news (6.2, SD ± 1.2 vs 6.6, SD ± 1.0, <0.001), and general health literacy (9.5, SD ± 3.2 vs 9.9, SD ± 2.6, p=0.002). Only regarding knowledge and beliefs about vaccination did “hesitant” differ from “anti-vaccination” participants (21.9, SD ± 2.9 and 20.0, SD ± 3.3, respectively, p<0.001). Details are given in Table 2 S in the Supplementary Material.
Table 2.
Univariate multinomial regression models of the associations between being “hesitant” or “anti-vaccination”, compared to being “pro-vaccination” (N=1640)
| Anti-vaccination vs Pro-vaccination |
Hesitant vs Pro-vaccination |
|||
|---|---|---|---|---|
| OR | 95 % CIs | OR | 95 % CIs | |
| SOCIO-DEMOGRAPHIC CHARACTERISTICS | ||||
| Sex Female vs Male | 1.81 | [1.29-2.56] | 1.52 | [1.01-2.29] |
| Age (years) ≥ 35 vs 18-34 | 0.67 | [0.46-0.99] | 1.07 | [0.71-1.63] |
| Marital status Single vs Couple | 1.02 | [0.79-1.31] | 1.28 | [0.94-1.76] |
| Having children No vs Yes | 1.46 | [0.98-2.18] | 1.12 | [0.71-1.77] |
| Student Yes vs No | 1.04 | [0.79-1.37] | 0.84 | [0.61-1.17] |
| Study or work in the health domain Yes vs No | 0.44 | [0.33-0.59] | 0.76 | [0.55-1.05] |
| Self-perceived health Good vs Bad | 0.82 | [0.57-1.17] | 0.71 | [0.46-1.09] |
| Lifelong medical history* Yes vs No | 0.77 | [0.60-0.99] | 0.81 | [0.59-1.11] |
| Up-to-date vaccination | ||||
| No vs Yes | 1.90 | [1.18-3.06] | 0.62 | [0.26-1.45] |
| I do not know vs Yes | 2.12 | [1.42-3.18] | 0.93 | [0.50-1.74] |
| Not being vaccinated against flu each year | 4.48 | [3.00-6.69] | 1.51 | [1.05-2.17] |
| ANSWERS RELATED TO COVID-19 | ||||
| Degree of concern about Covid-19 as a health issue | ||||
| Low worry (1-2) vs High worry (4-5) | 1.13 | [0.76-1.68] | 1.15 | [0.69-1.93] |
| Medium worry (3) vs High worry (4-5) | 1.06 | [0.65-1.71] | 1.56 | [0.87-2.80] |
| Perceived Dangerousness of Covid-19 | ||||
| Low worry (0-3) vs High worry (7-10) | 1.04 | [0.74-1.46] | 1.14 | [0.75-1.73] |
| Medium worry (4-6) vs High worry (7-10) | 0.88 | [0.66-1.17] | 0.91 | [0.64-1.31] |
| Agreeing with the fact that the epidemic will last several months and that our lives will strongly and durably affected Yes vs No |
0.94 | [0.69-1.29] | 0.89 | [0.60-1.31] |
| Trust in the discovery of a treatment | ||||
| No vs Yes | 2.33 | [1.46-3.73] | 0.44 | [0.14-1.43] |
| I do not know vs Yes | 1.25 | [0.89-1.77] | 2.73 | [1.92-3.88] |
| Ready to undergo a treatment against Covid-19 that has yet to be conclusively proven effective | ||||
| No vs Yes | 8.41 | [5.94-11.92] | 1.50 | [0.72-3.11] |
| I do not know vs Yes | 2.04 | [1.41-2.96] | 7.75 | [5.47-10.99] |
| Trust in public authorities to control the pandemic | ||||
| Low trust (0-3) vs High trust (7-10) | 2.28 | [1.64-3.16] | 1.76 | [1.16-2.68] |
| Medium trust (4-6) vs High trust (7-10) | 1.29 | [0.92-1.81] | 1.62 | [1.08-2.42] |
| KNOWLEDGE-RELATED SCALES | ||||
| Scale on knowledge and beliefs about vaccination Bad (6-18) vs Good (19-30) | 5.85 | [4.22-8.12] | 1.85 | [1.13-3.02] |
| Digital Vaccine Literacy scale Bad (7-20) vs Good (21-33) | 2.10 | [1.60-2.77] | 2.19 | [1.56-3.07] |
| Capacity to detect fake news scale Bad (0-5) vs Good (6-8) | 1.98 | [1.43-2.73] | 2.03 | [1.37-3.00] |
| General health literacy scale Bad (0-9) vs Good (10-15) | 1.66 | [1.28-2.14] | 1.57 | [1.14-2.16] |
At least one among the following : cardiovascular disease, hypertension, diabetes, chronic digestive disease, cancer, asthma or other respiratory disease, mental illness, other
OR : Odds Ratio ; 95 % CIs : Confidence Interval at 95 %.
3.2. Univariate multinomial regression models
When compared to “pro-vaccination”, “hesitant” individuals were more likely to be females (OR=1.52 (95 % CI [1.01-2.29]). They were also less likely to be vaccinated against flu each year (OR=1.51 [1.05-2.17]) ; to know whether a treatment against Covid-19 would be found (OR=2.73 [1.92-3.88]) ; to know whether they would take this treatment against Covid-19 (OR=2.04 [1.41-2.96]) ; to have high trust in public authorities to control the pandemic (OR=1.76[1.16-2.68] and OR=1.62[1.08-2.42], respectively) ; to have a good level of knowledge and beliefs about vaccination (OR=1.85 [1.13-3.02]) ; to have a good level of digital vaccine literacy (OR=2.19 [1.56-3.07]) ; to present a good capacity to detect fake news (OR=2.03 [1.37-3.00]) ; and to present a high level of general health literacy (OR=1.57 [1.14-2.16]). For the majority of the variables (e.g., sex, being vaccinated against flu each year, general health literacy), the direction of the association between “hesitant” and “anti-vaccination” was the same, i.e. the odds concerning “hesitant” between “pro-vaccination” and “anti-vaccination” participants were similar. Detailed results of the univariate analyses are reported in Table 2.
3.3. Multivariate analysis
Table 3 presents the results of the multivariate analyses adjusted on covariates.
Table 3.
Multivariate multinomial regression models of the associations between being “hesitant” or “anti-vaccination”, compared to being “pro-vaccination” (N=1640)
| Anti-vaccination vs Pro-vaccination |
Hesitant vs Pro-vaccination |
|||
|---|---|---|---|---|
| OR | 95 % CIs | OR | 95 % CIs | |
| SOCIO-DEMOGRAPHIC CHARACTERISTICS | ||||
| Sex : Among males* | ||||
| Student (Yes vs No) | 4.63 | [1.85-11.59] | 1.53 | [0.62-3.78] |
| Lifelong medical history*(Yes vs No) | 0.35 | [0.16-0.74] | 0.64 | [0.29-1.44] |
| Sex : Among females* | ||||
| Student (Yes vs No) | 1.03 | [0.69-1.51] | 0.87 | [0.55-1.38] |
| Lifelong medical history⁎⁎(Yes vs No) | 1.01 | [0.73-1.41] | 0.79 | [0.54-1.16] |
| Age (years) ≥ 35 vs 18-34 | 0.83 | [0.49-1.41] | 1.12 | [0.64-1.97] |
| Study or work in the health domain Yes vs No | 0.78 | [0.55-1.11] | 1.01 | [0.69-1.49] |
| Up-to-date vaccination | ||||
| No vs Yes | 1.69 | [0.95-2.99] | 0.52 | [0.21-1.30] |
| I do not know vs Yes | 1.64 | [1.02-2.65] | 0.54 | [0.27-1.10] |
| Being vaccinated against flu each year No vs Yes | 4.34 | [2.66-7.08] | 1.42 | [0.93-2.17] |
| ANSWERS RELATED TO COVID-19 | ||||
| Trust in the discovery of a treatment | ||||
| No vs Yes | 2.08 | [1.15-3.74] | 0.38 | [0.11-1.29] |
| I do not know vs Yes | 1.33 | [0.89-2.00] | 2.57 | [1.73-3.81] |
| Ready to take a treatment against COVID-19 that has yet to be conclusively proven effective | ||||
| No vs Yes | 15.33 | [9.99-23.53] | 1.86 | [0.88-3.94] |
| I do not know vs Yes | 2.11 | [1.40-3.18] | 7.07 | [4.89-10.22] |
| Trust in public authorities to control the pandemic | ||||
| Low trust (0-3) vs High trust (7-10) | 1.77 | [1.19-2.63] | 1.41 | [0.88-2.24] |
| Medium trust (4-6) vs High trust (7-10) | 1.08 | [0.73-1.61] | 1.37 | [0.88-2.12] |
| KNOWLEDGE-RELATED SCALES | ||||
| Scale on knowledge and beliefs about vaccination Bad (6-18) vs Good (19-30) | 4.11 | [2.77-6.09] | 1.53 | [0.88-2.66] |
| Digital Vaccine Literacy scale Bad (7-20) vs Good (21-33) | 1.10 | [0.78-1.56] | 1.70 | [1.14-2.54] |
| Capacity to detect fake news scale Bad (0-5) vs Good (6-8) | 1.64 | [1.11-2.42] | 1.54 | [0.99-2.39] |
| General health literacy scale Bad (0-9) vs Good (10-15) | 1.23 | [0.90-1.68] | 1.49 | [1.03-2.15] |
OR : Odds Ratio ; 95 % CIs : Confidence Interval at 95 %.
We tested interactions and found that sex was significantly associated with being a student and lifelong medical history, adjusted on all covariates.
At least one among the following : cardiovascular disease, hypertension, diabetes, chronic digestive disease, cancer, asthma or other respiratory disease, mental illness, other
Compared to “pro-vaccination”, “hesitant” individuals were more likely : not to know if a treatment would be discovered compared to those trusting in this discovery (OR=2.57 ; [1.73-3.81]) ; not to know if they would be ready to take a treatment against Covid-19 that has not yet been fully proven effective compared to those who declared themselves ready (OR=7.07 [4.89-10.22]) ; to have a bad level of digital vaccine literacy (OR=1.70 [1.14-2.54]) ; and to have a bad level of general health literacy (OR=1.49 [1.03-2.15]).
Multivariate analyses with multiple imputation are available in Table 3S in the Supplementary Material. Results of the imputation were robust and in accordance with findings without imputation. As a general rule, the imputed ORs followed the same pattern as the non-imputed ORs.
4. Discussion
This study was focused on the profiles of hesitant individuals as the group that could be induced to accept vaccination. While the anti-vaccination group might be difficult to convince concerning the benefits of a vaccine against coronavirus, sceptical persons might be more easily positively influenced [20,21], the objective being to prevent them from switching to anti-vaccination attitudes. Anti-vaccination individuals are those who express ardent vaccine denial and outright refusal to be vaccinated, rejecting scientific consensus on vaccines. In fact, they are not representative of numerous persons who might simply have questions or worries about vaccines, and are doubtful or hesitant.
Results showed that 11.0 % of participants were hesitant, which is a percentage more than twice as low as in a European online survey conducted on 7662 adults in seven European countries including France, which reported 28 % of hesitators [21]. On the other hand, anti-vaccination individuals were 18.5 %, a percentage which differing from those of other studies, which reported around 10 % [16] or 29 % [25]. These differences in percentages might be due to type of questions and answer modalities as well as recruitment strategies corresponding to varied degrees of representativeness [17]. More specifically, the definition we used for vaccine hesitancy was based on one question only. While larger scales indeed exist [41,42], some studies have used only one item to rapidly and readily measure in France [16,21,33,40] and elsewhere [43], [44], [45], as in the present study.
Descriptive statistics and univariate analyses showed that, compared to pro-vaccination, hesitant participants were more frequently female. This is in line with previous research in which womanhood is usually a predictor of reluctance to get vaccinated [22,23]. This is also the case for Covid-19 vaccines [16,24,25]. In the literature, the underpinning hypothesis is that women are usually more concerned about the dangerousness of vaccines with regard to their fertility or pregnancy, and about their children's health, and are consequently more cautious, and keener on alternative medicine [26].
Compared to pro-vaccination participants, and according to both descriptive and univariate analyses, hesitant persons were not vaccinated against flu each year. People not willing to receive influenza vaccination during ordinary years have a strong tendency to be reluctant about a future Covid-19 vaccine ; this has also been observed in other studies [27], [28], [29]. Previous research has documented that vaccination status is associated with vaccine hesitancy : those who hesitate are usually not in compliance with all recommended vaccination protocols [7,30]. In a European online survey [21], the reasons why respondents were unsure about being vaccinated had generally to do with the potential side effects of a vaccine and uncertain safety [23,25,31].
Descriptive, univariate and multivariate analyses reported that hesitant individuals were also less optimistic about the discovery of a treatment against Covid-19 in a few months and less ready to undergo the treatment, even at low risk to their health. Moreover, they presented the highest odds ratio for all variables. These results confirm a tendency to disbelieve health and scientific authorities on the production of medical drugs and treatments, including vaccines. For hesitant individuals, a vaccine or a new treatment seems riskier than Covid-19 itself. This reasoning can be explained by the Health Belief Model, which considers vaccination and treatment decisions as a function of perceived susceptibility to and severity of disease, along with as concern about the risks and benefits of vaccines and treatments [32].
Previous research has underlined the need to consider the importance of trust in Covid-19-related vaccine hesitancy [25,33]. According to descriptive and univariate analyses, hesitant individuals are less trustful of public health authorities to control the pandemic. This attitude is confirmed in other studies, in which lack of confidence in the government is associated with low vaccine uptake [28,[33], [34], [35]]. Low trust in political and health authorities means that the population might be disinclined to follow their recommendations and instructions.
In the descriptive statistics, similar scores on all knowledge-related scales characterised hesitant individuals. Compared to pro-vaccination participants, they had lower levels of digital vaccine literacy, less capacity to detect fake news, and lower general health literacy. In the multivariate models, the remaining variables similarly associated with hesitancy were digital vaccine literacy and general health literacy, which were strong predictors of hesitancy in comparison with the pro-vaccination group. Compared to the latter, in all models the characteristics of anti-vaccination persons were similar to those of the hesitant, albeit more pronounced. As in a previous UK study, those with worse health literacy were less willing to get vaccinated [36]. In general, the findings of this study were in line with the literature [37,38] and corresponded to the “calculation” dimension of the 5C model [12] : retrieval, understanding and evaluation of vaccine-related information is poorer in those hesitant about vaccination as compared to pro-vaccination individuals [28,35,38]. Increasing knowledge and appraisal of evidence-based information versus misinformation could lead to better empowerment with regard to requesting, seeking, and/or refusing health services such as vaccinations [15,22].
We also observed that the attitudes of hesitant individuals were “in between” the behaviours and characteristics of pro-vaccination and anti-vaccination groups. For the majority of the variables, the overall association between “hesitant” and “anti-vaccination” towards “pro-vaccination” was the same. The odds concerning “hesitant” were more or less midway between “pro-vaccination” and “anti-vaccination”. This is in line with the fact that vaccination acceptance behaviours appear to be on a continuum ranging from active demand to complete refusal of all vaccines rather than as dichotomous “pro- versus anti-vaccination” [39]. Furthermore, differences among the three groups were confirmed in multivariate analyses with or without multiple imputation. These findings corroborate the specificity of the hesitant group, for whom tailored interventions are needed, particularly in terms of trust in the authorities, knowledge and beliefs about vaccination digital vaccine literacy, capacity to detect fake news and general health literacy.
Other studies about Covid-19-related vaccine hesitancy have been conducted in France. A European survey including France reported that 28 % of French respondents were hesitant [21], which was the largest percentage in Europe in 2020. Hesitancy was measured through one item, and the population was representative in terms of region, gender, age group and education. Six consecutive surveys of a large, nationally representative sample (n= 6032) explored attitudes towards a future Covid-19 vaccine in France from May 2020 to November 2020 [40]. Respondents were asked with a single item whether they would agree to get vaccinated if a vaccine against the Covid-19 were available : “certainly”, “probably”, “probably not”, “certainly not”. Those answering “probably not” or “certainly not” were considered as anti-vaccination. While the coding was different, similarly to our study gender was associated with these two response items ; in brief, females were less likely to accept the vaccine. An experimental survey was conducted in a representative French working-age population in 2020 (n=1942) [25]. Vaccination intentions were assessed from repeated choice tasks among vaccines with varying characteristics, while background information on vaccination was controlled. No single item was used, but rather a series of questions involving fictional situations. As in our study, information on past vaccination behaviour, including influenza, was associated with vaccine hesitancy. Another 2020 French survey explored the intention to participate in a Covid-19 vaccine clinical trial and to get vaccinated against Covid-19 (n=3259) [16]. One item was used to classify Covid-19-related vaccine-hesitant individuals, once again using our “don't know” option like. Similarly, men were less hesitant. Lastly, an April 2020 online survey conducted in representative samples of the French population (n=5018) found that attitudes to Covid-19 vaccines were correlated to engagement with the political system ; lack of trust was associated with refusal to get vaccinated [33]. The study used only one item to measure vaccine hesitancy and found 16.1 % of participants to be hesitant.
4.1. Strengths and limitations
Strengths of the study include the use of several original and specific variables about Covid-19-related opinions, digital vaccine literacy, beliefs about vaccination, trust in authorities and recognition of fake news. These data enabled to draw up a clear-cut definition of the profiles of vaccine-hesitant individuals. Furthermore, our sample was large, with more than 1600 respondents throughout France.
This study is not without limitations. As with any online survey based on volunteering, our study was not representative of the French population and, particularly, of hesitant people in France [16]. Description is necessarily limited to those who participated to the study. For instance, women were overrepresented (78.4 %) and participants were predominantly young (84.5 % between 18 and 34 years). Moreover, the sample included only people who were “confined”. Those who worked during the lockdown (e.g., healthcare workers, employees of supermarkets or pharmacies, farmers) were not included. People not having access to the Internet or not being computer-literate were likewise excluded. All in all, a substantial portion of the French population was not considered, and when interpreting our results, selection bias should be taken into account. That said, our findings were similar to those of representative French studies with regard to the association of vaccine hesitancy with characteristics such as gender [40], poor compliance with recommended vaccinations in the past, presence of chronic diseases, and working age [25]. The robustness of our results might thereby be corroborated. Furthermore, another French study, which not representative of the French population, nonetheless reported similar results [16]. In any case, the objective of this study was not to report representative national statistics, but rather to profile hesitant individuals in France according to several covariates.
With this in mind, we defined groups of “hesitant”, “pro-vaccination” and “anti-vaccination” individuals based on an a priori categorization of response modalities, which were asymmetrical, including three options for “pro-vaccination” and only one option for “anti-vaccination”. We oversimplified the assumption that the “hesitant” were those replying “I don't know”, excluding the possibility that they might change their mind (e.g., with an item response such as “No, not at the moment”). In addition, some participants did not feel concerned by the question insofar as they thought that Covid-19 could affect only the elderly the chronic diseased [40,46].
4.2. General considerations
Vaccine hesitancy is context-specific [1]. Interpretation of our results should take into account the fact that the data were collected during the first nationwide lockdown (April-May 2020), at a time when vaccines were not developed. Now that Covid-19-related vaccines are have been developed and are readily available, hesitancy attitudes may have changed. The case of France is also peculiar, given its well-known vaccine hesitancy rate [3], and our results are to be interpreted that much more cautiously. Present-day proposal to the same population of the same questions on vaccine acceptability could provide new results to be compared with the 2020 findings, thereby observing the evolution of vaccine hesitancy concerning Covid-19 in France, now that vaccines are currently administered.
4.3. Implications
Producing and disseminating pro-vaccine campaigns as well as educational programs is pivotal to the fight against coronavirus. Through the profiling of vaccine hesitancy, we observed that the hesitant group was characterized and distinguished by both sociodemographic variables and modifiable factors. These elements should be considered when tailoring interventions to promote vaccination. For instance, it would be highly recommended to develop strategies to improve trust in the authorities (e.g., more transparency in political discourses and more citizen involvement in the local and national public health policy-making) and to enhance health literacy levels (e.g., peer-to-peer education, school-based health and science courses, community-delivered educational programs).
5. Conclusions
The results of this study showed that vaccine hesitancy is variable and depends on different characteristics, ranging from socio-demographic variables to knowledge and beliefs about Covid-19 and vaccination. While failing to identify straightforward predictors, our findings strongly suggest that continued education and communication campaigns focussed on improving vaccine literacy, particularly among women younger than 35, could increase the proportion of people accepting vaccination.
Funding
The i-Share team is currently supported by an unrestricted grant of the Nouvelle-Aquitaine Regional Council (Conseil Régional Nouvelle-Aquitaine, grant N°4370420). It has also received grants from the Nouvelle-Aquitaine Regional Health Agency (Agence Régionale de Santé Nouvelle-Aquitaine, grant N°6066R-8), Public Health France (Santé Publique France, grant N°19DPPP023-0), and The National Institute against cancer INCa (grant N°INCa_11502).
The funding bodies were not involved in either the study design, or in the collection, analysis, or interpretation of the data.
Data availability statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Standards
The study follows the principles of the Declaration of Helsinki and the collection, storage and analysis of the data comply with the General Data Protection Regulation (EU GDPR).
The study was approved by the French Committee for the Protection of Individuals (Comité de Protection des Personnes – CPP IDF X, nr. 46-2020) and by the National Commission on Informatics and Liberty (Commission Nationale de l'Informatique et des Libertés - CNIL, nr. MLD/MFI/AR205600).
CRediT authorship contribution statement
Ilaria Montagni: Conceptualization, Writing – original draft. Kevin Ouazzani-Touhami: Conceptualization, Writing – review & editing. Aude Pouymayou: Data curation, Formal analysis. Edwige Pereira: Formal analysis, Writing – review & editing. Nathalie Texier: Conceptualization, Project administration. Stéphane Schück: Conceptualization, Project administration. Christophe Tzourio: Conceptualization, Project administration, Writing – review & editing, Supervision.
Declaration of interest statement
We wish to confirm that there are no known conflicts of interest associated with this publication and that there has been no significant financial support for this work that could have influenced its outcome.
Acknowledgements
We wish to thank all members of the CONFINS group including the i-Share, Kappa Santé and Kap Code team members : Christophe Tzourio, Stéphane Schück, and Nathalie Texier conceived and designed the study cohort ; Edwige Pereira, Garance Perret, Aude Pouymayou and Mathilde Pouriel analyzed the data ; Julie Arsandaux, Shérazade Kinouani, Mélissa Macalli and Ilaria Montagni wrote and revised survey tools and manuscripts ; Raphaël Germain and Clothilde Pollet were in charge of the regulatory aspects ; Vanessa Marie-Joseph, Adel Mebarki, Elena Milesi and Marie Mougin were in charge of study communication and dissemination. The authors are also grateful to all the participants who volunteered to take part in the study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi : 10.1016/j.respe.2022.02.004.
Appendix. Supplementary materials
REFERENCES
- 1.MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B, et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015 doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 2.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, et al. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine. 2016:12. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward JK, Peretti-Watel P, Bocquier A, Seror V, Verger P. Vaccine hesitancy and coercion: all eyes on France. Nature Immunology. 2019;20 doi: 10.1038/s41590-019-0488-9. [DOI] [PubMed] [Google Scholar]
- 4.Skapinker M. Why rich countries are more prone to ‘vaccine hesitancy.’ Financial Times [Internet]. 2019 Jun; Available from: https://www.ft.com/content/2271a90c-942d-11e9-b7ea-60e35ef678d2
- 5.Williams SE. What are the factors that contribute to parental vaccine-hesitancy and what can we do about it? Hum Vaccines Immunother. 2014;10(9) doi: 10.4161/hv.28596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation SAGE . 2014. Sage Report. [Google Scholar]
- 7.Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Human Vaccines and Immunotherapeutics. 2013;9 doi: 10.4161/hv.25085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lazarus J.V., Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2020 doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vrdelja M, Kraigher A, Verčič D, Kropivnik S. The growing vaccine hesitancy: Exploring the influence of the internet. Eur J Public Health. 2018 doi: 10.1093/eurpub/cky114. [DOI] [PubMed] [Google Scholar]
- 10.Salali GD, Uysal MS. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychological Medicine. 2020 doi: 10.1017/S0033291720004067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm - An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30(25) doi: 10.1016/j.vaccine.2011.11.112. [DOI] [PubMed] [Google Scholar]
- 12.Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. BMC Public Health; 2013. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vrdelja M, Kraigher A, Verčič D, Kropivnik S. The growing vaccine hesitancy: Exploring the influence of the internet. Eur J Public Health. 2018;28(5) doi: 10.1093/eurpub/cky114. [DOI] [PubMed] [Google Scholar]
- 15.Montagni I, Ouazzani-Touhami K, Mebarki A, Texier N, Schück S, Tzourio C. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health (Bangkok) 2021 doi: 10.1093/pubmed/fdab028. (fdab028) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45) doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sallam M. Covid-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines. 2021;9 doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Debussche X, Lenclume V, Balcou-Debussche M, Alakian D, Sokolowsky C, Ballet D, et al. Characterisation of health literacy strengths and weaknesses among people at metabolic and cardiovascular risk: Validity testing of the Health Literacy Questionnaire. SAGE Open Med. 2018;6 doi: 10.1177/2050312118801250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cottrell G, Cot M, Mary JY. Vol. 57. Revue d'Epidemiologie et de Sante Publique; 2009. (L'imputation multiple des données manquantes aléatoirement : concepts généraux et présentation d'une méthode Monte-Carlo). [DOI] [PubMed] [Google Scholar]
- 20.Sibbald B. New ways to sway vaccine-hesitant parents. Canadian Medical Association journal = journal de l'Association medicale canadienne. 2017;189 doi: 10.1503/cmaj.109-5371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. European Journal of Health Economics. 2020 doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Machida M, Nakamura I, Kojima T, Saito R, Nakaya T, Hanibuchi T, et al. Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines. 2021;9(210):0–11. doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine Hesitancy: The Next Challenge in the Fight Against COVID-19. Res Square, Prepr. 2020:1–12. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zintel S, Flock C, Arbogast AL, Forster A, von Wagner C, Sieverding M. Gender Differences in the Intention to Get Vaccinated against COVID-19 - a Systematic Review and Meta-Analysis. SSRN Electron J. 2021 doi: 10.1007/s10389-021-01677-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Heal. 2021;6(4) doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hankivsky O. Women's health, men's health, and gender and health: Implications of intersectionality. Soc Sci Med. 2012;74(11) doi: 10.1016/j.socscimed.2011.11.029. [DOI] [PubMed] [Google Scholar]
- 27.Harapan H, Wagner AL, Yufikae A, Winardif W, Anwar S, Gana AK, et al. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Hum Vaccines Immunother. 2020:1–8. doi: 10.1080/21645515.2020.1819741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 Vaccine Acceptance in the US. medRxiv. 2020 doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kwok KO, Li KK, Wei WI, Tang A, Wong SYS, Lee SS. Are we ready when COVID-19 vaccine is available? Study on nurses′ vaccine hesitancy in Hong Kong. medRxiv. 2020:1–23. [Google Scholar]
- 30.Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126(SUPPL. 2) doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Vol. 8. Front Public Heal; 2020. (Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Janz NK, Becker MH. The Health Belief Model: A Decade Later. Heal Educ Behav. 1984;11(1) doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 33.Ward JK, Alleaume C, Peretti-Watel P, Seror V, Cortaredona S, Launay O, et al. The French public's attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc Sci Med. 2020:265. doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peretti-Watel P, Seror V, Cortaredona S, Launay O, Raude J, Verger P, et al. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. The Lancet Infectious Diseases. 2020;20 doi: 10.1016/S1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Preparing for a COVID-19 vaccine: Identifying and psychologically profiling those who are vaccine hesitant or resistant in two general population samples. PsyArxiv. 2020 [Google Scholar]
- 36.Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccines Immunother. 2020 doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Veldwijk J, van der Heide I, Rademakers J, Schuit AJ, de Wit GA, Uiters E, et al. Preferences for Vaccination. Med Decis Mak. 2015;35(8) doi: 10.1177/0272989X15597225. [DOI] [PubMed] [Google Scholar]
- 38.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann Intern Med. 2020 doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Review of Vaccines. 2014;14 doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 40.Hacquin A-S, Altay S, de Araujo E, Chevallier C, Mercier H. Sharp rise in vaccine hesitancy in a large and representative sample of the French population: reasons for vaccine hesitancy. 2020; Available from: https://psyarxiv.com/r8h6z/
- 41.Shapiro GK, Tatar O, Dube E, Amsel R, Knauper B, Naz A, et al. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine. 2018;36(5) doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 42.Howard MC. A more comprehensive measure of vaccine hesitancy: Creation of the Multidimensional Vaccine Hesitancy Scale (MVHS) J Health Psychol. 2021 doi: 10.1177/13591053211042062. [DOI] [PubMed] [Google Scholar]
- 43.Guay M, Gosselin V, Petit G, Baron G, Gagneur A. Determinants of vaccine hesitancy in Quebec: a large population-based survey. Hum Vaccines Immunother. 2019;15(11) doi: 10.1080/21645515.2019.1603563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl Trop Dis. 2020;14(12) doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwok KO, Li KK, WI WEI, Tang A, Wong SYS, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud. 2021;114 doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dryhurst S, Schneider CR, Kerr J, Freeman ALJ, Recchia G, van der Bles AM, et al. Risk perceptions of COVID-19 around the world. J Risk Res. 2020;23(7–8) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.