Abstract
Objective
Anorexia nervosa (AN) is a disorder with a significantly high prevalence. Affective disorders, including depressive disorder (DD), often coexist with this eating disorder (ED). In this review we will focus on its prevalence, associated vulnerability factors, clinical manifestations, possible etiological factors and its prognosis.
Methods
A bibliographic search was carried out in the PubMed database selecting those articles that approached the subject of comorbidity between AN and DD. The search was limited to articles published from January 1990 to December 2021.
Results
Of the 1891 abstracts reviewed, 33 studies met inclusion criteria. The prevalence of this comorbidity was extremely variable between studies, which exposed their heterogeneity. As to symptomatology this comorbidity presents itself with more severity, greater expression of psychological traits and greater cognitive impairment. Certain personality traits are postulated as vulnerability factors. Genetic factors such as neurochemicals seem to be involved in its pathogenesis.
Conclusion
The comorbidity between DD and ED have important influence in its symptomatic expression, severity and prognosis. Some of the analyzed studies provide consistent data, but there are others that are contradictory. It would be necessary to increase the number of studies and use a unified methodology.
Keywords: Anorexia nervosa, Depressive disorder, Comorbidity, Narrative review
INTRODUCTION
In recent years eating disorder (ED) and specifically anorexia nervosa (AN) have seen an increased both in their incidence as in their prevalence. These disorders have gone from being an epidemic limited to developed countries to becoming a pandemic as a result of the globalization of ideas and customs. We are faced with one of the most frequent pathological entities. Its incidence varies between 1%–10% depending on the culture. Its significances lie in its severity, as it is one of the ten most frequent causes of disability in women [1] and considered the mental disorder with the highest mortality rate [2]. This is mainly due to the medical complications derived from malnutrition and its high suicide rate.
AN may present itself with various complications including those associated with family, physical and psychiatric symptoms that will affect its prognosis. Affective disorders are some of the most frequent psychiatric complications amongst which depressive disorder (DD) is of distinctive relevance and the object of our study. It has been postulated that the presence of depressive symptomatology in AN could be directly correlated to the severity of weight loss. Although this hypothesis does not account for every case of depression in AN, it does seem to explain a large proportion of them. We are faced with one of the most frequent pathological entities, so it is very important to identify it as soon as possible in order to improve the prognosis and therapeutic response in patients with AN.
Given the frequent association between AN and DD, it is essential to question how this relationship is established. In this regard, two types of hypotheses have been developed. The first one speaks of a genetic and/or experiential predisposition that would lead to the development of a DD. Suffering from a depressive state creates feelings of low self-esteem and greater self-criticism as well as a worsening of the self-image, which in turn would act as vulnerability factors for the appearance of an ED [3]. The second of these hypotheses raises the possibility that an ED can appear in people without prior disposition for the development of an affective disorder. In this hypothesis, AN would develop in people with certain predisposing psychological factors that are subject to environmental risk factors. Once the ED has been established, the anorexic condition presents biological and cognitive-emotional characteristics that lead to the appearance of a concomitant DD.
We have conducted a narrative review to provide an up-to-date summary of the scientific evidence on the comorbidity between AN and DD, in order to clarify how these two entities are associated. The study population was those subjects who fulfilled the criteria for diagnosing AN and associated the presence of depressive symptoms. The intervention was to study the prevalence, prognosis, vulnerability and etipoatogenia of both comorbid entities, with the aim of seeing how both entities influence each other, compared to subjects in whom such comorbidity does not occur. Currently, our study takes on greater importance, given the significant increase in cases of AN that have arisen as a result of the COVID-19 pandemic, cases that stand out for their greater severity, which is why it is common for them to present greater comorbidity with depressive symptoms [4,5].
METHODS
Legibility criteria
The selected studies, dealt specifically with AN and its comorbidity with DD. Both longitudinal and cross-sectional studies were included, in the form of clinical trials, field studies or review articles. The inclusion criteria were the following: 1) diagnostic criteria for AN in International Classification of Diseases-10, Diagnostic and Statistical Manual of Mental Disorders (DSM)-III, DSM-IV, DSM-IV-R or DSM-5, 2) English published articles, 3) articles published between January 1990 and December 2021. The references of eligible articles were checked for any additional study not previously identified. All articles dealing with general ED without showing individualized results for AN were excluded. Clinical cases were also excluded, as well as those articles that did not deal with the previously mentioned items, such as prevalence, clinical features, vulnerability factors, etiopathogenesis, and prognosis.
Information sources and search
Studies were identified by searching the electronic database PubMed and Web of Science up to until the end of December 2021. The search criteria used were the following: Title: (depression) AND Title: (anorexia nervosa) OR Title: (depressive disorder) AND Title: (anorexia nervosa) OR Title (depressive symptoms) AND (anorexia nervosa).
Study selection
Screening and selection of articles is displayed in Figure 1. Where titles of articles appeared relevant, abstracts were screened for eligibility, and full texts of potentially eligible studies were then retrieved. Any full texts that did not meet full eligibility criteria were excluded from the review.
Figure 1.
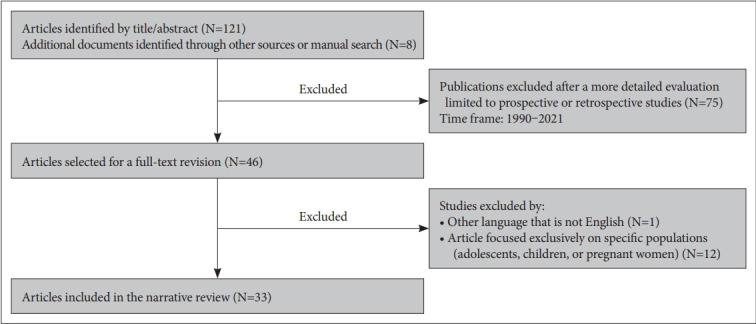
Flow chart of the article selection process.
Data collection
Independent study searches were carried out by two authors (MPCR and MINP). The selected articles were then classified according to the main subject at study: prevalence, clinical features, etiopathogenesis, and prognosis.
Synthesis of results
Studies were grouped by the main subject at study: three prevalence articles, nine clinical manifestations articles, two vulnerability articles, ten etiopathogenesis articles, and finally seven prognosis articles.
RESULTS
Prevalence
The results found in relation to the prevalence of AN and DD’s comorbidity are dissimilar, resulting from the heterogeneity of the different studies. It is worth mentioning that in recent years there has been a lack of studies focusing on prevalence (Table 1). Due to the great heterogeneity of the methodology used in the studies and of the samples analyzed, we have found a great variability in the prevalence between both pathologies, ranging from 36% to 80% [6,7].
Table 1.
Studies on the prevalence of AN and depression
| Study | Sample | Diagnostic criteria/evaluation | Results of OR and prevalence of depression |
|---|---|---|---|
| Solmi et al., 2019 [9] | 955 patients with AN diagnosis (631 with RAN and 324 with PAN) | SCL-90/EDI/Tridimensional Personality Questionnaire | OR for PAN (1.19–1.35) and OR for RAN (1.15–1.51) |
| Godart et al., 2015 [6] | 271 patients with ED (AN and BN) | MINI (DSM-IV-Version) | 80% prevalence of depression in AN |
| García-Alba., 2004 [7] | 150 subjects (50 with RAN, 50 MDD and 50 C) | Rorschach Test/MMPI | 36% prevalence of depressive symptoms in AN |
AN, anorexia nervosa; BN, bulimia nervosa; C, controls; ED, eating disorder; MDD, major depressive disorder; MINI, Mini International Neuropsychiatric Interview; MMPI, Minnesota Multiphasic Personality Inventory; OR, odds ratio; PAN, purgative anorexia nervosa; RAN, restrictive anorexia nervosa; SCL-90, Symptom Check-List-90; EDI, Eating Disorder Inventory; DSM, Diagnostic and Statistical Manual of Mental Disorders
Finally, in a recent analysis on psychopathology and psychiatric symptoms observed in patients with AN, it was noted that depression was one of the symptoms with the highest prevalence score [8].
Clinical features
Regarding clinical features, several studies have reflected that patients with AN and comorbid DD have a higher severity of eating symptoms (Table 2) [9,10]. Furthermore, the Eating Disorder Inventory (EDI) scale scores vary significantly depending on the severity of the depressive symptoms [10]. In addition, it has been observed that patients with comorbid depression present a greater number of suicides attempts [9,11] higher hospitalization rates [9] and greater physical complications such as an increased risk of long-term osteoporosis 12 than those without this comorbidity.
Table 2.
Studies on comorbidity between AN and depression clinical features
| Study | Sample | Diagnostic criteria/evaluation | Results of eating behaviour disorder |
|---|---|---|---|
| Abbate-Daga et al., 20151 [7] | Revision of 62 articles | Wisconsin Card Sorting Test, the Trail Making Task parts A and B, the Brixton Test, the Rey-Osterrieth Complex Figure Test and/or Iowa Gambling Task | Significant relationship between the degree of depression and the degree of cognitive impairment in patients with AN |
| Torres et al., 2015 [13] | 160 subjects (80 with AN and 80 C) | TAS-20/SDS | The greater the severity of depression is associated with a greater degree of alexithymia in AN |
| Brand-Gothelf et al., 2014 [9] | 88 patients with AN | EDI-2 | The greater the severity of the eating behaviour, the greater the risk of suicide attempt and the greater the number of hospitalizations |
| Lulé et al., 2014 [15] | 30 women (15 with AN and 15 C) | WISC/EDQ/EDI-2/YSR/ CBCL/BDI-II/STAI/TAS-20/SPF | Higher degree of alexithymia in AN than in control group |
| Wildes et al., 2007 [11] | 50 patients with AN | Mood Spectrum Self-Report | The greater the severity of depressive symptoms is associated with a higher risk of suicide attempt |
| Konstantynowicz et al., 2005 [12] | 45 patients with AN (14 with depressive symptomatology) | HRSD/MADRS | Comorbidity entails a higher risk of osteoporosis |
| Wilksch and Wade., 2004 [16] | 60 women (19 with AN, 20 RE and 21 C) | CES-D/EDE-Q/SSPA | Subjects with AN have greater concern for body silhouette and lower self-esteem than RE in the presence of depressive symptoms |
| Bizeul et al., 2003 [10] | 193 patients with AN (55 with severe depression, 77 with moderate depression and 32 with mild depression) | EDI/BDI | The greater the severity of depressive symptoms the greater the severity of eating behaviours |
| Sexton et al., 1998 [14] | 53 with ED and 14 C | TAS/BDI/SCID | Alexithymia scores higher in RAN. Alexithymia presents a strong association with the severity of the depression and avoidant personality |
AN, anorexia nervosa; BDI, Beck Depression Inventory; BN, bulimia nervosa; C, controls; CBCL, Child Behaviour Checklist; CES-D, Center for Epidemiological Studies Depression Scale; ED, eating disorder; EDI, Eating Disorder Inventory; EDQ, Eating Disorder Questionnaire; EDE-Q, Eating Disorder Examination Questionnaire; HRSD, Hamilton Rating Scales for Depression; MADRS, Montgomery-Asberg Depression Rating Scale; SCID, Structured Clinical Interviews for DSM-III-R; SDS, Zung-Self Rating Depression Scale; SSPA, Self-Perception Profile for Adolescents; STAI, State-Trait Anxiety Inventory; SPF, Saarbrücker Personlichkeitsfragebogen; RE, restrictive eaters; TAS, Toronto Alexithymia Scale; YSR: Youth Self Report; WISC, Wechsler Intelligence Scale for Children
Alexithymia is a term used to designate a difficulty in identifying and expressing emotions. It has been noted that patients with AN have higher levels of alexithymia than those of the general population. It is considered a characteristic feature in patients with this diagnosis. In the present review, several studies have been identified that focus on the investigation of how depressive symptomatology influences the expression of alexithymia in AN. A study of 160 women (80 with AN diagnosis and 80 controls), studied the presence of alexithymia based on several variables. The study concluded that the variable that best explained the variation in alexithymia was depression [13]. This points to the fact that the severity of depression would probably be related to a higher degree of alexithymia in patients with AN.
Another article aimed to study alexithymia’s relationship with ED based on the presence of depressive symptomatology as well as axis II psychopathology. For this they used the Toronto Alexithymia Scale (TAS) finding statistically significant differences with one of the factors that forms the scale: “difficulty in expressing emotions.” Higher scores were noted among patients with AN compared to patients with BN as well as compared to the control group [14]. Likewise, the severity of the depression as well as an avoidant personality was the variables that were most associated with alexithymia [14]. Finally, in patients with AN, higher levels of both depressive symptomatology and alexithymia were found when compared to control groups [14,15].
Other concepts, such as concern for weight loss and body image as well as self-esteem, were also the main focus of various researchers. Thus, in a study conducted on 60 patients (19 with AN, 20 with food restriction and 21 controls), it was perceived that patients with AN had a greater body image concern and lower self-esteem than patients who only had a restrictive diet. 16 These statistically significant results were correlated to the presence of concomitant DD, since once the depressive symptomatology was controlled, these significant differences found between both groups tended to disappear [16].
DDs usually co-exist with cognitive, physical, emotional and functional alterations. One of the most prevalent and important alterations are cognitive dysfunctions which can be observed in the comorbidity between AN and DD. A review including 62 studies intended to approach this matter by evaluating the impact of depressive symptoms on cognitive flexibility, coherence and decision-making capacity in individuals diagnosed with AN. Statistically significant differences were observed in 48% of the studies when approaching neurocognitive alterations and depressive symptomatology in these patients. This leads to show that the greater the severity of the depressive symptoms, the higher neurocognitive deterioration [17].
Vulnerability factors
Several investigations have noted how specific personality and character aspects can act as vulnerability factors in the comorbidity between AN and DD (Table 3).
Table 3.
Studies on vulnerability factors in comorbidity between AN and depressive disorder
| Study | Sample | Diagnostic criteria/evaluation | Results of eating behaviour disorder |
|---|---|---|---|
| Junne et al., 2016 [19] | 242 women with AN | CBT-E, FPT | Body image distortion in AN is associated with symptoms of anxiety and depression in all stages of the treatment |
| Speranza et al., 2005 [18] | 531 subjects (105 with RAN, 49 with PAN, 98 with BN and 279 C) | TAS-20, BDI, DEQ | Subjects with RAN present greater difficulty to describe feelings and greater self-criticism |
AN, anorexia nervosa; BDI, Beck Depression Inventory; BN, bulimia nervosa; CBT-E, enhanced cognitive behavioural therapy; C, controls; DEQ, Disordered Eating Questionnaire; FPT, focal psychodynamic therapy; PAN, purgative anorexia nervosa; RAN, restrictive anorexia nervosa; TAS, Toronto Alexithymia Scale
Alexithymia would also act as a vulnerability factor for comorbidity between AN and DDs. Patients with associated AN and DD were found to score higher in the Difficulty in Describing Emotions factor of the TAS as well as presenting higher levels of dependence and self-criticism [18].
Body image distortion is one of the nuclear symptoms of AN. A study conducted on a sample of 242 patients with AN between the ages of 18 and 56, studied the relationship between body image distortion’s severity and the appearance of depressive symptoms throughout the treatment. The results found that the degree of body image distortion in early stages would predict the appearance of depressive symptomatology throughout the course of the disorder. Moreover, it was noted that the maintenance of this distortion even after an increase in the body mass index (BMI), which would therefore be considered a good evolution, acted as a factor for the presence of depressive symptomatology [19]. Thus the persistence of body image distortion acts as a vulnerability factor for the appearance of comorbid DD.
Etiopathogenia
Focusing on the underlying causes behind AN and DD’s strong association, many authors have pointed out that genetics may play an important role (Table 4). Thus a 58% of heritability was observed in a sample of 2,163 twins with AN [20]. This same study mentioned that the comorbidity between AN and DD is probably due to genetic factors that influence the risk of occurrence of both disorders [20]. It has also been noted that both disorders would share common genes with the presence of a higher risk of suicide [21].
Table 4.
Studies on the etiopathogenesis of the comorbidity between AN and depressive disorder
| Study | Sample | Diagnostic criteria/evaluation | Results of eating behaviour disorder |
|---|---|---|---|
| Boehm et al., 2018 [24] | 130 subjects (35 with severe AN, 33 recovered from AN, 62 C) | Self-reports in which depressive and anhedonia symptoms were collected | No direct relationship between BMI and depression in AN. Anhedonia in AN is not related to depression |
| Thornton et al., 2016 [21] | 6,899 women from the Swedish study in twin adults | SCID-I | Shared genetic factors were observed for AN, depression and suicide risk |
| Lawson et al., 2013 [25] | 35 women (13 with AN, 9 recovered from AN and 13 C) | STAI, BDI-II/DSM-IV-TR | Abnormal postprandial secretion of oxytocin is associated with anxiety and depression in AN |
| Mattar et al., 2012 [22] | 24 women with AN | BMI, Y-BOCS/DSM-IV | Anxiety symptoms and depression improve with nutritional rehabilitation in AN. However, they are not directly related to the BMI |
| Mattar et al., 2011 [23] | Revision of 7 studies on AN, depression, anxiety and malnutrition | BMI, Y-BOCS/DSM-IV | Contradictory results were observed in the relationship between malnutrition, and anxiety and depression in AN |
| Lawson et al., 2009 [26] | 52 women (21 C, 13 with hypothalamic amenorrhea and 18 with AN and amenorrhea) | HRSA/HRSD | Higher levels of cortisol were found in patients with AN. Higher levels of cortisol were positively associated with depression and anxiety |
| Miller et al., 2007 [27] | 43 subjects with AN | HRSA/HRSD | Lower testosterone levels were associated with anxiety and depression in AN |
| Wade et al., 2000 [20] | 2,163 twin women (including 1,030 twin partners) | DSM-III-R structured clinical interview for anorectic and depressive symptoms | AN has a heritability of 58%. Genetic factors would be involved in the comorbidity between AN and depression |
| Berk et al., 1997 [29] | 12 patients with AN, 11 patients with BN and 17 C | HRSD | Patients with AN and depressive comorbidity, have an increased response to intracellular calcium, which is related to depression |
| Schweitzer et al., 1990 [28] | 20 subjects with AN | Dexamethasone suppression test | 50% of the sample obtained an abnormal response in the dexamethasone suppression test. No relationship was found with weight. Higher scores in depression where found in those with an abnormal response |
AN, anorexia nervosa; BN, bulimia nervosa; BDI, Beck Depression Inventory; BMI, body mass index; C, controls; HRSA, Hamilton Rating Scales for Anxiety; HRSD, Hamilton Rating Scales for Depression; SCID-I, Structured Clinical Interviews for DSM-IV; STAI, State-Trait Anxiety Inventory; Y-BOCS, Yale-Brown Obsessive Compulsive Scale; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; DSM-III-R, Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition, Revised
One of the main theories of the aetiology behind AN and DD’s comorbidity is its association with malnutrition. Thus, in a prospective study, it was pointed out that some of the depressive and anxious symptoms observed in patients with AN were partially reduced after nutritional rehabilitation [22]. However, it failed to find a direct association between the psychometric scales and the BMI modification [22]. In this regard, a review analyzed seven studies that dealt with malnutrition’s role in the appearance of depressive features in AN with contradictory and inconsistent results [23]. On the other hand, a recent study suggests that depressive symptoms found in AN are related to malnutrition, with a negative association between the BMI and depressive symptoms in acute patients [24].
Moreover, several studies have suggested that the etiopathogenesis of the comorbidity between AN and DD could be mediated by the existence of both endocrine and neurochemical factors.
A recent study carried over 35 women of which 13 had been diagnosed with AN, studied its association with oxytocin. The study concluded that the abnormal secretion of postprandial oxytocin in patients with AN was associated with a greater severity of anxiety and depressive symptoms. Thus, oxytocin secretion was able to explain up to 24% of the variation in the Beck Depression Inventory-II [25]. Another study chose to observe the association between cortisol levels in AN, hypothalamic amenorrhea and its association with the presence of affective disorders and bone density levels. The results showed that patients with AN had higher scores in depression and anxiety and higher cortisol levels than patients with functional hypothalamic amenorrhea [26]. Cortisol levels were positively related to anxiety and depression scores and negatively so to bone density levels. Therefore, this study suggests that hypercortisolemia could act as a mediator in the appearance of affective symptoms and low bone density in patients with AN [26]. Continuing with endocrinology, another study focused on androgen levels and its association with depressive and anxious symptoms in patients with AN. Low androgen levels have been linked to affective and behavioral alterations. Thus, it was found that testosterone levels were inversely related to the severity of anxiety and depressive symptoms, as well as the presence of thoughts and behaviors related to this ED [27]. Lastly, one final article sought to study the test results of dexamethasone suppression in a sample of 20 patients with AN and its relationship with various parameters. Half of these patients initially presented an altered dexamethasone suppression test that was not related to the percentage of weight loss. However, it was associated with a higher percentage of depressive symptoms [28].
Several research have studied the possible role of serotonin on the neurochemical factors involved in the pathogenesis between AN and DD. It was noted that those patients with AN and associated depressive symptomatology had an intracellular calcium increase in response to serotonin that was not observed in those patients with AN who scored low on depression scales. Thus, this serotonergic dysregulation appeared to a common trait, understanding that it could be mediated not so much by the ED as it would be by the affective disorder [29].
Prognosis of the comorbidity
Regarding the evolution of depressive symptomatology in patients with AN, it seems that patients that have recovered from long-term AN have higher depression levels than those who have never suffered from an ED [30] (Table 5). The relationship between nutritional recovery and improvement of depressive symptoms is contradictory, and some studies point to improvement of depressive symptoms with weight gain [31]; however, others suggest that they are not statistically significant [32].
Table 5.
Studies on prognosis in the comorbidity between AN and depressive disorder
| Study | Sample | Diagnostic criteria/evaluation | Results |
|---|---|---|---|
| Carretier et al., 2021 [32] | Eight studies dealing with 10–18 year old inpatient or outpatient adolescents presenting an AN complicated by a major depressive disorder | DSM-5 | There is a need to identify faster severe depressive disorders in adolescents with AN in order to provide a more intensive treatment of mood symptoms |
| Kahn et al., 2019 [35] | 56 patients with AN | EDE/BSI | During hospitalization depression in AN has not an association with a bad prognosis. If depressive symptoms persist beyond 1 month during hospitalization the risk of relapsing back to AN is higher |
| Mischoulon et al., 2011 [33] | 51 patients with RAN, 85 with PAN and 110 with BN | LIFE-EAT-II | A higher severity in depression was noted in RAN |
| Holtkamp et al., 2005 [30] | 39 patients with AN and 39 C | BMI | Patients with anxiety, depression and obsessive symptoms scored higher that those with just AN |
| Pollice et al., 1997 [31] | Women with AN in different stages (low weight, short-term weight restoration and long-term weight restoration) are compared with a group of healthy women | BDI/HRSD/STAI/Y-BOCS | Malnutrition aggravates anxiety-depressive and obsessive symptoms. Anxious-depressive symptoms persist mildly or moderately in AN and could be related to their pathogenesis |
| Herpertz-Dahlmann et al., 1995 [34] | 34 patients with AN | HRSD/SDS | Depression at the start of AN holds no association with its prognosis. Throughout the follow-up, a statistically significant relationship was observed between depression and AN prognosis |
AN, anorexia nervosa; BN, bulimia nervosa; BDI, Beck Depression Inventory; BMI, body mass index; BSI, Brief Symptom Inventory; C, controls; EDE, Eating Disorder Examination; HRSD, Hamilton Rating Scales for Depression; LIFE-EAT-II, Eating Disorders Longitudinal Inverval Follow-up Evaluation; PAN, purgative anorexia nervosa; RAN, restrictive anorexia nervosa; SDS, Zung-Self Rating Depression Scale; STAI, State and Trait Anxiety Inventory; Y-BOCS, Yale-Brown Obsessive Compulsive Scale; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition
Additionally, recovering from these depressive symptoms is highly related to the ED’s subtype, with restrictive AN bearing the worst prognosis [33]. However, despite weight restoration, anxious and depressive symptoms can remain mild or moderate in subjects who have suffered from AN, which could mean that these symptoms are indeed linked to AN’s pathogenesis [31].
Focusing on the role of depressive symptomatology in AN’s evolution, it has been noticed that the presence of onset depressive symptoms [31] does not act as a prognostic indicator [34]. However, the persistence of depressive symptomatology throughout the follow-up of AN is firmly associated with its evolution [34-36]. Likewise, another study carried on AN hospitalized patients observed that depressive symptoms during the disease’s onset did not predict the results of the treatment; however, higher relapse rates were observed in those hospitalized patients who presented depressive symptomatology after one month of hospital admission [35].
DISCUSSION
Prevalence
In regard to the prevalence of this comorbidity, the first thing that attracts our attention is the lack of studies that have been carried out in recent years in order to determine its prevalence. Furthermore, the prevalence figures are very disparate ranging from 36% to 80%, thus it is difficult to establish an average prevalence.
The reason of this disparity could be the heterogeneity of the studies. Furthermore, the scales and measuring instruments used for the assessment of depressive symptomatology were not homogeneous. However, despite these dissimilarities, final results seem to point to a considerable prevalence of this comorbidity. Therefore, the detection of depressive symptoms in patients with AN is of great importance for both its treatment and its prognosis. In recent years, given the impact of COVID-19 on AN cases [4,5], more studies will be needed to establish the current prevalence of this comorbidity.
Clinical manifestations
Regarding clinical manifestations, the studied articles confirm that certain character traits are closely linked to AN and, in short, to those with comorbid depressive symptoms.
Thus, depressive symptoms would act as modulators of alexithymia’s severity degree in patients with AN [13,14]. Ultimately, we can state that the comorbidity under study leads to an aggravation of those psychological factors that have been classically related to AN.
In scientific literature it is pointed out that both DD and ED present somatic, cognitive and functional complications, amongst other symptoms. Many studies to this date suggest that depressive symptoms significantly influence the aggravation of neurocognitive alterations in patients with AN [17]. Studies on cognition in AN adjusted for depressive symptoms are scarce, however, given the role of depression in neurocognition that many articles suggest, it would be of great clinical utility to explore the presence of comorbid depressive symptoms in patients with AN and marked alterations in the cognitive spheres.
Vulnerability factors
The reviewed articles suggest that the main vulnerability factors for the development of a comorbid DD in patients with AN are those associated with personality traits and certain psychological features of the patients in question.
Among personality traits, self-direction, harm avoidance, self-criticism or dependence are factors that have classically been related to an emotional disorder of the depressive pole. Likewise, these traits have also been associated to restrictive AN so they appear to be common features for both disorders [37].
If we focus on the above-mentioned hypotheses, we can establish an association between the existence of an ED and a comorbid DD. Thus, in the first hypothesis, it was pointed out that biological and/or experiential factors would contribute to the appearance of a DD. The presence of depression would produce a worsening of body image as well as greater self-criticism, both which would in turn act as vulnerability factors for the development of a comorbid ED [18,19]. The research that we have found points to the confirmation of this hypothesis. However, the temporal sequence of both disorders still has not been established, which means that which of these disorders would act as a predisposing agent for the other one cannot be established yet [38].
Etiopathogenia
Regarding the role of genetics, studies have pointed to the existence of genetic factors that increase the risk of both AN and DD [20,21]. However, these studies only provide approximate data, so we are far from determining exactly which genetic factors are involved.
As to the role of malnutrition as a causal element of the appearance of depressive symptomatology in patients with AN, the results seem to be contradictory. As noted in the scientific literature, although many depressive symptoms can be explained by weight loss, it cannot explain every case of comorbidity between AN and DD [23].
Finally, studies suggest that the cause of this frequent association could rely on biological factors. However, most results are not too specific. For example, there seem to be higher plasma levels of cortisol in AN as well as in patients with associated depressive and/or anxious symptoms [26]. However, cortisol levels are increased in any given situation that causes stress, so such finding would lack specificity. Regarding the dexamethasone suppression test, there existed a limitation of the sample size (n=20), so conclusive results cannot be obtained. However, previous studies point to a close relationship between non-suppression and low weight, which in turn was related to the appearance of greater depressive symptomatology [28].
Prognosis of this comorbidity
Depressive symptomatology seems to be related to the severity of the eating symptoms, being more severe among restrictive disorders and improving with weight gain. However, regarding ED’s evolution and its association with depressive symptomatology, most of the reviewed studies suggest depressive symptoms do not condition the final outcome of the treatment. The only exception would be the presence of depressive symptomatology after one month’s hospitalization which would be related to the appearance of greater depressive symptoms [35]. Therefore, it seems that the influence of both disorders is not clearly bidirectional.
Finally, it should be noted that the majority of studies present in this review have a cross-sectional design and of great heterogeneity, which makes it difficult not only to establish causal relationships, but also to compare the results.
Limitations
The main limitation of this article is that it has not been possible to perform a meta-analysis that would provide more scientific evidence, due to the heterogeneity in the methodology of the articles included, as well as the diversity of variables that have been analysed.
Conclusions
Affective disorders and among them DD constitute one of the main comorbid disorders of AN. This is due both to its prevalence and to its influence over the symptomatic expression and evolution of AN. Throughout this article, relevant data has been found that points to a symptomatic aggravation, to the existence of vulnerability factors and to common etiopathogenic pathways. However, this bibliography is not exempt from some contradictory data.
This may be due to the fact that a large part of the studies we have worked with generalized depressive symptomatology instead of making it specific for DD.
Acknowledgments
The authors would like to gratefully acknowledge the collaboration of Department of Psychiatry members in the University of Granada.
Footnotes
Availability of Data and Material
All the data are extracted from the articles reviewed.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Maria Pilar Calvo-Rivera, Luis Gutiérrez-Rojas. Data curation: all authors. Formal analysis: Maria Pilar Calvo-Rivera, Luis Gutiérrez-Rojas. Investigation: Maria Pilar Calvo-Rivera. Methodology: Maria Pilar Calvo-Rivera, Luis Gutiérrez-Rojas. Project administration: Luis Gutiérrez-Rojas. Resources: Maria Pilar Calvo-Rivera. Software: Luis Gutiérrez-Rojas. Supervision: Luis Gutiérrez-Rojas. Validation: Maria Isabel Navarrete-Páez, IB. Visualization: Luis Gutiérrez-Rojas. Writing—original draft: Maria Pilar Calvo-Rivera, Luis Gutiérrez-Rojas. Writing—review & editing: all authors.
Funding Statement
None
REFERENCES
- 1.Matthers CD, Vos ET, Stevenson CE, Begg SJ. The Australian Burden of Disease Study: measuring the loss of health from diseases, injuries and risk factors. Med J Aust. 2000;172:592–596. doi: 10.5694/j.1326-5377.2000.tb124125.x. [DOI] [PubMed] [Google Scholar]
- 2.Millar HR, Wardell F, Vyvyan JP, Naji SA, Prescott GJ, Eagles JM. Anorexia nervosa mortality in Northeast Scotland, 1965-199. Am J Psychiatry. 2005;162:753–757. doi: 10.1176/appi.ajp.162.4.753. [DOI] [PubMed] [Google Scholar]
- 3.Rivinus TM, Biederman MD, Herzog DB, Kemper K, Harper GP, Harmatz JS, et al. Anorexia nervosa and affective disorders: a controlled family history study. Am J Psychiatry. 1984;141:1414–148. doi: 10.1176/ajp.141.11.1414. [DOI] [PubMed] [Google Scholar]
- 4.Hunter R, Gibson C. Narratives from within ‘lockdown’: a qualitative exploration of the impact of COVID-19 confinement on individuals with anorexia nervosa. Appetite. 2021;166:105451. doi: 10.1016/j.appet.2021.105451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miniati M, Marzetti F, Palagini L, Marazziti D, Orrù G, Conversano C, et al. Eating disorders spectrum during the COVID pandemic: a systematic review. Front Psychol. 2021;12:663376. doi: 10.3389/fpsyg.2021.663376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Godart N, Radon L, Curt F, Duclos J, Perdereau F, Lang F, et al. Mood disorders in eating disorder patients: prevalence and chronology of ONSET. J Affect Disord. 2015;185:115–122. doi: 10.1016/j.jad.2015.06.039. [DOI] [PubMed] [Google Scholar]
- 7.García-Alba C. Anorexia and depression: depressive comorbidity in anorexic adolescents. Span J Psychol. 2004;7:40–52. doi: 10.1017/s113874160000473x. [DOI] [PubMed] [Google Scholar]
- 8.Solmi M, Collantoni E, Meneguzzo P, Tenconi E, Favaro A. Network analysis of specific psychopathology and psychiatric symptoms in patients with anorexia nervosa. Eur Eat Disord Rev. 2019;27:24–33. doi: 10.1002/erv.2633. [DOI] [PubMed] [Google Scholar]
- 9.Brand-Gothelf A, Leor S, Apter A, Fenning S. The impact of comorbid depressive and anxiety disorders on severity of anorexia nervosa in adolescent girls. J Nerv Ment Dis. 2014;202:759–762. doi: 10.1097/NMD.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 10.Bizeul C, Brun JM, Rigaud D. Depression influences the EDI scores in anorexia nervosa patients. Eur Psychiatry. 2003;18:119–123. doi: 10.1016/s0924-9338(03)00033-6. [DOI] [PubMed] [Google Scholar]
- 11.Wildes JE, Marcus MD, Gaskill JA, Righam R. Depressive and manic-hypomanic spectrum psychopathology in patients with anorexia nervosa. Compr Psychiatry. 2007;48:413–418. doi: 10.1016/j.comppsych.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 12.Konstantynowicz J, Kadziela-Olech H, Kaczmarski M, Zebaze RM, Juliano-Burns S, Piotrowska-Jastrzebaska J, et al. Depression in anorexia nervosa: a risk factor for osteoporosis. J Clin Endocrinol Metab. 2005;90:5382–5385. doi: 10.1210/jc.2005-0026. [DOI] [PubMed] [Google Scholar]
- 13.Torres S, Guerra MP, Lencastre L, Miller K, Vieira FM, Roma-Torres A, et al. Alexithymia in anorexia nervosa: the mediating role of depression. Psychiatry Res. 2015;225:99–107. doi: 10.1016/j.psychres.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 14.Sexton MC, Sunday SR, Hurt S, Halmi KA. The relationship between alexithymia, depression, and axis II in eating disorder inpatients. Int J Eat Disord. 1998;23:277–286. doi: 10.1002/(sici)1098-108x(199804)23:3<277::aid-eat5>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 15.Lulé D, Schulze UM, Bauer K, Schöll F, Müller S, Fladung AK, et al. Anorexia nervosa and its relation to depression, anxiety, alexithymia and emotional processing deficits. Eat Weight Disord. 2014;19:209–216. doi: 10.1007/s40519-014-0101-z. [DOI] [PubMed] [Google Scholar]
- 16.Wilksch S, Wade TD. Differences between women with anorexia nervosa and restrained eaters on shape and weight concerns, self-esteem and depression. Int J Eat Disord. 2004;35:571–578. doi: 10.1002/eat.10273. [DOI] [PubMed] [Google Scholar]
- 17.Abbate-Daga G, Buzzichelli S, Marzola E, Aloi M, Amianto F, Fassino S. Does depression matter in neuropsychological performances in anorexia nervosa? A descriptive review. Int J Eat Disord. 2015;48:736–745. doi: 10.1002/eat.22399. [DOI] [PubMed] [Google Scholar]
- 18.Speranza M, Corcos M, Loas G, Stéphan P, Guilbaud O, Pérez-Díaz F, et al. Depressive personality dimensions and alexithymia in eating disorders. Psychiatry Res. 2005;135:153–163. doi: 10.1016/j.psychres.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Junne F, Zipfel S, Wild B, Martus P, Giel K, Resmark G, et al. The relationship of body image with symptoms of depression and anxiety in patients with anorexia nervosa during outpatient psychotherapy: results of the ANTOP study. Psychotherapy (Chic) 2016;53:141–151. doi: 10.1037/pst0000064. [DOI] [PubMed] [Google Scholar]
- 20.Wade TD, Bulik CM, Neale M, Kendler KS. Anorexia nervosa and major depression: shared genetic and environmental risk factors. Am J Psychiatry. 2000;157:469–471. doi: 10.1176/appi.ajp.157.3.469. [DOI] [PubMed] [Google Scholar]
- 21.Thornton LM, Welch E, Munn-Chernoff MA, Lichtenstein P, Bulik CM. Anorexia nervosa, major depression and suicide attempts: shared genetic factors. Suicide Life Threat Behav. 2016;135:153–163. doi: 10.1111/sltb.12235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mattar L, Thiébaud MR, Huas C, Cebula C, Godart N. Depression, anxiety and obsessive-compulsive symptoms in relation to nutritional status and outcome in severe anorexia nervosa. Psychiatry Res. 2012;200:513–517. doi: 10.1016/j.psychres.2012.04.032. [DOI] [PubMed] [Google Scholar]
- 23.Mattar L, Huas C, Duclos J, Apfel A, Godart N. Relationship between malnutrition and depression or anxiety in Anorexia Nervosa: a critical review of the literature. J Affect Disord. 2011;132:311–318. doi: 10.1016/j.jad.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 24.Boehm I, Flohr L, Steding J, Holzapfel L, Sleitz J, Roessner V, et al. The trajectory of anhedonic and depressive symptoms in anorexia nervosa: a Longitudinal and cross-sectional Approach. Eur Eat Disord Rev. 2018;26:69–74. doi: 10.1002/erv.2565. [DOI] [PubMed] [Google Scholar]
- 25.Lawson EA, Holsen LM, Santin M, DeSanti R, Meenaghan E, Eddy KT, et al. Postprandial oxytocin secretion is associated with severity of anxiety and depressive symptoms in anorexia nervosa. J Clin Psychiatry. 2013;74:e451–457. doi: 10.4088/JCP.12m08154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lawson EA, Donoho D, Miller KK, Misra M, Meenaghan E, Lydecker J, et al. Hypercortisolemia is associated with severity of bone loss and depression in hypothalamic amenorrhea and anorexia nervosa. J Clin Endocrinol Metab. 2009;94:4710–4716. doi: 10.1210/jc.2009-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller KK, Wexler TL, Zha AM, Lawson EA, Meenaghan EM, Misra M, et al. Androgen deficiency: association with increased anxiety and depression symptom severity in anorexia nervosa. J Clin Psychiatry. 2007;68:959–965. doi: 10.4088/jcp.v68n0621. [DOI] [PubMed] [Google Scholar]
- 28.Schweitzer I, Szmukler GI, Maguire KP, Harrison LC, Tuckwell V, Davies BM. The dexamethasone suppression test in anorexia nervosa. The influence of weight, depression, adrenocorticotrophic hormone and dexamethasone. Br J Psychiatry. 1990;157:713–717. doi: 10.1192/bjp.157.5.713. [DOI] [PubMed] [Google Scholar]
- 29.Berk M, Kessa K, Szabo CP, Butkow N. The augmented platelet intracellular calcium response to serotonin in anorexia nervosa but not bulimia may be due to subsyndromal depression. Int J Eat Disord. 1997;22:57–63. doi: 10.1002/(sici)1098-108x(199707)22:1<57::aid-eat7>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 30.Holtkamp K, Müller B, Heussen N, Remschmidt H, Herpertz-Dahlmann B. Depression, anxiety and obssesionality in long-term recovered patients with adolescent-onset anorexia nervosa. Eur Child Adolesc Psychiatry. 2005;14:106–110. doi: 10.1007/s00787-005-0431-5. [DOI] [PubMed] [Google Scholar]
- 31.Pollice C, Kaye WH, Greeno CG, Weltzin TE. Relationship of depression, anxiety and obsessionality to state of illness in anorexia nervosa. Int J Eat Disord. 1997;21:367–376. doi: 10.1002/(sici)1098-108x(1997)21:4<367::aid-eat10>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 32.Carretier E, Blanchet C, Moro MR, Lachal J. Comorbid major depressive disorder of anorexia nervosa in adolescence: a scoping review of treatment strategies. Encephale. 2021;47:72–78. doi: 10.1016/j.encep.2020.05.017. [DOI] [PubMed] [Google Scholar]
- 33.Mischoulon D, Eddy KT, Keshaviah A, Dinescu D, Ross SL, Kass AE, et al. Depression and eating disorders: treatment and course. J Affect Disord. 2011;130:470–477. doi: 10.1016/j.jad.2010.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herpertz-Dahlmann BM, Wewetzer C, Remschmidt H. The predictive value of depression in anorexia nervosa. Results of a seven-year follow-up study. Acta Psychiatr Scand. 1995;91:114–9. doi: 10.1111/j.1600-0447.1995.tb09750.x. [DOI] [PubMed] [Google Scholar]
- 35.Kahn M, Brunstein-Klomek A, Hadas A, Snir A, Fennig S. Early changes in depression predict outcomes of inpatient adolescent anorexia nervosa. Eat Weight Disord. 2020;25:777–785. doi: 10.1007/s40519-019-00686-9. [DOI] [PubMed] [Google Scholar]
- 36.Pleplé A, Lalanne C, Huas C, Mattar L, Hanachi M, Flament MF, et al. Nutritional status and anxious and depressive symptoms in anorexia nervosa: a prospective study. Sci Rep. 2021;11:771. doi: 10.1038/s41598-020-79410-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marzola E, Fassino S, Amianto F, Abbate-Daga G. Affective temperaments in anorexia nervosa: the relevance of depressive and anxious traits. J Affect Disord. 2017;218:23–29. doi: 10.1016/j.jad.2017.04.054. [DOI] [PubMed] [Google Scholar]
- 38.Deep AL, Nagy LM, Weltzin TE, Rao R, Kaye WH. Premorbid onset of psychopathology in long-term recovered anorexia nervosa. Int J Eat Disord. 1995;17:291–297. [PubMed] [Google Scholar]


