Short abstract
Content available: Author Audio Recording
Abbreviations
- AH
acute hepatitis
- ALD
alcoholic liver disease
- ATD
antitubercular drug
- CLD
chronic liver disease
- DILI
drug‐induced liver injury
- HAV
hepatitis A virus
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- HEV
hepatitis E virus
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
Listen to an audio presentation of this article.
Liver diseases are fast being recognized as public health priorities in India. The burden of liver disease in India is significant because it alone contributed to 18.3% of the two million global liver disease–related deaths in 2015. 1 Contribution of cirrhosis and its complications, collectively chronic liver diseases (CLDs), as causes of mortality in India have been increasing progressively since 1980, compared with China, the other country in Asia with a large population, where it remains stationary and is even showing downward trends (Fig. 1). 2 In India, similar to many developing nations, there are limitations in the quality of the available epidemiological data resources in liver disease in the context of diagnostic precision and clinical phenotyping, uniformity of reporting, and nonexistent electronic databases across the country. Despite this, a fair body of evidence is available that suggests the increasing impact of liver diseases on the country’s economy and health care resources, apart from being a cause of premature death and disability. The cultural–lifestyle transition that India is passing through currently with progressive adoption of a western diet, sedentary habits, along with an aura of freedom from long‐held taboos around alcohol in the society create grounds for a spectrum of liver diseases in India that shows signs of a rapid switch. 3 This change includes increasing overall importance of alcoholic liver disease (ALD) and nonalcoholic fatty liver disease (NAFLD) as causes of liver disease over and above viral causative factors (Table 1). The expanding size of the population and an increasing life expectancy in the country are important demographic determinants of this change. In keeping with this, encouraging health system response strategies have been adopted in India. A federally funded National Viral Hepatitis Control Program is operational in India since 2018 that includes both preventive (vaccination, blood safety) and early detection: linkage‐to‐care (screening at‐risk population, provision of drugs, surveillance of CLD) strategies. 4 Further, a national NAFLD control program has just been launched in 2021 with activities that integrate liver disease control more broadly into an other noncommunicable diseases control program.
FIG 1.
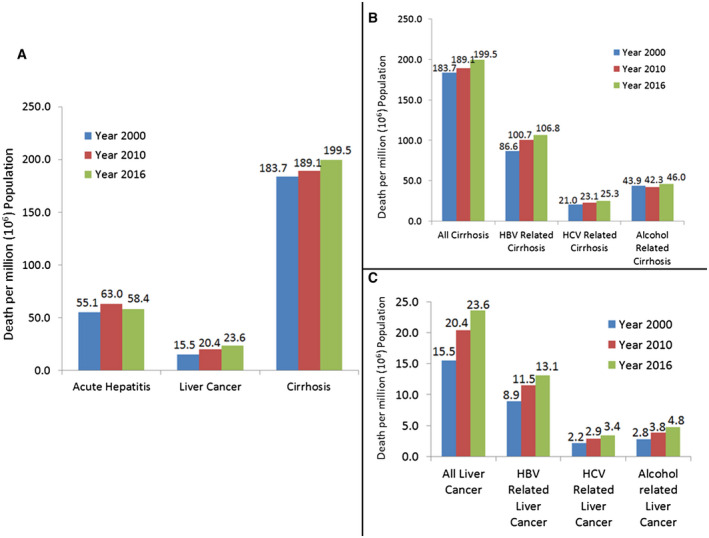
Changes in mortality pattern in India over time. Calculation of cause‐specific death rates is done from the data available from the World Health Organization (WHO) Global Disease Burden database (https://www.who.int/data/gho/data/themes/mortality‐and‐global‐health‐estimates/ghe‐leading‐causes‐of‐death). (A) Changes in death rates in acute hepatitis, cirrhosis, and liver cancer. (B) Changes in death rates in cirrhosis overall, as well as in HBV, HCV, and alcohol‐related cirrhosis. (C) Changes in death rates in liver cancer overall, as well as in HBV, HCV, and alcohol‐related liver cancers.
TABLE 1.
Frequency of Etiologies in Different Syndromes of Liver Disease and Liver Cancer
| Syndromes of Liver Disease | Etiology | Prevalence (%) | Contribution to Mortality (%) |
|---|---|---|---|
| Acute liver disease | HAV | 1.7‐33 | 5‐6.3 |
| HEV | 30‐50 | 30‐40 | |
| HBV | 13.9‐27.6 | 55‐60 | |
| Non‐A‐E virus | 14.6‐43.9 | 0.5‐2 | |
| Drugs (ATD and others)* | 0‐15 | ||
| CLD including cirrhosis | HBV | 17.6‐47.9 | 30‐60 |
| HCV | 5.2‐44.9 | 10‐22 | |
| Alcohol | 10.9‐31.9 | 20‐25 | |
| NAFLD/NASH | 2.6‐43.6 | 10‐15 | |
| Others* | 9.7‐23.2 | 5‐10 | |
| Liver cancer | HBV | 46.8 | 40‐60 |
| HCV | 14.8 | 10‐20 | |
| Alcohol | 9.6 | 15‐20 | |
| NAFLD/NASH | 4.6‐19 | 5‐10 | |
| Prevalence of population‐level risk factors | HBV | 2.4‐3.7 | – |
| HCV | 0‐5.2 | – | |
| NAFLD/NASH | 8.7‐32 | – | |
| Hazardous drinking habit among alcohol users | 44.4 | – |
Different CLDs and cirrhosis accounted for 2.1% of all deaths in India in the year 2016. 5 An issue that impedes early treatment and taxes health care resources is that CLDs in India present fairly late in the clinical course, most commonly after decompensation has set in. 3
Acute hepatitis (AH) in India is most often due to hepatitis E virus (HEV) in adults, while hepatitis B virus (HBV), alcoholic hepatitis, and drug‐induced liver injury (DILI) are other important causes of AH in adults. 6 Hepatitis A virus (HAV) mostly causes AH in children, whereas adults are generally exposed and immune to it. This epidemiological pattern is currently changing, with HAV emerging as a cause of sporadic AH in adults, largely because of improved water supply and sanitation measures with diminished exposure and immunity to HAV in childhood. AH caused by HEV in women in the third trimester of pregnancy and in DILI caused by antitubercular drugs (ATDs) are two particularly important causative settings of acute liver failure in India. 7
HBV is the most common overall cause of CLD, including cirrhosis and hepatocellular carcinoma (HCC), in India, although alcohol abuse is rapidly increasing and is showing trends to replace HBV as the predominant cause of CLD. 3 , 6 NAFLD burden is similarly increasing in India with an upward‐moving body mass index and diabetes incidence. 8 In contrast, hepatitis C virus (HCV) burden is diminishing following treatment programs over the past half decade. 9 India is a vast country, and regional difference for the causative factors is noteworthy. HBV is most prevalent in areas of North‐East, East, and South India, while HCV prevalence is high in North India, along with pockets of high prevalence in North‐East, particularly among intravenous drug users. ALD prevalence, along with NAFLD, is relatively uniform across the country. 3 HCC prevalence and detection rates are also increasing over time. HCC in India occurs mostly related to HBV and occurs in the setting of advanced cirrhosis with decompensation, complicating detections and outcomes. 3
Prevalence of HBV in the general population (2.4%) is showing decline over time. This is due to improvements in injection habits, transfusion safety, and HBV vaccination of newborns as a component of a national immunization program since 2008. Arunachal Pradesh represents a continuing pocket of high prevalence and in view of the geographic spread of that state, implementing an HBV prevention program in the challenging terrains calls for innovative, contextually effective vaccination strategies for control. 10 HBV transmission is mainly horizontal in India, while mother‐to‐child transmission still occurs. HCV prevalence in the country is less than 1%, with zones of high prevalence in Punjab, Manipur, and Mizoram. 9 Alcoholism, in contrast, is increasing across the country with younger age at onset of drinking, high per capita consumption of alcohol, drinking patterns that are potentially harmful, and coexistence of diabetes in many alcoholics. These are all features that increase the potential impact of alcohol on liver disease. NAFLD prevalence in the general population varies from 8% to 20%, with high prevalence being reported from urban, selected population groups, as well as “ultrasound‐only”–driven studies, and the lower prevalence from rural, stringently defined study. In view of the fact that a disproportionate majority of the Indian population and patients with NAFLD are still nonobese by standard anthropometric criteria compared with the western world, metabolic disorders, including diabetes and NAFLD, in “lean” individuals present challenges in definition and genesis of the metabolic derangements. DILI has a wider canvas and dimensions in India than elsewhere in view of the prevalent widespread nonprescription and unmonitored use of drugs. ATD and antibiotics are important, while the contribution of alternative medicine remedies remains an almost unexplored territory.
Liver disease epidemiology in India is in a transition. Better screening strategies, more effective linkage to care for early‐stage liver disease, and improved awareness on preventive steps in an integrated way could be useful interventions.
Key Points
CLD is gradually becoming a public health priority in India.
Overall, NAFLD and ALD are emerging as important causes of CLD in the country paralleling the changes in lifestyle and social customs.
Regional variability of etiologies for CLD is evident in this geographically and ethnically diverse country.
Hepatitis B still remains the major cause of CLD and liver cancer.
Hepatitis C is showing a decreasing trend because of an effective National Viral Hepatitis Control Program.
India needs a liver disease registry and morbidity/mortality database to combat the upcoming burden of CLD in the country.
Potential conflict of interest: Nothing to report.
References
- 1. Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med 2014;18:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization . Global Health Estimates: Life expectancy and leading causes of death and disability. Available at: http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/. Accessed February 24, 2021.
- 3. Mukherjee PS, Vishnubhatla S, Amarapurkar DN, et al. Etiology and mode of presentation of chronic liver diseases in India: a multi centric study. PLoS One 2017;12:e0187033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Health Portal India . National Viral Hepatitis Control Program (NVHCP). Available at: https://www.nhp.gov.in/national‐viral‐hepatitis‐control‐program‐(nvhcp)_pg. Accessed February 24, 2021.
- 5. India State‐Level Disease Burden Initiative Collaborators . Nations within a nation: variations in epidemiological transition across the states of India, 1990‐2016 in the Global Burden of Disease Study. Lancet 2017;390:2437‐2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sarin SK, Kumar M, Eslam M, et al. Liver diseases in the Asia‐Pacific region: a Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol Hepatol 2020;5:167‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Anand AC, Nandi B, Acharya SK, et al.; INASL Task‐Force on Acute Liver Failure . Indian National Association for the Study of the Liver Consensus Statement on Acute Liver Failure (Part 1): Epidemiology, Pathogenesis, Presentation and Prognosis. J Clin Exp Hepatol 2020;10:339‐376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li J, Zou B, Yeo YH, et al. Prevalence, incidence, and outcome of non‐alcoholic fatty liver disease in Asia, 1999‐2019: a systematic review and meta‐analysis. Lancet Gastroenterol Hepatol 2019;4:389‐398. [DOI] [PubMed] [Google Scholar]
- 9. Dhiman RK, Satsangi S, Grover GS, et al. Tackling the hepatitis C disease burden in Punjab, India. J Clin Exp Hepatol 2016;6:224‐232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Abutaleb A, Khatun M, Clement J, et al. A model of care optimized for marginalized remote population unravels migration pattern in India. Hepatology 2021;73:1261‐1274. [DOI] [PMC free article] [PubMed] [Google Scholar]


