Abstract
Background. Interest in electroencephalographic (EEG) coronavirus disease 2019 (COVID-19) findings has been growing, especially in the search for a specific-features EEG of encephalopathy. Methods. We made a retrospective analysis of 29 EEGs recorded in 15 patients with COVID-19 and neurological symptoms. We classified the EEGs as “Acute EEG” and “follow-up EEG.” We did a statistical analysis between voltage and respiratory status of the patient, stay or not in the intensive care unit (ICU), days of stay in the ICU, sedative drugs, pharmacological treatment, type of symptoms predominating, and outcome. Results. We found EEG abnormalities in all patients studied. We observed the amplitude of background <20 µV at 93% of “acute EEG,” versus only 21.4% of “follow-up EEG.” The average voltage went from 12.33 ± 5.09 µV in the acute EEGs to 32.8 ± 20.13 µV in the follow-up EEGs. A total of 60% of acute EEGs showed an intermittent focal rhythmic. We have not found a statistically significant association between voltage of acute EEG and nonneurological clinical status (including respiratory) that may interfere with the EEG findings. Conclusions. Nonspecific diffuse slowing EEG pattern in COVID-19 is the most common finding reported, but we found in addition to that, as a distinctive finding, low voltage EEG, that could explain the low prevalence of epileptic activity published in these patients. A metabolic/hypoxic mechanism seems unlikely on the basis of our EEG findings. This pattern in other etiologies is reminiscent of severe encephalopathy states associated with poor prognosis. However, an unreactive low voltage pattern in COVID-19 patients is not necessarily related to poor prognosis.
Keywords: COVID-19, SARS-CoV2, coronavirus, electroencephalogram, neurophysiology, neurological, central nervous system, brain, confusional, delirium, mental alteration
Introduction
Since neurological complications have been reported in patients with COVID-19,1–8 interest in EEG COVID-19 findings has been growing, especially in the search for a specific features EEG of encephalopathy in the setting of COVID-19. Today, continuous monitoring of EEG activity is a routine practice in certain specialized units such as critical care units or epilepsy units, and the advantage of follow-up studies in all types of EEG disturbances is becoming increasingly evident. At the onset of the pandemic, fear of increased COVID-19 infections led many clinical centers to cancel all EEG studies, especially continuous EEG monitoring studies. However, in hospitals where some activity has been maintained in the EEG units, it has been found that in strict compliance with safety rules, there was no increase in the number of infections.9 Thanks to this, it has been possible to demonstrate the usefulness of EEG studies in severe acute respiratory syndrome coronavirus 2 (SARS-CoV2)-infected patients with neurological manifestations and especially the importance of EEG monitoring. Given the high temporal resolution of the EEG, it allows us to perform a functional study of the patient, which also helps us to better understand the pathophysiology of the disease and its evolution: EEG is not only important for their acute clinical management but also might contribute to our understanding of the pathophysiological mechanisms of this novel disease, especially now that central neurological sequelae are being discovered.
At the beginning of the pandemic, there were many case reports concerning nonconvulsive status epilepticus (NCSE) and epileptic seizures (many of them in patients with preexisting neurological vulnerability),10–23 but relatively few case series with available descriptive EEG studied systematically.6,24–27 In the recent literature the most prevalent EEG finding was generalized continuous slow-wave activity as an expression of diffuse encephalopathy; and curiously, epileptic activity, NCSE and seizures were less prevalent than observed in other infectious pathologies16,24,25,28–32.
We describe the different electroencephalographic findings collected in patients with respiratory COVID-19 infection requiring hospital admission and neurological symptoms as well as its clinical and EEG evolution.
Material and Methods
Study Population
We retrospectively reanalyzed 29 EEGs performed in 15 patients diagnosed with COVID-19 (positive reverse transcription polymerase chain reaction for SARS-CoV-2), from March 29, 2020 to May 29, 2020, at Ramón y Cajal University Hospital Clinical (Madrid, Spain), during the coronavirus pandemic.
EEG recordings were carefully chosen from the Local EEG Database from the neurophysiology department. In addition, the medical charts of these patients have been consulted.
Study Design
We classified the EEGs according to the time they were performed with respect to evolution of the neurological symptoms in: “Acute EEG” (first EEG record performed urgently by neurological onset of symptoms); and “follow-up EEG” (performed for the second/third time on the patient as assessment of neurological development).
We performed 15 acute EEGs to 1 patient located in the Emergency Unit, 8 patients in the ICU and 6 patients in the non-intensive care unit (standard ward). These patients (14 male and 1 female, between 58 and 94 years of age) shown clinical alterations such as low level of awareness (7 patients), disorientation (6 patients), agitation (4 patients), suspicion of epileptic seizure (5 patients), aggressiveness (2 patients), aphasia (1 patient), confusion (1 patient), inattention (1 patient), dyscalculia (1 patient), disinhibition (1 patient), acute worsening of cognitive impairment (1 patient), and hemiparesis (1 patient). According to the predominant clinical symptoms, we classify encephalopathy into hypoactive (9 patients) and hyperactive (6 patients) (see Table 1).
Table 1.
Clinical Situation.
| Patient no. sex age | Reason for request EEG (hypoactive encephalopathy) | Comorbidities | Capillary oxygen saturation/supplemental oxygen/FiO2 | Hospital area at EEG/days since admission to EEG/need of ICU intubation | Sedative drugs (withdrawal >1 h before the EEG) | Pharmacological treatment previous weeks | Outcome |
|---|---|---|---|---|---|---|---|
| 1. m 58 | Aphasia, agitation (hyperactive) | Subclinical hypothyroidism, monoclonal gammopathy of undetermined significance | 94%/NC/FiO2 24% | Emergency room/EEG day 0 after admission/No ICU | Yes | Between the 1st and 2nd EEG: AZT, ACV, HCQ, CFT | Favorable (Complete resolution of the neurological state at discharge). |
| 2. m 61 | Somnolence, altered level of consciousness (hypoactive) | Ischemic heart disease, microhematuria | 97%/VM/FiO2 35% | ICU/EEG day + 33 after admission/ICU 29 days, intubated 28 days | No | LPV/r, CFT, TCL, BTF, RDV, PCTB, MPL, MPN, LZL | Favorable (Complete resolution of the neurological state at discharge). |
| 3. m 76 | Low awareness (hypoactive) | Asthma, obesity, hypertension, cardiac insufficiency | 98%/IV | ICU/EEG day + 28 after admission/ICU 23 days, intubated 22 days | Yes | HCQ, LPV/r, TCL, BTF | Deceased |
| 4.m 71 | Confusion, agitation and disorientation (hyperactive) | Diabetes mellitus type 2, obesity, hypertension | 97%/NRM/FiO2 35% | Ward/EEG day + 23 after admission/No ICU | No | HCQ, CFT, AZT, TCL | Favorable (Complete resolution of the neurological state at discharge). |
| 5. m 61 | Agitation, disorientation and inattention (hyperactive) | Hemochromatosis carrier, chronic inactive Hepatitis B virus, hepatic steatosis, tophaceous gout. | 96%/No supplemental oxygen | Ward/EEG day + 39 after admission/ICU 9 days, intubated 8 days | No | HCQ, LPV/r, BTF | Favorable (Mild encephalopathy at discharge: partial temporal disorientation, improving). |
| 6. m 52 | Disorientation, dyscalculia, disinhibition, and. flaccid tetraparesis. (hypoactive) | Secondary hypothyroidism, secondary hypogonadism, morbid obesity and hypertension, diabetes mellitus type 2, and dyslipidemia. | 96%/VM/FiO2 31% | Ward/EEG day + 26 after admission/ICU 17 days, intubated 12 days. | No | HCQ, LPV/r, AZT, TCL, MPL, VCM, LZL, ADF, MPN, PCTB | Favorable (Resolution of encephalopathy. Residual weakness of lower limbs, motor rehabilitation at discharge required). |
| 7. m 82 | Disorientation,aggressivenes,voluntary rigidity (hyperactive) | Hypertension and dyslipidemia | 94%/NC/FiO2 24% | Ward/EEG day + 32 after admission/No ICU | No | HCQ, LPV/r, CFT, AZT | Favorable (Mild encephalopathy at discharge). |
| 8. m 66 | Low awareness (hypoactive) | Pulmonary asbestosis | 97%/IV | ICU/EEG day + 49 after admission/ICU 17 days, intubated 16 days. | No | HCQ, LPV/r, CFT, AZT, MPL, BTF, MPN, FCZ, VCM, ERM | Stable (ICU. Moderate encephalopathy: fluctuating agitation and disorientation). |
| 9. m 78 | Disorientation, agitation, and mental decline (hyperactive) | Early-stage Alzheimer's disease | 95%/No supplemental oxygen | Ward/EEG day + 10 after admission/No ICU | No | Has not received drugs. | Favorable (No encephalopathy at discharge with mild cognitive impairment previous to admission). |
| 10. m 94 | Suspicion of epileptic seizures, disorientation, aggressiveness (hyperactive) | Mild cognitive impairment, hypothyroidism, hypertension, and dyslipidemia | 97%/NC/24% | Ward/EEG day + 12 after admission/No ICU | No | HCQ, AZT | Favorable (No encephalopathy at discharge with mild cognitive impairment previous to admission). |
| 11. m 62 | Low awareness and myoclonus (hypoactive) | Hypertension, dyslipidemia, and obesity | 94%/IV | ICU/EEG day + 34 after admission/ICU 27 days. intubated 18 days | Yes | HCQ, LPV/r, CFT, AZT, TCL, MPL, MPN, LZL | Deceased |
| 12. m 63 | Low awareness (hypoactive) | None reported | 96%/IV | ICU/EEG day + 40 after admission/ICU 39 days, intubated 39 days | Yes | HCQ, LPV/r, CFT, TCL, MPL, MPN, LZL, CXC, FCZ, CPF, RFP, GTM, DPT, ANB | Deceased |
| 13. m 60 | Low awareness, diabetic ketoacidosis + epileptic seizures (hypoactive) | Chronic supratentorial ischemic lacunar infarcts, diabetes mellitus type 2, and hypertension | 98%/VM/FiO2 50% | ICU/EEG day + 27 after admission/ICU 20 days, intubated 17 days | No | HCQ, CFT, LZL, ADF, MPN. Levetiracetam | Favorable. (Hospitalized. No encephalopathy, polyneuropathy). |
| 14. m 65 | Suspicion of epileptic seizures (hypoactive) | None reported | 96%/IV | ICU/EEG day + 52 after admission/ICU 33 days, intubated 33 days | Yes | HCQ, LPV/r, AZT, TCL, MPL, LZL, PCTB, LFX, TMP/SMX, RFP, GCV, ANB | Stable (ICU. Low awareness). |
| 15. f 79 | Low awareness and hemiparesis. (hypoactive) | Angioimmunoblastic T-cell lymphoma | 97%/IV | ICU/EEG day + 70 after admission/ICU 79 days, intubate 79 days | No | HCQ, LPV/r, CFT, AZT, MPL, PCTB, IMI, VCM, MPN, CPF, GCV, LFL, CFAV, BRTX | Deceased |
Abbreviations: HCQ, hydroxicloroquina; CFT, ceftriaxona; ACV, aciclovir; AZT, azitromicina; LPV/r, lopinavir/ritonavir; TCL, tocilizumab; RDV, remdesivir; BTF, betaferon; PCTB, piperacilina/tazobactam; MPL, metilprednisolona; MPN, meropenem; LZL, linezolid; ADF, anidulafulgina; FCZ, fluconazol; VCM, vancomicina; CXC, cloxacilina; ACM, acetazolamida; ERM, eritromicina; CPF, caspofungina; RFP, rifampicina; GTM, gentamicina; DPT, daptomicina; AMK, amikacina; ANB, anfotericina B; LFX, levofloxacino; TMP/SMX, trimetroprim/sulfametoxazol; GCV, ganciclovir; IMI, imipenem; LFL, levofloxacino; CFAV, ceftazidima/avibactam; BRTX, brentuximab; nasal cannulae (NC); Venturi mask (VM); nonrebreather mask (NRM); invasive ventilation (IV).
In addition, we have performed 14 follow-up EEGs to 11 patients (4 deceased) done at variable times between 2 and 51 days.
At all times, the safety rules established in our hospital were strictly respected, and the recommendations of the Spanish Society of Clinical Neurophysiology were followed. All personnel who were in contact with patients infected with SARS-CoV2 (both for electrode placement and clinical examination during the EEG study) followed safety protocols: personal protective equipment for COVID-19 (protective suits, filtering facepiece particle masks, double gloves, goggles, and face shields). No SARS-CoV2 infection was reported in the staff during EEG performance/interpretation. Equipment and material were carefully cleaned and there was no transmission to other patients who were not infected with SARS-CoV2.
EEG recordings were performed using 2 models of a 32-channel digital system: EEG32U, NeuroWorks, XLTEK; and EEG32U, Sienna Ultimate, MS biomedical. In this study, we used the Clinical Neurophysiology department protocols, with an electro-cap with 21 electrodes using the International Standard 10/20 System and an additional electrocardiogram channel (full montage for evaluation of the temporal lobe and the inferior part of the frontal33). Electro-caps instead of subdermal needle electrodes were used to allow us to minimize impedances and artifacts of head movement, and to avoid accidental injury to the technicians. Recordings were performed at a 512 Hz sampling rate, with a filter bandwidth of 0.5 to 70 Hz and notch filter of 50 Hz. Electrode impedance was usually bellow 15 kΩ. The recordings were synchronized with a video and had a minimum duration of at least 20 min.
Depending on the patient's level of consciousness, the exploration of the reactivity of the trace was different: in patients with a good level of consciousness or discrete tendency to sleepiness at the time of the EEG, we ask the patients to open and close their eyes and external stimuli of the sound type (patients were called by their names) were performed; when the level of consciousness was diminished, external stimuli of the sound (patients were called by their names) and pain type (strong pinch held in the submental region) were performed for all patients. EEG background reactivity was defined as any change in amplitude or frequency after external stimuli.34
Although the aim of the recordings was to perform a standard EEG of short duration and not a complete sleep analysis, spontaneous sleep was recorded in 8 EEG out of 29 made (5 acute EEG and 3 follow-up EEG), which allowed us to better characterize the encephalopathies see Table 2.
Table 2.
Background: Acute Electroencephalogram (EEG) + Follow-up EEG.
| Patient | Symmetry | Posterior dominant rhythm | Background EEG frequency | Antero-posterior gradient | Variability | Reactivity | Longitudinal bipolar voltage (µV). Referential voltage (µV) | Stage II sleep transients (min sleep/min recording) | Continuity | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1a | 1st EEG Day 0 | Symmetric | Absent | Theta–Delta | Absent | Absent | Absent | Bipolar: low (15 µV) Referential: low (16 µV) | / | Continuous |
| 2nd EEG. + 51 d | Symmetric | Present | Alpha | Present | Present | Present | Bipolar: normal (24 µV) Referential: normal (26 µV) | / | Continuous | |
| 2 | 1st EEG Day 0 | Symmetric | Absent | Theta–Delta | Absent | Present | Unclear | Bipolar: suppressed (7 µV) Referential: suppressed (7 µV) | Present but abnormal (15/23) | Continuous |
| 2nd EEG. + 46 d | Symmetric | Present | Alpha (10 Hz) | Present | Present | Present | Bipolar: normal (90 µV) Referential: normal (117 µV) | / | Continuous | |
| 3 | 1st EEG | Symmetric | Absent | Isoelectric | Absent | Absent | Absent | Bipolar: suppressed (3 µV) Referential: suppressed (4 µV) | / | Continuous |
| 4 | 1st EEG Day 0 | Symmetric | Absent | Theta–Delta | Absent | Present | Absent | Bipolar: low (12 µV) Referential: low (16 µV) | Absent (10/30) | Continuous |
| 2nd EEG + 12 | Symmetric | Absent | Theta (7 Hz) | Present | Present | Unclear | Bipolar: normal (34 µV) Referential: normal (41 µV) | / | Continuous | |
| 3rd EEG + 14 | Symmetric | Absent | Theta (7-8 Hz) | Present | Present | Unclear | Bipolar: normal (35 µV) Referential: normal (31 µV) | / | Continuous | |
| 5 | 1st EEG Day 0 | Symmetric | Absent | Theta–Delta | Absent | Present | Absent | Bipolar: low (14 µV) Referential: low (16 µV) | / | Continuous |
| 2nd EEG + 18 | Symmetric | Present | Theta (7 Hz) | Present | Present | Present | Bipolar: normal (25 µV) Referential: normal (26 µV) | Present but abnormal (5/23) | Continuous | |
| 6 | 1st EEG Day 0 | Symmetric | Absent | Theta | Absent | Present | Absent | Bipolar: low (18 µV) Referential: low (19 µV) | Absent (5/20) | Continuous |
| 2nd EEG + 10 | Symmetric | Present | Theta (6-7 Hz) | Present | Present | Present | Bipolar: normal (30 µV) Referential: normal (27 µV) | Absent (6/20) | Continuous | |
| 3rd EEG + 17 | Symmetric | Present | Theta (6-7 Hz) | Present | Present | Present | Bipolar: normal (30 µV) Referential: normal (27 µV) | / | Continuous | |
| 7 | 1st EEG Day 0 | Symmetric | Absent | ≥Alpha | Absent | Absent | Absent | Bipolar: low (14 µV) Referential: low (17 µV) | / | Continuous |
| 2nd EEG + 8 | Symmetric | Present | Alpha (8-9 Hz) | Present | Present | Present | Bipolar: normal (27 µV) Referential: normal (28 µV) | / | Continuous | |
| 8 | 1st EEG Day 0 | Symmetric | Absent | Theta–Delta | Absent | Present | Absent | Bipolar: low (11 µV) Referential: low (14 µV) | / | Continuous |
| 2nd EEG + 19 | Symmetric | Absent | Theta (7 Hz) | Absent | Present | Absent | Bipolar: normal (20 µV) Referential: normal (23 µV) | / | Continuous | |
| 9 | 1st EEG Day 0 | Symmetric | Absent | Theta (7 Hz) | Present | Present | Unclear | Bipolar: low (13 µV) Referential: low (17 µV) | Absent (7/24) | Continuous |
| 2nd EEG + 25 | Symmetric | Present | Alpha (9-10 Hz) | Present | Present | Present | Bipolar: normal (29 µV) Referential: normal (33 µV) | / | Continuous | |
| 10 | 1st EEG Day 0 | Symmetric | Absent | Theta–Delta | Absent | Present | Absent | Bipolar: suppressed (7 µV) Referential: suppressed (8 µV) | / | Continuous |
| 2nd EEG + 16 | Symmetric | Present | Alpha (8 Hz) | Present | Present | Present | Bipolar: normal (27 µV) Referential: normal (26 µV) | Absent (10/27) | Continuous | |
| 11 | 1st EEG | Symmetric | Absent | Theta–Delta | Absent | Present | Absent | Bipolar: suppressed (5 µV) Referential: suppressed (7 µV) | / | Burst-suppression |
| 12 | 1st EEG | Symmetric | Absent | Theta–Delta | Absent | Absent | Absent | Bipolar: low (13 µV) Referential: low (18 µV) | / | Continuous |
| 13 | 1st EEG Day 0 | Symmetric | Absent | Theta (7 Hz) | Present | Present | Absent | Bipolar: normal (20 µV) Referential: normal (22 µV) | Absent (9/23) | Continuous |
| 2nd EEG + 14 | Symmetric | Present | Alpha (9 Hz) | Present | Present | Present | Bipolar: normal (40 µV) Referential: normal (32 µV) | / | Continuous | |
| 14 | 1st EEG | Symmetric | Absent | Theta–Delta | Absent | Absent | Absent | Bipolar: low (13 µV) Referential: low (18 µV) | / | Continuous |
| 2nd EEG + 11 | Symmetric | Absent | Theta-Delta | Absent | Absent | Absent | Bipolar: low (15 µV) Referential: low (19 µV) | / | Continuous | |
| 3rd EEG + 17 | Symmetric | Absent | Theta–Delta | Absent | Absent | Unclear | Bipolar: low (15 µV) Referential: low (19 µV) | Absent (17/21) | Continuous | |
| 15a | 1st EEG | Symmetric | Absent | Theta–Delta | Absent | Present | Absent | Bipolar: low (19 µV) Referential: low (19 µV) | / | Continuous |
Breach effect absent in all of them.
After antiepileptic: no changes.
The studies were carried out without sedation effects or any drugs with EEG influence in a known way, except in 5 patients, whose hemodynamic situation only allowed the withdrawal of sedative drugs 1 h before our study (patient #1, patient #3, patient #11, patient #12, and patient #14) (see Table 1).
A specialist (with several years of experience in EEG) and a resident in Clinical Neurophysiology (MD) were present during the complete performance of all the recordings and prepared clinical reports.
Afterwards, the description of the EEG records was made according to the American Neurophysiology Society standardized critical-care EEG terminology, albeit not all patients were in the ICU, to have a systematic procedure for a better comparison with other series35 (see Tables 2 and 3). We applied the Salzburg Consensus Criteria to the diagnosis of suspicion of NCSE.36
Table 3.
Rhythmic and Periodic Patterns Superimposed Over Background: Acute Electroencephalography (EEG) and Follow-up EEG.
| Patient | Acute EEG Follow-up EEG | Main term 1 | Main term 2 | Major modifiers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| “Localization” | “Waveform” | Prevalence | Duration | Frequency | Number of phases | Sharpness | Absolute amplitude | Relative amplitude | Polarity | Stimulus induced | Evolution | ||
| 1a | 1st EEG Day 0 | Lateralized (left fronto-temporal lobe. Sometimes bilateral asymmetric). | Rhythmic delta activity (RDA) (theta) | Abundant | Brief | >4/s | 1 | Blunt (236 ms) | Low (40 µV) | / | Negative | Spontaneous only | Static |
| 2nd EEG. + 51 d | Lateralized (left fronto-temporal: bilateral asymetric). | Irregular theta (arrhythmic theta) | Frequent (20%) | Very brief (2 s) | >4/s (4.6 Hz) | 1 | Blunt (220 ms) | Low (28 µV) | / | Negative | Spontaneous only | Static | |
| 2 | 1st EEG Day 0 | Lateralized (left fronto-temporal. Bilateral asymmetric) | RDA (theta and delta) | Occasional | Very brief | >4/s | 1 | Blunt | Medium (80 µV) | / | Negative | Spontaneous | Static |
| 2nd EEG. + 46 d | Lateralized (left fronto-temporal) | Irregular theta (arrhythmic theta) | Occasional | Very brief | >4/s | 1 | Sharply contoured | Low (40 µV) | / | Negative | Spontaneous only | Static | |
| 3 | 1st EEG | No rhythmic or periodic patterns | |||||||||||
| 4 | 1st EEG Day 0 | Generalized | RDA (theta) | Abundant (80%) | Brief | >4/s (6-7 Hz) | 1 | Blunt (236 ms) | Low (27 µV) | / | Negative | Spontaneous only | Static |
| 2nd EEG + 12 d | Lateralized (left temporal: bilateral asymmetric) | Irregular delta | Frequent (20%) | Very brief (<10 s) | 0.5-1 Hz | 1 | Blunt | Low (35-40 µV) | / | Negative | Spontaneous only | Static | |
| 3rd EEG + 14 d | Lateralized (left temporal: bilateral asymmetric) | Irregular delta | Occasional (5%) | Very brief (<10 s) | 0.5-1 Hz | 1 | Blunt | Low (35-40 µV) | / | Negative | Spontaneous | Static | |
| 5 | 1st EEG Day 0 | No rhythmic or periodic patterns | |||||||||||
| 2nd EEG + 18 d | No rhythmic or periodic patterns | ||||||||||||
| 6 | 1st EEG Day 0 | Generalized | RDA (theta) | Abundant | Brief | >4/s (5 Hz) | 1 | Blunt | Low (10-20 µV) | / | Negative | Spontaneous | Static |
| 2nd EEG + 10 d | No rhythmic or periodic patterns | ||||||||||||
| 3rd EEG + 17 d | No rhythmic or periodic patterns | ||||||||||||
| 7 | 1st EEG Day 0 | No rhythmic or periodic patterns | |||||||||||
| 2nd EEG + 8 d | No rhythmic or periodic patterns | ||||||||||||
| 8 | 1st EEG Day 0 | Generalized | RDA (theta) | Abundant (50%) | Brief | >4/s (6 Hz) | 1 | Blunt | Low (15 µV) | / | Negative | Spontaneous | Static |
| 2nd EEG + 19 d | No rhythmic or periodic patterns | ||||||||||||
| 9 | 1st EEG Day 0 | No rhythmic or periodic patterns | |||||||||||
| 2nd EEG + 25 d | No rhythmic or periodic patterns | ||||||||||||
| 10 | 1st EEG Day 0 | Lateralized (fronto-temporal left) | RDA | Continuous | Intermediate duration | >4/s (5 Hz) | 1 | Blunt | Low (25 µV) | / | Negative | Spontaneous | Static |
| 2nd EEG + 16 d | Lateralized (left frontotemporal lobe) | RDA (theta) | Continuous | Intermediate duration | >4 Hz (5 Hz) | 1 | Blunt | Low (25 µV) | / | Negative | Spontaneous | Static | |
| 11 | 1st EEG | Generalized | RDA (theta) | Frequent | Brief | >4/s (7 Hz) | 1 | Blunt | Low (13-15 µV) | / | Negative | Spontaneous | Static |
| 12 | 1st EEG | No rhythmic or periodic patterns | |||||||||||
| 13 | 1st EEG Day 0 | Lateralized (right parieto-temporal) | Irregular delta (1-2 Hz) | Occasional | Very brief | 0.5-1/s | 1 | Blunt | Low (40 µV) | / | Negative | Spontaneous | Static |
| 2nd EEG + 14 d | No rhythmic or periodic patterns | ||||||||||||
| 14 | 1st EEG | No rhythmic or periodic patterns | |||||||||||
| 2nd EEG + 11 d | No rhythmic or periodic patterns | ||||||||||||
| 3rd EEG + 17 d | No rhythmic or periodic patterns | ||||||||||||
| 15a | 1st EEG | Lateralized (bilateral asymmetric) | periodic discharges (PD) | Continuous | Long | 1/s | 2 | Sharp | Low (40-50 µV) | >2 | Negative | Spontaneous only | Static |
After antiepileptic: no changes.
Voltage amplitude (in µV) was obtained in longitudinal bipolar recordings with standard 10-20 electrodes measured from peak to trough as required by the American Clinical Neurophysiology Society's Standardized Critical Care EEG Terminology,35 in occipitoparietal differential channels, and we choose the higher value. The same channels were used to identify the dominant frequency of the posterior rhythm. Additionally, the voltage amplitude was measured in referential montage (referenced to average) in the channel “P4.” (see Table 2).
Additionally, we have consulted the medical charts of these patients, and the following variables were studied: bio-demographic characteristics, personal history, metabolic disturbances, inflammatory markers and thyroid hormone in serum analytic, cerebrospinal fluid analysis (if performed), capillary oxygen saturation, clinical symptoms, clinical evolution, the place where the EEG (critical care unit or standard ward) was performed, neuroimaging findings, present of sedative drugs during EEG recording, and drugs used in the previous weeks (see Table 1).
Most of the variables of the EEGs did not offer variability in the characteristics found (100% of the traces were symmetrical, 100% of the acute EEGs did not present a dominant posterior rhythm, 13 EEGs out of 15 showed reactivity absent, 14 EEG out of 15 were continuous). For this reason, we did not make a statistical analysis relating these variables of the EEG trace with the clinical parameters.
However, we did an exploratory statistical analysis, since we have a small number of patients, shown in Table 4. We considered the voltage variable as continuous and analyze it separately with measurements in bipolar montage and with measurements in reference montage. We will analyze the relationship of this variable with the respiratory status of the patient at that time, using the variable as ordinal (no oxygen supply required, nasal cannulas, Venturi mask, no rebreather mask, invasive ventilation); with days of stay in the ICU (as a continuous variable); with outcome, using the variable as ordinal (favorable, stable, deceased); with the stay or not in ICU (categorical variables); with sedative drugs withdrawal >1 h before EEG or not sedative drugs (categorical variables); with pharmacological treatment in the previous weeks or no pharmacological treatment (categorical variables); with type of symptoms predominating in encephalopathy: hypoactive or hyperactive (categorical variables). We use Spearman's correlation coefficient (Rho of Spearman) for continuous variables and Mann–Whitney U for categorical and ordinal variables.
Table 4.
Statistical Analysis.
| Bipolar montage | Referential montage | ||||
|---|---|---|---|---|---|
| Median (percentile 25; percentile 75) | Mann–Whitney U | Median (percentile 25; percentile 75) | Mann–Whitney U | ||
| Stay in ICU | No | 14 (12; 15) | 0.40 | 16 (16; 17) | 0.89 |
| Yes | 12 (6; 16) | 16 (7; 18.5) | |||
| Sedative drugs | No | 13.5 (11; 18) | 0.29 | 16.5 (14; 19) | 0.45 |
| Yes (withdrawal >1 h before the EEG) | 13 (5; 13) | 16 (7; 18) | |||
| Pharmacological treatment previous weeks | No | 14 (13; 15) | 0.57 | 16.5 (16; 17) | 0.99 |
| Yes | 13 (7; 14) | 16 (8; 18) | |||
| Type of symptoms predominating in encephalopathy | Hypoactive | 13 (7; 18) | 0.79 | 18 (7; 19) | 0.66 |
| Hyperactive | 13.5 (7; 15) | 16 (16; 17) | |||
| Spearman's rho | Signification level (P) | Spearman's rho | Signification level (P) | ||
| Respiratory status | −0.29 | P = .28 | −0.04 | P = .88 | |
| Days of stay in ICU | −0.02 | P = .92 | 0.17 | P = .53 | |
| Outcome of the COVID-19 | −0.31 | P = .25 | −0.11 | P = .69 | |
Abbreviations: ICU, intensive care unit; COVID-19, coronavirus disease-2019.
A cutoff P-value of 0.05 was considered significant.
Results
The demographics description, clinical symptoms and evolution, capillary oxygen saturation, serum analysis, hospital area where the EEG was performed, days since admission to EEG, need of ICU/intubation, if sedative drugs were used at time to perform EEG, pharmacological treatment previous weeks to perform EEG, are shown in Table 1. All patients remained above 94% saturation, although they needed different oxygen supplies due to their variable respiratory situation.
Cerebrospinal fluid analysis was performed in 7 patients and was normal. Cranial magnetic resonance imaging (MRI) or computerized tomography demonstrated no specific findings, except patient #3 (acute diffuse punctiform lesions) and patient #14 (acute left frontal hematoma). Metabolic analytical data at the time of EEG showed no hepatic, renal alterations, or acidosis. Thyroid hormones were normal in all patients except one (near normal, for previous subclinical hypothyroidism). All patients showed inflammatory data (interleukins or C reactive protein).
In total, 29 EEG recordings were analyzed.
The descriptions of the 15 acute EEG recordings (performed urgently on each patient for presenting all of the neurological symptoms at that moment) and 14 follow-up EEGs are shown in Table 2 (background activity) and Table 3 (superimposed rhythmic or periodic activity).
With respect to the background activity, 100% of acute EEG and follow-up EEG were symmetric; 100% of acute EEG versus only of 35% of follow-up EEG presented an absence of a posterior dominant rhythm; the background EEG frequency was: alpha at 6.6% on acute EEG versus at 42.8% of follow-up EEG, theta at 20% of acute EEG versus at 42.8% follow-up EEG, theta–delta at 66.6% of acute EEG versus at 14.2% of follow-up EEG, and isoelectric at 6.6% of acute EEG versus at 0% of follow-up EEG; the antero-posterior gradient was absent in 86% of acute EEG versus only in 21.4% of follow-up EEG; the variability was absent at 33.3% of acute EEG versus at 14.2% of follow-up EEG; reactivity was absent at 86.6% of acute EEG versus only at 14.2% of follow-up EEG; unclear at 13.3% of acute EEG versus at 21.4% of follow-up EEG, and present at 0% of acute EEG versus at 64.2% of follow-up EEG; the voltage was similar when measured in bipolar montage than when measured in reference montage; in total voltage ≤20 µV at 100% of “acute EEG,” versus only 21.4% of “follow-up EEG”: was suppressed at 26.6% of acute EEG versus at 0% follow-up EEG, low at 66.6% of acute EEG versus at 14.2% of follow-up EEG, and normal at 6.6% of acute EEG (only 1 EEG at just 20 µV) versus at 85.7% of follow-up EEG; when spontaneous sleep was recorded at standard records (duration of 20-30 min), stage II sleep transients were absent in 80% of acute EEG with sleep versus in 75% of follow-up EEG, present but abnormal in 20% of acute EEG versus at 25% of follow-up EEG, and present and normal at 0% of acute EEG versus at 0% of follow-up EEG; 93.3% of acute EEG versus 100% of follow-up EEG was continuous, and 6.6% of acute EEG versus 0% of follow-up EEG showed a burst-suppression.
The average voltage of the background activity of the acute EEG was 12.33 ± 5.09 µV and of the follow-up EEGs was 32.8 ± 20.13 µV.
Four of the initial 15 patients died in the initial phase and we did not perform a follow-up EEG. Of the 11 patients who underwent EEG control, 6 patients progressed to normal EEG and 4 achieved present and reactive background activity with normal voltage but in the theta frequency: these findings correlate with the patient's mental state at the time (asymptomatic or returning to baseline), although we do not have EEG records of those patients prior to COVID-19. And finally 1 patient persisted with several similar low voltage EEGs and clinically remained with a low level of consciousness.
Spontaneous sleep was recorded in 8 EEGs out of 29 made (5 acute EEGs and 3 follow-up EEGs). Acute EEG: in patient #2 of 23 min recorded, 15 were sleepy, with sleep spindles present but abnormal; in patient #4 of 30 min recorded, 10 were sleepy, with absence of sleep spindles; in patient #6 of 20 min recorded, 5 were sleepy, with absence of sleep spindles; in patient #9 of 24 min recorded, 7 were sleepy, with absence of sleep spindles; in patient #13 of 23 min recorded, 9 were sleepy, with absence of sleep spindles; follow-up EEGs: in patient #5 of 23 min recorded, 5 were sleepy, with sleep spindles present but abnormal; in patient #6 of 20 min recorded, 6 were sleepy, with absence of sleep spindles; in patient #10 of 27 min recorded, 10 were sleepy, with absence of sleep spindles; at patient #14 of 21 min recorded, 17 were sleepy, with absence of sleep spindles.
With respect to the superimposed rhythmic or periodic activity, 60% of acute EEG versus 35.7% of follow-up EEGs presented a superimposed rhythmic and monomorphic theta-range focal activity, which appears intermittently over the front temporal region in all of them. According to American Clinical Neurophysiology Society's Standardized Critical Care EEG Terminology none of these rhythmic or periodic patterns had “Plus Modifiers.” Regarding to “Minor Modifiers,” all of them had a “Sudden Onset,” but no “Triphasic” morphology, nor was “Lag” observed. None of them had “Sporadic Epileptiform Discharges.”
Only one EEG (Patient #15) presented continuous sharp lateralized periodic discharges (generalized with predominance over left frontal-central regions), 1/s frequency, and medium absolute amplitude (just 20 µV). As “Minor Modifiers,” it had a “Sudden Onset,” with no “Triphasic” morphology nor “Lag.”
As NCSE was suspected in patient #1 and patient #15, the Salzburg consensus criteria were applied to assess the modifications of the traces after the administration of an intravenous antiepileptic drug (lacosamide 200 mg), as they presented a pattern with “epileptiform discharges (2.5 Hz) or rhythmic delta/theta activity (> 0.5 Hz)”36 with a continuous prevalence and long duration. The pattern did not change after lacosamide administration, with no changes in the symptoms, so NCSE was discarded in both patients.
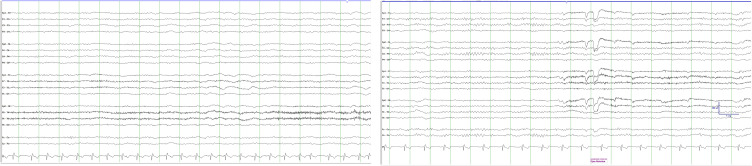
In Figure 1, we can see an example (patient #4) of the evolution of the trace over time. In the left panel, we see a low voltage acute EEG with no posterior dominant rhythm over which a bilateral front-temporal intermittent rhythmic activity is superimposed, of left predominance (left panel). In the right panel, we see a follow-up EEG (12 days later) with posterior dominant rhythm, with normal voltage, over which a focal slow activity persists over front-temporal region (right panel). At the time of the second recording, the patient is asymptomatic.
Figure 1.
Patient #4. Acute electroencephalography (EEG) with no posterior dominant rhythm and low voltage on which is highlighted rhythmic activity bilateral fronto-temporal with left predominance (left panel); and 12 days later, follow-up EEG (right panel) with posterior dominant rhythm and normal voltage on which is added arrhythmic left fronto-temporal activity. Notch filter 50 Hz; Filter bandwidth of 0.3 to 70 Hz 10 µV/mm; 30 mm/s.
We have not found a statistically significant association between voltage of acute EEG (neither measured with bipolar nor with reference montage) and the respiratory situation (P = .28 for bipolar montage; P = .88 for referential montage), area of the hospital where the EEG is performed (P = .40 for bipolar montage, P = .89 for referential montage), period of stay in ICU (P = .92 for bipolar montage; P = .53 for referential montage), sedative drugs withdrawal >1 h before the EEG or not sedative drugs (P = .29 for bipolar montage, P = .45 for referential montage), pharmacological treatment in previous weeks (P = .57 for bipolar montage, P = .99 for referential montage), predominance of hyperactive or hypoactive encephalopathy (P = .79 for bipolar montage, P = .66 for referential montage), final prognosis (P = .25 for bipolar montage; P = .69 for referential montage).
The way of measuring the voltage of the registers (bipolar longitudinal montage vs. referential montage) did not cause them to change category according to the ACNS classification. In Figure 2, we can see the same trace of patient #5 presented at bipolar longitudinal montage (left panel) and referential montage (right panel).
Figure 2.
Patient #5. Acute electroencephalography (EEG) presented at bipolar longitudinal montage (left panel) and average referential (right panel). Notch filter 50 Hz; Filter bandwidth of 0.3 to 70 Hz; 10 µV/mm; 30 mm/s.
Discussion
At the present time there is a great scientific debate on whether the nonspecific but similar findings in the published case series with COVID-19 encephalopathy (disorganized background activity with diffuse slowing of frontal predominance, many of them nonreactive) can be considered distinctive features of COVID-19 or if on the contrary it is due to a multifactorial origin not directly caused by the virus.
In our series, we found similar results to those published regarding a pattern with no background activity, largely nonreactive, but the most striking finding is a reduction in voltage. Few articles published on EEG and COVID-19 mention the voltage of the background activity.24,29,31 Some authors have also found low voltage but relate it to metabolic or ischemic causes without demonstrating it. We believe that the problem may be that most published studies have been done with a different methodology than the standard: only 9 electrodes instead of 21 (to reduce the risk of contagion). The currently accepted voltage normality values as well as the criteria of the American Neurophysiology Society standardized critical care EEG terminology are obtained with 21-electrode assemblies, considered the gold standard.35 It is known that the distance between the electrodes influences the voltage37 so that 10-electrode recordings double the interelectrode distance and obtain a higher voltage, so they should have their own normative values (not yet established).
Low voltage patterns are also described in 10% of normal individuals38 who are not able to generate an alpha-dominant rhythm, but always show reactivity, and beta and alpha frequencies are intermixed. During sleep, typical waveforms appear.38,39 In our series, we found 100% of our patient with voltage at or below 20 µV and we rarely found reactivity. We performed standard EEG with insufficient duration to explore sleep, but when patient spontaneously fell asleep the spindles were absent or were abnormal. In follow-up registers performed in patients with a favorable outcome revealed the emergence of a posterior dominant theta rhythm that ruled out that our patients had a physiological absence of posterior alpha rhythm.
Low voltage or generalized suppression patterns is often associated with extensive cortical and subcortical lesions such as anoxic encephalopathy or severe head trauma. This pattern was related to an unfavorable prognosis (score 4 qualitative classification of EEG alteration: Amodio et al., 1999)40–42 or irreversible character as at ischemic encephalopathy39,42–45 with the exception of hypothyroid encephalopathy, which is reversible except for cretinism.39,42,43,45–47, but in our series we found a good evolution in 60% of the patients. It has also been described in diffuse neuronal dysfunction like hypothermia, intoxication by central nervous system depressant drugs or anesthesia,39,43,44 but we have ruled out all these causes in our patients.
EEG patterns we observe has findings like those observed in ischemic encephalopathy described in the literature (low voltage and unreactive to external stimuli).39,40,42–45 However, by performing follow-up EEGs, we have been able to document how our patients present a reversible picture both in the clinic and in the EEG. So, we also believe that ischemia does not appear to be the cause of these EEG findings, in addition to the fact that the respiratory and hemodynamic status of patients does not suggest it (some patients did not even need oxygen).
It could be thought that since the common feature of all our patients is a respiratory disorder related to SARS-CoV-2, EEG findings may be due to neurological manifestations of habitual pneumonia. However, EEG findings in respiratory failure are already known33,42,48 and different from what we have observed in our series; moreover, our patients did not have hypercapnia.
We have found a good correlation between the clinical situation at the time of performing EEG and voltage of EEG (both in the acute EEG and in the follow-up EEG), but we have not found a correlation between voltage of acute EEG and final outcome.
A systematic review of EEG findings in 617 patients publishes frontal findings are frequent and have been proposed as a biomarker for COVID-19 encephalopathy46 and there is 1 report describing focal frontotemporal hypoperfusion in patients with COVID-19, in MRI.6 In 4 of our 15 patients we have observed a focal rhythmic activity over frontotemporal regions, without any structural abnormality in the standard sequences of MRI. In two patients, we ruled out an NCSE using the Salzburg consensus criteria. In the follow-up EEG in some patients this focal activity persisted, but we do not know how to explain the significance.
Our study is limited by the small sample size and the fact that it is a retrospective study. However, perhaps the low prevalence of epileptic activity (NCS, seizures, and interictal epileptiform discharges) described in patients with COVID-19,16,24,25,28–31 could be explained by the low voltage findings in our EEG series possibly due to desynchronization. Low voltage EEG does not exclude the possibility of epilepsy but it is rarer to find low voltage patterns in epilepsy.38 In our series, the only patient who has presented epileptiform discharges is the one with the highest voltage in the background activity of all our patients (20 µV).
A recent publication, based on the high percentage of “alpha coma/spindle coma” pattern in their case series (given how rare this pattern is),31,49 hypothesizes on a possible neurotropic effects of SARS-CoV-2 on the ascending reticular formation within the brainstem–talamus axis, which could also explain some cases of associated flaccid tetraparesis. This debate is very important because, a brainstem affectation (with the danger of a respiratory center alteration) could totally change the way patients are handled.
If this finding is confirmed, an affectation of the ascending reticular formation (within the brainstem–talamus axis) would be a possible cause of the low voltage finding in our series, since a functional integrity of the ascending reticular system is needed to generate a synchronization of the EEG trace with higher voltage. It could even explain the absence of reactivity in many of the EEGs, which in the rest of the pathologies has always been classically associated with a poor prognosis although it is not yet validated for the COVID, as it seems that it could be an exception. In our series, we were not able to predict the final prognosis of the patient with the acute EEG and we have been able to demonstrate that an unreactive low voltage pattern in COVID-19 patients is not necessarily related to poor prognosis.
In addition to the level of affectation, it would also be necessary to discover whether the mechanism of action is a functional affectation (which may be transitory) or a structural lesion (which would be more irreversible). Future studies are needed in order to clarify the role of inflammatory agents in the EEG findings, and whether there are transient alterations in neurotransmitters as observed in septic or metabolic encephalopathies.39,50
Following safety protocols for personnel, continuous and follow-up studies should be performed on patients with neurological manifestations in COVID-19, because of the valuable information it provides.
Conclusions
We have found an unspecific pattern of EEG in patients with COVID-19 similar to those described in the literature, which is different from the ones encountered in other infectious or metabolic encephalopathies. However, we found, as a distinctive finding, a low voltage that has not been described in the published reports of COVID-19, and is reminiscent of severe encephalopathy states associated with poor prognosis. We have been able to demonstrate that an unreactive low voltage pattern in COVID-19 patients is not necessarily related to poor prognosis. We have seen this common pattern both in ICU and standard ward patients and patients with favorable evolution or progressive worsening. In those with a favorable outcome the abnormalities found a trend to wane into a normal EEG. A metabolic/hypoxic mechanism seems unlikely on the basis of our EEG findings. Our finding of low voltage EEG possibly due to desynchronization could explain the low prevalence of epileptic activity described in patients with COVID-19. Our series points out the necessity of prospective and large-scale studies (with complete international standard 10/20 montage) to delineate precisely the neurophysiological manifestations of COVID-19.
Acknowledgments
We thank Alfonso Muriel García for her assistance with the statistical study of the manuscript.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The local board of the Ethics Committee of our center (Comité de Ética e Investigación de Medicamentos IRICYS—Fundación para la Investigación Biomédica del Hospital Universitario Ramón y Cajal) approved the research protocol of this study and written informed consent was not required.
ORCID iDs: Isabel Sáez-Landete https://orcid.org/0000-0003-1089-4004
Adriana Gómez-Domínguez https://orcid.org/0000-0003-4965-2707
Alba Díaz-Cid https://orcid.org/0000-0001-8416-5205
References
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson R. Pandemic potential of 2019-nCoV. Lancet Infect Dis. 2020;20(3):280. doi: 10.1016/S1473-3099(20)30068-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients With coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683-690. doi: 10.1001/jamaneurol.2020.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18-22. doi: 10.1016/j.bbi.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268-2270. doi: 10.1056/NEJMc2008597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paterson RW, Brown RL, Benjamin L, et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020;143:3104-3120. doi: 10.1093/brain/awaa240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egbert AR, Cankurtaran S, Karpiak S. Brain abnormalities in COVID-19 acute/subacute phase: a rapid systematic review. Brain Behav Immun. 2020;89:543-554. doi: 10.1016/j.bbi.2020.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campanella S, Arikan K, Babiloni C, et al. Special report on the impact of the COVID-19 pandemic on clinical EEG and research and consensus recommendations for the safe use of EEG. Clin EEG Neurosci. 2021;52(1):3-28. doi: 10.1177/1550059420954054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Filatov A, Sharma P, Hindi F, Espinosa PS. Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus. 2020;12(3):e7352. doi: 10.7759/cureus.7352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duong L, Xu P, Liu A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in downtown Los Angeles, early April 2020. Brain Behav Immun. 2020;87:33. doi: 10.1016/j.bbi.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flamand M, Perron A, Buron Y, Szurhaj W. Pay more attention to EEG in COVID-19 pandemic. Clin Neurophysiol. 2020;131:2062-2064. doi: 10.1016/j.clinph.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vellieux G, Rouvel-Tallec A, Jaquet P, Grinea A. Sonneville R, d’Ortho M-P. COVID-19 associated encephalopathy: is there a specific EEG pattern? Clin Neurophysiol. 2020;131(8):1928-1930. doi: 10.1016/j.clinph.2020.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Somani S, Pati S, Gaston T, Chitlangia A, Agnihotri S. De novo status epilepticus in patients with COVID-19. Ann Clin Transl Neurol. 2020;7(7):1240-1244. doi: 10.1002/acn3.51071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cecchetti G, Vabanesi M, Chieffo R, et al. Cerebral involvement in COVID-19 is associated with metabolic and coagulation derangements: an EEG study. J Neurol. 2020;267:3130-3134. doi: 10.1007/s00415-020-09958-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vespignani H, Colas D, Lavin BS, et al. Report on electroencephalographic findings in critically ill patients with COVID-19. Ann Neurol. 2020;88:626-630. doi: 10.1002/ana.25814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galanopoulou AS, Ferastraoaru V, Correa DJ, et al. EEG findings in acutely ill patients investigated for SARS-CoV-2/COVID-19: a small case series preliminary report. Epilepsia Open. 2020;5(2):314-324. doi: 10.1002/epi4.12399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdel-Mannan O, Eyre M, Löbel U, et al. Neurologic and radiographic findings associated with COVID-19 infection in children. JAMA Neurol. 2020;77:1440-1445. doi: 10.1001/jamaneurol.2020.2687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Stefano P, Nencha U, De Stefano L, Mégevand P, Seeck M. Focal EEG changes indicating critical illness associated cerebral microbleeds in a Covid-19 patient. Clin Neurophysiol Pract. 2020;5:125-129. doi: 10.1016/j.cnp.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hepburn M, Mullaguri N, George P, et al. Acute symptomatic seizures in critically Ill patients with COVID-19: is there an association? Neurocrit Care. 2021;34:139-143. doi: 10.1007/s12028-020-01006-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vollono C, Rollo E, Romozzi M, et al. Focal status epilepticus as unique clinical feature of COVID-19: a case report. Seizure. 2020;78:109-112. doi: 10.1016/j.seizure.2020.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elgamasy S, Kamel MG, Ghozy S, Khalil A, Morra ME, Islam SMS. First case of focal epilepsy associated with SARS-coronavirus-2. J Med Virol. 2020;92:2238-2242. doi: 10.1002/jmv.26113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roy-Gash F, Marine DM, Jean-Michel D, Herve V, Raphael B, Nicolas E. COVID-19-associated acute cerebral venous thrombosis: clinical, CT, MRI and EEG features. Crit Care. 2020;24(1):419. doi: 10.1186/s13054-020-03131-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pastor J, Vega-Zelaya L, Martín Abad E. Specific EEG encephalopathy pattern in SARS-CoV-2 patients. J Clin Med. 2020;9(5):1545. doi: 10.3390/jcm9051545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petrescu A-M, Taussig D, Bouilleret V. Electroencephalogram (EEG) in COVID-19: a systematic retrospective study. Neurophysiol Clin. 2020;50(3):155-165. doi: 10.1016/j.neucli.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pilato MS, Urban A, Alkawadri R, et al. EEG Findings in coronavirus disease. J Clin Neurophysiol. Published online July 1, 2020. Online ahead of print. doi: 10.1097/WNP.0000000000000752 [DOI] [PubMed] [Google Scholar]
- 27.Scullen T, Keen J, Mathkour M, Dumont AS, Kahn L.Coronavirus 2019 (COVID-19)-associated encephalopathies and cerebrovascular disease: the New Orleans experience. World Neurosurg. 2020;141:e437-e446. doi: 10.1016/j.wneu.2020.05.192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pasini E, Bisulli F, Volpi L, et al. EEG Findings in COVID-19 related encephalopathy. Clin Neurophysiol. 2020;131(9):2265-2267. doi: 10.1016/j.clinph.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skorin I, Carrillo R, Perez CP, et al. EEG Findings and clinical prognostic factors associated with mortality in a prospective cohort of inpatients with COVID-19. Seizure. 2020;83:1-4. doi: 10.1016/j.seizure.2020.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Canham LJW, Staniaszek LE, Mortimer AM, Nouri LF, Kane NM. Electroencephalographic (EEG) features of encephalopathy in the setting of Covid-19: a case series. Clin Neurophysiol Pract. 2020;5:199-205. doi: 10.1016/j.cnp.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koutroumanidis M, Gratwicke J, Sharma S, Whelan A, Tan SV, Glover G. Alpha coma EEG pattern in patients with severe COVID-19 related encephalopathy. Clin Neurophysiol. 2021;132:218-225. doi: 10.1016/j.clinph.2020.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kubota T, Prasannakumar KG, Naoto K. Meta-analysis of EEG findings in patients with COVID-19. Epilepsy Behav. 2021;115:107682. 10.1016/j.yebeh.2020.107682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gelisse P, Rossetti AO, Genton P, Crespel A, Kaplan PW. How to carry out and interpret EEG recordings in COVID-19 patients in ICU? Clin Neurophysiol. 2020;131:2023-2031. doi: 10.1016/j.clinph.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsetsou S, Novy J, Oddo M, Rossetti AO. EEG Reactivity to pain in comatose patients: importance of the stimulus type. Resuscitation. 2015;97:34-37. doi: 10.1016/j.resuscitation.2015.09.380 [DOI] [PubMed] [Google Scholar]
- 35.Hirsch LJ, LaRoche SM, Gaspard N, et al. American Clinical Neurophysiology Society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30(1):1-27. doi: 10.1097/WNP.0b013e3182784729 [DOI] [PubMed] [Google Scholar]
- 36.Leitinger M, Beniczky S, Rohracher A, et al. Salzburg consensus criteria for non-convulsive status epilepticus—approach to clinical application. Epilepsy Behav. 2015;49:158-163. doi: 10.1016/j.yebeh.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 37.Tjepkema-Cloostermans MC, Hofmeijer J, Hom HW, Bosch FH, van Putten MJAM. Predicting outcome in postanoxic coma: are ten EEG electrodes enough? J Clin Neurophysiol. 2017;34(3):207-212. doi: 10.1097/WNP.0000000000000337 [DOI] [PubMed] [Google Scholar]
- 38.Synek VM. The low-voltage electroencephalogram. Clin Electroencephalogr. 1983 Apr;14(2):102-105. [DOI] [PubMed] [Google Scholar]
- 39.Schomer DL, Lopes da Silva FH. Niedermeyer’s Electroencephalography: Basic Principles, Clinical Applications, and Related Fields. Edición: 7. OUP USA; 2018.
- 40.Sutter R, Kaplan PW. Clinical and electroencephalographic correlates of acute encephalopathy. J Clin Neurophysiol. 2013;30(5):443-453. doi: 10.1097/WNP.0b013e3182a73bc2 [DOI] [PubMed] [Google Scholar]
- 41.Amodio P, Marchetti P, Del Piccolo F, et al. Spectral versus visual EEG analysis in mild hepatic encephalopathy. Clin Neurophysiol. 1999;110(8):1334-1344. doi: 10.1016/S1388-2457(99)00076-0 [DOI] [PubMed] [Google Scholar]
- 42.Kaplan PW. The EEG in metabolic encephalopathy and coma. J Clin Neurophysiol. 2004;21(5):307-318. [PubMed] [Google Scholar]
- 43.Ebersole John S, Husain AM, Nordli DR., Jr.Current Practice of Clinical Electroencephalography Fourth Edition. LWW; 2014. [Google Scholar]
- 44.Kaplan PW, Rossetti AO. EEG Patterns and imaging correlations in encephalopathy: encephalopathy part II. J Clin Neurophysiol. 2011;28(3):233-251. doi: 10.1097/WNP.0b013e31821c33a0 [DOI] [PubMed] [Google Scholar]
- 45.Juan E, Kaplan PW, Oddo M, Rossetti AO. EEG As an indicator of cerebral functioning in postanoxic coma. J Clin Neurophysiol. 2015;32(6):465-471. doi: 10.1097/WNP.0000000000000199 [DOI] [PubMed] [Google Scholar]
- 46.Antony AR, Haneef Z. Systematic review of EEG findings in 617 patients diagnosed with COVID-19. Seizure. 2020;83:234-241. doi: 10.1016/j.seizure.2020.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Toledano M, Davies NWS. Infectious encephalitis: mimics and chameleons. Pract Neurol. 2019;19(3):225-237. doi: 10.1136/practneurol-2018-002114 [DOI] [PubMed] [Google Scholar]
- 48.Laxenaire-Aug MC, Laxenaire M, Collombier N, Weber M, Saunier C. Modifications de l’électroencéphalographie au cours de l’insuffisance respiratoire aiguë des pulmonaires chroniques. RES. 1970;27(4):345-362. doi: 10.1159/000192692 [DOI] [PubMed] [Google Scholar]
- 49.Nuwer MR. Alpha coma in COVID encephalopathy. Clin Neurophysiol. 2021;132:202-203. doi: 10.1016/j.clinph.2020.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Iacobone E, Bailly-Salin J, Polito A, Friedman D, Stevens RD, Sharshar T. Sepsis-associated encephalopathy and its differential diagnosis. Crit Care Med. 2009;37(10 Suppl):S331-S336. doi: 10.1097/CCM.0b013e3181b6ed58 [DOI] [PubMed] [Google Scholar]