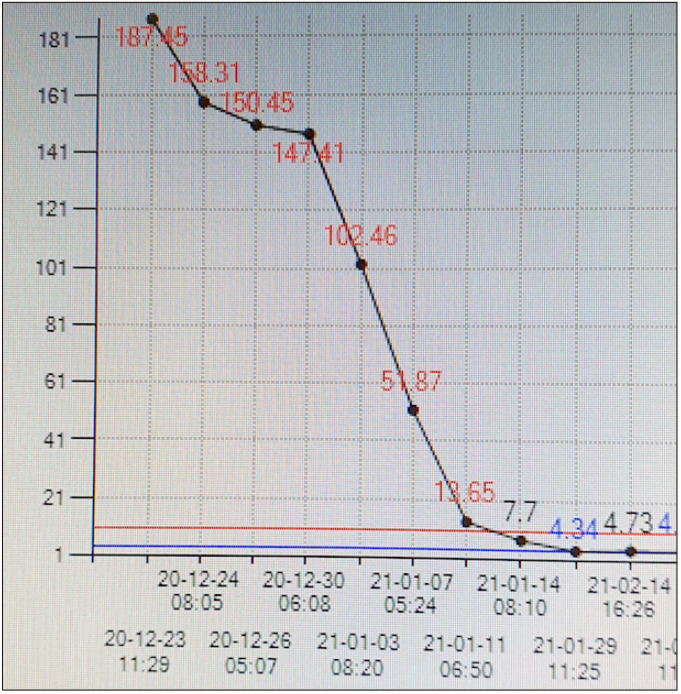
TO THE EDITOR: A 62-year-old-lady visited the emergency room for diarrhea followed by fever in December 2020 when she had leukocytosis (187,400/mL with 72% neutrophils) and pneumonia predominantly at the lower lobes (Fig. 1). She looked relatively well with no respiratory distress in WHO performance score of I, but febrile up to 39.0°C. Pallor, jaundice, lymphadenopathy, and bleeding tendency were absent. Heart rate was rapid and regular without murmurs. Crackles were heard on the lung bases. The abdomen was scaphoid with a palpable spleen. The remainder of the physical exam was unremarkable. A diagnosis of chronic myeloid leukemia (CML) in the chronic phase was immediately made using peripheral blood polymerase chain reaction (PCR) for the BCR-ABL fusion gene and later by marrow study. Pneumonia was confirmed to be coronavirus disease 2019 (COVID-19) by reverse transcription (RT)-PCR of a nasopharyngeal swab for severe acute respiratory syndrome coronavirus 2 ribonucleic acid (SARS CoV-2 RNA). Her fever ranged from 38.1 to 39.0°C, lasted for 3 days, and disappeared right after starting remdesivir. Following remdesivir treatment at 100 mg for five consecutive days, imatinib was started at 600 mg daily, higher than the usual dose, for the risk of leukostatic hemorrhage. The drug was continued and reduced to 400 mg QD on the 13th day as leukocyte count returned to normal (Fig. 2). She tolerated imatinib very well and the drug did not deteriorate the clinical course of COVID-19. She was COVID-19 positive via RT-PCR for 6 weeks and became negative when her pneumonia resolved. Pneumonia was completely gone after two and a half months (Fig. 1).
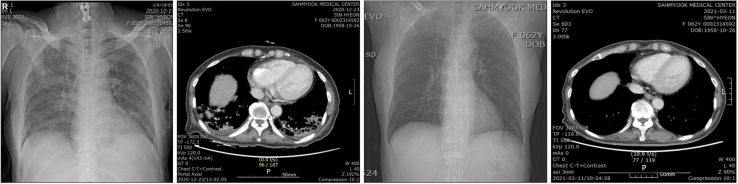
Fig. 1.
Pneumonia shown on chest radiograph and CT scan taken day 1 was completely gone on radiograph and CT scan taken day 78.
Fig. 2.
Leukocytosis was gone after starting imatinib.
There has been concern about the susceptibility for contracting SARS CoV-2 and unfavorable impact on the clinical course of COVID-19 among cancer patients. The International CML Foundation collected 110 cases of COVID-19 with concurrent CML from the global network in March–July 2020 [1] and reported the clinical outcomes including incidence, severity, and mortality. Their data showed that older age, COVID-19 severity, and imatinib treatment predicts mortality. They attributed the absence of imatinib’s theoretical advantage to compounding factors caused by the inhomogeneous population of their study. Contrary to the negative impact of imatinib on survival in their report [1], Italian data suggested that imatinib possibly protects from COVID-19 in Philadelphia+ acute lymphoblastic leukemia [2] and CML [3]. This supports the in vitro inhibiting activity of imatinib against SARS-CoV and Middle Eastern Respiratory Syndrome -CoV [4], as well as low infection/replication rate of torquetenovirus and upregulation of anti-viral genes after tyrosine kinase inhibitor (TKI) exposure [5]. The prevalence of COVID-19 among CML patients appeared similar to the normal population [6].
In COVID-19, concurrent with newly diagnosed CML, delayed introduction of TKI therapy is not recommended [7]. This is based on the the European Hematology Association Scientific Working Group meeting’s conclusion on 29 March 2020 that uncontrolled leukocytosis may worsen lung damage and aggravate gas exchange in cases of severe COVID-19. Delayed TKI introduction may also increase the risk of CML progression to advanced phases. An extreme caution should be practiced during the first three months of TKI treatment for the risk of severe cytopenia, aggravating the clinical course of COVID-19 in case of severe disease. Two of five cases of COVID-19 among already known CML patients in Turkey were continuously placed on imatinib with no deterioration of COVID-19 [8]. Our case aptly demonstrates that TKI could be safely used if COVID-19 is not severe and TKI induced leukopenia can be closely monitored.
Footnotes
Authors’ Disclosures of Potential Conflicts of Interest
No potential conflicts of interest relevant to this article were reported.
REFERENCES
- 1.Rea D, Mauro MJ, Cortes JE, et al. COVID-19 in patients (pts) with chronic myeloid leukemia (CML): results from the International CML Foundation (iCMLf) CML and COVID-19 (CANDID) study. Blood (ASH Annual Meeting Abstracts) 2020;136(Suppl):46–7. doi: 10.1182/blood-2020-140161. [DOI] [Google Scholar]
- 2.Foà R, Bonifacio M, Chiaretti S, et al. Philadelphia-positive acute lymphoblastic leukaemia (ALL) in Italy during the COVID-19 pandemic: a Campus ALL study. Br J Haematol. 2020;190:e3–5. doi: 10.1111/bjh.16758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breccia M, Abruzzese E, Bocchia M, et al. Chronic myeloid leukemia management at the time of the COVID-19 pandemic in Italy. A campus CML survey. Leukemia. 2020;34:2260–1. doi: 10.1038/s41375-020-0904-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman CM, Sisk JM, Mingo RM, Nelson EA, White JM, Frieman MB. Abelson kinase inhibitors are potent inhibitors of severe acute respiratory syndrome coronavirus and Middle East respiratory syndrome coronavirus fusion. J Virol. 2016;90:8924–33. doi: 10.1128/JVI.01429-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galimberti S, Petrini M, Baratè C, et al. Tyrosine kinase inhibitors play an antiviral action in patients affected by chronic myeloid leukemia: a possible model supporting their use in the fight against SARS-CoV-2. Front Oncol. 2020;10:1428. doi: 10.3389/fonc.2020.01428.008940af48964fb69bb44c865433b1e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ector GICG, Huijskens EGW, Blijlevens NMA, Westerweel PE. Prevalence of COVID-19 diagnosis in Dutch CML patients during the 2020 SARS-CoV2 pandemic. A prospective cohort study. Leukemia. 2020;34:2533–5. doi: 10.1038/s41375-020-0964-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.EHA Scientific Working Group, author. CML, TKI treatment and COVID-19 disease. iCMLf; Bexhill, UK: 2020. [Accessed November 18, 2021]. https://www.cml-foundation.org/news-icmlf-mobile/1452-cml-tki-treatment-and-covid-19-disease.html. [Google Scholar]
- 8.Yılmaz U, Pekmezci A, Gül Y, Eşkazan AE. COVID-19 in chronic-phase chronic myeloid leukemia patients: a single-center survey from Turkey. Turk J Haematol. 2021;38:79–81. doi: 10.4274/tjh.galenos.2020.2020.0472. [DOI] [PMC free article] [PubMed] [Google Scholar]