Abstract
Background: Although illegal in most countries, cannabis remains the most common illicit drug in Switzerland and worldwide. While there is growing evidence on adverse effects of cannabis use, most users do not report any problems or negative consequences. In the face of a sustained high prevalence of cannabis use and the recent legalization waves in different parts of the world, it is important to know how cannabis is perceived in the general population and how current users regulate their own use. The present study aims to investigate users’ and non-users’ attitudes towards cannabis regulations and towards current users. Additionally, self-rated health measures as well as protective behavioral strategies and other cannabis related variables were assessed.
Design and methods: We collected data from 380 current users and 659 non-users who were recruited by invitation letter or online media platforms. The data was analyzed using basic descriptive statistical procedures.
Results: Results revealed that both groups favor moderate cannabis regulation measures over prohibition and no regulation at all. On average, they report the same subjective health. Protective strategies are often used and are associated with better health and lower severity of dependence in cannabis users.
Conclusions: Taken together, results indicate that safe use of cannabis is possible for most users, while there is a group of users at risk of 15-20%, which may benefit from control by regulatory measures.
Significance for public health.
In the face of recent legalization waves in different parts of the world and the current public discourse on a possible legalization in Switzerland, it is important to know how cannabis is perceived in the general population and how current users regulate their own use. The manuscript contributes to the literature by showing that in Switzerland, users and non-users prefer a moderate regulation of cannabis over prohibition. Further, support is shown for recent findings that highlight the protective effect of behavioral strategies (measured by the Protective Behavioral Strategies for Marijuana, Pedersen et al.1) on adverse effects of marijuana, such as perceived dependence.
Key words: Cannabis use, attitudes, regulation, health, Switzerland
Introduction
Cannabis is produced in almost all countries across the world. In 2017, approximately 2.8% of the global population between 15 and 64 years old (188 million people) consumed the plant-based drug at least once in their life. Since 2007, these numbers remained relatively consistent.2 The use of cannabis is also widespread in Switzerland. More than one third of the population has tried cannabis at least once in their life,3 and 7.6 % of men and 3.4 % of women use cannabis regularly (within the past six months). According to Marmet and Gmel,4 20.8% of all regular users show problematic cannabis use. This proportion is considerable higher in men (26.2%) compared to women (8.7%).
Most countries prohibit the production, use, and distribution of recreational cannabis. However, the legal framework for cannabis regulation is changing worldwide. In the Netherlands cannabis has been quasi-legalized through the introduction of “coffeeshops”, which are licensed cannabis sale outlets. In the USA, various states such as Alaska, Colorado, Oregon and Washington legalized cannabis for personal use. Retail and production systems were introduced in Uruguay in 2014 and in Canada in 2018. Alternatives to prohibition vary from decriminalization to regulation and legalization.5
Despite scientific, economic and political considerations, policy makers need to be informed about the attitudes towards legalization in the general population. Research shows that there is a significant difference between cannabis users and non-users in their attitudes towards cannabis policies. Skretting6 showed in Norway that only 65% of cannabis users were in favor of prohibition of cannabis compared to 95% of non-users. Another study in Huston (USA) found users and non-users to exhibit different attitudes toward drug policies: 68% of drug users were in favor of legalizing cannabis, while only 33% of the non-users showed approval.7 In 2008, only 7% of cannabis users in the Netherlands were in favor of cannabis prohibition, compared to 50% of nonusers. 8 In fact, by consuming cannabis, users may learn about potential harmful effects, which may alter their attitudes towards legalization.9 A representative telephone survey conducted by Umbricht10 showed that the majority of the Swiss population would support the legalization of cannabis, with a new regulatory model for medical and recreational use.
Williams et al.11 discovered a causal connection between user status and opinions on cannabis policy. They analyzed Australian data from cross-sectional surveys over the period 1993-2007 and used a quasi-panel approach to account for potential endogeneity of cannabis use. Their analysis showed that former users leaned towards legalization more than never-users, which is consistent with information on net benefits of cannabis use. Their positive experiences with cannabis shaped former users’ thinking about legalization. In current users instead, they argued self-interest may confound with past cannabis use experiences, making it unclear to what degree both factors influence their attitudes towards legalization. Another study from the Netherlands concluded that personal experience with cannabis use had a causal effect on the support for more liberal policies. Current users and those who used cannabis in the past were more favorable to legalization compared to neverusers. 12
Already in the 19th century, cannabinoids were used to treat different health problems ranging from chronic pain, spasticity to nausea.13 The high potency of cannabis in alleviating these symptoms accounts for its medical use.14Worldwide and in Switzerland, the main indication for medical use of cannabis is chronic pain.15 Two well-studied active agents found in Cannabis are mainly responsible for its properties - THC and CBD. Only cannabis with a THC-content higher than 1% is controlled by the Swiss narcotics legalization. Products rich in CBD and low in THC have been legally sold as tobacco substitutes since 2018. Their consumption has recently become increasingly popular for both therapeutic and recreational purposes.16 The use of cannabis has important implications for public health.17A variety of health, social and academic problems is associated with excessive use.18-20 Indeed, cannabis use has adverse effects on physical as well as mental health and negatively affects important life outcomes such as educational attainment and labor market position.21-25 Moreover, cannabis use has been associated with different health problems, such as psychotic episodes, injury risk and dependence.26-28 Dependence syndrome was found to be one of the most common health problems caused by frequent cannabis use,29 which is, in turn, linked to a many other health conditions, such as externalizing disorders.30
Until today, a variety of instruments has been proposed to measure and screen for cannabis dependence. Among others, the Severity of Dependence Scale (SDS) is a short and valuable tool composed of five items to assess psychological (without addressing tolerance and withdrawal) components of dependence to any kind of drug.31 Steiner et al.32 adapted the SDS for cannabis users from the German general population, reporting high internal consistency and significant correlations with the DSM-IV diagnosis and frequency of use. Consuming cannabis is not equally harmful to every user.9 Van Ours and Williams33 concluded from their literature review that no serious harmful health effects occur after moderate cannabis use, but that there is evidence of reduced mental well-being in heavy users who are susceptible to mental health problems. Given that the majority of the Swiss population favors a new regulatory model for cannabis use,10 increasing prevalence and the potential risks,4 it is imperative to determine the factors that support people in their self-management of cannabis use. Therefore, we need to understand how users deal with their cannabis use and its effects, how they regulate their own use and how they protect themselves from experiencing negative consequences. Pedersen et al.1 examined Protective Behavioral Strategies for Marijuana (PBSM) in US-college students. They refer to behaviors that can be employed before, during, after, or instead of using cannabis to limit heavy use and reduce the risk for negative consequences. In adolescents, young adults and veterans, the use of PBSM is significantly associated with less frequent cannabis use, experiencing fewer negative consequences and lower dependency rates.1,34-38 The more often such strategies are employed, the less likely it is that problematic aspects of cannabis use arise. PBSM represent an interesting mechanism for regulating one’s own cannabis use, for harm reduction and ultimately for preventive and therapeutic interventions. The present study aims to obtain information about current cannabis users and non-users from an urban population. Differences in attitudes towards cannabis regulation as well as non-users’ attitudes towards current users will be assessed. In a second part, self-rated health-measures will be compared in both groups. Additionally, the associations between health measures, protective strategies, severity of dependence and use frequency will be analyzed in the subgroup of occasional, moderate and heavy users. Our results will shed light on the current situation of regular cannabis use in an urban population both from the inside perspective of current users as well as from the outside perspective of non-users.
Design and methods
This article is based on an online survey that comprised existing questionnaires and self-developed items assessing a variety of variables connected to cannabis use.
Participants
A random sample of 6000 households in the inner city of Bern was contacted by a postal letter containing general information about the study, an anonymity statement and the web access to the online survey. By starting the online survey participants consented that their responses will be collected only for the purpose of this research project and that there will be no possibility to trace them back. The city administration provided us the addresses, which were deleted from our servers immediately after sending the letters. The survey was also distributed by online media and the website of the University of Bern between April and May 2019. The study was approved by the ethical board of the canton of Bern, Kantonale Ethikkomission für die Forschung (KEK-Nr: Req-2019-00253). A total of 1303 individuals engaged in the survey. After sorting out responses collected before the official start date (e.g., internal staff and journalists testing) and nonsensical cases (e.g., 100% missing values), the sample comprised 1266 cases. 762 individuals were recruited via postal letter, which corresponds to a response rate of 12.7%.
Dropout analysis
18% of the cases had incomplete data. A chi-square test of independence and Bonferroni adjusted post-hoc inspection of the corrected residuals were used to compare the frequency of completers and non-completers on important variables. Participants who had been contacted by online media were more likely to drop out, compared to those contacted by invitation letter (χ2 (2, n=1242) = 25.75, p<0.01). Adolescents 13-19-years-old were more likely to drop out compared to all other age groups (χ2 (6, n=1236) = 40.07, p<0.01). Results in this age group need to be interpreted with caution since more than one third (25 out of 63 cases) dropped out. Moreover, those who never used cannabis were more likely to drop out, whereas those who had used cannabis at least once in their life were more likely to complete the survey (χ2 (1) = 8.26, p<0.01). The chi-square was also significant for educational level, occupation, relationship status and past year use, but post-hoc group analysis showed no significant difference between completers and non-completers on the group level. Results were nonsignificant for gender, housing situation, income or cannabis use frequency. After excluding all non-completers, 1039 cases remained in the final analysis sample.
Measures
Seven self-developed items (depicted in the results section) assessed attitudes towards the regulation of cannabis use by asking “Please indicate how useful you consider the following suggestions”. Answers ranged from 1 = not useful at all to 4 = very useful. Additionally, non-users were asked “would you use cannabis if it was legal?” and current users were asked “would you use cannabis more often if it was legal?” and “would you prefer to use cannabis legally?” with the response options “yes” and “no”.
The following items are depicted in Appendix A1, A2 and A3. We were also interested in the attitudes that non-users have towards current cannabis users: Nine of the 36 items of the protective behavioral strategies (PBSM) scale were presented to nonusers (e.g., “use marijuana only among trusted peers” or “buy less marijuana at a time so you smoke less”). They were asked how much they think, users adhere to those strategies to regulate their own use of cannabis (from 1 = “don’t agree at all” to 4 = “totally agree”). Furthermore, nine items assessing negative consequences of cannabis use were presented to non-users (e.g., “They have more problems with their partners or other relatives” or “They do lower quality work than non-users”). They were asked how much they agree that cannabis users experience these consequences (1 = “don’t agree at all” to 4 = “totally agree”). Finally, 11 items that assess general self-regulation-skills (e.g., “They can work successfully towards long-term goals”) were given to non-users. They were asked how much they think these skills apply to cannabis users (1 = “don’t agree at all” to 4 = “totally agree”). For each of the three sets of items a mean was calculated.
Subjective general health was assessed following the item structure in the SF-12.39 We used the item “How would you describe your general health?” (from 1 = bad to 5 = excellent). Additionally, a health score was created based on the mean of four items: how often are you (1) “calm and at ease?”; (2) “vital and full of energy?”; (3) “discouraged or sad?” (reverse coding); (4) “confident, optimistic?” (from 1 = never to 6 = always).
Dependent cannabis use was assessed in current users using the severity of dependence scale SDS31, which captures psychological factors of dependence for different kinds of drugs. Its five items deal with the feeling of impaired control and concerns about one’s use. Its score ranges from 0 = never/almost never to 3 = always/almost always. Steiner et al.32 found the validity of this scale to be satisfying and reliable for the German general population Germany, proposing a cut-off of two for the general population and four for male cannabis users.
PBSM were assessed with the 36 item scale developed by Pedersen et al.37 Items ranged from 1 = never to 6 = always. They were translated by our project group and then back-translated by a native speaker. Discrepancies between original and back-translated items were discussed again and changed if necessary.
Procedure
The questions of the survey were programmed with the online application Qualtrics®. All analyses were run using IBM SPSS® Statistics Version 25.0.0.1.
To compare attitudes towards cannabis use regulation between users and non-users, we used seven independent t-tests with biascorrected and accelerated (BCa) bootstrap estimates. To correct for type I error accumulation, the standard alpha level of 0.05 was divided by seven and adjusted to 0.007; t-tests with BCa bootstraps were also used to compare general health and the health score between users and non-users. In the group of current users, we analyzed health variables, severity of dependence, behavioral strategies and cannabis use frequency. Since most of these variables are ordinal scaled, we present the mean, median, standard deviation, range and Spearman’s non-parametric correlation coefficient rs to describe these results. We also calculated the BCa bootstrapped confidence intervals.
Missing values
Patterns of missing values were analyzed for users and nonusers separately. Since we excluded participants who didn’t finish the survey, all missing values represented participant skipping single items or item lists. Among users 0.76 % of all data points were missing with a maximum of 2.4 % on single variables. Little’s Test for the assumption of missing completely at random (MCAR) was not significant χ2 (1173, n=380) = 1190.729, p=0.353, indicating that missing values were independent of observed and unobserved variables.40 Among non-users 1.64 % of the data was missing with a maximum of 3.6 on single variables. Little’s test was not significant, χ2 (1498, n=659) = 1578.13, p=0.07. Multiple imputations and subsequent pooling were performed using the SPSS 25.0.0.1 default workflow both for the users and the non-users data separately. All analyses were then conducted with a combined dataset containing users and non-users information data.
Sample description
The sample was drawn from the inner city population of Bern, since most suburbs are separate municipalities, which were not included. Age ranged from 15 to 81 (M = 39.12, SD = 14.34). 53.5% were male, 45.2% were female and 0.7% identified themselves as diverse. A majority of 68.8% finished higher education (higher college or university), whereas 23.2% finished apprenticeship, 7.1% finished school and 0.9% had no degree. Nearly two third, 62.5%, were employees and 16% were in education. The average household income was between 0 and 50’000 CHF for 26.4%, between 50’000 and 100’000 CHF for 40.8% and above 100’000 CHF for 32.8% of the sample. A big majority, 83.3%, had used cannabis at least once in their lives and 45.7% during the past year. There was a strong age effect, χ2(6) = 144.91, p<0.001, with adolescents and young adults reporting significantly higher rates in past-year use (78.9% and 66.3%) than 50-59 year olds (28.5%) and 60-69 year old (11.5%). On average, 36.6% had used cannabis at least once a month during the last year. They are referred to as current cannabis users in this article. All others are called non-users.
Current cannabis users
The sub-sample of current users comprised 380 participants. They were on average 32.56 years old (SD = 11.93). They were more likely male than female, χ2 (1) = 55.17, p<0.001, with 2.74 times higher odds of being a male current user. They used cannabis occasionally (approx. once a month) in 21.3% of the cases, moderately (approx. 1-4 times per week) in 34.2% of the cases and heavily (5-7 times per week) in 44.5% of the cases. Women were more likely to show occasional or heavy use and less likely to show moderate use of cannabis compared to men, χ2 (2) = 7.83, p=0.02. There was a significant effect of age on cannabis use frequency, F(2, 377) = 8.5, p<0.001, with heavy users being significantly older than occasional and moderate users.
Non-users
The sub-sample of non-users comprised 659 participants. They were on average 10.37 years older (M = 42.91, SD = 14.25) than users, t(905.74) = 12.5, p<0.001. The odds ratio for non-users being female compared to male was 2.74 higher.
Results
Attitudes towards cannabis use regulation between current users and non-users
Figure 1 shows attitudes towards cannabis regulation, means and adjusted standard errors for users, non-users and the total scores. Independent t-tests based on a Bonferroni-adjusted alpha level of 0.007 and BCa-Bootstraps revealed significant differences between users and non-users (Mdiff 0.26 to 0.37, p=0.001). Only “Controlled sale in specialized shops with trained staff” with a mean difference of 0.057 (t(827.1) = 1.17, p=0.24, BCa 99% CI [0.056, 0.058]) was non-significant. However, visual inspection of the bar chart reveals major differences between the items, independently of user status: “General prohibition” (M = 1.35, [1.3, 1.39]), “No regulation” (M = 1.83, [1.78, 1.88]) and “Buying only with official approval” (M = 2.04, [1.99, 2.09]) were seen as “not at all useful” or only “a little useful” to regulate the use of cannabis. “Quantity restriction” was seen as M = 2.7, [2.64, 2.75] “a little useful” by most participants. However, there is a pronounced gap to “Controlled sale in specialized shops with trained staff” (M = 3.34, [3.29, 3.39]), “Ban on advertisement” (M = 3.36, [3.3, 3.42]) and “Age restriction” (M = 3.48, [3.43, 3.52]), which were seen by both groups as “rather useful” or “very useful”. Note that current users scored significantly higher on “Age restriction” than non-users (Mdiff = 0.260, BCa 99% CI [0.259, 0.261], t(973.4) = 5.75, p<0.001). We also asked participants if they would change their behavior if the use of cannabis were legal. 22.6% of non-users said they would use cannabis if it were legal and 77.4% said they would not do so. Among current users, 9.5% said they would use cannabis more often if it were legal and 90.5% said they would not. If asked, if they would prefer to use cannabis legally, 94.2% of current users said yes and 5.8% said no.
What do non-users think about current users?
The following results show what non-users, on average, thought about current users’ employment of behavioral strategies, self-regulation skills as well as the negative consequences they may face. Each set of items was rated from 1 = “don’t agree at all” to 4 = “totally agree”: for the use of strategies, results show a mean of 2.08 (SD = 0.56) with a BCa 95% CI from 2.04 to 2.12. This suggests that non-users tend to disagree that users adopt protective strategies to regulate their cannabis consumption. They neither agree nor disagree that current users experience negative consequences from using cannabis, M = 2.38, SD = 0.64; [2.33, 2.43]. Note, that “they later turn to harder drugs” was the consequence where non-users disagreed the most (M = 1.78, SD = 0.84; [1.71, 1.84]). For self-regulation skills, results were M = 2.48, SD = 0.57; [2.44, 2.52], suggesting that non-users neither agree nor disagree that current users have lower general self-regulation skills.
Self-rated health status
The mean of the general health item was M = 3.74, SD = 0.82; BCa 95 % CI [3.66, 3.82] in users and M = 3.72, SD = 0.81; [3.66, 3.78] in non-users. The mean-difference of 0.02, [-0.08, 0.13] was not significant. The mean of the health-score (mean average from: feeling, relaxed, alive, depressed, confident) was M = 4.40, SD = 0.59; [4.34, 4.46] in users and M = 4.38, SD = 0.66; [4.33, 4.43] in non-users. The mean-difference of 0.02, [-0.06, 0.10] was also not significant. Overall, there was no difference between users and non-users on the self-rated health measures, which were used in this study.
Current cannabis users’ health, dependence and strategies
In Table 1 we present descriptive results, which were measured in current users, but not in non-users.
Self-rated general health was negatively associated with the severity of dependence, rs = -0.28 BCa 95% CI [-0.38, -0.18] and cannabis use frequency, rs = -0.27 [-0.37, -0.16], and positively associated with the PBSM-Score, rs = 0.18, [0.06,0.28] (all ps <0.001). The health score was negatively associated with the severity of dependence, rs = -033 [-0.43, -0.24], p<0.001 and cannabis use frequency, rs = -0.14 [-0.24, -0.03], p=0.007. It was positively associated with the PBSM-Score, rs = 0.16 [0.06, 0.25], p=0.002. This indicates that participants who use cannabis more often and who experience impaired control and concerns about their use-behavior, rate their health significantly lower than other current users. The use of protective strategies seemed to be associated with better self-rated health. The PBSM-Score correlated negatively with the severity of dependence, rs = -.038 [-0.47, -0.27], and cannabis use frequency, rs = -0.46 [-0.54, -0.37] (both ps <0.001), suggesting that the more users adopted protective strategies, the less frequently they consumed cannabis and the fewer symptoms of dependence they experienced. Severity of dependence had a strong positive association with use frequency, rs=0.54 [0.46, 0.61], p<0.001, indicating that symptoms of dependence aggravated with increasing cannabis use. As presented in Table 2, current users had a SDS mean score of 2.39 (SD 2.56); 32.6% scored zero on the SDS; 27.3% scored 1-2 and 22.3% scored 3-4; 11.7% scored 5-6, 3.2% scored 7-8, 1.3% scored 9-10 and 1.6% scored 11-12 on the SDS. No participant scored above 12. Among heavy users, 34.5% had SDS sum scores of five or higher compared to 5.5% among moderate users and 2.4% among occasional users. Figure 2 shows the scatterplot of the SDS and PBSM values grouped by use frequency. There were almost no occasional users above SDS = 3. Furthermore, visible inspection suggests that the moderate correlation between SDS and PBSM (Table 1) is mostly based on values of SDS <5. With and above five the relationship is less evident. To investigate this, we split the subsample and compared the correlation coefficients between the two groups. Current users with a SDS <5 had a correlation between SDS and PBSM of r (n=311) = -0.20, p<0.001. Those with a SDS >=5 had a correlation of r (n=69) = -0.22, which was not significant, p=0.07. These findings may indicate a weak but stable relationship between PBSM and SDS up to a SDS mean score of four. Values above four mostly belong to heavy users for which the linear relationship between dependence and the use PBSM appears to be weakened.
Figure 1.
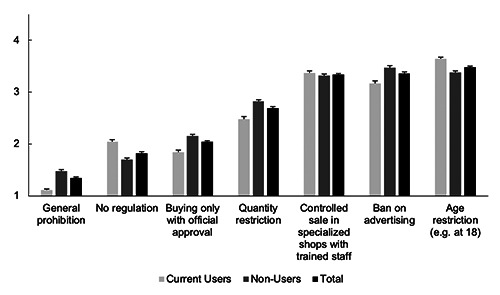
Attitudes on possible cannabis use regulations between current users and non-users. Participants were asked “Please indicate how useful you consider the following suggestions to regulate cannabis use”. 1 = not useful at all, 2 = only little useful, 3 = rather useful, 4 = very useful. The error-bars represent standard errors.
Table 1.
Descriptive statistics and Spearman correlations between health measures and cannabis use variables among current cannabis users (n=380).
| 1 | 2 | 3 | 4 | 5 | Median | Mean | SD | Range | |
|---|---|---|---|---|---|---|---|---|---|
| 1. General health | 1 | 4 | 3.74 | 0.82 | 1 – 5 | ||||
| 2. Health Score | 0.40** | 1 | 4.5 | 4.40 | 0.59 | 1 – 6 | |||
| 3. PBSM | 0.18** | 0.16* | 1 | 4.17 | 4.08 | 0.83 | 1 – 6 | ||
| 4. SDS | -0.28** | -0.33** | -0.38** | 1 | 2 | 2.39 | 2.56 | 0-12 | |
| 5. Use Frequency | -0.27** | -0.14* | -0.46** | 0.54** | 1 | 2 | 2.23 | 0.78 | 1-3 |
PBSM, protective behavioral strategies for marijuana; SDS, severity of dependence scale; use frequency categories: 1 = occasional, 2 = moderate, 3 = heavy; *p<0.01, **p<0.001.
Discussion
In this study, current cannabis users and non-users from the general population were compared in regard to socio-demographic variables, health related measures, and attitudes towards cannabis use, self-regulation as well as policies. Additionally, attitudes of non-users towards current users’ self-regulation, negative consequences of use and use-strategies were assessed. Following variables were analyzed more closely in the group of current users: health, use-strategies and severity of dependence.
Figure 2.
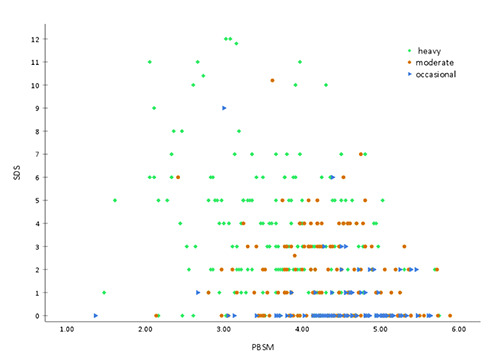
Scatterplot of SDS and PBSM values grouped by use frequency. The scatterplot shows the relationship between PBSM and SDS for heavy (green, 5-7x/week), moderate (orange, 1-4x/week), and occasional (blue, 1x/month) users of cannabis.
Table 2.
Distribution of SDS mean scores by use frequency.
| 0 | 1-2 | 3-4 | 5-6 | 7-8 | 9-10 | 11-12 | SDS mean score | n | |
|---|---|---|---|---|---|---|---|---|---|
| Frequency | |||||||||
| Occasional | 71.6% | 22.2% | 3.7% | 1.2% | 0.0% | 1.2% | 0.0% | 0.60 | 81 |
| Moderate | 34.4% | 32.8% | 27.3% | 4.7% | 0.8% | 0.0% | 0.0% | 1.81 | 128 |
| Heavy | 12.5% | 25.6% | 27.4% | 22.0% | 6.5% | 2.4% | 3.6% | 3.70 | 16 |
| Total | 32.6% | 27.3% | 22.3% | 11.7% | 3.2% | 1.3% | 1.6% | 2.39 | 377 |
SDS, severity of dependence scale; the numbers in the cells represent percentages, the SDS mean score and the count (n) within the respective use frequency group; there was no value above SDS=12.
Current users were more likely to be male than female and were on average 32 years old. This corresponds to representative findings for past 6-month use in Switzerland.4 However, the fact that more than one third were current users, the high number of heavy users and the relatively high proportion of women among users were surprising findings. Moreover, more than two out of five participants were past year users and more than four out of five were lifetime users, suggesting that individuals with prior cannabis use were more motivated to participate to the study. The sample was drawn from the inner city population of Bern, where – like in other urban areas – the prevalence of cannabis use is above average.3,41 However, it remains unclear to what degree the sample represents the population, as it may have been distorted by response bias. The large proportion of older participants who were heavy users was also surprising, since recent studies generally found adolescents and young adults to display the most frequent cannabis use.4,41 As we found that younger participants were more likely to terminate our survey prematurely, this might have increased the percentage of older heavy users artificially. However, given that older users usually show significantly lower use frequency, it is unlikely that dropouts of younger users account for this discrepancy, rendering response bias more plausible.
Attitudes on possible measures to regulate cannabis use differed between current users and non-users. Non-users were significantly more in favor of a general prohibition, sale only with official approval, quantity restriction and banning advertisement for cannabis products. These findings are consistent with existing findings about cannabis policies being most rejected by those who they affect most.6,8,42 Nonetheless, according to the theory of rational addiction, it remains unclear whether the reported attitudes of current users were driven by self-interest or the experience of genuine benefits and low perceived harm.1. In addition, most nonusers in our sample had experience with cannabis. Thus, their responses might have been influenced either by positive experiences leading to favoring legal cannabis use and soft regulatory measures or by negative experiences and regret, leading to opposition of legal cannabis use and a desire for strict regulation. Palali and van Ours12 previously demonstrated that former users’ support for legalization was causally related to positive experiences during their past use. Our groups shared positive attitudes towards cannabis being sold in specialized shops with trained staff. Interestingly, current users were even more in favor of an age restriction than non-users. This indicates that current users are aware of the harmful effects of cannabis (e.g., overdosing, early onset), which may be attributed to direct or peer experience. They agree on the need for some sort of regulation that is not too restrictive. Close inspection of our results revealed that all between group-differences were very small compared to within-group differences between items. Both, current users and non-users clearly preferred moderate regulatory measures like specialized shops, banning advertisement and age restriction over a general prohibition (the situation right now) or no regulation at all.
We analyzed non-users’ attitudes towards current users. As presented in the results section, attitudes towards current users’ self-regulation skills and negative consequences were neutral. One item (“they later turn to harder drugs”) was rated markedly lower than all other negative consequences. This item touches on the debate about the gateway hypothesis which is debated since decades on the societal as well as on the scientific level (see Arnold and Sade43 for a recent comment on the debate). Non-users that were presented with the nine selected items from the 36-item list rather disagreed that users employ PBSM to actively regulate their cannabis use. In contrast, the majority of current users reported adopting these nine selected strategies occasionally to sometimes.
Overall, it is worth noting that despite expected differences between users and non-users, they have quite similar views on possible future regulatory measures. This suggests that current users have a nuanced view on the benefits and risks of cannabis use, which is most likely based on direct and/or peer experience. Nonusers have a similar, but slightly more restrictive view on the topic. Nevertheless, it must be taken into account that the non-user group comprised a majority of former users and that the sample was drawn from an inner-city population. Even though non-users neither agreed nor disagreed on users having low self-regulation skills or experiencing negative consequences, they tended to disagree on current users actively managing their cannabis use by using PBSM. It remains unclear whether non-users think that users do not need protective strategies or that they are not able to follow them. However, users’ and non-users’ attitudes towards cannabis are far from polarized. On the contrary, they reveal similar patterns of judgement on risks, the need for legal regulations and individual abilities for self-regulation.
The majority of both, current users and non-users rated their subjective general health as good or very good. There was no significant difference between the groups. The same was the case for the health score consisting of four additional items. However, among current users we found small but significant correlations between use frequency and both health measures. The more often cannabis was used, the lower users rated their health. Similarly, use frequency was strongly associated with the severity of dependence. Taken together, these findings indicate that subjective health is not affected by monthly use of cannabis. It is rather heavy cannabis consumption that is associated with lower subjective health and increased dependence symptoms.
According to Figure 2, most current users show little or no signs of dependence, as less than a fifth scored five or more on the SDS. In comparison, Steiner et al.32 found a cut-off of two for a representative sample, Swift et al.44 found one of three for longterm weekly users, and Van der Pol, Liebregts et al.45 found one of four for young adult frequent users. Still, a standard cut off value for the SDS does not exist and needs to be defined for different samples as pinpointed by Steiner et al.32 Van der Pol et al.45 even suggest to not use the SDS to differentiate between dependent and non-dependent users. In this study we recruited from an urban population including high amounts of heavy users. After analyzing the SDS distribution within user subgroups and its correlations with PBSM and subjective health, we propose a seriously dependent user group of around 17% in our sample. In this group, protective strategies have lost their buffering effect on dependence symptoms. This group is probably smaller in the general population, since we recruited high rates of heavy users in this study compared to representative data.
PBSM can function as a protective factor, buffering risks and limiting heavy use and the development of addiction, as tested and discussed in several studies published in the past three years:37,46-48 consistently, PBSM have been shown to be associated with lower use frequency, negative consequences, and dependence and to mitigate known risk factors for heavy use. The present study is in line with these findings. On average, current users employed protective strategies between sometimes and most of the time. Their application of the strategies correlated significantly with SDS and cannabis use frequency. Our study extends the validity of these results by analyzing a sample drawn from the general urban population. Furthermore, we reveal a positive association between high self-rated health and frequent use of PBSM.
The subjective health level was equivalent in current users and non-users. It was independent of age, gender and social status. Current users were able to actively and consciously manage their cannabis intake using PBSM. On average, they used cannabis one to four times per week (moderate) and showed two signs of psychological dependence according to the SDS. Among current users there is a risk group of 15-20% who uses cannabis heavily, employs little PBSM, report lower health and has increased symptoms of dependence.
Limitations
Although the survey was widely distributed in the urban population of Bern and data from all social and age groups were obtained, our sample was not representative. Lifetime, current and heavy use were far above those found in epidemiological studies. However, we were successful in collecting a high number of current user information, which was crucial given the question we aimed to address. As inherent to voluntary survey studies,49 the current sample was likely influenced by non-response bias due to population characteristics. Strikingly, higher educated participants comprising almost 70 % of our sample. Bias due to survey characteristic was less clear. On one hand, current users may have been more motivated to participate if they perceived the survey as an opportunity to reflect on what is important to them. On the other hand, it is also possible that they refused to participate to avoid being confronted with their own (problematic) behavior. However, non-users were more likely to drop out than lifetime users, suggesting that the survey was generally more appealing to current or former users. Since we also recruited online, we do not know how many participants came from outside of Bern. However, there were mostly local online newspapers who reported on the survey.
Implications
The present study reveals that protective behavioral strategies are a common way of controlling one’s use of cannabis. The number of adopted strategies directly correlates with self-rated health and is negatively related to the severity of dependence. In addition to legal regulatory strategies, favored by current, past and nonusers, the importance of self-management could be emphasized in educational institutions. Prevention campaigns and specialized advice centers could promote the use of these strategies. Overall, our study clearly shows that most regular cannabis users already adopt such strategies. Self-determination is key to making safe use of cannabis possible. However, for a small group of users at risk for uncontrolled consumption, regulatory measures are required.
Acknowledgments
The authors thank Michèle Borgmann for her very helpful feedback on the online survey that clearly pushed the quality of the questionnaire.
Funding Statement
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Pedersen ER, Hummer JF, Rinker DV, et al. Measuring protective behavioral strategies for marijuana use among young adults. J Stud Alcohol Drugs 2016;77:441-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United Nations Office on Drugs and Crime. World Drug Report 2019. Available from: https://wdr.unodc.org/wdr2019/ [Google Scholar]
- 3.Sucht Schweiz, Gmel G, Kuendig H, et al. [Suchtmonitoring Schweiz - Konsum von Alkohol, Tabak und illegalen Drogen in der Schweiz im Jahr 2016].[Report in German]. Sucht Schweiz. 2017. Available from: https://www.suchtmonitoring.ch/docs/library/gmel_5lbj5rqv9y5i.pdf [Google Scholar]
- 4.Sucht Schweiz, Marmet S, Gmel G. Suchtmonitoring Schweiz - Themenheft zum problematischen Cannabiskonsum in der Schweiz im Jahr 2016].[Report in German]. Sucht Schweiz. 2016. Available from: https://www.suchtmonitoring.ch/docs/library/marmet_yzymdlgacrpp.pdf [Google Scholar]
- 5.European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2019: Trends and Developments. Publications Office of the European Union, Luxembourg; 2019. Available from: https://www.emcdda.europa.eu/system/files/publications/11364/20191724_TDAT19001ENN_PDF.pdf [Google Scholar]
- 6.Skretting A. Attitude of the Norwegian population to drug policy and drug-offences. Addiction 1993;88:125-31. [DOI] [PubMed] [Google Scholar]
- 7.Trevino RA, Richard AJ. Attitudes towards drug legalization among drug users. Am J Drug Alcohol Abuse 2002;28:91-108. [DOI] [PubMed] [Google Scholar]
- 8.van der Sar R, Brouwers EPM, van de Goor LAM, Garretsen HFL. The opinion on Dutch cannabis policy measures: A cross-sectional survey. Drugs Educ Prev Policy 2011;18:161-71. [Google Scholar]
- 9.Orphanides A, Zervos D. Rational addiction with learning and regret. J Polit Econ 1995;103:739-58. [Google Scholar]
- 10.Umbricht A. Telefonische Omnibus-Befragung zum Konsum und Handel von Cannabis. gfs-zürich, Markt- & Sozialforschung. 2017. Available from: https://fachverbandsucht.ch/download/427/Chartreport_Fachverband_Sucht_2017.pdf [Google Scholar]
- 11.Williams J, van Ours JC, Grossman M. Attitudes to legalizing cannabis use. Health Econ 2016;25:1201-16. [DOI] [PubMed] [Google Scholar]
- 12.Palali A, van Ours JC. Cannabis use and support for cannabis legalization. Empir Econ 2017;53:1747-70. [Google Scholar]
- 13.Le Foll B, Tyndale RF. Cannabinoids: Friend or foe? Clin Pharmacol Ther 2015;97:528-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: A systematic review and meta-analysis. JAMA 2015;313:2456-73. [DOI] [PubMed] [Google Scholar]
- 15.Kilcher G, Zwahlen M, Ritter C, et al. Medical use of cannabis in Switzerland: Analysis of approved exceptional licences. Swiss Med Wkly 2017;147:w14463. [DOI] [PubMed] [Google Scholar]
- 16.Hädener M, Gelmi TJ, Martin-Fabritius M, et al. Cannabinoid concentrations in confiscated cannabis samples and in whole blood and urine after smoking CBD-rich cannabis as a “tobacco substitute.” Int J Legal Med 2019;133:821-32. [DOI] [PubMed] [Google Scholar]
- 17.Fischer B, Imtiaz S, Rudzinski K, Rehm J. Crude estimates of cannabis-attributable mortality and morbidity in Canada– implications for public health focused intervention priorities. J Public Health 2016;38:183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bell R, Wechsler H, Johnston LD. Correlates of college student marijuana use: results of a US National Survey. Addiction 1997;92:571-81. [PubMed] [Google Scholar]
- 19.Caldeira KM, Arria AM, O’Grady KE, et al. The occurrence of cannabis use disorders and other cannabis-related problems among first-year college students. Addict Behav 2008;33:397-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hammersley R, Leon V. Patterns of cannabis use and positive and negative experiences of use amongst university students. Addict Res Theory 2006;14:189-205. [Google Scholar]
- 21.Arseneault L, Cannon M, Witton J, Murray RM. Causal association between cannabis and psychosis: Examination of the evidence. Focus 2007;5:270-8. [DOI] [PubMed] [Google Scholar]
- 22.Brook JS, Balka EB, Whiteman M. The risks for late adolescence of early adolescent marijuana use. Am J Public Health 1999;89:1549-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.French MT, Roebuck MC, Alexandre PK. Illicit drug use, employment, and labor force participation. South Econ J 2001;68:349-68. [Google Scholar]
- 24.van Ours JC. Cannabis, cocaine and jobs. J Appl Econom 2006;21:897-917. [Google Scholar]
- 25.van Ours JC, Williams J, Fergusson D, Horwood LJ. Cannabis use and suicidal ideation. J Health Econ 2013;32:524-37. [DOI] [PubMed] [Google Scholar]
- 26.Di Forti M, Quattrone D, Freeman TP, et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. Lancet Psychiatry 2019;6:427-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hartman RL, Brown TL, Milavetz G, et al. Cannabis effects on driving lateral control with and without alcohol. Drug Alcohol Depend 2015;154:25-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States Between 2001-2002 and 2012-2013. JAMA Psychiatry 2015;72:1235-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction 2015;110:19-35. [DOI] [PubMed] [Google Scholar]
- 30.van der Pol P, Liebregts N, de Graaf R, et al. Mental health differences between frequent cannabis users with and without dependence and the general population. Addiction 2013;108:1459-69. [DOI] [PubMed] [Google Scholar]
- 31.Gossop M, Darke S, Griffiths P, et al. The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction 1995;90:607-14. [DOI] [PubMed] [Google Scholar]
- 32.Steiner S, Baumeister SE, Kraus L. [Severity of Dependence Scale: Establishing a cut-off point for cannabis dependence in the German adult population].[Article in German with English Abstract]. SUCHT 2008;54:57-63. [Google Scholar]
- 33.van Ours JC, Williams J. Cannabis use and its effects on health, education, and labor market success. J Econ Surv 2015;29:993-1010. [Google Scholar]
- 34.Bravo AJ, Anthenien AM, Prince MA, Pearson MR. Marijuana protective behavioral strategies as a moderator of the effects of risk/protective factors on marijuana-related outcomes. Addict Behav 2017;69:14-21. [DOI] [PubMed] [Google Scholar]
- 35.Bravo AJ, Prince MA, Pearson MR. Can i use marijuana safely? An examination of distal antecedents, marijuana protective behavioral strategies, and marijuana outcomes. J Stud Alcohol Drugs 2017;78:203-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pearson MR, Bravo AJ, Conner BT. Distinguishing subpopulations of marijuana users with latent profile analysis. Drug Alcohol Depend 2017;172:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pedersen ER, Huang W, Dvorak RD, et al. The Protective Behavioral Strategies for Marijuana Scale: Further examination using item response theory. Psychol Addict Behav 2017;31:548-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pedersen ER, Villarosa-Hurlocker MC, Prince MA. Use of protective behavioral strategies among young adult veteran marijuana users. Cannabis 2018;1:14-27. [PMC free article] [PubMed] [Google Scholar]
- 39.Morfeld M, Kirchberger I, Bullinger M. [SF-12 Fragebogen zum Gesundheitszustand. Selbstbeurteilungsbogen, Zeitfenster 4 Wochen. 2., ergänzte und überarbeitete Auflage].[in German]. Hogrefe Verlag, Göttingen; 2012. [Google Scholar]
- 40.Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc 1988;83:1198-202. [Google Scholar]
- 41.Schulenberg JE, Johnston LD, O’Malley PM, et al. Monitoring the future national survey results on drug use, 1975-2018. Volume II, College Students & Adults Ages 19-60. Ann Arbor: The University of Michigan, Institute for Social Research; 2019. Available from: https://files.eric.ed.gov/fulltext/ED599071.pdf [Google Scholar]
- 42.Fetherston J, Lenton S. SPECIAL SECTION: EVALUATION OF THE WESTERN AUSTRALIAN CANNABIS INFRINGEMENT NOTICE SCHEME—PHASE 1: Community attitudes towards cannabis law and the proposed Cannabis Infringement Notice scheme in Western Australia. Drug Alcohol Rev 2005;24:301-9. [DOI] [PubMed] [Google Scholar]
- 43.Arnold JF, Sade RM. Regulating marijuana use in the United States: Moving past the gateway hypothesis of drug use. J Law Med Ethics 2020;48:275-8. [DOI] [PubMed] [Google Scholar]
- 44.Swift W, Copeland J, Hall W. Choosing a diagnostic cut-off for cannabis dependence. Addiction 1998;93:1681-92. [DOI] [PubMed] [Google Scholar]
- 45.van der Pol P, Liebregts N, de Graaf R, et al. Reliability and validity of the Severity of Dependence Scale for detecting cannabis dependence in frequent cannabis users. Int J Methods Psychiatr Res 2013;22:138-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bravo AJ, Weinstein AP, Pearson MR. The relationship between risk factors and alcohol and marijuana use outcomes among concurrent users: A comprehensive examination of protective behavioral strategies. J Stud Alcohol Drugs 2019;80:102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jordan HR, Madson MB, Bravo AJ, Pearson MR. Post-traumatic stress and marijuana outcomes: The mediating role of marijuana protective behavioral strategies. Subst Abus 2020;41:375-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prince MA, Jenzer T, Brown W, et al. Examining cannabis protective behavioral strategy use using multiple methods. Drugs Alcohol Toda. 2019;19:295-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cheung KL, ten Klooster PM, Smit C, et al. The impact of nonresponse bias due to sampling in public health studies: A comparison of voluntary versus mandatory recruitment in a Dutch national survey on adolescent health. BMC Public Health 2017;17:276. [DOI] [PMC free article] [PubMed] [Google Scholar]


