Abstract
The challenges of identifying and eliminating racial disparities regarding the exposure, transmission, prevention, and treatment of communicable diseases within the healthcare system have been a mounting concern since the COVID-19 pandemic began. The African, Caribbean, and Black (ACB) populations in Canada represent a fast-expanding and underprivileged community, which have been previously found to have higher susceptibility to communicable diseases and lower sensitivity to intervention measures. Currently, there is insufficient evidence to adequately identify racial patterns in the prevalence and healthcare utilization among the ACB population within the context of the ongoing pandemic. Our proposed study will explore the association between the social determinants of health (SDH) and COVID-19 health outcomes in ACB populations in high-income countries (UK, US, Australia, Canada). We will explore the current evidence through a systematic review of COVID-19 pandemic literature covering the period between December 2019 and October 2020. The objectives include investigating the effect of SDH on the ACB populations’ risk to COVID-19 health outcomes, including COVID-19 infection incidence, severity of disease, hospitalization, mortality and barriers to the treatment and management of COVID-19 for Black people in Canada. In addition, this project aims to investigate the effect of COVID-19 on ACB communities in Ontario by examining the challenges that front-line healthcare workers and administrators have during this pandemic as it pertains to service provisions to ACB communities. A systematic review of original and review studies will be conducted based on the publications on eleven databases (MEDLINE, Web of Science, Cochrane Library, CINAHL, NHS EDD, Global Health, PsychInfo, PubMed, Scopus, Proquest, and Taylor and Francis Online Journals) Primary outcomes will include the rate of COVID-19 infection. The systematic review will include a meta-analysis of available quantitative data, as well as a narrative synthesis of qualitative studies. This systematic review will be among the first to report racial disparities in COVID-19 infection among the ACB population in Canada. Through synthesizing population data regarding the risk factors on various levels, the findings from this systematic review will provide recommendations for future research and evidence for clinical practitioners and social workers. Overall, a better understanding of the nature and consequences of racial disparities during the pandemic will provide policy directions for effective interventions and resilience-building in the post-pandemic era.
Significance for public health.
Since the outbreak of the recent COVID-19 pandemic, there has been a growing concern regarding the challenges in identifying and eliminating racial disparities in exposure to transmission of communicable diseases and access to preventive and curative healthcare services. This is particularly the case for the countries that experience high numbers of immigrants, including Canada, where the racial inequality remains a major public health concern. Existing research suggests that the African, Caribbean, and Black (ACB) population in Canada represent a fast-expanding and underprivileged community previously found to have higher susceptibility to communicable diseases and lower sensitivity to intervention measures. However, currently there is no systematic research on the social determinants that underlie the disproportionately higher prevalence of COVID-19 among the ACB population. The findings of our systematic review will contribute to evidence-based policy making targeted at addressing the COVID-19 related vulnerabilities among ACB population and thereby ensuring more effective containment of the pandemic.
Key words: African, Caribbean and Black population, Canada, COVID- 19, health inequality, pandemic, racial disparities
Introduction
Health and disease are influenced by the complex interplay between various micro (biochemistry and genetics) and macro (sociocultural and environmental) level factors.1–4 This is the basis of the social determinants of health (SDH) approach to health promotion and diseases prevention programs at all levels. The African diaspora experience systemic challenges that perpetuate health inequities, which can be critically analyzed through the different social determinants of health such as income, education, employment, housing, food access, gender, disability, and race. Actions towards addressing health disparities not only help tackle the pandemic, but also develop better resilience and healthcare capacity building during the post-pandemic era. This would require informed policy guidelines for best-practices and effective intervention strategies by bridging the knowledge gap in the key areas of COVID-19 related to vulnerabilities among the ACB populations.5-8
The SDH applies in pandemics,9,10 including the current COVID-19 pandemic, which seems to be caused by a pathogen of unknown origin and to reach beyond the control of healthcare systems. Among the healthcare-related factors, lack of culturally competent healthcare providers and fear of cross-transmission in the healthcare facilities can significantly affect care-seeking behavior among ACB populations. Similar findings are being reported in the COVID-19 literature, which show how economic, social, or environmental disadvantages determine the susceptibility of infection.11-13
Indeed, diseases are deeply social phenomena in their origin, distribution, impact, and in the responses that they engender among populations.14 So far, large volumes of studies have been dedicated to exploring how our exposure and chance of survival from a particular health condition are influenced by social and environmental conditions.15-18
These social structures deliberately manipulate the distribution of power, resources, capacities, and opportunities as it relates to the ACB community; in the context of COVID-19, they manifest as the discriminatory barriers to prevention and intervention measures. High-exposure occupations, financial strains to afford prevention interventions, ineffective health promotion efforts, systemic anti-Black racist policies, and inadequate living conditions facilitate disproportional COVID-19 transmission for ACB peoples. For instance, in Illinois, African Americans account for 17% of the COVID-19 cases and 29.7% of COVID-19-attributable mortalities while making up only 15% of the state’s population.19 Similarly in Chicago, African Americans already account for 52% of total cases and 72% of COVID-19-attributable mortalities while making up only 30% of the city’s population.20
Increased burden of COVID-19 morbidity and mortality among marginalized populations translates to greater challenges for healthcare systems and for governments through loss of social capital, productive labour force, and erosion of cultural equity.21-23
In terms of reducing the risk for COVID-19, health equity must be achieved by maintaining the highest possible standard of healthcare for all people and giving special attention to the needs of populations most at-risk of infection based on the SDH.24 From this viewpoint, addressing the racial disparities should be regarded as integral to infection-control measures and ultimate recovery from the pandemic.25-27 Ensuring equitable access and provisions of care will require the creation of race-sensitive and culturally competent workforces across the healthcare continuum; including administrators, clinicians, epidemiologists, information systems professionals, safety personnel, nurses, and funders.28,29
The proposed systematic review is part of a CIHR funded project entitled “Advancing Healthcare for COVID-19 in Ontario: Strengthening providers’ capacity for best practices in African, Caribbean and Black (ADHECO-ACB)”. It is in line with the Coordinated Global Research Roadmap by WHO & Global Research Collaboration for Infectious Disease Preparedness and Response (GLOPID-R). This project aims to investigate the effect of COVID-19 in ACB communities in Ontario, examine the challenges that front-line health workers and administrators have during this pandemic as it pertains to the service provision to ACB communities, and elucidate the strategies necessary for post-pandemic health equity.
There are a growing number of systematic reviews and metaanalyses on the effect of racism on outcomes such as health conditions and healthcare seeking behaviours.30,31 However, these studies are mostly limited in their scope to chronic health conditions32,33 and there is limited evidence regarding the associations between racism and its impacts on COVID-19. The proposed systematic review will explore whether there are any associations between the social determinants of health and COVID-19 health outcomes specifically within ACB population in high-income countries (e.g., UK, USA, Australia).
Methods and analyses
Search strategy for identification of studies
We will conduct an exhaustive search of published studies in eleven databases - Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Cochrane Library, the National Health Service Economic Development Database (NHS EDD), Global Health, PsychInfo, PubMed, Scopus, Proquest, Taylor & Francis Online Journals and Web of Science. The following search terms will be used in combination with the primary outcome variable (“COVID-19″, “novel coronavirus”, “2019-ncov”, “ncov”, “novel betacov”)”race”, “racism”, “Black health”, “ethnicity”; “Health disparity”; “”people of color”
Criteria for including studies
Types of studies
Studies included in the review will be experimental and observational including quantitative, qualitative and mixed methods data. In addition, evidence syntheses will be included in the review.
Inclusion and exclusion criteria
For inclusion in the review studies must include data on SDH (such as income, education, and social exclusion) related to COVID-19 health outcomes in African, Caribbean, and Black (ACB) populations.7 Studies based in high-income countries (UK, USA, Australia, Canada) will be exclusively included in the review. Papers published till October 2020 in English language will be assessed for review. Studies involving clinical factors, genetic, pharmacological aspects will be excluded.
Outcomes
The primary outcomes of this systematic review include:
Effect of the SDH, such as race, housing, and employment status, on COVID-19 health outcomes specifically for ACB populations.
The COVID-19 health outcomes (rate of COVID-19 infection, severity of disease, hospitalization, mortality) that are most significantly influenced by the social determinants of health in ACB populations
Screening
All references retrieved will be imported into Covidence to facilitate study screening and selection. Covidence will remove duplicate studies prior to undertaking the title and abstract screening. Each article will be screened by two independent reviewers, including JE, BG, PD, JD, WA, GA, SA, FW, SB, IT. Conflicts will be resolved by a third author who has not screened the article JE, BG, PD, JD, WA, GA, SA, FW. Our screening form will be developed and applied independently to a sample of 50 abstracts to ensure consistency of use and clarity of the instrument. A Cohen’s kappa statistic will be used to measure inter-rater reliability, and screening will start when >60% agreement was achieved.3
Data collection and analyses
Data extraction
The data from each retrieved studies will be independently extracted by two authors (JE, BG, PD, JD, WA, GA, SA, FW) using standardized forms. Any disagreement will be resolved via discussion by JE and BG. We will extract bibliometric information such as authors’ names, journal, and year of publication. We will also extract the number of participants, study design, location, outcomes reported, outcome measures, and the phenomena of interest.
Assessment of methodological quality
Eligible studies will be critically appraised by all independent reviewers for methodological quality using Covidence. Any disagreements that arise between the reviewers will be resolved with a third reviewer. The results of critical appraisal will be reported in narrative form and in a table. Studies that do not meet a certain quality threshold will be excluded.
Analyses and reporting
Findings will be reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.5-7
This process will include aggregating and categorizing the findings based on similar meanings. These categories will then be subjected to a synthesis in order to produce a single comprehensive set of findings that can be used as a basis for evidence-based practice. Where textual pooling is not possible the findings will be presented in narrative form.
Assessing confidence in the findings
We reviewed the Cochrane method, JBI and thematic synthesis to determine the most appropriate approach for our study. The Cochrane method uses primary research to generate new knowledge about the effects of an intervention; however, most of the research we retrieved from our search were based on retrospective studies and secondary data. JBI employs the ConQual method which is tailored for qualitative studies; however, we will include various study types including commentaries and quantitative research. Therefore, due to the unique composition of studies we opted to analyse the extracted data through a process we have called ‘Thematic Mapping’ (Figure 1).
Following completion of data extraction, thematic mapping, a process that consists of three main stages will guide the research process. These stages have been adapted from Ryan34 and Duran35 approaches to narrative synthesis and involve i) grouping articles by differences and similarities, such as quantitative, qualitative and commentary; ii) thematic synthesis encompassing ‘within-group’ analysis to create analytical themes; and iii) ‘across-group’ analysis of the analytical themes. This mapping process helps to identify the relationships between analytical themes across groups to produce the major themes of the whole systematic review results. Thematic synthesis will be performed on selected studies in the three-step process of i) creating initial codes, ii) creating descriptive themes, iii) creating analytical themes, as outlined by Joo and Liu36 and Thomas and Harden.37 In step 1, studies will be entered verbatim into a database and pairs of reviewers will use inductive reasoning to code the primary studies line by line for content and meaning, without hierarchy. These initial “free codes” will be grouped by the reviewers into a hierarchical tree structure based on the codes’ similarities and differences. In step 2 new codes will be generated based on the meaning of these groups, thus creating several layers of descriptive themes. A draft summary of the descriptive themes will be composed by one reviewer and subsequently re-reviewed by two additional reviewers, followed by discussions until a final consensus is achieved. In step 3 the resultant descriptive themes will be inductively analyzed to answer questions pertaining to the effects of the SDH on ACB populations risk to COVID-19 and barriers to the treatment and management of Black people in Canada Ontario. Inferences, with consideration to risk factors and the nature and consequences of racial disparities, will be initially reviewed in pairs then reviewed as a group. Group discussions will generate analytical themes which will be re-examined against previous themes and altered as necessary; this iterative process will be repeated until all inferred findings and descriptive themes are inclusively described by the resultant analytical themes. Analytical themes from each group will then go through the third stage of thematic mapping, i.e. across group analysis with the aim of generating the main themes of the systematic review. To ensure methodological rigor all steps will be performed in pairs, twice for each study.
Discussion
Globally in many high-income countries, ACB populations experience anti-Black racism, poverty, and stigma that contribute to reduced overall health outcomes.33,38 The social determinants of health, as outlined by Canadian scholar Dr. Raphael, describe the complex interactions between human biological health and various sociological and socioeconomic factors such as income, housing, social safety nets, employment and working conditions, and race.39,40 In the context of the current COVID-19 pandemic, these influence significant risk factors to COVID-19 exposure, transmissibility, and health outcomes.35,41 This systematic review begins an exploration of the unique social positioning of the African diaspora in various high-income countries and aims to expose the important effect of the SDH in COVID-19 health outcomes for ACB communities. This systematic review could be used to improve healthcare management policy, development of new health promotion strategies, and inform post-pandemic public health and safety practices. A key limitation of this systematic review is the novelty of the research topic, which may demonstrate a lack of sufficient publications. This may result in missing data of important real-world consequences of COVID-19 in ACB communities. In addition, only English studies were considered in this review, which may exclude data from other high-income countries such as France, Germany, and Italy. However, the comprehensive search strategy in the literature on this unique population will illustrate some key factors to consider in research and public health policy globally.
Figure 1.
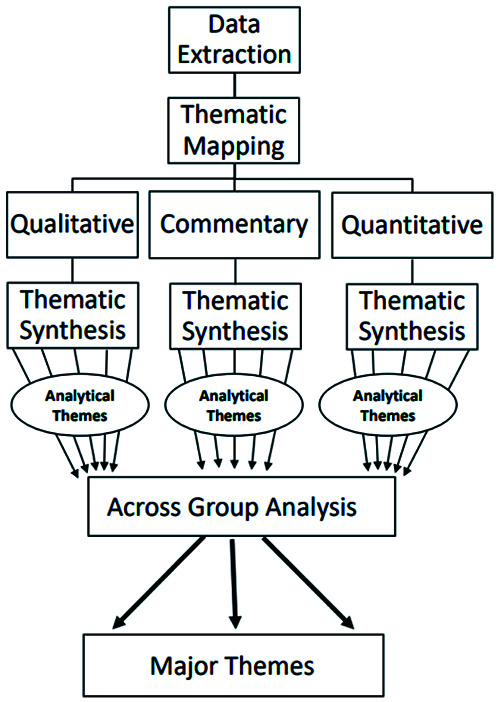
Thematic mapping.
Acknowledgments
We acknowledge the intellectual and technical support by many of our colleagues and especially the librarians.
Funding Statement
Funding: The study is funded by Canadian Institute of Health Research. Grant no: FRN 172739.
References
- 1.Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Ann Fam Med 2004;2:576–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wade DT, Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil 2017;31:995-1004. [DOI] [PubMed] [Google Scholar]
- 3.Amzat J, Razum O. Sociology and health. In: Amzat J, Razum O, editors. Medical Sociology in Africa. Cham: Springer; 2014. p. 1-19. [Google Scholar]
- 4.Mechanic D. Sociology and public health: perspectives for application. Am J Public Health 1972;62:147–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014;129:s19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Islam MM. Social determinants of health and related inequalities: Confusion and implications. Front Public Health 2019;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. Can Med Assoc J 2016;188:e474–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marmot M, Allen JJ. Social determinants of health equity. Am J Public Health 2014;104:S517–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lowcock EC, Rosella LC, Foisy J, et al. The social determinants of health and pandemic H1N1 2009 influenza severity. Am J Public Health 2012;102:e51-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lenzi L, de Mello ÂM, da Silva LR, et al. Pandemic influenza A (H1N1) 2009: risk factors for hospitalization. J Bras Pneumol 2012;38:57–65. [DOI] [PubMed] [Google Scholar]
- 11.Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths. Ann Intern Med 2021;174:362-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson G, Frank JW, Naylor CD, et al. Using socioeconomics to counter health disparities arising from the covid-19 pandemic. BMJ 2020;369:m2149. [DOI] [PubMed] [Google Scholar]
- 13.Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:964-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Public Books [Internet]. Pandemic Syllabus. 2020. Accessed: 30 Jul 2020. Available from: https://www.publicbooks.org/pandemic-syllabus/ [Google Scholar]
- 15.Annang L, Walsemann KM, Maitra D, Kerr JC. Does education matter? Examining racial differences in the association between education and STI diagnosis among Black and White young adult females in the U.S. Public Health Rep 2010;125:s110–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adedini SA, Odimegwu C, Imasiku ENS, Ononokpono DN. Ethnic differentials in under-five mortality in Nigeria. Ethn Health 2015;20:145–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odimegwu C, Somefun OD. Ethnicity, gender and risky sexual behaviour among Nigeria youth: an alternative explanation. Reprod Health 2017;14:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Antai D. Inequalities in under-5 mortality in Nigeria: do ethnicity and socioeconomic position matter? J Epidemiol 2011;21:13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamidian Jahromi A, Hamidianjahromi A. Why African Americans are a potential target for COVID-19 infection in the United States. J Med Internet Res 2020;22:e19934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Global News [Internet]. Chicago’s rate of coronavirus deaths, illness among Black residents alarms U.S. cities. Accessed: 30 Apr 2020. Available from: https://globalnews.ca/news/6785622/coronavirus-black-chicago-deaths-covid/ [Google Scholar]
- 21.McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat Med 2020;26:640-2. [DOI] [PubMed] [Google Scholar]
- 22.Martínez-Martínez OA, Rodríguez-Brito A. Vulnerability in health and social capital: a qualitative analysis by levels of marginalization in Mexico. Int J Equity Health 2020;19:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Your University [Internet]. New study finds higher social capital and trust leads to better COVID-19 response in some U.S. states. Accessed: 3 May 2020. Available from: https://www.yorku.ca/laps/2020/04/02/new-study-finds-higher-social-capital-and-trust-leads-to-better-covid-19-response-in-some-u-sstates/ [Google Scholar]
- 24.Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep 2014;129:s5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abedi V, Olulana O, Avula V, et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities 2021;8:732-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishnan L, Ogunwole SM, Cooper LA. Historical insights on coronavirus disease 2019 (COVID-19), the 1918 influenza pandemic, and racial disparities: Illuminating a path forward. Ann Intern Med 2020;173:474–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tucker CM, Marsiske M, Rice KG, et al. Patient-centered culturally sensitive health care: Model testing and refinement. Health Psychol 2011;30:342–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tucker CM, Mirsu-Paun A, Van den Berg JJ, et al. Assessments for measuring patient-centered cultural sensitivity in community-based primary care clinics. J Natl Med Assoc 2007;99:609–19. [PMC free article] [PubMed] [Google Scholar]
- 29.Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilization: A systematic review and meta-analysis. PLoS One 2017;12:e0189900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financ Rev 2000;21:75–90. [PMC free article] [PubMed] [Google Scholar]
- 31.Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord 2021;281:91–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med 2020;8e35. [PMC free article] [PubMed] [Google Scholar]
- 33.Spigner C. Race, health, and the African Diaspora. Int Q Community Health Educ 2006-2007;27:161-76. [DOI] [PubMed] [Google Scholar]
- 34.Ryan KE, Gandha T, Culbertson MJ, Carlson C. Focus group evidence: Implications for design and analysis. Am J Eval 2014;35:328-45. [Google Scholar]
- 35.Duran B. Posttraumatic growth as experienced by childhood cancer survivors and their families: a narrative synthesis of qualitative and quantitative research. J Pediatr Oncol Nurs 2013;30:179–97. [DOI] [PubMed] [Google Scholar]
- 36.Joo JY, Liu MF. Nurses’ barriers to caring for patients with COVID-19: a qualitative systematic review. Int Nurs Rev 2021;68:202-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kerani RP, Kent JB, Sides T, et al. HIV among African-born persons in the United States: a hidden epidemic? J Acquir Immune Defic Syndr 2008;49:102-6. [DOI] [PubMed] [Google Scholar]
- 39.Burström B, Tao W. Social determinants of health and inequalities in COVID-19. Eur J Public Health 2020;30:617–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020;8:659-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saha S, Beach MC, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Natl Med Assoc 2008;100:1275–85. [DOI] [PMC free article] [PubMed] [Google Scholar]


