Abstract
This report describes a case of acute uveitis following COVID-19 vaccination. A 21-year-old patient was referred to our department for decreased visual acuity and injection of the left eye. Two days prior, the patient received her second dose of the severe acute respiratory syndrome coronavirus 2 vaccine (BNT162b2, Pfizer-BioNTech). On ocular examination, her left eye's best-corrected visual acuity was 20/250, and its intraocular pressure was 16 mm Hg on a noncontact tonometer. Hypopyon, 4+ cells, and flares were observed in the anterior chamber. The patient was diagnosed with acute uveitis. She received topical dexamethasone (0.1%) hourly and systemic prednisone (50 mg/day). After 7 days, her inflammatory symptoms were mostly resolved. COVID-19 vaccination can cause acute anterior uveitis, which is responsive to steroids.
Keywords: COVID-19, Uveitis, Vaccination
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a highly infectious agent that causes COVID-19, which was first reported in Wuhan, China, on December 31, 2019 [1]. COVID-19 vaccines were rapidly developed based on previous vaccines for pathogens, such as the Middle East respiratory syndrome and severe acute respiratory syndrome [2]. In December 2020, the US Food and Drug Administration authorized the BNT162b1 (Pfizer Inc., New York, NY, USA; BioNTech, Inc., Mainz, Germany) and mRNA-1273 (Moderna, Inc., Cambridge, MA, USA) mRNA vaccines. Adenovirus vector vaccines (ChAdOX1 nCov-19 produced by AstraZeneca and Ad26.COV2.S produced by Janssen − Johnson & Johnson) have also been approved and distributed worldwide. The vaccines reduced the morbidity and mortality rates of the disease [3]. However, systemic side effects, such as thrombosis, have been reported [4]. Herein, we report a case of acute uveitis following COVID-19 vaccination.
Case Report/Case Presentation
A 21-year-old female patient was referred to our clinic for decreased visual acuity and injection of the left eye. The patient received her second dose of a SARS-CoV-2 vaccine (BNT162b2, Pfizer) 2 days before the symptom onset. Moreover, she had no history of uveitis.
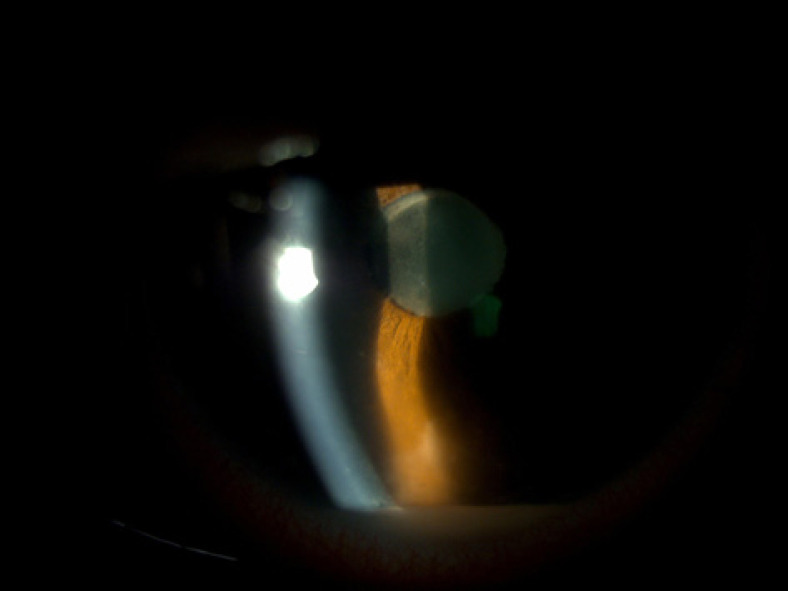
On ocular examination, her best-corrected visual acuity was 20/20 in the right eye and 20/250 in the left eye. The intraocular pressure was 14/16 mm Hg on a noncontact tonometer. On slit-lamp examination, conjunctival injection and hypopyon with 4+ cells were observed in the left eye (Fig. 1). On fundus examination, the posterior pole was not observed because of dim vision and poor pupil dilation.
Fig. 1.
Slit-lamp image at the initial visit.
The patient was diagnosed with acute uveitis. She then received topical dexamethasone (0.1%) hourly, atropine sulfate eye drops (1%) twice a day, and systemic prednisone (50 mg). She underwent routine blood tests, C-reactive protein levels, antineutrophil, cytoplasmic antibody, streptolysin O, syphilis, tuberculosis, and HLA-B27. All test results were unremarkable. Three days after treatment, her best-corrected visual acuity improved to 20/200 in the left eye. On slit-lamp examination, the hypopyon was nearly resolved; however, 4+ cells were observed in the anterior chamber of the left eye. Dilated fundus examination revealed no vitritis or posterior uveitis in either eye. The patient continued receiving topical eye drops and systemic prednisone.
A slit-lamp examination was performed 7 days after treatment. Flares and 2+ cells were observed in the anterior chamber (Fig. 2). The best-corrected visual acuity was 20/40 in the left eye, and the dilated fundus examination was normal. One month later, the cells and flares had subsided, and the best-corrected visual acuity was 20/20.
Fig. 2.
Slit-lamp image on day 7 posttreatment.
Discussion/Conclusion
In this report, we present a case of acute uveitis in a young woman who received her second dose of the BNT162b2 vaccine. Vaccine-induced ocular complications rarely occur, and few studies on the ocular complications of the COVID-19 vaccine have been reported. A severe ocular complication is graft rejection postvaccination. There have been several reports of graft rejection following BNT162b2 vaccination [5, 6]. The occurrence of acute corneal epithelial rejection of living-related conjunctival limbal allograft has also been reported in a patient, who received the mRNA-1273 vaccine [7]. The World Health Organization recently released the interim recommendations on the use of the inactivated SARS-CoV-2 vaccine (BBIBP-CorV, Sinopharm, Beijing, China) [8]. El Sheikh et al. reported a case of uveitis following inactivated SARS-CoV-2 vaccination (BBIBP-CorV, Sinopharm, Beijing, China) [9]. Furthermore, Pan et al. reported a case of bilateral uveitis following administration of the same vaccine [10]. Recently, Rabinovitch et al. describe uveitis cases after the BNT162b2 mRNA SARS-CoV-2 vaccination [11], and they reported that uveitis after vaccination is uncommon and manifests most often as a mild to moderate uveitis.
Vaccination possibly contributed to the occurrence of uveitis based on the temporal association between vaccination and the onset of uveitis. However, the exact pathogenesis of uveitis following vaccination remains unclear. Cunningham proposed a mechanism based on the molecular similarities between uveal self-peptides and vaccine peptides, delayed-type hypersensitivity, and immune responses against vaccine adjuvants [12]. Steinemann et al. suggested that increased vascular permeability after vaccination affected the immunologic capability of the cornea. Immune complex deposition in the uvea and iris initiates a local inflammatory response [13]. In our case, the patient's favorable response to prednisolone indicated the association between uveitis and the vaccine-induced immune response. In this patient, hypopyon and severe visual distortion were observed. These were not seen in previous uveitis cases, associated with BBIBP-CorV vaccination. However, the inflammation was adequately controlled and quickly responded to steroids. Based on previous reports on vaccine-induced uveitis, the inflammatory reaction, induced by inactivated vaccines, was more severe than that induced by mRNA vaccines. In conclusion, we reported a case of acute uveitis following a COVID-19 vaccination. Although initially severe, the patient's uveitis responded well to steroid therapy. In patients complaining of congestion or impaired vision postvaccination, the anterior chamber should be evaluated for inflammation to check for uveitis.
Statement of Ethics
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. This retrospective review of patient data did not require ethical approval in accordance with local guidelines. All procedures followed were in accordance with ethical standards and the Helsinki Declaration.
Conflict of Interest Statement
We have no conflict of interest to declare.
Funding Sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
Substantial contributions to the conception or design of the work: J.H.H. Acquisition of data for the work: J.H.H. Drafting the work: J.H.H.
Data Availability Statement
All data generated or analyzed during this study are included in this article, and further inquiries can be directed to the corresponding author.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang BMS, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 Feb;382((8)):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aslam S, Goldstein DR, Vos R, Gelman AE, Kittleson MM, Wolfe C, et al. COVID-19 vaccination in our transplant recipients: the time is now. J Heart Lung Transplant. 2021 Mar;40((3)):169–171. doi: 10.1016/j.healun.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook TM, Roberts JV. Impact of vaccination by priority group on UK deaths, hospital admissions and intensive care admissions from COVID-19. Anaesthesia. 2021 May;76((5)):608–616. doi: 10.1111/anae.15442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang JC, Hawley HB. Vaccine-associated thrombocytopenia and thrombosis: Venous endotheliopathy leading to venous combined micro-macrothrombosis. Medicina. 2021 Nov;5757((1111)):1163. doi: 10.3390/medicina57111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phylactou M, Li JO, Larkin DFP. Characteristics of endothelial corneal transplant rejection following immunisation with sars-cov-2 messenger RNA vaccine. Br J Ophthalmol. 2021 Apr;105((7)):893–896. doi: 10.1136/bjophthalmol-2021-319338. [DOI] [PubMed] [Google Scholar]
- 6.Abousy M, Bohm K, Prescott C, Bonsack JM, Rowhani-Farid A, Eghrari AO. Bilateral ek rejection after covid-19 vaccine. Eye Contact Lens. 2021 Nov;47((11)):625–628. doi: 10.1097/ICL.0000000000000840. [DOI] [PubMed] [Google Scholar]
- 7.de la Presa M, Govil A, Chamberlain WD, Holland EJ. Acute corneal epithelial rejection of LR-CLAL after SARS-CoV-2 vaccination. Cornea. 2021 doi: 10.1097/ICO.0000000000002914. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 8.Wang H, Zhang Y, Huang B, Deng W, Quan Y, Wang W, et al. Development of an inactivated vaccine candidate, BBIBP-CorV, with potent protection against SARS-CoV-2. Cell. 2020 Aug;182((3)):713–21.e9. doi: 10.1016/j.cell.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.ElSheikh RH, Haseeb A, Eleiwa TK, Elhusseiny AM. Acute uveitis following COVID-19 vaccination. Ocul Immunol Inflamm. 2021:1–3. doi: 10.1080/09273948.2021.1962917. [DOI] [PubMed] [Google Scholar]
- 10.Pan L, Zhang Y, Cui Y, Wu X. Bilateral uveitis after inoculation with COVID-19 vaccine: a case report. Int J Infect Dis. 2021 Dec;113:116–118. doi: 10.1016/j.ijid.2021.09.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabinovitch T, Weintrob YB, Blum TH, Shaer B, Dai VV, Shulman S, et al. Uveitis after the BNT162b2 mRNA vaccination against SARS-CoV-2 infection: a possible association. Retina. 2021;41((12)):2462–713. doi: 10.1097/IAE.0000000000003277. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham ET, Moorthy RS, Fraunfelder FW, Zierhut M. Vaccine-associated uveitis. Ocul Immunol Inflamm. 2019;27((4)):517–520. doi: 10.1080/09273948.2019.1626188. [DOI] [PubMed] [Google Scholar]
- 13.Steinemann TL, Koffler BH, Jennings CD. Corneal allograft rejection following immunization. Am J Ophthalmol. 1988 Nov;106((5)):575–578. doi: 10.1016/0002-9394(88)90588-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article, and further inquiries can be directed to the corresponding author.