Abstract
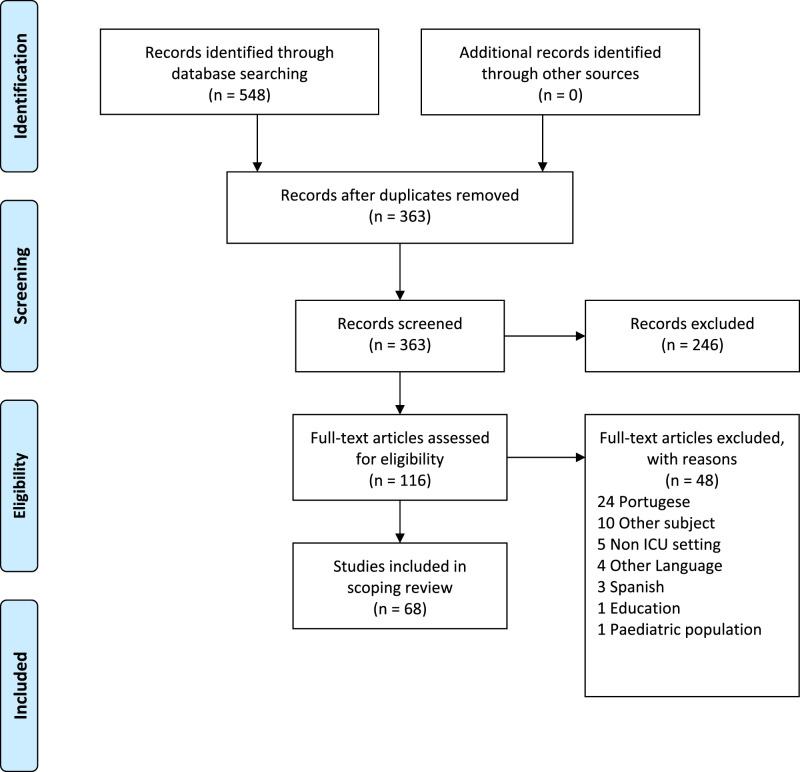
Significant scientific and technological advances in intensive care have been made. However, patients in the intensive care unit may experience discomfort, loss of control, and surreal experiences. This has generated relevant debates about how to humanize the intensive care units and whether humanization is necessary at all. This paper aimed to explore how humanizing intensive care is described in the literature. A scoping review was performed. Studies published between 01.01.1999 and 02.03.2020 were identified in the CINAHL, Embase, PubMed, and Scopus databases. After removing 185 duplicates, 363 papers were screened by title and abstract. Full-text screening of 116 papers led to the inclusion of 68 papers in the review based on the inclusion criteria; these papers mentioned humanizing or dehumanizing intensive care in the title or abstract. Humanizing care was defined as holistic care, as a general attitude of professionals toward patients and relatives and an organizational ideal encompassing all subjects of the healthcare system. Technology was considered an integral component of intensive care that must be balanced with caring for the patient as a whole and autonomous person. This holistic view of patients and relatives could ameliorate the negative effects of technology. There were geographical differences and the large number of studies from Spain and Brazil reflect the growing interest in humanizing intensive care in these particular countries. In conclusion, a more holistic approach with a greater emphasis on the individual patient, relatives, and social context is the foundation for humanizing intensive care, as reflected in the attitudes of nurses and other healthcare professionals. Demands for mastering technology may dominate nurses’ attention toward patients and relatives; therefore, humanized intensive care requires a holistic attitude from health professionals and organizations toward patients and relatives. Healthcare organizations, society, and regulatory frameworks demanding humanized intensive care may enforce humanized intensive care.
Keywords: Dehumanizing, humanizing, intensive care, intensive care unit, scoping review
Introduction
Significant scientific and technological advances within intensive care units (ICUs) have been made, improving survival rates.1,2 Patients in the ICU have life-threatening illnesses and injuries that require monitoring and specialized treatment for survival. 3 The clinical scenarios of ICU patients are complex and characterized by the potential for organ failure and death.3,4 A patient’s condition can shift rapidly from improvement to deterioration, and patients can descend into liminal states and face life-or-death situations,5,6 and several studies have shown that ICU patients may experience discomfort, panic, anxiety, unreal experiences, and dreams.5–7 In this situation, patients depend on nurses’ attention and ability to understand and respond to their emotions, symptoms, and needs.8–10
However, the occasional brutal realities of contemporary ICUs have generated relevant debates about how to humanize the ICU and whether humanization is necessary at all.11,12 Moreover, a wide variety of interventions have been suggested to humanize the ICU, ranging from improved visitation policies,13–15 practices to humanize the environment,13,14,16–18 improved communication, 16 the implementation of diaries, 19 and professional education and care models. 20 Although much effort has been made to improve the perception of intensive care among patients, relatives, and healthcare professionals, 21 humanizing intensive care remains veiled behind the multitude of interventions claiming to humanize the ICU. Consequently, a deeper understanding of what constitutes humanizing intensive care needs to be achieved. 22 Therefore, this paper aims to explore how humanizing intensive care is described in the literature.
Methods
The framework described by Arksey and O’Malley 23 and further refined by others24,25 was applied in this scoping review and includes the following steps: identifying the research question; identifying the relevant studies; selecting studies; charting the data; collating, summarizing and reporting the results, and performing a consultation exercise. 23 According to Arksey and O’Malley, 23 the scoping review process is not linear but iterative, requiring researchers to engage with each stage of the research process in a reflexive way and, where necessary, repeat steps to ensure that the literature is covered in a comprehensive manner.
Identification of relevant studies
In February 2020, a detailed search was performed in the CINAHL, Embase, PubMed, and Scopus databases for articles published between 01.01.1999 and 02.03.2020. We limited our scope to studies published since 1999, given that a paradigm shift in intensive care occurred with the use of light sedation, allowing patients to be more conscious and alert.26,27 In collaboration with a research librarian, we developed a search strategy consisting of both truncated keywords and medical subject headings. The main search terms used were intensive care unit, critically ill patients, critical care nursing, humanism, holistic nursing, and patient centered care. The search terms were combined with the Boolean operators “AND” and “OR” to both narrow and expand the search.
Any mentioning of humanizing or dehumanizing intensive care in the title or abstract was explored to find eligible literature for inclusion. This counted research article, conference abstract, editorial, or commentary. We chose to exclude literature focusing on end-of-life care, organ donation, pediatric or neonatal intensive care, laboratory studies, or settings outside intensive care were excluded to focus on ICU patients and their relatives simply being in the ICU receiving treatment and care. Literature not published in English, Norwegian, Danish, or Swedish were also excluded.
Collating, summarizing, and reporting results
We uploaded our search results to Covidence, an internet-based application for handling, screening, and including papers in systematic reviews. After removing 185 duplicates, 363 papers were screened by title and abstract. Full-text screening of 116 papers led to the inclusion of 68 papers in the review. Screening was performed in Covidence, allowing two assessors to independently assess each paper for inclusion. In case of disagreement, a third assessor made the final decision. A priori, we decided to extract the following data from each included paper: authors, publication year, journal, title, country of origin, publication type, aim, methods, findings, or results. Data extraction and descriptions of humanized care from each paper were reviewed by a second assessor. The qualitative extraction of data was not supported by Covidence but was managed using an Excel spreadsheet.
We summarized the entire data set in terms of publication year, country of origin, and publication type. The description of humanized care was thoroughly reviewed and related to other studies to identify how humanized intensive care is described, definition of humanizing intensive care, words used to describe humanizing intensive care, and theoretical background for humanizing intensive care. During the analysis process, the authors continuously reflected on the findings and discussed their implications.
We consulted with two stakeholders within the ICU community to examine our approach to the review and they contributed additional valuable insights regarding our results. This process is in line with the recommendations of Arksey and O’Malley 23 to enhance the meaning and applicability of the scoping review.
We used the Preferred Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA Statement to construct the flow diagram.28
Figure 1.
PRISMA flow diagram. From: Moher et al. (2009).
Results
The included 68 unique articles included 32 empirical research papers, 10 abstracts from conferences, six editorials, six point-of-view papers, five systematic reviews, two essays, three posters, two commentaries, one theoretical paper, and 1 case study. Geographically, studies were from Brazil (15), the US (13), the UK (10), Spain (10), and Canada (7) with a few studies from Australia (4), Jordan (1), Iran (1), Denmark (1), France (1), Portugal (1), the Netherlands (1), Nepal (1), Ecuador (1), and New Zealand (1). The majority (42 of the 69) of the papers were published between 2015 and 2020 (see Tables 1 and 2).
Table 1.
Type of paper by year published.
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Empirical research | 1 | 1 | 2 | 1 | 2 | 2 | 3 | 2 | 2 | 5 | 1 | 3 | 7 | 32 | ||||||||
| Abstracts from conferences | 1 | 2 | 1 | 1 | 2 | 3 | 10 | |||||||||||||||
| Editorials | 1 | 1 | 2 | 1 | 1 | 6 | ||||||||||||||||
| Point-of-view papers | 1 | 1 | 2 | 1 | 1 | 6 | ||||||||||||||||
| Systematic reviews/reviews | 1 | 1 | 3 | 5 | ||||||||||||||||||
| Essays | 1 | 1 | 2 | |||||||||||||||||||
| Posters | 1 | 1 | 1 | 3 | ||||||||||||||||||
| Commentaries | 1 | 1 | 2 | |||||||||||||||||||
| Theoretical papers | 1 | 1 | ||||||||||||||||||||
| Case study | 1 | 1 | ||||||||||||||||||||
| Total | 2 | 0 | 1 | 3 | 0 | 2 | 1 | 2 | 1 | 2 | 3 | 2 | 0 | 1 | 3 | 4 | 5 | 8 | 6 | 9 | 13 | 68 |
Table 2.
Type of paper by country of origin.
| Australia | Brazil | Canada | Denmark | Ecuador | France | Iran | Jordan | Nepal | New Zealand | Netherlands | Portugal | Spain | UK | US | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Empirical research | 1 | 12 | 3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | 2 | 32 | |||
| Abstracts from conferences | 1 | 1 | 1 | 1 | 2 | 4 | 10 | |||||||||
| Editorials | 1 | 2 | 3 | 6 | ||||||||||||
| Point-of-view papers | 1 | 1 | 4 | 6 | ||||||||||||
| Systematic reviews/reviews | 1 | 1 | 3 | 5 | ||||||||||||
| Essays | 1 | 1 | 2 | |||||||||||||
| Posters | 2 | 1 | 3 | |||||||||||||
| Commentaries | 2 | 2 | ||||||||||||||
| Theoretical papers | 1 | 1 | ||||||||||||||
| Case study | 1 | 1 | ||||||||||||||
| Total | 4 | 15 | 7 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | 10 | 13 | 68 |
Humanizing intensive care was defined as holistic care of the patient, a general attitude of professionals toward the patients and relatives, or an organizational trait toward all subjects of the healthcare system. Technology was seen as an integral part of intensive care that needed counterbalancing by humanistic care. The large number of studies from Spain and Brazil reflected the strong and growing interest in humanizing intensive care in these particular countries.
Defining humanizing care
This scoping review revealed that a consensus on what humanized care is and how it is described is lacking. All included papers were reviewed for explicit descriptions of humanizing care. Twelve papers took steps to define humanization in intensive care.11,13,14,17,29–36 Two of the 12 papers drew on the Royal Spanish Academy’s definition of humanization as an effort “to make someone human, familiar and affable,”11,17 whereas the remaining 10 papers revolved around three main themes: “humanizing care as holistic care of the patient”; “humanizing care as a general attitude of professionals toward the patients”; and “humanizing care as an organizational trait toward all subjects of the healthcare system.”
Humanizing care as holistic care of the patient
Some papers described humanizing care as being holistic,14,32,35 which implied seeing the patient as a whole 35 and taking into account both the family and social context. 32 Although not using the word holism in relation to humanized care, other papers point in the same direction by stressing that the patient is not only a biological entity but also an autonomous person 32 with psychosocial and spiritual needs30,34 and inherent ethical dignity. 34 Humanized care encompasses that relatives are met as whole, autonomous persons as well. 31 Moreover, families should be encouraged to play an active part in the team around the patient,14,18 and the wellbeing and autonomy of families should be a healthcare goal.14,35,36
Humanizing care as a general attitude at an interpersonal level
Humanizing care respects and preserves the patient’s human dignity.31,33,34 The act of humanizing care must come from health professionals, as suggested by Heras La Calle et al., 29 Heras La Calle et al., 30 and Mondadori et al. 33 It must be a personal and collective vow to humanize the healthcare system by promoting health in all aspects of clinical practice,29,30,33 including prevention, care, rehabilitation and end-of-life care, 33 as well as relationships, behaviors, and the environment. 29 This implies understanding oneself as part of an intricate and complex system spanning policies, management, and culture, all of which influence the ability to place the patient at the center of health care. 30 Good communication among management, healthcare professionals, patients, and relatives is viewed as essential to achieve a humanized attitude toward patients.33,36
Humanizing care: An organizational trait favoring all its subjects
On an organizational level, healthcare systems are described by Heras la Calle et al., as humanized when they place themselves at the service of patients, relatives, and healthcare professionals. 30 Serving the individual implies that organizations are aware of subjective vulnerabilities29,36 and actively try to protect vulnerable patients, relatives, and healthcare professionals by coping with power asymmetries and dehumanizing attitudes. 36 To minimize dehumanization, healthcare systems should strive to create environments and working conditions30,32,37 that enable healthcare professionals to engage with patients in high-quality30,34 multiprofessional health care.14,35
Emotional distancing by dehumanizing patients may protect professionals
Dos Santos et al., 38 García Martínez et al., 39 and Lopes and Brito 31 underlined healthcare professionals’ attitudes as key to humanizing intensive care for patients. However, patients continue to be referred to in terms of diagnoses, tasks, or organ failures.12,40 In a 2015 editorial in Intensive Care Medicine, Kompanje et al. 12 argue that dehumanizing patients by referring to them as things serves a distinct purpose: it protects physicians from feeling the pain of patients and relatives and allows them to go on working in the intensive care unit over time. 12 This is supported by McLean et al., 40 who argue that different ways of talking about patients serve different purposes. Specifically, talking about the patient in terms of organ failure may help the nurse analyze the situation, whereas talking about the patient in terms of tasks may help the nurse prioritize their time. In addition, Pereira et al. 34 suggest that the conflict between reality and ideality may cause nurses to experience emotional distress and burnout. This finding is similar to the findings of McLean et al., 40 who demonstrated that nurses reported frustration and moral distress when they failed to care for the “whole person.” Additionally, moral conflicts as a source of burnout in healthcare professionals corresponds well with the views of Kompanje et al., 12 who also note the difficulties associated with the emotional involvement and suffering of patients and relatives. However, Kompanje et al. 12 stress that it is sufficient for healthcare professionals to know that their patients and relatives suffer and act to relieve this suffering. 12 In this context, the actual actions of healthcare professionals are key to humanizing the care of patients and relatives in the ICU.
Mastering and transcending all-present technology to provide humanized care
Technological developments in health care have contributed to the reduction of morbidity and mortality, increased life expectancy, and optimized technical activities in the ICU. However, this development has not secured care focused on human values. 34 Rather, de la Fuente-Martos et al. 17 stated that one main cause of dehumanization is the intensive use of technology and the “dictatorship of technology,” which leads to patients being seen as “things.” Nevertheless, Wilkin and Slevin 41 found that technological competence was an essential part of ICU nursing despite the notion that nurses cite that technology to conflicts with humanistic care. This is supported by the findings of Alasad, 42 namely, that the use of technology and machinery in routine intensive care is considered demanding and time-consuming despite making nurses feel safe and in control. However, Alasad 42 also found that when nurses’ technological competencies increased, their attention shifted toward the patient and family while the equipment faded into the background. Moreover, nurses were valued for supporting the patient. Therefore, nurses need to balance humanistic caring and technology.41,43 This balancing requires nurses to be experienced and therefore able to prioritize care for the individual patient. 41 Alliex and Irurita 44 found that experienced nurses manipulated technology and the environment when they thought it was for the benefit of the patient, for example, decreasing alarms or protecting the patient from lights and sounds to keep the patient relaxed.
Additionally, patients had a nuanced perspective on technology as both alienating and reassuring, uncomfortable but comforting, and impersonal yet personal. 45 The patients found that nurses could minimize the alienating effect of technology by maintaining a close and supportive presence and providing comfort and care. 45 The call for presence and personal care is supported by McCallum, 43 who suggests human touch, being present and using patient names as key features of humanistic caring used to ameliorate the negative consequences of technology. 43 Consequently, nurses need to master technology to transcend it and thus be able to focus on the patient as a whole, not just as an extension of the technological equipment. 46 To facilitate this transcendence, da Silva and Ferreira 47 claim that it is essential that the use of technology in intensive care should be guided by humanistic principles such as respect for the uniqueness of the individual and human dignity. As a result, intensive care nursing performed in the ICU environment is expected to combine technique, technology, and humanizing care.
The Brazilian and Spanish movements toward humanizing intensive care
Our literature search excluded 39 Brazilian papers and 12 Spanish papers not published in English and, therefore, inaccessible to us. Nonetheless, this large number of studies adds to our finding of a strong and growing interest in humanizing intensive care in Spain and Brazil. We included 15 papers from Brazil.20,31–34,36,38,47–54 Most of the Brazilian papers included in this review referred to either the National Humanitarian Assistance Program (PNHAH) launched by the Brazilian Ministry of Health in 200120,32–34,36,48–51 or one of the several editions of the Brazilian National Humanization policy launched as early as 2004.36,48 The recurring references to national policies and programs indicate that a national political interest in promoting humanism in health care may have a tremendous effect on health care and function as a framework for healthcare research. However, Lugarinho et al. 54 describe a program of humanizing intensive care as early as 1996, which is 5 years prior to the founding of the Brazilian National Humanitarian Assistance Program. 36 Thus, a nascent trend toward humanized health care within intensive care preceded the national initiatives launched by the Brazilian Ministry of Health.
We included 10 papers from Spain.11,14,17,29,30,35,55–58 These 10 Spanish papers were initiated by an editorial by Kompanje et al. 12 in Intensive Care Medicine in 2015. Quite boldly, the authors ask whether the ICU is a branch of Hell as claimed by a former patient on national TV. In 2014, the influential Spanish research project aiming to humanize intensive care (Proyecto HU-CI) was launched. 30 This research initiative highly impacted the literature included in this review. Of the 10 included papers originating from Spain, 4 papers stemmed directly from the HU-CI project14,29,30,55, and three others refer to the HU-CI project.17,35,58 One paper raises some form of critique of the humanizing movement and the proposed need to change healthcare professionals but acknowledges that humanized intensive care benefits patients. 11
Discussion
In reviewed papers, we found that humanized care was defined in terms of holistic care of patients and relatives, as a professional attitude toward patients and as a capacity of the healthcare organization. Technology has risk to dehumanize patients; therefore, it is essential that healthcare professionals proficiently master technology, allowing them to see beyond technology to the patient as a human being. To prevent emotional burnout, healthcare professionals may distance themselves from the patient; however, if patient suffering is acknowledged and addressed, humanized care may be provided. Geographical differences were noted. The humanizing care movement seemed particularly strong in Spain and Brazil sparked by research and political initiatives, whereas papers describing humanizing care in other parts of the world were lacking. However, this lack of publications does not mean that a similar discussion is not warranted or occurring; rather, it may indicate that other concepts, such as patient-centered care, patient involvement, or patient wellbeing, have been in focus.
Patient-centered care has been defined as the provision of care consistent with the patient’s values, needs, and desires. To achieve patient-centered care, health professionals must involve patients in decisions on health care. 59 While patient involvement is necessary for the provision of patient-centered care, patient involvement may reflect a wish to encourage consumerist thinking among those who receive care and a wish for patients to take a more active part in their own care. 60 A taxonomy on patient involvement developed by Thompson 60 linked the level of patient involvement to the level of patient power suggesting that some patients may not have the energy to be involved in healthcare decisions. A scoping review by Olding et al. 61 supports this and shows that more research is needed to understand how patient involvement in the ICU can be practiced given the limitations ICU patients may experience. Thompson 60 identified patient involvement to be codetermined by healthcare professionals and patients. This concept corresponds with the findings of this review, which has identified the attitudes of professionals as pivotal to achieving humanized care.
This review showed that humanized care was often defined as holistic care, which was described in terms of seeing the patient as a whole and taking into account psychosocial and spiritual needs, but no consistent definition of holism was adhered to. Supporting this notion is an editorial by Bullington and Fagerberg 62 that refers to holistic care “a fuzzy concept” and argues that more research is needed. A recent study by Jasemi et al. 63 identified holistic care and patient-centered care as two concepts used interchangeably. However, Jasemi et al. 63 proposed that holistic care should be defined as care for all of the patients’ needs, considering the patient as unique being with the primary objective to provide comfort. Moreover, holistic care should not be limited to the patients’ needs. Importantly, their culture and spiritual needs should be taken into account and holistic care should improve conditions for both patients and healthcare personnel. 63 Consequently, the definition proposed by Jasemi et al. 63 goes well beyond patient-centered care and may be compared to defining humanizing care as an organizational trait toward patients, relatives, and healthcare professionals. Moreover, it shows that the provision of holistic care is closely linked to proficiency and personal growth in healthcare professionals. A similar concept is found in this review, where the importance of overcoming the dehumanizing effects of technology is closely related to nurses’ competencies that allow them to manage and look beyond technology to see patients as fellow human beings.
Todres et al. propose lifeworld perspectives as a “humanizing force” to moderate the grip technological progress holds to processes, systems, and institutions of health care. 64 Lifeworld-led health care seeks to understand what meaning the situation holds to the unique person, provide language to this understanding, and use it to underpin health care for that person. 64 Relating this to the findings of this review, humanized care involves seeing the patient and relative as fellow human beings, providing attention to their needs and their situation and expressing this attention in action and interaction between patients, relatives, healthcare professionals, and healthcare organizations.
Strengths and limitations
Stakeholder consultations validated and nuanced our findings reminding us to broaden our findings to all patients in the ICU regardless of their level of consciousness and ability to communicate with healthcare professionals. Furthermore, stakeholders agreed that acknowledging patients over technology was important to humanize care in the ICU, but that the healthcare organizations including working conditions should be viewed as an equal contributor to humanized care in the ICU.
In this scoping review, a major limitation may be the language inclusion criteria (English and Scandinavian) as our initial search showed a large body of literature in Portuguese and Spanish that was excluded. Nevertheless, we believe that the included papers mirror the general trend in the literature on humanizing intensive care in Spain and Brazil. We did not appraise the quality of evidence of the included studies but rather presented how humanizing intensive care is described in the variety of studies.
Implications and recommendations for practice
We recommend that nurses and other healthcare professionals, organizations, and societies work for holistic and humanized intensive care that involves seeing the patient and relative as fellow human beings, providing attention to their needs and their situation, and expressing this attention in action and interaction between patients, relatives, healthcare professionals, and healthcare organizations. To achieve this, healthcare professionals must receive appropriate training on technology equipment to balance the lifesaving effects of technology with respect for human dignity.
Conclusion
A multitude of perspectives on humanizing intensive care, especially from the Spain and Brazil, reflects a growing interest in humanizing intensive care. To achieve humanized intensive care from the patients’ and relatives’ perspectives, a holistic view of the patient must be reflected in the attitudes of nurses and other healthcare professionals. This implies balancing the lifesaving effects of technology with a greater emphasis on the individual patient and respect for human dignity. Furthermore, humanized intensive care may be enforced by healthcare organizations by establishing humanizing conditions for patients, relatives, and healthcare professionals and by society by setting up a regulatory framework demanding humanized care for patients in the ICU.
Acknowledgments
We are grateful to Veronica Rojas, Research Nurse, Critical Care Unit Hospital Clínico, Universidad de Chile and Member of the HU-CI Project and Gemma Via Clavero, Critical Care Nurse, Hospital Universitari de Bellvitge, Associate Professor, School of Nursing, Faculty of Medicine and Health Sciences, University of Barcelona, Nursing Research Group (GRIN-IDIBELL), Barcelona, and Member of the Proyecto HU-CI for reading and commenting on the manuscript.
Footnotes
Author contributions: All three have contributed to conception and design, analysis and interpretation of data, and drafting the article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Monica Evelyn Kvande https://orcid.org/0000-0003-4384-4695
Sanne Angel https://orcid.org/0000-0001-7669-6743
Anne Højager Nielsen https://orcid.org/0000-0002-8955-9374
References
- 1.Vincent J-L, Slutsky AS, Gattinoni L. Intensive care medicine in 2050: the future of ICU treatments. Intens Care Med 2017; 43: 1401–1402. DOI: 10.1007/s00134-016-4556-4. [DOI] [PubMed] [Google Scholar]
- 2.Vincent J-L, Lefrant J-Y, Lefrant J-Y, et al. Comparison of European ICU patients in 2012 (ICON) versus 2002 (SOAP). Intens Care Med 2018; 44: 337–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valentin A, Ferdinande P, Ferdinande P. Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intens Care Med 2011; 37: 1575. DOI: 10.1007/s00134-011-2300-7. [DOI] [PubMed] [Google Scholar]
- 4.Klepstad P. Intensivmedisinen og dens utfordringer. Tidsskr Den Norske Legeforen 2010; 130: 12. [DOI] [PubMed] [Google Scholar]
- 5.Egerod I, Bergbom I, Lindahl B, et al. The patient experience of intensive care: a meta-synthesis of Nordic studies. Int J Nurs Stud 2015; 52: 1354–1361. [DOI] [PubMed] [Google Scholar]
- 6.Cutler LR, Hayter M, Ryan T. A critical review and synthesis of qualitative research on patient experiences of critical illness. Intens Crit Care Nurs 2013; 29: 147–157. [DOI] [PubMed] [Google Scholar]
- 7.Tsay S-F, Mu P-F, Lin S, et al. The experiences of adult ventilator-dependent patients: a meta-synthesis review. Nurs Health Sci 2013; 15: 525–533. [DOI] [PubMed] [Google Scholar]
- 8.Kvande M, Delmar C, Lykkeslet E, et al. Foresight and awareness of incipient changes in a patient’ clinical conditions - perspectives of intensive care nurses. Intens Crit Care Nurs 2015; 31: 261–268. [DOI] [PubMed] [Google Scholar]
- 9.Kvande M, Delmar C, Lykkeslet E, et al. Assessing changes in a patient’s condition - perspectives of intensive care nurses. Nurs Crit Care 2017; 22: 99–104. [DOI] [PubMed] [Google Scholar]
- 10.Kelly DM, Kutney-Lee A, McHugh MD, et al. Impact of critical care nursing on 30-day mortality of mechanically ventilated older adults*. Crit Care Med 2014; 42: 1089–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arias-Rivera S, Sánchez-Sánchez M. Do Spanish Intensive Care Units Need to Be «humanised»? Enfermeria intensiva 2017; 28(1): 1–3. [DOI] [PubMed] [Google Scholar]
- 12.Kompanje EJO, van Mol MM, Nijkamp MD. ‘I just have admitted an interesting sepsis’. Do we dehumanize our patients? Intens Care Med 2015; 41: 2193–2194. [DOI] [PubMed] [Google Scholar]
- 13.Galvin IM, Leitch J, Gill R, et al. Humanization of critical care-psychological effects on healthcare professionals and relatives: a systematic review. Can J Anesthes 2018; 65: 1348–1371. [DOI] [PubMed] [Google Scholar]
- 14.Alonso-Ovies Á, Heras La Calle G. Humanizar los cuidados reduce la mortalidad en el enfermo crítico. Medicina Intensiva 2020; 44: 122–124. DOI: 10.1016/j.medin.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Corner EJ, Murray EJ, Brett SJ. Qualitative, grounded theory exploration of patients’ experience of early mobilisation, rehabilitation and recovery after critical illness. BMJ Open 2019; 9: e026348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connelly C, Jarvie L, Daniel M, et al. Understanding what matters to patients in critical care: an exploratory evaluation. Nurs Critical Care 2020; 25: 214–220. [DOI] [PubMed] [Google Scholar]
- 17.de la Fuente-Martos C, Rojas-Amezcua M, Gómez-Espejo MR, et al. Humanization in healthcare arises from the need for a holistic approach to illness. Medicina Intensiva 2018; 42: 99–109. DOI: 10.1016/j.medin.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Fontaine DK, Briggs LP, Pope-Smith B. Designing humanistic critical care environments. Crit Care Nurs Q 2001; 24: 21–34. DOI: 10.1097/00002727-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Garrouste-Orgeas M, Périer A, Mouricou P, et al. Writing in and reading ICU diaries: qualitative study of families’ experience in the ICU. PLoS One 2014; 9: e110146. DOI: 10.1371/journal.pone.0110146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silva RCd, Ferreira MdA, Apostolidis T, et al. A conceptual framework of clinical nursing care in intensive care. Rev Lat Am Enferm 2015; 23: 837–845. DOI: 10.1590/0104-1169.0501.2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haque OS, Waytz A. Dehumanization in medicine. Persp Psychol Sci 2012; 7: 176–186. [DOI] [PubMed] [Google Scholar]
- 22.Brown SM, Beesley SJ, Hopkins RO. Humanizing Intensive Care: Theory, Evidence, and Possibilities, Annual Update in Intensive Care and Emergency Medicine 2016. Berlin, Germany: Springer, 2016, pp. 405–420. [Google Scholar]
- 23.Arksey H, O’Malley L. scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8: 19–32. [Google Scholar]
- 24.Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clinical Epidemiology 2014; 67: 1291–1294. [DOI] [PubMed] [Google Scholar]
- 25.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010; 5: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laerkner E, Stroem T, Toft P. No-sedation during mechanical ventilation: impact on patient’s consciousness, nursing workload and costs. Nurs Crit Care 2016; 21: 28–35. [DOI] [PubMed] [Google Scholar]
- 27.Egerod I, Albarran JW, Ring M, et al. Sedation practice in Nordic and non-Nordic ICUs: a European survey. Nurs Crit Care 2013; 18: 166–175. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calle GH, Martin MC, Nin N. Seeking to humanize intensive care. Rev Bra Ter Intensiva 2017; 29: 9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heras La Calle G, Oviés ÁA, Tello VG. A plan for improving the humanisation of intensive care units. Intens Care Med 2017; 43: 547–549. [DOI] [PubMed] [Google Scholar]
- 31.Lopes FM, Brito ES. Humanização da assistência de fisioterapia: estudo com pacientes no período pós-internação em unidade de terapia intensiva. Rev Bra Ter Intensiva 2009; 21: 283–291. DOI: 2009/08/01. [PubMed] [Google Scholar]
- 32.Milani P, Lanferdini IZ, Alves VB. Caregivers’ perception when facing the care humanization in the immediate postoperative period from a cardiac surgery procedure/percepção dos cuidadores frente à humanização da assistência no pós- operatório imediato de cirurgia cardíaca. Rev De Pesquisa Cuidado é Fundam Online 2018; 10: 810–816. DOI: 10.9789/2175-5361.2018.v10i3.810-816. [DOI] [Google Scholar]
- 33.Mondadori AG, Zeni EdM, Oliveira Ad, et al. Humanização da fisioterapia em unidade de terapia intensiva adulto: estudo transversal. Fisioterapia e Pesquisa 2016; 23: 294–300. DOI: 10.1590/1809-2950/16003123032016. [DOI] [Google Scholar]
- 34.Pereira MMM, Germano RM, Câmara AG. Aspects of nursing care in the intensive care unit. J Nurs UFPE 2014; 8: 545–554. DOI: 10.5205/reuol.5149-42141-1-SM.0803201408. [DOI] [Google Scholar]
- 35.Rodriguez‐Almagro J, Quero Palomino MA, Aznar Sepulveda E, et al. Experience of care through patients, family members and health professionals in an intensive care unit: a qualitative descriptive study. Scand J Caring Sci 2019; 33: 912–920. [DOI] [PubMed] [Google Scholar]
- 36.Silveira de Carli B, Ubessi LD, Pettenon MK, et al. The humanization theme in intensive care in health studies. Revista Pesquisa Cuida Fundam 2018; 10. [Google Scholar]
- 37.Page P, Simpson A, Reynolds L. Bearing witness and being bounded: the experiences of nurses in adult critical care in relation to the survivorship needs of patients and families. J Clin Nurs 2019; 28: 3210–3221. [DOI] [PubMed] [Google Scholar]
- 38.dos Santos EL, De Araújo Dórea SN, De Souza Maciel MdPG, et al. Assistência humanizada: percepção do enfermeiro intensivista. Rev Baiana Enferm 2018; 32. DOI: 10.18471/rbe.v32.23680. [DOI] [Google Scholar]
- 39.García Martínez MA, Rebolledo Malpica DM, Pérez Ruiz ME, et al. Bioethical foundations application for practice of critical care in ICU patients. Rev Cubana Invest Biomed 2019; 38: 210–225. [Google Scholar]
- 40.McLean C, Coombs M, Gobbi M. Talking about persons - thinking about patients: an ethnographic study in critical care. Int J Nurs Stud 2016; 54: 122–131. [DOI] [PubMed] [Google Scholar]
- 41.Wilkin K, Slevin E. The meaning of caring to nurses: an investigation into the nature of caring work in an intensive care unit. J Clin Nurs 2004; 13: 50–59. DOI: 10.1111/j.1365-2702.2004.00814.x. [DOI] [PubMed] [Google Scholar]
- 42.Alasad J. Managing technology in the intensive care unit: the nurses’ experience. Int J Nurs Stud 2002; 39: 407–413. [DOI] [PubMed] [Google Scholar]
- 43.McCallum C. Balancing technology with the art of caring. Nurs New Zealand 19952002; 8: 21–23. [PubMed] [Google Scholar]
- 44.Alliex S, Irurita VF. Caring in a technological environment: how is this possible? Contemp Nurse 2004; 17: 32–43. DOI: 10.5172/conu.17.1-2.32. [DOI] [PubMed] [Google Scholar]
- 45.Stayt LC, Seers K, Tutton E. Patients’ experiences of technology and care in adult intensive care. J Adv Nurs 2015; 71: 2051–2061. DOI: 10.1111/jan.12664. [DOI] [PubMed] [Google Scholar]
- 46.Wallis M. Caring and evidence-based practice: the human side of critical care nursing. Intens Crit Care Nurs 2005; 21: 265–267. [DOI] [PubMed] [Google Scholar]
- 47.Silva RCd, Ferreira MdA. Clínica do cuidado de enfermagem na terapia intensiva: aliança entre técnica, tecnologia e humanização. Rev Esc Enferm USP 2013; 47: 1325–1332. DOI: 10.1590/S0080-623420130000600011. [DOI] [PubMed] [Google Scholar]
- 48.Urizzi F, Carvalho LM, Zampa HB, et al. The experience of family members of patients staying in intensive care units. Reva Bras Ter Intensiva 2008; 20: 370–375. DOI: 2008/12/01. [PubMed] [Google Scholar]
- 49.Evangelista VC, Domingos TdS, Siqueira FPC, et al. Equipe multiprofissional de terapia intensiva: humanização e fragmentação do processo de trabalho. Rev Bras Enferm 2016; 69: 1099–1107. DOI: 10.1590/0034-7167-2016-0221. [DOI] [PubMed] [Google Scholar]
- 50.Gibaut MdAM, Hori LMR, Freitas KS, et al. Comfort of the patient’s family in an intensive care unit related to welcoming. Rev Esc Enferm USP 2013; 47: 1114–1121. DOI: 10.1590/S0080-623420130000500015. [DOI] [PubMed] [Google Scholar]
- 51.Medeiros ACd, Siqueira HCHd, Zamberlan C, et al. Comprehensiveness and humanization of nursing care management in the intensive care unit. Rev Esc Enferm USP 2016; 50: 816–822. DOI: 10.1590/S0080-623420160000600015. [DOI] [PubMed] [Google Scholar]
- 52.Fabiane U, Corrêa AK. Relatives’ experience of intensive care: the other side of hospitalization. Rev Lat Am Enferm 2007; 15: 598–604. DOI: 10.1590/s0104-11692007000400012. [DOI] [PubMed] [Google Scholar]
- 53.Facioli A, Amorim FF, de Almeida KJ. A model for humanization in critical care. Perman Jl 2012; 16: 75–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lugarinho M, Castro PPG, Peixoto L. What bothers the patient in an intensive care unit? An interdisciplinary perspective. Intens Care Med 2010; 36: S150. [Google Scholar]
- 55.Alonso-Ovies Á, Heras La Calle G. ICU: a branch of hell? Intens Care Med 2016; 42: 591–592. DOI: 10.1007/s00134-015-4023-7. [DOI] [PubMed] [Google Scholar]
- 56.Debue AS, Kentish-Barnes N. Positive. Perceived obstacles to satisfactory interaction in treating ICU ventilated patients. Intens Care Med 2014; 40: S140. [Google Scholar]
- 57.Escudero D, Viña L, Calleja C. For an open-door, more comfortable and humane intensive care unit. It is time for change. Medicina Intensiva 2014; 38: 371–375. DOI: 10.1016/j.medin.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 58.Fernández-Truillo A, Vallverdú-Cartié H, Román-Maestre B. Care ethics. A new bioethical approach to humanize the ICU. Medicina Intensiva 2016; 40: 511–513. DOI: 10.1016/j.medin.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 59.Constand MK, MacDermid JC, Dal Bello-Haas V, et al. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res 2014; 14: 271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thompson AGH. The meaning of patient involvement and participation in health care consultations: a taxonomy. Soc Sci Med 2007; 64: 1297–1310. [DOI] [PubMed] [Google Scholar]
- 61.Olding M, McMillan SE, Reeves S, et al. Patient and family involvement in adult critical and intensive care settings: a scoping review. Health Expect 2016; 19: 1183–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bullington J, Fagerberg I. The Fuzzy Concept of ‘Holistic Care’: A Critical Examination. Scandinavian Journal of Caring Sciences 2013; 27(3): 493–4. [DOI] [PubMed] [Google Scholar]
- 63.Jasemi M, Valizadeh L, Zamanzadeh V, et al. A concept analysis of holistic care by hybrid model. Ind J Palliat Care 2017; 23: 71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Todres L, Galvin K, Dahlberg K. Lifeworld-led healthcare: revisiting a humanising philosophy that integrates emerging trends. Med Health Care Philosop 2007; 10: 53–63. [DOI] [PubMed] [Google Scholar]