Abstract
The human body has tremendous self-healing capacity and regeneration after injuries and pathogen invasions. These factors are particularly important in older adults which take longer to heal and recover physically. In addition to clinical investigations, perspectives from both experts in the field and the living experiences of the general public could play significant roles to enhance the body’s healing mechanisms in older adults. A semi-structured interview was conducted which included 15 participants (9 experts and 6 older adults aged 65 years and older). Content analysis with an inductive approach was employed about participants’ experiences and perspectives. All participants in this study revealed that self-healing mechanisms can be enhanced through physiological, psychological, and socio-environmental factors. When more of these factors can be integrated into a recovery management plan, it can hasten self-healing in older adults. Social capability has a profound impact on an individual’s mental health while oral health and hygiene significantly affect the nutritional intake status. In regards to physical aspects, regular daily activity patterns, nutritious eating, moderate exercise, and sleep quality are significant, while psychological aspects such as cheerfulness, positive attitudes, and good interpersonal relationships can help control chronic diseases.
Keywords: older adults, healthy aging, recovery management, self-healing
Introduction
For many centuries, medical care was based on observation and logical thinking to treat various diseases. Once medicine became a scientific endeavor and the scientific method became a common practice, mysticism as part of medical treatment gradually faded away (Bynum, 2001; Labisch, 2015). Nosology, which arose in the 18th century directed the medical care system toward physical structure-based medicine, specifically, the various human body systems. Physical examination and the use of pathologic anatomy became the main diagnosis and basis for treatment methods through medical research and later developed into the basic foundation of medical knowledge in the West. Over the past decades, clinical and evidence-based medicine have brought disease examination to molecular and biochemical levels (Lohff, 2001). Currently, the interpretation of wellbeing and disease relies on numbers and values obtained from medical equipment or diagnostic testing which reduces the importance of medical records of patient symptoms and disease presentation (Benjamin, 1967). A rising tide of non-communicable diseases that often originate from lifestyle and poor recovery management practices underlines the importance of lifestyle changes and interventions for geroprotection.
Life expectancy increased by more than 10 years worldwide over the last few decades, yet the proportion of life spent in poor health increased, suggesting that people are suffering from additional chronic illness and disabilities during old age (GBD 2015 DALYs and HALE Collaborators, 2016). Delaying the onset of age-related conditions, especially during crucial early years of life and middle age can result in a long and healthy life many years later (Moskalev et al., 2015). The older population worldwide will substantially increase in the future and so will the disease burden, as older adults are more fragile and take longer to recover. Therefore, a highly important issue for public health worldwide is to take proper measures and initiatives with aiding older adults in the self-healing and recovery management processes.
Illness is a state of unbalance often caused by bad habits, such as eating, sleeping, exercise patterns, pressure from interpersonal relationships or financial concerns, as well as other physiological and psychological factors (Robb, 2006). When certain unfavorable stimulation from the external environment causes illness, the body’s self-healing mechanisms try to return it to a healthy, homeostatic state (Caldwell, 2010; Sturmberg and Carmel, 2013). Hippocrates stated that healing is not the treatment accomplished by a physician but is due to the vis medicatrix naturae (self-healing) within a human body (Mott, 1923; Logan & Selhub, 2012). Self-healing refers to the dynamic equilibrium within the body and extends into the realm of mental health (Thomson, 1914). This intrinsic capacity for self-healing can be improved through behavioral medical approaches, such as hypnosis, biofeedback, exercise, relaxation, imagery, stress regulation, mindfulness practices and nutrition, and a healthy lifestyle (Charlson et al., 2014; Esch, 2020; Loizzo et al., 2009; Offidani et al., 2017; World Health Organization [WHO], 2015). Further, self-healing is the main bridge between treatment and health (Logan & Selhub, 2012). It goes beyond traditional medicine, from back-end disease treatment models to front-end disease prevention and health promotion, and evokes an individual’s power of self-recovery (Humphrey & Skoyles., 2012). For healthy aging, it is important to explore the characteristics of self-healing in terms of how self-healing can help older adults.
By 2025, the estimated older adults population in Taiwan will reach 20% of the total population, making it a “super-aging society” according to the World Health Organization (National Development Council, 2020). A recent survey shows that over 84.7% of Taiwan’s older adults suffer from at least one chronic disease (National Health Research Institutes, 2017). The World Report on Ageing and Health issued by the World Health Organization emphasizes that self-health management is an essential factor in healthy aging.
In addition to physiological and psychological factors, the aging process and life in old age are influenced by social interactions. Social isolation and loneliness; experiencing the death of friends and/or partners; and life transitions, such as retirement and relocation, which cause negative health outcomes and early mortality, have been well documented in various studies (Courtin & Knapp, 2017; Dawson-Townsend, 2019; World Health Organization, 2018). Studies reveal that the important factors influencing health status in older age include social skills, physical activity, nutrition, and oral health. The causes of chronic illnesses are closely correlated with lifestyle (Cruz-Jentoft & Landi, 2014; Dahany et al., 2014; Jankovic et al., 2014). The maintenance of an active lifestyle and regular physical activity in old age can slow down health degeneration and immunity breakdown caused by feelings of loneliness and social isolation (Hutchinson et al., 2009). The optimal way to improve the quality of life of older adults is to maintain their intrinsic healing powers. There are limited international or Taiwan-based studies that focus on self-healing in older adults. This study investigates important factors which promote self-healing and recovery management in older adults through a qualitative approach, by interviewing both healthcare experts and older adults.
Methods
Study Design
A qualitative, semi-structured design was employed, consisting of in-depth interviews 25–40 minutes in duration. Content analysis with an inductive approach was used purposefully to interpret the interviews with participants (Liang et al., 2012).
Study Participants
Stratified convenience sampling using the snowball method was employed. The 15 participants included nine experts in the aging healthcare field including health education, health management, sports, leisure and hospitality management, psychology, aging service management, communication, medicine, and sociology. There were also six older adults aged 65 years and older. The inclusion criteria were those who can communicate in Mandarin or Taiwanese dialects and are independent in daily life/activities without cognitive impairments.
Data Collection and Analysis
The study design was approved by the Institutional Review Board at the university hospital (NTU-REC No:201701ES013). Informed consent was obtained before data collection. All interviewees were notified of their rights and the privacy protection measures. Data were collected through semi-structured, face-to-face, in-depth interviews, which were audio-recorded. The interview guidelines were developed based on the purpose of this research, which was generated by literature reviews and opinions from gerontology specialists, and included the use of open-end responses (Table 1). All interviews were conducted in a private room of a community center and transcribed within 24 hours. For quality and consistency of data collection, the interviewer had qualitative research training and at least 5 years of clinical working experience. Throughout the research process, recordings were used to help with data collection and to present the interview content. Data collection and analysis were conducted simultaneously and main data were consistently presented and described. To ensure reliability, content analysis, coding, and conceptualization were used and integrated into the data analysis.
Table 1.
Interview guide.
| For experts | |
| 1 | Please tell me what health means to you and what do you do for your health in daily life/activities? |
| 2 | How do you regard self-healing power and nature power? |
| 3 | Are you familiar with the dimensions of self-healing? |
| 4 | What do you think are some of the important components of self-healing? |
| 5 | How do you perceive the relationship between the power of self-healing and health conditioning? |
| For older adults | |
| 1 | Please describe what health means to you |
| 2 | What do you do for your health in daily life/activities? |
| 3 | Tell me about your health concerns and what are you doing to improve your health? |
| 4 | What is your interpretation of self-healing power? |
| 5 | Do you think there is a link between self-healing power and the health behaviors you mentioned? Please explain |
Data collection and analysis were conducted simultaneously. Data were analyzed and categorized based on Hu’s theory (Hu, 2008). Content analysis was conducted to thoroughly distinguish differences among self-healing, natural power, and health (Liang et al., 2012). The analysis process started with reading the transcripts in their entirety, then reread to mark the natural transitions in the content. The data were then categorized into a unit of analysis and coded into themes and subthemes based on possible meanings in interviewees. Afterward, 10–15% unit of analysis was reconfirmed or reorganized into categories or themes. Then, peer debriefing was conducted by a second experienced qualitative researcher. Four criteria, namely, credibility, auditability, conformability, and fittingness, were used to evaluate the rigor of the data collection and analysis (Bandura, 1986).
Results
Themes and subthemes were derived from the transcripts. Self-healing included the four main themes of physiology, psychology, spiritual aspects, and interpersonal relations. Physiology included the subthemes of lifestyle, sleeping and eating habits, and chronic illness control. Psychology included the subthemes of positive thinking, emotional pleasure, living in the moment, and self-worth. Interpersonal relations included the subtheme of family, friends, and social networks. The themes comprising opinions from experts and older individuals are displayed in Table 2.
Table 2.■■■.
| Themes | Subthemes | Perspectives | |
|---|---|---|---|
| Health experts | Older adults | ||
| Physiology | Lifestyle | Health lifestyle, balance diet, regular exercise, oral health | Healthy diet, walking |
| Sleep | Sleep | Sleep | |
| Eating habits | Good appetite | ||
| Chronic illness control | Health care management | Chronic disease management | |
| Psychology | Positive thinking | Mindfulness | Optimism |
| Emotional pleasure | Stress management | Stress management | |
| Living in the moment | Learning activity | Education | |
| Self-worth | Self-value | ||
| Spiritual aspect | Spiritual pursue | ||
| Interpersonal relations | Having friends | Intimate relationship | Social interaction |
Sample characteristics
The demographic characteristics of the interviewees, nine experts, and six older adults, are listed in Table 3. The nine experts were between the ages of 38 and 54 years, whereas the six older adults were between the ages of 67 and 83 years old.
Table 3.
The demographic characteristics of the interviewees.
| No | Age | Sex | Education | Marital Status | Employment | Field |
|---|---|---|---|---|---|---|
| Experts | ||||||
| A | 53 | M | Doctoral degree | Married | Professor | Health education |
| B | 42 | F | Doctoral degree | Married | Director | Aging health management |
| C | 54 | M | Doctoral degree | Married | Professor | Sport, leisure, and hospitality management |
| D | 38 | M | Doctoral degree | Married | Professors | Psychology |
| E | 40 | F | Master’s degree | Married | Foundation chief executive | Aging service management |
| F | 50 | F | Master’s degree | Married | Chief executive | Healthcare journal |
| G | 40 | M | Master’s degree | Married | Clinical physician | Medicine |
| H | 48 | F | Master’s degree | Married | Chief executive | Sociology |
| I | 51 | F | Doctoral degree | Married | Professor | Aging service management |
| Older adults | ||||||
| A | 70 | M | Associate’s degree | Married | Security | |
| B | 71 | F | Primary school | Married | Retired | |
| C | 67 | F | High school | Married | Retired | |
| D | 83 | F | Primary school | Married | Retired | |
| E | 67 | F | Primary school | Married | Housekeeper | |
| F | 77 | F | High school | Married | Retired | |
Health Experts
Physiology
Lifestyles
In regards to regular work and daily activities, including exercise and diet management that promote physical health, expert F said, “A good lifestyle consists of exercise, proper care of oneself, eating healthy, enough sleep, drinking plenty of water, no smoking, and little alcohol consumption. . .”
Sleep
In regards to promoting physical health through proper sleep and rest, expert G stated, “Sleep is very important and the best way to recover.” Additionally, expert F said, “Our body can tell us what comes naturally: I want to eat, I want to live and I need to have enough sleep to continue living.”
Eating habits
Based on a daily recommended three-meal diet that focuses on nutritious meals, eating with joy, and eating appropriate amounts expert E stated, “One should not eat too much; that is, he/she should not eat more than three meals a day. In addition, one should also cook his meals.”
Chronic illness control
Expert G stated, “If a person living with a chronic illness adheres to a healthy lifestyle, he can live with a much lower illness impact and burden and perhaps continue to improve and feel better. It is not uncommon for older adults that quit unhealthy habits to feel better as they age.”
Psychology
Positive thinking
Positive thinking can help one to maintain equilibrium when he experiences stress-induced events. Expert B stated, “My thoughts are mostly happy ones. When there is some pressure or problem, I try to find a way to solve it, while maintaining positive thinking.” Expert G said, “I think a positive attitude, an intention to improve yourself, and determination/willpower are important.”
Emotional pleasure
Expert G stated, “Freedom is a higher-level emotion, it’s spiritual. And joy is an emotion that brings a state of wellbeing; to express good emotions brings a pleasant psychological state.”
Living in the moment
Expert F said, “I hope to live well. I hope to live every day the way I want to and to feel fulfilled.”
Self-worth
Expert C expressed, “The ability of older adults to rediscover the value of their life is important in terms of psychological health and overall wellbeing.” Expert E said, “When you know your self-worth and discover the true value of your life, you are more resistant to external effects and various illnesses.”
Spiritual aspects
Self-dialogue
Expert G stated, “When you talk to yourself, you will become better, you will search power within yourself, you will become more confident, and you will feel relieved. Thus, you should do this.” Expert G commented, “Talking to yourself involves a lot of self-reflection as well as thoughts on what and how to improve yourself, and especially how to forgive yourself.”
Interpersonal relations
Having friends
Expert C noted, “Everything gets reversed as one ages. With age, the number of interpersonal relationships decreases from 10 to 9, then to 8, as peers, friends, and relatives pass away and younger people no longer find you interesting or appealing. Eventually, one’s relationships and interactions are often diminished to children, grandchildren, and sometimes great-grandchildren, while interactions with other people are rare.” Expert F said, “One smile or compliment from a family member or an encouraging word from a friend may give you the power to do things, to perceive yourself as healthy and normal, and make you believe that your life has meaning and purpose.”
Older Adults
Older adults defined self-healing as resilience on self to maintain good health, proper stamina, and the leading of a healthy lifestyle to maintain one’s physical and psychological health as well as to reduce the effects of aging. They emphasized three main themes of the self-healing process, physiology, psychology, and interpersonal relations. They referred to exercise as an important aspect of physiology, providing muscle strength, proper sleeping, a healthy appetite, and a means of illness control. Referring to psychology the older adults in our study emphasized letting go of pressure or stress, avoiding conflicts, optimism and openness, the absence of economic concerns, and maintaining good interpersonal relations.
Physiology
Exercise keeps us alive
Aging involves the degeneration of bodily organs and systems, the older adults stated. They expressed there are ways, however, to maintain physiological functions. The aging process can be slowed down through exercise aimed at endurance in particular. They considered exercise to be one of the most effective disease treatment and prevention methods. Participant B said, “I think I’m already exercising when I walk every day.” Participant C stated, “I jog and do stretching exercises which help me stay healthy; my blood pressure, blood sugar, and blood lipid levels are normal.”
Sleep
Participant A stated, “I sleep well. Sleep, particularly sleep quality, is important. Although I hear with age, sleeping time decreases, I go to sleep at 10:30 in the evening and get up at 5:00 in the morning.” Participant D said, “Quality sleep is induced by a great deal of moving around. A person should move around enough in order to sleep enough.”
Eating habits
Participant C said, “When I cook for myself, I use less oil and salt. When I eat out, I dip my food in a bowl of water to wash out the oil and salt. I believe one’s physical state, food intake, and oral health are related and equally important.”
Illness control
Participant C said, “I exercise to keep my blood pressure low.” Participant D noted, “Self-care is a lot more than taking appropriate medicine. One should not just take medicine and refuse to exercise and eat properly.” Participant F commented, “I have high blood pressure now. When I can control it, I am happy.”
Psychological aspects
Letting go of the pressure
Participant C said, “When you’re facing pressure, you’re against yourself. When I have pressure at work, I just have to accept, face, and overcome the challenges I’m faced with.” Participant E comments, “When I feel stress or pressure if I go out and walk for a bit, I feel more relaxed and my mind is at ease.”
Avoiding conflict
Participant A said, “Don’t quarrel with people and don’t hold a grudge; the body and mind will then be naturally healthy.” Participant C noted, “If you don’t argue and fight, you are free, you take care of yourself. Is this not good? There’s no need to blame anyone.”
Optimism and openness
Participant A said, “Health should be about being carefree. Stop being anxious! Then the body will naturally get healthy.” Participant D stated, “I am rarely unhappy. Emotions affect a person’s health. The absence of worries will naturally lighten psychological burdens.”
Economic concerns
Participant F stated, “I am glad that I retired as a government official, and the government supports me. I don’t have to take money from my son. So, I’m content.”
Interpersonal relations
Interactions with family members
Participant D said, “I go to the market myself. I never eat alone. They (family) always take me out.” Participant E noted, “I can’t go out. I have to take care of those two (in-laws). My mother-in-law is already 96. I can’t go far. I feed them, and when they rest, I can go out for a walk. In the morning, I simply can’t go out.”
Having friends
Participant C stated, “If, for example, a classmate or colleague invites me to spend time together, I will go, and I think having friends has a positive impact on my life.” Integrated experts and older adults interview results.
Discussion
This study is preliminary research on self-healing and its findings provide constructive perspectives on the current conceptualization of self-healing between health experts and older adults, respectively. The concept in the biopsychosocial model of self-healing in Table 2 is correlated to the experts and older adults interviewed for the scope of enhancing the process of regaining and maintaining older adult health.
Four main themes, physiology, psychology, spiritual aspects, and interpersonal relations were emphasized in this study. Eating habits, exercise, sleep, and chronic illness control are physiological components, whereas optimism, mindfulness, and stress management are psychological components emphasized by both experts and older adults. Interpersonal relations were detailed by the viewpoints of the experts and older adults in regards to intimate relationships and social interactions. Economic status was regarded as a major concern in older adults; self-value and spiritual satisfaction both were mentioned by experts, however, further research is needed on the effect of these two aspects on the process of self-healing and recovery management.
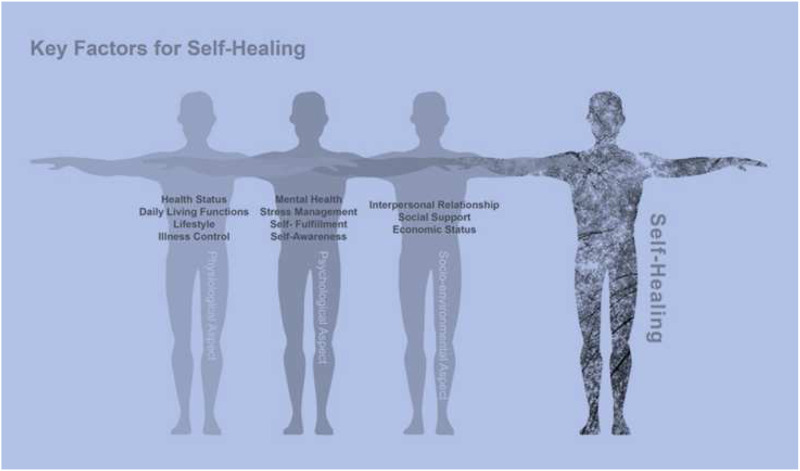
The experts and older adults in our study both considered self-healing or the body’s ability to recover as a very important issue that can be promoted through physiological and psychological factors (Figure 1). Physiological factors include engaging in normal work and rest and controlling chronic illnesses through nutrition, exercise, and sleep. Psychological factors include emotional aspects such as pleasure, positive thinking, and the absence of unnecessary stress and/or negative emotions. Regular, daily interactions with family and friends are great enhancers of physiological and psychological health (Fisher & Lassa, 2017; Hutchinson et al., 2009). The results of the interviews with the experts and older adults in this study were similar in terms of defining the self-healing concept, which refers to related physiological, psychological, and spiritual effects (Kabat-Zinn, 1982). To adapt to and overcome physiological issues, older adults should embrace proper exercise, healthy habits, and limit psychological distress. In addition, they need to have the support of a good public health program and social system (e.g., older adult social programs, friends, family), which can aid older adults with a healthy physical and psychological status and adaptability to gradual or even abrupt aging (Dahany et al., 2014).
Figure 1.
Factors enhancing self-healing. The important factors and aspects that enhance self-healing and management recovery in older adults.
This study found that certain social interactions and/or social environments often affect the mood of older adults (e.g., annoyed by children and youth, annoyed by current politics and state of society). In 2013, The Taiwan Ministry of Health and Welfare conducted a senior citizens survey which indicated that 50% of older adults have a busy social life and societal engagement which play important roles in the wellbeing of older adults. Among their main daily activities, the most important was meeting and talking with friends and family. A cross-sectional survey of older adults aged 65 and older with normal cognitive functions showed that healthy aging included competency of social skills (Dahany et al., 2014).
The results in this study also emphasize that nutrition, regular patterns of daily life, and exercise are important for maintaining one’s intrinsic abilities and delay physical/mental degeneration. Similarly, previous studies have found that regular physical activity, good oral hygiene, and an appetizing, soft food diet can help to compensate for an aging-induced diminished appetite and nutritional intake caused by a reduced smell and taste (Naito et al., 2010; Wu, 2016). A study in which an oral health epidemiological survey among older adults was conducted found that oral health and overall health are closely correlated (Sáez-Prado et al., 2016). Thus, maintaining good oral health is also important besides nutrition.
Relaxing and breathing exercises can additionally improve and alleviate a depressed mental state. For example, meditation could bring about beneficial changes to the body and mind, can improve one’s self-healing capacity, activate the parasympathetic system, and change one’s physiological state (Kabat-Zinn, 1982).
Recommendations from the World Health Organization suggest four layers of a concentric circle (World Health Organization, 2015). The first layer is to strengthen one’s intrinsic capacity or self-healing through the course of life, such as regular exercise, healthy diets, good lifestyles, and cognitive stimulation; the second layer is to stay active both in body and mind by participating in societal roles; the third layer is to establish integrated care based on people with aging in place; the fourth layer is medical care support (Wu, 2016).
This study has several limitations. First, the study is not a completely random sample from the older population in Taiwan. Second, our findings may be limited in the application across different age levels and ethnic groups. The sample is small, and additional research is necessary to build on these practical results and observations to further benefit the public health sector for older adults worldwide.
Conclusions and Practical Implications
A rapid increase of an aging society worldwide is expected in the future which will likely increase burdens on public health and healthcare systems worldwide (Barton, 2014). Therefore, public health sectors should strive to provide and maintain programs that enhance self-healing and recovery management in older adults. Such programs should encourage cooperation among experts and the public in order to benefit and improve older adults’ health. The strategies in enhancing self-healing should promote healthy lifestyles, positive emotional states and also encourage support from relatives and friends to aid older adults in recovering faster and to enhance the management of chronic diseases and the effect can be assessed by a self-healing assessment scale (Hutchinson et al., 2009; Wu, 2016; Wu et al., 2021), moreover, quantitative methods will be used in the future to obtain additional, valuable information about self-healing. The dissemination of the self-healing concept could aid older adults today and in the future, especially for improving recovery management and self-efficacy toward healthy aging, and a reduced illness burden on both individuals and healthcare systems.
Acknowledgments
We would like to express our sincere appreciation to the participants from Cheng-Hsin Hospital in Taiwan for their willingness to share their experiences with us.
Appendix. (Original Version of Questions for Experts and Older Adults in Chinese)
The interview questions for experts (Chinese version)
1. 甚麼是叫健康?包含那些面向?在您的生活落實那些有關健康的行為?
2. 你認為甚麼是Self-Healing Power (自然癒合力) and Nature power(自然力)?(先用英文問定義)
3. 你認為Self-Healing Power (自然癒合力)具備那些面向?
4. 這些面向包含那些內涵?
5. Self-Healing Power (自然癒合力)與健康之間的相關性, 您認為是?
The interview questions for older adults (Chinese version)
1. 你認為什麼叫健康, 健康包含那些層面
2. 你目前對於健康, 落實那些行爲
3. 你目前有那些身體的問題(包含慢性病), 你有那些方法或行爲是針對這些問題來幫助或促進你的健康
4. 自癒能力, 就你目前的了解(字面上), 你的解讀(如果長輩答不出, 可以稍微說, 身體自行修復能力)
5. 就你前面提到健康行爲, 你覺得跟自癒力的連結
Footnotes
Ethics Approval: The study design was approved by the Institutional Review Board at the university hospital (NTU-REC No: 201701ES013).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Daniel L Clinciu https://orcid.org/0000-0001-5272-1414
References
- Bandura A. (1986). Social foundations of thought and action: A social cognitive theory. New Jersey, NJ: Prentice-Hall. [Google Scholar]
- Barton M. K. (2014). Affordable oncologic care: A challenging goal. CA: A Cancer Journal for Clinicians, 64(2), 75–78. https://doi-org.lib.ym.edu.tw/10.3322/caac.21216 [DOI] [PubMed] [Google Scholar]
- Benjamin A. (1967). The principle of totality in choosing the remedy. British Homoeopathic Journal, 56(1): 27–29. https://doi-org/10.1016/S0007-0785(67)80006-1 [Google Scholar]
- Bynum W. F. (2001). Nature’s helping hand. Nature, 414(6859), 21. https://doi-org/10.1038/35102123 [DOI] [PubMed] [Google Scholar]
- Caldwell M. D. (2010). Wound surgery. The Surgical clinics of North America, 90(6), 1125–1132. https://doi-org/10.1016/j.suc.2010.09.001 [DOI] [PubMed] [Google Scholar]
- Charlson M. E., Loizzo J., Moadel A., Neale M., Newman C., Olivo E., Wolf E., Peterson J. C. (2014). Contemplative self healing in women breast cancer survivors: A pilot study in underserved minority women shows improvement in quality of life and reduced stress. BMC Complementary and Alternative Medicine, 14, 349. https://doi-org.lib.ym.edu.tw/10.1186/1472-6882-14-349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtin E., Knapp M. (2017). Social isolation, loneliness and health in old age: A scoping review. Health & Social Care in the Community, 25(3), 799–812. https://doi-org/10.1111/hsc.12311 [DOI] [PubMed] [Google Scholar]
- Cruz-Jentoft A. J., Landi F., Schneider S. M., Zúñiga C., Arai H., Boirie Y., Chen L. K., Fielding R. A., Martin F. C., Michel J. P., Sieber C., Stout J. R., Studenski S. A., Vellas B., Woo J., Zamboni M., Cederholm T. (2014). Sarcopenia. Clinical Medicine (London, England), 43(2), 748–759. https://doi-org/10.7861/clinmedicine.14-2-183 [Google Scholar]
- Dahany M.-M., Dramé M., Mahmoudi R., Novella J.-L., Ciocan D., Kanagaratnam L., Morrone I., Blanchard F., Nazeyrollas P., Barbe C., Jolly D. (2014). Factors associated with successful aging in persons aged 65 to 75 years. European Geriatric Medicine, 5(6):365–370. https://doi-org/10.1016/j.eurger.2014.09.005 [Google Scholar]
- Dawson-Townsend K. (2019). Social participation patterns and their associations with health and well-being for older adults. SSM - Population Health, 8, 100424. https://doi-org/2410.1016/j.ssmph.2019.100424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esch T. (2020). Der Nutzen von Selbstheilungspotenzialen in der professionellen Gesundheitsfürsorge am Beispiel der Mind-Body-Medizin [Self-healing in health-care: Using the example of mind-body medicine]. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz, 63(5), 577–585. https://doi-org/10.1007/s00103-020-03133-8 [DOI] [PubMed] [Google Scholar]
- Fisher R., Lassa J. (2017). Interactive, open source, travel time scenario modelling: Tools to facilitate participation in health service access analysis. International Journal of Health Geographics, 16(1), 13. https://doi-org/10.1186/s12942-017-0086-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 DALYs and HALE Collaborators (2016). Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England), 388(10053), 1603–1658. https://doi-org.lib.ym.edu.tw/10.1016/S0140-6736(16)31460-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y. (2008). Qualitative research: Theories, methods and examples of local and women’s studies in Taiwan. Taipei, Taiwan: Chuliu. [Google Scholar]
- Humphrey N., Skoyles J. (2012). The evolutionary psychology of healing: A human success story. Current Biology: CB, 22(17), R695–R698. https://doi-org.lib.ym.edu.tw/10.1016/j.cub.2012.06.018 [DOI] [PubMed] [Google Scholar]
- Hutchinson T. A., Hutchinson N., Arnaert A. (2009). Whole person care: Encompassing the two faces of medicine. CMAJ: Canadian Medical Association Journal = Journal de l’Association medicale canadienne, 180(8), 845–846. https://doi-org/10.1503/cmaj.081081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankovic N., Geelen A., Streppel M. T., de Groot L. C., Orfanos P., van den Hooven E. H., Pikhart H., Boffetta P., Trichopoulou A., Bobak M., Bueno-de-Mesquita H. B., Kee F., Franco O. H., Park Y., Hallmans G., Tjønneland A., May A. M., Pajak A., Malyutina S., Kubinova R., Amiano P., Kampman E., Feskens E. J. 2014). Adherence to a healthy diet according to the World Health Organization guidelines and all-cause mortality in elderly adults from Europe and the United States. American Journal of Epidemiology, 180(10), 978–988. https://doi-org.lib.ym.edu.tw/10.1093/aje/kwu229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. https://doi-org.lib.ym.edu.tw/10.1016/0163-8343(82)90026-3 [DOI] [PubMed] [Google Scholar]
- Labisch A. (2015). Medicine, history of Western. International Encyclopedia of the Social & Behavioral Sciences, 2(15), 118–125. https://doi-org/10.1016/b978-0-08-097086-8.62121-9 [Google Scholar]
- Liang S. Y., Chuang Y. H., Wu S. F. (2012). Preliminarily application of content analysis to qualitative nursing data. The Journal of Nursing, 59(5), 84–90. https://doi-org/10.6224/JN.59.5.84 [DOI] [PubMed] [Google Scholar]
- Logan A. C., Selhub E. M. (2012). Vis Medicatrix naturae: Does nature “minister to the mind”? BioPsychoSocial Medicine, 6, 11. https://doi-org/10.1186/1751-0759-6-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohff B. (2001). Self-healing forces and concepts of health and disease. A historical discourse. Theoretical Medicine and Bioethics, 22(6), 543–564. https://doi:10.1023/A:1014467523084. [DOI] [PubMed] [Google Scholar]
- Loizzo J., Charlson M., Peterson J. (2009). A program in contemplative self-healing: stress, allostasis, and learning in the Indo-Tibetan tradition. Annals of the New York Academy of Sciences, 1172(1), 123–147. https://doi-org.lib.ym.edu.tw/10.1111/j.1749-6632.2009.04398.x [DOI] [PubMed] [Google Scholar]
- Moskalev A., Chernyagina E., de Magalhães J. P., Barardo D., Thoppil H., Shaposhnikov M., Budovsky A., Fraifeld V. E., Garazha A., Tsvetkov V., Bronovitsky E., Bogomolov V., Scerbacov A., Kuryan O., Gurinovich R., Jellen L. C., Kennedy B., Mamoshina P., Dobrovolskaya E., Aliper A., Kaminsky D., Zhavoronkov A. (2015). Geroprotectors.org: A new, structured and curated database of current therapeutic interventions in aging and age-related disease. Aging, 7(9), 616–628. https://doi-org.lib.ym.edu.tw/10.18632/aging.100799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mott F. W. (1923). An address on the vis mediatrix naturae. Lancet, 202(5231):1171–1220. [Google Scholar]
- Naito M., Kato T., Fujii W., Ozeki M., Yokoyama M., Hamajima N., Saitoh E. (2010). Effects of dental treatment on the quality of life and activities of daily living in institutionalized elderly in Japan. Archives of Gerontology and Geriatrics, 50(1), 65–68. https://doi-org.lib.ym.edu.tw/10.1016/j.archger.2009.01.013 [DOI] [PubMed] [Google Scholar]
- National Development Council . (2020). Population estimation of the Republic of China (2020-2070 year). https://www.ndc.gov.tw/Content_List.aspx?n=6EA756F006B2A924 [Google Scholar]
- National Health Research Institutes (2017). National Health Interview survey. https://www.hpa.gov.tw/Pages/ashx/File.ashx?FilePath=∼/File/Attach/13636/File_15832.pdf [Google Scholar]
- Offidani E., Peterson J. C., Loizzo J., Moore A., Charlson M. E. (2017). Stress and response to treatment: Insights from a pilot study using a 4-week contemplative self-healing meditation intervention for posttraumatic stress in breast cancer. Journal of Evidence-Based Complementary & Alternative Medicine, 22(4), 715–720. https://doi-org.lib.ym.edu.tw/10.1177/2156587217708522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robb W. J. (2006). Self-healing: A concept analysis. Nursing Forum, 41(2), 60–77. https://doi-org/10.1111/j.1744-6198.2006.00040.x [DOI] [PubMed] [Google Scholar]
- Sáez-Prado B., Haya-Fernández M. C., Sanz-García M. T. (2016). Oral health and quality of life in the municipal senior citizen’s social clubs for people over 65 of Valencia, Spain. Medicina Oral, Patologia Oral Y Cirugia Bucal, 21(6), e672–e678. https://doi-org.lib.ym.edu.tw/10.4317/medoral.21305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturmberg J. P., Carmel M. (2013). Handbook of systems and complexity in Health. New York, NY: Springer. [Google Scholar]
- Thomson J. A. (1914). The popular lecture: vis medicatrix naturae. The British Medical Journal, 2, 2797:277–279. https://doi-org/10.1136/bmj.2.2797.277 [Google Scholar]
- World Health Organization . (2015). World Report on ageing and Health. Geneva, Switzerland: World Health Organization. [Google Scholar]
- World Health Organization . (2018). Ageing and health. Available at: https://www.who.int/news-room/fact-sheets/detail/ageingand-health [Google Scholar]
- Wu H. C. (2016). Comprehensive care service improving promotion of health and quality of life in older adults. Public Governance Quarterly, 4(1):43–52. [Google Scholar]
- Wu Y.-C., Hsu H.-I., Tung H.-H., Pan S.-J., Lin S.-W. (2021). Psychometric properties of the self-healing assessment scale for community-dwelling older adults. Healthcare (Basel, Switzerland), 9(4), 484. https://doi-org/10.3390/healthcare9040484 [DOI] [PMC free article] [PubMed] [Google Scholar]