Abstract
Rationale:
Nondilated obstructive uropathy (NDOU) is a rare cause of acute renal failure reported in less than 5% of cases of obstructive uropathy. It is typically associated with intrapelvic malignancies and diseases causing retroperitoneal lymphadenopathy and retroperitoneal fibrosis. As these conditions may prevent radiographic dilation of the collecting system, the diagnosis of NDOU may be missed by usual diagnostic testing.
Presenting concerns of the patient:
We present a case of acute anuric renal failure in a middle-aged woman with metastatic breast cancer associated with abdominal and retroperitoneal lymphadenopathy. Acute kidney injury was initially deemed secondary to drug-induced acute tubular necrosis (ATN) from bisphosphonate; however, there remained a high clinical suspicion of NDOU due to the presence of enlarged retroperitoneal lymph nodes on CT abdomen and pelvis with concerns for encasement of bilateral renal pelvic regions and ureters.
Diagnoses:
The patient underwent a retrograde pyelogram which demonstrated questionable narrowing bilaterally at the level of the renal pelvices. This led to an even stronger clinical suspicion of NDOU and urology service was consulted for evaluation.
Intervention:
Bilateral ureteral stents were placed by urology which led to robust urine output and rapid reversal of renal failure over the next 24 to 48 hours.
Outcomes:
Despite 2 weeks of anuria and hemodialysis, this patient’s creatinine came back to her baseline. She was able to discontinue hemodialysis and her creatinine stabilized at 88.4 μmol/L (1 mg/dL).
Teaching points:
Nondilated obstructive uropathy is rare but important diagnosis that requires a high clinical suspicion in the appropriate clinical scenario. The lack of dilatation is believed to be related to encasement of the collecting system by tumor, fibrosis, or as in our case metastatic retroperitoneal lymphadenopathy. As this diagnosis cannot be overlooked, aggressive direct visualization or even intervention with internal or external stenting may be required to both diagnose and treat this condition.
Keywords: acute kidney injury, obstructive uropathy, acute tubular necrosis, retroperitoneal lymphadenopathy
Abrégé
Justification:
L’uropathie obstructive sans dilatation (UOSD) est une cause rare d’insuffisance rénale aiguë (IRA) rapportée dans moins de 5 % des cas d’uropathie obstructive. Elle est généralement associée à des tumeurs malignes intrapelviennes et de maladies entraînant une lymphadénopathie rétropéritonéale et une fibrose rétropéritonéale. Ces conditions pouvant empêcher la dilatation radiographique du système collecteur, il arrive que le diagnostic de l’UOSD soit manqué lors des tests de diagnostic habituels.
Présentation du cas:
Nous présentons un cas d’IRA anurique chez une femme d’âge moyen atteinte d’un cancer du sein métastatique associé à une lymphadénopathie abdominale et rétropéritonéale (LAR). L’IRA avait initialement été considérée comme secondaire à une nécrose tubulaire aiguë induite par le bisphosphonate. La présence de ganglions lymphatiques rétropéritonéaux hypertrophiés sur la tomographie de l’abdomen et du bassin a toutefois soulevé un doute clinique d’UOSD; une obstruction des régions bilatérales du bassinet rénal et des uretères a été soupçonné.
Diagnostic:
La patiente a subi un pyélogramme rétrograde qui a montré un rétrécissement bilatéral suspect au niveau des bassinets rénaux, ce qui a soulevé un doute clinique encore plus important quant à la présence d’une UOSD. Le service d’urologie a été consulté pour évaluation.
Intervention:
Des endoprothèses urétérales ont été insérées bilatéralement par urologie. L’intervention a entraîné une forte production d’urine et la disparition de l’insuffisance rénale dans les 24 à 48 heures suivantes.
Résultats:
Malgré deux semaines d’anurie et d’hémodialyse, le taux de créatinine de la patiente est retourné à sa valeur initiale. La patiente a pu interrompre l’hémodialyse et son taux de créatinine s’est stabilisé à 88,4 micromoles/L (1 mg/dl).
Enseignements tirés:
Le diagnostic de l’UOSD est rare, mais important, car il requiert un doute clinique élevé dans le scénario clinique approprié. On pense que l’absence de dilatation pourrait être liée à l’obstruction du système collecteur rénal par une tumeur ou en raison d’une fibrose ou, comme ici, d’une lymphadénopathie rétropéritonéale métastatique. Puisque le diagnostic de l’UOSD ne doit pas être négligé, une visualisation directe plus poussée et l’insertion d’une endoprothèse interne ou externe pourraient s’avérer nécessaires pour diagnostiquer et traiter cette affection.
Introduction
Acute kidney injury (AKI) can be broadly classified into prerenal, renal, and postrenal etiologies. Evaluation of AKI with imaging is typically recommended in all cases of AKI unless there is an otherwise obvious etiology other than obstructive uropathy. Diagnostic evaluation for urinary obstruction is usually done with a renal ultrasound and is recommended within 12 hours in cases of suspected obstruction. 1 Both renal ultrasound and computed tomographic (CT) scanning are cost-effective, noninvasive methods of evaluating a patient for obstructive uropathy by looking for the presence of hydronephrosis or hydroureter. However, although highly sensitive (93%) and specific (100%), noninvasive imaging with renal ultrasound cannot rule out obstruction with complete certainty, 2 especially in patients with volume depletion or early hydronephrosis. Some retroperitoneal processes can encase the kidneys or ureters and cause AKI through either complete or partial obstruction of urinary flow, without allowing the collecting system to dilate. This is termed nondilated obstructive uropathy (NDOU) and is a rare subtype of postrenal AKI accounting for <5% of total cases. 3 Over the course of the last several years, it has been increasingly recognized in the literature. Approximately 60% of NDOU cases are associated with an intrapelvic malignancy 4 ; other reported but less common causes include retroperitoneal fibrosis and retroperitoneal lymphadenopathy from a number of processes. As clinicians generally rely on renal ultrasound or CT in the screening for obstructive uropathy, the consideration for NDOU in a patient with AKI requires a high index of suspicion, the cornerstone in making a timely diagnosis. The diagnosis of NDOU usually requires cystoscopy and retrograde pyelography and thus depends upon close collaboration with the nephrologist and urologist.
Case Presentation
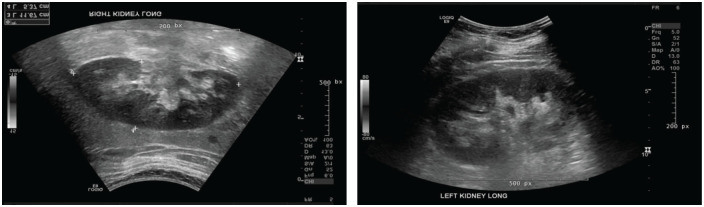
We present a case of a middle-aged woman with a past medical history significant for hormone receptor–positive invasive breast cancer. She also had biopsy-proven metastasis to the retroperitoneal lymph nodes evident on imaging. She was started on chemotherapy with fulvestrant along with intravenous zoledronic acid (ZA) due to bony metastasis. At the time of initiation of chemotherapy, her baseline serum creatinine (sCr) was 53.04 μmol/L (0.6 mg/dL). One month after she received ZA, her serum Cr increased up to 114.9 μmol/L (1.3 mg/dL). She noted decreased urine output with new-onset abdominal pain. Renal ultrasound (Figures 1A and 1B) and CT imaging at this point showed no evidence of hydronephrosis. Her urinalysis was benign. She initially received intravenous fluids without any improvement in sCr and repeat renal ultrasound was unremarkable for any obstructive cause despite volume repletion. However, she eventually became anuric and hemodialysis was initiated. Her AKI was postulated to be ATN from bisphosphonate use. A renal biopsy was felt to be contraindicated because she was on systemic anticoagulation for deep venous thromboses. She was discharged on hemodialysis (HD). Despite the potential explanation of ATN from ZA for the AKI, there was a high clinical suspicion for NDOU due to her anuria in the presence of enlarged retroperitoneal lymph nodes on CT abdomen and pelvis with concerns for encasement of bilateral renal pelvic regions. A bilateral retrograde pyelogram was performed 2 weeks after discharge (while on HD). While the pyelogram showed no clear evidence of obstruction, there were questionable areas of mild ureteral segmental narrowing which in conjunction with enlarged retroperitoneal lymph nodes on CT scan led to suspicion of NDOU and therefore bilateral ureteral stents were placed empirically by urologist.
Figure 1.
Ultrasound of (A) left kidney (B) right kidney without overt hydronephrosis.
Outcome
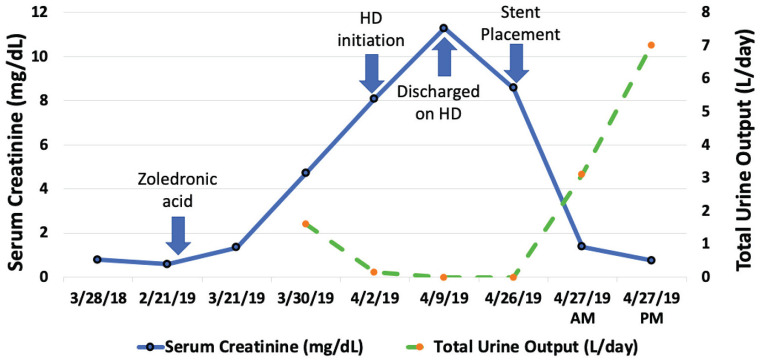
There was an immediate diuresis with an average urine output of 300 mL/h over the next 24 to 36 hours with significant improvement of renal functions (Figure 1). Her sCr improved from 760 μmol/L (8.6 mg/dL) to 70.7 μmol/L (0.8 mg/dL) over the next 24 hours and she remained off hemodialysis thereafter (Figure 2). Although ZA-related ATN was initially suspected, it would be highly speculative to consider ATN resolution at exactly the same time as of stent placement. Furthermore, the marked increase in urine output consistent with a “postobstructive diuresis” and the immediate drop in sCr to this degree after stenting further supported that the AKI was from an obstructive etiology. Of note, prior to stent placement, patient had not received dialysis for almost 72 hours and therefore was volume overloaded and azotemic with blood urea nitrogen (BUN) of 23.57 mmol/L (66 mg/dL). The BUN decreased to 5.71 mmol/L (16 mg/dL) within 24 hours of stenting and we suspected a solute diuresis (both Na and urea) was contributing to the postobstructive diuresis. She was managed with 0.45% normal saline and allowed to drink to her thirst without any hypernatremia on subsequent labs.
Figure 2.
Patient’s clinical course.
Follow-Up
Her hospital course was complicated by ischemic stroke. She subsequently opted for comfort care due to advanced malignancy and an overall guarded prognosis. However, she remained off dialysis until she passed away.
Discussion
Obstructive uropathy is one of the major reversible causes of AKI. Imaging of both upper and lower urinary tract with noninvasive techniques of renal ultrasound and abdominal CT scan has been traditionally used to delineate the site of obstruction. Both imaging modalities are very sensitive to visualize even minimal dilation in the urinary tract. However, approximately 5% of cases of obstructive uropathy will present without any objective evidence of pelviceal, calyceal, or ureteral dilation on conventional imaging. 3 Although rare, an increasing number of NDOU cases are being reported. Onuigbo et al demonstrated 3 cases of NDOU within the short span of 6 months. 3 This alludes to the fact the NDOU might be more common than currently speculated, as it can be easily missed.
Most of the cases are seen in the setting of intrabdominal malignancy or retroperitoneal fibrosis. 5 In NDOU associated with pelvic malignancies, it remains unclear whether some of those cases truly represented NDOU or were nondilated obstructed because uropathy versus having “false-negative” imaging study as these individuals with advanced malignancies are more likely to be malnourished and volume depleted with the volume depletion masking the obstruction.
A small number of cases have been reported in conjunction with conditions such as nephrolithiasis and pyelonephritis. 6 In most of these clinicopathological conditions, imaging with antegrade/retrograde pyelogram will make the diagnosis. In a few case reports, NDOU was not evident even with contrast renography, and surgical exploration with nephrostomy tube placement was required to make the diagnosis. 7 False-negative imaging can be due to decreased ureteral peristalsis with encasing retroperitoneal fibrosis or tumor, small size of renal pelvis, 8 very early stages of hydronephrosis, in volume-depleted patients. 9
In our case, we initially had a plausible explanation of intravenous ZA as being responsible for the patient’s AKI. Exact incidence of ATN from intravenous ZA is not known. According to one study AKI was observed in approximately 9.3% of subjects who received 4 mg of ZA for the treatment of skeletal metastases in patients with breast cancer or osteolytic lesions of multiple myeloma. 10 A review of FDA Adverse Event Reporting System from August 2001 to March 2003 identified around 72 cases of intravenous ZA-induced ATN. 11 Most of them had also had underlying malignancies. Twenty-five percent of these patients received only one dose of ZA and had renal failure after an average of 11 days. 11 This is compatible with our case; however, anuria is unusual for ATN. That and the patient’s history of retroperitoneal involvement of her malignancy led to further urologic evaluation that provided the diagnosis and successful treatment of her NDOU. It is remarkable that despite 2 weeks of anuria and hemodialysis, this patient’s creatinine came back to her baseline!
Surgical management primarily encompasses the insertion of ureteral stents or percutaneous nephrostomy tubes. 12 Appropriate decompression leading to renal salvage can be very rewarding in any case of AKI from urinary obstruction, but especially so in NDOU. As incidence of NDOU is still quite low, the suspecting clinician may find it difficult to convince other physician team members (urology or interventional radiology) to pursue furthermore definitive diagnostic studies, despite their invasive nature. However, one must also keep in mind the significant risk of recurrent malignant obstruction with poor prognosis especially in advanced cases of cancers. 13 Overall prognosis and goals of cares must be assessed prior to subjecting patients to any intervention in these particular cases.
While rare, NDOU should always be considered in the appropriate clinical context of AKI and when suspected requires direct communication with our urologic or interventional radiology colleagues to pursue this reversible cause of AKI.
Learning Points
Nondilated obstructive uropathy is rare but important diagnosis that requires a high clinical suspicion in the appropriate clinical scenario.
The lack of dilatation in NDOU is related to encasement of the collecting system by tumor or fibrosis.
Both renal ultrasound and CT can be false-negative in early hydronephrosis and in volume-depleted individuals as well and a repeat ultrasound should be considered after correction of volume repletion to exclude false-negative imaging.
Nondilated obstructive uropathy cannot be overlooked and aggressive direct visualization or intervention with internal or external stenting may be required to both diagnose and treat this condition.
Footnotes
Ethics Approval and Consent to Participate: Ethics approval for participation and publication was taken from the Department of Nephrology, Rush University Medical Center since the patient is herself deceased; exhaustive attempts were made to reach the family without any avail. Paper was sufficiently anonymized not to cause harm to patient’s family.
Consent for Publication: Consent for publication was provided by all authors.
Availability of Data and Materials: The data that support the findings of this study are available from the corresponding author, M.A.S, upon reasonable request.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Muhammad Asim Shahzad  https://orcid.org/0000-0003-1729-8520
https://orcid.org/0000-0003-1729-8520
References
- 1. National Clinical Guideline Centre (UK). Acute Kidney Injury: Prevention, Detection and Management Up to the Point of Renal Replacement Therapy. London, England: Royal College of Physicians (UK); 2013. [PubMed] [Google Scholar]
- 2. Ather MH, Jafri AH, Sulaiman MN. Diagnostic accuracy of ultrasonography compared to unenhanced CT for stone and obstruction in patients with renal failure. BMC Med Imaging. 2004(4):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Onuigbo MA, Lawrence K, Onuigbo NT. Non-dilated obstructive uropathy—an unrecognized cause of acute renal failure in hospitalized US patients: three case reports seen over 6 months in a northwestern Wisconsin nephrology practice. Ren Fail. 2010;32(10):1226-1229. [DOI] [PubMed] [Google Scholar]
- 4. Kocurek JN, Orihuela E, Saltzstein DR. Nondilated obstructive uropathy and renal failure as a result of carcinoma of the intrapelvic area. Surg Gynecol Obstet. 1991;173(6):470-472. [PubMed] [Google Scholar]
- 5. Spital A, Valvo JR, Segal AJ. Nondilated obstructive uropathy. Urology. 1988;31(6):478-482. [DOI] [PubMed] [Google Scholar]
- 6. Ashmore AE, Thompson CJ. Pyelonephritis and obstructive uropathy: a case of acute kidney injury. Case Reports. 2016;2016:bcr2015212028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rascoff JH, Golden RA, Spinowitz BS, Charytan C. Nondilated obstructive nephropathy. Arch Intern Med. 1983;143(4):696-698. [PubMed] [Google Scholar]
- 8. Lyons K, Matthews P, Evans C. Lesson of the week: obstructive uropathy without dilatation: a potential diagnostic pitfall. Br Med J (Clin Res Ed). 1988;296(6635):1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ghani AR, Gronich J, Hamid M. Does absence of hydronephrosis rules out obstruction as an etiology of ARF? Int J Collab Res Intern Med Public Health. 2017;9(5):692-693. [Google Scholar]
- 10. Rosen LS, Gordon D, Kaminski M, et al. Zoledronic acid versus pamidronate in the treatment of skeletal metastases in patients with breast cancer or osteolytic lesions of multiple myeloma: a phase III, double-blind, comparative trial. Cancer J. 2001;7(5):377-387. [PubMed] [Google Scholar]
- 11. Chang JT, Green L, Beitz J. Renal failure with the use of zoledronic acid. New Eng J Med. 2003;349(17):1676-1679. [DOI] [PubMed] [Google Scholar]
- 12. Naidich JB, Rackson ME, Mossey RT, Stein HL. Nondilated obstructive uropathy: percutaneous nephrostomy performed to reverse renal failure. Radiology. 1986;160(3):653-657. [DOI] [PubMed] [Google Scholar]
- 13. Wong LM, Cleeve LK, Milner AD, Pitman AG. Malignant ureteral obstruction: outcomes after intervention. Have things changed? J Urol. 2007;178(1):178-183. [DOI] [PubMed] [Google Scholar]