ABSTRACT
HEARTS in the Americas is the regional adaptation of the World Health Organization’s Global Hearts Initiative, which will be the model for risk management for cardiovascular disease (CVD) in primary health care in the Region of the Americas by 2025. It has already been implemented in 21 countries and 1045 primary health care centers throughout Latin America and the Caribbean. It takes a public health and health systems approach to systematically introduce simplified interventions at the primary health care level and focuses on hypertension as a clinical entry point. This paper introduces a new, improved application (app), the main component of which is the calculator for CVD risk and hypertension management. The paper summarizes the risk assessment approach and the methodology used by the World Health Organization to update its cardiovascular risk charts in 2019; describes the app, its use, functionality and validation process; and provides a set of practical recommendations for optimizing CVD risk and hypertension management by using the app in clinical practice. The HEARTS app is a powerful tool to improve the quality of care provided in primary health settings. The creation and dissemination of the HEARTS app is an essential step in the journey towards eliminating preventable CVD in the Americas.
Keywords: Heart disease risk factors, hypertension, medical informatics applications
RESUMEN
HEARTS en las Américas es la adaptación regional de la Iniciativa Global Hearts de la Organización Mundial de la Salud, que será el modelo para el manejo del riesgo de la enfermedad cardiovascular (ECV) en la atención primaria de la salud en la Región de las Américas para el año 2025. Ya se ha implementado en 21 países y 1045 centros de atención primaria de salud en toda América Latina y el Caribe. Adopta un enfoque de salud pública y sistemas de salud para introducir sistemáticamente intervenciones simplificadas en el nivel de atención primaria de salud y se centra en la hipertensión como punto de entrada clínico. En este artículo se presenta una aplicación (app) nueva y mejorada cuyo componente principal es la calculadora de riesgo de ECV y de manejo de la hipertensión. Se resume el enfoque de evaluación del riesgo y la metodología utilizada por la Organización Mundial de la Salud para actualizar sus tablas de riesgo cardiovascular en 2019; se describe la app, su uso, su funcionalidad y su proceso de validación; y se proporciona un conjunto de recomendaciones prácticas para optimizar el manejo del riesgo de ECV y de la hipertensión mediante el uso de la app en la práctica clínica. La app HEARTS es una herramienta robusta para mejorar la calidad de la atención prestada en los centros de atención primaria. La creación y difusión de la aplicación HEARTS es un paso esencial en el camino hacia la eliminación de la ECV prevenible en las Américas.
Palabras clave: Factores de riesgo de enfermedad cardíaca, factores de riesgo, hipertensión, aplicaciones de la informática médica
RESUMO
HEARTS nas Américas é a adaptação regional da Iniciativa Global Hearts da Organização Mundial da Saúde, que será o modelo para o gerenciamento de risco de doenças cardiovasculares (DCV) na atenção primária à saúde na Região das Américas até 2025. Ele já foi implementado em 21 países e 1045 centros de saúde primária em toda a América Latina e Caribe. Adota uma abordagem de saúde pública e sistemas de saúde para introduzir sistematicamente intervenções simplificadas no nível da atenção primária à saúde e concentra-se na hipertensão como um ponto de entrada clínica. Este documento introduz uma nova e melhor aplicação (app), cujo principal componente é a calculadora de risco de DCV e gerenciamento de hipertensão. O artigo resume a abordagem de avaliação de risco e a metodologia usada pela Organização Mundial da Saúde para atualizar seus gráficos de risco cardiovascular em 2019; descreve o aplicativo, seu uso, funcionalidade e processo de validação; e fornece um conjunto de recomendações práticas para otimizar o gerenciamento do risco de DCV e da hipertensão, usando o aplicativo na prática clínica. O aplicativo HEARTS é uma ferramenta potente para melhorar a qualidade dos cuidados prestados em ambientes de saúde primária. A criação e disseminação do aplicativo HEARTS é um passo essencial para eliminar a DCV evitável nas Américas.
Palavras-chave: Fatores de risco de doenças cardíacas, fatores de risco, hipertensão, aplicações da informática médica
Despite decades of remarkable progress, cardiovascular disease (CVD) remains the leading disease burden in the Region of the Americas, accounting for one third of all deaths and producing substantial adverse economic and social impacts. Indeed, a study estimated that in 2017 there were 14 million new cases of CVD, 80 million people living with CVD and 2 million deaths from CVD. In addition, a slowdown in premature mortality from CVD was detected during 2007–2013, but this was followed by stagnation during 2013–2017 in almost all countries of the Region (1).
The CVD crisis is consistent with the high prevalence of its main risk factors at population level: more than 60% of people in the Region are overweight or obese; 20% have raised blood pressure; on average, 9 g of salt are consumed per day; 8% have raised blood glucose; and 15% use tobacco (2). In parallel, our lack of capacity to provide adequate care for people with hypertension is apparent. For instance, despite progress, the control of hypertension – which is the the leading risk factor for CVD – is unacceptably poor (3). There are many determinants of CVD, but central determinants are a health system’s failure to identify people at risk, secure access to quality medicines and meet accepted standards of care.
To respond to these challenges, the World Health Organization’s (WHO’s) Global Hearts Initiative for CVD prevention and control has been implemented in the Region via HEARTS in the Americas, an initiative led by ministries of health and supported by the Pan American Health Organization and other partners, including the U.S. Centers for Disease Control and Prevention and Resolve to Save Lives, a global public health initiative. This initiative is active in 21 countries and 1045 primary health centers throughout Latin America and the Caribbean. It takes a public health and health systems approach to systematically introduce simplified interventions at the primary health care level and focuses on hypertension as a clinical entry point. HEARTS in the Americas will be the model for CVD risk management in primary health care in the Region by 2025 (4).
This paper introduces the new, improved application (app), the main component of which is a calculator that can help optimize CVD risk assessment and hypertension management. First, the paper summarizes the risk assessment approach and the methods used to update WHO’s cardiovascular risk charts in 2019 (5). Then the app, its use, functionality and validation process are described, and a set of practical recommendations are provided for optimizing risk assessment by using the calculator in clinical practice.
RISK ASSESSMENT APPROACH
Poor control of CVD risk factors results from a lack of awareness among individuals of their risk status. Therefore, health care providers are essential to identifying risk levels as a means of detecting those at high risk of CVD and identifying who could benefit from treatment for raised blood pressure, abnormal blood lipids and raised blood glucose (6). Recommendations for assessing and managing such risk factors have evolved in CVD guidelines. This evolution is a response to an improved ability to identify those at highest risk, the increase in the population affected by these risk factors, changes in generic therapies available and a recognition that despite these changes, we are failing globally to prevent CVD, particularly in low- and middle-income countries.
One change in hypertension guidelines has been the greater use of overall CVD risk levels to determine the therapeutic goal and intensity of treatments. The additional focus on overall risk has occurred for three main reasons. First, there was recognition that individuals who may have multiple risk factors, even if each risk factor is only moderately elevated, may be at high risk overall compared with someone who has only an isolated elevated risk factor and who may be at relatively low risk overall. For example, a middle-aged woman with several moderate-level risk factors could have a 5- to 10-fold increased risk of having CVD in 10 years compared with a young man with a single elevated risk factor. Second, targeting those who have the highest risk was recognized to lead to greater efficiency in benefit in terms of the number of events avoided. Thus, relative risk reduction would be applied to a higher baseline risk (7). Likewise, assigning fewer individuals who were at low baseline risk to more intensive treatment preserves limited resources and minimizes side-effects among a group who will have only limited benefit from treatment. Therefore, targeting patients at high risk of CVD is the most critical priority in a risk stratification approach (8). Third, improved computing and statistical methods have allowed researchers to pool large global data sets to create more accurate risk prediction tools for various populations.
Moreover, as the cost of medicines is a significant component of the total cost of preventive health care, it is crucial to base treatment decisions about medicines principally on an individual’s risk level and less on criteria such as the ability to pay or on blanket preventive strategies. In addition, when treating the same number of patients, guidelines that are based on total CVD risk and use risk-scoring methods are less expensive and more effective than guidelines based on single risk factors (7). Finally, a risk stratification approach is particularly suited to settings with limited resources, where saving the greatest number of lives at the lowest cost becomes imperative.
WHO 2019 CARDIOVASCULAR RISK CHARTS
WHO updated the 2007 WHO–International Society of Hypertension cardiovascular risk prediction charts (5) by forming a cross-sectoral collaboration of academics, policymakers and end-users of CVD risk scores. The revision of the model took place in three steps.
First, risk prediction algorithms were developed using individual participant data from 376 177 patients from 85 prospective cohort studies that had long-term follow up in the Emerging Risk Factors Collaboration. The 10-year risks for fatal and non-fatal CVD outcomes were assessed. The risk factors used in the prediction models were age, sex, smoking status, systolic blood pressure, diabetes, total cholesterol and body mass index (BMI). Second, to adjust the algorithms to contemporary circumstances in different global regions, they were recalibrated using age-specific and sex-specific incidence rates and risk factor values obtained from the Global Burden of Disease (GBD) Study and the Noncommunicable Disease Risk Factor Collaboration. Third, the performance of the algorithms was assessed by external validation using individual participant data from a further 19 prospective cohort studies (i.e. studies distinct from those used in the algorithm derivation).
The updated WHO CVD risk charts (5) were developed for 21 global regions defined by the GBD study to maximize between-region variability and minimize heterogeneity in mortality and major drivers of health outcomes within each region. The WHO charts are intended to allow for the introduction of a total-risk stratification approach for CVD management. The updated WHO CVD risk charts are presented as laboratory-based and non-laboratory-based. Laboratory-based algorithms include age, sex, smoking status, systolic blood pressure, history or evidence of diabetes mellitus, and total cholesterol. Non-laboratory-based algorithms include BMI; information about diabetes mellitus and cholesterol is unnecessary for these charts.
The risk stratification for the updated charts differs from that used in the 2007 charts in recognition of changes in reported CVD incidence in the GBD study. The new stratification is: <5% 10-year CVD risk (denoted in green), 5% to <10% risk (yellow), 10% to <20% risk (orange), 20% to <30% risk (red) and ≥30% risk (dark red). The category >40% is not retained because there are only very few people in it. This risk stratification scheme is aligned with WHO’s recommendations for the management of CVD risk. Countries can find the relevant charts by using the appropriate GBD regional charts.
HEARTS IN THE AMERICAS RISK CALCULATOR
HEARTS in the Americas transformed the 2019 WHO CVD risk charts (5) into an online electronic calculator, updating the previous 2014 CardioCal app (9). The new app can be downloaded for free at the HEARTS in the Americas website (https://www.paho.org/en/hearts-americas/cardiovascular-risk-calculator-app). It is trilingual (Spanish, Portuguese and English) and available for mobile devices with Android or iOS software. The app is intended to be used in clinical practice, especially at the primary health care level. However, it can also be used by anyone in the general population who is interested in knowing their cardiovascular risk.
The app includes an easy-to-use tutorial, clear messages on risk estimates, clinical recommendations and estimates of the expected effect of modifying traditional risk factors on the risk of CVD. The main component of the app is the CVD risk calculator. Like the 2014 CardioCal app, this app includes calculation of BMI and the glomerular filtration rate based on creatinine values, both of which are relevant for the comprehensive assessment of CVD risk. Notably, this app incorporates the specific, standardized hypertension treatment protocols defined by ministries of health in the countries implementing HEARTS that have these protocols; for countries that have not yet adopted protocols, it includes the generic protocols from the HEARTS technical package. Furthermore, the app includes recommendations for optimizing the assessment of CVD risk for primary and secondary prevention, a brief video describing the technical aspects of obtaining accurate blood pressure measurements and advice on modifying CVD risk through pharmacological and non-pharmacological interventions (Figure 1).
FIGURE 1. The three steps to using the HEARTS app for assessing cardiovascular disease risk and hypertension management.
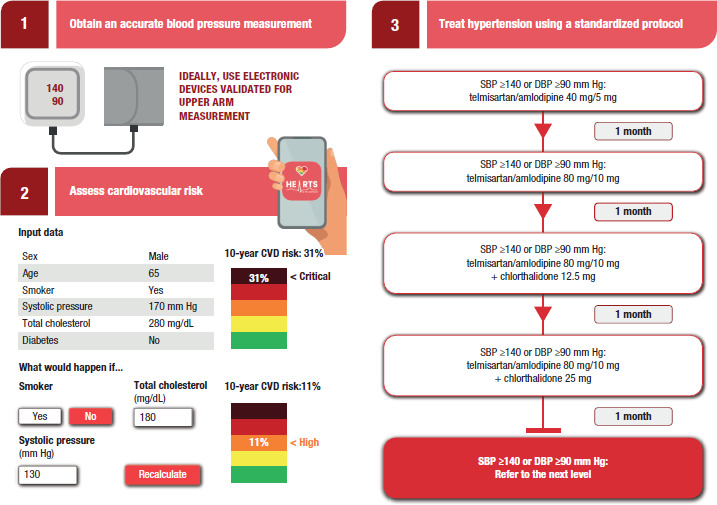
CVD: cardiovascular disease; DBP: diastolic blood pressure; SBP: systolic blood pressure.
Source: Figure prepared by the authors based on the HEARTS app.
The HEARTS risk calculator mimics the colored charts in the CardioCal app (9). After the user enters the requested data, the risk calculator quantifies the 10-year CVD risk for myocardial infarction, stroke and death from CVD, with color-coded risk categories ranging from green to dark red. Initially, an algorithm was developed using Excel spreadsheets for each of the 6 regions in the Americas, with or without a cholesterol value; the included regions are High-income North America, the Caribbean, Central Latin America, Andean Latin America, Tropical Latin America and Southern Latin America. These were then comprehensively validated. An initial evaluation included 504 cases to cover each of the parts of the color charts (84 cases for each of the 6 regions, 56 for the calculator with cholesterol and 28 without cholesterol). In addition, data on systolic blood pressure, cholesterol and BMI were randomly assigned. Twelve professionals collaborated in the first evaluation, 6 of whom reported their results using the color charts and 6 using the calculator. The results were marked on the colored sheets, and screenshots of each calculator result were taken to verify the origin of any errors. As a result, seven errors were detected, two in data entry and five due to three formula errors: (a) the cut point for cholesterol was changed from 154 mg/dL to 155 mg/dL; (b) the cut point for systolic blood pressure was changed from 179 mm Hg to 180 mm Hg; and (c) an error was detected in the code for the Caribbean tables. The same procedure was repeated after reviewing the original tables and formulas. In the new iteration, another 504 cases were evaluated and there was total agreement. Finally, the algorithm was converted to formats suitable for the Internet, personal computers and smartphones.
HOW CAN THE TOOL BE OPTIMIZED IN CLINICAL PRACTICE?
Ideally, a CVD risk calculator should provide a reliable and accurate estimate of risk using easy-to-obtain demographic and biometric data. In addition, the tool should be simple to use, provide an estimate quickly and provide clear recommendations that are appropriate for the individual and the care setting where it is being used (10). Training to use the tool should also be simple and quick. The HEARTS CVD risk calculator meets these criteria.
The HEARTS CVD risk calculator can be optimized by using it for those individuals whose risk is uncertain. After the CVD risk estimate is calculated, it can be used to educate the patient, inform the health care team and help prioritize appropriate care within the health care system. For people aged 40–74 years without known CVD (primary prevention), diabetes mellitus or chronic kidney disease, the HEARTS app can help determine when it is necessary to initiate antihypertensive pharmacological treatment at a lower threshold, the blood pressure treatment goal and the recommended follow-up interval.
The optimal use of the HEARTS app also involves applying it to high-risk individuals, such as people aged 40–74 years with known CVD, diabetes or chronic kidney disease. In such cases, the tool’s value is to enhance treatment guidance about managing risk factors based on the individual’s risk profile. For example, the HEARTS app may recommend a lower treatment target for blood pressure and more frequent follow up for high-risk individuals. Additionally, people with known CVD (secondary prevention) may be advised to consider aspirin and statin therapy or the health care provider may seek input from a specialist (Figure 2). Health care providers are likely to find that using the tool becomes easier and faster over time as they become more familiar with it and the program’s recommendations.
FIGURE 2. Optimizing the HEARTS cardiovascular risk assessment tool in clinical practice.
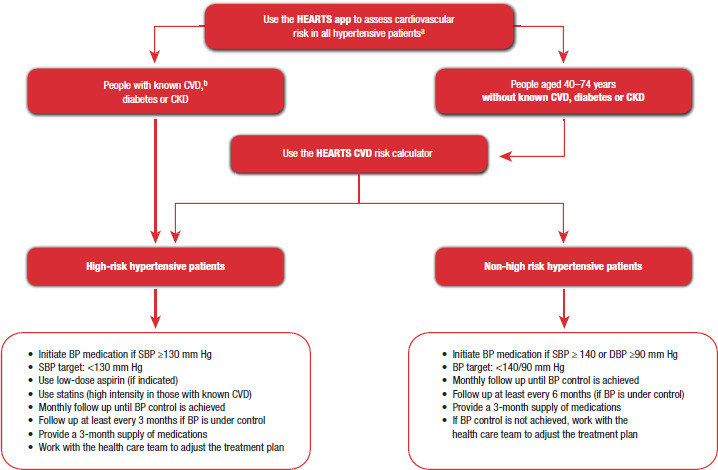
a Obtaining the CVD risk score must not delay the initiation of pharmacological treatment.
b CVD comprises ischemic heart disease, peripheral artery disease and stroke.
BP: blood pressure; CKD: chronic kidney disease; CVD: cardiovascular disease; DBP: diastolic blood pressure; SBP: systolic blood pressure.
Source: Figure prepared by the authors based on the HEARTS app.
LIMITATIONS
Despite the 2019 WHO CVD risk charts (5) having a high discriminative capacity, they are not intended to cover the entire context of CVD risk. For example, the laboratory-based option does not incorporate variables such as overweight or obesity, nor does it include a family history of coronary or vascular disease occurring at an early age, disadvantaged socioeconomic status or a sedentary lifestyle, all factors that, if present, imply more significant risk. However, although risk categories for more than 80% of adults were classified similarly by both the laboratory-based and non-laboratory-based models, the non-laboratory-based model substantially underestimated risk among patients with diabetes (11). Finally, this calculator does not include variables for mental health, certain inflammatory conditions or high-sensitivity C-reactive protein results as a marker of inflammation.
Clinicians frequently ask for defined decision thresholds that should trigger intervention in primary care settings; however, these are problematic since risk is a continuum, and there is no precise point above which, for instance, a medicine is automatically indicated nor below which lifestyle advice may not be useful. Thus, for example, among people aged ≤50 years, those with a high relative or lifetime risk for CVD must be counseled about lifestyle interventions, and those with a single CVD risk factor, such as total cholesterol >300 mg/dL or persistent systolic blood pressure >140 mm Hg, will require an additional intervention. Furthermore, it is essential to identify individuals with a family history of premature CVD and those who should be tested and treated for familial hypercholesterolemia.
CONCLUSIONS
The HEARTS app is not intended to replace clinical judgment; instead, this tool aims to help individuals and health professionals to improve their understanding of CVD risk and the relevance of detecting and addressing modifiable risk factors and to support proven interventions that are part of the health strategies implemented in most countries. Moreover, the optimization of any tool depends not only on using it properly but also on ensuring sustained and consistent implementation of the recommendations generated by the tool.
In summary, the HEARTS app is a powerful clinical tool that can help to improve the effectiveness and efficiency of interventions and improve the quality of care in primary care settings. Thus, the HEARTS app is an essential step in the journey towards eliminating preventable CVD in the Region of the Americas.
Disclaimer.
PO is staff member of and CT, YAR and AR are consultants for the Pan American Health Organization. Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the Revista Panamericana de Salud Pública/Pan American Journal of Public Health or those of the Pan American Health Organization (PAHO).
Funding Statement
Funding. The Pan American Health Organization (PAHO), with financial support from the U.S. Centers for Disease Control and Prevention (CDC), transformed the published color-coded tables into an online electronic calculator for use on computers and smartphones. PAHO and the CDC had no influence over the design of the app, data collection and analysis, the writing of the paper and the decision to publish these results.
Footnotes
Authors’ contributions.
PO and CT conceived the original idea for the paper and wrote the first draft of the manuscript. CT conducted and supervised the adaptation of WHO’s 2019 CVD risk charts into an online electronic calculator, updating the previous 2014 CardioCal app. All authors (PO, CT, TG, YAR, AR and MGJ) contributed content and reviewed the paper. All authors reviewed and approved the final version.
Conflicts of interest.
None declared.
REFERENCES
- 1.Martinez R, Soliz P, Mujica OJ, Reveiz L, Campbell NRC, Ordunez P. The slowdown in the reduction rate of premature mortality from cardiovascular diseases puts the Americas at risk of achieving SDG 3.4: A population trend analysis of 37 countries from 1990 to 2017. J Clin Hypertens (Greenwich) 2020;22(8):1296–1309. doi: 10.1111/jch.13922. [DOI] [PMC free article] [PubMed] [Google Scholar]; 1. Martinez R, Soliz P, Mujica OJ, Reveiz L, Campbell NRC, Ordunez P. The slowdown in the reduction rate of premature mortality from cardiovascular diseases puts the Americas at risk of achieving SDG 3.4: A population trend analysis of 37 countries from 1990 to 2017. J Clin Hypertens (Greenwich). 2020;22(8):1296-1309. [DOI] [PMC free article] [PubMed]
- 2.Pan American Health Organization . Washington (DC): Pan American Health Organization; 2019. NCDs at a glance: NCD mortality and risk factor prevalence in the Americas.https://iris.paho.org/handle/10665.2/51696 [Google Scholar]; 2. Pan American Health Organization. NCDs at a glance: NCD mortality and risk factor prevalence in the Americas. Washington (DC): Pan American Health Organization; 2019. https://iris.paho.org/handle/10665.2/51696
- 3.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population–representative studies with 104 million participants. Lancet. 2021;398:957–980. doi: 10.1016/S0140-6736(21)01330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]; 3. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population–representative studies with 104 million participants. Lancet. 2021;398:957-80. [DOI] [PMC free article] [PubMed]
- 4.Campbell NRC, Ordunez P, Giraldo G, Rodriguez Morales YA, Lombardi C, Khan T, et al. WHO HEARTS: A global program to reduce cardiovascular disease burden: experience implementing in the Americas and opportunities in Canada. Can J Cardiol. 2021;37(5):744–755. doi: 10.1016/j.cjca.2020.12.004. [DOI] [PubMed] [Google Scholar]; 4. Campbell NRC, Ordunez P, Giraldo G, Rodriguez Morales YA, Lombardi C, Khan T, et al. WHO HEARTS: A global program to reduce cardiovascular disease burden: experience implementing in the Americas and opportunities in Canada. Can J Cardiol. 2021;37(5):744-55. [DOI] [PubMed]
- 5.WHO CVD Risk Chart Working Group World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]; 5. WHO CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332-45. [DOI] [PMC free article] [PubMed]
- 6.Lewington S, Clarke R. Combined effects of systolic blood pressure and total cholesterol on cardiovascular disease risk. Circulation. 2005;112:3373–3374. doi: 10.1161/CIRCULATIONAHA.105.581934. [DOI] [PubMed] [Google Scholar]; 6. Lewington S, Clarke R. Combined effects of systolic blood pressure and total cholesterol on cardiovascular disease risk. Circulation. 2005;112:3373-4. [DOI] [PubMed]
- 7.Gaziano TA, Steyn K, Cohen DJ, Weinstein MC, Opie LH. Cost-effectiveness analysis of hypertension guidelines in South Africa: absolute risk versus blood pressure level. Circulation. 2005;112(23):3569–3576. doi: 10.1161/CIRCULATIONAHA.105.535922. [DOI] [PubMed] [Google Scholar]; 7. Gaziano TA, Steyn K, Cohen DJ, Weinstein MC, Opie LH. Cost-effectiveness analysis of hypertension guidelines in South Africa: absolute risk versus blood pressure level. Circulation. 2005;112(23):3569-76. [DOI] [PubMed]
- 8.Gaziano TA. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005;112(23):3547–3553. doi: 10.1161/CIRCULATIONAHA.105.591792. [DOI] [PubMed] [Google Scholar]; 8. Gaziano TA. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005;112(23):3547-53. [DOI] [PubMed]
- 9.Ordunez P, Tajer C. Disseminating cardiovascular disease risk assessment with a PAHO mobile app: a public eHealth intervention. Rev Panam Salud Publica. 2015 Jul;38(1):82–85. [PubMed] [Google Scholar]; 9. Ordunez P, Tajer C. Disseminating cardiovascular disease risk assessment with a PAHO mobile app: a public eHealth intervention. Rev Panam Salud Publica. 2015 Jul;38(1):82-5. [PubMed]
- 10.Tuzzio L, O’Meara ES, Holden E, Parchman ML, Ralston JD, Powell JA, et al. Barriers to implementing cardiovascular risk calculation in primary care: alignment with the Consolidated Framework for Implementation Research. Am J Prev Med. 2021;60(2):250–257. doi: 10.1016/j.amepre.2020.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]; 10. Tuzzio L, O’Meara ES, Holden E, Parchman ML, Ralston JD, Powell JA, et al. Barriers to implementing cardiovascular risk calculation in primary care: alignment with the Consolidated Framework for Implementation Research. Am J Prev Med. 2021;60(2):250-7. [DOI] [PMC free article] [PubMed]
- 11.Ueda P, Woodward M, Lu Y, Hajifathalian K, Al-Wotayan R, Aguilar-Salinas CA, et al. Laboratory-based and office-based risk scores and charts to predict 10-year risk of cardiovascular disease in 182 countries: a pooled analysis of prospective cohorts and health surveys. Lancet Diabetes Endocrinol. 2017;5:196–213. doi: 10.1016/S2213-8587(17)30015-3. [DOI] [PMC free article] [PubMed] [Google Scholar]; 11. Ueda P, Woodward M, Lu Y, Hajifathalian K, Al-Wotayan R, Aguilar-Salinas CA, et al. Laboratory-based and office-based risk scores and charts to predict 10-year risk of cardiovascular disease in 182 countries: a pooled analysis of prospective cohorts and health surveys. Lancet Diabetes Endocrinol. 2017;5:196–213. [DOI] [PMC free article] [PubMed]


