Abstract
Objective:
The purpose of this study was to survey US Veterans Health Administration (VA) chiropractors to assess current demographic and professional characteristics, including practice parameters, interprofessional collaboration, academic experience and scholarly activity.
Methods:
A cross-sectional survey was performed from August 21, 2019 to September 6, 2019 that included all chiropractors identified with any VA appointment. Research Electronic Data Capture (REDCap) was used to conduct the survey. Data from surveys were exported to Microsoft Excel for data analysis.
Results:
Of the 177 available providers solicited, 118 returned completed surveys (67% response rate). Respondents predominantly self-reported as white (84%), male (77.1%), with a mean age of 47 years old, and reported at least 75% of time being spent on clinical care. Most respondents reported they were VA employees (96%) with full-time appointments (94%). Approximately half reported having prior hospital training (48%), supervising chiropractic students (53%) and students in other health professions (47%), and authored or co-authored ≥1 peer-reviewed publications (42%). Chiropractors reported seeing an average of 6–15 new patient consultations and 31–60 follow-up visits per week. Most patient referrals to chiropractic originated from primary care providers, with low back conditions without radiculopathy as the most frequently seen condition. Diversified manipulation and flexion-distraction techniques along with myofascial therapies, therapeutic exercises, and self-management advice were the most commonly reported interventions.
Conclusion:
We report provider and practice characteristics from chiropractors working in a large, integrated healthcare system. Most are full-time employees, work in physical medicine departments, and have held their position for up to 5 years. The majority of respondents report diagnostic and treatment approaches concordant with current Clinical Practice Guidelines.
Keywords: chiropractic, integrative medicine, physical and rehabilitation medicine, surveys, veteran
Introduction
The US Veterans Health Administration (VA) began providing on-station chiropractic services at selected VA facilities in late 2004. The number of locations has increased to 148 facilities as of March 2020.1,2 VA is currently in the process of a systematic expansion of its chiropractic program which is projected to result in chiropractic clinics at a total of more than 200 facilities by December 31, 2021.3
Previous studies regarding doctors of chiropractic (DC) and the patients who seek their care in the United States and Canada have shown variation among providers in professional training, practice parameters, interprofessional collaboration, academic experience, and scholarly activity.4,5,6,7 A 2008 survey of VA DCs found provider characteristics were similar to those in US private practice, with limited academic and research experience or prior hospital training or experience.8
Per national policy, VA aims to deliver evidence-based, guideline-concordant chiropractic care.3 Previous work assessing clinical coding in VA administrative data demonstrated chiropractic care has been provided consistent with guidelines for non-operative spinal conditions,9 yet the degree to which this accurately reflects the practice of VA chiropractors is not fully understood. As VA continues to grow its chiropractic program, this evolution presents an opportunity to assess features of chiropractors and clinics in a large, integrated healthcare system. Chiropractic practice includes a number of evidence-based nonpharmacological treatment approaches that have been identified as priorities for expansion in VA, thus a better understanding of VA chiropractor professional characteristics may help inform workforce development, as well as program assessment and improvement initiatives.10 Additionally, since VA is the largest integrated healthcare system in the US, characteristics of its chiropractic workforce may be relevant to chiropractic care within other healthcare systems.11 Therefore, the purpose of this study was to assess provider characteristics and clinical practice patterns of the current VA DC workforce.
Methods
Study Design and Participant Recruitment
We conducted a cross-sectional survey of all licensed DCs with appointments at VA facilities at the time of the survey commencement (August 22, 2019), identified from the VA Chiropractic Program Office managerial data records. Study investigators were not excluded from the survey. Doctors of chiropractic who obtained their VA appointment after the initiation of the study, as well as in-training individuals, such as students, residents, and fellows, were excluded. The VA Connecticut Healthcare System Research and Development Department designated this project as program assessment and thereby this study was exempted from Institutional Review Board review.
Survey Development
The survey instrument was modeled after the previous survey of VA DCs, with adaptations based on a national survey of DCs conducted by the National Board of Chiropractic Examiners and other surveys of US-based DCs.4,6,8,12 The survey was piloted on three current DCs at VA Connecticut Healthcare System for clarity and revised as indicated prior to launch. The final survey consisted of 6 demographic questions, 14 questions pertaining to educational and professional activities, and 27 questions regarding clinical practice characteristics. (See Supplemental File for survey) Only those who responded “yes” to providing patient care were asked to complete survey questions on clinical practice.
Data Collection
Survey responses were collected from August 21, 2019 to September 6, 2019 and managed using Research Electronic Data Capture (REDCap) housed on a VA Informatics and Computing Infrastructure (VINCI) server at the Austin Information Technology Center. REDCap is a data management platform developed by Vanderbuilt University to support clinical and translational research. 13 Those DCs meeting inclusion criteria received invitational emails with unique survey links sent directly from the REDCap system. Reminder emails were sent at 7 and 14 days following the initial request to complete the survey to those who had not completed the survey and had not opted out of future contact. Survey responses were collected anonymously and exported into Microsoft Excel (Microsoft Corporation, Redmond, WA). Incomplete surveys were excluded from the final analysis.
Statistical Analysis
Descriptive statistics were calculated for categorical variables of completed surveys. Surveys were considered complete if the respondent finished the survey in its entirety. Post-hoc, exploratory sub-group comparisons were completed for gender and years of employment to assess any descriptive differences in these groups. .
Results
Emails were sent to 177 chiropractors, of whom 132 returned responses, and 118 of these were complete, for a completed response rate of 67%. Respondents were predominantly white (84%), non-Hispanic or non-Latino (86%) and male (77%), with a mean age of 47 years (26–67 years). Twenty-six (22%) respondents were Veterans.
Educational and Professional Characteristics
As shown in Table 1, the majority of respondents graduated from chiropractic school within the last 20 years (n=66, 56%), with 34 (29%) graduating in the last 10 years. Sixty-seven respondents (47%) reported prior hospital training prior to obtaining their VA position. Fifty (42%) indicated they had published one or more peer-reviewed publications, with 22 (20%) reporting having been a co-investigator or principal investigator on a funded research project.
Table 1.
Educational characteristics of 118 DCs
| n (%) | ||
|---|---|---|
| Chiropractic school graduation year | Prior to 2000 | 52 (44%) |
| 2000–2009 | 32 (27) | |
| 2010–2019 | 34 (29) | |
| Chiropractic school conferring DC degree | Cleveland University, Kansas City (Cleveland Chiropractic College) | 3 (3) |
| D’Youville University | 1 (1) | |
| Life University, College of Chiropractic (Life College) | 6 (5) | |
| Life University, West | 1 (1) | |
| Logan College of Chiropractic | 14 (11) | |
| National University of Health Sciences, Illinois (National College of Chiropractic) | 3 (3) | |
| National University of Health Sciences, Florida | 2 (2) | |
| New York Chiropractic College | 16 (14) | |
| Northwestern health Sciences University (Northwestern College of Chiropractic) | 8 (7) | |
| Palmer College of Chiropractic, Davenport | 26 (22) | |
| Palmer College of Chiropractic, Florida | 2 (2) | |
| Palmer College of Chiropractic, West | 7 (6) | |
| Parker University, College of Chiropractic | 7 (6) | |
| Sherman College of Chiropractic | 2 (2) | |
| Southern California University of Health Sciences (Los Angeles College of Chiropractic) | 7 (6) | |
| Texas Chiropractic College | 1 (1) | |
| University of Bridgeport School of Chiropractic (University of Bridgeport College of Chiropractic) | 5 (4) | |
| University of Western States (Western States Chiropractic College) | 7 (6) | |
| Other professional degrees/certifications | EMT | 9 (8) |
| LAc/MAOM | 6 (5) | |
| PT/DPT/OT | 5 (4) | |
| ATC | 2 (2) | |
| RN/LPN | 1 (1) | |
| NP/APRN | 1 (1) | |
| JD | 1 (1) | |
| Other degrees and certifications | Master’s Degree | 32 (27) |
| Chiropractic Diplomate | 26 (22) | |
| Prior hospital training | Hospital-based chiropractic student rotation | 37 (31) |
| Hospital-based chiropractic residency program | 16 (14) | |
| Other formal hospital-based training | 14 (12) |
Employment Characteristics
Most respondents reported that they were VA employees (n=113, 96%), with full-time appointments (n=111, 94%) and employed by VA for five years or less (n=79, 68%). The chiropractic clinics in which respondents work were most commonly administratively aligned under Rehabilitation/Physical Medicine and Rehabilitation, Pain Medicine/Pain Management, and Whole Health service lines (Table 1 and 2).
Table 2.
Professional Characteristics of Respondents (N = 118)
| 0 | 68 (58) | |
| 1–5 | 38 (32) | |
| 6–10 | 6 (5) | |
| 11–20 | 2 (2) | |
| >20 | 4 (3) | |
| Years working at VA | < 1 year | 23 (20) |
| 1–5 years | 56 (48) | |
| 6–10 years | 13 (11) | |
| 10–15 years | 20 (17) | |
| >15 years | 6 (5) | |
| Employment | Full-time | 111 (94) |
| Part-time | 7 (6) | |
| Administrative service line of chiropractic clinic | Rehabilitation/Physical Medicine and Rehabilitation | 61 (53) |
| Pain Medicine/Pain Management | 16 (14) | |
| Whole Health | 15 (13) | |
| Geriatrics/Extended Care | 10 (9) | |
| Primary Care | 6 (5) | |
| Surgical | 4 (3) | |
| Ambulatory Care | 2 (2) | |
| Other | 2 (2) | |
| Other professional activities | Hospital Committees | 62 (53) |
| In-Service Presentations | 75 (64) | |
| Train/Supervise Chiropractic Student Trainees | 62 (53) | |
| Train/Supervise Chiropractic Resident/Fellows | 17 (14) | |
| Train/Supervise MD/DO Students/Residents/Fellows | 55 (47) | |
| Quality Improvement Activities | 69 (58) | |
| Research Activities | 51 (43) |
Clinical Characteristics
Of the 118 respondents, 116 (98%) reported actively providing patient care. . Eighty-seven respondents (74%) reported having at least one additional DC providing full-time or part-time clinical care at their VA facility and 37 (32%) reported support staff, including nurses and chiropractic assistants, assisting with patient care.
Patient referrals and characteristics
Incoming referrals to the chiropractic clinic most commonly originated from primary care, with approximately 91% of clinicians reporting they received referrals from this department most frequently, at least several times per day or week (Table 3). Other common referral sources were pain medicine/management, physiatry, neurology, and orthopedic surgery. Respondents reported outgoing referrals were most commonly sent to primary care, pain medicine/management, physiatry, orthopedic surgery, and neurology and/or neurosurgery.
Table 3.
Patient referral patterns of 116 DCs-n (%)
| Incoming Referrals | |||||
| Several per day | Several per week | Several per month | Several per year | Never | |
| Primary Care | 70% | 21% | 5% | 2% | 3% |
| Pain Medicine | 16 | 28 | 31 | 16 | 9 |
| Physiatry | 10 | 20 | 27 | 16 | 28 |
| Orthopedic surgery | 1 | 2 | 14 | 41 | 43 |
| Neurology | 0 | 6 | 22 | 34 | 39 |
| Emergency Dept | 0 | 5 | 16 | 31 | 47 |
| Neurosurgery | 0 | 4 | 17 | 29 | 49 |
| Rheumatology | 0 | 1 | 10 | 32 | 57 |
| Spinal Cord Injury | 0 | 2 | 4 | 28 | 66 |
| Podiatry | 0 | 2 | 8 | 24 | 66 |
| Dentistry | 0 | 0 | 0 | 10 | 90 |
| Optometry | 0 | 0 | 0 | 1 | 99 |
| Outgoing referrals | |||||
| Several per day | Several per week | Several per month | Several per year | Never | |
| Primary Care | 6% | 22% | 38% | 23% | 11% |
| Pain Medicine | 3 | 8 | 47 | 27 | 16 |
| Physiatry | 3 | 4 | 36 | 29 | 28 |
| Orthopedic surgery | 1 | 2 | 18 | 47 | 33 |
| Neurosurgery | 0 | 1 | 14 | 53 | 33 |
| Neurology | 0 | 1 | 14 | 53 | 33 |
| Podiatry | 0 | 1 | 14 | 47 | 39 |
| Emergency Dept | 0 | 0 | 4 | 53 | 43 |
| Rheumatology | 0 | 0 | 6 | 40 | 54 |
| Spinal Cord Injury | 0 | 0 | 0 | 16 | 85 |
| Dentistry | 0 | 0 | 1 | 7 | 92 |
| Optometry | 0 | 0 | 1 | 9 | 91 |
Most commonly, respondents saw a range of 6–15 new patient consults per week, and spent 45–60 minutes reviewing records, interacting with the patient and documenting the encounter. The majority reported seeing between 31–60 established patient follow-up encounters per week, with a range of 16–45 minutes for chart review, treatment and documentation (Table 4).
Table 4.
Patient visit characteristics of 116 DCs
| n (%) | ||
|---|---|---|
| Average number of new-patient consult visits in one week | <6 | 12 (10%) |
| 6–15 | 79 (59) | |
| >15 | 25 (22) | |
| Average number of established patient follow-up visits in one week | <31 | 16 (14) |
| 31–60 | 73 (63) | |
| >60 | 27 23) | |
| Total average time spent with a new patient consult visit | <16 minutes | 6 (5) |
| 16–45 minutes | 28 (24) | |
| 45–60 minutes | 50 (43) | |
| >60 minutes | 32 (28) | |
| Total average time spent with established patient follow-up visit | <16 minutes | 11 (9) |
| 16–45 minutes | 75 (65) | |
| 45–60 minutes | 16 (14) | |
| >60 minutes | 2 (2) |
Clinicians reported seeing low back and cervical pain conditions without radiculopathy most frequently (96% several times per day or week). This was followed by low back pain with radiculopathy (85%) and cervical pain with radiculopathy (72%) (Table 5).
Table 5.
Frequency of conditions treated of 116 DCs-n (%)
| Several per day | Several per week | Several per month | Several per year | Never | |
|---|---|---|---|---|---|
| Low back w/o Radiculopathy | 81% | 15% | 3% | 2% | 0% |
| Cervical w/o Radiculopathy | 72 | 23 | 3 | 2 | 0 |
| Low back w/ Radiculopathy | 50 | 35 | 13 | 2 | 0 |
| Cervical w/ Radiculopathy | 32 | 41 | 21 | 6 | 0 |
| Tension Headache | 16 | 42 | 29 | 12 | 1 |
| Cervicogenic Headache | 15 | 43 | 32 | 10 | 1 |
| Lower extremity | 10 | 31 | 41 | 17 | 1 |
| Upper extremity | 10 | 30 | 41 | 17 | 1 |
| Migraine Headache | 9 | 36 | 38 | 16 | 2 |
Examination Procedures
On initial diagnostic work-up of new patients, the great majority reported routinely using widely accepted clinical evaluation methods such as: patient interview/history, orthopedic and neurological examination, joint and soft tissue palpation, and range of motion assessment A majority of respondents never included: galvanic skin response, thermography, electrocardiography, electrodiagnostic studies, eye/ear examination, heart/lung examination. (Figure 1)
Figure 1.
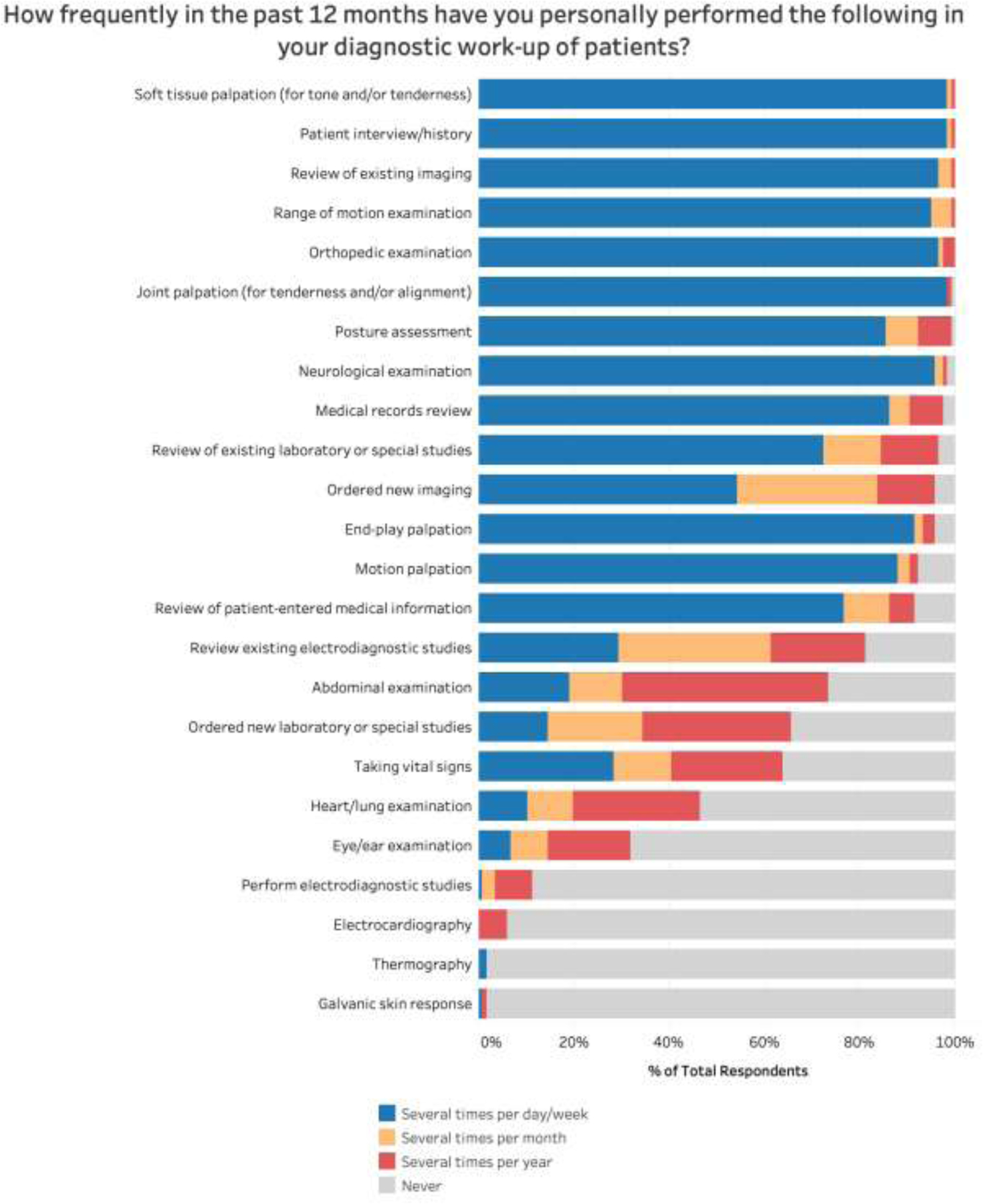
Participants responses to frequency of use of selected diagnostic procedures
The most common reasons reported for ordering radiographs were diagnosis of structural pathology (99%) or serious/treatable pathology (85%), based on widely accepted indications. Some respondents reported ordering radiographs to assess spinal alignment/posture to determine chiropractic technique approach (27%) or for outcome assessment (20%).
Treatment Procedures
The most common manipulative treatment techniques used by respondents were diversified (95%), manual mobilization (79%), Cox/Flexion-Distraction (68%), and Thompson/Drop Table (52%). Additional therapies used commonly (at least several times per week) included manual myofascial techniques (88%), active release/pin and stretch (51%), neuromuscular re-education (46%), and Mechanical Diagnosis and Treatment/McKenzie (41%) (Figure 2). Respondents reported prescribing active care commonly, including therapeutic exercises (90%), ergonomic/ADL modifications (83%), self-management advice (83%), lifestyle counseling (72%) and patient education on disease factors and/or natural history (66%) (Figure 3).
Figure 2.
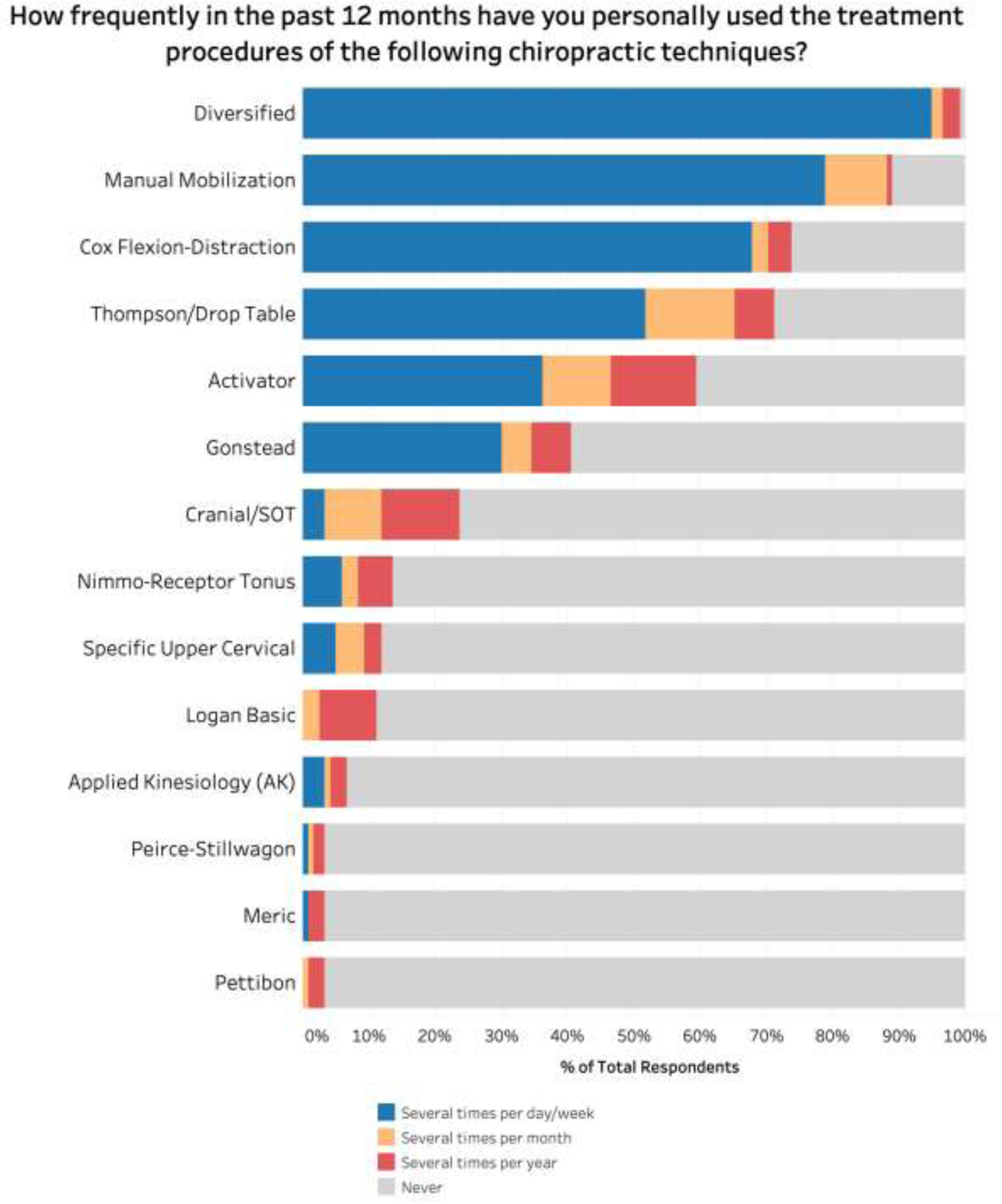
Participants responses to frequency of use of selected chiropractic technique procedures
Figure 3.
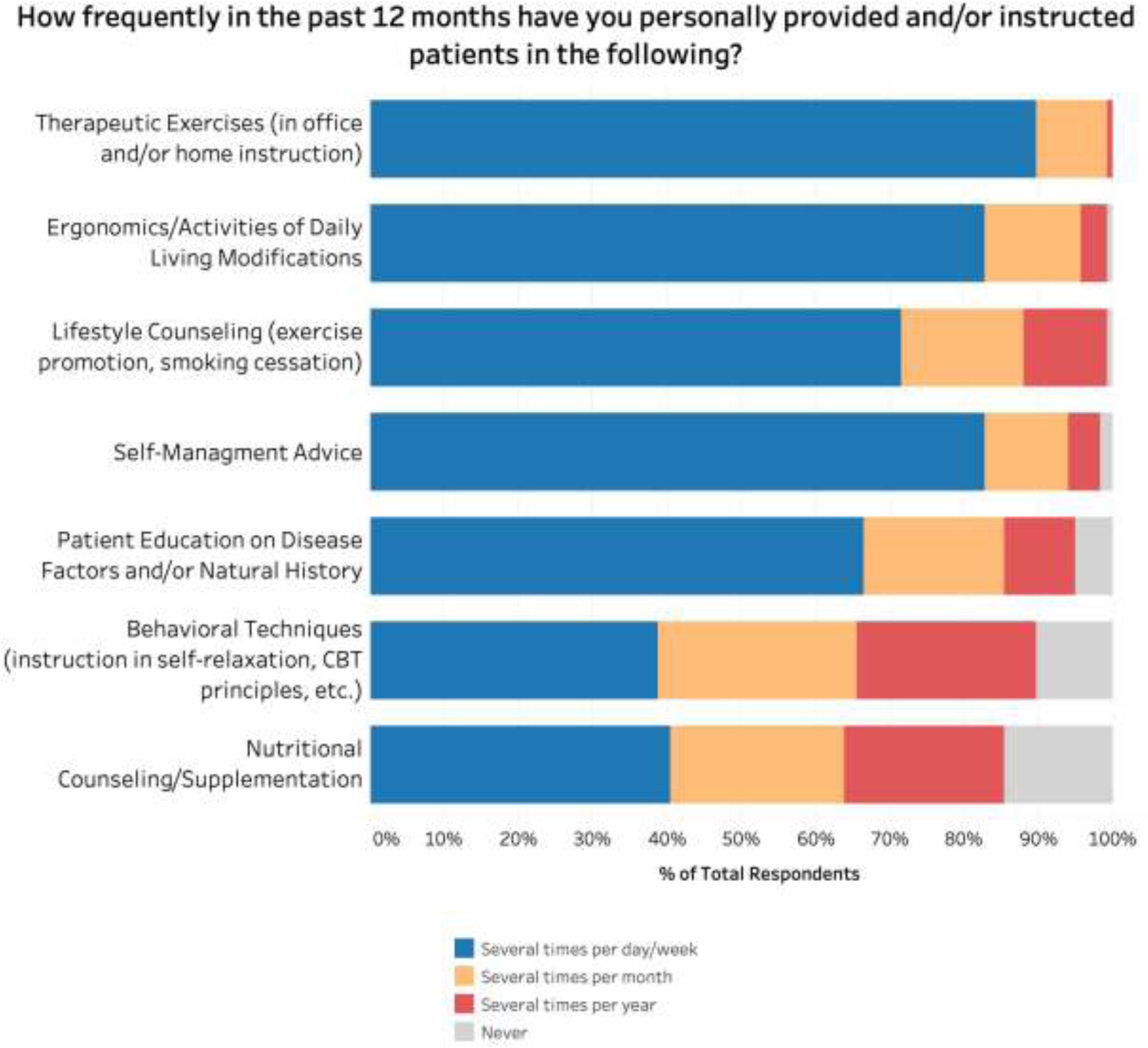
Participant responses to frequency of providing or instructing patients in supportive treatments, behaviors, and/or lifestyle interventions
Other Professional Activities
More than half of respondents reported participating in hospital committee work, quality improvement activities, and in-service presentations, and roughly half reported training or supervising chiropractic students and/or supervising MD/DO trainees. Additionally, fifty-one (43%) report participating in research activities (Table 1).
Subgroup Analysis
Female respondents were on average younger than males (42.7 vs 47.7 years), but there were no other substantial differences. When comparing those with up to 5 years of VA employment to those with greater than five years, the latter were more likely to have authored one or more peer-reviewed publication, be older (51.3 v. 44 years), further from graduation (22.8 years v. 16 years), have increased workload in educational activities (5% v. 2%), and less likely to have prior hospital training (33% v. 53%).
Discussion
This work adds to the current body of knowledge on chiropractors in the VA system. Since expansion of chiropractic care is a policy priority for VA, and hospital practice is rare among US chiropractors the VA system is a key environment in which to assess multiple aspects of hospital-based chiropractors and their practice patterns.12
The demographics of VA DCs in our study (77% male, 84% white, average age 47 years) closely match VA administrative data for all VA chiropractors employed during our data collection timeframe (75% male, 89% white, average age 46 years), and are similar to those reported of the general US chiropractor population (67% male, 85% white, 65% between 30–60 years).12 While it is beyond the scope of this paper to assess if our respondents’ demographic distribution has any impact on patient care (e.g. patient preference, clinical outcomes), it is interesting to note that this distribution is close to the Veteran patient population (91% male, 78% white, median age 64 years old),15 but varies from the general US chiropractic patient population, where more women are typically seen (76% female, 90% white, average age 48 years old).16
As expected, most respondents worked at VA medical centers, in physical medicine and rehabilitation service lines, primarily providing patient care. The reported bi-directional referral patterns, case types seen, and treatments delivered are generally consistent with prior studies assessing VA administrative data.8,9
The patient care elements reported are broadly concordant with current clinical practice guidelines (CPG) for neck and low back pain management, which recommend diagnosis with appropriate history and examination with selective use of imaging, and front line treatment with a group of nonpharmacological therapies including spinal manipulation, exercise, self-management strategies, and behavioral approaches. 17,18, 19, 20 Our respondents reported they provide these types of diagnostic and therapeutic services routinely as part of standard patient care. VA DCs reported frequent use of spinal manipulation, and the majority also reported using therapeutic exercise, self-management advice, lifestyle counseling, and other active approaches as components of multimodal chiropractic care.
We identified one potential deviation from guideline-concordant care. The majority of respondents reported using radiographs based on widely accepted indications, such as diagnosing serious or treatable pathology. However 27% reported ordering radiographs to assess spinal alignment/posture to determine chiropractic technique approach, and 20% to assess spinal alignment/posture for routine follow-up. This is in contrast with current recommendations and may represent an area for education and professional development.17,18,19,20,21
Our results show several differences from the 2009 study of VA DCs, which included responses from 33 of the then 36 chiropractors.8 Our respondents included a greater proportion of females (23% v. 6%), employees (95% v. 67%), and a lesser proportion of sole chiropractors at their site (26% v. 67%). Additionally, our respondents were more likely to report prior hospital training (47% v. 33%) and having at least one peer-reviewed publication (43% v. 33%) and a master’s degree. In 2009, 24% reported involvement with training chiropractic students or other trainees within VA, whereas current respondents report training both chiropractic students and medical students, residents and fellows approximately double this rate.
The increased hospital training reported by VA DCs could include student preceptorship, residency, or fellowship, and may be related to the increased number of such trainees continuing to obtain positions within the VA system. These unique training opportunities may have allowed for increased interface with medical professionals, better preparing the DC for a position within a hospital system. Alternately, DC trainees interested in working in an integrated setting may seek out these training opportunities to increase qualification for such positions.
Some key practice characteristics identified by our respondents are different from those of general US private practice DCs, as measured by the 2019 NBCE survey.14 Overall, private practice DCs are more likely to use radiography both for initial diagnosis and for assessing treatment response. While both groups report using manipulative treatments for a majority of their patients, 71.9% of private practice DCs reports using instrument assisted manipulation on spinal regions several times per day, compared to less than 40% of VA DCs reporting using instrument assisted manipulation several times per day or week. Additionally, 54.3% and 45.1% of private practice DCs report using unattended and attended physiotherapy modalities, respectively, while less than 25% of VA DCs report using hot/cold packs, electric stimulation, ultrasound, microcurrent or cold laser. Therapeutic exercises are used more commonly by VA DCs, with 90% reporting employing these management strategies several times per day or week, while 58.4% of private practice DCs report using in-office rehab at least once per day with patients. Since VA delivers chiropractic care using in-house VA DCs as well as purchases care from community DCs, a better understanding of differences between these provider groups can be helpful in assessing Veteran outcomes and experiences.
The exploratory subgroup analysis showed DCs who have been employed at VA for greater than 5 years were more likely to have increased workload in education, such as work with trainees or an educational institution, while those with less than 5 years of VA employment were more likely to have prior hospital training. This may be partly due to the increased number of hospital-based clinical rotations for chiropractic students in recent years, as well as the implementation of the VA chiropractic residency program. Recent graduates are more likely to have had an opportunity to train in a hospital while still in school, while DCs with longer tenure are more likely to have a faculty appointment at a chiropractic or medical school and train chiropractic or medical preceptors/interns, residents, or fellows in a clinical and/or teach classroom setting. Since chiropractic practice approaches in the US may vary, understanding the current professional characteristics of VA chiropractors can inform system and provider educational efforts aimed to improve care quality and patient access to care.12
Furthermore, as the largest integrated healthcare system in the US, additional work assessing the characterizes and functions of chiropractic physicians in VA may help to inform ongoing integration efforts of chiropractors in other healthcare systems.
Limitations
Limitations of this study include recall or reporting bias, question wording or understanding and/or decision fatigue, which are commonly associated with survey data collection. Respondents may have experienced motivation to provide what they perceived as more favorable answers, or any answers at all, in order to appease the program office conducting the survey. However, we did inform participants that we would not know the specific answers of any given respondent. A 33% non- response rate raises the possibility for selection bias, although our respondents were comparable to VA national data on demographic and employment characteristics. Only chiropractors with clinical appointments at VA facilities were surveyed in this study. Results may not be transferable to DCs in other settings.
Regarding data, VA follows the CMS cell size suppression policy in that population values of 1–10 in any given category cannot be reported since this can be a privacy violation. Thus, some demographic data were not able to be reported. For our survey, we used the same Likert scale similar to the NBCE in an effort to be able to compare the 2 surveys and we modeled our questions off of the NBCE survey. However, in our survey we broke out the modalities into individual questions instead lumping them together in 1 category, which may results in different interpretation of our findings.
Conclusion
Most chiropractors within the current VA DC workforce report being full-time employees, working in physical medicine departments, have held their positions for up to 5 years, most frequently manage low back and neck conditions, and report routine bi-directional referrals with primary care, pain medicine and physiatry clinics. The diagnostic and therapeutic services they report commonly using are consistent with current clinical practice guidelines for managing spinal conditions.
Supplementary Material
FUNDING SOURCES AND CONFLICTS OF INTEREST
This work is supported by the National Institutes of Health (NIH) through cooperative agreement UH3AT009761 from the National Center for Complementary and Integrative Health (NCCIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health nor reflect the position or policy of the U.S. Department of Veterans Affairs or the United States Government. Conflicts of interest reported for this study include: Christine Goertz: grants from NCCIH/NIH, personal fees from The Spine Institute for Quality, Palmer College of Chiropractic and the American Chiropractic Association; Cynthia Long: grant from NCCIH/NIH; Anthony Lisi: grant from NCCIH/NIH; Brian Coleman: Postdoctoral Fellowship Support from US Dept. of Veterans Affairs, Office of Academic Affiliations; Todd Kawecki: None; Stephanie Halloran: grant from NCCIH/NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lisi AJ, Khorsan MM, Smith M, Mittman BS. Variations in the implementation and characteristics of chiropractic services in VA. Med Care. 2014; 52(12 Suppl 5):S97–S104. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Veterans Affairs [Internet]. Rehabilitation and Prosthetic Services: Chiropractic Care Facility Locations. Available from: https://www.prosthetics.va.gov/chiro/locations.asp
- 3.Veterans Health Administration [Internet]. Directive 1210: Chiropractic care. 2018; Available from: https://www.va.gov/vhapublications/publications.cfm?pub=1&order=asc&orderby=pub_Number
- 4.Mootz RD, Cherkin DC, Odegard CE, Eisenberg DM, Barassi JP, Deyo RA. Characteristics of chiropractic practitioners, patients, and encounters in Massachusetts and Arizona. J Manipulative Physiol Ther. 2005; 28(9):645–53. [DOI] [PubMed] [Google Scholar]
- 5.Coulter ID, Shekell PG. Chiropractic in North American: A descriptive analysis. J Manipulative Physiol Ther. 2005; 28(2):83–9. [DOI] [PubMed] [Google Scholar]
- 6.Bronston LJ, Austin-McClellan LE, Lisi AJ, Donovan KC, Engle WW. A survey of American Chiropractic Association members’ experiences, attitudes, and perceptions of practice in integrated health care settings. J Chiropr Med. 2015; 14(4): 227–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beliveau PJH, Wong JJ, Sutton DA, Simon NB, Bussieres AE, Mior SA, French SD. The chiropractic profession: a scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropr Man Therap. 2017;25:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lisi AJ, Goertz C, Lawrence DJ, Satyanarayana P, Characteristics of Veterans Health Administration chiropractors and chiropractic clinics. J Rehabil Res Dev. 2009;46(8):997–1002. [DOI] [PubMed] [Google Scholar]
- 9.Lisi AJ, Brandt CA. Trends in the use and characteristics of chiropractic services in the Department of Veterans Affairs. J Manipulative Physiol Ther. 2016; 39(5):381–386. [DOI] [PubMed] [Google Scholar]
- 10.Kligler B, Bair MJ, Banerjea R, DeBar L, Ezeji-Okoye S, Lisi A, Murphy JL, Sandbrink F, & Cherkin DC. Clinical policy recommendations from the VHA state-of-the-art conference on non-pharmacological approaches to chronic musculoskeletal pain. J Gen Intern Med. 2018; 33(Suppl 1), 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Department of Veterans Affairs. Veterans Health Administration: About VHA. Available from: http://www.va.gov/health/aboutvha.asp
- 12.National Board of Chiropractic Examiners [Internet]. Practice analysis of chiropractic: a project report, survey analysis, and summary of the practice of chiropractic within the United States. 2015; Available from: https://www.nbce.org/news/analysis-2015/
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Board of Chiropractic Examiners [Internet]. Practice analysis of chiropractic: a project report, survey analysis, and summary of the practice of chiropractic within the United States. 2020; Available from: https://mynbce.org/wp-content/uploads/2020/05/Practice-Analysis-of-Chiropractic-2020-5.pdf
- 15.United States Department of Veterans Affairs. Key Statistics by Veteran Status and Period of Services. 2016. Available from: https://www.va.gov/vetdata/docs/SpecialReports/KeyStats.pdf
- 16.Herman PM, Kommareddi M, Sorbero ME, Rutter CM, Hays RD, Hilton LG, Ryan GW, Coulter ID Characteristics of Chiropractic Patients Being Treated for Chronic Low Back Pain and Neck Pain. J Manipulative Physiol Ther. 2018;41(6):445–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137)2368–83 [DOI] [PubMed] [Google Scholar]
- 18.Qaseem A, Wilt TJ, McLean RM, Forciea MA, for the Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530. [DOI] [PubMed] [Google Scholar]
- 19.Haldeman S, Carroll L,Cassidy JD, Schubert J, Nygren A; Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: executive summary. Spine (Phila Pa 1976). 2008. Feb 15;33(4 Suppl):S5–7. doi: 10.1097/BRS.0b013e3181643f40. [DOI] [PubMed] [Google Scholar]
- 20.Côté P, Wong JJ, Sutton D, Shearer HM, Mior S, Randhawa K, Ameis A, Carroll LJ, Nordin M, Yu H, Lindsay GM, Southerst D, Varatharajan S, Jacobs C, Stupar M, Taylor-Vaisey A, van der Velde G, Gross DP, Brison RJ, Paulden M, Ammendolia C, David Cassidy J, Loisel P, Marshall S, Bohay RN, Stapleton J, Lacerte M, Krahn M, Salhany R. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J. 2016. Jul;25(7):2000–22. doi: 10.1007/s00586-016-4467-7. Epub 2016 Mar 16. [DOI] [PubMed] [Google Scholar]
- 21.Bussieres AE, Taylor JA, Peterson C Diagnostic imaging practice guidelines for musculoskeletal complaints in adults – an evidence-based approach – part 3: spinal disorders. J Manipulative Physiol Ther. 2008; 31(1):33–88. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


