A 64-year-old woman, unvaccinated against COVID-19, presented to the University of Colorado Hospital Radiation Oncology clinic (Aurora, CO, USA) in April, 2021, with a 7-week history of left chest wall burning, redness, and skin breakdown. These symptoms began with the onset of upper respiratory symptoms confirmed to be COVID-19 infection. She recovered from COVID-19 with conservative care; however, her pain and wound worsened, requiring opioid analgesics, and prompting her to seek care.
Her oncological history included an initial diagnosis of triple-negative node-positive left breast cancer in 2012, which had been treated with paclitaxel–bevacizumab and doxorubicin–cyclophosphamide, mastectomy with axillary dissection, and radiotherapy to the chest wall and axilla (50·4 Gy) at a different hospital elsewhere. After a disease-free interval of less than 6 months, she had an extensive biopsy-proven, unresectable inflammatory skin recurrence in June, 2013, and underwent four cycles of gemcitabine–carboplatin and a second course of radiotherapy with doses of 45–60 Gy, which she completed in March, 2014. She has since been disease free, with late radiotherapy toxicity consisting of chest wall telangiectasias and fibrosis, and had no evidence of disease from recurrent breast cancer on presentation at the hospital.
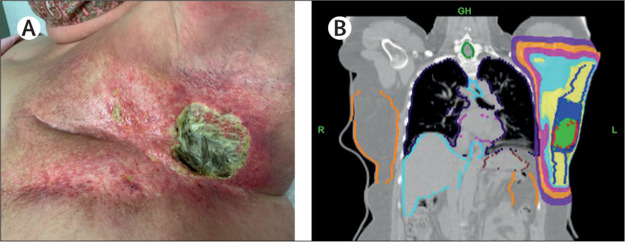
On presentation (figure, A ), there was intense erythema with well-demarcated borders confined to her left chest wall and a necrotic wound. These skin findings correlated anatomically to the radiotherapy dose gradient delivered 7 years previously (figure, B), with the greatest skin reaction (necrosis) in the region that had received the highest dose (shown in green on figure B). Laboratory investigations were notable for a positive SARS-CoV-2 nucleocapsid protein IgG, and elevated D-dimer, C-reactive protein, and erythrocyte sedimentation rate (all non-specific inflammatory markers). Complete blood count and comprehensive metabolic panel were normal, and interleukin-6 levels, which were measured to stratify COVID-19 disease severity, were normal. CT scan of the chest showed no lung parenchymal findings.
Figure.
Photograph of radiation recall and prior radiotherapy treatment plan
(A) Radiation recall consisting of confluent dermatitis and erythema of entire previously treated left chest wall with well-defined borders. Focal area of soft tissue necrosis in lateral left chest wall corresponds to region of highest radiation dose delivered 7 years earlier, coloured in green (B). GH=gantry head (superior). L=left. R=right.
She was diagnosed with radiation recall, a well-recognised inflammatory response of irradiated tissue triggered by anti-neoplastic therapy (most commonly), antibiotics, simvastatin, COVID-19 vaccination, or, in this case, COVID-19 infection. Until now, there has been only one other report of radiation recall in the context of COVID-19 infection with pneumonitis 3 years after radiotherapy for lung cancer. The present case is notable for the severity of the skin reaction correlating to the dose gradient many years after radiotherapy. Her symptoms initially improved with oral dexamethasone (4 mg of oral decadron twice daily for 3 days, followed by a taper over the following 9 days [4 mg daily for 3 days, 2 mg daily for 6 days]), wound care and debridement, and hyperbaric oxygen therapy (100% oxygen at 2·4 atmospheres absolute for 80 min × 50 treatments). However, after receiving her first viral-vector COVID-19 vaccination in July, 2021, the area of necrosis expanded. Biopsy showed extensive dermal sclerosis consistent with a radiotherapy effect without malignancy. She is currently planned to undergo vacuum-assisted wound closure and possible autologous tissue transfer.
Since most women with locoregional breast cancer maintain long-term disease control, follow-up presents many non-malignant and treatment-related issues. Radiation recall should be considered in the differential diagnosis when evaluating patients with localised symptoms and a history of radiotherapy treatment. COVID-19 infection, known to stimulate inflammation in tissues with elevated ACE2 receptors (such as lung and keratinocytes), can now be recognised as a trigger for this process. A thorough medical history evaluation and physical examination is important to distinguish between this typically self-limited benign disease and recurrent malignancy.
Declaration of interests
We declare no competing interests.
Acknowledgments
Contributors
RBR contributed to conceptualisation, investigation, methodology, writing of the original draft, review and editing, and visualization. RR contributed to conceptualisation, investigation, methodology, writing of the original draft, review and editing, visualisation, and supervision of the patient. Both authors contributed equally. Written informed consent to publication was obtained.