Abstract
Background:
Pediatric catheter-associated urinary tract infection (CAUTI) prevention guidelines encourage family engagement; however, there is a dearth of research on parent-facing CAUTI prevention resources. We aimed to meet the learning needs of parents about CAUTI prevention in the hospital by developing and refining an educational pamphlet with parents.
Methods:
Phase 1: We compiled existing evidence from CAUTI prevention guidelines and conducted a focus group with parents to form learning objectives. Phase 2: We developed prototype design elements, tested initial designs with a survey, and conducted qualitative participatory design sessions with parents to iteratively refine the pamphlet until design saturation was reached.
Results:
We identified the following key themes and preferences: 1) Clear boundaries for engagement (e.g., parents would not be emptying the catheter); 2) Positive, actionable framing (e.g., what should proper catheter positioning look like?); 3) What to expect (e.g. is the catheter painful for my child?); 4) Parents considered both their and their child’s comprehension of the content when providing feedback.
Conclusions:
Overall, we demonstrated the utility of remote participatory design methods in developing and refining a CAUTI prevention resource based on parents’ preferences. Future research should consider adapting these methods and implementing formal evaluation for comprehension for eventual integration into clinical practice.
Keywords: Patient and family engagement, patient safety, healthcare-associated infections, catheter-associated urinary tract infections, pediatric, infection prevention
Background
Catheter-associated urinary tract infections (CAUTI) are among the most frequently-occurring healthcare-associated infections in children and can lead to adverse complications such as kidney infections, antibiotic resistance, and in severe cases, death. 1–3 Nearly 70% of CAUTI are preventable through the implementation of evidence-based practices.2 Existing guidelines, including the CAUTI prevention implementation guide from the Association for Professionals in Infection Control and Epidemiology, highlight family-centered care approaches such as family education as integral facets of CAUTI prevention in children.4 Family members, caregivers, and/or legal guardians (hereinafter referred to as “parents”) are commonly present at the bedside and as such, may communicate changes in their child’s health status to their clinicians.4,5 Moreover, family-centered care approaches have a beneficial impact on pediatric quality of care and safety, parent satisfaction, and cost.6
Existing experimental interventions that involve the patient/family in CAUTI prevention provide little to no measurement of or description about their development, content, and/or implementation, which prevents us from understanding what components are or are not effective in communicating key messages to their target audiences.7–10 Moreover, CAUTI prevention interventions exist for adults but there is a dearth of existing research on parent-facing CAUTI prevention interventions in pediatrics, despite pediatrics having comparable incidence rates and risk of developing CAUTI compared to adults.1,3
Prior research on parent-facing engagement methods reveals that a combination of visuals, text, and prompts for communication are effective at promoting increased parental knowledge of chronic pediatric conditions and at-home fever management for children.11,12 Similarly important to note is that information should be presented in a comprehensible and accessible way to target users, as incomprehensible health information resources can lead to a ‘backfire’ effect in which parents might feel anxious, confused, overwhelmed, and/or fearful to initiate communication with the healthcare team.12 One effective way to communicate health information to a wide audience is by using information visualizations intended to support comprehension.13 For instance, researchers have successfully used visualizations with parents of varying levels of health literacy to communicate asthma management information, and to identify medication errors.14 Moreover, the use of visualizations as communication aids in pediatric medical consultations has shown promise in encouraging dialogue, recall, and parent understanding of their child’ s health condition.15,16
Despite a growing body of evidence that supports the use of parent-facing resources to improve the management of their child’s care and guideline recommendations to engage parents in CAUTI prevention, there is a dearth of research on the development of rigorous and testable resources regarding CAUTI prevention in hospitalized children.10 Therefore, the objective of this study is to meet the learning needs of parents about pediatric CAUTI prevention in the hospital setting by developing and refining the graphical and text elements of a parent-facing CAUTI prevention educational pamphlet.
Theoretical Framework
This study is guided by the Data-Frame Theory of Sensemaking, which asserts that users interpret information by fitting it into a ‘frame’ of understanding that is based on their experiences.17 Different ‘frames’ can be rejected and/or improved until the information ‘makes sense’ to them. In this study, we communicated with parents to determine the appropriate text and graphical elements that suggest an appropriate ‘frame’ that supports parents’ comprehension of key CAUTI prevention messages.
Methods
Formative Work
Prior to starting the design process, the research team obtained institutional review board approval for the study and conducted formative work to inform the prioritization of learning objectives for parents. The research team comprised three members: one PhD student in nursing, and two field experts – one PhD-prepared registered nurse with pediatric and infection prevention experience, and one PhD-prepared registered nurse specializing in participatory design methods. The team collated CAUTI prevention evidence-based practices by reviewing existing literature and CAUTI prevention guidelines to identify information relevant for parents. We arrived at four priority categories of information: 1) hand hygiene, 2) skin care and assessment, 3) bag care and assessment, and 4) warning signs/causes for concern.
We then developed a discussion guide and conducted a focus group with parents (N = 13) from a family advisory committee at a large academic pediatric medical center to learn about their experiences with urinary catheters and to obtain feedback on two existing CAUTI prevention resources. The existing resources were a hospital-created educational resource provided by the APIC Implementation Guide to Preventing CAUTI and a CDC flyer on healthcare-associated infection prevention.8,18 The goal of this focus group was to help the research team develop learning objectives and key messages for parents and learn about parents’ desired format for message delivery by presenting existing tools and obtaining feedback on aspects that parents found helpful or not.
Based on feedback from the focus group, we developed learning objectives and key messages (i.e., text that accompanied the graphics in the resource) for parents and decided that the resource would take the form of an informational pamphlet. We framed the key messages and corresponding ideas for images around the following assumptions:
The goal of this pamphlet is to provide parents with information about what a urinary catheter is, the risk of CAUTI, and steps to prevent CAUTI in their child. Features of the pamphlet that will support parents’ comprehension are an accessible reading level (i.e., 5th to 6th grade)19,20 and a combination of images and text.
We will display priority categories information based on suggestions from the focus group, which include: background information (e.g., what a catheter is), hand hygiene, proper catheter positioning, and warning signs/causes for concern (including assessment of the catheter bag and the surrounding skin).
We will display infection risk, stylistically, by reaching a balance of ‘friendly’ (e.g., cartoons) and ‘realistic’ imagery (e.g., anatomical figures), and we will convey infection risk through using imagery that shows the seriousness of the problem without overstating its severity and causing alarm.
Most of the pamphlet will be focused on handwashing because it is the most important way that parents can be involved in practicing infection prevention.
We will display both ‘dos and don’ts’ of proper urinary catheter positioning.
We then collaborated with an illustrator/graphic designer to prototype multiple options for each of the graphical elements used to depict the list of key messages. The subsequent study procedures used this set of prototype graphical elements as a starting point for the visual content of the pamphlet.
Study Design
This study was conducted in two phases: Phase 1 was an online survey that elicited parents’ image preferences and rankings on the relative importance of key informational elements. This information was used to inform the initial prototype design of the pamphlet by narrowing down the images judged by parents to be most effective for illustrating each of the key concepts. The survey also served to identify the amount of information parents desired on certain topics. Phase 2 comprised individual participatory design sessions based on established methods,13,21 during which parents were shown various prototype pamphlet designs, discussed which designs they preferred, and gave feedback on how these could be improved. The design of the pamphlet was iteratively refined over the course of the sessions based on the feedback.
In studies of this nature, iterative participatory design sessions are typically conducted in person with small groups of participants (~4–10) to help establish group consensus and get detailed feedback.22 However, in-person group data collection was not possible because Phases 1 & 2 occurred during the months of April – July 2020, during the first wave of the COVID-19 pandemic in the United States.23 Therefore, we used the online surveys as a means of establishing broad consensus and the individual design sessions to elicit rich and detailed feedback. All data collection occurred using HIPAA-compliant online survey and video conference platforms.
Setting and Sample
Participants were eligible for either phase of the study if they self-reported the ability to see and read large print English text and were the primary parent (or caregiver/guardian) of at least one child aged 6 to 12 years old. We found it necessary to select a specific age range due to the varying developmental needs of the pediatric population. We selected school-age children due to their relatively stable stage of physical development, during which they’re not undergoing the substantial milestones seen at younger ages that would impact the implementation of CAUTI prevention principles (e.g., need for diapers, crawling, etc.). Participants were excluded if they had prior experience with having or caring for someone with a urinary catheter as the purpose of the educational resource is to communicate information to an audience with no prior urinary catheter experience or awareness. Therefore, inexperienced participants provided feedback and observations that represent the experiences of the target audience.
Participants were recruited using snowball sampling through e-mail and internet using connections within the social and professional networks of the study team, and through online platforms (i.e., Facebook, LinkedIn, Twitter, Reddit, Craigslist, Prolific) using IRB-approved scripts and advertisements that were targeted towards parent community groups on Facebook across the US, and communities in the New York City area on Craigslist.
Data collection
Surveys (Phase 1).
After prototype graphical elements were created, we conducted Phase 1 of the study through an online survey software (Qualtrics). The survey included a total of 24 items (Appendix A).
In first part of the survey, we showed multiple prototype graphical elements to represent each of the following and asked parents to select the image(s) they felt would “get the message across clearly”: 1) pamphlet cover, 2) illustrations of germs in the bladder, 3) icons to represent ways parents can help prevent infection, and 4) icons to represent ‘prompts to communicate with healthcare team’. Participants were able to select more than one option to indicate their preferences. We also provided an ‘other’ box with each group of images, asking parents to ‘describe the image that you would prefer’.
In the next part of the survey, we presented multiple ‘importance ranking’ questions to determine the desired level of emphasis for broader categories that would likely contribute to comprehension of key messages. The 5-point importance ranking scale ranged from “not at all important” to “extremely important”. These topics included: 1) What a urinary catheter looks like (i.e., “How important is each of these things to you when learning about what a urinary catheter looks like?”) and 2) Handwashing (i.e., “How important is each of these things to you when learning about washing your hands or using hand sanitizer?”) Again, we provided ‘other’ slots where we asked what additional information participants would like to know. At the end of the survey, we inquired about any additional information participants would like to know in an educational resource about urinary catheters in their child, followed by a brief demographic questionnaire. We applied the results of this survey to the prototype pamphlet designs that were subsequently presented in the design sessions.
Design Sessions (Phase 2).
In Phase 2, designs were refined based on parent feedback. One or two members of the team conducted remote individual participatory design sessions using HIPAA-compliant video-conference software with eligible participants. At the beginning of the 60 to 90 minute-long sessions, a member of the research team obtained informed consent from the participant, conducted a health literacy assessment using the Newest Vital Sign (Out of 6 possible points, a score of 0–1 indicates a high likelihood of limited health literacy, 2–3 indicates the possibility of limited literacy, and 4–6 almost always indicates adequate literacy) and collected demographic information.24 Video calls were video-recorded after demographic information was collected. Next, participants were provided with brief background information on urinary catheters and were presented with various graphical elements and text relating to predetermined key messages to be included in the resource on individual PowerPoint slides. The interviewer(s) followed a semi-structured discussion guide (Appendix B) to elicit feedback from participants based on the images and/or text presented. Participants were first asked about their initial impressions of the elements presented, and for images presented side-by-side, we asked more in-depth questions about their preferences between them and encouraged suggestions for improvement including whether to add or remove any information. In later iterations where the pamphlet was presented as a whole, participants were asked to ‘talk the interviewer through’ what they were seeing and were asked for their impressions of the layout and format. Then, the interviewer(s) focused on each section of the pamphlet and asked for suggestions. If participants disliked an element, they were shown alternative image options and asked about their thoughts for improvement.
One researcher took detailed field notes of participant feedback and reactions to the pamphlet during the sessions, and audio recordings were transcribed following each session. Each participant was compensated with a $50 gift card for their time. The research team collectively discussed observations and feedback from design sessions during weekly team meetings. Proposed changes were summarized and communicated to the illustrator who applied changes to the pamphlet accordingly. Generally, changes were applied to an image after being suggested in at least two design sessions. To confirm the preference for the design changes, we presented the images side-by-side in following design sessions and asked participants to identify the preferred image, and provide suggestions for improvement, if any. Design sessions were conducted until design saturation, meaning that participants were no longer providing feedback that would have a substantive impact on the design or comprehensibility of the pamphlet.25
Data Analysis
Survey responses were analyzed using descriptive statistics. At the end of the design sessions, one researcher performed a content analysis on the transcripts to extract thematic categories, which were discussed to consensus with the research team weekly as a means of validating design decisions. The team maintained an audit-trail of the various iterations of the resource, accompanied by the corresponding design session and field note transcriptions from each session.
Results
Participants
Phase 1
A total of 89 participants completed the Phase 1 survey. Most participants were female (n = 53, 59%), White or Caucasian (n = 65, 73%), with a 4-year college degree (n = 33, 37%) or professional degree/doctorate (n = 22, 24.7%), with one child (n = 59, 66.3%). The demographic characteristics of participants in Phase 1 are detailed in Table 1.
Table 1.
Summary of demographic characteristics from total participants in Phase 1 (survey indicating feedback on initial design elements)
| Demographic | n (N = 89) | % |
|---|---|---|
|
| ||
| Sex | ||
|
| ||
| Male | 36 | 40.4 |
| Female | 53 | 59.6 |
| Education | ||
| Less than High School | 1 | 1.1 |
| High School Diploma or GED | 15 | 16.9 |
| Some college or technical school | 13 | 14.6 |
| 2-year degree | 5 | 5.6 |
| 4-year degree | 33 | 37.1 |
| Professional degree/Doctorate | 22 | 24.7 |
| Race | ||
| White | 65 | 73 |
| Black or African American | 9 | 10.1 |
| Native American or Alaska Native | 1 | 1.1 |
| Asian | 14 | 15.7 |
| Native Hawaiian or Pacific Islander | 0 | 0 |
| Another race not listed | 2 | 2.2 |
| Hispanic, Latino, Spanish Origin | ||
| Yes | 14 | 15.7 |
| No | 74 | 83.1 |
| No Response | 1 | 1.1 |
| Number of Children | ||
| One | 59 | 66.3 |
| Two | 29 | 32.6 |
| Three | 1 | 1.1 |
Phase 2
In Phase 2, we conducted a total of 10 individual design sessions with participants (7 female, 3 male). Race/ethnicity representation in the sample included: Hispanic (n = 2, 20%), Asian (n = 3, 30%), Black/African American (n = 2, 20%), and White (n = 3, 30%). The average age of participants was 41 years old. Most participants were bachelor’s prepared (n = 7, 70%), married (n = 7, 70%), and employed full time (n = 6, 60%) with commercial insurance (n = 7, 70%). On average, participants had 2 children, whose ages ranged between 2 and 13 years old. The average score on the NVS Health Literacy was 4.6 (adequate literacy), with scores ranging between 2 (possibility of limited literacy, n = 1) to 6 (adequate literacy, n = 4).
Survey Outcomes
A summary of data fields and results are provided in Appendix A. Overall, respondents reacted favorably to the cover image that depicted a family (n = 60, 58.8%). Respondents did not show a clear preference to see a realistic image of a bladder (n = 60, 47.6%) compared to a cartoon-style depiction of germs (n = 54, 60.7%), which led us to present all options in the first design session. Respondents preferred either icons (n = 29, 28.4%) or checkmarks (n = 59, 57.8%) to represent the three sections of the brochure.
In terms of importance ranking, parents found it extremely important or very important to see what the structure of the catheter looks like outside the body after it is inserted (n = 77, 86.5%), and what the entire structure of the catheter looks like (n = 77, 86.5%). Nearly all participants found the handwashing prompts to be moderately to extremely important (ranging from 85 (95.5%) to 88 (98.9%)). Lastly, after analyzing open-ended responses, we found that participants wanted to know additional details about the risks of CAUTI, how to assess the catheter, and who to contact if they notice something wrong with the catheter.
Design Session Outcomes
We tested 14 prototype graphical elements for inclusion in the initial survey. Of these, 4 were retained for the final pamphlet and an additional 13 were developed throughout the design process. After 10 rounds of design sessions, we arrived at a final pamphlet that parents indicated met our learning objectives. The final design had combinations of imagery and text on a double gate-folded pamphlet design with 8 panels (Appendix C) that comprised a cover page (Figure 1), an inner spread (Figure 2), a main spread (Figure 3), and a back cover (Figure 4). Participants in later sessions who saw the full pamphlet reacted favorably to it, as exemplified by the following quotes:
Figure 1.
Rendering of the Cover Image of the Final Pamphlet
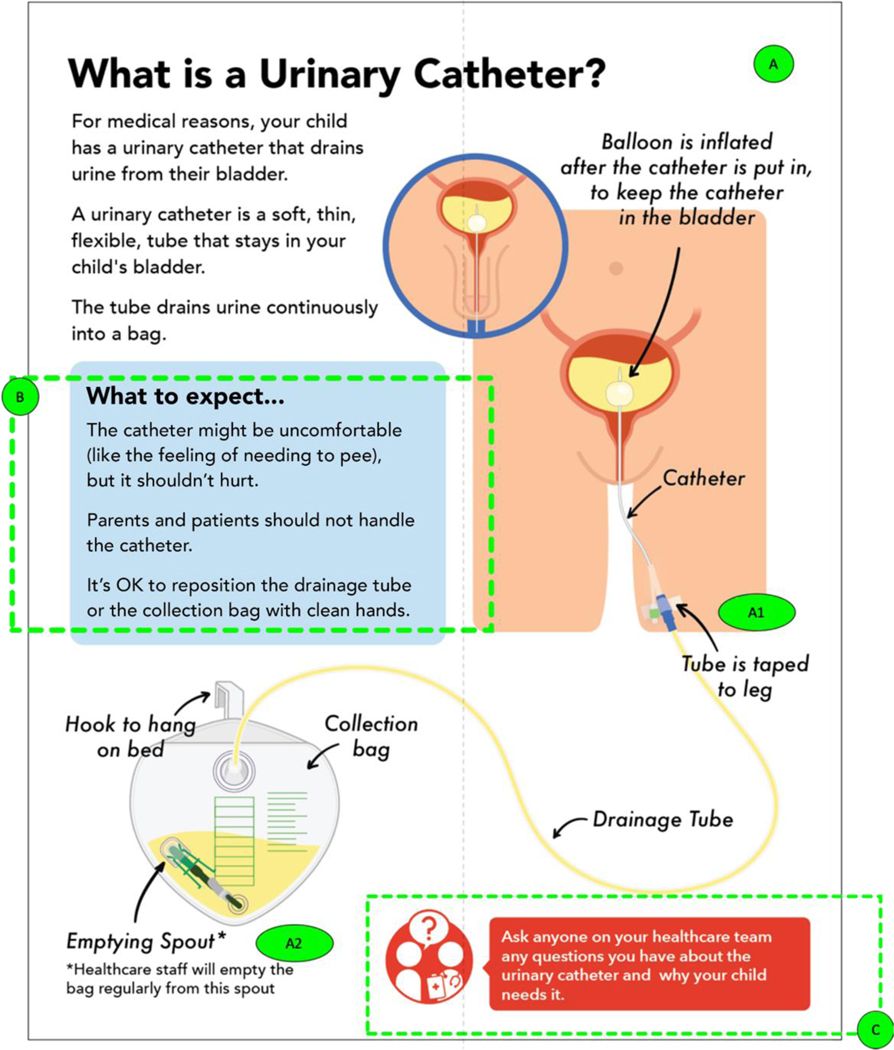
Figure 2. Annotated Rendering of the Inner Spread of the Final Pamphlet.
A- This page is an introduction to the basic structure and functioning of a urinary catheter, along with a visual representation of what the urinary catheter looks like both inside and outside the body; A1 & A2 – Labels placed to show parts of the catheter with clarification that the healthcare staff will empty the bag; B – What to Expect section added to describe the subjective experience of the child and provide additional boundaries for what parents can interact with; C– Prompt to communicate with healthcare team if parents have more specific questions about their child’s urinary catheter.
Figure 3. Annotated Rendering of the Main Spread of the Final Pamphlet.
D – Section introducing the risk of CAUTI with use of a urinary catheter; D1 – Image depicting bladder infection with redness, pain lines, and arrow; E – Introduction to the subsequent sections of the pamphlet, with 3 actionable components in which parents can be involved; F – Notification for parents to check in with healthcare team about the necessity of the catheter because risk of CAUTI increases with additional catheter days; G – Hand hygiene section 1 (of 3) – describes the significance of handwashing and highlights commonly missed areas of the hand to emphasize thorough hand hygiene procedures; H – Hand hygiene section 2 – describes general directions to wash and dry hands; I – Hand hygiene section 3 – describes optimal procedure for using hand sanitizer effectively; J – Hand hygiene call-out – prompt for parents to advocate for their child by encouraging anyone in contact with their child to wash their hands; K – Summary of what proper catheter positioning should look like, with visual indicators and descriptive sentences that include steps on how to maintain proper positioning.
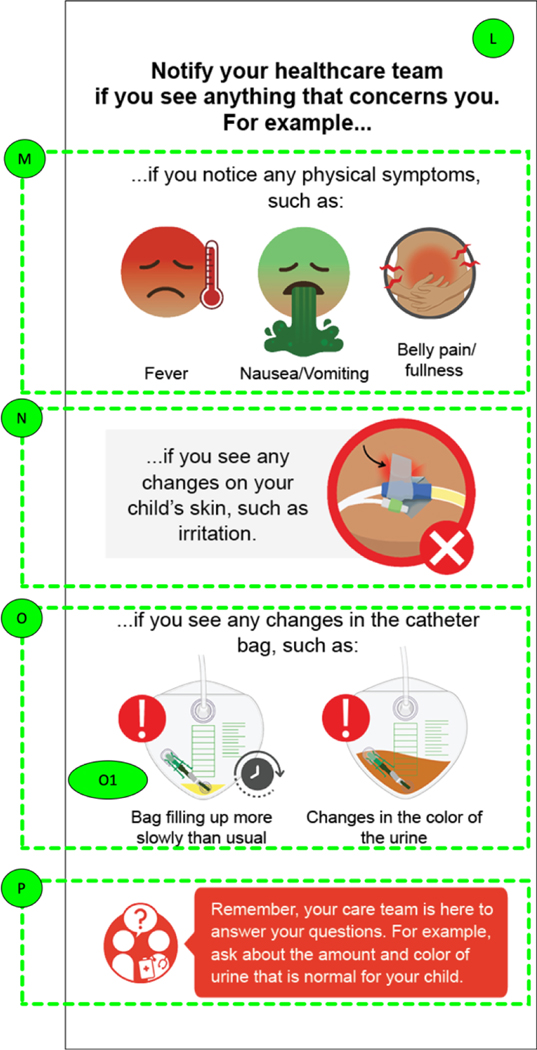
Figure 4. Annotated Rendering of the Back Cover of the Final Pamphlet.
L – Back cover: Causes of concern and reasons to notify your healthcare team; M – Depiction of physical symptoms that may indicate signs of infection; N – Skin irritation depicted to demonstrate the catheter tubing pulling on the skin, or irritation caused by the tape; O – Changes in the catheter bag depicted with two scenarios that parents can observe; P – Call to action for parents to communicate with the healthcare team to identify what ‘normal’ values to look for in their child’s specific scenario.
I would be motivated to be involved-- it has enough imagery, and it’s a good balance of imagery and text. It’s not fully text and not full imagery, but it hits on the most important points for the parent to know. -Session 7, Mother of 4 children between ages 5–12 years old.
I think this really does a good job of explaining what the key factors I should be looking for in a child [are]. – Session 10, Father of 2 and 6-year-old
Throughout the design sessions, parents provided feedback relating to imagery, supporting text, and formatting that they felt best supported comprehension of the intended messages. The following thematic categories emerged from parents’ feedback that most contributed to content acceptability: 1) boundaries for engagement; 2) positive, actionable framing, 3) risk conveyed explicitly; 4) anticipatory guidance; 5) parent and child comprehension.
Boundaries for engagement
Parents wanted us to clearly communicate the boundaries of how they should and should not interact with the catheter and preferred to see clear indications on the ways in which they could contribute to care, and what the healthcare team would be responsible for. For example, we removed the label “port to inflate balloon” from a diagram of a catheter based on a suggestion from a parent because only trained members of the healthcare team could access this port and did not want to know about it if they could not be involved. We replaced this label with another label “taped to leg” (Figure 2, Annotation A1) because parents can be engaged by monitoring whether the tape is securely adhered to their child’s leg.
Additionally, upon viewing the image of the entire structure of the catheter and seeing the label “Emptying spout” (Figure 2, Annotation A2), parents voiced concern about how they would empty the bag. As a result, we added a sub-note to our label, “emptying spout,” to indicate that that healthcare staff, not the parents, would be emptying the bag from this spout. The changes to these labels were well-received in following sessions.
Me, I probably would have tried to empty it from the spout, but, you know, now I know not to. So that’s good. –Session 4, Father of 10 and 4-year-old
Positive, Actionable Framing
Parents generally preferred positive framing of actionable messages. When considering the positioning of the urinary catheter, parents wanted to see images that showed what actions to take. For instance, when presented with both “dos” and “don’ts,” of proper catheter positioning, parents overwhelmingly preferred to see only the correct positioning of a urinary catheter, deeming the rest of the information unnecessary (Figure 3, Annotation K).
Between the picture and the wording, you know that this is what it’s supposed to look like. And you know what it’s not supposed to look like if you have any type of common sense. It clearly says don’t twist or bend the tubing. -Session 4, Father of 10 and 4-year old
Additionally, parents found that our negatively-framed message about handwashing was unnecessary (i.e., “Did you know? Parents don’t wash their hands as often as they should to prevent infection”). Parents only wanted to see what areas on the hand were commonly missed, and requested us to delete additional text in hand hygiene section 1 (Figure 3, Annotation G).
Conveying risks explicitly
Participants preferred to see imagery that explicitly denoted risks to indwelling urinary catheters, when choosing from among images representing a range of severity. One participant preferred that the image depicting a bladder infection should almost be threatening to bring across the intended message. For example, when shown several versions of an image of an inflected bladder, participants consistently chose the bright red, most severe-looking image with radiating pain lines (Figure 3, Annotation D1):
“I think, honestly, this? is more...I don’t want to say shock value, but it kind of is in a way. Like, if it gets infected, this it could be the result of it. Like we don’t want it to get to this point, basically.”– Session 7, Mother of 4 children between ages 5–12 years.
Also, another participant preferred to see ‘skin irritation’ with a lot of redness and texture to bring across the point that skin irritation is a cause for concern (Figure 4, Annotation L).
I get that it’s the catheter taped on the leg, but I didn’t get that it was irritation. Maybe show some bumps like the raised bumps or something. It’s irritating. Like 3-D it, make it really vibrant. You know, make it jump out. That would be really good. – Session 9, Mother of 10-year-old
Anticipatory Guidance
Subjective experience of the child.
Parents wanted to know what was to be expected as ‘normal’ and how to know if something was a cause for concern. In response to this information need, we added a ‘what to expect’ section in the introduction to the urinary catheter (Figure 2, Annotation B), because parents were often concerned about what the catheter would feel like and whether it would be painful.
The idea that knowing ... it might be a little uncomfortable...that’s comforting. You know, at least they’re not in pain, that this thing isn’t painful that’s attached to them. – Session 5, Mother of 11 and 3-year-old
Benchmarks for normal values.
One of the warning signs featured in the pamphlet is if the catheter bag contains less urine than usual (Figure 4, Annotation O1). However, parents requested specific benchmark values for volume of urine, or a reference point so they would be able to determine what was considered ‘normal’.
What is less urine? What will be a concerning ‘less amount’ of it? ... At what level will I have a red flag? That’s not in this picture. – Session 1, Mother of 9-year-old and 7-year-old I would probably use like a little arrow...Like this might be normal for your child, anything less than normal in that time period is not. – Session 7, Mother of 4 children between ages 5–12 years
This information is inherently difficult to depict because catheter use is a dynamic situation – not only do all children have varied levels of ‘normal’, but it is also difficult to depict in an illustration that the amount of urine in the bag depends on how long ago it was last emptied. To mitigate this, we added in a call-out text telling parents to ask their healthcare team what color and amount of urine is expected for their child.
Parent and Child Comprehension
When asked to react to the various sections of the pamphlet, parents also considered the potential for them to use the pamphlet to help teach their child about the intended message. For instance, one parent requested that we depict both female and male genitalia versions of the image used to illustrate the basic structure of a urinary catheter and its location inside the body. The parent considered how the resource could help both parents and children understand what the catheter looks like inside the body by giving additional context.
“I think it will be important that it is shown for boys, too, because it can be a little scary just to see that something is coming out of you. And also for parents, just to show that it’s going to look different.” – Session 1, Mother of 9 and 7-year-old
Additionally, when viewing images of the bladder depicting ‘bladder infections’, this participant preferred the image with the most context: this image depicted a bladder, germs inside the bladder, pain lines, and an arrow pointing upwards indicating germs moving up into the bladder (Figure 3, Annotation D1).
“I like to see how things work and how things are affected. And this would be good to explain to my child what’s going on in their body ... I want to show them, you know, this is what’s happening.” – Session 4, Father of 10 and 4-year-old
Discussion
Overall, parents provided valuable feedback that influenced the elements included in the pamphlet. Notably, many of the original design and content assumptions we made at the beginning of the study did not hold, which led to multiple iterations based on parent suggestions to improve the pamphlet until design saturation was reached.
In this study, we recognized that parents prefer to see CAUTI risk framed with severe imagery and wanted clear boundaries for elements they could act upon. For instance, parents preferred the most explicit depiction of bladder infection and skin irritation to portray risk of infection, and they preferred to see what they ‘should do’ to prevent CAUTI, rather than what they ‘should not do’. This was contrary to our assumptions that participants would prefer a balance between serious but not overstated or threatening to show the severity of infection risk, and that they would prefer to see both the ‘dos and don’ts’ of CAUTI prevention actions. The depiction of clear, actionable elements and severe risk are important to consider when testing future interventions regarding the sensemaking process17 that parents go through when learning about infection prevention. Furthermore, these preferences may be attributable to the fact that CAUTI may become severe, despite being largely preventable. This is also consistent with other studies that show that positive and negative framing preferences and effects on behavior can vary across resources depending on the condition and situation. For example, parents prefer gain-framing with vaccinations (e.g. peace of mind about child’s health) over loss framing (e.g. risk of illness) to prompt conversations with doctors, but when presented with messages to promote physical activity in their child, parents preferred loss framing (e.g. risks of physical inactivity) over gain framing (e.g. benefits of physical activity).26,27 Therefore, it is important to present multiple frames when testing the most appropriate way for conveying key messages in infection prevention, and allow the target audiences to determine their preferences for how the intended messages are portrayed.
We found that parents preferred and appreciated content that provided anticipatory guidance about the subjective experience of the child. Based on feedback, we added a section about ‘what to expect’, and parents especially appreciated the information indicating that the catheter may be uncomfortable but should not be painful. This is consistent with prior research in which parents were interested in receiving guidance on the subjective experience of their child, particularly in cases such as craniofacial abnormality and acute injury, where parents were consistently concerned with knowing how the child feels, how the change would affect their child, and what emotional and physical changes to expect in the future.28,29 Another study that used participatory design to develop tailored asthma infographics also showed that participants resonated the most with imagery that reflected their subjective experience of asthma and its severity.21 We did not anticipate including this information because it was out of the scope of our focus to provide enough context to encourage infection prevention practices. We assumed that further information about the subjective experience with the catheter would be communicated through verbal communication with the healthcare team. However, we found that this information was important to parents and provided them with a feeling of comfort.
Parents considered how the pamphlet would support their child’s comprehension alongside their own comprehension of key messages. We initially set a modest goal for the resource to support parent comprehension of key messages and did not specifically include information for children because the pamphlet is targeted for parents of children ages 6–12 years old, which includes a wide range of learning needs and requirements. However, in addition to their own interest in the pamphlet, parents were enthusiastic about using the pamphlet as a tool to teach their children. Prior research on engaging children in care is largely focused on preparing a child for a painful or invasive procedure or focus on improving self-management or coping with chronic conditions.30–33 Our study found that parents were interested in teaching their children about infection risk and infection prevention practices, which poses an opportunity for future research on how to best deliver this information to support both parent and child comprehension.
Limitations
There were several limitations to this study. First, design sessions were conducted virtually due to restrictions on in-person research. It is possible that certain cues and feedback were missed during design sessions, for instance, participants were unable to hold a physical copy of the pamphlet, which prevented feedback on the full experience of interacting with a physical artifact. Additionally, participants in virtual sessions were able to zoom in on images, which prevented us from fully assessing the acceptability of font size and smaller details in the images. Finally, because sessions were held individually, we were unable to facilitate group conversations about participants’ reactions to the pamphlet. We mitigated this limitation by conducting an online survey to reach consensus on priority imagery and messaging.
In terms of our final sample of participants, they generally had adequate health literacy levels (average score of 4.6 on a scale for which scores above 4 are considered adequate literacy), which may be because participants mostly consisted of those with a bachelor’s degree or higher (n = 8, 80%) and were recruited online and therefore have access to health information via the internet. More research is warranted among populations with low health literacy to ensure that graphical and text elements are comprehensible and clear, regardless of health literacy level. Lastly, our assessment of comprehension was informal and subjective, so we are unable to draw conclusions about how much content participants learned, or how they would enact that knowledge in an appropriate circumstance. As such, further research is needed in the clinical setting.
Conclusion
In this study, we summarized parents’ format and message-framing preferences to receive health information about CAUTI prevention in children. They reacted favorably to imagery and text that clearly communicated what their role was, preferred positively framed messaging, and were interested in learning more about the subjective experience of the child. Most messages needed to be accompanied by supplemental text, which underscores the importance for future research to include individuals with low health literacy. Additionally, we demonstrated that participatory design methods can be adapted to be remote, and future research should consider formal testing for comprehension of key elements and eventual integration into the clinical setting.
Supplementary Material
Acknowledgments
We would like to thank our graphic designer/illustrator, Lauren Berger for her instrumental role in creating this resource with us.
Funding
This research was supported by Reducing Health Disparities Through Informatics (RHeaDI), T32NR007969 at Columbia University School of Nursing
Footnotes
Conflicts of Interest
The authors have no conflicts of interest to declare in relation to the present manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mack EH, Stem CT. Prevention of CAUTIs, CLABSIs, and VAPs in Children. Curr Treat Options Pediatr. 2017;3(3):221–235. doi: 10.1007/s40746-017-0094-8 [DOI] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Catheter-associated Urinary Tract Infections (CAUTI). https://www.cdc.gov/hai/ca_uti/uti.html. Published 2015.
- 3.Letica-Kriegel AS, Salmasian H, Vawdrey DK, Youngerman BE, Green RA, Furuya EY, et al. Identifying the risk factors for catheter-associated urinary tract infections: A large cross-sectional study of six hospitals. BMJ Open. 2019;9(2). doi: 10.1136/bmjopen-2018-022137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Association for Professionals in Infection Control and Epidemiology. Guide to Preventing Catheter-Associated Urinary Tract Infections. 2014. [Google Scholar]
- 5.Eichner JM, Johnson BH, Betts JM, Chitkara MB, Jewell JA, Lye PS, et al. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129:394–404. doi: 10.1542/peds.2011-3084 [DOI] [PubMed] [Google Scholar]
- 6.Shields L, Zhou H, Pratt J, Taylor M, Hunter J, Pascoe E. Family-centred care for hospitalised children aged 0–12 years. Cochrane Database Syst Rev. 2012;10:CD004811-CD004811. doi: 10.1002/14651858.CD004811.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oman KS, Makic MBF, Fink R, Schraeder N, Hulett T, Keech T, et al. Nurse-directed interventions to reduce catheter-associated urinary tract infections. Am J Infect Control. 2012;40(6):548–553. doi: 10.1016/j.ajic.2011.07.018 [DOI] [PubMed] [Google Scholar]
- 8.Purvis S, Gion T, Kennedy G, Rees S, Safdar N, VanDenBergh S, et al. Catheter-associated urinary tract infection: A successful prevention effort employing a multipronged initiative at an academic medical center. J Nurs Care Qual. 2014;29(2):141–148. doi: 10.1097/NCQ.0000000000000037 [DOI] [PubMed] [Google Scholar]
- 9.Sarpong Y, Nattanmai P, Schelp G, Bell R, Premkumar K, Stapleton E, et al. Improvement in quality metrics outcomes and patient and family satisfaction in a neurosciences intensive care unit after creation of a dedicated neurocritical care team. Crit Care Res Pract. 2017:1–6. doi: 10.1155/2017/6394105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mangal S, Pho A, Arcia A, Carter E. Patient and family engagement in catheter-associated urinary tract infection (CAUTI) prevention: A systematic review [published online May 31, 2021]. Jt Comm J Qual Patient Saf. doi: 10.1016/j.jcjq.2021.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young M, Watts R, Wilson S. The effectiveness of educational strategies in improving parental/caregiver management of fever in their child: A systematic review. JBI Libr Syst Rev. 2010;8(21):826–868. doi: 10.11124/jbisrir-2010-148 [DOI] [PubMed] [Google Scholar]
- 12.Nightingale R, Friedl S, Swallow V. Parents’ learning needs and preferences when sharing management of their child’s long-term/chronic condition: A systematic review. Patient Educ Couns. 2015;98(11):1329–1338. doi: 10.1016/j.pec.2015.05.002 [DOI] [PubMed] [Google Scholar]
- 13.Arcia A, Suero-Tejeda N, Bales ME, Merrill JA, Yoon S, Woollen J, et al. Sometimes more is more: iterative participatory design of infographics for engagement of community members with varying levels of health literacy. J Am Med Inform Assoc. 2016;23(1):174–183. doi: 10.1093/jamia/ocv079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin HS, Gupta RS, Mendelsohn AL, Dreyer B, van Schaick L, Brown CR, et al. Use of a low-literacy written action plan to improve parent understanding of pediatric asthma management: A randomized controlled study. J Asthma. 2017;54(9):919–929. doi: 10.1080/02770903.2016.1277542 [DOI] [PubMed] [Google Scholar]
- 15.Kaufman J, Ryan R, Walsh L, Horey D, Leask J, Robinson P, et al. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev. 2018;2018(5). doi: 10.1002/14651858.CD010038.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnekow K, Shyken P, Ito J, Deng J, Mohammad S, Fishbein M. Magnetic resonance imaging: A personalized approach to understanding fatty liver disease. J Pediatr Gastroenterol Nutr. 2019;68(6):777–781. doi: 10.1097/MPG.0000000000002316 [DOI] [PubMed] [Google Scholar]
- 17.Klein G, Phillips JK, Rall EL, Peluso D. A data-frame theory of sensemaking. Expert out Context Proc Sixth Int Conf Nat Decis Mak. January 2007:113–155 [Google Scholar]
- 18.Centers for Disease Control and Prevention. Despite progress, ongoing efforts needed to combat infections impacting hospital patients. CDC Press Release. https://www.cdc.gov/media/releases/2014/p0326-hospital-patients.html. Published 2014. [Google Scholar]
- 19.The Joint Commission: Advancing effective communication, cultural competence, and patient- and family-centered care: A roadmap for hospitals. Oakbrook Terrace, IL: The Joint Commission, 2010. [Google Scholar]
- 20.Weiss BD. Health literacy: A manual for clinicians. Chicago: American Medical Association, 2008. [Google Scholar]
- 21.Arcia A, George M, Lor M, Mangal S, Bruzzese JM. Design and comprehension testing of tailored asthma control infographics for adults with persistent asthma. Appl Clin Inform. 2019;10(4):643–654. doi: 10.1055/s-0039-1693713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arcia A, Bales ME, Brown W 3rd, Co MC Jr, Gilmore M, Lee YJ, et al. Method for the development of data visualizations for community members with varying levels of health literacy. AMIA Annu Symp Proc. 2013;2013:51–60. [PMC free article] [PubMed] [Google Scholar]
- 23.Cucinotta D, Vanelli M. WHO Declares COVID-19 a pandemic. Acta Bio-Medica Atenei Parm. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weiss BD, Mays MZ, Martz W, Merriam Castro K, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: The newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arcia A, Suero-Tejeda N, Spiegel-Gotsch N, Luchsinger JA, Mittelman M, Bakken S. Helping Hispanic family caregivers of persons with dementia “get the picture” about health status through tailored infographics. The Gerontologist. 2019;59(5):e479–e489. doi: 10.1093/geront/gnz085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gainforth HL, Cao W, Latimer-Cheung AE. Message framing and parents’ intentions to have their children vaccinated against HPV. Public Health Nurs. 2012;29(6):542–552. doi: 10.1111/j.1525-1446.2012.01038.x [DOI] [PubMed] [Google Scholar]
- 27.Drouin O, Young M, King N. Message framing and counseling of parents on children’s physical activity – An experimental study. Health Psychol Behav Med. 2018;6(1):214–225. doi: 10.1080/21642850.2018.1515018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wiseman T, Curtis K, Young A, Van C, Foster K. “It’s turned our world upside down”: Support needs of parents of critically injured children during emergency department admission - A qualitative inquiry. Australas Emerg Care Online. 2018;21(4):137–142. doi: 10.1016/j.auec.2018.09.002 [DOI] [PubMed] [Google Scholar]
- 29.Billaud Feragen K, Myhre A, Stock NM. “Exposed and vulnerable”: Parent reports of their child’s experience of multidisciplinary craniofacial consultations. Cleft Palate Craniofac J. 2019;56(9):1230–1238. doi: 10.1177/1055665619851650 [DOI] [PubMed] [Google Scholar]
- 30.Knibb RC, Alviani C, Garriga‐ Baraut T, Mortz CG, Vazquez-Ortiz M, Angier E, et al. The effectiveness of interventions to improve self‐ management for adolescents and young adults with allergic conditions: A systematic review. Allergy. 2020;75(8):1880–1897. doi: 10.1111/all.14269 [DOI] [PubMed] [Google Scholar]
- 31.Ramsey RR, Plevinsky JM, Kollin SR, Gibler RC, Guilbert TW, Hommel KA. Systematic review of digital interventions for pediatric asthma management. J Allergy Clin Immunol Pract. 2020;8(4):1284–1293. doi: 10.1016/j.jaip.2019.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rantala A, Pikkarainen M, Miettunen J, He HG, Pölkki T. The effectiveness of web-based mobile health interventions in paediatric outpatient surgery: A systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. 2020;76(8):1949–1960. doi: 10.1111/jan.14381 [DOI] [PubMed] [Google Scholar]
- 33.Birnie KA, Noel M, Chambers CT, Uman LS, Parker JA. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2018;2018(10). doi: 10.1002/14651858.CD005179.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.