Abstract
Pneumatosis cystoides intestinalis (PCI) is a rare condition characterized by the presence of air collection within the subserosa and/or submucosa of the gastrointestinal wall. Due to the lack of specific symptoms, PCI is likely to be misdiagnosed or missed without the use of imaging techniques or gastrointestinal endoscopy. Here, we report a patient who complained of abdominal distention and constipation after chemotherapy for hematological malignancies, and was diagnosed with secondary PCI via computed tomography (CT) and exploratory laparotomy. Pneumoperitoneum was no longer observed after two weeks of conservative treatments. Notably, the possibility of intra-abdominal pressure (IAP) as a predictor for surgical intervention was proposed. Furthermore, we conducted a literature review on PCI after chemotherapy in hematological malignancies to raise awareness of etoposide-related PCI, while whether PCI could be identified as an adverse event of etoposide requires more evidence.
Keywords: Pneumatosis cystoides intestinalis, Pneumoperitoneum, Intra-abdominal pressure, Etoposide, Hematological malignancy
Introduction
Pneumatosis cystoides intestinalis (PCI), first described by Du Vernoi in 1730, is characterized by the presence of air collection within the subserosa and/or submucosa of the gastrointestinal wall particularly in the ileum and colon [1, 2]. PCI is a rare condition that lacks accurate morbidity estimates due to the lack of specific symptoms, and should be suspected in the setting of pneumoperitoneum or free gas under the diaphragm without peritoneal irritation [3]. An increasing number of cases have been identified recently with the assistance of imaging examination and gastrointestinal endoscopy. The clinical manifestations of PCI vary from asymptomatic to lethal conditions, and common symptoms include abdominal pain, abdominal distention, nausea, vomiting, diarrhea and constipation [4, 5]. Primary PCI, which is relatively uncommon, is defined as an idiopathic disorder, and has been reported to be closely associated with chronic trichloroethylene exposure [6]. PCI secondary to various clinical conditions accounts for 85% of cases [7], including: (a) mechanical trauma: acute gastrointestinal diseases [8], and gastrointestinal carcinoma [9]; (b) autoimmune disorders: inflammatory bowel diseases (IBD) [10], and connective tissue diseases [11–13]; (c) infections: Clostridium difficile [14], and HIV [15, 16]; (d) pulmonary diseases: chronic obstructive pulmonary disease (COPD) [17]; (e) immunosuppressive states: during and after chemotherapy for malignant tumors [18, 19], and post hematopoietic stem cell transplantation (HSCT) [20]; and (f) drug induced: diabetes treated with alpha-glucosidase inhibitors (α-GI) [5]. Here, we present a case of PCI after etoposide-related chemotherapy for hematological malignancies that was initially misdiagnosed as gastrointestinal perforation with equivocal CT findings and underwent an exploratory laparotomy, confirming the diagnosis of PCI.
Case presentation
A 14-year-old male patient was urgently sent to our hospital due to sudden dyspnea and disturbance of consciousness four hours earlier. He had complained about a week of vague body pain and two days of fever, progressively worsening manifesting as distinct abdominal distension and an absence of flatus one day before, with a small amount of stool being observed the day before.
Suffering from recurrent fever and noticeable enlargement of cervical lymph nodes, this pediatric patient was diagnosed with chronic active Epstein-Barr virus (CAEBV) infection a year earlier before and received long-term treatment with prednisone (40 mg/d). The parents were healthy and denied a history of familial cancers or genetic disorders. Herpes with rupture on the inner left thigh prompted the first visit to our hospital two months prior, when the patient had developed EBV-lymphoproliferative disease (EBV-LPD) merged with hemophagocytic syndrome (HPS). The ED regimen (etoposide 100 mg biw + dexamethasone 15 mg qd) was initiated three weeks earlier. Given the potential of lymphoma, tislelizumab, an inhibitor of programmed cell death-1 (PD-1), was provided at a dose of 100 mg two weeks earlier. The dose of primary regimen was reduced due to hyperpyrexia occurring five days later, which was presumed to be related to cytokine release syndrome (CRS) induced by the PD-1 inhibitor. The cumulative dose of etoposide was 425 mg. The patient did not complain of any abdominal discomfort in the week after using tislelizumab, and the stool was normal.
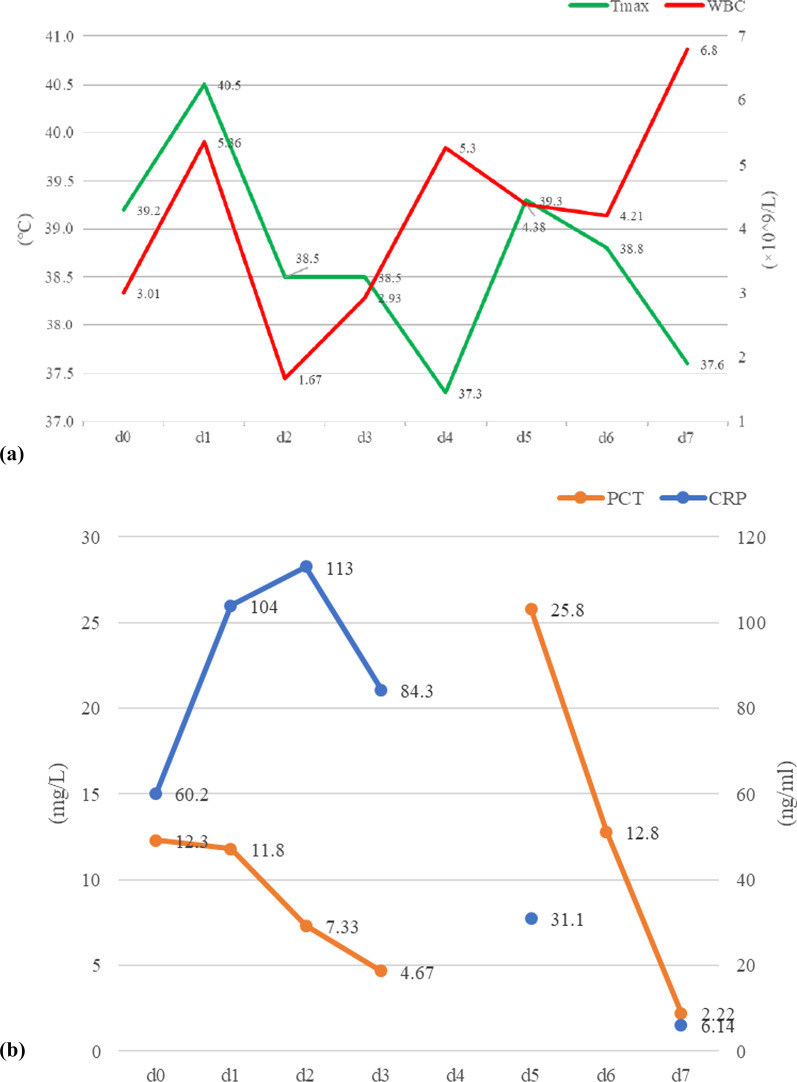
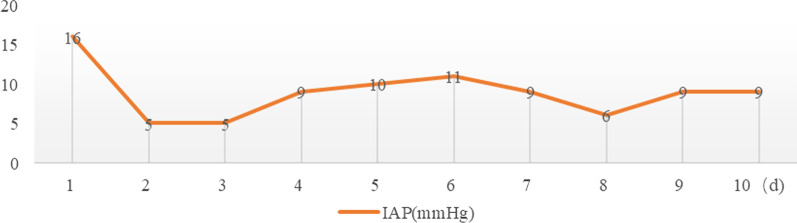
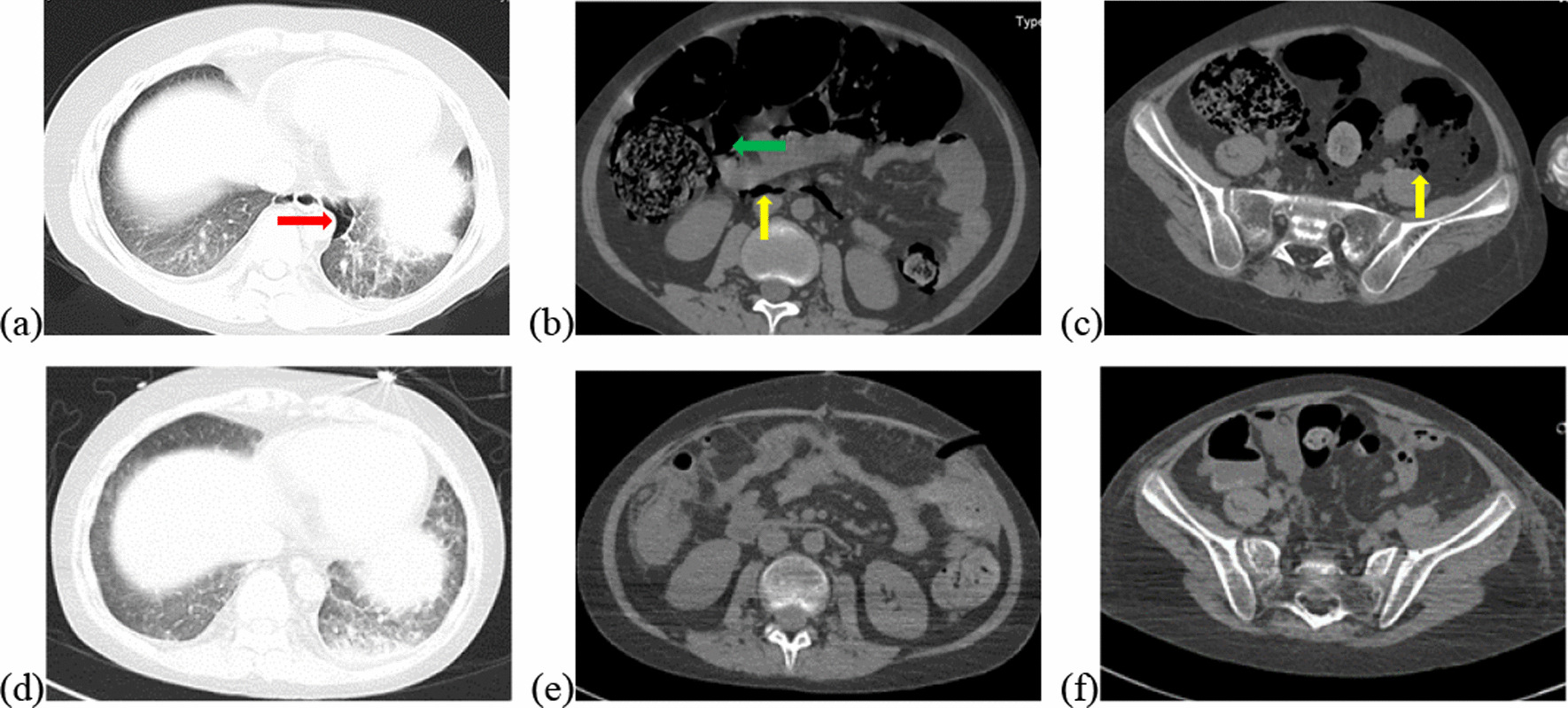
Vital signs at admission were as follows: T 38.4℃, P 190 bpm, R 25 bpm, BP 122/87 mmHg, and SpO2 70%. An abdominal CT scan demonstrated that massive free gas was collecting within the colon wall (Fig. 1b), and even within the retroperitoneal space of the abdominal (Fig. 1b) and pelvic cavities (Fig. 1c), without enough evidence for peritonitis or seroperitoneum. Free air could be observed in the mediastinum in the lung view of chest CT (Fig. 1a) with slight pulmonary inflammation. Since we suspected gastrointestinal perforation, an exploratory laparotomy was performed immediately but no inflammation or gastrointestinal perforation was discovered. Intriguingly, gas accumulation was observed throughout the mesocolon wall with noteworthy crepitus (Fig. 2), confirming the diagnosis of PCI. The patient was admitted to the intensive care unit due to failure of postoperative tracheal extubation. Arterial blood gas analysis showed: pH 7.398, PaO2 179.9 mmHg, PaCO2 25.7 mmHg, lactic acid 2.3 mmol/L, and HCO3 15.5 mmol/L. Subsequent auxiliary examinations supported the activation of EBV infection with an increased level of EBV-DNA (3.29 × 104 copies/ml) and impairment of the immune system (CD3 counts 555 cell/ul, CD4 counts 123 cell/ul, CD8 counts 392 cell/ul). Furthermore, HPS was activated with the presentation of pancytopenia (HGB 68 g/L, WBC 3.01 × 109/L, PLT 36 × 109/L) and prominent elevation of ferritin (27,487 ng/ml) and IL-2R (1752 u/ml). Simultaneous liver function tests exhibited the following: AST 109 IU/L, ALT 60 IU/L, ALP 512 IU/L, and LDH 2479 IU/L. Body temperature and inflammatory biomarkers observed the following week are presented in Fig. 3. Prolonged fever was assumed to be associated with HPS since repeated secretion and serological cultures for etiological evidence of infection were inconclusive, and the determination for Clostridium difficile infection was not performed. Considering acute respiratory failure syndrome (ARDS) and latent intestinal infections, mechanical ventilation and antibiotic therapy were provided. In addition, nasogastric tube drainage and parenteral nutrition were both administered. Chemotherapy was interrupted and replaced by an injection of dexamethasone (7.5 mg/d) without additional adverse effects. Abdominal distention and constipation were gradually alleviated, and little free gas was observed in the bowel wall two weeks later (Fig. 1d–f). Furthermore, intra-abdominal pressure (IAP) was measured based on the trans-bladder technique in the first ten days (Fig. 4), which suggested an elevated IAP in the beginning, consistent with the significant abdominal distention.
Fig. 1.
Initial abdominal CT and one week later. Initial abdominal CT scan showed massive free gas collected in the colon wall denoted by the green arrow (b). The gas could even be observed in the mediastinum in the lung view (a) denoted by the red arrow, retroperitoneal space in the abdomen (b) and pelvic cavities view (c) denoted by the yellow arrows. Free accumulated gas was gradually absorbed after one week of conservative treatments in the same view (d–f)
Fig. 2.

Intraoperative finding in exploratory laparotomy. Several bright bubbles could be observed within the colon wall with noteworthy crepitus. A bubble was denoted by the red arrow
Fig. 3.
Observation of body temperature and inflammatory biomarkers in the following week (d1–d7) after the surgery. Abbreviation: Tmax = the highest body temperature in the day (the green line), WBC white blood cells (the red line), PCT procalcitonin (the orange line), CRP C reaction protein (the blue line)
Fig. 4.
IAP was measured based on the trans-bladder technique in the first ten days
Search strategy and literature review
PCI is a benign phenomenon of pneumatosis intestinalis (PI), which is more frequently reported in adults and males according to a systematic analysis [21]. According to a literature review, PI in hematological disorders was frequently reported in debilitated patients after bone marrow transplantation, complicated with cutaneous or digestive graft versus host diseases (GVHD) in particular [22–26], while the significance of causative agents remains to be explored due to a limited number of cases. Hence, we conducted an advanced retrieval in the PubMed database up to December 2021 with a result of 2878 articles based on the following search strings: “pneumatosis cystoides intestinalis” OR “pneumatosis intestinalis” OR “pneumatosis”. Reviews and cases concerning nonhematologic disorders were excluded, and six studies [27–32] were filtered from the original 34 results based on the inclusion criteria: (1) clinical cases with a detailed description; (2) hematologic malignancy as the major diagnosis; and (3) treatment post chemotherapy without allo-HSCT. Twelve cases reported in the selected literature are listed in Table 1, where steroids (prednisolone/dexamethasone) and etoposide were used to treat eleven and three patients, respectively, and no records referred to tislelizumab-related therapy.
Table 1.
Previous cases of PI/PCI post chemotherapy in hematologic malignancies
| Case [Ref.] | Sex/age (yr) | Underlying disease | Chemotherapeutics | Clinical symptoms | Diagnosis/tools/location | Treatments |
|---|---|---|---|---|---|---|
| 1 [27] | F/2.5 | c-ALL | Prednisone, daunorubicin, vincristine, asparaginase, and intrathecal triple therapy | Lethargy abdominal distension | PCI/X-ray/colon | Antibiotics |
| 2 [28] | M/55 | Ph + CML | Nilotinib | Abdominal distension abdominal pain | PI/CT/small intestine | Oxygen therapy |
| 3 [29] | M/31 | T-ALL | Cyclophosphamide, mercaptopurine, cytosine arabinoside, and prednisone | Abdominal pain | PI/X-ray + CT/colon | Parenteral nutrition antibiotics |
| 4 [29] | M/58 | Lymphoma | BCNU, melphalan, and etoposide, cytosine arabinoside and dexamethasone | None | PI/X-ray + CT/colon | Parenteral nutrition antibiotics |
| 5 [29] | F/64 | Lymphoma | Cyclophosphamide, vincristine, doxorubicin, and prednisone | Abdominal pain fever, nausea, diarrhea | PI/CT/small intestine + colon | Parenteral nutrition antibiotics |
| 6 [29] | F/49 | SAA | Ciclosporine A, prednisone | Fever | PI/CT/enterocoelia | Parenteral nutrition antibiotics |
| 7 [30] | M/18 | B-ALL | Prednisolone, daunorubicin, vincristine, asparaginase, and intrathecal methotrexate | Abdominal distension anorexia | PI/X-ray + CT /colon + enterocoelia | Oxygen therapy antibiotics parenteral nutrition |
| 8 [31] | F/33 | APL | ATRA, idarubicin, dexamethasone | Abdominal pain nausea, diarrhea | PI/CT/small intestine + colon | Antibiotics |
| 9 [32] | M/51 | Lymphoma | Methotrexate, leukovorine rescue, mithoxantrone, cyclophosphamide, vincristine, prednisolone, and etoposide | Vague abdominal discomfort | PCI/X-ray/colon | Oxygen therapy antibiotics parenteral nutrition |
| 10 [32] | F/42 | AML-M1 | Behenoyl cytosine arabinoside, daunorubicin, 6-mercaptopurine, and prednisone | Abdominal distension abdominal pain | PCI/X-ray/colon | Oxygen therapy |
| 11 [32] | F/58 | Lymphoma | Methotrexate, leukovorine rescue, mithoxantrone, cyclophosphamide, vincristine, prednisolone, and etoposide | Abdominal distension | PCI/X-ray/colon | Oxygen therapy parenteral nutrition |
| 12 [32] | M/74 | AML-M2 | Cytosine arabinoside, prednisolone, etopside, and mitoxantrone | Abdominal distension | PCI/X-ray/colon | Oxygen therapy parenteral nutrition |
F female, M male, ALL acute lymphocytic leukemia, CML chronic granulocytic leukemia, SAA severe aplastic anemia, APL acute promyelocytic leukemia, AML acute myeloblastic leukemia, PI pneumatosis intestinalis, PCI pneumatosis cystoides intestinalis, ATRA all-trans retinoic acid, BCNU carmustine
Although steroids have been proven to be significantly linked to the development of PCI [1, 33], our patient had received corticosteroid treatment for a long period even during PCI therapy. Therefore, further research on PCI/PI post chemotherapy based on etoposide and/or tislelizumab was conducted. As a novel monoclonal antibody in recent years, PD-1 inhibitors have shown great potential in hematologic malignancies, while reported side-effects concerning PI are lacking.
Six cases of PCI/PI associated with etoposide are described in Table 2 [29, 32, 34, 35]. Details including sex, age, underlying diseases, chemotherapy, causative agent, location, associated symptoms, diagnostic tool, treatments, outcome and time to recovery, were collected. The results suggested that abdominal distension was the most common symptom in etoposide-related PCI/PI. The majority of cases were diagnosed with X-ray (83.33%), and notably, the colon was the most frequent location (100%). Conservative treatments were effective and pneumoperitoneum subsided in no more than 30 days.
Table 2.
Previous cases of PI/PCI post etoposide-based chemotherapy
| Case [Ref.] | Sex/Age (yr) | Underlying disease | Chemotherapy | Causative agent, dose | Location | Diagnostic tools | Associated symptoms | Complications | Treatments | Outcome | Time to recovery |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 [29] | M/58 | Lymphoma | NA | Etoposide, NA | Total colon | X-ray + CT | None | No | Parenteral nutrition antibiotics | Resolved | 30 days |
| 2 [32] | M/51 | Lymphoma | MNCOP-V | Etoposide, 100 mg | Total colon | X-ray | Septicemia and abdominal discomfort | No | Oxygen therapy parental nutrition antibiotics | Resolved | NA |
| 3 [32] | F/58 | Lymphoma | MNCOP-V | Etoposide, 95 mg | Total colon + terminal ileum | X-ray | Slight abdominal distension | No | Oxygen therapy parental nutrition | Resolved | 1 week |
| 4 [32] | M/74 | AML-M2 | NA | Etoposide, NA | Total colon | X-ray | Abdominal distension | No | Oxygen therapy parental nutrition | Resolved | 2 weeks |
| 5 [34] | F/53 | Breast cancer | Various | Etoposide, 50 mg qd | Total colon + rectum | X-ray + CT + colonoscopy | Severe abdominal distension with decreased flatus | No | Oxygen therapy antibiotics | Resolved | 3 weeks |
| 6 [35] | M/69 | Small cell lung cancer | Carboplatin (d1) + etoposide (d1–3) | Etoposide, 100 mg | Sigmoid colon + retroperitoneum + posterior mediastinum | CT | Abdominal distension | No | Oxygen therapy antibiotics | Resolved | 2 weeks |
M male, F female, AML acute myeloid leukemia, MNCOP-V methotrexate with leucovorin rescue, mitoxantrone, cyclophosphamide, vincristine, prednisolone and etoposide, NA not available
Discussion and conclusion
In this study, we presented a 14-year-old male patient who suffered from EBV-related hematological malignancies developed PCI after chemotherapy. It was reasonable to consider the potential of gastrointestinal perforation due to the massive amount of free gas in the abdominal cavity and even within the mediastinum, and the dramatically deteriorated conditions. PCI was confirmed in our patient with exploratory laparotomy, although this has been reported less often in the literature. The pathogenesis of PCI remains to be explored involving four major hypotheses to be discussed [5, 21, 36]: (a) The mechanical theory; increased intraluminal colonic gas and pressure due to fever or ileus caused impaired structural integrity of the intestinal wall, leading to relative ischemia on the mesocolon side of the lumen allowing leakage of air. (b) The pulmonary theory; pulmonary alveolar rupture induced by chronic pulmonary diseases, reached the bowel wall along the aorta and mesenteric vessels. (c) The bacterial theory; immunity was reduced by chemotherapy medications, and aerogenic bacteria penetrated the mucosal barrier via the relative ischemic zone producing gas within the bowel wall. (d) The chemical theory or nutritional deficiency theory; the toxic effects of chemotherapy on cell proliferation and apoptosis led to a compromised self-healing function of the intestinal mucosa. Malnutrition, which frequently occurs in patients post chemotherapy, increases bacterial fermentation by interfering with the consumption of carbohydrates, causing a subsequent accumulation of gas and aggravated damage to the bowel walls.
To search for the specific causative agent in our case, a literature review was conducted focused on PI/PCI post chemotherapy without allo-HSCT in hematological malignancies, which indicated the possible pathogenicity of etoposide. As a broad-spectrum chemotherapeutic agent that negatively targets topoisomerase II, and interferes with the restoration of impaired DNA [37], etoposide has been approved for clinical use by the Food and Drug Administration (FDA) of the USA in small lung cell cancer, reproductive system tumors, hematological malignancies, etc. [38, 39]. PI/PCI after etoposide-based chemotherapy has been observed in patients with lymphomas, acute myeloid leukemia, small cell lung cancer and breast cancer (Table 2). A potential mechanism was proposed by PK Bhamidipati1 et al. [24]., stating that chemotherapy and immunosuppression might result in atrophy of Peyer’s patches, leading to loss of intestinal mucosa integrity and inducing intestinal infection or gas migration. In addition, pneumoperitoneum after chemotherapy could be a manifestation of neutropenic enterocolitis (NE) complicated with bowel perforation [40], which could aggravate mucosal damage and intestinal infection. While suspected tislelizumab-induced PCI should not be excluded, albeit no previous description has been published. Temporary agranulocytosis was observed in our patient, conferring a risk of infection. The gastrointestinal tract is known to be a commonly affected system, and enterocolitis induced by immune checkpoint inhibitors (ICIs) is considered to be a secondary cause of IBD [41], which is more frequently reported in cytotoxic T-lymphocyte-associated protein-4 (CTLA-4) than PD-1 checkpoint blockade [42, 43]. Moreover, the patient’s bowel movement was normal during the week after injection of tislelizumab, and the patient presented with constipation instead of diarrhea in the early stage of onset.
Concerning the treatments for PI, conservative treatments, including oxygen therapy, antibiotics and parenteral nutrition, are recommended for individuals with apparent manifestations [8]. Compared to plain radiography, CT is more sensitive in the accurate diagnosis of PI with benefits in identifying linear gas bubbles as potential life-threatening situations [44]. PI complicated with bowel obstruction or ischemia tends to require emergency surgical intervention, which could be associated with a higher clinical severity score (including degrees of pain, diarrhea, fever, tenderness, blood per rectum, and hypotension) and metabolic acidosis (particularly increased lactic acid and significantly elevated serum amylase) [45]. Recently, a retrospective study indicated that surgical intervention was more frequently performed in the geriatric group (age ≥ 60 years) with WBC > 12 × 109/L and/or emesis, while sepsis might be a risk factor for death [46]. Moreover, IAP was monitored in our case to consider its role as an alternative predictor of surgical intervention (Fig. 4). According to expert consensus [47], intra-abdominal hypertension (IAH) was defined as a sustained elevation of IAP > 12 mmHg (> 10 mmHg for children), and a decompressive laparotomy is recommended only in cases of overt abdominal compartment syndrome (ACS) recognized as IAP > 20 mmHg. Although sequential organ failure was seldom reported in patients with PI, the elevated IAP indicated a potential burden of ischemia due to excess gas trapped in the intestinal wall when surgical intervention should be considered. Compared to laparotomy, diagnostic laparoscopy was recommended as a priority for patients presenting with a threatened bowel and/or compromised bowel without significant bowel distension [48].
To our knowledge, this is the first review focused on etoposide-related PCI. Furthermore, the possibility of IAP as a predictor for surgical intervention was proposed innovatively. We shared this case with the hope of raising a clinical awareness of PCI associated with etoposide, while whether PCI could be identified as an adverse event caused by etoposide requires more evidence.
Acknowledgements
We sincerely appreciate Dr. Wubin, Department of Radiology and Dr. Yangkun, Department of Gastrointestinal Surgery, for their assistance in the case presentation.
Abbreviations
- PCI
Pneumatosis cystoides intestinalis
- PI
Pneumatosis intestinalis
- CT
Computed tomography
- IBD
Inflammatory bowel diseases
- HIV
Human immunodeficiency virus
- COPD
Chronic obstructive pulmonary disease
- allo-HSCT
Allogeneic hematopoietic stem cell transplantation
- α-GI
Alpha-glucosidase inhibitors
- CAEBV
Chronic active Epstein-Barr virus
- EBV-LPD
EBV-lymphoproliferative disease
- HPS
Hemophagocytic syndrome
- biw
Biweekly
- qd
Quaque die
- PD-1
Programmed cell death-1
- CRS
Cytokine release syndrome
- T
Temperature
- P
Pulse
- R
Respiration
- bpm
Beats per minute
- BP
Blood pressure
- SpO2
Pulse oximetry saturation
- pH
Potential of hydrogen
- PaO2
Partial pressure of Oxygen
- PaCO2
Partial pressure of carbon dioxide
- HCO3
Bicarbonate
- CD
Cluster of differentiation
- HGB
Hemoglobin
- WBC
White blood cell
- PLT
Platelet
- IL-2R
Interleukin-2 receptor
- AST
Glutamic oxaloacetic transaminase
- ALT
Glutamic pyruvic transaminase
- ALP
Alkaline phosphatase
- LDH
Lactic dehydrogenase
- ARDS
Acute respiratory failure syndrome
- IAP
Intra-abdominal pressure
- IAH
Intra-abdominal hypertension
- GVHD
Digestive graft versus host diseases
- NE
Neutropenic enterocolitis
- CTLA-4
Cytotoxic T-lymphocyte-associated protein-4
- ACS
Abdominal compartment syndrome
Authors' contributions
LQY acquired clinical information of the patient and wrote the manuscript. XZ, HY, and QW performed a literature review. YPG provided further discussion of the case. BW revised the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by 1·3·5 project for disciplines of excellence of West China Hospital, Sichuan University, P. R. China (project number ZYJC180006).
Availability of data and materials
The clinical information of the patient and materials generated during the current study are included within the article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication was obtained from the parents of the patient.
Competing interests
The authors declare that there are no conflicts of interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Liqing Yang, Email: LQ_Yang2020@aliyun.com.
Xi Zhong, Email: zhongxivip2006@163.com.
Hao Yang, Email: 154441945@qq.com.
Qin Wu, Email: qinwu0221@gmail.com.
Yuping Gong, Email: gongyuping2010@aliyun.com.
Bo Wang, Email: wchicu@126.com.
References
- 1.Ezuka A, Kawana K, Nagase H, Takahashi H, Nakajima A. Improvement of pneumatosis cystoides intestinalis after steroid tapering in a patient with bronchial asthma: a case report. J Med Case Rep. 2013;7:163. doi: 10.1186/1752-1947-7-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jamart J. Pneumatosis cystoides intestinalis. A statistical study of 919 cases. Acta Hepatogastroenterol. 1979;26(5):419–422. [PubMed] [Google Scholar]
- 3.Tsujimoto T, Shioyama E, Moriya K, Kawaratani H, Shirai Y, Toyohara M, Mitoro A, Yamao J, Fujii H, Fukui H. Pneumatosis cystoides intestinalis following alpha-glucosidase inhibitor treatment: a case report and review of the literature. World J Gastroenterol. 2008;14(39):6087–6092. doi: 10.3748/wjg.14.6087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang YJ, Wang YM, Zheng YM, Jiang HQ, Zhang J. Pneumatosis cystoides intestinalis: six case reports and a review of the literature. BMC Gastroenterol. 2018;18(1):100. doi: 10.1186/s12876-018-0794-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ling F, Guo D, Zhu L. Pneumatosis cystoides intestinalis: a case report and literature review. BMC Gastroenterol. 2019;19(1):176. doi: 10.1186/s12876-019-1087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yamaguchi K, Shirai T, Shimakura K, Akamatsu T, Nakama H, Kono K, Sakato M, Shigeno T, Furuta S, Nakajima T, et al. Pneumatosis cystoides intestinalis and trichloroethylene exposure. Am J Gastroenterol. 1985;80(10):753–757. [PubMed] [Google Scholar]
- 7.Koss LG. Abdominal gas cysts (pneumatosis cystoides intestinorum hominis); an analysis with a report of a case and a critical review of the literature. AMA Arch Pathol. 1952;53(6):523–549. [PubMed] [Google Scholar]
- 8.Arikanoglu Z, Aygen E, Camci C, Akbulut S, Basbug M, Dogru O, Cetinkaya Z, Kirkil C. Pneumatosis cystoides intestinalis: a single center experience. World J Gastroenterol. 2012;18(5):453–457. doi: 10.3748/wjg.v18.i5.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bilici A, Karadag B, Doventas A, Seker M. Gastric pneumatosis intestinalis associated with malignancy: an unusual case report. World J Gastroenterol. 2009;15(6):758–760. doi: 10.3748/wjg.15.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forde KA, Whitlock RT, Seaman WB. Pneumatosis and cystoides intestinalis. Report of a case with colonoscopic findings of inflammatory bowel disease. Am J Gastroenterol. 1977;68(2):188–190. [PubMed] [Google Scholar]
- 11.Kaneko M, Sasaki S, Teruya S, Ozaki K, Ishimaru K, Terai E, Nakayama H, Watanabe T. Pneumatosis cystoides intestinalis in patients with systemic sclerosis: a case report and review of 39 Japanese cases. Case Rep Gastrointest Med. 2016;2016:2474515. doi: 10.1155/2016/2474515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wada Y, Murayama N, Hirose S, In H, Kuroda T, Ito S, Nakano M, Gejyo F. A case of pneumatosis cystoides intestinalis in a patient with polymyositis and interstitial pneumonia. Mod Rheumatol. 2004;14(3):260–263. doi: 10.1007/s10165-004-0304-7. [DOI] [PubMed] [Google Scholar]
- 13.Nakatani K, Kato T, Okada S, Matsumoto R, Nishida K, Komuro H, Suganuma T. Successful treatment with hyperbaric oxygen therapy for pneumatosis cystoides intestinalis as a complication of granulomatosis with polyangiitis: a case report. J Med Case Rep. 2017;11(1):263. doi: 10.1186/s13256-017-1421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ha D, Tsai CJ. Pneumatosis intestinalis in a patient with recurrent Clostridium difficile infection. BMJ Case Rep. 2012;2012:66. doi: 10.1136/bcr-2012-006720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collins CD, Blanshard C, Cramp M, Gazzard B, Gleeson JA. Case report: pneumatosis intestinalis occurring in association with cryptosporidiosis and HIV infection. Clin Radiol. 1992;46(6):410–411. doi: 10.1016/s0009-9260(05)80690-7. [DOI] [PubMed] [Google Scholar]
- 16.Lefor AT, Konishi F, Horie H, Togashi K, Yasuda Y. Pneumatosis intestinalis associated with human immunodeficiency virus infection. Am Surg. 2010;76(5):541–543. [PubMed] [Google Scholar]
- 17.Iida A, Naito H, Tsukahara K, Yumoto T, Nosaka N, Kawana S, Sato K, Takeuchi N, Soneda J, Nakao A. Pneumatosis cystoides intestinalis presenting as pneumoperitoneum in a patient with chronic obstructive pulmonary disease: a case report. J Med Case Rep. 2017;11(1):55. doi: 10.1186/s13256-017-1198-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee YS, Han JJ, Kim SY, Maeng CH. Pneumatosis cystoides intestinalis associated with sunitinib and a literature review. BMC Cancer. 2017;17(1):732. doi: 10.1186/s12885-017-3744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shikuma H, Inoue S, Hatayama T, Mukai S, Muto M, Miyamoto S, Sadahide K, Fujii S, Sekino Y, Goto K, et al. Pneumatosis cystoides intestinalis linked to sunitinib treatment for renal cell carcinoma. IJU Case Rep. 2019;2(6):318–320. doi: 10.1002/iju5.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korhonen K, Lovvorn HN, 3rd, Koyama T, Koehler E, Calder C, Manes B, Evans M, Bruce K, Ho RH, Domm J, et al. Incidence, risk factors, and outcome of pneumatosis intestinalis in pediatric stem cell transplant recipients. Pediatr Blood Cancer. 2012;58(4):616–620. doi: 10.1002/pbc.23242. [DOI] [PubMed] [Google Scholar]
- 21.Wu LL, Yang YS, Dou Y, Liu QS. A systematic analysis of pneumatosis cystoids intestinalis. World J Gastroenterol. 2013;19(30):4973–4978. doi: 10.3748/wjg.v19.i30.4973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keklik F, Cayci Z, Arndt P, Ustun C. Spontaneous complete resolution of pneumomediastinum and pneumatosis intestinalis caused by acute GVHD. Am J Hematol. 2016;91(7):749–750. doi: 10.1002/ajh.24337. [DOI] [PubMed] [Google Scholar]
- 23.Suzuki HI, Izutsu K, Watanabe T, Oshima K, Kanda Y, Motokura T, Chiba S, Kurokawa M. Late-onset pneumatosis cystoides intestinalis associated with non-infectious pulmonary complications after allogeneic hematopoietic stem cell transplantation. Int J Hematol. 2008;88(1):116–118. doi: 10.1007/s12185-008-0110-7. [DOI] [PubMed] [Google Scholar]
- 24.Bhamidipati PK, Ghobadi A, Bauer S, DiPersio JF, Pusic I. Conservative management of pneumatosis intestinalis after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014;49(11):1436–1438. doi: 10.1038/bmt.2014.148. [DOI] [PubMed] [Google Scholar]
- 25.Venkataramani V, Seif Amir Hosseini A, Schulze MH, Trumper L, Wulf G, Bacher U, Jung W. Intestinal pneumatosis associated with tuberculosis after allogeneic hematopoietic stem cell transplantation. Acta Haematol. 2017;137(1):51–54. doi: 10.1159/000452436. [DOI] [PubMed] [Google Scholar]
- 26.Vlieghe V, Chantrain CF, Benmiloud S, Brichard B, Dupont S, de Ville de Goyet J, Reding R, Hermans D, Bachy A, Vermylen C. Conservative management of pneumatosis intestinalis following haematopietic stem cell transplantation for major beta thalassemia. Eur J Pediatr. 2007;166(6):615–6. [DOI] [PubMed]
- 27.Groninger E, Hulscher JB, Timmer B, Tamminga RY, Broens PM. Free air intraperitoneally during chemotherapy for acute lymphoblastic leukemia: consider pneumatosis cystoides intestinalis. J Pediatr Hematol Oncol. 2010;32(2):141–143. doi: 10.1097/MPH.0b013e3181ced397. [DOI] [PubMed] [Google Scholar]
- 28.Fujimi A, Sakamoto H, Kanisawa Y, Minami S, Nagamachi Y, Yamauchi N, Ibata S, Kato J. Pneumatosis intestinalis during chemotherapy with nilotinib in a patient with chronic myeloid leukemia who tested positive for anti-topoisomerase I antibodies. Clin J Gastroenterol. 2016;9(6):358–364. doi: 10.1007/s12328-016-0683-2. [DOI] [PubMed] [Google Scholar]
- 29.Galm O, Fabry U, Adam G, Osieka R. Pneumatosis intestinalis following cytotoxic or immunosuppressive treatment. Digestion. 2001;64(2):128–132. doi: 10.1159/000048852. [DOI] [PubMed] [Google Scholar]
- 30.Shin DK, Oh J, Yoon H, Kim JE, Chong SY, Oh D. Asymptomatic pneumatosis intestinalis following chemotherapy for B lymphoblastic leukemia with recurrent genetic abnormalities in an adolescent patient. Korean J Hematol. 2012;47(1):74–76. doi: 10.5045/kjh.2012.47.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mangaonkar A, Mansour J, Keen R, Kukkadapu T, Chintalapally R, Kota V. Pneumatosis intestinalis in a patient with acute promyelocytic leukemia. Case Rep Hematol. 2015;2015:576042. doi: 10.1155/2015/576042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hashimoto S, Saitoh H, Wada K, Kobayashi T, Furushima H, Kawai H, Shinbo T, Funakoshi K, Takahashi H, Shibata A. Pneumatosis cystoides intestinalis after chemotherapy for hematological malignancies: report of 4 cases. Intern Med. 1995;34(3):212–215. doi: 10.2169/internalmedicine.34.212. [DOI] [PubMed] [Google Scholar]
- 33.Tsai NY, Chou CH, Cheng YC. Pneumatosis cystoides intestinalis in a patient with aseptic meningitis: a case report. Int J Colorectal Dis. 2019;34(10):1805–1808. doi: 10.1007/s00384-019-03383-2. [DOI] [PubMed] [Google Scholar]
- 34.Shih IL, Lu YS, Wang HP, Liu KL. Pneumatosis coli after etoposide chemotherapy for breast cancer. J Clin Oncol. 2007;25(12):1623–1625. doi: 10.1200/JCO.2006.10.5742. [DOI] [PubMed] [Google Scholar]
- 35.Faria LD, Anjos CH, Fernandes GD, Carvalho IF. Pneumatosis intestinalis after etoposide-based chemotherapy in a patient with metastatic small cell lung cancer: successful conservative management of a rare condition. Einstein. 2016;14(3):420–422. doi: 10.1590/S1679-45082016RC3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Azzaroli F, Turco L, Ceroni L, Galloni SS, Buonfiglioli F, Calvanese C, Mazzella G. Pneumatosis cystoides intestinalis. World J Gastroenterol. 2011;17(44):4932–4936. doi: 10.3748/wjg.v17.i44.4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baldwin EL, Osheroff N. Etoposide, topoisomerase II and cancer. Curr Med Chem Anticancer Agents. 2005;5(4):363–372. doi: 10.2174/1568011054222364. [DOI] [PubMed] [Google Scholar]
- 38.Hande KR. Etoposide: four decades of development of a topoisomerase II inhibitor. Eur J Cancer. 1998;34(10):1514–1521. doi: 10.1016/s0959-8049(98)00228-7. [DOI] [PubMed] [Google Scholar]
- 39.Reyhanoglu G, Tadi P. Etoposide. In: StatPearls. Treasure Island, FL; 2022.
- 40.Rodrigues FG, Dasilva G, Wexner SD. Neutropenic enterocolitis. World J Gastroenterol. 2017;23(1):42–47. doi: 10.3748/wjg.v23.i1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ghouri YA, Tahan V, Shen B. Secondary causes of inflammatory bowel diseases. World J Gastroenterol. 2020;26(28):3998–4017. doi: 10.3748/wjg.v26.i28.3998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rajha E, Chaftari P, Kamal M, Maamari J, Chaftari C, Yeung SJ. Gastrointestinal adverse events associated with immune checkpoint inhibitor therapy. Gastroenterol Rep (Oxf) 2020;8(1):25–30. doi: 10.1093/gastro/goz065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramos-Casals M, Brahmer JR, Callahan MK, Flores-Chavez A, Keegan N, Khamashta MA, Lambotte O, Mariette X, Prat A, Suarez-Almazor ME. Immune-related adverse events of checkpoint inhibitors. Nat Rev Dis Primers. 2020;6(1):38. doi: 10.1038/s41572-020-0160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Di Pietropaolo M, Trinci M, Giangregorio C, Galluzzo M, Miele V. Pneumatosis cystoides intestinalis: case report and review of literature. Clin J Gastroenterol. 2020;13(1):31–36. doi: 10.1007/s12328-019-00999-3. [DOI] [PubMed] [Google Scholar]
- 45.Knechtle SJ, Davidoff AM, Rice RP. Pneumatosis intestinalis. Surgical management and clinical outcome. Ann Surg. 1990;212(2):160–165. doi: 10.1097/00000658-199008000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Greenstein AJ, Nguyen SQ, Berlin A, Corona J, Lee J, Wong E, Factor SH, Divino CM. Pneumatosis intestinalis in adults: management, surgical indications, and risk factors for mortality. J Gastrointest Surg. 2007;11(10):1268–1274. doi: 10.1007/s11605-007-0241-9. [DOI] [PubMed] [Google Scholar]
- 47.Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M, Leppaniemi A, Ejike JC, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39(7):1190–1206. doi: 10.1007/s00134-013-2906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sanford Z, Brown S, Tran MN, Zahiri HR, Feather C, Wormuth J, Buckley B. Updates on the utility of diagnostic laparoscopy in the management of pneumatosis intestinalis: an improvement to the current treatment algorithm. Surg Innov. 2018;25(6):648–650. doi: 10.1177/1553350618803742. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The clinical information of the patient and materials generated during the current study are included within the article.