Abstract
Objectives
Little is known about how the coronavirus disease 2019 (COVID-19) pandemic affected influenza vaccine utilization and disparities. We sought to estimate changes in the likelihood of receiving an influenza vaccine across different demographic subgroups during the COVID-19 pandemic.
Methods
In this cohort study, we analyzed influenza vaccine uptake from 2019 to 2020 using Optum commercial insurance claims data. Eligible individuals were aged 18 or above in 2018 and continuously enrolled from 08/01/2018 through 12/31/2020. Multivariable logistic regressions were fitted for the individual-level influenza vaccine uptake. Adjusting for demographic factors and medical histories, we estimated probabilities of receiving influenza vaccines before and after the COVID-19 pandemic across demographic subgroups.
Results
From August to December 2019, unadjusted influenza vaccination rate was 42.3%, while in the same period of 2020, the vaccination rate increased to 45.9%. Females had a higher vaccination rate in 2019 (OR: 1.16, 95% CI 1.15–1.16), but the increase was larger for males. Blacks and Hispanics had lower vaccination rates relative to whites in both flu seasons. Hispanics showed a greater increase in vaccination rate, increasing by 7.8 percentage points (p < .001) compared to 4.4 (p < .001) for whites. The vaccination rate for Blacks increased by 5.2 percentage points (p < .001). All income groups experienced vaccination improvements, but poorer individuals had lower vaccination rates in both seasons. The most profound disparities occurred when educational cohort were considered. The vaccination rate increased among college-educated enrollees by 8.8 percentage points (p < .001) during the pandemic compared to an increase of 2.8 percentage points (p < .001) for enrollees with less than a 12th grade education. Past influenza infections or vaccination increased the likelihood of vaccination (p < .001).
Conclusions
The COVID-19 pandemic was associated with increased influenza vaccine utilization. Disparities persisted but narrowed with respect to gender and race but worsened with respect to income and educational attainment.
Keywords: Vaccination, Health Disparity, COVID-19, Influenza
1. Introduction
Influenza vaccination is one of the most widely recommended preventative measures against influenza-related illness and death [1]. Although the effectiveness of influenza vaccines has been well established, vaccination rate remains low in US. Only an estimated 48.4% of US adults received an influenza vaccine in the 2019–2020 flu season [2]. Furthermore, disparities in influenza immunization persist. Vaccination rates for Black and Hispanic adults (41.2% and 38.3%) were lower than the national average [2]. Gender, poverty, and educational level also contributed to low influenza vaccine uptake [3], [4]. Given that racial and ethnic minorities also had higher rates of influenza-related hospitalization and death than non-Hispanic White individuals, socio-demographic disparities in vaccination rates may enlarge existing disparities in adverse health outcomes from influenza-related illness [5].
Low influenza vaccination rates and their disparities in rates were of great concerns during the coronavirus disease 2019 (COVID-19) pandemic, given the prospect of a potential twindemic of influenza and COVID-19 [6]. To avoid this, there were significant efforts to promote influenza vaccine uptake in 2020 [7], [8]. The Centers for Disease Control and Prevention (CDC) took steps to increase the availability of vaccines and conducted extensive educational outreach activities [9]. In addition to external efforts, it was anticipated living in a pandemic itself would also raise people’s awareness of influenza and other respiratory diseases, and lead to higher influenza vaccine uptake [10]. On the other hand, healthcare utilization in general declined dramatically during the pandemic in US [11], [12], [13]. Most non-influenza immunizations decreased by 60 percent in mid-April in 2020 but rebounded by October, compared with 2019 [14]. It is possible that influenza vaccinations may have experienced a similar pattern, owing to the implementation of COVID-19 mitigation measures, reduced influenza prevalence, and concerns about potential COVID-19 exposure in the healthcare settings [15], [16], [17]. These factors also raised concerns that existing disparities in influenza vaccinations would be exacerbated [6]. Additionally, the COVID-19 pandemic has disproportionally affected non-Hispanic Black and Hispanic individuals, revealing that racial/ethnic minorities historically suffered from lack of healthcare resources and bore higher risks of infection due to socioeconomic status [18], [19], [20], [21], [22]. Understanding how the pandemic affected utilization of preventive measures across different socioeconomic groups is an important step to predict long-term effects of the COVID-19 pandemic on health outcomes, especially for vulnerable populations.
Identifying how the COVID-19 pandemic affected influenza vaccination will help with understanding individuals’ behavior during the pandemic, evaluating the effectiveness of vaccine-related campaigns, and addressing gaps between different socio-demographic groups. Existing pilot studies have to date provided mixed findings. Whereas some analyses found that influenza vaccination intention and uptake among adults in the 2020–21 flu season was higher than the previous season [15], [23], [24], a recent study found that the COVID-19 pandemic exacerbated polarization in attitudes towards vaccination rather than motivating parents to vaccinate their children against influenza [25]. These studies were generally based on small samples of self-reported survey data and have not been validated with national claims data.
In this study, we used a national database of private medical claims to quantify rates of influenza vaccination before and during the COVID-19 pandemic. We examined changes in individual influenza vaccine uptake during the 2019–20 and 2020–21 flu seasons across different socio-demographic groups to investigate how different socioeconomic groups responded to the pandemic in terms of their measurable behavior against the risk of influenza, and to assess whether the pandemic lessened or worsened disparities in vaccine uptake.
2. Methods
2.1. Data source and patient selection
This retrospective cohort study utilized de-identified commercial and Medicare Advantage administrative claims data from the Optum Clinformatics® Data Mart, a national database comprised of administrative health claims for members of a large national managed care company in all 50 US states and District of Columbia. The database contains complete health care events for enrollees covered with both medical and prescription drug coverage. All administrative claims were verified, adjudicate, adjusted, and de-identified by Optum.
The study included all patients in the database that were continuously enrolled from August 1, 2018 through December 31, 2020 and aged 18 years or above in 2018. Because influenza vaccine distribution generally begins in August, we constructed flu seasons to span from August 1 of the current year to July 31 of the next year [26], [27]. As data from January 1, 2021 to July 31, 2021 are not yet available and more than 95% of influenza vaccinations were administered before December 31, 2020 [24], those who received influenza vaccines from January to July in 2020 were excluded in the analysis. Hence the identification period was August 1–December 31 for each flu season. An additional year of continuous enrollment was required for each flu season to obtain medical history information. The continuous enrollment requirement also reduced the potential confounding effect of COVID-related unemployment and related change in insurance status.
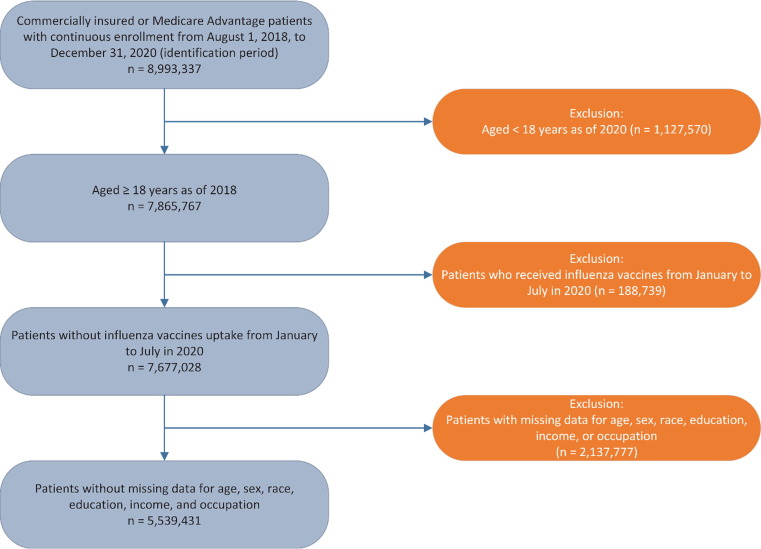
The proclamation of a national public health emergency due to COVID-19 was introduced in March 2020 [28]. Therefore, the pre-pandemic period consisted of the 5 months from August 1 through December 31, 2019 (2019–20 flu season) and the “pandemic” period consisted of the 5 months from August 1 through December 31, 2020 (2020–21 flu season). Finally, we excluded individuals with missing data for any of the demographic variables to further ensure the homogeneity of our study population across years (Fig. 1 ).
Fig. 1.
Patient Selection and Attrition.
2.2. Measures
2.2.1. Outcome Variable: Influenza vaccine uptake
We identified influenza vaccine uptake at the individual level for each flu season based on the CPT administration code (Appendix A) in the medical claims or the National Drug Code (NDC) in the pharmacy claims [29], [30]. The service date of the vaccination was defined as the date of the first influenza-vaccine-related claim in the flu season. Individuals who did not receive an influenza vaccine in a flu season were coded as non-uptake. Therefore, each individual had up to one uptake event for each flu season. The place of service (physician medical office, pharmacy, or other) for the uptake was also recorded.
2.2.2. Covariates
We obtained demographic characteristics, including age in 2018, gender, race/ethnicity, educational level, and household income level. The socioeconomic status (SES) data were based on the application of proprietary analytic and demographic models by Optum Insight to Census data linked to additional sources. Only the most recent education and household income were reported in the dataset and used in our analysis.
Influenza history and influenza vaccination history have been found to be important predictors of influenza vaccine uptake [27], [31], [32]. We obtained influenza and influenza vaccination in the previous flu season using corresponding ICD-10-CM codes, CPT administration codes, and NDCs (Appendix A).
2.3. Statistical analysis
All analyses were conducted using SAS software version 9.4 (SAS Institute, Cary, NC). GNU Image Manipulation Program (GIMP) and Microsoft Excel were also used for figure generation. All study variables were analyzed descriptively. Unadjusted vaccination rates by demographic characteristics and flu season were calculated. Cumulative counts of influenza vaccine uptake for every 7 days after August 1 in both flu seasons were computed. We conducted trend analysis based on the percent change in cumulative influenza vaccine uptake (Appendix B).
We ran a logistic regression model to examine the association of individual influenza vaccine uptake with age, sex, race/ethnicity, education, household income, being diagnosed with influenza in the previous year, receiving the influenza vaccine in the previous year, and being in the COVID pandemic. As a sensitivity check, a similar model without the COVID indicator was also employed for 2019 and 2020 separately. Finally, we added interaction terms between the COVID indicator and all other variables of interest to the logistic regression model to evaluate the impact of COVID on influenza vaccine uptake for different demographic groups. Predicted probabilities of getting flu vaccine were calculated for each subgroup (Appendix C). We predicted probabilities of vaccination based on demographic distributions of both our analytical sample and the US population obtained from the 2019 American Community Survey (ACS). Given the strong similarity between the two sets of predictions, we opted to represent our main results based on distributions of our analytical sample. In all analyses, P values ≤0.05 were considered to indicate statistical significance and hypothesis tests were two-sided.
3. Results
Compared to individuals not included in the analyses due to missing demographic information, individuals with complete demographic information in our analyses were more likely to be non-Hispanic White individuals, more likely to be aged 65 years or above in 2018, less likely to have higher annual household income, and more likely to have an educational attainment between a high school diploma and bachelor’s degree (Appendix D). Descriptive statistics for the 5,539,431 unique commercially insured individuals were provided in Table 1 . In our analytical sample, 2,972,875 (53.7%) were women, 4,060,893 (73.3%) were non-Hispanic White individuals, 1,248,051 (22.5%) had annual household income less than $40,000, and 1,113,895 (20.1%) had a bachelor or higher degree. Ages in 2018 ranged from 18 to 88 years, with a mean (SD) age of 59.3 (18.7) years. Compared to the general US adult population, commercially insured individuals included in our analyses were more likely to be non-Hispanic White individuals, aged 65 years or above in 2018, have annual household incomes above $100,000, have an educational attainment between a high school diploma and bachelor’s degree (Table 1).
Table 1.
Demographic Characteristics.
| Characteristic | Patients, No.a, b | Patients, %a, b | US population, %b, c |
|---|---|---|---|
| Total | 5,539,431 | – | – |
| Sex | |||
| Male | 2,566,556 | 46.3 | 48.4 |
| Female | 2,972,875 | 53.7 | 51.6 |
| Race | |||
| Asian | 260,477 | 4.7 | 5.9 |
| Black | 551,765 | 10.0 | 12.8 |
| Hispanic | 666,296 | 12.0 | 19.1 |
| White | 4,060,893 | 73.3 | 62.2 |
| Age in 2018 | |||
| Mean (SD), y | 59.3 (18.7) | – | – |
| 18–24 | 310,614 | 5.6 | 11.6 |
| 25–34 | 421,000 | 7.6 | 18.0 |
| 35–44 | 593,737 | 10.7 | 16.4 |
| 45–54 | 712,639 | 12.9 | 16.2 |
| 55–64 | 766,501 | 13.8 | 16.7 |
| ≥65 | 2,734,940 | 49.4 | 21.1 |
| Income | |||
| <$40 K | 1,248,051 | 22.5 | 29.0 |
| $40–$49 K | 421,119 | 7.6 | 8.1 |
| $50–$59 K | 460,672 | 8.3 | 7.2 |
| $60–$74 K | 634,094 | 11.5 | 9.3 |
| $75–$99 K | 905,404 | 16.3 | 12.3 |
| $100 K+ | 1,870,091 | 33.8 | 34.1 |
| Education | |||
| Less than 12th grade | 27,997 | 0.5 | 10.6 |
| High school diploma | 1,322,847 | 23.9 | 28.3 |
| Less than Bachelor Degree | 3,074,692 | 55.5 | 27.8 |
| Bachelor Degree Plus | 1,113,895 | 20.1 | 33.3 |
Estimates based on the analytical sample of commercially insured adults.
Percentages may not add up to 100% due to rounding.
US population, based on 2019 US Census estimates from the American Community Survey. For age and race variables, we dropped the missing categories and normalized the remaining data to ensure they summed up to 100%.
In 2019–2020, 54.6% doses were administered at physician offices and 38.7% were administered at pharmacies, whereas in 2020–2021, 48.0% were administered at physician offices and 46.3% were administered at pharmacies. Other settings of influenza vaccination included hospital outpatient departments and mass immunization centers.
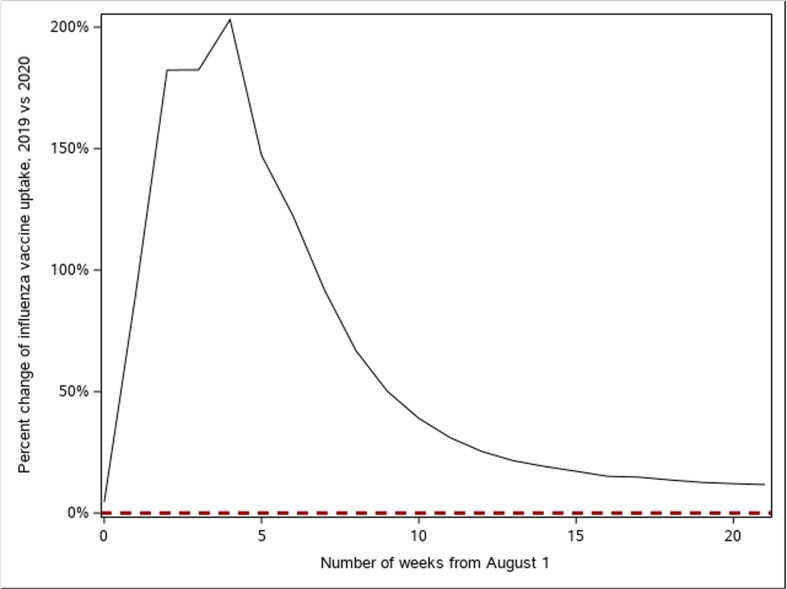
Unadjusted influenza vaccination rate increased from 42.3% in the 2019–20 flu season to 45.9% in the 2020–21 flu season (Table 2 ). Fig. 2 shows the percent change in cumulative influenza vaccine uptake from August 1, 2020, compared to 2019. More adults got influenza vaccines earlier, with the uptake tripled in the first 4 weeks of the 2020–21 flu season compared to the same period in the 2019–20 flu season. During the COVID-19 pandemic, influenza vaccine uptakes at pharmacies substantially increased, while the uptakes at other settings slightly decreased (Appendix B). Controlling for demographic characteristics and medical histories, the COVID-19 pandemic was associated with an increased likelihood of receiving influenza vaccine (OR: 1.23, 95% CI 1.23–1.24) (Table 3 ). The adjusted probability of influenza vaccination increased from 39.6 percent (95% CI 39.5%–39.6%) in 2019–20 to 44.7 percent (95% CI 44.6%–44.7%) (Appendix Table C2).
Table 2.
Influenza Vaccine Uptake by Flu Season, Demographic Characteristics, and Medical Histories.
| Characteristic | 2019–20, No. (%) | 2020–21, No. (%) |
|---|---|---|
| Total | 2,344,252 (42.3) | 2,540,263 (45.9) |
| Demographic characteristics | ||
| Sex | ||
| Male | 994,404 (38.7) | 1,091,964 (42.6) |
| Female | 1,349,848 (45.4) | 1,448,299 (48.7) |
| Race | ||
| White | 1,791,926 (44.1) | 1,928,153 (47.5) |
| Asian | 109,792 (42.2) | 126,891 (48.7) |
| Black | 213,868 (38.8) | 229,075 (41.5) |
| Hispanic | 228,666 (34.3) | 256,144 (38.4) |
| Age in 2018 | ||
| 18–24 | 54,293 (17.5) | 62,714 (20.2) |
| 25–34 | 93,799 (22.3) | 106,768 (25.4) |
| 35–44 | 146,880 (24.7) | 175,494 (29.6) |
| 45–54 | 197,600 (27.7) | 243,555 (34.2) |
| 55–64 | 305,563 (39.9) | 354,070 (46.2) |
| ≥65 | 1,546,117 (56.5) | 1,597,662 (58.4) |
| Income | ||
| $100 K+ | 773,107 (41.3) | 880,049 (47.1) |
| $75–$99 K | 399,646 (44.1) | 431,256 (47.6) |
| $60–$74 K | 274,902 (43.4) | 293,833 (46.3) |
| $50–$59 K | 198,171 (43.0) | 209,695 (45.5) |
| $40–$49 K | 172,018 (40.9) | 181,418 (43.1) |
| <$40 K | 526,408 (42.2) | 544,012 (43.6) |
| Education | ||
| Bachelor Degree Plus | 506,179 (45.4) | 578,758 (52.0) |
| Less than Bachelor Degree | 1,299,227 (42.3) | 1,399,255 (45.5) |
| High school diploma | 529,193 (40.0) | 551,997 (41.7) |
| Less than 12th grade | 9,653 (34.5) | 10,253 (36.6) |
| Medical history | ||
| Diagnosed with influenza last flu season | ||
| No | 2,308,168 (42.3) | 2,497,828 (45.9) |
| Yes | 36,084 (46.3) | 42,435 (43.6) |
| Received influenza vaccine last flu season | ||
| No | 474,898 (14.6) | 621,419 (19.5) |
| Yes | 1,869,354 (81.5) | 1,918,844 (81.9) |
Fig. 2.
Percent Change of Weekly Influenza Vaccine Uptake, 2019 vs 2020. Percent change of weekly influenza vaccine uptake after August 1, 2020, compared with same weeks in 2019. Methodology details are presented in Appendix B.
Table 3.
Factors Associated with Influenza Vaccination.
| Odds Ratio (95% CI)a |
|||
|---|---|---|---|
| Factor | 2019–2021 | 2019–2020 | 2020–21 |
| COVID-19 pandemic | |||
| No | 1 [Reference] | ||
| Yes | 1.23 (1.23–1.24) | ||
| Demographic characteristics | |||
| Sex | |||
| Male | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Female | 1.14 (1.14–1.15) | 1.16 (1.15–1.16) | 1.13 (1.12–1.13) |
| Race | |||
| White | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Asian | 1.07 (1.06–1.07) | 0.96 (0.95–0.97) | 1.17 (1.16–1.18) |
| Black | 0.92 (0.92–0.93) | 0.90 (0.90–0.91) | 0.94 (0.93–0.95) |
| Hispanic | 0.86 (0.86–0.87) | 0.80 (0.79–0.80) | 0.93 (0.92–0.93) |
| Age in 2018 | |||
| 18–24 | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 25–34 | 1.35 (1.33–1.36) | 1.42 (1.40–1.44) | 1.29 (1.28–1.31) |
| 35–44 | 1.50 (1.49–1.52) | 1.46 (1.44–1.48) | 1.55 (1.53–1.57) |
| 45–54 | 1.76 (1.75–1.78) | 1.63 (1.61–1.65) | 1.89 (1.87–1.91) |
| 55–64 | 2.50 (2.48–2.52) | 2.35 (2.32–2.38) | 2.65 (2.62–2.69) |
| ≥65 | 3.22 (3.19–3.24) | 3.19 (3.16–3.23) | 3.24 (3.20–3.27) |
| Income | |||
| $100 K+ | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| $75–$99 K | 0.92 (0.91–0.92) | 0.94 (0.93–0.95) | 0.90 (0.89–0.90) |
| $60–$74 K | 0.88 (0.87–0.88) | 0.90 (0.89–0.91) | 0.86 (0.85–0.86) |
| $50–$59 K | 0.84 (0.84–0.85) | 0.87 (0.86–0.88) | 0.82 (0.81–0.83) |
| $40–$49 K | 0.81 (0.80–0.81) | 0.84 (0.83–0.85) | 0.78 (0.77–0.79) |
| <$40 K | 0.78 (0.78–0.78) | 0.82 (0.82–0.83) | 0.74 (0.74–0.75) |
| Education | |||
| Bachelor Degree Plus | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Less than Bachelor Degree | 0.80 (0.80–0.80) | 0.87 (0.86–0.87) | 0.75 (0.74–0.75) |
| High school diploma | 0.75 (0.75–0.76) | 0.85 (0.85–0.86) | 0.67 (0.67–0.68) |
| Less than 12th grade | 0.71 (0.69–0.73) | 0.80 (0.78–0.83) | 0.64 (0.62–0.66) |
| Medical history | |||
| Diagnosed with influenza last flu season | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.52 (1.50–1.54) | 1.66 (1.63–1.70) | 1.40 (1.38–1.43) |
| Received influenza vaccine last flu season | |||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 18.56 (18.50–18.62) | 21.65 (21.55–21.75) | 16.08 (16.01–16.15) |
Abbreviation: CI = confidence interval.
Multivariable analysis adjusted for demographic characteristics and medical histories. Specifications are presented in Appendix C.
Table 2 demonstrated the unadjusted influenza vaccination rate by different demographic characteristics and medical history during August 1-December 31 in each flu season. For most of the subgroups, influenza vaccination rates in 2020–21 were above the 2019–20 levels, except that individuals who were diagnosed with influenza in the previous season experienced a decreased vaccination rate (from 46.3% to 43.6%). Most subgroups experienced similar trends (Appendix B).
Females had higher odds of receiving an influenza vaccine than males in both flu seasons (2019–20: OR = 1.16, 95% CI 1.15–1.16; 2020–21: OR = 1.13, 95% CI 1.12–1.13) (Table 3), but the increase in influenza vaccine uptake was smaller than males. By December 31, 2020, the predicted probability of receiving an influenza vaccine increased by 4.9 percentage points (p < .001) among females and 5.4 percentage points (p < .001) among males, compared to 2019–20 (Appendix Table C2).
For race and ethnicity, White individuals had the highest probability of influenza vaccination before the pandemic, followed by Asians (OR = 0.96, 95% CI 0.95–0.97), Black individuals (OR = 0.90, 95% CI 0.90–0.91), and Hispanic individuals (OR = 0.80, 95% CI 0.79–0.80). Among Hispanic individuals, the probability of influenza vaccination substantially improved by 7.8 percentage points (p < .001) during the pandemic. Asians also experienced an increase of 9.4 percentage points (p < .001) and had the highest vaccination rate during the pandemic. Within the insured population, Black and White individuals experienced relatively smaller influenza vaccination rate improvements. The probability of influenza vaccination increased by 5.2 percentage points (p < .001) for Black individuals and by 4.4 percentage points (p < .001) for White individuals (Appendix Table C2).
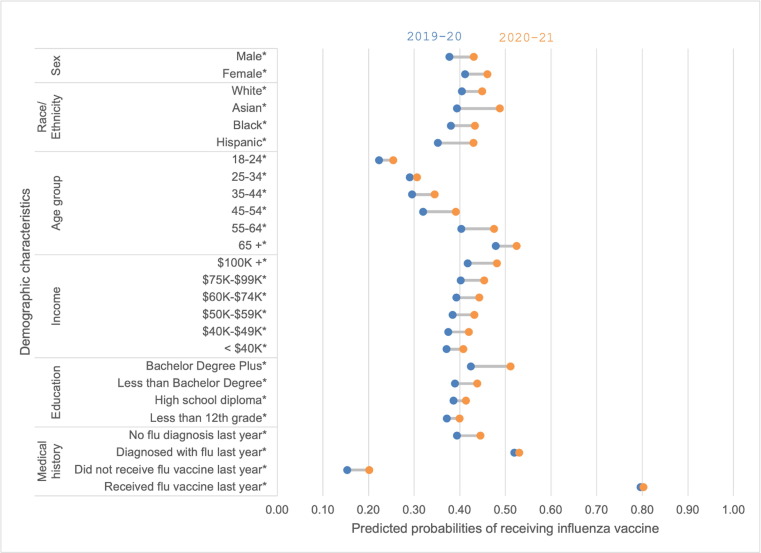
Before the pandemic, influenza vaccination rate increased with age (Fig. 3 ). Influenza vaccination rate among the middle-aged (35–64 years old) increased the most. The predicted probability of influenza vaccination increased by 5.0 percentage points (p < .001) among individuals aged 35–44, by 7.2 percentage points (p < .001) among individuals aged 45–54, and by 9.1 percentage points (p < .001) among individuals aged 55–64. The youngest and oldest cohorts experienced relatively smaller changes: the predicted probability of influenza vaccination for individuals aged 65 and above increased by 4.5 percentage points (p < .001) compared to the 2019–20 flu season; the predicted probability for individuals aged between 18 and 24 increased by 3.1 percentage points (p < .001); and the predicted probability for individuals aged between 25 and 34 increased by 1.6 percentage points (p < .001) (Appendix Table C2).
Fig. 3.
Predicted Probabilities of Receiving Influenza Vaccines by Sample Characteristics and Flu Season. *Significance at 0.05 level. Predicted probabilities of receiving influenza vaccines in the 2019–20 season (blue dots) and the 2020–21 season (orange dots), predicted from the fitted logistic regression models, holding other predictors constant at their analytical sample mean. Specifications, estimates, 95% confidence intervals, and p-values are in Appendix C. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Influenza vaccination rate increased with household income level in both periods (Fig. 3). The poorest group was least likely to get an influenza vaccine compared to the richest group (2019–20: OR = 0.82, 95% CI 0.82–0.83; 2020–21: OR = 0.74, 95% CI 0.74–0.75) (Table 3). All income groups had higher vaccination rates against influenza during the pandemic (Fig. 3). While the richest group had greatest improvement, with the probability of vaccination increasing by 6.4 percentage points (p < .001), and the poorest group had least improvement, with the probability of vaccination increasing by 3.7 percentage points (p < .001) (Appendix Table C2).
In both seasons, influenza vaccination rates increased with level of educational attainment (Fig. 3). During the pandemic, college-educated individuals experienced the largest increase in influenza vaccination rate, increasing by 8.8 percentage points (p < .001). The vaccination rate increased by 2.8 percentage points (p < .001) for enrollees with less than 12th grade education, by 2.7 percentage points (p < .001) for enrollees with a high school diploma, and by 4.8 percentage points (p < .001) for enrollees between high school diploma and bachelor’s degree (Appendix Table C2).
An influenza infection in the previous season increased the odds of receiving an influenza vaccine in the current season (2019–20: OR = 1.66, 95% CI 1.63–1.70; 2020–21: OR = 1.40, 95% CI 1.38–1.43) (Table 3). Receiving an influenza vaccination in the previous season also increased the odds of receiving an influenza vaccine in the current season (2019–20: OR = 21.65, 95% CI 21.55–21.75; 2020–21: OR = 16.08, 95% CI 16.01–16.15) (Table 3). During the pandemic, the increase in predicted probability of vaccination was 5.2 percentage points (p < .001) among individuals without influenza infection in the previous season, compared with 1.1 percentage points (p = .001) among individuals with influenza infection in the previous season. Comparing populations based on prior flu vaccination status yielded similar differences, with an increase in the probability of vaccination at 4.9 percentage points (p < .001) without vaccination in the previous season, and 0.7 percentage points (p < .001) with vaccination in the previous season (Appendix Table C2).
Appendix Table C2 also reported the comparison of predicted probabilities of influenza vaccination in our data and predicted probabilities in the US adult population for main demographic variables found in the ACS. As noted above, given the strong similarity between the two sets of results with respect to the impact of the COVID-19 pandemic, we opted to present results based on the analytical sample in the above.
4. Discussion
This study found that the COVID-19 pandemic was associated with an increased likelihood of receiving an influenza vaccine by December 2020, controlling for individual demographic characteristics and medical histories in the previous flu season. The improvement in influenza vaccination rate was observed in both genders, all race/ethnicity groups, across most age cohorts, all household income levels, and all educational levels, though the magnitudes varied across different subgroups. These findings add to the limited existing evidence of how individual vaccination decisions changed during the pandemic.
The increase in influenza vaccination rate we estimated is qualitatively consistent with several surveys conducted or sponsored by CDC [33], [34]. Our estimated adult vaccination rates of 42.3% in 2019–20 season and 45.9% in 2020–21 season are similar but somewhat lower than estimates from the Behavioral Risk Factor Surveillance System (BRFSS) (48.4% in 2019–20 and 50.2% in 2020–21; see Appendix E). However, the BRFSS usually collects data by asking survey participants if they received influenza vaccines “in past 12 months”, and hence relies on memory recall. Additionally, the survey applies to the whole calendar year, rather than the flu season. Our data track uptakes during the main flu season, i.e., August to December, suggesting that the differences are likely overstated. Moreover, our reasonably lower estimates are claims-based and verified by medical records, thus avoiding recall bias.
Our findings were also validated by the comparison to CDC’s reported estimates of number of influenza vaccines administered in pharmacies and physician medical offices [24]. While CDC claim-based estimates relied on a larger national (all-payer) sample, both sets of estimates suggest that more influenza vaccines were administered during 2020–21 season, but the number of doses administered at physician medical offices was slightly lower than in 2019–20. Note that CDC only reported unadjusted vaccination uptakes and trends from aggregated claims. To our knowledge, our study is the first to analyze adjusted influenza vaccine uptake based on individual demographic characteristics and medical histories, while quantifying the impact of the COVID-19 pandemic on influenza vaccine utilization and disparities among commercially insured adults across the US.
In the commercially insured population, disparities with respect to gender and race persisted but narrowed during the pandemic. Although influenza vaccination rates improved for both genders, males had lower vaccination rates than females in both flu seasons than females, but the improvement among males was larger. For race and ethnicity, the Hispanic and Black individuals had lower vaccination rates than Asians and White individuals before the pandemic. Our pre-pandemic estimates are consistent with existing evidence [2], [32], [35], [36], [37]. Hispanics and Asians experienced substantial vaccination rate improvements while Black and white individuals had relatively smaller improvements. Narrowed racial and ethnic disparities suggested effectiveness of CDC’s communication outreach, particularly to Black and Hispanic populations [9]. For age, we found the largest increase in vaccination rates occurred in the middle-aged cohort (35–64 years old).
When comparing vaccination rates across income groups, disparities persisted and even worsened during the pandemic. Influenza vaccination rate increased with household income in both flu seasons. Although all income groups experienced vaccination rate improvements during the pandemic, those with annual household income of more than $100,000 experienced the greatest increase of influenza vaccination rate.
Similarly, we found profound and significant disparities based on educational cohorts. Before the COVID-19 pandemic, college-educated individuals had a higher influenza vaccination rate than non-college-educated individuals. Our estimates are consistent with established literature which showed that higher educational levels are associated with increased acceptance and utilization of influenza vaccination [38], [39]. The pandemic exacerbated these disparities. While college-educated individuals have become more inclined to be vaccinated against influenza, individuals with low educational attainment remained relatively unchanged. Among non-college-educated working adults, educational attainment has been acknowledged as a main driver of worse health outcomes such as higher rates of chronic disease conditions, substance use-related death and suicide [40]. Therefore, the reduced immunizations in this population during the COVID-19 pandemic elevates concerns about their long-term health outcomes.
We also found that decisions on influenza vaccination were affected by past behavior of individuals. Past influenza infections can raise the awareness of vaccinating against the disease, which is consistent with literature showing that patients can learn from adverse health events [27]. Such learning effects grew larger during the pandemic. In our data, influenza vaccination rates among those who were vaccinated in the previous season was high, although not perfect. Before the pandemic, about 80% of individuals who vaccinated against influenza in 2018–20 season would continue to be vaccinated in 2019–20 season. The pandemic slightly increased the rate. It is further gratifying to note that vaccination rates among individuals without past influenza infection or vaccination also improved, suggesting that vaccine attitude may have changed during the pandemic.
With the circulation of SARS-CoV-2, the increased influenza vaccine utilization among most commercially insured adults suggests that the heightened awareness of the new respiratory infectious disease may have had beneficial spillover effects on taking preventive measures against other respiratory infectious diseases. In addition, given that education programs historically played important roles in promoting vaccination rate [41], extensive influenza vaccine campaigns and special educational efforts for minority groups during the COVID-19 pandemic appear to have been similarly effective.
Although influenza-related infections, hospitalizations, and deaths substantially declined in the 2020–21 flu season [42], how increased utilization of influenza vaccines contributed to a suppressed flu season remains unclear. Besides vaccination, studies found strong COVID-19 mitigating measures reduced the circulation of influenza viruses during the recent flu season [43]. In the US, while some of the social distancing measures were lifted with declining COVID-19 cases, other respiratory infections began to rebound [44]. Similarly, findings from other countries suggest the relaxation of COVID-19 mitigation measures was associated with increased influenza activity [43].
Nevertheless, the role of vaccination in combating flu outbreaks will remain important, as mitigation measures against COVID-19 begin to rescind. Thus, targeting policies to directly impact influenza vaccination rates remains a critical issue [45]. Generally, a better understanding of behaviors among subgroups can help policymakers to incentivize vaccine uptake and reduce disparities more efficiently. Future influenza vaccination campaigns can target minority groups with persistently low vaccination rates, such as the Hispanic and black populations, and other vulnerable groups such as the elderly. Our analysis further underscores the need to target low-income groups, and individuals with low educational attainment even when generous insurance coverage is available.
This study has several limitations. First, our analytical sample was limited to commercially insured adults, and thus not nationally representative. Our findings should not be generalized to uninsured adults and those with other health insurance coverage. Nevertheless, even in this relatively well-off segment of the population, disparities in influenza vaccination persist with respect to demographic and socioeconomic characteristics. Compared to private health insurance, public health insurance and no insurance were associated with worse access to care and less routine health visits, leading to lower influenza vaccination [46], [47]. Given that racial/ethnic minorities, low-income, and low-education groups are less likely to have private insurance coverage, we can expect disparities in the general population to be more severe.
Second, although we captured important demographic information in our estimates, other factors may be associated with our outcome variable. Third, our definition of influenza was based on ICD code and limited to lab-confirmed influenza. If influenza infections were more likely to be diagnosed for individuals who regularly get influenza vaccines, our estimates would be taken as an upward bound of the effect of past infection on vaccination.
Last, while our database has the advantage of being drawn from comprehensive health claims data for insured enrollees, health events with no claims submitted by health providers would not have been captured in the data. Hence, we cannot assess utilization of vaccine which provided directly by employers at workplaces or other non-healthcare locations. To the extent that employers provided expanded opportunities for vaccination during the pandemic that were not paid for through their insurance plans, our analyses would provide an underestimate of the uptick in vaccination rates. In contrast, virtual work opportunities may have caused some employees to substitute conventional locations for employer-based sites, potentially leading to overestimates of disparities with respect to income and education during the pandemic. In practice, these effects are likely to be small.
5. Conclusions
In a national sample of commercially insured US adults, individuals were 1.23 times as likely to get vaccinated against influenza in 2020, compared to 2019. More people received an influenza vaccine at the beginning of the 2020–21 influenza season than the previous season. While disparities with respect to gender and race narrowed, they worsened across income groups and educational levels. Although all income groups experienced increases of vaccination rates, the richest group improved the most. Poorer individuals had lower vaccination rates in both periods. The vaccination rate rose substantially during the pandemic for college-educated enrollees while improvements for non-college-educated enrollees were relatively smaller. These disparities were likely to be more pronounced in the general population.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
We thank Wei Lyu, PhD for helpful comments.
Author contributions
K. Li conceptualized the presented idea and wrote the first draft. T. Yu conducted the statistical analysis and wrote the first draft. S. A. Seabury and A. Dor supervised the study. All authors designed the study and critically revised the manuscript. K. Li and T. Yu should be considered joint first author.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Research data for this article
The data that support the findings of this study are available from the Optum Clinformatics® Data Mart. Restrictions apply to the availability of these data, which were used under license for this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.03.058.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Rolfes M.A., Flannery B., Chung J.R., O’Halloran A., Garg S., Belongia E.A., et al. Effects of Influenza Vaccination in the United States During the 2017–2018 Influenza Season. Clin Infect Dis. 2019;69(11):1845–1853. doi: 10.1093/cid/ciz075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Flu Vaccination Coverage, United States, 2019–20 Influenza Season. Published October 1, 2020. Accessed August 17, 2021. https://www.cdc.gov/flu/fluvaxview/coverage-1920estimates.htm.
- 3.Jain A., van Hoek A.J., Boccia D., Thomas S.L. Lower vaccine uptake amongst older individuals living alone: A systematic review and meta-analysis of social determinants of vaccine uptake. Vaccine. 2017;35(18):2315–2328. doi: 10.1016/j.vaccine.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Galarce E.M., Minsky S., Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine. 2011;29(32):5284–5289. doi: 10.1016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 5.CDC. Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Published July 6, 2021. Accessed August 17, 2021. https://www.cdc.gov/flu/highrisk/disparities-racial-ethnic-minority-groups.html.
- 6.Grohskopf L.A., Liburd L.C., Redfield R.R. Addressing Influenza Vaccination Disparities During the COVID-19 Pandemic. JAMA. 2020;324(11):1029–1030. doi: 10.1001/jama.2020.15845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grohskopf L.A., Alyanak E., Broder K.R., Blanton L.H., Fry A.M., Jernigan D.B., et al. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2020–21 Influenza Season. MMWR Recomm Rep. 2020;69(8):1–24. doi: 10.15585/mmwr.rr6908a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Medicare & Medicaid Services. CMS announces launch of 2020 flu season campaign, providing partner resources. Accessed August 17, 2021. https://www.cms.gov/newsroom/press-releases/cms-announces-launch-2020-flu-season-campaign-providing-partner-resources.
- 9.CDC. Upcoming 2020-2021 Influenza Season. Centers for Disease Control and Prevention. Published July 22, 2021. Accessed September 4, 2021. https://www.cdc.gov/flu/season/faq-flu-season-2020-2021.htm.
- 10.May T. Public Communication, Risk Perception, and the Viability of Preventive Vaccination Against Communicable Diseases. Bioethics. 2005;19(4):407–421. doi: 10.1111/j.1467-8519.2005.00452.x. [DOI] [PubMed] [Google Scholar]
- 11.Commonwealth Fund. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges. doi: 10.26099/ds9e-jm36.
- 12.Health Care Cost Institute. The Impact of COVID-19 on the Use of Preventive Health Care. HCCI. Accessed August 17, 2021. https://healthcostinstitute.org/hcci-research/the-impact-of-covid-19-on-the-use-of-preventive-health-care.
- 13.Alexander G.C., Tajanlangit M., Heyward J., Mansour O., Qato D.M., Stafford R.S. Use and Content of Primary Care Office-Based vs Telemedicine Care Visits During the COVID-19 Pandemic in the US. JAMA Network Open. 2020;3(10):e2021476. doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schweiberger K., Patel S.Y., Mehrotra A., Ray K.N. Trends in Pediatric Primary Care Visits During the Coronavirus Disease of 2019 Pandemic. Acad Pediatrics. 2021;21(8):1426–1433. doi: 10.1016/j.acap.2021.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC. Early-Season Influenza Vaccination Uptake and Intent Among Adults – United States, September 2020. Published December 23, 2020. Accessed August 17, 2021. https://www.cdc.gov/flu/fluvaxview/nifs-estimates-sept2020.htm.
- 16.Macy M.L., Smith T.L., Cartland J., Golbeck E., Davis M.M. Parent-reported hesitancy to seek emergency care for children at the crest of the first wave of COVID-19 in Chicago. Acad Emerg Med. 2021;28(3):355–358. doi: 10.1111/acem.14214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CDC. Weekly U.S. Influenza Surveillance Report. Published August 13, 2021. Accessed August 17, 2021. https://www.cdc.gov/flu/weekly/index.htm.
- 18.Racial Data Dashboard. The COVID Tracking Project. Accessed November 2, 2021. https://covidtracking.com/race/dashboard.
- 19.CDC. COVIDView, Key Updates for Week 22. Centers for Disease Control and Prevention. Published June 5, 2020. Accessed November 2, 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/past-reports/06052020.html.
- 20.Kim E.J., Kim T., Conigliaro J., Liebschutz J.M., Paasche-Orlow M.K., Hanchate A.D. Racial and Ethnic Disparities in Diagnosis of Chronic Medical Conditions in the USA. J Gen Intern Med. 2018;33(7):1116–1123. doi: 10.1007/s11606-018-4471-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Link B.G., Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995 Spec No: 80-94. [PubMed] [Google Scholar]
- 22.Selden T.M., Berdahl T.A. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Affairs. 2020;39(9):1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- 23.Freeman S. Flu vaccination this season likely to be highest ever. UGA Today. Published February 24, 2021. Accessed August 17, 2021. https://news.uga.edu/flu-vaccination-this-season-likely-highest-ever/.
- 24.CDC. Influenza Vaccinations Administered to Adults in Pharmacies and Physician Medical Offices, United States. Published May 5, 2021. Accessed August 29, 2021. https://www.cdc.gov/flu/fluvaxview/dashboard/vaccination-administered.html.
- 25.Sokol R.L., Grummon A.H. COVID-19 and parent intention to vaccinate their children against influenza. Pediatrics. 2020;146(6) doi: 10.1542/peds.2020-022871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.CDC. Seasonal Influenza Vaccine Supply for the U.S. 2021-2022 Influenza Season. Published July 1, 2021. Accessed August 17, 2021. https://www.cdc.gov/flu/prevent/vaxsupply.htm.
- 27.Jin G.Z., Koch T.G. Learning By Suffering?: Patterns in Flu Vaccination Take-Up. Am J Health Econ. 2021;7(1):68–94. doi: 10.1086/711564. [DOI] [Google Scholar]
- 28.The White House. Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak – The White House. Accessed August 17, 2021. https://trumpwhitehouse.archives.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/.
- 29.Centers for Medicare & Medicaid Services. Flu Shot Coding. Accessed September 4, 2021. https://www.cms.gov/medicare/preventive-services/flu-shot-coding.
- 30.CDC. IIS: NDC Lookup Crosswalk. Published September 25, 2018. Accessed September 4, 2021. https://www.cdc.gov/vaccines/programs/iis/code-sets.html.
- 31.Chapman G.B., Coups E.J. Predictors of Influenza Vaccine Acceptance among Healthy Adults. Prev Med. 1999;29(4):249–262. doi: 10.1006/pmed.1999.0535. [DOI] [PubMed] [Google Scholar]
- 32.Quinn S.C., Jamison A.M., Freimuth V.S., An J., Hancock G.R. Determinants of influenza vaccination among high-risk Black and White adults. Vaccine. 2017;35(51):7154–7159. doi: 10.1016/j.vaccine.2017.10.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.CDC. 2019 BRFSS Survey Data and Documentation. Published August 31, 2020. Accessed September 4, 2021. https://www.cdc.gov/brfss/annual_data/annual_2019.html.
- 34.CDC. 2020 BRFSS Survey Data and Documentation. Published August 27, 2021. Accessed September 4, 2021. https://www.cdc.gov/brfss/annual_data/annual_2020.html.
- 35.Lu P.-J., O'Halloran A., Bryan L., Kennedy E.D., Ding H., Graitcer S.B., et al. Trends in racial/ethnic disparities in influenza vaccination coverage among adults during the 2007–08 through 2011–12 seasons. Am J Infect Control. 2014;42(7):763–769. doi: 10.1016/j.ajic.2014.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu D., Qiao Y., Brown N.E., Wang J., Cowling B.J. Racial and Ethnic Disparities in Influenza Vaccination among Adults with Chronic Medical Conditions Vary by Age in the United States. PLoS ONE. 2017;12(1):e0169679. doi: 10.1371/journal.pone.0169679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quinn S.C., Jamison A., Freimuth V.S., An J., Hancock G.R., Musa D. Exploring racial influences on flu vaccine attitudes and behavior: Results of a national survey of White and African American adults. Vaccine. 2017;35(8):1167–1174. doi: 10.1016/j.vaccine.2016.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Worasathit R., Wattana W., Okanurak K., Songthap A., Dhitavat J., Pitisuttithum P. Health education and factors influencing acceptance of and willingness to pay for influenza vaccination among older adults. BMC Geriatr. 2015;15:136. doi: 10.1186/s12877-015-0137-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lin C.J., Nowalk M.P., Toback S.L., Rousculp M.D., Raymund M., Ambrose C.S., et al. Importance of vaccination habit and vaccine choice on influenza vaccination among healthy working adults. Vaccine. 2010;28(48):7706–7712. doi: 10.1016/j.vaccine.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Case A, Deaton A. Deaths of Despair and the Future of Capitalism; 2021. Accessed August 29, 2021. https://press.princeton.edu/books/paperback/9780691217079/deaths-of-despair-and-the-future-of-capitalism.
- 41.Armstrong K., Berlin M., Schwartz S.J., Propert K., Ubel P.A. Educational Content and the Effectiveness of Influenza Vaccination Reminders. J Gen Intern Med. 1999;14(11):695–698. doi: 10.1046/j.1525-1497.1999.11098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zipfel C.M., Colizza V., Bansal S. The missing season: The impacts of the COVID-19 pandemic on influenza. Vaccine. 2021;39(28):3645–3648. doi: 10.1016/j.vaccine.2021.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sovann L.Y., Sar B., Kab V., Yann S., Kinzer M., Raftery P., et al. An influenza A (H3N2) virus outbreak in the Kingdom of Cambodia during the COVID-19 pandemic of 2020. Int J Infect Dis. 2021;103:352–357. doi: 10.1016/j.ijid.2020.11.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.CDC. RSV National Trends – NREVSS. Published August 9, 2021. Accessed August 17, 2021. https://www.cdc.gov/surveillance/nrevss/rsv/natl-trend.html.
- 45.Wen FT, Malani A, Cobey S. The beneficial effects of vaccination on the evolution of seasonal influenza. 2020: 1625. doi: 10.1101/162545.
- 46.Cambou M.C., Copeland T.P., Nielsen-Saines K., Macinko J. Insurance status predicts self-reported influenza vaccine coverage among pregnant women in the United States: A cross-sectional analysis of the National Health Interview Study Data from 2012 to 2018. Vaccine. 2021;39(15):2068–2073. doi: 10.1016/j.vaccine.2021.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Akpalu Y., Sullivan S.J., Regan A.K. Association between health insurance coverage and uptake of seasonal influenza vaccine in Brazos County, Texas. Vaccine. 2020;38(9):2132–2135. doi: 10.1016/j.vaccine.2020.01.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.