Abstract
Background and Purpose
Recent epidemiological data indicate that the absolute number of hemorrhagic stroke cases increased by 47% between 1990 and 2010 and continued to cause high rates of death and disability. The last systematic review and meta-analysis of incidence and long-term survival of intracerebral hemorrhage (ICH) were published 11 and 7 years ago, respectively, and lacked comparison between different income groups, therefore, a more up to date analysis is needed. We aim to investigate the ICH incidence and long-term survival data in countries of different income groups.
Materials Methods
We systematically searched Ovid Medline for population-based longitudinal studies of first-ever spontaneous ICH published from January 2000 to December 2020. We performed meta-analyses on the incidence and survival rate in countries of 4 different income groups with random-effects models (severe inconsistency). The I2 was used to measure the heterogeneity. Heterogeneity was further investigated by conducting the meta-regression on the study mid-year. Time trends of the survival rate were assessed by weighted linear regression.
Results
We identified 84 eligible papers, including 68 publications reporting incidence and 24 publications on the survival rate. The pooled incidence of ICH per 100,000 per person-years was 26.47 (95% CI: 21.84–32.07) worldwide, 25.9 (95% CI: 22.63–29.63) in high-income countries (HIC), 28.45 (95% CI: 15.90–50.88) in upper-middle-income countries, and 31.73 (95% CI: 18.41–54.7) in lower-middle-income countries. The 1-year pooled survival rate was from 50% (95% CI: 47–54%; n = 4,380) worldwide to 50% (95% CI: 47–54%) in HIC, and 46% (95% CI: 38–55%) in upper-middle income countries. The 5-year pooled survival rate was 41% (95% CI: 35–48%; n = 864) worldwide, 41% (95% CI: 32–50%) in high-income and upper-middle countries. No publications were found reporting the long-term survival in lower-middle-income and low-income countries. No time trends in incidence or survival were found by meta-regression.
Conclusion
The pooled ICH incidence was highest in lower-middle-income countries. About half of ICH patients survived 1 year, and about two-fifths survived 5 years. Reliable population-based studies estimating the ICH incidence and long-term survival in low-income and low-middle-income countries are needed to help prevention of ICH.
Systematic Review Registration
https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=170140, PROSPERO CRD42020170140.
Keywords: intracerebral hemorrhage, stroke, incidence, survival, systematic review, meta-analysis
Introduction
Stroke pathological subtypes include ischemic stroke and hemorrhagic stroke [primary intracerebral hemorrhage (ICH) and subarachnoid hemorrhage (SAH)]. Non-traumatic (spontaneous) ICH is caused by the rupture of small penetrating arteries in the brain and has high mortality and severe disability (1). ICH accounts for 10–15% of strokes worldwide, approximately 20% in low- and middle-income (LMIC) countries and 10% in high-income countries (HIC) (2). According to Global Burden of Disease (GBD) 2010, the absolute number of hemorrhagic stroke cases increased 47% between 1990 and 2010 and caused about 62.8 million disability-adjusted life years (DALYs) lost (86% in LMIC), a significant regional difference in incidence was also found (3).
Long-term prospective population-based studies can provide the most reliable data on stroke incidence. The last systematic review and meta-analysis of population-based studies on ICH incidence were published 11 years ago. Charlotte van Asch et al. found that the worldwide ICH incidence has not decreased over time (4). The overall stroke incidence in low- to middle-income countries has exceeded 20% more than that of high-income countries; however, the comparison of ICH incidence in different income groups remains unclear (2). The last meta-analysis of long-term survival (1 year or more) after ICH was published 7 years ago (5). However, they did not report ICH survival in countries of different income levels. In addition, the pooled estimates of incidence and survival rate in those reviews spanned about 40 years of the study period, which may reduce the comparability and reliability. Since then, several new population-based studies have been published, resulting in a need to update systematic reviews. We, therefore, carried out this systematic review and meta-analysis to update the incidence and long-term survival data of ICH in various income groups.
Methods
The systematic review and meta-analysis were conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA), Meta-analysis of Observational Studies in Epidemiology (MOOSE), and this study has been registered on PROSPERO (CRD42020170140) (6, 7). The study protocol was not previously published.
Search Strategy
We searched Ovid Medline and PubMed database for population-based longitudinal studies of spontaneous ICH from January 2000 to December 2020, using the comprehensive electronic literature search strategy with a combination of different keywords “population,” “population-based,” “regional,” “community,” “stroke register,” “incidence,” “fatality,” “mortality,” “trend,” “survival,” “h(a)emorrhagic stroke,” “intracranial h(a)emorrhage,” “cerebral h(a)emorrhage,” “intracerebral h(a)emorrhage,” “haemorrhage,” or “h(a)ematoma.” The detailed searching strategy is in Appendix 1 in Supplementary Material. Further eligible studies were reviewed through reference lists and advice from experts to avoid missing any literature.
Eligibility Criteria
We included population-based studies reporting incidence or long-term survival (1 year and 5 years) of lifetime ICH. We only included prospective studies in the incidence analysis because there are numbers of new cases of ICH in the target population over the specified study period, which enable us to calculate incidence. However, we included both prospective and retrospective studies in the survival analysis. Only papers published in English were included.
We excluded studies if: (1) they only investigated the >85 years old and pediatric/adolescent (<18 years old) population; (2) hospital-based studies; (3) the data cannot be extracted for analysis; (4) ICH was not an incident event; (5) they included non-spontaneous or traumatic ICH cases into the ICH group; (6) they included subarachnoid hemorrhage or pure intraventricular hemorrhage into the ICH group; (7) there was no clear illustration of most ICH case ascertainment using imaging or pathological methods (autopsy) since the imaging techniques for identifying stroke subtypes were widely used since the 1990s; (8) over half of the study period was before 1995; (9) the total study sample size less than 20, which means the cohort or population size in incidence studies and ICH patient numbers in survival studies; and (10) it was not first-ever ICH.
Study Selection
Two investigators (XL and LZ) independently undertook the search and screening. One investigator (XL) first screened all titles and abstracts after removing duplicate papers. The remaining studies were read in full for eligibility assessment to be included in the final analysis by the second investigator (LZ). The disagreements and uncertainties in the process were resolved by discussion with a third reviewer (YW).
Data Extraction
We extracted each study period accurate to month if possible and calculated the study midyear, which is used to represent the study time for each independent study. If the study period was an even number, we assessed the midyear as the next year of the middle time point (e.g., study period: 2001, 2002, 2003, 2004, midyear: 2003). Additionally, we assessed the number of incident ICH cases in the study period, number of person-years, number of survivors after 1 year or 5 years, and the number of study population if applicable. We calculated person-years by multiplying the number of the study population and total study years together if it was not directly reported in the study. If several published papers were from the same longitudinal study (e.g., stroke registry), we extracted data from papers with the longest person-years or papers reporting different periods of the same stroke study. We recorded the age information for studies reporting incidence. Countries and their income levels {(I) high income, (II) upper-middle income, (III) lower to middle income, (IV) low income according to the World Bank's country classification (8)} were recorded.
Quality Assessment of Studies
The Newcastle Ottawa scale (NOS) (9) was used to evaluate the quality of the cohort study. The evaluation criteria initially include (I) selection: (1) the representativeness of the exposed cohort, (2) selection of the non-exposed cohort, (3) ascertainment of exposure, (4) outcome of interest was not present at the start of the study; (II) (5&6) comparability of exposed and non-exposed cohorts; (III) outcome: (7) assessment of outcome, (8) length, and (9) adequacy of follow up. However, due to the nature of our eligible studies, there is no information about the exposed cohort. Therefore we use (1), (4), (7), (8), and (9) to perform the quality assessment; the maximum score is 5, which means very high quality, 4 means high quality, 3 means acceptable quality, and 1 and 2 means relatively low quality.
Statistical Methods
The incidence was computed as the number of ICH cases per 100,000 person-years. Survival rate was calculated as the proportion of survivors of ICH at 1 year or 5 years. Incidences and survival rates were separately visualized in world maps. Different shades of color means the density and the gray area indicates no data. Median was used if more than one study reported incidences or survival rates in one country. We performed meta-analyses for both incidences, 1-year survival rate and 5-year survival rate using statistical software R.3.6.3. The I2 and Cochran's Q-test were used to measure the heterogeneity across studies. About 25, 50, and 75% were considered the cut-off of I2values that indicate the low, moderate, and high degree of heterogeneity, respectively. A random-effects model with DerSimonian and Laird method was used in the meta-analyses of incidence and survival rate of ICH to generate a pooled estimate because of the high heterogeneity across studies. Subgroup analyses of countries on different income levels and meta-regression of study midyear were conducted to identify the source of heterogeneity. A weighted linear regression was used to assess the temporal trend of the survival between survival and the mid-year of study periods; the reverse of standard error in each study was used as weight. Sensitivity analyses were performed to examine the impact of any single study on the pooled estimate result. Funnel plots were used to evaluate the publication bias. A p < 0.05 was considered statistically significant.
Results
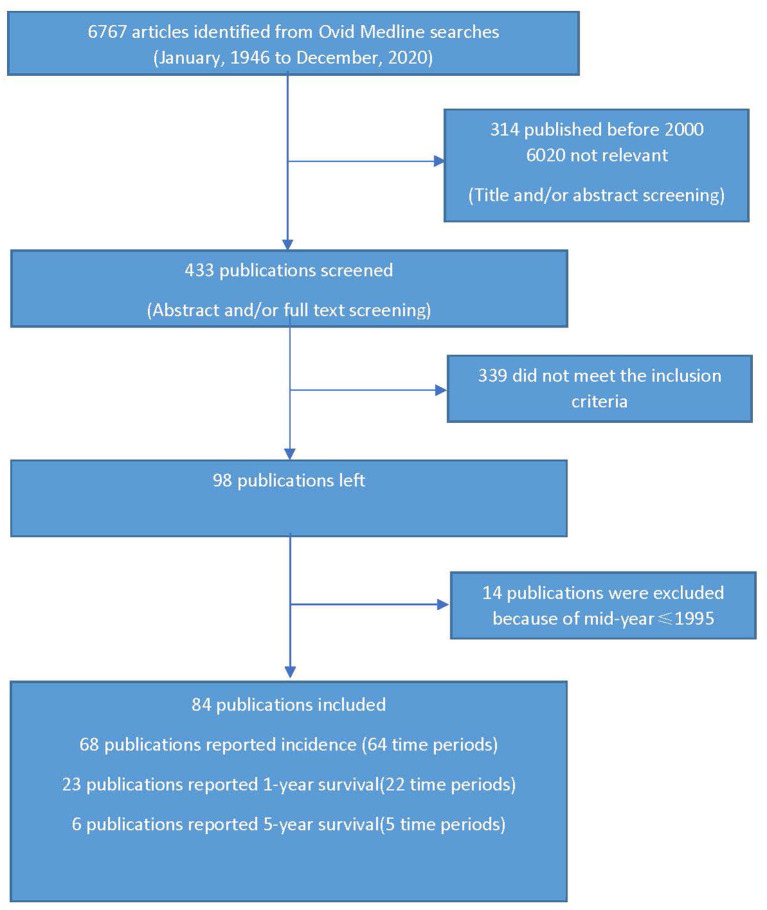
We initially retrieved 6,767 potentially relevant publications (Figure 1). The titles, abstracts, and publication time were scanned for appropriateness for our review, and those not relevant were removed (6,334). The abstracts and full text of the remaining 433 studies were reviewed to meet the inclusion criteria and 339 publications were removed. Data of the remaining 98 manuscripts were then extracted, which led to the exclusion of a further 14 manuscripts whose mid-year of study period did not meet the eligibility criteria. Thus, 84 eligible population-based studies in 25 countries were available for analysis, of which 68 articles reported 64 time periods about incidence, 23 articles reported 22 time periods about 1-year survival, 6 articles reported 5 time periods about 5-year survival (Tables 1, 2; Figure 5). There are 8 publications reporting both incidence and survival. All these eligible papers were published after 2000, in which the study time periods ranged from 1987 to 2017. One publication may report several time periods of incidence or survival rate (studies with long follow-up time). Several publications may report the same time periods (publications from the same database or stroke center/registry). Therefore we use “time periods” other than “studies” to specifically represent the parameter included in this meta-analysis.
Figure 1.
Literature search.
Table 1.
Characteristics of studies reporting incidences on intracerebral hemorrhage (ICH).
| References | Country | Income level | Study period | Mid-year of study | ICH patients (n)/person years | Incidence rate (per 100,000 per year) | Age range |
|---|---|---|---|---|---|---|---|
| Wolfe et al. (10) | Dijon, France | High | 1995.01–1997.12 | 1996 | 37/429,264 | 8.62 | No |
| Thrift et al. (11) | Melbourne, Australia | High | 1996.05–1997.04 | 1996 | 40/429,264 | 29.89 | No |
| Di Carlo et al. (12) | Vibo Valentina, Italy | High | 1996.01–1996.12 | 1996 | 62/179,186 | 34.60 | No |
| Sacco et al. (13) | l'Aquila, Italy | High | 1994.01–1998.12 | 1996 | 549/1,488,225 | 36.89 | No |
| Marini et al. (14) | |||||||
| D'Alessandro et al. (15) | Valle d'Aosta, Italy | High | 1996.11–1997.10 | 1997 | 36/118,723 | 30.32 | No |
| Kita et al. (16) | Takashima, Japan | High | 1996–1998 | 1997 | 73/166,353 | 43.88 | No |
| Ishikawa et al. (17) | 12 districts, Japan | High | 1992.04–2005.12 | 1998 | 102/131,718 | 77.44 | No |
| Zhang et al. (18) | China | Upper-middle | 1996–2000 | 1998 | 2,275/5,657,595 | 40.21 | >25 |
| Smadja et al. (19) | Martinique | High | 1998.06–1999.05 | 1998 | 83/360000 | 23.06 | No |
| Thrift et al. (20) | Melbourne, Australia | High | 1997.05–1999.04 | 1998 | 151/613,262 | 24.62 | No |
| Correia et al. (21) | North Portugal | High | 1998.10–2000.09 | 1999 | 108/243,116 | 44.42 | No |
| Appelros et al. (22) | Örebro, Sweden | High | 1999.02–2000.01 | 1999 | 44/123503 | 35.63 | No |
| Syme et al. (23) | Scotland, UK | High | 1998.10–2000.09 | 1999 | 50/212,704 | 23.51 | No |
| Suzuki et al. (24) | Akita, Japan | High | 1995–2004 | 1999 | 7,423/12,000,000 | 61.86 | No |
| Kolominsky-Rabas et al. (25) | Erlangen, Germany | High | 1995.01–2002.12 | 1999 | 194/841,312 | 23.06 | No |
| Correia et al. (26) | Porto, Portugal | High | 1998–2000 | 1999 | 78/172,046 | 45.34 | No |
| Islam et al. (27) | Perth, Australia | High | 2000.02–2001.02 | 2000 | 19/143,417 | 13.25 | No |
| Heuschmann et al. (28) | South London, UK | High | 1995–2004 | 2000 | 395/2,701,909 | 14.62 | No |
| Smeeton et al. (29) | |||||||
| Giroud et al. (30) | Dijon, France | High | 1987.01–2012.12 | 2000 | 530/3,896,484 | 13.60 | No |
| Kita et al. (16) | Takashima, Japan | High | 1999–2001 | 2000 | 89/166,353 | 53.50 | No |
| Vaartjes et al. (31) | Netherlands | High | 2000 | 2000 | 3,791/13,657,649 | 27.76 | No |
| Hallstrom et al. (32) | Lund, Sweden | High | 2001.03–2002.02 | 2001 | 46/235,505 | 19.53 | >15 |
| Hallstrom et al. (33) | |||||||
| Lavados et al. (34) | Iquique, Chile | High | 2000.07–2002.06 | 2001 | 69/396,712 | 17.39 | No |
| Lavados et al. (35) | |||||||
| Feigin et al. (36) | Auckland, New Zealand | High | 2002.03–2003.02 | 2002 | 177/897,882 | 19.71 | >15 |
| Corbin et al. (37) | Barbados | High | 2001.10–2002.09 | 2002 | 42/239,068 | 17.57 | No |
| Manobianca et al. (38) | Puglia, Italy | High | 2001.01–2002.12 | 2002 | 24/77,474 | 30.98 | No |
| Vibo et al. (39) | Tartu, Estonia | High | 2001.12–2003.11 | 2002 | 57/202,244 | 28.18 | No |
| Li et al. (40) | Tianjin, China | Upper-middle | 1999–2005 | 2002 | 53/100,297 | 52.84 | No |
| Wang et al. (41) | |||||||
| Wang et al. (42) | |||||||
| Manobianca et al. (43) | Puglia, Italy | Upper-middle | 2001.01–2002.12 | 2002 | 24/77,470 | 30.98 | No |
| Dalal et al. (44) | Oxford, UK | High | 2002.04–2004.03 | 2003 | 34/273,318 | 12.44 | No |
| Rothwell et al. (45) | |||||||
| Minelli et al. (46) | Matão, Brazil | Upper-middle | 2003.11–2004.10 | 2004 | 11/75,053 | 14.66 | No |
| Carlsson et al. (47) | Tromsø, Norway | High | 1995.01–2012.12 | 2004 | 226/453,152 | 49.87 | ≥30 |
| Kleindorfer et al. (48) | 5 counties, USA | High | 2005.01–2005.12 | 2005 | 321/1,319,856 | 24.32 | No |
| Kissela et al. (49) | |||||||
| Corso et al. (50) | Aosta, Italy | High | 2004.01–2005.12 | 2005 | 58/247,496 | 23.43 | No |
| Groppo et al. (51) | Ferrara, Italy | High | 2002–2007 | 2005 | 10/323,250 | 3.09 | 15-44 |
| Dalal et al. (44) | Mumbai, India | Lower-middle | 2005.01–2006.12 | 2006 | 67/313,722 | 21.36 | >25 |
| Cabral et al. (52) | Joinville, Brazil | Upper-middle | 2005–2006 | 2006 | 88/791,675 | 11.12 | No |
| Cabral et al. (53, 54) | |||||||
| Kelly et al. (55) | Dublin, Ireland | High | 2005.12–2006.11 | 2006 | 56/294,529 | 19.01 | No |
| Amiri et al. (56) | Mashhad, Iran | Upper-middle | 2006.11–2007.11 | 2007 | 90/450,229 | 19.99 | No |
| Azarpazhooh et al. (57) | |||||||
| Boden-Albala et al. (58) | Alaska, USA | High | 2005.10–2009.10 | 2007 | 47/560,000 | 8.39 | No |
| Kolominsky-Rabas et al. (25) | Erlangen, Germany | High | 2003.01–2010.12 | 2007 | 200/841,312 | 23.77 | No |
| Palm et al. (59) | Ludwigshafen, Germany | High | 2006.01–2010.12 | 2008 | 152/838,285 | 18.13 | No |
| Janes et al. (60) | Udine, Italy | High | 2007.04–2009.03 | 2008 | 95/306,624 | 30.98 | No |
| Pikija et al. (61) | VaraŽdin, Croatia | High | 2007.07–2009.06 | 2008 | 123/368,230 | 33.40 | No |
| Li et al. (40) | Tianjin, China | Upper-middle | 2006–2012 | 2009 | 106/100,157 | 105.83 | No |
| Wang et al. (41) | |||||||
| Wang et al. (42) | |||||||
| Gattellari et al. (62) | New South Wales, Australia | High | 2005.01–2013.12 | 2009 | 12986/51,185,251 | 25.37 | No |
| Neelamegam et al. (63) | Penang Island, Malaysia | Upper-middle | 2010.04–2011.03 | 2010 | 32/197,131 | 16.23 | No |
| Correia et al. (26) | Porto, Portugal | High | 2009–2011 | 2010 | 43/204,424 | 21.03 | No |
| Cabral et al. (52) | Joinville, Brazil | Upper-middle | 2010–2011 | 2011 | 82/760,172 | 10.79 | No |
| Stranjalis et al. (64) | The Isle of Lesvos, Greece | High | 2010.06–2011.05 | 2011 | 52/86,436 | 60.16 | No |
| Tsivgoulis et al. (65) | Evros, Greece | High | 2010–2012 | 2011 | 83/119,805 | 69.28 | >20 |
| Takashima et al. (66) | Shiga, Japan | High | 2011 | 2011 | 551/1,400,745 | 39.34 | No |
| Samarasekera et al. (67) | Scotland, UK | High | 2010.06–2011.05 | 2011 | 128/695,335 | 18.41 | ≥16 |
| Okon et al. (68) | Akure, Nigeria | Lower-middle | 2010.11–2011.10 | 2011 | 265/491,033 | 54.00 | No |
| Sacco et al. (69) | l'Aquila, Italy | High | 2011.01–2012.12 | 2012 | 115/596,686 | 19.27 | No |
| Pandian et al. (70) | Ludhiana, India | Lower-middle | 2012.03–2013.03 | 2012 | 290/1,065,127 | 27.23 | ≥18 |
| Olindo et al. (71) | Martinique | High | 2011.11–2012.10 | 2012 | 84/370,854 | 22.65 | No |
| Chen et al. (72) | 10 areas, China | Upper-middle | 2008.01–2017.01 | 2012 | 7,440/4,406,274 | 168.85 | 35–74 |
| Wang et al. (73) | China | Upper-middle | 2013 | 2013 | 391/479,044 | 81.62 | ≥20 |
| Saliba et al. (74) | Israel | High | 2010.01–2017.12 | 2014 | 4170/10,730,915 | 38.86 | ≥40 |
| Cabral et al. (52) | Joinville, Brazil | Upper-middle | 2014–2015 | 2015 | 79/789,418 | 10.01 | No |
| Nzwalo et al. (75) | Algarve, Portugal | High | 2015.01–2015.12 | 2015 | 82/280,081 | 29.28 | No |
| Minelli et al. (76) | Matao, Brazil | Upper-middle | 2015.08–2016.07 | 2016 | 10/78,890 | 12.68 | No |
| Appelros et al. (77) | Örebro, Sweden | High | 2017.01–2017.12 | 2017 | 36/150,291 | 23.95 | No |
Table 2.
Characteristics of studies reporting survival rate after 1 year and/or 5 years on ICH.
| Studies | Country | Income level | Study period | Mid-year of study | ICH patients (n) | 1-year survivors (n) | 5-year survivors (n) |
|---|---|---|---|---|---|---|---|
| Thrift et al. (11) | Melbourne, Australia | High | 1996.05–1997.04 | 1996 | 40 | 20 | |
| Di Carlo et al. (12) | Vibo Valentina, Italy | High | 1996.01–1996.12 | 1996 | 62 | 27 | |
| Sacco et al. (13) | L'Aquila, Italy | High | 1994–1998 | 1996 | 464 | 225 | |
| Hillen et al. (78) | London, UK | High | 1995–2000 | 1998 | 222 | 110 | 72 |
| Thrift et al. (20) | Melbourne, Australia | High | 1997–1999 | 1998 | 151 | 76 | |
| Syme et al. (23) | Southeast Scotland, UK | High | 1998.10–2000.09 | 1999 | 50 | 22 | |
| Vibo et al. (39) | Tarsu, Estonia | High | 2001–2003 | 2002 | 57 | 26 | |
| Hansen et al. (79) | Southern Sweden | High | 1996–2009 | 2003 | 323 | 172 | 127 |
| Waziry et al. (80) | Rotterdam, Netherlands | High | 1991–2015 | 2003 | 162 | 55 | |
| McCormick et al. (81) | London, UK | High | 1995–2011 | 2003 | 562 | 297 | |
| van Beijnum et al. (82) | Oxford, UK | High | 2002–2007 | 2005 | 56 | 22 | |
| Shoeibi et al. (83) | Mashhad, Iran | Upper-middle | 2006.11–2007.11 | 2007 | 86 | 38 | |
| Palm et al. (59) | Ludwigshafen, Germany | High | 2006–2010 | 2008 | 152 | 85 | |
| Desikan et al. (84) | London, UK | High | 2005–2012 | 2009 | 204 | 106 | |
| Farzadfard et al. (85) | Mashhad, Iran | Upper-middle | 2006–2012 | 2009 | 80 | 38 | 31 |
| Samarasekera et al. (67) | Scotland, UK | High | 2010.06–2011.05 | 2010 | 128 | 56 | |
| Oie et al. (86) | Norway | High | 2008.01–2014.12 | 2011 | 452 | 249 | |
| Tsivgoulis et al. (87) | Southern Greece | High | 2010– 2012 | 2011 | 83 | 44 | |
| Nzwalo et al. (88) | Algarve, Portugal | High | 2009–2015 | 2012 | 545 | 296 | |
| Olindo et al. (89) | Martinique | High | 2011.11–2012.10 | 2012 | 84 | 43 | |
| Takashima et al. (90) | Shiga, Japan | High | 2011–2013 | 2012 | 551 | 390 | |
| Sacco et al. (69) | L'Aquila, Italy | High | 2011–2012 | 2012 | 115 | 55 | |
| Cabral et al. (91) Cabral et al. (92) |
Joinvile, Brazil | Upper-middle | 2010.01–2015.12 | 2013 | 35 | 18 | 16 |
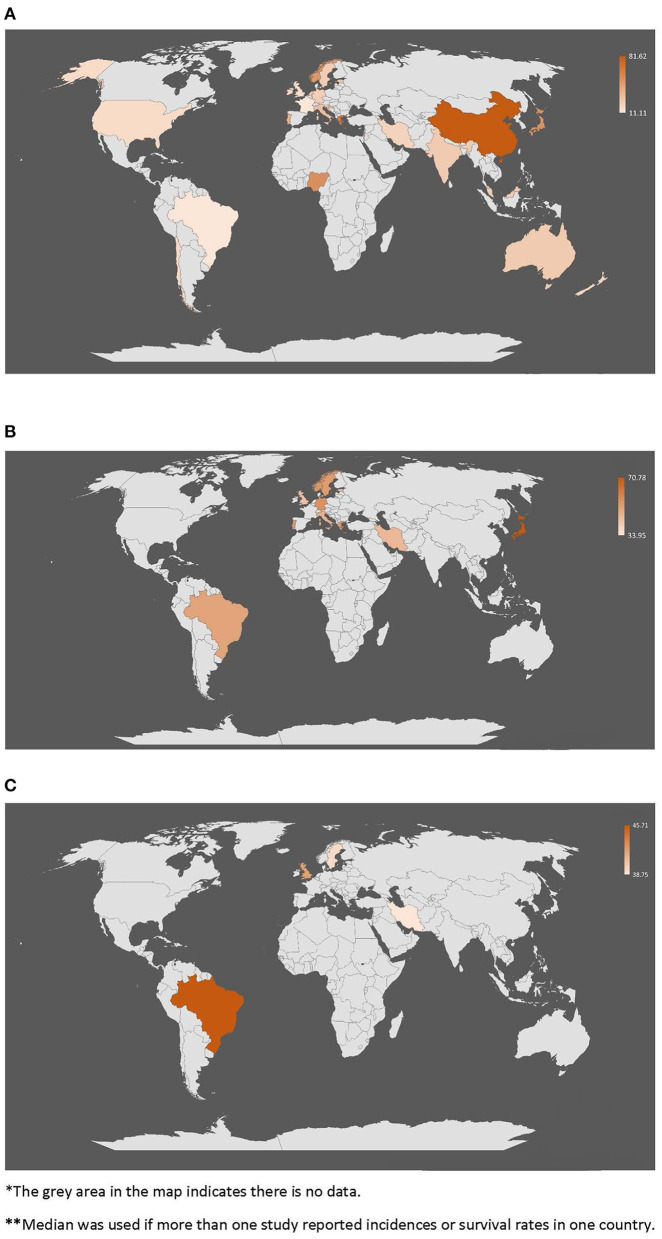
Figure 5.
World map * of incidence and 1-year/5-year survival rates **. (A) Incidences of intracerebral hemorrhage across the world (per 100,000 per year). (B) 1-year survival rate of intracerebral hemorrhage across the world (%). (C) 5-year survival rate of intracerebral hemorrhage across the world (%).
Incidence of ICH
Overall, 64 time periods with 45,224 patients of 127,308,087 person-years were included, of which 19 time periods had a number of person-years less than 200,000, 33 time periods from 200,000 to 1,000,000, 8 time periods from 1,000,000 to 10,000,000, and only 4 study periods more than 10,000,000 (Table 1). However, the range of crude incidence varied from 3.09 to 105.83 per 100,000 person-years across studies. The greatest incidence, 168.85 per 100,000 person-years from China, was about 6 times greater than the median incidence (average of the United States and Australia) 24.47 per 100,000 persons-years. Japan has the greatest incidence 77.44 per 100,000 person-years among high-income countries (HIC) and 53.97 per 100,000 person-years in Akure, Nigeria is the greatest in lower-middle income countries. Studies of 12 time periods had an age limitation, of which one study in Ferrara, Italy includes only patients from 15 to 44 years old (51). The sensitivity analysis of the incidence in 52 time periods in studies without age limitation was 25.38 (95% CI: 21.97–29.32, I2 = 99.10%) per 100,000 person-years.
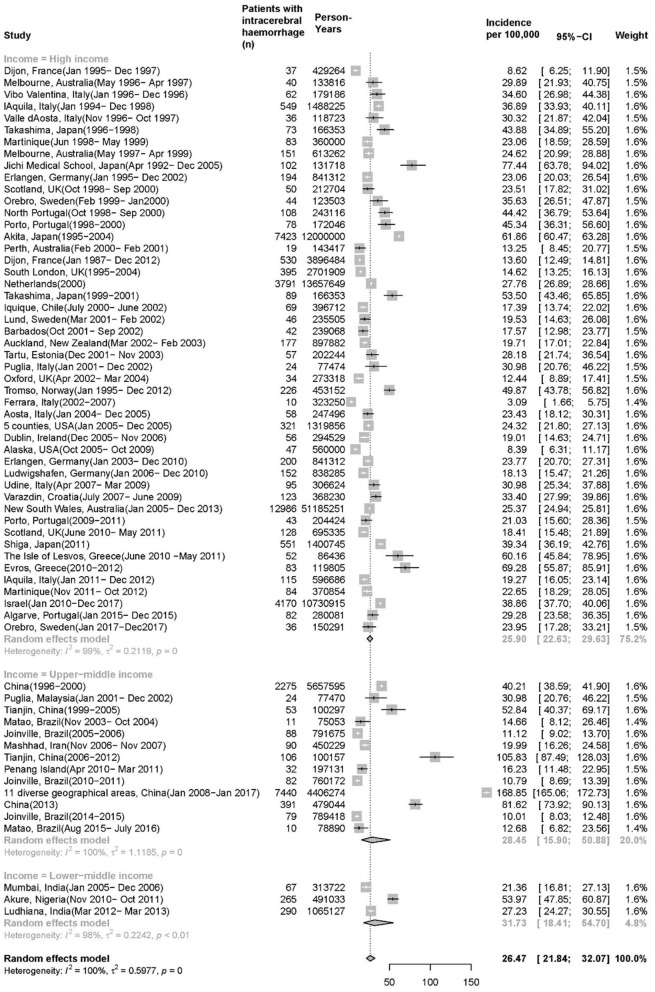
There are 48 time periods with 33,921 patients and 111,474,800 person-years, 13 time periods with 10,681 patients and 13,963,405 person-years, 3 time periods with 411 patients and 1,869,882 person-years of high-income, upper-middle income and low-middle income countries, respectively (Figure 2). The pooled ICH incidence for 64 time periods was 26.47 per 100,000 persons per year (95% CI: 21.84, 32.07), with significant heterogeneity (I2 = 100%, p = 0). The pooled incidence in HIC was 25.90 per 100,000 person-years (95% CI: 22.63, 29.63, I2 = 99%, p = 0), which is marginally lower than that of the upper-middle income countries 28.45 per 100,000 person-years (95% CI: 15.90, 50.88, I2 = 100%, p = 0), and the lower-middle income countries has the highest incidence 31.73 per 100,000 person-years (95% CI: 18.41, 54.70, I2= 99%, p < 0.01). There are 11 time periods in the upper-middle income group but only from 4 countries (China, Malaysia, Brazil, and Iran).
Figure 2.
Incidence of intracerebral hemorrhage (ICH).
In meta-regression analysis, after adjusting for incidence data and midyear of each study period, it indicated that midyears are not significantly associated with effect size differences in all studies, and incidence of ICH has not decreased from 1996 to 2017 (annual decrease of 0.0056 per 100,000 person-years, 95% CI: −0.0318 to 0.0206, p = 0.67, tau2 = 0.30). There was either no temporal trend in incidence of HIC from 1995 to 2015 (annual decrease of 0.0060 per 100,000 person-years, 95% CI: −0.0383 to 0.0264, p = 0.7179, tau2 = 0.32).
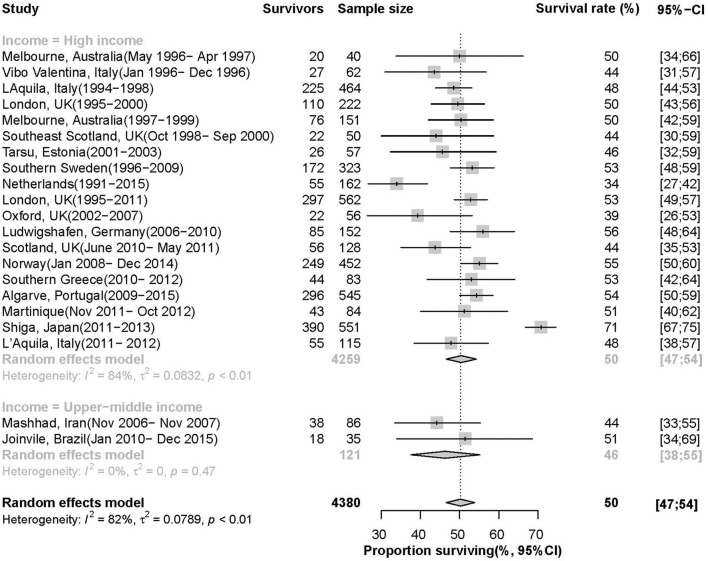
Survival After ICH
Figure 3 showed that 22 time periods reporting the 1-year survival rate of ICH patients, with 2,326 survivors and 4,380 patients in total, the pooled estimate is 50% (95 CI: 47%, 54%, I2= 82%, p < 0.01). The survival rate in HIC is 50% (95 CI: 47%, 54%, I2= 84%, p < 0.01), which is higher than 46% (95 CI: 38%, 55%, I2= 0%, p = 0.47) in upper-middle income countries. There was no temporal trend in 1-year survival from 1996 to 2015 (annual increase of 0.6% per year, 95% CI: 0.0–0.12%, p = 0.40).
Figure 3.
Survival rate of patients 1 year after ICH.
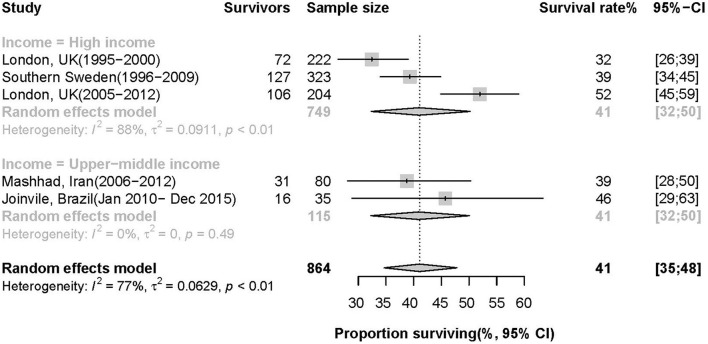
There were 352 survivors of 864 patients with ICH in studies reporting a 5-year survival rate, of which the pooled estimate was 41% (95% CI: 35%, 48%, I2= 99%, p = 0.19). The 5-year survival rate varies from 32 to 46% across 5 studies (Figure 4). The two different income groups had the same pooled 5-year survival rate but different degrees of heterogeneity as 41% (95 CI: 32%, 50%, I2= 88%, p < 0.01) and 41% (95 CI: 32%, 50%, I2= 0%, p = 0.49) in high-income and upper-middle countries, respectively. There was no temporal trend in 5-year survival from 1995 to 2015 (an annual increase of 1.1% per year, 95% CI: −0.4 to 2.7%, p = 0.11).
Figure 4.
Survival rate of patients 5 years after ICH.
Quality Assessment, Sensitivity Analysis, and Publication Bias
Approximately 90% of the eligible studies were of very high quality (details in Supplementary Material). There were no significant changes in incidence and 1-year survival meta-analyses when any study was removed. Funnel plots of three meta-analyses are slightly asymmetric, indicating modest publication bias of studies (Appendix 3–5 in Supplementary Material).
Discussion
Overall, this systematic review and meta-analysis of 80 population-based longitudinal cohort publications about the incidence and long-term survival after spontaneous primary ICH found that pooled overall incidence was 26.47 per 100,000 person-years, the 1-year survival rate was 49%, and 5-year survival rate was 41%. The incidence and survival rate have not changed over time.
The pooled overall incidence worldwide in our review was slightly higher than the systematic review and meta-analysis published 11 years ago (26.47 vs. 24.6 per 100,000 person-years) (4). The difference may result from the completion of more population-based stroke studies in recent years in upper-middle countries with high incidences, such as China (18, 40, 42, 72, 73). Neither study found a decrease in ICH incidence worldwide over time (1980–2006 and 1995–2015). However, the Oxford Vascular Study (OXVASC; 2002–2017) found that ICH incidence declined by comparing stroke incidence with Oxfordshire Community Stroke Project (OCSP; 1981–1986) and other population-based studies in HIC (93). They only include studies that can compare incidence with themselves between the 1990s and 2010s, which can avoid other confounding factors. In the United Kingdom, the OXVASC group stated that the fall in ICH incidence under 75 years old between 1981 and 2006 might result from the prevention and management of hypertension (94). However, the South London stroke Register did not find a steady decrease every 2 years from 1995 to 2004 (95).
Intracerebral hemorrhage location may impact the incidence, some studies in high-income groups reported different incidence trend in lobar or deep ICH (69, 94, 96). The OXVASC (94) study and Dijon stroke registry (96) both found the increasing incidence of non-hypertensive lobar ICH in elderly was related to amyloid angiopathy, maybe partly due to the antithrombotic drugs use. Those trends could be different in low-income countries, in which hypertensive ICH is a rising problem because of less hypertension prevention (3).
China and Japan had the highest incidence in upper-middle income and high-income groups, respectively, (17, 40–42, 72), which may indicate that the ICH incidence was associated with ethnicity in addition to income levels. A systematic review stated that the Chinese people were more likely to have ICH than white people (pooled proportion 33 vs. 12%) (97), but a study in New Zealand found no difference between Asian migrants and white people regarding ICH incidence (36). The most effective solution to reduce the stroke incidence is primary prevention (98); the HIC that have the lowest ICH incidence may be a result from the improvement in primary vascular prevention (2). A recent paper about stroke burden in Latin American countries stated that their progress on the prevention was slower than HIC (99).
There are no available population-based studies on the long-term survival after ICH in low-income and lower-middle income countries. However, a systematic review and meta-analysis of hospital-based studies in sub-Saharan Africa (countries with poverty) stated that the overall 30-day survival of overall stroke was much lower compared with western HIC due to weak healthcare systems (100). We found improved long-term survival compared with the systematic review published 7 years ago (1-year survival: 49 vs. 46%, 5-year survival: 41 vs. 29%), they also reported no temporal trend in survival (5). The better long-term survival maybe due to the better management of the independent risk factor (diabetes mellitus and atrial fibrillation) and the more appropriate use of anticoagulation therapy at ICH onset (78, 79).
Brazil, an upper- to middle-income country, has relatively lower incidences (10.01, 10.79, 11.12, 12.68, 14.66 per 100 000 person-years) (46, 52–54, 76) and higher survival rates (1-year survival rate: 51% and 5-year survival rate: 46%) (91, 92) than some European countries in high-income group. The age distribution could be one reason explaining the better results in Brazil. The percentage of the Brazilian population older than 65 is only 6.0%, which ranging from 13.1 to 21% in other studies (20, 23, 30, 45). Older people have a higher risk of being affected by ICH. The mean age in the Joinville study in Brazil was 63 years old, which is lower than 72 and 73 in Oxfordshire and Perth (54, 101–103). Therefore, the younger age in Brazil for first-ever ICH might contribute to a better survival rate than other populations. Other reasons, such as new drugs for secondary prevention and decreased prevalence of smoking (104) in Brazil cannot be accurately measured, especially when compared with the high-income group. Further research can investigate more on better results in Brazil.
Temporal trends on the long-term survival were not found in this study. This is the reason why we analyze the incidence and survival rate of different time periods together. However, several studies report an improvement in case-fatality after ICH across years in the same region. Sipilä et al. found the case fatality of hospital-treated ICH decreased in 2004–2018 in Finland (105). Béjot et al. found that 30-day case fatality of ICH decreased from 40.9 to 29.6% between 1985 to 2011 in Dijon, France (106). A study in Ontario, Canada, reported substantial reductions in ICH case fatality from 2003 to 2017 (107). We included studies from many different regions, with markedly different healthcare systems, across different study periods in the linear regression, this may represent a relevant bias.
We did not include studies that only investigated less than 18 years old and pediatric (<18 years old) population because the population >85 years of age was a strong predictor of death after stroke (108) and stroke is rare in pediatric patients (109), which may seriously bias the pooled estimates. Studies with midyear before 1995 were excluded because of the significant decrease of stroke incidence in the HIC in the last 20 years (2, 93).
Strengths and Limitations
The main strengths of this study are three-fold. First, this review consisted of all population-based studies, ensuring the data were reliable and of high quality and allowing accurate calculation of incidence and survival rate. Second, this review is the latest update on ICH incidence and survival. Third, we performed subgroup analyses on meta-analysis, providing pooled estimates of incidence and survival rate by different country income levels. The present study has several limitations: first, there was significant heterogeneity between the studies reporting incidence of ICH, which cannot be explained by the subgroup analysis on income level or meta-regression on study midyear. The long-range of the study period, the various sample sizes, different regions, age, and ethnicities may contribute to heterogeneity. Two systematic reviews and meta-analyses on stroke and ICH conducted about 10 years ago had significant unexplained heterogeneity across eligible studies (2, 4). Second, our study was based on aggregated data. We have no access to individual data in eligible publications, so we cannot do standardized analysis, age, or sex-based analysis to further investigate the potential sources of heterogeneity. Third, although we have performed a subgroup analysis on income groups, many more studies were from high-income groups than other groups. The imbalance in the distribution of countries by income group may result in less representation of studies from lower-middle income regions. Fourth, ethnicity could be a factor that can explain the difference in the incidence and survival rate. We did not report in different ethnic groups because many countries are multi-ethnic, so that it is ambiguous to classify a country into ethnicity groups. Our future studies could focus on ethnicity differences in ICH incidence and survival. Despite these limitations, this meta-analysis offered a comprehensive, comparable, robust, and latest overview of ICH incidence and long-term survival with population-based studies.
Conclusion
The pooled ICH incidence was highest in lower-middle-income countries and lowest in HIC. Incidence has not decreased with time. About a half of patients with ICH survived 1 year, and about two-fifths survived 5 years. There were no time trends on survival. Good-quality incidence and survival data can help us improve the prevention of ICH in primary care and its functional outcome and survival in secondary care. More multi-center population-based stroke registers with long follow-up years or surveillance design are needed. They should be continued, especially in low-income and lower-middle-income regions, to provide reliable data on stroke epidemiology. Future studies on ICH should also clarify the case ascertainment based on the brain imaging technique.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
XL, CW, and YW: conceptualization. XL and LZ: formal analysis. CW and YW: supervision and writing-review and editing. XL: writing-original draft. All authors contributed to the article and approved the submitted version.
Funding
This study/project is funded by the National Institute for Health Research (NIHR) [Program Grants for Applied Research (NIHR202339)].
Author Disclaimer
The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors acknowledge support from the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) South London at King's College Hospital (KCH) NHS Foundation Trust, and the NIHR Biomedical Research Centre (BRC), Guy's and St Thomas' NHS Foundation Trust and King's College London, UK, and the Program of the China Scholarships Council (CSC 201808320212).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.819737/full#supplementary-material
References
- 1.Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. (2009) 373:1632–44. 10.1016/S0140-6736(09)60371-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. (2009) 8:355–69. 10.1016/S1474-4422(09)70025-0 [DOI] [PubMed] [Google Scholar]
- 3.Krishnamurthi RV, Moran AE, Forouzanfar MH, Bennett DA, Mensah GA, Lawes CM, et al. The global burden of hemorrhagic stroke: a summary of findings from the Gbd 2010 study. Glob Heart. (2014) 9:101–6. 10.1016/j.gheart.2014.01.003 [DOI] [PubMed] [Google Scholar]
- 4.Van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. (2010) 9:167–76. 10.1016/S1474-4422(09)70340-0 [DOI] [PubMed] [Google Scholar]
- 5.Poon MTC, Fonville AF, Salman RA-S. Long-term prognosis after intracerebral haemorrhage: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. (2014) 85:660–7. 10.1136/jnnp-2013-306476 [DOI] [PubMed] [Google Scholar]
- 6.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. (2010) 8:336–41. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 7.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. (2000) 283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 8.Group TWB,. World Bank Country Lending Groups. The World Bank (2021). Available online at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed March 21, 2021).
- 9.Wells GA, Shea B, O'Connell Da, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (Nos) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Oxford: Oxford University Press; (2000). [Google Scholar]
- 10.Wolfe CD, Giroud M, Kolominsky-Rabas P, Dundas R, Lemesle M, Heuschmann P, et al. Variations in stroke incidence and survival in 3 areas of Europe. European Registries of Stroke (Eros) Collaboration. Stroke. (2000) 31:2074–9. 10.1161/01.STR.31.9.2074 [DOI] [PubMed] [Google Scholar]
- 11.Thrift AG, Dewey HM, Macdonell RA, McNeil JJ, Donnan GA. Incidence of the major stroke subtypes: initial findings from the North East Melbourne Stroke Incidence Study (Nemesis). Stroke. (2001) 32:1732–8. 10.1161/01.STR.32.8.1732 [DOI] [PubMed] [Google Scholar]
- 12.Di Carlo A, Inzitari D, Galati F, Baldereschi M, Giunta V, Grillo G, et al. A Prospective community-based study of stroke in Southern Italy: the Vibo Valentia Incidence of Stroke Study (Viss). Methodology, incidence and case fatality at 28 days, 3 and 12 months. Cerebrovasc Dis. (2003) 16:410–7. 10.1159/000072565 [DOI] [PubMed] [Google Scholar]
- 13.Sacco S, Marini C, Toni D, Olivieri L, Carolei A. Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke. (2009) 40:394–9. 10.1161/STROKEAHA.108.523209 [DOI] [PubMed] [Google Scholar]
- 14.Marini C, Totaro R, De Santis F, Ciancarelli I, Baldassarre M, Carolei A. Stroke in young adults in the community-based l'aquila registry: incidence and prognosis. Stroke. (2001) 32:52–6. 10.1161/01.STR.32.1.52 [DOI] [PubMed] [Google Scholar]
- 15.D'Alessandro G, Bottacchi E, Di Giovanni M, Martinazzo C, Sironi L, Lia C, et al. Temporal trends of stroke in Valle D'aosta, Italy. Incidence and 30-day fatality rates. Neurol Sci. (2000) 21:13–8. 10.1007/s100720070113 [DOI] [PubMed] [Google Scholar]
- 16.Kita Y, Turin TC, Ichikawa M, Sugihara H, Morita Y, Tomioka N, et al. Trend of stroke incidence in a Japanese Population: Takashima stroke registry, 1990-2001. International Journal of Stroke. (2009) 4:241–9. 10.1111/j.1747-4949.2009.00293.x [DOI] [PubMed] [Google Scholar]
- 17.Ishikawa S, Kayaba K, Gotoh T, Nago N, Nakamura Y, Tsutsumi A, et al. Incidence of total stroke, stroke subtypes, and myocardial infarction in the Japanese Population: the JMS cohort study. J Epidemiol. (2008) 18:144–50. 10.2188/jea.JE2007438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang LF, Yang J, Hong Z, Yuan GG, Zhou BF, Zhao LC, et al. Proportion of Different subtypes of stroke in China. Stroke. (2003) 34:2091–6. 10.1161/01.STR.0000087149.42294.8C [DOI] [PubMed] [Google Scholar]
- 19.Smadja D, Cabre P, May F, Fanon JL, Rene-Corail P, Riocreux C, et al. Ermancia: epidemiology of stroke in Martinique, French West Indies: Part I: methodology, incidence, and 30-day case fatality rate. Stroke. (2001) 32:2741–7. 10.1161/hs1201.099385 [DOI] [PubMed] [Google Scholar]
- 20.Thrift AG, Dewey HM, Sturm JW, Srikanth VK, Gilligan AK, Gall SL, et al. Incidence of stroke subtypes in the North East Melbourne Stroke incidence study (Nemesis): differences between men and women. Neuroepidemiology. (2009) 32:11–8. 10.1159/000170086 [DOI] [PubMed] [Google Scholar]
- 21.Correia M, Silva MR, Matos I, Magalhaes R, Lopes JC, Ferro JM, et al. Prospective community-based study of stroke in Northern Portugal: incidence and case fatality in rural and urban populations. Stroke. (2004) 35:2048–53. 10.1161/01.STR.0000137606.34301.13 [DOI] [PubMed] [Google Scholar]
- 22.Appelros P, Nydevik I, Seiger A, Terent A. High incidence rates of stroke in Orebro, Sweden: further support for regional incidence differences within Scandinavia. Cerebrovasc Dis. (2002) 14:161–8. 10.1159/000065680 [DOI] [PubMed] [Google Scholar]
- 23.Syme PD, Byrne AW, Chen R, Devenny R, Forbes JF. Community-based stroke incidence in a scottish population: the Scottish Borders Stroke Study. Stroke. (2005) 36:1837–43. 10.1161/01.STR.0000177873.82478.1c [DOI] [PubMed] [Google Scholar]
- 24.Suzuki K, Izumi M. The incidence of hemorrhagic stroke in Japan is twice compared with Western Countries: the Akita Stroke registry. Neurol Sci. (2015) 36:155–60. 10.1007/s10072-014-1917-z [DOI] [PubMed] [Google Scholar]
- 25.Kolominsky-Rabas PL, Wiedmann S, Weingartner M, Liman TG, Endres M, Schwab S, et al. Time trends in incidence of pathological and etiological stroke subtypes during 16 years: the Erlangen stroke project. Neuroepidemiology. (2015) 44:24–9. 10.1159/000371353 [DOI] [PubMed] [Google Scholar]
- 26.Correia M, Magalhaes R, Felgueiras R, Quintas C, Guimaraes L, Silva MC. Changes in stroke incidence, outcome, and associated factors in Porto between 1998 and 2011. Int J Stroke. (2017) 12:169–79. 10.1177/1747493016669846 [DOI] [PubMed] [Google Scholar]
- 27.Islam MS, Anderson CS, Hankey GJ, Hardie K, Carter K, Broadhurst R, et al. Trends in incidence and outcome of stroke in Perth, Western Australia during 1989 to 2001: the Perth Community Stroke Study. Stroke. (2008) 39:776–82. 10.1161/STROKEAHA.107.493643 [DOI] [PubMed] [Google Scholar]
- 28.Heuschmann PU, Grieve AP, Toschke AM, Rudd AG, Wolfe CD. Ethnic group disparities in 10-year trends in stroke incidence and vascular risk factors: the South London Stroke Register (Slsr). Stroke. (2008) 39:2204–10. 10.1161/STROKEAHA.107.507285 [DOI] [PubMed] [Google Scholar]
- 29.Smeeton NC, Heuschmann PU, Rudd AG, McEvoy AW, Kitchen ND, Sarker SJ, et al. Incidence of hemorrhagic stroke in Black Caribbean, Black African, and White Populations: The South London Stroke Register, 1995–2004. Stroke. (2007) 38:3133–8. 10.1161/STROKEAHA.107.487082 [DOI] [PubMed] [Google Scholar]
- 30.Giroud M, Delpont B, Daubail B, Blanc C, Durier J, Giroud M, et al. Temporal trends in sex differences with regard to stroke incidence: the Dijon Stroke registry (1987–2012). Stroke. (2017) 48:846–9. 10.1161/STROKEAHA.116.015913 [DOI] [PubMed] [Google Scholar]
- 31.Vaartjes I, Reitsma JB, de Bruin A, Berger-van Sijl M, Bos MJ, Breteler MM, et al. Nationwide incidence of first stroke and Tia in the Netherlands. European Journal of Neurology. (2008) 15:1315–23. 10.1111/j.1468-1331.2008.02309.x [DOI] [PubMed] [Google Scholar]
- 32.Hallstrom B, Jonsson AC, Nerbrand C, Petersen B, Norrving B, Lindgren A. Lund stroke register: hospitalization pattern and yield of different screening methods for first-ever stroke. Acta Neurol Scand. (2007) 115:49–54. 10.1111/j.1600-0404.2006.00738.x [DOI] [PubMed] [Google Scholar]
- 33.Hallstrom B, Jonsson AC, Nerbrand C, Norrving B, Lindgren A. Stroke incidence and survival in the beginning of the 21st century in Southern Sweden: comparisons with the late 20th century and projections into the future. Stroke. (2008) 39:10–5. 10.1161/STROKEAHA.107.491779 [DOI] [PubMed] [Google Scholar]
- 34.Lavados PM, Sacks C, Prina L, Escobar A, Tossi C, Araya F, et al. Incidence, 30-day case-fatality rate, and prognosis of stroke in Iquique, Chile: a 2-year community-based prospective study (Piscis Project). Lancet. (2005) 365:2206–15. 10.1016/S0140-6736(05)66779-7 [DOI] [PubMed] [Google Scholar]
- 35.Lavados PM, Sacks C, Prina L, Escobar A, Tossi C, Araya F, et al. Incidence of lobar and non-lobar spontaneous intracerebral haemorrhage in a predominantly hispanic-mestizo population–the piscis stroke project: a community-based prospective study in Iquique, Chile. Neuroepidemiology. (2010) 34:214–21. 10.1159/000289353 [DOI] [PubMed] [Google Scholar]
- 36.Feigin V, Carter K, Hackett M, Barber PA, McNaughton H, Dyall L, et al. Ethnic disparities in incidence of stroke subtypes: Auckland regional community stroke study, 2002–2003. The Lancet Neurology. (2006) 5:130–9. 10.1016/S1474-4422(05)70325-2 [DOI] [PubMed] [Google Scholar]
- 37.Corbin DO, Poddar V, Hennis A, Gaskin A, Rambarat C, Wilks R, et al. Incidence and case fatality rates of first-ever stroke in a Black Caribbean population: the barbados register of strokes. Stroke. (2004) 35:1254–8. 10.1161/01.STR.0000127371.24658.df [DOI] [PubMed] [Google Scholar]
- 38.Manobianca G, Zoccolella S, Petruzzellis A, Miccoli A, Logroscino G. Low incidence of stroke in Southern Italy: a population-based study. Stroke. (2008) 39:2923–8. 10.1161/STROKEAHA.108.519421 [DOI] [PubMed] [Google Scholar]
- 39.Vibo R, Korv J, Roose M. The Third Stroke registry in Tartu, Estonia, from 2001 to 2003. Acta Neurol Scand. (2007) 116:31–6. 10.1111/j.1600-0404.2006.00773.x [DOI] [PubMed] [Google Scholar]
- 40.Li B, Lou Y, Gu H, Long X, Wang T, Wei J, et al. Trends in incidence of stroke and transition of stroke subtypes in rural Tianjin, China: a population-based study from 1992 to 2012. PLoS ONE. (2015) 10:e0139461. 10.1371/journal.pone.0139461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang J, Bai L, Shi M, Yang L, An Z, Li B, et al. Trends in age of first-ever stroke following increased incidence and life expectancy in a low-income Chinese population. Stroke. (2016) 47:929–35. 10.1161/STROKEAHA.115.012466 [DOI] [PubMed] [Google Scholar]
- 42.Wang J, Ning X, Yang L, Tu J, Gu H, Zhan C, et al. Sex differences in trends of incidence and mortality of first-ever stroke in rural Tianjin, China, from 1992 to 2012. Stroke. (2014) 45:1626–31. 10.1161/STROKEAHA.113.003899 [DOI] [PubMed] [Google Scholar]
- 43.Manobianca G, Zoccolella S, Petruzzellis A, Miccoli A, Logroscino G. The incidence of major stroke subtypes in Southern Italy: a population-based study. Eur J Neurol. (2010) 17:1148–55. 10.1111/j.1468-1331.2010.02983.x [DOI] [PubMed] [Google Scholar]
- 44.Dalal PM, Malik S, Bhattacharjee M, Trivedi ND, Vairale J, Bhat P, et al. Population-based stroke survey in Mumbai, India: incidence and 28-day case fatality. Neuroepidemiology. (2008) 31:254–61. 10.1159/000165364 [DOI] [PubMed] [Google Scholar]
- 45.Rothwell PM, Coull AJ, Giles MF, Howard SC, Silver LE, Bull LM, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, Uk from 1981 to 2004 (Oxford Vascular Study). Lancet. (2004) 363:1925–33. 10.1016/S0140-6736(04)16405-2 [DOI] [PubMed] [Google Scholar]
- 46.Minelli C, Fen LF, Minelli DP. Stroke incidence, prognosis, 30-Day, and 1-year case fatality rates in Matao, Brazil: a population-based prospective study. Stroke. (2007) 38:2906–11. 10.1161/STROKEAHA.107.484139 [DOI] [PubMed] [Google Scholar]
- 47.Carlsson M, Wilsgaard T, Johnsen SH, Vangen-Lonne AM, Lochen ML, Njolstad I, et al. Temporal trends in incidence and case fatality of intracerebral hemorrhage: the tromso study 1995–2012. Cerebrovasc Dis Extra. (2016) 6:40–9. 10.1159/000447719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, et al. Stroke incidence is decreasing in whites but not in blacks: a population-based estimate of temporal trends in stroke incidence from the greater Cincinnati/Northern Kentucky Stroke Study. Stroke. (2010) 41:1326–31. 10.1161/STROKEAHA.109.575043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, et al. Age at stroke: temporal trends in stroke incidence in a large, biracial population. Neurology. (2012) 79:1781–7. 10.1212/WNL.0b013e318270401d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Corso G, Bottacchi E, Giardini G, De la Pierre F, Meloni T, Pesenti Campagnoni M, et al. Community-based study of stroke incidence in the Valley of Aosta, Italy. care-cerebrovascular aosta registry: years 2004-2005. Neuroepidemiology. (2009) 32:186–95. 10.1159/000195688 [DOI] [PubMed] [Google Scholar]
- 51.Groppo E, De Gennaro R, Granieri G, Fazio P, Cesnik E, Granieri E, et al. Incidence and prognosis of stroke in young adults: a population-based study in Ferrara, Italy. Neurol Sci. (2012) 33:53–8. 10.1007/s10072-011-0654-9 [DOI] [PubMed] [Google Scholar]
- 52.Cabral NL, Freire AT, Conforto AB, Dos Santos N, Reis FI, Nagel V, et al. Increase of stroke incidence in young adults in a middle-income country: A 10-year population-based study. Stroke. (2017) 48:2925–30. 10.1161/STROKEAHA.117.018531 [DOI] [PubMed] [Google Scholar]
- 53.Cabral NL, Goncalves AR, Longo AL, Moro CH, Costa G, Amaral CH, et al. Incidence of stroke subtypes, prognosis and prevalence of risk factors in Joinville, Brazil: a 2 year community based study. J Neurol Neurosurg Psychiatry. (2009) 80:755–61. 10.1136/jnnp.2009.172098 [DOI] [PubMed] [Google Scholar]
- 54.Cabral NL, Goncalves AR, Longo AL, Moro CH, Costa G, Amaral CH, et al. Trends in stroke incidence, mortality and case fatality rates in Joinville, Brazil: 1995–2006. J Neurol Neurosurg Psychiatry. (2009) 80:749–54. 10.1136/jnnp.2008.164475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kelly PJ, Crispino G, Sheehan O, Kelly L, Marnane M, Merwick A, et al. Incidence, event rates, and early outcome of stroke in Dublin, Ireland: The North Dublin Population stroke study. Stroke. (2012) 43:2042–7. 10.1161/STROKEAHA.111.645721 [DOI] [PubMed] [Google Scholar]
- 56.Amiri A, Kapral MK, Thrift AG, Sposato LA, Saber H, Behrouz R, et al. The incidence and characteristics of stroke in urban-dwelling Iranian women. J Stroke Cerebrovasc Dis. (2018) 27:547–54. 10.1016/j.jstrokecerebrovasdis.2017.09.050 [DOI] [PubMed] [Google Scholar]
- 57.Azarpazhooh MR, Etemadi MM, Donnan GA, Mokhber N, Majdi MR, Ghayour-Mobarhan M, et al. Excessive incidence of stroke in Iran: evidence from the Mashhad Stroke Incidence Study (Msis), a population-based study of Stroke in the Middle East. Stroke. (2010) 41:e3–e10. 10.1161/STROKEAHA.109.559708 [DOI] [PubMed] [Google Scholar]
- 58.Boden-Albala B, Allen J, Roberts ET, Bulkow L, Trimble B. Ascertainment of Alaska Native Stroke Incidence, 2005–2009: Lessons for assessing the global burden of stroke. J Stroke Cerebrovasc Dis. (2017) 26:2019–26. 10.1016/j.jstrokecerebrovasdis.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 59.Palm F, Henschke N, Wolf J, Zimmer K, Safer A, Schroder RJ, et al. Intracerebral haemorrhage in a population-based stroke registry (Lusst): incidence, aetiology, functional outcome and mortality. J Neurol. (2013) 260:2541–50. 10.1007/s00415-013-7013-0 [DOI] [PubMed] [Google Scholar]
- 60.Janes F, Gigli GL, D'Anna L, Cancelli I, Perelli A, Canal G, et al. Stroke incidence and 30-day and six-month case fatality rates in Udine, Italy: a population-based prospective study. Int J Stroke. (2013) 8 Suppl A100:100-5. 10.1111/ijs.12000 [DOI] [PubMed] [Google Scholar]
- 61.Pikija S, Cvetko D, Malojcic B, Trkanjec Z, Pavlicek I, Lukic A, et al. A population-based prospective 24-month study of stroke: incidence and 30-day case-fatality rates of first-ever strokes in Croatia. Neuroepidemiology. (2012) 38:164–71. 10.1159/000336114 [DOI] [PubMed] [Google Scholar]
- 62.Gattellari M, Goumas C, Jalaludin B, Worthington JM. Population-based stroke surveillance using big data: State-wide epidemiological trends in admissions and mortality in New South Wales, Australia. Neurol Res. (2020) 42:587–96. 10.1080/01616412.2020.1766860 [DOI] [PubMed] [Google Scholar]
- 63.Neelamegam M, Looi I, Cheah WK, Narayanan P, Hamid AM, Ong LM. Stroke incidence in the South West District of the Penang Island, Malaysia: Pearls: Penang Acute Stroke Research Longitudinal Study. Preventive Med. (2013) 57 Suppl:S77–9. 10.1016/j.ypmed.2012.12.022 [DOI] [PubMed] [Google Scholar]
- 64.Stranjalis G, Kalamatianos T, Gatzonis S, Loufardaki M, Tzavara C, Sakas DE. The incidence of the first-ever stroke in a Mediterranean Island Population: the Isle of Lesvos Stroke study. Neuroepidemiology. (2014) 43:206–12. 10.1159/000365849 [DOI] [PubMed] [Google Scholar]
- 65.Tsivgoulis G, Patousi A, Pikilidou M, Birbilis T, Katsanos AH, Mantatzis M, et al. Stroke incidence and outcomes in Northeastern Greece: the Evros Stroke registry. Stroke. (2018) 49:288–95. 10.1161/STROKEAHA.117.019524 [DOI] [PubMed] [Google Scholar]
- 66.Takashima N, Arima H, Kita Y, Fujii T, Miyamatsu N, Komori M, et al. Incidence, management and short-term outcome of stroke in a general population of 14 million Japanese - Shiga Stroke Registry. Circul J. (2017) 81:1636–46. 10.1253/circj.CJ-17-0177 [DOI] [PubMed] [Google Scholar]
- 67.Samarasekera N, Fonville A, Lerpiniere C, Farrall AJ, Wardlaw JM, White PM, et al. Influence of intracerebral hemorrhage location on incidence, characteristics, and outcome: population-based study. Stroke. (2015) 46:361–8. 10.1161/STROKEAHA.114.007953 [DOI] [PubMed] [Google Scholar]
- 68.Okon M, Adebobola NI, Julius S, Adebimpe O, Taiwo AO, Akinyemi A, et al. Stroke incidence and case fatality rate in an Urban Population. J Stroke Cerebrovasc Dis. (2015) 24:771–7. 10.1016/j.jstrokecerebrovasdis.2014.11.004 [DOI] [PubMed] [Google Scholar]
- 69.Sacco S, Ornello R, Degan D, Tiseo C, Pistoia F, Carolei A. Declining incidence of intracerebral hemorrhage over two decades in a population-based study. Eur J Neurol. (2016) 23:1627–34. 10.1111/ene.13099 [DOI] [PubMed] [Google Scholar]
- 70.Pandian JD, Singh G, Kaur P, Bansal R, Paul BS, Singla M, et al. Incidence, short-term outcome, and spatial distribution of stroke patients in Ludhiana, India. Neurology. (2016) 86:425–33. 10.1212/WNL.0000000000002335 [DOI] [PubMed] [Google Scholar]
- 71.Olindo S, Chausson N, Mejdoubi M, Jeannin S, Rosillette K, Saint-Vil M, et al. Trends in incidence and early outcomes in a Black Afro-Caribbean population from 1999 to 2012: Etude Realisee En Martinique Et Centree Sur L'incidence Des Accidents Vasculaires Cerebraux Ii Study. Stroke. (2014) 45:3367–73. 10.1161/STROKEAHA.114.005930 [DOI] [PubMed] [Google Scholar]
- 72.Chen Y, Wright N, Guo Y, Turnbull I, Kartsonaki C, Yang L, et al. Mortality and recurrent vascular events after first incident stroke: a 9-year community-based study of 05 Million Chinese adults Lancet Glob Health (2020) 8:e580–e90. 10.1016/S2214-109X(20)30069-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 Adults. Circulation. (2017) 135:759–71. 10.1161/CIRCULATIONAHA.116.025250 [DOI] [PubMed] [Google Scholar]
- 74.Saliba W, Barnett-Griness O, Gronich N, Molad J, Naftali J, Rennert G, et al. Association of diabetes and glycated hemoglobin with the risk of intracerebral hemorrhage: a population-based cohort study. Diab Care. (2019) 42:682–8. 10.2337/dc18-2472 [DOI] [PubMed] [Google Scholar]
- 75.Nzwalo H, Nogueira J, Felix C, Guilherme P, Baptista A, Figueiredo T, et al. Incidence and case-fatality from spontaneous intracerebral hemorrhage in a Southern Region of Portugal. J Neurol Sci. (2017) 380:74–8. 10.1016/j.jns.2017.07.006 [DOI] [PubMed] [Google Scholar]
- 76.Minelli C, Cabral NL, Ujikawa LT, Neto FAB, Chiozzini EML, Dos Reis GC, et al. Trends in the incidence and mortality of stroke in Matão, Brazil: the Matão preventing Stroke (Maps) study. Neuroepidemiology. (2020) 54:75–82. 10.1159/000503005 [DOI] [PubMed] [Google Scholar]
- 77.Appelros P. Secular trends of stroke epidemiology in Orebro, Sweden, 2017 compared to the trends in 1999: a population-based study. Cerebrovasc Dis. (2019) 48:149–56. 10.1159/000504082. 10.1159/000504082 [DOI] [PubMed] [Google Scholar]
- 78.Hillen T, Coshall C, Tilling K, Rudd AG, McGovern R, Wolfe CD, et al. Cause of stroke recurrence is multifactorial: patterns, risk factors, and outcomes of stroke recurrence in the South London stroke register. Stroke. (2003) 34:1457–63. 10.1161/01.STR.0000072985.24967.7F [DOI] [PubMed] [Google Scholar]
- 79.Hansen BM, Nilsson OG, Anderson H, Norrving B, Saveland H, Lindgren A. Long term (13 years) prognosis after primary intracerebral haemorrhage: a prospective population based study of long term mortality, prognostic factors and causes of death. J Neurol Neurosurg Psychiatry. (2013) 84:1150–5. 10.1136/jnnp-2013-305200 [DOI] [PubMed] [Google Scholar]
- 80.Waziry R, Heshmatollah A, Bos D, Chibnik LB, Ikram MA, Hofman A, et al. Time trends in survival following first hemorrhagic or ischemic stroke between 1991 and 2015 in the Rotterdam study. Stroke. (2020) 51:STROKEAHA119027198. 10.1161/STROKEAHA.119.027198 [DOI] [PubMed] [Google Scholar]
- 81.McCormick J, Chen R. Impact of socioeconomic deprivation on mortality in people with haemorrhagic stroke: a population-based cohort study. Postgrad Med J. (2016) 92:501–5. 10.1136/postgradmedj-2015-133663 [DOI] [PubMed] [Google Scholar]
- 82.van Beijnum J, Lovelock CE, Cordonnier C, Rothwell PM, Klijn CJ, Al-Shahi Salman R, et al. Outcome after spontaneous and arteriovenous malformation-related intracerebral haemorrhage: population-based studies. Brain. (2009) 132(Pt 2):537–43. 10.1093/brain/awn318 [DOI] [PubMed] [Google Scholar]
- 83.Shoeibi A, Salehi M, Thrift AG, Kapral MK, Farzadfard MT, Azarpazhooh A, et al. One-year case fatality rate following stroke in the mashhad stroke incidence study: a population-based study of stroke in Iran. Int J Stroke. (2015) 10:96–102. 10.1111/ijs.12611 [DOI] [PubMed] [Google Scholar]
- 84.Desikan A, Crichton S, Hoang U, Barratt B, Beevers SD, Kelly FJ, et al. Effect of exhaust- and nonexhaust-related components of particulate matter on long-term survival after stroke. Stroke. (2016) 47:2916–22. 10.1161/STROKEAHA.116.014242 [DOI] [PubMed] [Google Scholar]
- 85.Farzadfard MT, Thrift AG, Amiri A, Kapral MK, Hashemi P, Sposato LA, et al. Five-year case fatality following first-ever stroke in the Mashhad Stroke incidence study: a population-based study of stroke in the Middle East. J Stroke Cerebrovasc Dis. (2018) 27:1085–9. 10.1016/j.jstrokecerebrovasdis.2017.11.018 [DOI] [PubMed] [Google Scholar]
- 86.Oie LR, Madsbu MA, Solheim O, Jakola AS, Giannadakis C, Vorhaug A, et al. Functional outcome and survival following spontaneous intracerebral hemorrhage: a retrospective population-based study. Brain Behav. (2018) 8:e01113. 10.1002/brb3.1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tsivgoulis G, Katsanos AH, Patousi A, Pikilidou M, Birbilis T, Mantatzis M, et al. Stroke recurrence and mortality in Northeastern Greece: the Evros Stroke Registry. J Neurol. (2018) 265:2379–87. 10.1007/s00415-018-9005-6 [DOI] [PubMed] [Google Scholar]
- 88.Nzwalo H, Felix C, Nogueira J, Guilherme P, Ferreira F, Salero T, et al. Predictors of long-term survival after spontaneous intracerebral hemorrhage in southern Portugal: a retrospective study of a community representative population. J Neurol Sci. (2018) 394:122–6. 10.1016/j.jns.2018.09.019 [DOI] [PubMed] [Google Scholar]
- 89.Olindo S, Saint-Vil M, Jeannin S, Signate A, Edimonana-Kaptue M, Cabre P, et al. One-year disability, death and recurrence after first-ever stroke in a black Afro-Caribbean population. Int J Stroke. (2017) 12:844–50. 10.1177/1747493016685720 [DOI] [PubMed] [Google Scholar]
- 90.Takashima N, Arima H, Kita Y, Fujii T, Miyamatsu N, Komori M, et al. Two-year survival after first-ever stroke in a general population of 14 Million Japanese—Shiga Stroke Registry. Circul J. (2018) 82:2549–56. 10.1253/circj.CJ-18-0346 [DOI] [PubMed] [Google Scholar]
- 91.Cabral NL, Nagel V, Conforto AB, Amaral CH, Venancio VG, Safanelli J, et al. Five-year survival, disability, and recurrence after first-ever stroke in a middle-income country: a population-based study in Joinvile, Brazil. Int J Stroke. (2018) 13:725–33. 10.1177/1747493018763906 [DOI] [PubMed] [Google Scholar]
- 92.Cabral NL, Muller M, Franco SC, Longo A, Moro C, Nagel V, et al. Three-year survival and recurrence after first-ever stroke: the Joinville stroke registry. BMC Neurol. (2015) 15:70. 10.1186/s12883-015-0317-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li L, Scott CA, Rothwell PM, Study OV. Trends in stroke incidence in high-income countries in the 21st century: population-based study and systematic review. Stroke. (2020) 51:1372–80. 10.1161/STROKEAHA.119.028484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lovelock C, Molyneux A, Rothwell P. Change in incidence and aetiology of intracerebral haemorrhage in Oxfordshire, Uk, between 1981 and 2006: a population-based study. Lancet Neurol. (2007) 6:487–93. 10.1016/S1474-4422(07)70107-2 [DOI] [PubMed] [Google Scholar]
- 95.Bhatnagar P, Scarborough P, Smeeton NC, Allender S. The incidence of all stroke and stroke subtype in the United Kingdom, 1985 to 2008: a systematic review. BMC Public Health. (2010) 10:1–11. 10.1186/1471-2458-10-539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Béjot Y, Cordonnier C, Durier J, Aboa-Eboulé C, Rouaud O, Giroud M. Intracerebral haemorrhage profiles are changing: results from the Dijon population-based study. Brain. (2013) 136:658–64. 10.1093/brain/aws349 [DOI] [PubMed] [Google Scholar]
- 97.Tsai C-F, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology. (2013) 81:264–72. 10.1212/WNL.0b013e31829bfde3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2011) 42:517–84. 10.1161/STR.0b013e3181fcb238 [DOI] [PubMed] [Google Scholar]
- 99.Martins SCO, Sacks C, Hacke W, Brainin M, de Assis Figueiredo F, Pontes-Neto OM, et al. Priorities to reduce the burden of stroke in Latin American Countries. Lancet Neurol. (2019) 18:674–83. 10.1016/S1474-4422(19)30068-7 [DOI] [PubMed] [Google Scholar]
- 100.Adoukonou T, Kossi O, Fotso Mefo P, Agbetou M, Magne J, Gbaguidi G, et al. Stroke case fatality in sub-Saharan africa: systematic review and meta-analysis. Int J Stroke. (2021) 2021:1747493021990945. 10.1177/1747493021990945 [DOI] [PubMed] [Google Scholar]
- 101.Burn J, Dennis M, Bamford J, Sandercock P, Wade D, Warlow C. Long-term risk of recurrent stroke after a first-ever stroke. The Oxfordshire Community Stroke Project. Stroke. (1994) 25:333–7. 10.1161/01.STR.25.2.333 [DOI] [PubMed] [Google Scholar]
- 102.Hankey GJ, Jamrozik K, Broadhurst RJ, Forbes S, Burvill PW, Anderson CS, et al. Long-term risk of first recurrent stroke in the Perth Community Stroke Study. Stroke. (1998) 29:2491–500. 10.1161/01.STR.29.12.2491 [DOI] [PubMed] [Google Scholar]
- 103.Hardie K, Jamrozik K, Hankey GJ, Broadhurst RJ, Anderson C. Trends in five-year survival and risk of recurrent stroke after first-ever stroke in the Perth Community Stroke Study. Cerebrovasc Dis. (2005) 19:179–85. 10.1159/000083253 [DOI] [PubMed] [Google Scholar]
- 104.Monteiro CA, Cavalcante TM, Moura EC, Claro RM, Szwarcwald CL. Population-based evidence of a strong decline in the prevalence of smokers in Brazil (1989-2003). Bull World Health Organ. (2007) 85:527–34. 10.2471/BLT.06.039073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sipilä JO, Ruuskanen JO, Rautava P, Kytö V. Case Fatality of hospital-treated intracerebral hemorrhage in Finland—a Nationwide Population-Based Registry Study. J Neurol Sci. (2021) 425:117446. 10.1016/j.jns.2021.117446 [DOI] [PubMed] [Google Scholar]
- 106.Béjot Y, Grelat M, Delpont B, Durier J, Rouaud O, Osseby G-V, et al. Temporal trends in early case-fatality rates in patients with intracerebral hemorrhage. Neurology. (2017) 88:985–90. 10.1212/WNL.0000000000003681 [DOI] [PubMed] [Google Scholar]
- 107.Joundi RA, Smith EE, Amy Y, Rashid M, Fang J, Kapral MK. Temporal trends in case fatality, discharge destination, and admission to long-term care after acute stroke. Neurology. (2021) 96:e2037–e47. 10.1212/WNL.0000000000011791 [DOI] [PubMed] [Google Scholar]
- 108.Kammersgaard LP, Jørgensen H, Reith J, Nakayama H, Pedersen P, Olsen T. Short-and long-term prognosis for very old stroke patients. The Copenhagen Stroke Study. Age Ageing. (2004) 33:149–54. 10.1093/ageing/afh052 [DOI] [PubMed] [Google Scholar]
- 109.Tsze DS, Valente JH. Pediatric stroke: a review. Emerg Med Int. (2011) 2011:734506. 10.1155/2011/734506 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.