Abstract
Objective:
The effectiveness of filtering facepiece respirators such as N95 respirators is heavily dependent on the fit. However, there have been limited efforts to discover the size of the gaps in the seal required to compromise filtering facepiece respirator performance, with prior studies estimating this size based on in vitro models. In this study, we measure the size of leak necessary to compromise the fit of N95 respirators.
Methods:
Two methods were used to create a gap of specific dimensions. A set of 3D-printed resin spacers and hollow steel rods were used to generate gaps in N95 respirators while worn on 2 participants. Occupational Safety and Health Administration (OSHA) quantitative fit testing methods were used to quantify mask performance with gaps between 0.4 and 2.9-mm diameters.
Results:
Gap size was regressed against fit factor, showing that overall, the minimum gap size to compromise N95 performance was between 1.5 mm2 and 3 mm2.
Conclusions:
These findings suggest the fit of a N95 respirator is compromised by gaps that may be difficult to visually detect. The study also adds to the body of evidence supporting the routine use of quantitative fit testing to ensure that masks are well-fitting.
Keywords: coronavirus, COVID-19, face coverings, quantitative testing, SARS-CoV-2
Introduction
Throughout the course of the coronavirus disease (COVID-19) pandemic, the fit of N95 respirators has emerged as an increasingly important and rapidly growing area of research. 1,2 Research has shown that fit is a primary factor in determining the effectiveness of respirators such as N95 masks, and that inadequate fit can negate the potential benefit of wearing respiratory protection. 1,3,4 Prior research has shown that users have poor ability to determine whether gaps, which lead to air leakage and thus compromise protection, are present. 1,5,6 As users cannot reliably detect leakage, it is of critical importance that the design and use of the mask be such as to ensure fit and protection. To better design and regulate the use of respirators, we must understand what type of gaps are necessary to compromise mask fit.
Research into the impact of respirator gaps has primarily been conducted on elastomeric half face and full face respirators. Research has investigated the impact of gap location, 4,7,8 flow rate, 9,10 and size 9 on elastomeric respirator protection. However, while widely used in industry, elastomeric respirators are rare in health care professions, where filtering facepiece respirators such as N95 and FFP3 masks are the standard. It was on these facepiece respirators that frontline workers depended on during the COVID-19 pandemic. As these respirators have a different design than elastomeric respirators, it is important to understand how gaps affect these types of respirators. In particular, it is necessary to understand what size of a gap is necessary to render a filtering facepiece respirator non-protective. N95 respirators are designed to form a tight seal around the face in order that all air that enters the breathing apparatus is filtered. 1 If the seal is inadequate and/or gaps are present around the edges of the mask, inhaled air is expected to take the path of least resistance and bypass the filtration. 11 The goal of this study is to ascertain what size of gap is necessary to compromise the fit of N95 masks when masks are worn.
In this study, we examine the impact of gaps with total surface areas ranging from 0.13 mm 2 to 6.61 mm 2 on N95 respirators, which require fit testing before they are used. It has been noted that when the fit of these masks is poor, the effectiveness can be greatly reduced, to the level of surgical masks and fabric face coverings. 1
Materials and Methods
To quantify the degree of poor fit is difficult as the size of gaps may change when the wearer moves and breathes. We used 2 methods for producing gaps: (1) resin spacers inserted between the mask and facial skin and (2) steel tubes inserted through the material of the mask close to the edge of the face. These methods are similar to those used to generate leaks in prior studies on respirator leaks. 10,12 Our first testing apparatus, a set of 2-cm long and 0.3-cm deep 3D-printed resin spacers with holes of various diameters, allowed for a realistic model of gaps in a mask. Despite careful efforts to properly place the spacer, a slight movement of the facial muscles and skin during the test could cause the spacer to be displaced. This could either result in an extra gap around 1 end of the spacer (leading to a lower fit score) or the opening in the apparatus being blocked by skin (leading to a higher fit score). To help prevent such incidents, an observer was present at all times to monitor the placement and positioning of the spacer. Our second apparatus, a set of steel tubes of various sizes, was more consistent but less accurately represented a model of a gap in the seal of a mask.
Quantitative fit testing is well recognized as the industry standard procedure for assessing the fit of face masks and was the method utilized in this study. 6 Quantitative fit testing was performed with a TSI PortaCount Pro Respirator Fit Tester model 8038+, capable of assessing masks with less than 99% filtration efficiency. The device measures particles with a minimum size of 0.02 micrometers at a sampling flow rate of 350 cm^3/min. The PortaCount compared the number of particles inside the mask with the number of particles outside the mask to generate an industry-standard fit factor. The fit factor score is the ratio of the number of particles outside the mask to the number of particles inside the mask. Scores for N95 and FFP3 masks range from a maximum score of 200, indicating a perfect fit mask, to 1. Occupational Safety and Health Administration (OSHA) safety standards require N95 respirators to score above 100 for use in work environments where N95 protection is warranted. 13
Two National Institute for Occupational Safety and Health (NIOSH) certified N95 respirators were utilized in this study, the 3M 8511 and 3M 8200. Two individuals were used during the tests to account for any irregularities in breathing pattern. Face shape was controlled for by a set of calibration tests ensuring perfect fit without gaps. The researcher assisted in the correct placement of the spacer to create a gap. An abbreviated fit test consisting of only 1 activity, normal breathing, was conducted. Other qualitative fit testing activities, such as nodding the head, were excluded due to the probability that such activity would displace the spacer.
3D-printed resin spacers fit tightly between the skin of the cheek and the mask. Each 2-cm long and 3-mm deep spacer contained a small hole of various diameters: 0.5 mm, 0.95 mm, and 1.4 mm. The design of these spacers most accurately reflected the position and location of gaps when a mask was worn. Tests were also performed by puncturing a hole in the mask near the cheek and inserting a steel tube. The steel tubes had internal diameters of 0.4 mm, 0.8 mm, 1.4 mm, and 2.9 mm and a length of 2.5 cm, which allowed for consistent placement and for monitoring by the observer.
Multiple tests were conducted with each spacer. Fit scores with the same spacer could differ due to numerous factors including breathing patterns, movement of the mask, and the apparatus hole being covered temporarily or permanently by the skin. The research observer carefully inspected the edge of the mask and area around the spacer by eye and with a USB microscope after the spacer was placed to ensure no additional gaps affected testing. If a gap was found, the spacer was removed, the mask refit, and any test data discarded.
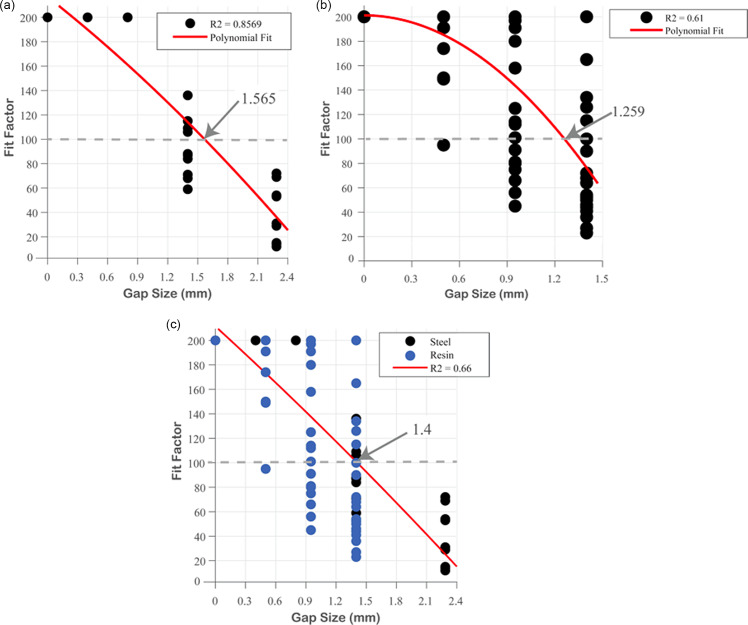
Independent statistical analysis was conducted and a linear model with a second-degree polynomial fit used. The formula for such was p1x 2 + p2x + p3, where
p1 = −63.55; p2 = −0.1425, p3 = 201.2 for resin spacers
p1 = −6.311, p2= −64.57; p3 = 216.8 for steel spacers
p1 = −2.79, p2 = −75.06, p3 = 211.5 for both.
This study was approved by the Cambridge University Engineering Department Ethics Review Committee, and written consent was obtained from all participants.
Results
When interpreting fit factor graphs, it is important to note that fit factor does not have a linear relationship to filtration efficiency (FE). The formula for fit factor causes data points, which are in actuality closely grouped, to appear widely spaced. Comparing fit factor with filtration efficiency shows that the OSHA measurements capture very small variations in data, giving a visual impression of significant variation when, in truth, there is very close grouping. For example, comparing leak data from a 1.4-mm gap had a fit factor standard deviation of 23.9 but a filtration efficiency standard deviation of only 0.0036.
Steel Tube Experiments
In the steel tube experiments, we noted that gap diameters of 0.4 mm and 0.8 mm had no effect on fit factor while a gap size of 1.4 mm appeared to decrease fit factor by a factor of 2, and a 2.9-mm gap decreased fit factor by approximately a factor of 4 (Figure 1A). A linear regression model predicted that gaps with a diameter greater than approximately 1.6 mm compromised the fit of the mask to the extent that the fit factor would fall below recommended levels.
Figure 1.
The effect of the gap sizes on the fit factor of an N95 respirator. A: The effect of the gap sizes on the fit factor of an N95 respirator using a steel tube to hold open a hole in a mask. For each size, n = 10. The coefficient of determination, R 2 was 0.86, indicating strong positive correlation. B: The effect of the gap sizes on the fit factor of an N95 respirator using a 3D-printed resin spacer to hold open a hole in a mask. The model indicates a 1.26 mm diameter gap compromises the fit of N95 respirators. For each size, n = 22. Some dots are not visible due to overlapping data points. The coefficient of determination, R 2 was 0.61, indicating moderate positive correlation. C: The effect of gap sizes with combined spacer data. OSHA required fit was found to be compromised at 1.4 mm diameters. The coefficient of determination, R 2 was 0.66, indicating moderate positive correlation.
3D-Printed Spacer Experiments
Results between the gap studies using 3D-printed spacers and metal spacers were generally concordant. Tests using 3D-printed spacers showed that the only measured gap size that had a significant effect on fit was 1.4 mm (see Figure 1B). Gap sizes of 0.5 mm and 0.95 mm produced insignificant decreases in fit. A linear regression model with polynomial fit predicted that gaps with a diameter of approximately 1.3 mm would compromise fit to the extent that the fit factor would fall below recommended levels.
Comparison Between Experiments
In both studies, we found that gap sizes smaller than 1 mm did not produce a significant decrease in fit. In both cases, gap sizes of 1.4 mm (and above) resulted in the fit being undermined to levels that would not pass OSHA requirements. Figure 1C superimposes both sets of results and a new polynomial model was fitted according to the data of both gap creation methods. The combined polynomial model supports the suggestion that gap sizes above 1.4 mm in diameter compromise fit below OSHA requirements, though it should be noted that small diameters may also have an effect. In several tests, a gap size of 0.95 mm produced fit factors below recommended levels.
Discussion
Summary of Key Findings
From these data, it can be assumed that gaps of diameters of 1.4 mm or larger will compromise the fit of N95 respirators in many wearers while gaps larger than 2 mm diameter will compromise fit in all or almost all wearers. Gaps smaller than 1.4 mm may compromise fit, although our findings suggest gaps of less than 0.9 mm diameter are unlikely to have an impact on OSHA fit requirements at normal breathing rates. Circular gaps with diameters of 1.4 mm and 2 mm correspond to gaps with a total area of approximately 1.5 mm 2 and 3 mm 2 , respectively. That such small gaps can result in fit failure is concerning. To put these findings in perspective, Figure 2 demonstrates the size of these gaps when compared with an adult female finger. Our findings broadly agree with the results of Konda et al. (2020) who noted that, when mask fabric was mounted on a tube in controlled conditions, 2 small gaps of 0.635 mm diameter each were able to substantially degrade filtration efficiency. 14
Figure 2.
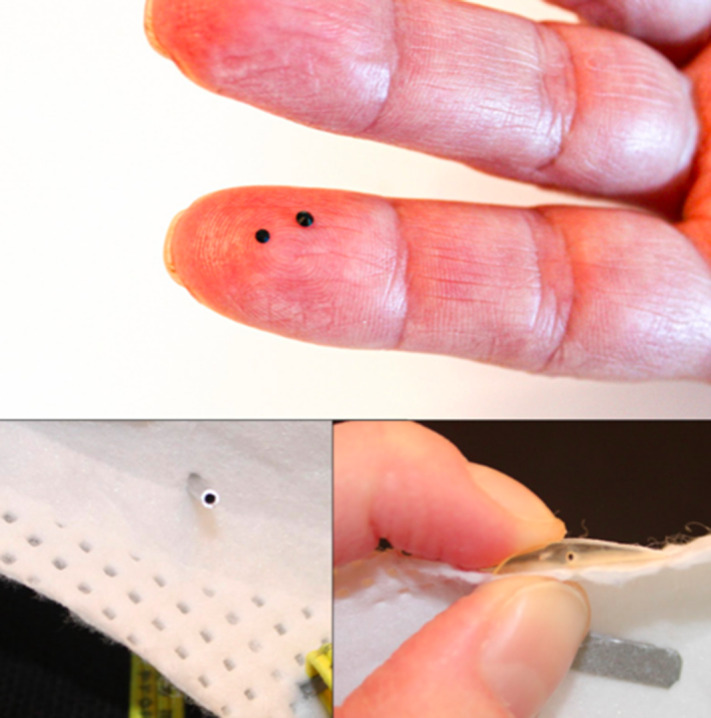
Top: For visualizing the size of the gaps, 1.5-mm diameter and 2-mm diameter dots placed on an adult female finger. Bottom left: A steel rod spacer placed through the material of the mask. Bottom right: The 3D printed resin spacer held against the edge of the mask. A small hole in the middle of the spacers allowed air to flow through.
Though results from both methodologies were broadly consistent, the use of steel tubes produced narrower confidence intervals than the measurements obtained with the resin-printed spacers. A possible explanation for this is that the resin spacers were more difficult to accurately place and had a tendency to move (see Figure 2). This may be a worthy consideration for further studies. Nonetheless, an important benefit of the 3D-printed spacers was the ability to more accurately recreate the airflow caused by a gap on the edge of the mask, which more naturally simulates the common configuration of poor fit by wearers. For stability, the steel tubes were inserted approximately 1 cm into the mask. This created greater security but is likely to disrupt the natural airflow dynamics of the mask.
Implications of Findings
It is well-established that the effectiveness of a face mask is a function of the filter efficiency and the tightness of the mask-to-face seal. 15 N95 respirators by design have a very high filtration efficiency but the effect of leaks can have significant effects. 1 A previous study, looking to explore how the location of a gap impacted performance, used a hypodermic needle of 0.84 mm diameter to create a gap and found that this was enough to create a sizeable leak of approximately 80 ml/min but the fit factor remained above 100. 4 A previous mannequin study used 3 artificial leak sources each of 0.84 mm to assess the relationship between leak size and leak flow rate, with 1, 2, and 3 leak sources introduced. 9 However, the relationship between leak size and fit factor was not reported. In the closest study to the one reported in this paper, a 14-gauge Angiocath (1.3 mm diameter) was used to introduce a fixed leak size, testing whether this compromised fit factor. It was reported that 25 of 26 participants had fit factors above 100 when the leak was plugged compared to 2/26 when the leak was open. 5
This study confirms earlier findings and explains the high variability found in the fit of N95 respirators in prior research. These findings suggest the fit of a N95 respirator is compromised by smaller gaps than might have previously been expected. The small size of these gaps also supports previous suggestions that compromising gaps may be difficult for wearers to self-detect. 1,5,6 This study highlights the importance of fit testing as opposed to mere fit checking to ensure that N95 respirators are effective when they are worn. It shows the potential for self-fit checks to be unreliable and provides data for those seeking to improve the design and fit of masks. It should be noted that fit checks do have advantages and are recommended in literature, but that they are noted to be used in addition to fit testing. 16,17
Limitations
The primary goal of this study was to provide a picture of “real life” protection given various gap sizes. While this study provides insight into the impact of gap sizes when filtering facepiece respirators are worn, there are many variables we chose not to explore.
While it has been noted that improved fit of surgical masks and fabric face coverings augments their performance, the fit of these masks is typically poor and so they are not included in this study. 18 As we were not measuring the impact of facial dimensions on fit, our study was limited to a small pool of participants.
It has previously been noted that the majority of leaks occur at the nose or chin and are usually in the shape of a slit rather than a round orifice. 7 Our study was designed to use a methodology in line with prior work, and thus the shape of the gaps created was circular. This may have some effect on airflow and thus total area needed to compromise fit.
This research did not account for the impact of factors such as particle diameter, pressure drop, and airflow on leakage, which are best measured in vitro and have been explored in other work. 10,12 This research also did not investigate the correlation between leak location and leak size. Last, these experiments are intended to contribute to the conversation on gap size and begin a discussion regarding the size of gap necessary to negate N95 fit, not to make definite conclusions. Further research, using different activities and conditions, is needed to corroborate the exact size of gap at which a filtering facepiece respirator is compromised.
Conclusions
Small gaps can compromise the fit of N95 respirators, to the extent that a mask would fail a fit test. We found that gaps with a diameter of 1.4 mm could compromise fit in the majority of our tests and gaps of over 2 mm compromised fit in all trials. To put this in perspective, a mechanical pencil lead can have a lead with a diameter of 1.4 mm while the tip of an unused crayon is approximately 2 mm. That such small gaps can compromise the fit of N95 respirators reinforce the importance of proper fit testing procedures. Future research efforts should seek to replicate these findings with larger sample sizes and varying orifice shapes to create leaks.
Acknowledgments
Independent data analysis was conducted by Trishna Mukherjee, University of Chicago.
Author contributions
O’Kelly: conceptualization, methodology, writing—original draft preparation, writing—review and editing, project administration. Arora: writing—original draft preparation, writing—review and editing. Pirog: formal analysis, visualization. Ward: conceptualization, supervision. Clarkson: conceptualization, supervision.
Conflict(s) of interest
None.
Ethical standards
Written informed consent was obtained from all participants.
References
- 1. O’Kelly E, Arora A, Pirog S, et al. Comparing the fit of N95, KN95, surgical, and cloth face masks and assessing the accuracy of fit checking. PLoS One. 2021;16(1):e0245688. 10.1371/journal.pone.0245688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. O’Kelly E, Arora A, Pearson C, et al. Performing qualitative mask fit testing without a commercial kit: fit testing which can be performed at home and at work. Disaster Med Public Health Prep. 2020. 10.1017/dmp.2020.352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cho KJ, Reponen T, McKay R, et al. Large particle penetration through N95 respirator filters and facepiece leaks with cyclic flow. Ann Occup Hyg. 2010;54(1):68-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Crutchfield CD, Park DL. Effect of leak location on measured respirator fit. Am Ind Hyg Assoc J. 1997;58(6):413-418. [DOI] [PubMed] [Google Scholar]
- 5. McKay RT, Davies E. Capability of respirator wearers to detect aerosolized qualitative fit test agents (sweetener and Bitrex) with known fixed leaks. Appl Occup Environ Hyg. 2000;15(6):479-484. [DOI] [PubMed] [Google Scholar]
- 6. Lam SC, Lee JKL, Yau SY, Charm CYC. Sensitivity and specificity of the user-seal-check in determining the fit of N95 respirators. J Hosp Infect. 2011;77(3):252-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Oestenstad RK, Dillion HK, Perkins LL. Distribution of face seal leak sites on a half-mask respirator and their association with facial dimensions. Am Ind Hyg Assoc J. 1990;51(5):285-290. [DOI] [PubMed] [Google Scholar]
- 8. Oestenstad RK, Bartolucci AA. Factors affecting the location and shape of face seal leak sites on half-mask respirators. J Occup Environ Hyg. 2010;7(6):332-341. [DOI] [PubMed] [Google Scholar]
- 9. Krishnan U, Willeke K, Juozaitis A, et al. Variation in quantitative respirator fit factors due to fluctuations in leak size during fit testing. Am Ind Hyg Assoc J. 1994;55(4):309-314. [DOI] [PubMed] [Google Scholar]
- 10. Hinds WC, Kraske G. Performance of dust respirators with facial seal leaks: I. Experimental. Am Ind Hyg Assoc J. 1987;48(10):836-841. [DOI] [PubMed] [Google Scholar]
- 11. Kähler CJ, Hain R. Fundamental protective mechanisms of face masks against droplet infections. J Aerosol Sci. 2020;148:105617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hinds WC, Bellin P. Performance of dust respirators with facial seal leaks: II. Predictive model. Am Ind Hyg Assoc J. 1987;48(10):842-847. [DOI] [PubMed] [Google Scholar]
- 13.1910.134 App A—Fit Testing Procedures (Mandatory). Occupational Safety and Health Administration. 2004. Accessed March 6, 2021. https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134AppA
- 14. Konda A, Prakash A, Moss GA, et al. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14(5):6339-6347. [DOI] [PubMed] [Google Scholar]
- 15. Rengasamy S, Eimer BC. Nanoparticle penetration through filter media and leakage through face seal interface of N95 filtering facepiece respirators. Ann Occup Hyg. 2012;56(5):568-580. [DOI] [PubMed] [Google Scholar]
- 16. Or P, Chung J, Wong T. Does training in performing a fit check enhance N95 respirator efficacy? Workplace Health Saf. 2012;60(12):511-515. [DOI] [PubMed] [Google Scholar]
- 17. Regli A, Sommerfield A, von Ungern-Sternberg BS. The role of fit testing N95/FFP2/FFP3 masks: a narrative review. Anaesthesia. 2021;76(1):91-100. [DOI] [PubMed] [Google Scholar]
- 18. O’Kelly E, Arora A, Pirog S, et al. Face mask fit hacks: improving the fit of KN95 masks and surgical masks with fit alteration techniques. PLoS One. 2022;17(2):e0262830. 10.1371/journal.pone.0262830 [DOI] [PMC free article] [PubMed] [Google Scholar]