Abstract
In response to the COVID-19 pandemic, governments enacted a range of public health measures aimed at preventing the spread of the virus. These measures resulted in school closures, social isolation, and job loss, which all contributed to increased psychosocial stress, particularly among families with pre-existing vulnerability factors. Given the relationship between increased psychosocial stress and intimate partner violence (IPV), this rapid review investigated change in the prevalence and correlates of IPV victimization during the first six months of the pandemic. PsycINFO, MEDLINE, Embase, PubMed, Scopus, and the Cochrane COVID-19 registry were reviewed. This search resulted in 255 unique results, of which 24 studies were included. There were 19 studies that examined changes in the rate of IPV from before the COVID-19 pandemic to during the pandemic. Of the studies examining changes in the rate of IPV, 11 found a significant increase. Key vulnerability factors contributing to the increase include low socioeconomic status, unemployment, a personal or familial COVID-19 diagnosis, family mental illness, or overcrowding. Six studies examined whether the presence of children in the home was associated with IPV, but the direction of this relationship was inconsistent. This review finds preliminary evidence of a relationship between COVID-19 induced stressors, pre-existing vulnerabilities, and increased IPV, which present important implications for policy and practice.
Keywords: Intimate partner violence, COVID-19, Coronavirus, Mental health, Family violence
Introduction
COVID-19 Prevalence and Lockdown Measures Worldwide
The World Health Organization declared COVID-19 a pandemic on March 11, 2020 (World Health Organization, 2020). At this point, there were 118,000 COVID-19 cases across 114 countries. By September 28, 2020, cases globally had increased to 2,128,438, with 35.72% of cases in North America, 28.90% of cases in South-East Asia, 26.92% of cases in Europe, 6.02% of cases in the Eastern Mediterranean, 1.28% of cases in Africa, and 1.16% of cases in the Western Pacific (World Health Organization, n.d.). Almost all countries enacted lockdown measures to control the spread of COVID-19 in March 2020 (Onyeaka et al., 2021). Common shelter-in-place policies included physical distancing, working from home, and closing non-essential businesses and schools. These restrictions were consistent across many geographic regions (Haug et al., 2020), and social and economic disruption emerged globally as a consequence of the strict public health measures. In addition to the societal-level effects, family-level disruption occurred, which prompted the question: did intimate partner violence (IPV), which is known to be associated with family-level stress (Lucero et al., 2016; Weitzman & Behrman, 2016), also increase during the early stages of COVID-19? Based on this question, in this rapid review, we aimed to investigate change in the prevalence, correlates, and impacts of IPV victimization during the first six months of the pandemic.
COVID-19 and Family Disruption
The COVID-19 pandemic resulted in a range of disruptions for families, including school closures, job loss, and isolation (Brown et al., 2020). These reflect one layer of a cascading process in which couple and family wellness may be adversely affected by COVID-19 (Prime et al., 2020). Theoretical models suggest that COVID-19 disruptions can contribute negatively to caregiver well-being through the increase of psychosocial stress, which may ultimately disrupt family relationships (Prime et al., 2020). Parental perceived stress is also associated with COVID-19 related stressors (Brown et al., 2020), and Merrill et al. (2021) demonstrated that COVID-19 public health restrictions are associated with increased family stress and conflict. Moreover, COVID-19 has disproportionately impacted families with pre-existing vulnerabilities such as low socioeconomic status (SES) or disabilities (Karmakar et al., 2021).
Correlates of Intimate Partner Violence
IPV is defined as “physical violence, sexual violence, stalking and psychological aggression (including coercive tactics) by a current or former intimate partner” (Breiding et al., 2015, p. 11). Intimate partner violence has been identified as a significant global health concern, exemplified by the United Nations Sustainable Development target to eliminate violence towards women by 2030 (United Nations, 2015). The global estimate of the lifetime prevalence of IPV among women is 30% (World Health Organization, 2013). In the United States, 22.3% of women and 14.0% of men have experienced physical IPV (Breiding et al., 2015).
The pre-pandemic correlates of IPV, such as social isolation (Kim, 2019) and unemployment (Schneider et al., 2016) are well established, and these risk factors were exacerbated by the COVID-19 pandemic (Hwang et al., 2020; ILO, 2020). A systematic review and meta-analysis completed by Yakubovich et al. (2018) found that a low level of education was one of the greatest risk factors for IPV. Yakubovich and colleagues explain that level of education could potentially be interpreted as a proxy for SES (2018).
In contrast to the risk factors of IPV, protective factors such as social connection were put at risk by the pandemic (Kim, 2019). Social support and community cohesion are both key protective factors that promote resilience in survivors of IPV (Howell et al., 2018). Specifically, the absence of social isolation has been found to protect against IPV (Fernbrant et al., 2014). A systematic review examining intimate partner violence against Chinese women found that formal and informal social control is protective against IPV (Cao et al., 2021). Cao et al. (2021) also concluded that good health is protective, which is understandable given that a final protective factor is regular contact with a family physician, because the primary care setting is a critical environment for detecting IPV (Peralta & Fleming, 2003).
Intimate Partner Violence During the COVID-19 Pandemic
As a result of the strict public health measures implemented to control the spread of COVID-19, it is possible that the prevalence of IPV was impacted. Brink and colleagues (2021) examined changes in IPV in Europe during the initial weeks of the pandemic. They found that the prevalence of IPV increased in six countries, while decreasing in two and remaining the same in two. Empirical studies have shown that stay-at-home orders and social distancing measures have increased women’s vulnerability to IPV and further obstruct access to their support networks (Bradbury-Jones & Isham, 2020; Usher et al., 2020). Additionally, a rapid review by completed by Mojahed et al. (2021) examined social and geographic isolation in the context of the COVID-19 pandemic, and they found a significant association between social and geographic isolation and increased risk of IPV. Furthermore, pre-existing vulnerabilities, in conjunction with new stressors emerging from the pandemic, increase the risk of IPV exposure (Boserup et al., 2020). For instance, many households face increased financial strain because of the pandemic; 12.4% of Canadian paid workers were laid off in response to COVID-19 (Statistics Canada, 2020). This speaks to experiences of marginalized groups (Bowleg, 2020). These findings gain importance as economic vulnerabilities are a critical indicator of increased rates and severity of IPV (National Institute of Justice, 2009). Still, it should be noted that the association between IPV and economic hardship is likely reciprocal (Renzetti & Larkin, 2009).
Couples with children (in contrast to those without) may have also experienced increases in IPV during the early stages of the pandemic. Prior to the pandemic, IPV occurred disproportionately within families with children, specifically when young children were present within the home (Bair-Merritt et al., 2008). As previous studies have demonstrated that women with children are more vulnerable to IPV (Peek-Asa et al., 2017), increased IPV becomes a likely consequence of the COVID-19 pandemic and further highlights the importance of a family system lens in conceptualizing this phenomenon. Both social disadvantage and exposure to IPV are related to poor developmental outcomes for children (Evans et al., 2008; Pingley, 2017) which exemplifies the importance of understanding how COVID-19 related stressors have contributed to cumulative psychosocial risk among families. Reviews assessing the precipitating factors contributing to changes in IPV during the pandemic are limited. Thus, it remains unclear how the increased stress resulting from the COVID-19 pandemic influenced rates of IPV and whether there was a disproportionate impact for specific groups (e.g., low SES, families).
Research Objectives
Our first set of research aims were to understand the prevalence of IPV victimization during the coronavirus pandemic and examine whether the prevalence has changed relative to existing estimates. The second objective was to explore what driving factors contributed to IPV during the COVID-19 pandemic. Specifically, pre-existing vulnerabilities and COVID-19 induced stressors were both examined. We also explored whether there was a differential impact on rates of IPV for couples with and without children because school closures were a unique challenge to couples who are also parents.
Methods
Search Strategy
The rapid review protocol adhering to the preferred reporting items for systematic review and meta-analysis (PRISMA) guidelines (Moher et al., 2015) was submitted for registration with PROSPERO [CRD42020213143] on October 27, 2020. The “strategy for data synthesis” portion of the protocol was updated and resubmitted, and the protocol was accepted for registration on November 23rd, 2020. Rapid reviews offer unique benefits not seen in other types of reviews. Rapid reviews are particularly beneficial in the context of public health emergencies, such as COVID-19, when policy makers require timely evidence for health system decision making (Tricco et al., 2017). By expediting the review process, appropriate policies and resources can be established to support survivors of IPV throughout the remainder of the pandemic. Furthermore, by pre-registering and adhering to evidence-based scientific standards, the quality of the review can be maintained (Tricco et al., 2017). One limitation of this method is that grey literature was not examined. The search was restricted to papers published in English, with data collection taking place during the first 6 months of the pandemic (i.e., before September 11th, 2020, six months after the World Health Organization declared the pandemic), and the raw dataset of studies was created on October 30, 2020. This period was selected because a global lockdown occurred at this point of the pandemic, and nearly every country in the world implemented some degree of domestic lockdown (Onyeaka et al., 2021). Additionally, the early months of the pandemic consisted of great economic uncertainty and increased financial stress at the individual level, as well as increased fear and decreased access to education (Onyeaka et al., 2021). Given this is a global review, selecting an early timeframe when most countries in the world were locking down allows us to draw more concrete conclusions across geographic regions. Data needed to be included regarding the prevalence of IPV and/or the factors contributing to IPV during the COVID-19 pandemic. PsycINFO, MEDLINE, Embase, PubMed, Scopus, and the Cochrane COVID-19 Study registry were searched. The article title, abstract, and keyword fields were examined using the following search string: ((“COVID-19” OR Coronavirus OR “SARS-CoV-2”) AND (“family violence” OR “domestic violence” OR “domestic abuse” OR “domestic conflict" OR "marital conflict" OR "intimate partner violence”)). Quantitative, empirical study designs (i.e., randomized controlled trials, non-randomized control trials, interrupted time-series studies), qualitative interview studies, analytical observational studies (i.e., retrospective cohort studies, case–control studies, and cross-sectional analysis), and mixed methods studies were included. Reviews, as well as comments, editorials, and letters to the editor were excluded.
Data Collection
A list of all resulting studies was compiled in an Excel spreadsheet, and duplicate studies were removed. Reviewer one performed pilot testing to clarify inclusion and exclusion criteria. Two reviewers screened the abstracts against the inclusion criteria independently. Interrater reliability was calculated based on agreement on inclusion, exclusion, and requiring further review categorization for 20% of the studies. Interrater reliability was achieved indicated by a kappa value of 0.83. The second stage of reliability focused on examining the full-text reports for abstracts where there was uncertainty about inclusion. Independent reviewers overlapped on 20% of the remaining studies, and interrater reliability at this stage was k = 1.0. Data extraction was then completed for all studies meeting the inclusion criteria. The type of study and time of data collection were recorded, as well as the country where the study was conducted. Sample characteristics were noted including age group(s), sample size, population, ethnicity, SES, household composition, and relationship status. The prevalence of IPV at all available timepoints was also noted. Pre-existing vulnerabilities were recorded as well as stressors resulting from COVID-19. Measures used to assess outcomes of interest were also noted.
Quality Appraisal
Following the screening process, a quality assessment was performed to assess the risk of bias in eligible studies using the Quality Assessment for Diverse Studies (QuADS) (Harrison et al., 2021). This tool is a revised version of the quality assessment tool for Studies with Diverse Designs (Sirriyeh et al., 2012). This tool was selected because the reviewed studies employ a range of designs, and this tool shows strong inter-rater reliability and content and face validity across study designs (Sirriyeh et al., 2012). The tool employs 13 questions to assess quality. For each article, questions were scored between 0 (not at all) and 3 (complete). Studies were not excluded based on their quality, but the results are reported, and the information was considered when drawing conclusions. In our PROSPERO registration, we stated that two reviewers would perform a risk of bias assessment based on a series of five questions. Because of the range of studies reviewed, the QuADS tool was selected to better capture the different methodologies. Resource limitations also meant that only one reviewer performed the quality appraisal.
Data Analytic Approach
Popay and colleagues’ guidelines (2006) were used to inform narrative data synthesis, which offers the best method to synthesize data from studies employing different methodological approaches. A preliminary synthesis took place whereby findings were organized to describe the vulnerability factors contributing to IPV during the COVID-19 pandemic. Any significant findings showing a difference in IPV prevalence or precipitating factors between couples with and without children were noted. Patterns across studies were also examined and the direction and size of effects were determined (Popay et al., 2006). Next, relationships between the data were explored to understand any differences in results between studies. Table 2 presents key findings from all the individual studies that meet inclusion criteria (see Appendix 1). Key findings were extracted from each study and summarized individually in the results section. Trends and similarities across studies were noted, and the findings were used to frame the discussion, where specific policy recommendations were made.
Study Characteristics
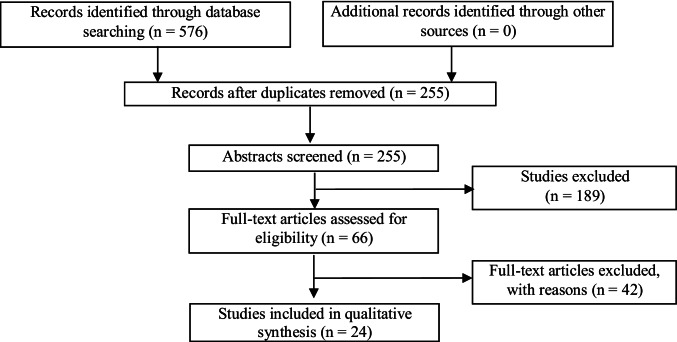
In total, 255 non-duplicated abstracts were identified in the initial search, and 66 studies were identified as potentially meeting inclusion criteria based on their abstract. These 66 studies underwent a full-text assessment for eligibility, and 24 studies met the eligibility criteria. See Fig. 1 for the PRISMA flowchart. Included studies span a range of geographic regions, with nine studies taking place in Europe, eight occurring in the United States, and additional studies taking place in Australia, Peru, Bangladesh, and Tunisia. All studies reported data that were collected during the COVID-19 pandemic, but some also extended back to prior months and years for comparison. Most studies (n = 14) drew on data from existing databases. Five studies analyzed forensic data and six studies examined hospital admissions data and extracted information related to the prevalence of IPV. Finally, two studies examined call logs to domestic abuse helplines and one study looked at referral data for a domestic abuse program.
Fig. 1.
Prisma Flowchart
Ten studies performed primary data collection or analyzed multiple variables based on secondary data. Nine of these studies explored differences in IPV across different groups at one timepoint or asked participants to retrospectively consider how their experience of IPV changed since the start of the pandemic. One of the highest quality studies in this review used an interrupted time series design to examine changes in self-reported IPV (Hamadani et al., 2020). Given the nature of the data presented in this review, no causal inferences about the relationship between COVID-19 and IPV can be made, and all conclusions are correlational.
Results
Quality Appraisal Findings
The quality appraisal scores are reported in table 2, and scores ranged from 14/39 (35.90%) to 31/39 (79.49%), with an average quality score of 66.56% (see appendix 1). Overall, the studies in this review stated clear research aims (M = 2.63) and provided a description of the target population and setting (M = 2.63). The study designs (M = 2.54) and data collection tools used (M = 2.54) were also adequate to address target research aims. However, only two studies considered relevant research stakeholders (M = 0.17), and there was a lack of justification provided for the data collection tools (M = 1.50) and analytic methods (M = 1.08) selected.
Changes in IPV During the COVID-19 Pandemic
Of the 24 studies included, 19 examined changes in the prevalence of IPV during the pandemic compared to pre-pandemic. Most of these studies (n = 11) documented an upsurge in IPV, and this was determined through the retrospective examination of past hospital or police records (Hassan et al., 2020; Leslie & Wilson, 2020; Mohler et al., 2020; Payne et al., 2020; Rhodes et al., 2020), self-report of IPV change (Hamadani et al., 2020; Sabri et al., 2020; Sediri, et al., 2020), or helpline calls (Agüero, 2021; Bracewell et al., 2020; Weller et al., 2021). Agüero (2021) found a 48% increase in calls to domestic violence helplines. Rhodes et al. (2020) showed a significant increase in domestic violence as a percentage of emergency department admissions during the pandemic, and Hamadani et al. (2020) found that during COVID-19, IPV increased for over half of the women who had reported experiencing it before (Hamadani et al., 2020). Finally, Sediri and colleagues documented a significant increase in IPV, from 4.4% to 14.8% (p < 0.001). Together these findings suggest an increase in IPV.
Four studies reported no change in IPV (Jacob et al., 2020; Jetelina et al., 2021; Pakenham et al., 2020; Piquero et al., 2020), and three studies illustrated a decrease (Gosangi et al., 2021; Halford et al., 2020; Olding et al., 2021). Murphy et al. (2020) found an initial reduction in orthopedic referrals, but the proportion of IPV related cases remained stable. Gosangi et al. (2021) found an overall decrease in IPV survivors seeking hospital care during the COVID-19 pandemic (146 in 2017; 106 in 2018; 104 in 2019; and 62 in 2020) (p < 0.001), but they revealed a higher incidence of lethal physical violence including strangulation and use of weapons. The percentage of survivors of physical violence was 12% in 2017 to 19 compared to 42% in 2020 (p = 0.01) (Gosangi et al., 2021). Olding et al. (2021) reported a decline in the proportion of physical traumas resulting from IPV during the COVID-19 pandemic in comparison to past years (89% from March 23rd to April 29th, 2019, and 63% from March 23rd to April 29th, 2020). Similarly, Halford et al. (2020) found a decrease in IPV during the pandemic, based on police records. Halford et al. (2020) argue that while it is possible the decrease is genuine, it is likely attributable to decreased reporting.
Types of IPV During the COVID-19 Pandemic
Different types of IPV were examined across studies including physical, psychological, and/or sexual violence. The six studies examining emergency department trauma consults and admissions were limited to physical violence (Blackhall et al., 2020; Hassan et al., 2020; Jacob et al., 2020; Murphy et al., 2020; Olding et al., 2021; Rhodes et al., 2020). Two studies found an increase in the incidence of lethal IPV involving weapons (Gosangi et al., 2021; Rhodes et al., 2020). Specifically, Rhodes et al. (2020) demonstrated that penetrating assaults increased from 2.6% of all assaults before the COVID-19 pandemic to 18% during the pandemic.
Hamadani et al. (2020) examined changes in the rate of victimization and revealed that all types of IPV increased during the pandemic. Based on self-report of participants’ experiences of both physical and psychological IPV during the COVID-19 pandemic, psychological IPV was noted as more prevalent than physical IPV (Gebrewahd et al., 2020; Hamadani et al., 2020; Iob et al., 2020; Sediri et al., 2020). Iob et al. (2020) found that psychological violence was significantly more common than physical violence (8.3% compared to 2.9%, respectively; p < 0.05). Finally, in an interview and questionnaire study, Gebrewahd et al. (2020) reported that psychological violence was the most common type of violence (13.3%) followed by physical violence (8.3%). The results indicate that verbal IPV is more prevalent, but there is some evidence that physical violence may also be increasing.
Vulnerability Factors for Increased IPV During the COVID-19 Pandemic
Unemployment and low SES were frequently associated with an increase in IPV, with findings from seven studies indicating a relationship between job loss, unemployment, or low SES and an increase in IPV (Bracewell et al., 2020; Davis et al., 2020; Gebrewahd et al., 2020; Iob et al., 2020; Jetelina et al., 2021; Payne et al., 2020; Sabri et al., 2020) Agüero (2021) and Leslie and Wilson (2020) reported no relationship between SES and the prevalence of IPV. A significantly higher percentage of IPV was reported among women who were unemployed (psychological abuse = 14.7%; physical abuse = 6.7%) compared to those who were working (psychological abuse = 7.8%; physical abuse = 2.4%) (Iob et al., 2020). Jetelina et al., (2021) found that IPV was significantly more prevalent for survivors who experienced job loss or loss of income during the pandemic (OR = 1.63; 95% CI 1.17 to 2.27), compared to survivors whose income was not affected. Davis et al. (2020) found that individuals who lost their job due to COVID-19 were 2.5 to 3 times more likely to be survivors of IPV. Finally, Sabri et al. (2020) performed qualitative interviews with 45 immigrant women in the United States who have experienced IPV. A common concern that emerged was increased stress resulting from the social and economic disruption, as well as financial hardship.
Pre-existing mental health difficulties were commonly associated with an increase in IPV during COVID-19 (Iob et al., 2020; Sabri et al., 2020; Sediri et al., 2020). When compared to survivors without a mental illness, those with a mental health diagnosis were significantly more likely to experience psychological violence (6.5% vs. 15.9%, respectively) and physical abuse (2.3% vs. 5.7%, respectively) during the pandemic (Iob et al., 2020). Iob et al. (2020) also compared the prevalence of abuse across participants with severe, moderate, and mild depression and anxiety symptoms, based on the PHQ-9 (Kroenke et al., 2001) and GAD-7 (Spitzer et al., 2006), respectively. Participants with severe depressive symptoms were significantly more likely to experience psychological (26.5%) and physical (12.0%) abuse compared to those with mild (psychological abuse = 4.6%; physical abuse = 1.2%) symptoms. Participants with severe anxiety were also significantly more likely to experience psychological (21.5%) and physical (9.1%) abuse compared to those with mild (psychological abuse = 5.7%; physical abuse = 1.6%) symptoms. Sediri et al. (2020) found that violence during lockdown was associated with higher depression and anxiety for IPV survivors. Finally, qualitative interviews revealed that factors such as more caregiver demands, economic stress, and social isolation negatively impacted mental health for immigrant survivors (Sabri et al., 2020).
A personal COVID-19 diagnosis was significantly correlated with an increased prevalence of IPV. Iob et al. (2020) found that participants with a COVID-19 diagnosis were significantly more likely to experience psychological abuse (17.6%) and physical abuse (9.0%) in comparison to those without (psychological abuse = 8.3%; physical abuse = 2.9%). Davis et al. (2020) also found that participants with a COVID-19 diagnosis were almost three times more likely to experience IPV, and the number of COVID-19 cases within a state predicted the overall prevalence of IPV in the same area. This finding could be explained by structural factors, such that living in low-income neighborhoods or in overcrowded settings predicts both an increased prevalence of IPV and an increased likelihood of getting COVID-19.
A final vulnerability factor was related to the physical environments that survivors of IPV were living in. Overcrowding and lack of physical space were associated with increased IPV. Iob et al. (2020) found a significantly higher percentage of IPV among participants living in overcrowded households (psychological abuse = 14.4%; physical abuse = 9.1%) compared to those who had adequate space (psychological abuse = 8.1%; physical abuse = 2.7%). This is problematic because Pakenham et al. (2020) found that on average, people lacked adequate physical space. Another theme related to the physical environment was a lack of privacy, which impaired treatment seeking (Sabri et al., 2020). A qualitative study, by Bracewell et al. (2020) also found quarantine measures and working from home increased stalking behaviour due to increased opportunities for tracking and surveillance. Notably, Agüero (2021) and Leslie and Wilson (2020) found no relationship between physical space and IPV. A summary of vulnerability factors can be found in Table 1.
Table 1.
Summary of Vulnerability Factors for IPV
| Correlate | Proportion of studies | Resulting Conclusions |
|---|---|---|
| Unemployment and low SES | 7 of 9 (77.78%) studies examining the relationship between SES and IPV | Positive association between low SES or job loss and the prevalence of IPV |
| Mental Illness | 3 of 3 (100.00%) studies examining the relationship between mental illness and IPV | Positive association between pre-existing mental illness and the prevalence of IPV |
| Personal diagnosis of COVID-19 | 2 of 2 (100.00%) studies examining the relationship between a diagnosis of COVID-19 and IPV | The prevalence of IPV was significantly higher among people with a diagnosis of COVID-19 compared to those without |
| Lack of physical space and privacy | 3 of 5 (60.00%) studies examining the relationship between lack of physical space and IPV | Positive association between a lack of physical space or privacy and the prevalence of IPV |
The proportion of studies column refers to, of studies examining the variable of interest, what proportion identified the variable as a correlate of increased IPV during COVID-19?
Children and IPV During the COVID-19 Pandemic
There was limited information regarding the impact that children being at home has had on rates of IPV. Iob et al. (2020) found the prevalence of IPV was significantly higher among households with children (verbal abuse = 9.8%; physical abuse = 3.3%) compared to households without (verbal abuse = 7.8%; physical abuse = 2.8%). However, Jetelina et al. (2021) found no significant effect of children being home on the prevalence or severity of IPV during the pandemic. Halford et al. (2020) found that both IPV and vulnerable child offences decreased as a proportion of all crimes following lockdown, but the authors caution that this decrease could be a result of decreased reporting. One theme that emerged was a concern for child welfare. A study conducted in Norwegian refuges, which are shelters for IPV survivors, found that 83% of staff reported concern for children (Øverlien, 2020). Common concerns include decreased connection and support. Finally, qualitative interviews conducted by Sabri et al. (2020) revealed that children being outside of the home was a mechanism of accountability for perpetrators before the pandemic, and loss of this accountability contributed to the reciprocal and reinforcing relationship between stress and IPV.
Discussion
Based on this rapid review, there is some preliminary evidence that physical, psychological, and sexual IPV increased during the early stages of the pandemic, particularly for those with pre-existing vulnerabilities. This is supported by our result that 11 of 19 studies examining changes in the prevalence of IPV during the pandemic found an increase. Although the quality appraisal scores did not differ between studies that found an increase in IPV (M = 65.27) and studies that did not find an increase (M = 65.06), there are qualitative differences between the studies included in each group. Of the studies that found an increase in IPV, 18.18% of studies used hospital-based data. In contrast, of the studies that found no change or a decrease in IPV, 50.00% of studies used hospital-based data. This is an important difference because emergency departments observed an overall decrease in patient volume during the pandemic (Nourazari et al., 2021), and hospital findings indicating a decrease in IPV could be linked to this overall decrease in treatment seeking. In addition to examining the prevalence of IPV during the pandemic, this study sought to understand the influence that pre-existing vulnerability factors and COVID-19 induced stressor were having on rates of IPV. Four correlates of IPV during the pandemic emerged. Our results revealed that unemployment and low SES were associated with an increased prevalence of IPV. There was also a relationship between pre-existing mental illness, a personal diagnosis of COVID-19, and overcrowding, and an increased rate of IPV. It remains unclear whether the prevalence of IPV during the pandemic differs between couples with and without children. However, one theme that emerged in two qualitative studies was a concern for child wellbeing during the pandemic.
Implications for Practice
Primary Care
Primary care settings serve as a critical screening environment for IPV (McLennan & MacMillan, 2016). In response to the pandemic, primary care (e.g., family health teams, primary physicians) rapidly shifted to telemedicine to limit the spread of COVID-19 (Webster, 2020). In doing so, it is possible that IPV survivors lost an important point of contact for disclosing their experience of violence. This is because a limitation of telehealth during the pandemic is that abusive partners are more able to monitor help seeking attempts by listening during videocalls (Ragavan et al., 2020). As a result, a greater number of survivors might feel unsafe disclosing. Health policymakers need to consider the implications of having family physicians working virtually for survivors of IPV.
One approach to mitigate the consequences of telehealth for survivors of IPV is mobile remote monitoring, which allows for screening of IPV and the provision of peer and professional support (Krishnamurti et al., 2021). One critical requirement for clinicians working remotely is to assess whether their client is in a safe space to speak transparently (Ragavan et al., 2020). If an individual does not have this space, providing in-person support is an essential obligation (Ragavan et al., 2020). Virtual care for IPV also requires protective privacy features such as emergency exits and chat boxes (Ragavan et al., 2020). If a telehealth service has an emergency exit option where the survivor can quickly close the window and history of the appointment, healthcare providers need an alternative means to follow-up to ensure the client’s safety.
Another type of primary care that observed an overall decrease in presenting patients during the pandemic was hospital emergency departments (Nourazari et al., 2021). Thus, hospital findings indicating a decrease in IPV during the pandemic could be linked to the reduced accessibility of in-person primary care services. COVID-19 restrictions may also have resulted in an overrepresentation of the IPV instances involving high-risk physical violence in primary care (Gosangi et al., 2021), and an observed decrease in the reporting of less severe cases of IPV.
Increased Stressors
Stressors related to COVID-19 including job loss, lack of privacy, and a personal diagnosis of COVID-19 emerged as key correlates of IPV. When considering these results, it is important to acknowledge the positive relationship between low SES and overcrowding with both IPV and COVID-19 vulnerability (Patel et al., 2020). The intersection of these different stressors highlights the importance for government policy to address systemic factors, such as access to social services. Providing government financial assistance and subsidized housing for individuals who are unemployed because of the pandemic could help mitigate some of the structural factors contributing to further marginalization among vulnerable groups. This is critical because of the association between affordable housing and mental wellbeing (Bentley et al., 2011), and the increased risk of IPV exposure for women in the conditions of low-income and overcrowded housing.
Social Connection
Social connection helps to mitigate the adverse mental health outcomes that can result from IPV (Fernbrant et al., 2014). Social isolation is one consequence of the public health restrictions implemented to prevent the spread of COVID-19 (Brown et al., 2020). One example of community connection that was lost in response to the pandemic was community babysitting, where volunteers check-in with families where abuse is occurring, and this has been shown to be protective (Sabri et al., 2020). To compensate for the lost social support during the pandemic, communities need to ensure that people experiencing IPV can stay connected virtually. Creating accessible and confidential virtual services (e.g., peer support groups, counselling) for survivors is critical. In addition to providing adequate online alternatives for those previously accessing in-person IPV services, ensuring that people experiencing IPV for the first time can adequately connect with resources is crucial. Past online interventions have demonstrated the effectiveness of social media and smartphones in safety planning (Rempel et al., 2019), and implementing similar interventions throughout the pandemic could help support women who are unable to access in-person services. Given the reciprocal relationships between IPV, low SES, and job loss, ensuring that survivors are provided with the technology necessary to stay connected with formal and informal support networks will help to promote resilience.
Children and Families
Finally, our review revealed that there is a scarcity of literature about the impact of children being at home for extended periods of time on the prevalence of IPV. However, we know that children being at home and learning virtually has increased family stress (Hiraoka & Tomoda, 2020), and increased stress can adversely impact rates of IPV for vulnerable families (Bradbury-Jones & Isham, 2020). There is also the risk that children are being exposed to a greater frequency and severity of IPV. We know that child abuse is increasing throughout the pandemic (Brown et al., 2020); however, no studies have examined the mental health implications resulting from children witnessing IPV throughout COVID-19. Although six studies examined the relationship between children in the home and IPV, the findings were inconclusive. A crucial future research direction will be understanding the influence that this potential increase in exposure to IPV is having on children.
Limitations and Future Research Directions
This review aimed to understand the precipitating and vulnerability factors contributing to IPV during the COVID-19 pandemic. A systematic search strategy was used to ensure a comprehensive synthesis of the literature. It is unlikely that studies meeting inclusion criteria were missed; however, it should be acknowledged that only six databases were screened, and grey literature was not examined. Furthermore, new literature related to COVID-19 and IPV has emerged rapidly throughout 2021, and the conclusions drawn in this review are based only on literature available before October 30th, 2020. As a result, caution is required if generalizing the results of this review to periods beyond the early stages of the pandemic. Future research should examine how trends in IPV have changed throughout the pandemic and beyond.
Because of the novelty of COVID-19, longitudinal data was limited. Most studies were cross-sectional and examined the prevalence of IPV at a single timepoint. Retrospective recall was also common. This is valuable in understanding changes in IPV resulting from the pandemic; however, it does not provide an understanding of the mechanism responsible for the change. Many studies also examined changes in a single variable (e.g., crime rates) without providing demographic information which would help to establish the correlates of IPV.
Another limitation of our review is that European countries (n = 9) and the United States (n = 8) were overrepresented in our dataset of studies. As a result, the applicability of the review findings to other geographic regions may be limited. Additionally, we collapsed our findings across geographic regions. As a result, we did not consider specific differences in lockdown measures and the prevalence of COVID-19 between countries.
Future research should focus on understanding the mechanism responsible for a potential increase in IPV during the COVID-19 pandemic. This review provides preliminary evidence that IPV has increased in response to the COVID-19 pandemic. This increase is linked with certain intersecting vulnerabilities, particularly job loss, low SES, pre-existing mental health challenges, a personal or familial diagnosis of COVID-19, and crowded living. Understanding the precipitating and vulnerability factors contributing to the increase in IPV is necessary to ensure that policy focuses on protecting the most vulnerable throughout the remainder of COVID-19. Ideally, future research should examine the longitudinal impact of COVID-19 on rates of IPV. Drawing on past self-report data of IPV before the pandemic and following up throughout the remainder of the pandemic would be an ideal design. Because the psychosocial and economic consequences of the COVID-19 pandemic have become disproportionately negative for people at marginalized social locations (i.e., ethnic/racial minorities, people with disabilities, or low SES) (Bowleg, 2020), research focusing on marginalized communities is also needed.
Conclusion
The COVID-19 pandemic has increased psychosocial stress which is associated with increases in IPV. Because of the complex interplay between pre-existing vulnerability factors and COVID-19 induced stressors, specific groups are particularly vulnerable to the consequences of COVID-19. This review found preliminary evidence that IPV increased during the first 6-months of the COVID-19 pandemic, and that individuals with a low SES are the most at risk for an increased frequency and severity of IPV. The impact of children being home more frequently on rates of IPV during the pandemic remains unclear and should be examined in future investigations. Our results demonstrate the important role of social connections in protecting survivors of IPV, and services need to adapt to ensure that people experiencing IPV can feel supported throughout the remainder of the pandemic and beyond.
Appendix 1
Table 2.
Study Characteristics
| Study | Study Design | Location and Population | Measures of IPV | IPV prevalence | Vulnerability factors for higher IPV during COVID-19 |
Quality Appraisal |
|---|---|---|---|---|---|---|
| Agüero, 2021 |
• External database • January 2007 until July 2020 • Data tracking of calls to the helpline Línea 100 |
• Peru • Data at the month and state level on the volume of calls per 100,000 |
• Helpline calls |
• Increase in IPV • 48% increase in calls to the helpline since the pandemic • Prior to the pandemic, 60% of women were experiencing domestic abuse |
• Not driven by any demographic background characteristics, even when considering the pre-determined prevalence of domestic violence |
• 26/39 (66.67%) • Data collection method did not allow for information about the sample to be reported (i.e., caller demographic characteristics) |
| Blackhall et al., 2020 | • Prospective data collection beginning on March 26th, 2020 |
• United Kingdom • People presenting with maxillofacial injuries across five hospitals |
• Hospital records |
• No reported data on changes in IPV • 529 patients over six weeks • 44 cases of facial fractures with 17 cases related to domestic abuse |
• n/a |
• 24/39 (61.54%) • Limited justification for the choice of statistical analysis |
| Bracewell et al., 2020 |
• Unspecified timeframe • Semi-structured interviews and discussions following the start of the pandemic |
• United Kingdom • n = 15 survivors of IPV • n = 6 healthcare providers |
• Thematic analysis of transcribed participant interviews using NVivo v12 |
• Increase in IPV • 50–70% increase in initial requests for support via email from both survivors and wider services in the 3 months from April 2020 compared to the previous 3 months |
• Confinement to the home • Increased stalking and surveillance opportunities • Loss of employment or working from home • Delays in the criminal justice system |
• 24/39 (61.54%) • No consideration of the sample size requirements • Limited consideration of the validity and reliability of qualitative methods |
| Davis, et al., 2020 |
• April 22nd to April 30th • Cross sectional study |
• USA • N = 2045 non-institutionalized adults • Stratified quota sampling to ensure sample characteristics of sex, age, and race were representative • Respondents needed to be at least 18 years old |
• Four-item tool to assess IPV perpetration and victimization since the outbreak of COVID-19 • Self-reported demographic data, recent health history, and degree of personal social distancing |
• No reported data on changes in IPV |
• Reporting COVID-19 positive (almost 3 times more likely to experience IPV) • Living in states with higher spread of the COVID-19 virus • Losing a job due to COVID-19 (2.5–3 times more likely to experience physical IPV) |
• 31/39 (79.49%) • No consideration of the sample size requirements • Limited justification for the choice of statistical analysis |
| Gebrewahd et al., 2020 |
• April to May 2020 • Community based cross-sectional study consisting of interviews and a self-administered questionnaire |
• Ethiopia • N = 682 reproductive age women |
• Violence against women was measured using thirteen WHO questions regarding psychological, physical, and sexual violence |
• No reported data on changes in IPV • Psychological violence was the predominant type of violence (13.3%) • 8.3% of participants suffered from physical violence such as slapping or throwing objects • No participants experienced physical violence by threatening to use or using a gun, knife, or other weapon • Sexual violence experienced by 5.3% participants |
• After controlling for the confounding effects of age, IPV was associated with education level, occupation, type of marriage and husband’s age • 68.3% of participants were married with arranged marriage, and 31.7% of participants were living with their self-chosen husband • 52.9% of respondents had low family income • 34.6% of the women had no education • 5.3% of participants had no children • 62.8% of women reported that their husband had a drinking habit • 40.2% reported that their husband displayed aggression |
• 29/39 (74.36%) • No justification for the choice of statistical analysis |
| Gosangi et al., 2021 |
• External database • March 11, 2020 to May 3, 2020 • Examined data from the same period for 2019, 2018, and 2017 • Examined referrals to the institutional domestic violence and intervention and prevention program since 1997 |
• USA • Survivors of domestic violence referred to the program (96% female in 2020) |
• Frequency of referrals to the domestic violence intervention and prevention program |
• Decrease in number of survivors seeking hospital care during the pandemic (62 in 2020; 104 in 2019; 106 in 2018; 146 in 2017, p < 0.001) • The incidence of physical IPV and the severity of injuries were greater during the pandemic • The number of survivors of physical abuse was 26/62 (42%) in 2020 compared to 42/342 (12%) in 2017–19 (p = 0.01), • Number of survivors of severe grade injury was (38%) in 2020 compared to 17% from 2017–2019 (p = 0.03) |
• No significant differences in age, gender, or marital status between years • Race (significantly more white people presenting and less African American during COVID-19) • Higher incidence of survivors of high-risk abuse (strangulation, weapons, stab wounds, and burns) |
• 30/39 (76.92%) • No consideration of sample size requirements • Limited justification for the choice of statistical analysis • Single location prevents the results from being generalized to other geographic regions |
| Halford et al., 2020 |
• External database • Crimes recorded between March 8, 2020 and April 2, 2020 are compared to expected rates based on data from 2016 to 2019 • Use of crime data in the UK Police Force over the last 5 years, covering 2000 square miles and around 1.5 million people |
• United Kingdom | • Crime records |
• 1 week after lockdown, domestic abuse decreased 45% compared to an average of the previous 4 years • Declined significantly by over 40 percent one week after lockdown (March 16, 2020), with weekend peaks being less prominent • More likely to reflect a reduction in reporting and recording resulting from social distancing measures |
• Vulnerable children category was captured separately from domestic abuse, and found a decrease, but this was more likely a result of social distancing measures and school closures • Vulnerable child indications as a proportion of all crime also decreased |
• 27/39 (69.23%) • Data collection method did not allow for information about the sample to be reported (i.e., demographic information) • Limited information about validity and reliability of statistical analysis |
| Hamadani et al., 2020 |
• May 19, 2020 to June 18, 2020 • Interrupted time-series (randomly selected a subset of participants from an RCT) |
• Bangladesh • 3016 mothers, of whom N = 2424 agreed to participate |
• IPV questions based on the validated WHO multi-country survey tool addressing emotional, physical, and sexual violence • Single item scale asking whether IPV had changed since the onset of stay-at-home orders |
• Emotional, physical, and sexual violence increased among women experiencing IPV before COVID, with more than half reporting an increase • Of participants reporting emotional abuse, 66.8% reported an increase in insults, 66.0% humiliation, and 68.7% intimidation • 56.3% of participants reported increasing physical violence • 50.8% of participants reported increasing sexual violence |
• n/a |
• 31/39 (79.49%) • Limited consideration of sample size requirements • Limited rational for choice of data collection tools |
| Hassan et al., 2020 |
• External database • March 1st, 2020 through April 11 2020 (examined March 1–21 and then March 22 to April 11) which aligns with initiation of stay at home orders on March 21, 2020 • Chart review performed of all plastic surgery emergencies |
• USA • Patients presenting in the emergency department for trauma consults |
• Hospital records |
• Increase in IPV • In the pre stay at home order period, 2 surgeries were the result of domestic violence (2.3%) compared to 5 surgeries in the period following the order (8.1%) |
• n/a |
• 24/39 (61.54%) • Limited consideration of sample size requirements • Limited rational for choice of data collection tools |
| Iob et al., 2020 |
• External database • March 21, 2020, to April 20, 2020 • Secondary use of data from University College London’s COVID-19 Longitudinal Social Study |
• United Kingdom • N = 44,775 stratified sample of adults age 18 + , with 51% female and 49% male |
• Psychological abuse: experiences of being bullied, controlled, intimidated, or hurt by someone over the past week • Physical abuse: experiences of being harmed physically or hurt over the last week • Both items rated on a 4-point scale from ‘not at all’ to ‘nearly every day |
• No reported data on changes in IPV • Psychological abuse reported by 8.3% of participants (9.4% living alone, 11.7% living with adults other than their partner; 6.8% living with their partner or spouse) • Physical abuse reported by 2.9% of participants (3.7% living alone; 4.8% living with another adult other than their partner; and 2.0% living with their partner or spouse) |
• Having children in the household (9.8% psychological and 3.3% physical) compared to households without (7.8% psychological and 2.8% physical) • Low income • Pre-existing chronic physical illnesses • Mental illness • Unemployment due to disability • Seeking work and unemployed • Overcrowding • A COVID-19 diagnosis |
• 30/39 (76.92%) • Limited consideration of sample size requirements • Limited justification for the choice of statistical analysis |
| Jacob et al., 2020 |
• External database • March and April 2016, 2017, 2018, 2019, and 2020 • Cross sectional study using data from an external database |
• Australia • Single center study at Westmead hospital, which services 1.5 million people • Trends in trauma admissions |
• Hospital records |
• No change in IPV • No significant differences in the number of trauma admissions due to domestic violence |
• n/a |
• 25/39 (64.10%) • Limited rational for choice of data collection tools • Limited justification for the choice of statistical analysis • Single center study |
| Jetelina et al., 2021 |
• 14-day period in April 2020 • Cross sectional online survey |
• USA • N = 2411 participants completed the survey, of which N = 1759 reported having an intimate partner and were included in the analyses |
• Extended- Hurt, Insulted, Threatened, Scream scale (E-HITS) is a 5-item scale to assess the frequency of IPV from 1 = never to 5 = frequent • Five-point Likert scale indicating whether IPV had gotten better or worse since COVID-19 |
• No change in IPV • IPV reported by 18% • Of respondents positive for IPV, 54% stated IPV stayed the same during COVID-19, 17% stated IPV worsened, and 30% stated it improved • The risk of IPV worsening was 4.38 times greater for physical compared to emotional abuse, and 2.31 times higher for sexual abuse compared to other forms of abuse |
• Lower among women (OR = 0.63; 95% CI 0.50 to 0.82) compared to men • Job or income loss due to the pandemic (OR = 1.63; 95% CI 1.17 to 2.27) • Children being present had no significant effect on rates of IPV or severity change in IPV during the COVID-19 pandemic |
• 25/39 (64.10%) • Non-stratified convenience sample with a low response rate of 5.7% |
| Leslie & Wilson, 2020 |
• External database • January 1, 2020, to May 27, 2020, compared with data of the same period in 2019 • Examine police calls for service |
• USA • People calling police for concerns related to domestic violence |
• Crime records |
• Increase in IPV • 7.5% increase in IPV calls for service to the police during March through May of 2020, compared to the same period in 2019 • The increase began over a week before the first stay-at-home order, and the effects were largest during the first five weeks • IPV calls were up 9.7% in first 5 weeks |
• Not driven by any specific demographic group • Households without a history of domestic violence drove the increase |
• 28/39 (71.79) • Limited rational for choice of data collection tools • Limited justification for the choice of statistical analysis |
| Mohler et al., 2020 |
• External database • Baseline period from January 2, 2020, to March 16, 2020, compared to March 20, 2020, to April 18, 2020, in LA, and March 24, 2020, to April 21, 2020, in Indianapolis • Time series of verified crime reports per day and mean calls per day |
• USA • Trends in volume of calls for service related to assaults in Los Angeles and Indianapolis |
• Crime records |
• Increase in IPV • Overall assault calls were unchanged in both locations, but regression of daily calls for service rate against stay-at-home order indicator, when controlling for the day of the week and week of month effects, shows a significant increase in domestic violence in both cities |
• n/a |
• 25/39 (64.10%) • Limited rational for choice of data collection tools • Limited justification for the choice of statistical analysis |
| Murphy et al., 2020 |
• External database • January 2017 to April 26, 2020 • Retrospective access of orthopaedic services use data |
• United Kingdom • People referred to the on-call orthopaedic service at a UK District hospital which provides trauma care to a population of 625,000 people |
• Hospital records |
• No significant differences in referrals during the first 8 weeks of 2020 • During the remainder of COVID-19 there was a significant reduction in overall referrals • Cases of domestic abuse were comparable to previous years |
• n/a |
• 23/29 (58.97%) • Limited rational for choice of data collection tools • Limited justification for the choice of statistical analysis |
| Olding et al., 2021 |
• Existing database • March 23, 2021, to April 29, 2021 • Compared to data from the same period during the previous two years • Prospective data collection and review of past hospital data |
• United Kingdom • Data collected on all patients presenting with traumatic penetrating injuries |
• Hospital records |
• Decrease in IPV • Trauma numbers fell by 35% overall • Two cases of injury due to IPV and four injuries related to IPV more broadly • IPV as a percentage of trauma’s decreased from 2018 (96%) to 2019 (89%) to 2020 (63%) |
• n/a |
• 14/29 (35.90%) • Small sample size, particularly when dividing the sample based on aetiology • Limited justification for the choice of statistical analysis |
| Øverlien, 2020 |
• April 8th, 2020, reminder email April 20th, survey closed April 23rd • Cross sectional online survey |
• Norway • N = 46 Refuges providing services to survivors of domestic abuse • As of 2010, both men and women could seek support and shelter |
• The survey contained 15 items with fixed answers, follow‐up questions and opportunity for the refuges to provide supplement qualitative descriptions and examples |
• No reported data on changes of prevalence of IPV • 56% of clinician respondents reported a decrease in the number of requests from clients • Clinicians commonly reported that it is too quiet, and that survivors are not receiving adequate support |
• 83% of refuge staff reported being most concerned about children (for reasons including IPV and inadequate support in households) • 43% reported that their clients believed the presence of children in the home during the day increased the risk of violence and abuse • 57% of staff said their clients reported the virus control measures and the COVID-19 crisis, were increasing stress for abusers |
• 26/29 (66.67%) • Limited rational for choice of data collection tools • Limited justification for the choice of statistical analysis |
| Pakenham et al., 2020 |
• Unspecified, since COVID-19 • Online survey |
• Italy • N = 1035 Italian citizens at least 18 years of age • 45.4% of the sample was either married or living with a partner, and 54.6% were single, widowed or divorced |
• Twelve COVID-19 risk factors combined to form the COVID-19 lockdown Index (e.g., increase in IPV, COVID-19 diagnosis, duration of lockdown) |
• No change in IPV • The mean domestic violence rating was 1.27, denoting that on average, participants did not report an increase in domestic violence • 5.3% of participants reported a moderate to high increase in domestic violence |
• n/a |
• 29/39 (74.36%) • Lack of clear description of research setting and target population |
| Payne et al., 2020 |
• External database • February 2014 until March 2020 • Autoregressive integrated moving average (ARIMA) modeling was used to compute 6-month ahead forecasts of rates for criminal offenses |
• Australia • Monthly offense rates per 100 000 people in Queensland |
• Crime records |
• Increase in IPV • Domestic violence order breach rate in March 2020 was 57.5 per 100 000 which was higher than the prior month (52.0 per 100 000) • Long term upward trend is likely a reflection of increased orders and not necessarily the number of breaches • Insufficient evidence to suggest breaches increased with COVID-19 |
• Job loss due to COVID-19 • Financial and emotional stress and strain that may not become evident until the future months • Disrupted routine activities |
• 28/39 (71.79) • Limited rational for choice of data collection tools • Limited justification for the choice of statistical analysis |
| Piquero et al., 2020 |
• External database • January 1, 2020 to April 27, 2020 • Examining daily counts of all domestic violence incident reports |
• USA • People filing domestic violence incident reports |
• Crime records |
• No change in IPV • Implementation of the stay-at-home order is not associated with a significant increase in domestic violence incidents • Not enough evidence to suggest an increase in IPV throughout the month after the stay-at-home order |
• n/a |
• 30/39 (76.92%) • Limited information reported within/from the incident reports. (i.e., no demographic information about the abusers or survivors) |
| Rhodes et al., 2020 |
• External database • March 16, 2019 to April 30, 2019 compared with the same time periods in 2020 • Use of data on past emergency department patients presenting at the American College of Surgeons |
• USA • Patients arriving in the emergency department presenting with signs of assault • 2900 patients presented to the ED and 50 patients cause code for assault • Previously 7008 patients with 78 survivors of assault |
• Hospital records |
• Increase in IPV • Significant increase (p = 0.01) in assaults during COVID-19 particularly during the period after school closures • Overall trauma volume reduction • Significant increase in proportion of IPV related admissions • Mechanism of assault was largely penetrating: pierce (2.6% vs 18%) and knife (0% vs 12%) |
• n/a |
• 24/39 (61.54%) • Limited theoretical background provided • Limited justification for the choice of statistical analysis |
| Sabri et al., 2020) |
• Unspecified, prospective data since COVID-19 • Qualitative in-depth interviews conducted via Zoom or phone. Purposive and snowball sampling methods were used to recruit participants |
• USA • 45 in depth interviews conducted with survivors of IPV who spoke English, were over the age of 18, were born outside of USA, and were now living in USA permanently • 17 key-informant healthcare provider interviews were conducted as well |
• Qualitative, in-depth interviews |
• Increase in IPV • Reinforcing relationship between increased stressors and IPV due to COVID-19 • Increased severity and frequency of IPV for immigrant women in abusive relationships • Decrease in clients taking legal steps • Increased stalking and monitoring behaviour and financial abuse • Threatening to infect survivors with COVID-19 |
• Being undocumented (fear makes leaving abuse more difficult) • Increased proximity to abusers • Decreased privacy • Decreased ability of professionals to observe children • Decrease in protective mechanisms (community babysitting) • Fear of job loss and future financial strain • Unable to work or job loss due to additional childcare responsibilities • Closure of typical services and a shift to virtual services with lower access |
• 31/39 (79.49%) • Did not consider research stakeholders in the study design |
| Sediri et al., 2020 |
• April 25, 2020 to May 6, 2020 • Snowball sampling • Cross sectional online survey |
• Tunsia • N = 751 Females at least 18 years of age |
• The history of domestic violence and its types before and during the lockdown were assessed by yes and no questions |
• Increase in IPV • Significant increase in IPV during the lockdown (from 4.4 to 14.8%; p < 0.001) • Psychological abuse was the most frequent type of violence (96%) |
• Violence during lockdown was associated with higher scores in depression, anxiety, and stress • Women who had experienced abuse before the lockdown were at an increased risk of violence during lockdown (p < 0.001; OR = 19.34 [8.71–43.00] • 95% of participants were at no particular risk for COVID-19, 4.2% were under quarantine, and 0.8% tested positive for COVID-19 |
• 24/39 (61.54%) • Non-stratified convenience sample with no data on the total number of people invited to participate |
| Weller et al., 2021 |
• External database • January 2020 to May 17, 2020 • Data from evaluation of services in London and Surrey were analysed anonymously and in aggregate in Excel and STATA |
• United Kingdom • People seeking consultations for domestic violence |
• Aggregate data using Excel and STRATA |
• Increase in IPV • Initial reduction in the percentage of consultations (decreasing from 66% between March 9th and 22nd 2020 to 52% between March 23rd, 2020, and April 4th, 2020) • Increase was recorded in the percentage of IPV disclosures during lockdown (April 6th, 2020, to April 17th, 2020), compared with the 6 weeks prior to lockdown (February 10th 2020 to March 22nd 2020) with an increase from 0.22% (CI 0.14% to 0.32%) to 0.57% (CI 0.33% to 0.91%) (p = 0.002) |
• n/a |
• 15/39 (38.46%) • Limited theoretical background provided • Limited justification for the choice of data collection tools and statistical analysis |
Funding
Support for this project came from the Social Sciences and Humanities Research Council and Canada Research Chairs program (#950–232347).
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Aliya McNeil, Email: am4mcnei@uwaterloo.ca.
Lydia Hicks, Email: l3hicks@uwaterloo.ca.
Busra Yalcinoz-Ucan, Email: busra.yalcinoz@uwaterloo.ca.
Dillon T. Browne, Email: Dillon.browne@uwaterloo.ca
References
* Indicates that the article was included as one of the 24 reviewed articles
- *Agüero, J. M. (2021). COVID-19 and the rise of intimate partner violence. World development, 137. 10.1016/j.worlddev.2020.105217. [DOI] [PMC free article] [PubMed]
- Bair-Merritt MH, Holmes WC, Holmes JH, Feinstein J, Feudtner C. Does intimate partner violence epidemiology differ between homes with and without children? A population-based study of annual prevalence and associated risk factors. Journal of Family Violence. 2008;23(5):325–332. doi: 10.1007/s10896-008-9154-y. [DOI] [Google Scholar]
- Bentley R, Baker E, Mason K, Subramanian SV, Kavanagh AM. Association between housing affordability and mental health: A longitudinal analysis of a nationally representative household survey in Australia. American Journal of Epidemiology. 2011;174(7):753–760. doi: 10.1093/aje/kwr161. [DOI] [PubMed] [Google Scholar]
- *Blackhall, K. K., Downie, I. P., Ramchandani, P., Kusanale, A., Walsh, S., Srinivasan, B., ... & Singh, R. P. (2020). Provision of Emergency Maxillofacial Service During the COVID-19 Pandemic: A Collaborative Five Centre UK Study. British Journal of Oral and Maxillofacial Surgery, 58(6), 698-703. 10.1016/j.bjoms.2020.05.020. [DOI] [PMC free article] [PubMed]
- Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. The American Journal of Emergency Medicine. 2020;38(12):2753–2755. doi: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L. We’re not all in this together: On covid-19, intersectionality, and structural inequality. American Journal of Public Health. 2020;110(7):917–917. doi: 10.2105/AJPH.2020.305766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bracewell, K., Hargreaves, P., & Stanley, N. (2020). The consequences of the COVID-19 lockdown on stalking victimisation. Journal of family violence, 1-7. 10.1007/s10896-020-00201-0. [DOI] [PMC free article] [PubMed]
- Bradbury-Jones C, Isham L. The pandemic paradox: The consequences of COVID-19 on domestic violence. The International Journal of Clinical Nursing. 2020;29(13):2047–2049. doi: 10.1111/jocn.15296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiding, M., Basile, K. C., Smith, S. G., Black, M. C., & Mahendra, R. R. (2015). Intimate partner violence surveillance: Uniform definitions and recommended data elements. Version 2.0. Atlanta (GA): National Centre for Injury Prevention and Control, Centre for Disease Control and Prevention.
- Brink, J., Cullen, P., Beek, K., & Peters, S. A. (2021). Intimate partner violence during the COVID-19 pandemic in Western and Southern European countries. European Journal of Public Health, 31(5), 1058–1063. 10.1093/eurpub/ckab093 [DOI] [PMC free article] [PubMed]
- Brown, S. M., Doom, J. R., Lechuga-Peña, S., Watamura, S. E., & Koppels, T. (2020). Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect, 110(2).10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed]
- Cao J, Lee CY, Liu X, Gonzalez-Guarda RM. Risk and protective factors associated with intimate partner violence against Chinese women: A systematic review. Trauma, Violence, & Abuse. 2021 doi: 10.1177/15248380211030235. [DOI] [PubMed] [Google Scholar]
- *Davis, M., Gilbar, O., & Padilla-Medina, D. (2020). Intimate Partner Violence Victimization and Perpetration among US Adults during COVID-19: A Brief Report. medRxiv. 10.1101/2020.06.08.20125914. [DOI] [PubMed]
- Evans SE, Davies C, DiLillo D. Exposure to domestic violence: A meta-analysis of child and adolescent outcomes. Aggression and Violent Behavior. 2008;13(2):131–140. doi: 10.1016/j.avb.2008.02.005. [DOI] [Google Scholar]
- Fernbrant, C., Emmelin, M., Essén, B., Östergren, P. O., & Cantor-Graae, E. (2014). Intimate partner violence and poor mental health among Thai women residing in Sweden. Global health action, 7(1). 10.3402/gha.v7.24991 [DOI] [PMC free article] [PubMed]
- *Gebrewahd, G. T., Gebremeskel, G. G., & Tadesse, D. B. (2020). Intimate partner violence against reproductive age women during COVID-19 pandemic in northern Ethiopia 2020: a community-based cross-sectional study. Reproductive health, 17(1), 1–8. 10.1186/s12978-020-01002-w. [DOI] [PMC free article] [PubMed]
- *Gosangi, B., Park, H., Thomas, R., Gujrathi, R., Bay, C. P., Raja, A. S., ... & Harris, M. B. (2021). Exacerbation of physical intimate partner violence during COVID-19 lockdown. Radiology, 298(1), 38–45. 10.1148/radiol.2020202866. [DOI] [PMC free article] [PubMed]
- *Halford, E., Dixon, A., Farrel, G., Malleson, N., & Tilley, N. (2020). Crime and coronavirus: Social distancing, lockdown, and the mobility elasticity of crime. Crime Science, 9(1), 1–12. 10.1186/s40163-020-00121-w. [DOI] [PMC free article] [PubMed]
- *Hamadani, J. D., Hasan, M. I., Baldi, A. J., Hossain, S. J., Shiraji, S., Bhuiyan, M. S. A., ... & Pasricha, S. R. (2020). Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. The Lancet Global Health, 8(11), 1380–1389. 10.1016/S2214-109X(20)30366-1 [DOI] [PMC free article] [PubMed]
- Haug, N., Geyrhofer, L., Londei, A., Dervic, E., Desvars-Larrive, A., Loreto, V., ... & Klimek, P. (2020). Ranking the effectiveness of worldwide COVID-19 government interventions. Nature human behaviour, 4(12), 1303–1312. 10.1038/s41562-020-01009-0 [DOI] [PubMed]
- Harrison R, Jones B, Gardener P, Lawton R. Quality assessment with diverse studies (QuADS): An appraisal tool for methodological and reporting quality in systematic reviews of mixed-or multi-method studies. BMC Health Services Research. 2021;21(1):1–20. doi: 10.1186/s12913-021-06122-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hassan, K., Prescher, H., Wang, F., Chang, D. W., & Reid, R. R. (2020). Evaluating the effects of COVID-19 on plastic surgery emergencies: protocols and analysis from a Level I trauma center. Annals of Plastic Surgery. 10.1097/sap.0000000000002459. [DOI] [PMC free article] [PubMed]
- Hiraoka D, Tomoda A. Relationship between parenting stress and school closures due to the COVID-19 pandemic. Psychiatry and Clinical Neurosciences. 2020;74(9):497–498. doi: 10.1111/pcn.13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell KH, Thurston IB, Schwartz LE, Jamison LE, Hasselle AJ. Protective factors associated with resilience in women exposed to intimate partner violence. Psychology of Violence. 2018;8(4):438–447. doi: 10.1037/vio0000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics. 2020;32(10):1217–1220. doi: 10.1017/S1041610220000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ILO. (2020). Almost 25 million jobs could be lost worldwide as a result of COVID-19. Retrieved March 18, 2022, fromhttps://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_738742/lang--en/index.htm
- *Iob, E., Steptoe, A., & Fancourt, D. (2020). Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. The British Journal of Psychiatry, 217(4), 543–546. 10.1192/bjp.2020.130. [DOI] [PMC free article] [PubMed]
- Jacob S, Mwagiru D, Thakur I, Moghadam A, Oh T, Hsu J. Impact of societal restrictions and lockdown on trauma admissions during the COVID-19 pandemic: A single-centre cross-sectional observational study. ANZ Journal of Surgery. 2020;90(11):2227–2231. doi: 10.1111/ans.16307. [DOI] [PubMed] [Google Scholar]
- *Jetelina, K. K., Knell, G., & Molsberry, R. J. (2021). Changes in intimate partner violence during the early stages of the COVID-19 pandemic in the USA. Injury Prevention, 27(1), 93-97. 10.1136/injuryprev-2020-043831. [DOI] [PubMed]
- Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Network Open. 2021;4(1):2036462. doi: 10.1001/jamanetworkopen.2020.36462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim C. Social isolation, acculturative stress and intimate partner violence (IPV) victimization among Korean immigrant women. International Journal of Intercultural Relations. 2019;72:87–95. doi: 10.1016/j.ijintrel.2019.07.005. [DOI] [Google Scholar]
- Krishnamurti, T., Davis, A. L., Quinn, B., Castillo, A. F., Martin, K. L., & Simhan, H. N. (2021). Mobile remote monitoring of intimate partner violence among pregnant patients during the COVID-19 shelter-in-place order: quality improvement pilot study. Journal of medical Internet research, 23(2). 10.2196/22790. [DOI] [PMC free article] [PubMed]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Leslie, E., & Wilson, R. (2020). Sheltering in place and domestic violence: Evidence from calls for service during COVID-19. Journal of Public Economics, 189, 104241. 10.1016/j.jpubeco.2020.104241 [DOI] [PMC free article] [PubMed]
- Lucero JL, Lim S, Santiago AM. Changes in economic hardship and intimate partner violence: A family stress framework. Journal of Family and Economic Issues. 2016;37(3):395–406. doi: 10.1007/s10834-016-9488-1. [DOI] [Google Scholar]
- McLennan JD, MacMillan HL. Routine primary care screening for intimate partner violence and other adverse psychosocial exposures: What’s the evidence? BMC Family Practice. 2016;17(1):1–4. doi: 10.1186/s12875-016-0500-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill, K. A., William, T., Joyce, K. M., Roos, L. E., & Protudjer, J. (2021). Potential psychosocial impact of COVID-19 on children: A scoping review of pandemics & epidemics. Journal of Global Health Reports, 4. 10.29392/001c.18229
- Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., ... & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews, 4(1), 1-9. doi:10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed]
- *Mohler, G., Bertozzi, A. L., Carter, J., Short, M. B., Sledge, D., Tita, G. E., ... & Brantingham, P. J. (2020). Impact of social distancing during COVID-19 pandemic on crime in Los Angeles and Indianapolis. Journal of Criminal Justice, 68.10.1016/j.jcrimjus.2020.101692. [DOI] [PMC free article] [PubMed]
- Mojahed A, Brym S, Hense H, Grafe B, Helfferich C, Lindert J, Garthus-Niegel S. Rapid review on the associations of social and geographical isolation and intimate partner violence: Implications for the ongoing CoViD-19 pandemic. Frontiers in Psychiatry. 2021;12:486. doi: 10.3389/fpsyt.2021.578150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Murphy, T., Akehurst, H., & Mutimer, J. (2020). Impact of the 2020 COVID-19 pandemic on the workload of the orthopaedic service in a busy UK district general hospital. Injury, 51(10), 2142–2147. 10.1016/j.injury.2020.07.001 [DOI] [PMC free article] [PubMed]
- National Institute of Justice. (2009). Economic distress and intimate partner violence. Retrieved March 18, 2022, from https://nij.ojp.gov/topics/articles/economic-distress-and-intimate-partner-violence
- Nourazari S, Davis SR, Granovsky R, Austin R, Straff DJ, Joseph JW, Sanchez LD. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. The American Journal of Emergency Medicine. 2021;42:203–210. doi: 10.1016/j.ajem.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Olding, J., Zisman, S., Olding, C., & Fan, K. (2021). Penetrating trauma during a global pandemic: changing patterns in interpersonal violence, self-harm, and domestic violence in the Covid-19 outbreak. The Surgeon, 19(1), 9–13. 10.1016/j.surge.2020.07.004 [DOI] [PMC free article] [PubMed]
- Onyeaka, H., Anumudu, C. K., Al-Sharify, Z. T., Egele-Godswill, E., & Mbaegbu, P. (2021). COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Science Progress, 104(2). 10.1177/00368504211019854 [DOI] [PMC free article] [PubMed]
- *Øverlien, C. (2020). The COVID‐19 pandemic and its impact on children in domestic violence refuges. Child Abuse Review (Chichester, England: 1992). 10.1002/car/2650. [DOI] [PMC free article] [PubMed]
- *Pakenham, K. I., Landi, G., Boccolini, G., Furlani, A., Grandi, S., & Tossani, E. (2020). The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science, 17, 109–118. 10.1016/j.jcbs.2020.07.003. [DOI] [PMC free article] [PubMed]
- Patel, J. A., Nielsen, F. B. H., Badiani, A. A., Assi, S., Unadkat, V. A., Patel, B., ... & Wardle, H. (2020). Poverty, inequality and COVID-19: the forgotten vulnerable. Public health, 183, 110–111. 10.1016/j.puhe.2020.05.006. [DOI] [PMC free article] [PubMed]
- *Payne, J., Morgan, A., & Piquero, A. R. (2020). Covid-19 and social distancing measures in queensland australia are associated with short-term decreases in recorded violent crime. Journal of Experimental Criminology, 1–25. 10.1007/s11292-020-09441-y. [DOI] [PMC free article] [PubMed]
- Peek-Asa, C., Saftlas, A. F., Wallis, A. B., Harland, K., & Dickey, P. (2017). Presence of children in the home and intimate partner violence among women seeking elective pregnancy termination. PLoS one, 12(10). 10.1371/journal.pone.0186389 [DOI] [PMC free article] [PubMed]
- Peralta RL, Fleming MF. Screening for intimate partner violence in a primary care setting: The validity of “feeling safe at home” and prevalence results. The Journal of the American Board of Family Practice. 2003;16(6):525–532. doi: 10.3122/jabfm.16.6.525. [DOI] [PubMed] [Google Scholar]
- Pingley, T. (2017). The impact of witnessing domestic violence on children: A systematic review. Social Work Clinical Research Papers. Retrieved March 18, 2022, from https://ir.stthomas.edu/ssw_mstrp/773.
- *Piquero, A. R., Riddell, J. R., Bishopp, S. A., Narvey, C., Reid, J. A., & Piquero, N. L. (2020). Staying Home, Staying Safe? A Short-Term Analysis of COVID-19 on Dallas Domestic Violence. American Journal of Criminal Justice, 45(4), 601-635. 10.1007/s12103-020-09531-7 [DOI] [PMC free article] [PubMed]
- Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Rodgers, M., ... & Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version, 1, b92. 10.13140/2.1.1018.4643.
- Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist. 2020;75(9):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Ragavan, M. I., Garcia, R., Berger, R. P., & Miller, E. (2020). Supporting intimate partnerviolence survivors and their children during the COVID-19 pandemic. Pediatrics, 146(3). 10.1542/peds.2020-1276. [DOI] [PMC free article] [PubMed]
- Rempel E, Donelle L, Hall J, Rodger S. Intimate partner violence: A review of online interventions. Informatics for Health and Social Care. 2019;44(2):204–219. doi: 10.1080/17538157.2018.1433675. [DOI] [PubMed] [Google Scholar]
- Renzetti, C. M., & Larkin, V. M. (2009). Economic stress and domestic violence. VAWNet: National Resource Center on Domestic Violence. Retrieved March 18, 2022, from https://vawnet.org
- *Rhodes, H. X., Petersen, K., Lunsford, L., & Biswas, S. (2020). COVID-19 resilience for survival: occurrence of domestic violence during lockdown at a rural American college of surgeons verified level one trauma center. Cureus, 12(8). 10.7759/cureus.10059 [DOI] [PMC free article] [PubMed]
- *Sabri, B., Hartley, M., Saha, J., Murray, S., Glass, N., & Campbell, J. C. (2020). Effect of COVID-19 pandemic on women’s health and safety: A study of immigrant survivors of intimate partner violence. Health Care for Women International, 41(11-12), 1294–1312. 10.1080/07399332.2020.1833012 [DOI] [PMC free article] [PubMed]
- Schneider D, Harknett K, McLanahan S. Intimate partner violence in the great recession. Demography. 2016;53(2):471–505. doi: 10.1007/s13524-016-0462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Sediri, S., Zgueb, Y., Ouanes, S., Ouali, U., Bourgou, S., Jomli, R., & Nacef, F. (2020). Women’s mental health: acute impact of COVID-19 pandemic on domestic violence. Archives of women's mental health, 23(6), 749–756. 10.1007/s00737-020-01082-4. [DOI] [PMC free article] [PubMed]
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: The development and evaluation of a new tool. Journal of Evaluation in Clinical Practice. 2012;18(4):746–752. doi: 10.1111/j.1365-2753.2011.01662.x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2020). Covid-19 and job displacement: thinking about the longer term. Retrieved March 18, 2022, from https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00030-eng.htm
- Tricco, A. C., Langlois, E., Straus, S. E., & World Health Organization. (2017). Rapid reviews to strengthen health policy and systems: a practical guide. World Health Organization.
- United Nations. (2015). Transforming our world: the 2030 agenda for sustainable development. Retrieved March 18, 2022, from https://sdgs.un.org/2030agenda
- Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: Increased vulnerability and reduced options for support. International Journal of Mental Health Nursing. 2020;29:549–552. doi: 10.1111/inm.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster P. Virtual health care in the era of COVID-19. The Lancet. 2020;395(10231):1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman A, Behrman JA. Disaster, disruption to family life, and intimate partner violence: The case of the 2010 earthquake in Haiti. Sociological Science. 2016;3:167–189. doi: 10.15195/v3.a9. [DOI] [Google Scholar]
- *Weller, S. J., Tippetts, D., Weston, D., Aldridge, R. W., & Ashby, J. (2021). Increase in reported domestic abuse in Integrated Sexual Health (ISH) services in London and Surrey during COVID-19 ‘lockdown’: successful application of national guidance on routine enquiry during rapid transition to remote telephone consultation (telemedicine). Sexually Transmitted Infections, 97(3), 245-246. doi:10.1136/sextrans-2020-05472. [DOI] [PubMed]
- World Health Organization. (2020). WHO director-general’s opening remarks at the media briefing on COVID-19 11 March 2020. Retrieved March 18, 2022, from https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- World Health Organization. (2013). Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Retrieved March 18, 2022, from https://apps.who.int/iris/bitstream/handle/10665/85239/?sequence=1
- World Health Organization. (n.d.). WHO coronavirus (COVID-19) dashboard. Retrieved March 18, 2022, from https://covid19.who.int
- Yakubovich AR, Stöckl H, Murray J, Melendez-Torres GJ, Steinert JI, Glavin CE, Humphreys DK. Risk and protective factors for intimate partner violence against women: Systematic review and meta-analyses of prospective–longitudinal studies. American Journal of Public Health. 2018;108(7):1–11. doi: 10.2105/AJPH.2018.304428. [DOI] [PMC free article] [PubMed] [Google Scholar]