Abstract
Objectives
To develop and validate a short form of the Male Depression Risk Scale (MDRS-22) for use in primary care, examining associations with prototypic depression symptoms, psychological distress and suicidality.
Design
Cross-sectional study with 8-month follow-up.
Setting
Community-based.
Participants
A community sample of younger (n=510; 18–64 years) and older (n=439; 65–93 years) men residing in Australia (M age=58.09 years, SD=17.77) participated in the study. A subset of respondents (n=159 younger men; n=169 older men) provided follow-up data approximately eight months later.
Primary and secondary outcome measures
Quantitative data were obtained through a survey comprising a range of validated measures, including the MDRS-22, the Patient Health Questionnaire (PHQ-9) and the Kessler Psychological Distress Scale (K10). The MDRS-22 was refined using exploratory and confirmatory factor analysis in line with best practice guidelines. Analysis of variance and generalised linear models were conducted to explore relationships between variables.
Results
The short-form MDRS consisted of seven items (MDRS-7) and captured all of the domains in the original tool. Participants with mixed symptoms (PHQ-9 ≥ 10 and MDRS-7 > 5) had significantly higher risk of mental illness (K10 ≥ 25) and current suicidality (PHQ-9 item 9 ≥ 1) than those with exclusively prototypic symptoms (PHQ-9 ≥ 10 and MDRS-7 ≤ 5). Furthermore, the MDRS-7 was shown to be effective at predicting elevated symptoms of depression at follow-up, after controlling for previous depression diagnosis.
Conclusions
Findings provide preliminary evidence of the potential utility of the MDRS-7 as a screening tool for externalised and male-type symptoms associated with major depression in men. Field trials of the MDRS-7 in primary care settings may facilitate identification of men at risk of suicide and psychological distress who do not meet cut-off scores for existing measures of major depression symptoms.
Keywords: depression, externalising symptoms, short form, men, lifespan, help-seeking
Strengths and limitations of this study.
This is the first study to explore the psychometric properties of the Male Depression Risk Scale (MDRS-7) as a screening tool for externalised and male-type symptoms associated with major depression in men.
Use of the MDRS-7 in primary care settings may facilitate identification of men at risk of suicide and psychological distress.
Diagnosis of depression was not verified by clinical interview.
Field trials of the MDRS-7 are needed to demonstrate the utility of the tool in primary care settings.
Introduction
Major depressive disorder (MDD) is a common psychiatric condition and the leading cause of disability worldwide.1 2 MDD is twice as prevalent in women than men,3 and severe depression is known to significantly increase risk of suicide.4 Although men are less likely to be diagnosed with a depressive disorder,5 they are three times more likely to die by suicide compared with women.6 Current approaches to the diagnosis of depression (eg, as per International Classification of Diseases 11th Revision [ICD-11] or Diagnostic and Statistical Manual of Mental Disorders 5th Edition [DSM-5] criteria) emphasise symptoms including persistent sadness, loss of interest or pleasure in previously enjoyable activities, as well as changes in affect, cognition and neurovegetative functioning.7 8 However, a growing number of studies suggest that a significant proportion of men suffering from depression might experience a distinct phenotype.9–11 Congruent with masculine role norms, this male-typical phenotype includes anger, substance misuse, emotion suppression and risk-taking domains.10 12 However, these putative symptoms are not currently included in standard diagnostic criteria or screening measures, and it has been suggested that this might account in part for the underdiagnosis of male depression cases, and therefore under-recognition of (and treatment for) men at heightened risk of suicide.13
While men are often regarded as being less likely to seek help than women, recent statistics largely do not support this claim. In Australia, around 89% of men attend primary care annually.14 Among men experiencing mental health difficulties, annual primary care attendance is similarly high with estimates of 80%–96% of men with symptoms of depression reporting a visit to primary care within the previous 12 months.15 16 Similarly, findings from the UK demonstrate that although men are overall less likely to attend primary care compared with women, attendance rates in men and women with comparable underlying morbidities, including depression, are similar.17 Furthermore, findings from a population study of healthcare contacts among Canadian suicide decedents demonstrated that over 60% (n=1792) of men who died by suicide accessed professional mental healthcare in the year before their death.18 These findings highlight the essential role of primary care physicians in identifying depression and suicide risk in men in order to facilitate effective treatment.19
Growing interest in gender-sensitive assessment of men’s depression has seen the development of male-specific screening tools to identify symptoms that align with men’s socialisation and gender norm processes (eg, Brownhill et al,20 Zierau et al,21 Magovcevic and Addis22). One recently developed and widely validated measure for assessing externalising and male-type symptoms in men is the Male Depression Risk Scale (MDRS-22).23 The MDRS-22 consists of 22 items assessing six symptom domains including emotion suppression, drug use, alcohol use, anger and aggression, somatic symptoms and risk-taking.23 Recently, Zajac and colleagues24 demonstrated that this tool, used in conjunction with a measure of prototypic depression symptoms (PHQ-9), was able to stratify men into three distinct risk groups: (1) prototypic symptoms (consistent with current MDD diagnostic criteria), (2) externalising symptoms consistent with masculine socialisation and (3) mixed depressive symptoms, reflecting both internalised (i.e., prototypic) and externalised symptomology. Further analyses showed that men in the externalising only group—men who are arguably missed when using measures of internalising symptoms—were at significantly increased risk of suicide compared with non-depressed men. Moreover, those with elevated externalised and prototypic symptomology were at highest risk of mental illness as well as suicide,24 highlighting the potential early identification and intervention benefits of leveraging male-specific tools in primary care settings.
Two-stage screening methods are commonly used in primary care and have been shown to be effective for increasing the recognition of depression.25 However, many primary care physicians report that time is a limiting factor in their capacity to comprehensively assess psychological issues, including depression,19 26 despite management of common mental disorders rating as a top reason for general practice attendance.27 To help address this issue, brief screening tools consisting of 15 items or less are often used, given their completion time is usually just a couple of minutes.28 Examples include the PHQ-9,29 the Kessler Psychological Distress Scale (K10)30 and the Beck Depression Inventory for Primary Care (BDI-PC).31
To date, the MDRS-22 has demonstrated excellent psychometric properties as well as the ability to detect different groups of men who may be at increased risk of suicide and mental illness (eg, Zajac et al,24 Rice et al,32 Rice et al33). However, given time constraints in primary care settings, the length of the current MDRS-22 is arguably impractical.12 The purpose of the present study was to develop a short form of the MDRS-22 to facilitate its use as a screening tool in busy and time-pressured healthcare settings. We also aimed to establish an initial set of cut-off scores for interpretive purposes. If the MDRS short form is to have clinical utility, it needs to be able to identify broader aspects of psychopathology. Thus, a secondary aim was to explore current and longitudinal risk of suicidality and mental illness by adopting a previously utilised categorisation according to cut-off scores on the MDRS and the widely used PHQ-9, which assesses prototypic depression symptoms.24 Furthermore, as adherence to masculine gender norms has been found to decline as men get older,34 younger and older men were examined separately to examine the utility of the tool across age groups.
Method
Participants and procedure
This cross-sectional study included baseline data from a community sample of 510 younger men aged 18–64 years (M=45.43, SD=14.56) and 439 older men aged 65–93 years (M=72.79, SD=5.88). A subset of respondents (n=159 younger men; n=169 older men) participated in the follow-up component. On average, 35 weeks (M=248.56 days, SD=24.59 days) elapsed between the provision of time 1 and time 2. The mean age for the overall sample was 58.09 years (SD=17.77). Eligible participants were Australian male residents over the age of 18 years who considered themselves fluent in English. Participants were recruited via paid advertisements displayed to Australian members of the Facebook social networking site (n=601; 63.3%) and through promotion of the study to community organisations (eg, Rotary, Men’s Shed). Time 1 data were collected between August and November 2019 using an online questionnaire. However, participants from local community organisations were provided with the option to complete a paper version of the survey to ensure inclusivity and accessibility of the sample and n=5 participants completed a paper version. Ethics approval was obtained from the University of Adelaide Human Research Ethics Committee and the CSIRO Health and Medical Human Research Ethics Committee (approval number H-2019-109). All participants provided informed consent. Reporting adhered to the STROBE cross-sectional guidelines. Table 1 presents a summary of the characteristics of the study participants at time 1 and time 2.
Table 1.
Sociodemographic characteristics of participants
| Variable | Younger men (<65 years) | Older men (≥65 years) | ||
| Time 1 (n=510) | Time 2 (n=159) | Time 1 (n=439) | Time 2 (n=169) | |
| Age range (years) | 18–64 | 65–93 | ||
| Age, M (SD) | 45.43 (14.56) | 72.79 (5.88) | ||
| Relationship status, n (%) | ||||
| Single (never married) | 118 (23.1) | 27 (17.0) | 12 (2.7) | 6 (3.6) |
| Widowed/divorced/separated | 68 (13.3) | 19 (11.9) | 92 (21.0) | 44 (26.0) |
| Married/de facto | 322 (63.1) | 113 (71.1) | 332 (75.6) | 119 (70.4) |
| Prefer not to say | 2 (0.4) | 0 (0.0) | 3 (0.7) | 0 (0.0) |
| Employment status, n (%) | ||||
| Employed full-time | 227 (44.5) | 66 (41.5) | 22 (5.0) | 5 (3.0) |
| Employed part-time | 37 (7.3) | 11 (6.9) | 18 (4.1) | 4 (2.4) |
| Employed casually | 67 (13.1) | 19 (11.9) | 14 (3.2) | 5 (3.0) |
| Not employed or unpaid work | 94 (18.4) | 24 (15.1) | 13 (3.0) | 7 (4.1) |
| Retired | 73 (14.3) | 39 (24.5) | 370 (84.3) | 148 (87.6) |
| Prefer not to say | 12 (2.4) | 0 (0.0) | 2 (0.5) | 0 (0.0) |
| Household income, n (%) | ||||
| <$A35 000 | 136 (26.7) | 28 (17.6) | 141 (32.1) | 51 (30.2) |
| $A35 000–$A65 000 | 91 (17.8) | 32 (20.1) | 156 (35.5) | 55 (32.5) |
| $A65 000–$A105 000 | 100 (19.6) | 44 (27.7) | 80 (18.2) | 29 (17.2) |
| $A105 000–$A160 000 | 97 (19.0) | 26 (16.4) | 31 (7.1) | 15 (8.9) |
| >$A160 000 | 65 (12.7) | 20 (12.6) | 12 (2.7) | 4 (2.4) |
| Prefer not to say | 21 (4.1) | 9 (5.7) | 19 (4.3) | 15 (8.9) |
| Highest level of education, n (%) | ||||
| Year 11 or below | 49 (9.6) | 11 (6.9) | 81 (18.5) | 23 (13.6) |
| Year 12 | 52 (10.2) | 10 (6.3) | 48 (10.9) | 17 (10.1) |
| Certificate/diploma | 154 (30.2) | 55 (34.6) | 133 (30.3) | 50 (29.6) |
| Bachelor’s degree | 139 (27.3) | 44 (27.7) | 74 (16.9) | 34 (20.1) |
| Graduate certificate/diploma | 43 (8.4) | 15 (9.4) | 39 (8.9) | 20 (11.8) |
| Postgraduate degree | 72 (14.1) | 23 (14.5) | 56 (12.8) | 22 (13.0) |
| Prefer not to say | 1 (0.2) | 1 (0.6) | 8 (1.8) | 3 (1.8) |
Percentage may not equal 100% due to rounding.
¹ Houshold income reflects Australian Dollars.
Public involvement
Participants were not involved in the design or conduct of this research; however, participants could nominate to receive updates on the results of the study.
Measures
Demographics
Participants reported their age, gender, relationship status, employment status, level of education and household income. They also reported whether they had previously been diagnosed with depression.
Male Depression Risk Scale (MDRS-22)
Externalising and male-type depression symptoms were assessed by the MDRS-22.23 The MDRS-22 contains 22 self-report items designed to assess six broad domains of externalising and male-type depression symptoms present in the last month including anger and aggression, drug use, alcohol use, emotion suppression, risk-taking and somatic symptoms using the condensed five-point Likert scale response format ranging from 0 (none of the time) to 4 (all of the time). Cronbach’s alphas for the MDRS are reported in table 2 for both age groups and for the overall sample and are considered adequate.
Table 2.
Item loadings derived from exploratory factor analysis (maximum likelihood estimation)
| Domains | Items | 18–64 | 65+ | Overall | Time 2 |
| Emotion suppression | I bottled up my negative feelings | 0.67 | 0.72 | 0.71 | 0.68 |
| Alcohol use | I needed alcohol to help me unwind | 0.44 | 0.45 | 0.48 | 0.37 |
| Somatic symptoms | I had unexplained aches and pains | 0.56 | 0.59 | 0.58 | 0.63 |
| Aggression | I overreacted to situations with aggressive behaviour | 0.69 | 0.74 | 0.71 | 0.30 |
| Anger | It was difficult to manage my anger | 0.75 | 0.74 | 0.75 | 0.65 |
| Drug use | Using drugs provided temporary relief | 0.36 | 0.44 | 0.42 | 0.44 |
| Risk-taking | I stopped caring about the consequences of my actions | 0.63 | 0.62 | 0.65 | 0.80 |
| Eigenvalue | 2.52 | 2.74 | 2.72 | ||
| Variance explained (%) | 36.04 | 39.08 | 38.82 | ||
| Cronbach’s alpha | 0.68 | 0.71 | 0.72 | ||
| Correlation with MDRS-22 | 0.94 | 0.94 | 0.94 | ||
| Short form re-test reliability | 0.72 | 0.69 | 0.71 | ||
| M (SD) | 5.93 (4.04) | 3.57 (3.39) | 4.84 (3.93) |
Note: Time 2 loadings derived using confirmatory factor analysis in the combined sample.
All correlations were significant at p<0.001.
The Patient Health Questionnaire (PHQ-9)
The PHQ-929 is a self-report depression screening tool for use in primary care that assesses nine symptoms consistent with the DSM-5 diagnostic criteria for MDD.7 Participants endorse how often they have experienced each symptom (eg, ‘Feeling down, depressed, or hopeless’) during the preceding 2-week period using a four-point Likert scale ranging from 0 (not at all) to 3 (almost every day). A score of 10 and above is indicative of clinically significant depressive symptoms.35 In addition to utilising total PHQ-9 scores, we used item 9 as a measure of suicidality: ‘Over the past two weeks, how often have you been bothered by thoughts that you would be better off dead, or of hurting yourself in some way?’ We deemed those who scored 1 or more on this item to be currently experiencing suicidal ideation. Internal consistency of the PHQ-9 in the present study for the overall sample was high (α=0.93).
Kessler Psychological Distress Scale (K10)
The Kessler Psychological Distress Scale (K10)30 is a widely used measure in both research and primary care settings.36 It comprises 10 questions assessing a person’s negative emotional state in the preceding 30 days (eg, ‘About how often did you feel so nervous that nothing could calm you down’). Responses are based on a five-point Likert scale ranging from 1 (none of the time) to 5 (all of the time). In addition to examining K10 total scores, we created a binary variable with scores ≥25 indicating probable mental illness, consistent with published cut-off scores for the K10.37 Internal consistency of the K10 in this study for the overall sample was high (α=0.95).
Analytic sample
A total of 1114 participants commenced the study. However, 156 participants were not included in the analyses due to substantial missing data. Thus, N=949 participants who provided complete data for the items comprising the MDRS-22 were included in the item reduction process described below. Of this sample, n=29 did not provide complete data for the PHQ-9 or K10 items. Thus, models using these variables comprised n=920 participants.
Statistical analyses
Data for the present study were analysed using IBM SPSS Statistics (V.26.0) except for the confirmatory factor analysis (CFA) undertaken in JASP (V.0.13.138). Various recommendations exist for the selection of items for short-form surveys including both Rasch analysis39 and descriptive approaches.40 41 Broadly speaking, the focus is on selecting items with maximum variability and which retain the theorised underlying construct—as well as subdomains—measured by the long-form scale. Therefore, we calculated descriptive (means, SD and skewness) and relational statistics (correlations) for each item (see online supplemental file 1). Items were then scored based on each statistic within its corresponding domain (ie, largest SD, strongest correlation) and summed across the different descriptive indices to derive a total performance score for each item. Parallel analysis consisting of 1000 permutations of the original raw data was used to determine thresholds for retaining factors. Exploratory factor analysis of the best performing items was performed with maximum likelihood estimation within each age group and in the combined sample. Stability of this solution was then established using CFA of time 2 data (n=328). Fit indices reported include: comparative fit index (CFI); the Tucker-Lewis index (TLI); the root mean square error of approximation (RMSEA) and the standardised root mean residual (SRMR). Interpretation of these indices were guided by the recommendations of Hu and Bentler.42
bmjopen-2021-053650supp001.pdf (142.8KB, pdf)
In order to investigate the clinical utility of the reduced item scale, cut-off scores were determined for low (0–5), moderate (6–7), severe (8–12) and extremely severe (13+) symptom severity groups. The corresponding cumulative percentiles (cum%) at the upper boundaries of these categories were: low (cum%=63.5), moderate (cum%=77.5), severe (cum%=95.5), extremely severe (cum%=100.0). These category scores were determined using previously reported cumulative percentiles that represented differing degrees of increased risk of recent suicide attempt for the MDRS-22.33 A 2×2 analysis of variance was conducted to explore the effect of age group differences and MDRS-7 symptom categories on prototypic depression (PHQ-9) and psychological distress (K10). We classified individuals into depression groups using the MDRS-7 in combination with the PHQ-9 based on previous research24 with groups referred to as: not depressed (PHQ-9 < 10 and MDRS-7 ≤ 5), prototypic depression features (PHQ-9 ≥ 10 and MDRS-7≤ 5), mixed features (PHQ-9 ≥ 10 and MDRS-7 > 5) and externalising and male-type features (PHQ-9 < 10 and MDRS-7 > 5). In addition, we used the K10 to determine those individuals suffering a moderate mental illness (K10 ≥ 25) from those without a mental illness (K10 < 25), and current suicidality was ascribed based on scores ≥1 on PHQ-9 item 9: ‘Over the past two weeks, how often have you been bothered by thoughts that you would be better off dead, or of hurting yourself in some way?’ Based on these classifications, generalised linear models (GLMs) were used to determine the risk of mental illness and suicidality based on depressive symptom groupings while controlling for previous diagnosis of depression. An additional GLM examined risk of depression at time 2 (PHQ-9 ≥ 10) as a function of MDRS-7 categories at time 1. Assumptions of GLMs were considered through inspection of scatter plots and histograms of residuals and predicted values, with model results reported as standardised betas.
Results
Sample characteristics
Table 1 presents the characteristics of the participants at time 1 and time 2. As expected, there was a higher proportion of older participants who reported themselves as married/de facto or widowed/divorced/separated, in comparison with younger men. Regarding education, the majority of older participants completed year 11 or below, while the proportion of participants completing a Bachelor’s degree was higher in the younger sample. In addition, household income appeared to be higher in younger compared with older men, consistent with the majority of the older sample reporting themselves as being retired. Comparisons with 2016 Australian Census data indicate that participants in the current study were more likely to be married or in a de facto relationship (63.1% vs 58.1%), more likely to have completed a Bachelor degree level or above (49.8% vs 22.0%) and less likely to be employed full-time (44.5% vs 57.7%) compared with the Australian population.43 This likely reflects the trend towards older men in the current study. Sample characteristics at time 1 and time 2 were mostly comparable, with a higher proportion of participants at time 2 retired.
Item reduction
Descriptive and relational statistics for each of the MDRS-22 items across younger and older age groups are displayed in online supplemental table 1. For the emotion suppression, alcohol use, somatic symptoms and drug use domains, a single highest scoring item emerged congruent across age groups. For the anger and aggression domain, two different items were retained because of their performance across the age groups. Finally, although two risk-taking items scored equally well in the younger group, only one of these loaded within the older age group, and only this item was retained. This resulted in a total selection of seven items for the short-form scale covering all of the original MDRS-22 domains. The final scale and response format is presented in Appendix A
bmjopen-2021-053650supp002.pdf (66KB, pdf)
Factor analysis of these seven items revealed the presence of a single underlying domain that satisfied criteria determined by the parallel analysis; eigenvalues were required to exceed 1.16. As shown in table 2, all items demonstrated a moderate-to-strong loading on a single underlying factor except for those measuring alcohol and drug use, which loaded moderately. When modelling these seven items using CFA at time 2, the initial solution specifying all items loading on a single latent MDRS-7 factor was not quite adequate (χ2(14)=65.85, p<0.001, CFI=0.96, TLI=0.94, RMSEA=0.11 (0.08, 0.13), SRMR=0.10). However, allowing the errors of the two items assessing anger and physical aggression to covary resulted in acceptable model fit (χ2(13)=29.04, p≤0.01, CFI=0.99, TLI=0.98, RMSEA=0.06 (0.03, 0.09), SRMR=0.09).
Cut-off scores for the short scale
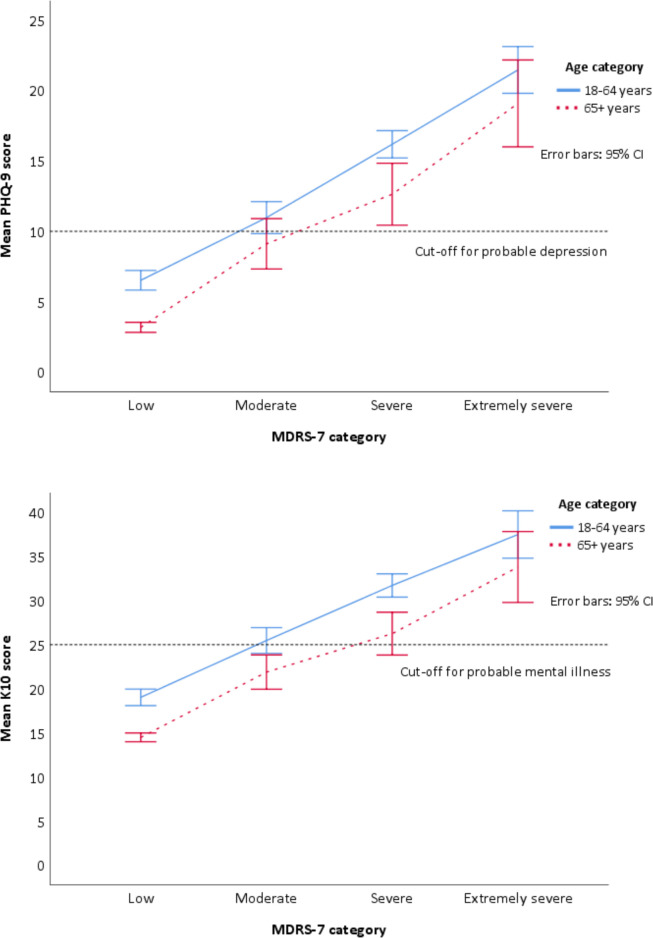
The proportion of men in each of the different MDRS-7 symptom severity categories is shown in online supplemental figure 1 for the total sample and by age group. As can be seen, older men appear more likely to be in the ‘low’ category of symptoms and less likely to be in the ‘severe’ or ‘extremely severe’ categories compared with younger men. Figure 1 shows the effect of age and MDRS-7 categories on prototypic depression (PHQ-9) and psychological distress (K10). For PHQ-9, there were significant differences between all MDRS-7 groups (F(3, 912)=208.05, p<0.001) and between age groups (F(1, 912)=26.76, p<0.001), with no significant interaction between MDRS-7 and age (F(3, 912)=0.59, p=0.625). For the K10, results were similar: significant differences between all MDRS-7 groups (F(3, 912)=188.95, p<0.001) and between younger and older men (F(3, 912)=33.05, p<0.001), but no interaction between MDRS-7 and age (F(3, 912)=0.44, p=0.719).
Figure 1.
Effect of age and Male Depression Risk Scale (MDRS-7) category on prototypic depression symptoms (PHQ-9) and psychological distress (K10).
Clinical utility of the MDRS-7
The proportion of men according to depressive classification type is shown in online supplemental figure 2. Externalised and male-type depression affected approximately 10% of younger and older men, while prototypic and mixed depressive symptoms were more common in younger men. Table 3 shows the risk of mental illness and suicidality compared with non-depressed participants within each age group after controlling for a previous diagnosis of depression. All classifications were associated with both outcome measures. Individuals with mixed symptoms have the highest risk of suicidality and mental illness.
Table 3.
Odds of mental illness and current suicidality controlling for previous diagnosis of depression
| Depressed group, n | Moderate mental illness, n (%) | Moderate mental illness, AOR (95% CI) | Suicidality, n (%) |
Suicidality, AOR (95% CI) |
|
| 18–64 years | |||||
| Not depressed | 189 | 11 (6) | 1 | 13 (7) | 1 |
| Prototypic depression | 69 | 54 (78) | 51.35*** (21.94 to 120.18) | 42 (61) | 18.76*** (8.86 to 39.72) |
| Externalised depression | 49 | 10 (20) | 4.09** (1.60 to 10.47) | 9 (18) | 2.99 * (1.19 to 7.50) |
| Mixed depression | 186 | 162 (87) | 91.35*** (43.00 to 194.06) | 136 (73) | 31.97*** (16.51 to 61.90) |
| 65+ years | |||||
| Not depressed | 308 | 5 (2) | 1 | 19 (6) | 1 |
| Prototypic depression | 20 | 8 (40) | 29.66*** (8.17 to 107.67) | 8 (40) | 8.14*** (2.89 to 22.97) |
| Externalised depression | 41 | 4 (10) | 5.37* (1.36 to 21.26) | 10 (24) | 4.34*** (1.83 to 10.29) |
| Mixed depression | 54 | 36 (67) | 105.05*** (36.48 to 302.50) | 41 (76) | 42.69*** (19.47 to 93.61) |
Total N=916 due to four respondents not reporting previous depression diagnosis. OR for previous depression diagnosis not shown. Moderate mental illness defined as K10 ≥ 25. Suicidality defined as ≥ 1 on PHQ-9 item 9. Externalised depression, PHQ-9 < 10 and MDRS-7 > 5; Mixed depression, PHQ-9 ≥ 10 and MDRS-7 > 5; Not depressed, PHQ-9 < 10 and MDRS-7 ≤ 5; Prototypic depression, PHQ-9 ≥ 10 and MDRS-7 ≤ 5.
***p<0.001, **p<0.01, *p<0.05.
AOR, adjusted odds ratio.
A final GLM considered the likelihood of being classified as depressed at follow-up based on responses to the PHQ-9 at time 2 (ie, score ≥ 10). MDRS-7 category was entered as a predictor controlling for PHQ-9 scores at time 1, previous diagnosis of depression and age. As shown in table 4, PHQ scores at time 1 were significantly associated with an increased risk of depression at time 2 although age and prior diagnoses were not significantly associated. Those classified as having moderate MDRS-7 symptoms at time 1 were significantly more likely than those in the low symptom category to be classified as depressed at time 2, while the severe and extremely severe categories were not associated with increased risk.
Table 4.
Odds of being classified as depressed at follow-up
| Outcome: Depressed (PHQ-9 ≥10) at time 2 (n=328) | ||
| OR | 95% CI | |
| Age (older) | 1.46 | 0.69 to 3.09 |
| Previous depression diagnosis (yes) | 1.87 | 0.88 to 3.99 |
| PHQ-9 (time 1) | 1.24*** | 1.15 to 1.34 |
| Moderate (MDRS-7) | 3.30** | 1.38 to 7.90 |
| Severe (MDRS-7) | 2.00 | 0.76 to 5.28 |
| Extremely severe (MDRS-7) | 1.64 | 0.28 to 9.54 |
Note: Reference category=low symptoms.
***p<0.001, **p<0.01.
MDRS-7, Male Depression Risk Scale; PHQ-9, Patient Health Questionnaire.
Discussion
Clinical reports and emergent empirical work suggest that men’s depression may be underdetected as a result of prototypic screening tools that may be insensitive to men’s gender role socialisation.11 13 44 The MDRS-22 assesses externalised and male-type symptoms of depression, such as substance misuse, risk-taking and anger. However, in its current 22-item form, it is impractical for rapid use in primary care, particularly when used alongside traditional depression screening tools.12 The present research aimed to derive a short form of the MDRS-22, examine its psychometric properties and relationships with psychological distress, depression and suicidal ideation in order to demonstrate its utility as a potential screening tool for primary and other healthcare settings.
The short form derived herein comprises seven items, representing one item for each of the original MDRS domains including emotion suppression, risk-taking, substance use, drug use, somatic symptoms and two items for the anger and aggression domain, based on criteria including variability within items, the item’s relationship to its original MDRS domain but also with the overall MDRS score. Of particular importance is our finding that the correlation between the MDRS-7 and the original MDRS-22 was near perfect (r=0.94). Five of the seven items demonstrated moderate-to-strong loadings on a single underlying construct presumed to reflect the male depression phenotype, while two items assessing alcohol and drug use loaded moderately. This likely reflects the reduced variability of participant responses on these items, with most participants reporting that these items applied to them none or a little of the time. However, these loadings still exceeded the minimum recommended factor loading of 0.32.45 In addition, items that tap these behaviours are important to retain, given that substance use is an important marker of depression and suicidality in men and particularly those who adhere to masculine norms.44 46 It is nonetheless important to note that substance use may reflect a comorbidity47 or maladaptive coping.48 These are important questions for future research to explore.
In the present study, externalising and male-type symptoms, either alone or in combination with prototypic symptoms, were found to be more common than exclusively prototypic symptoms. Approximately 10% of younger and older men were found to present with uniquely externalising and male-type symptoms, while 38% of younger men and 13% of older men presented with mixed symptoms. These findings are consistent with previous research using the MDRS-2224 and highlight the potential utility of the MDRS-7 for detecting additional cases of men at risk. Men with exclusively externalised and male-type depression are a subset who score below threshold on traditional prototypic measures but who report a degree of externalised behaviours that might be problematic in terms of their physical and mental health. Furthermore, both younger and older men in the mixed symptom group had increased risk of a mental illness—after controlling for a previous diagnosis of depression—demonstrating unequivocally that this represents a unique group of psychologically distressed, at-risk men. Similarly, both younger and older men in the mixed symptom group had a significantly elevated risk of suicidality. These findings are consistent with research by Zajac and colleagues24 and highlight the clinical importance of considering a broad range of potential presentations of depression in men, all of which are associated with increased risk of poor outcomes.
The MDRS-7 was also shown to be effective at predicting depression at a later time point, suggesting a possible prodromal effect. These findings are consistent with those by Kendler and Gardner49 who demonstrated that externalising and male-type symptoms predicted a future depressive episode in men. Hence, our findings may reflect early symptom expression or even attempts of men to cope with what has the potential to develop into a threshold depressive disorder. This further highlights the potential value of screening for externalising and male-type symptoms to facilitate early intervention and prevention of further mental health issues.50 In addition, given the externalised nature of male-typical symptoms of depression, it is important to note that these symptoms not only affect men’s health and well-being but also the health well-being of their families, friends and communities.13 51 52 Hence, the better identification and management of male depression is likely to have substantial public health implications.
Clinical implications
There is an urgent need for health services and providers to use more sensitive diagnostic tools as a means of improving the detection of depression and psychological distress in men and addressing the high rates of male suicide.13 The use of brief tools such as the MDRS-7 may assist with detecting unique cases of men who would score below threshold on measures such as the PHQ-9. However, an added benefit of using this scale alongside prototypic measures is the ability to detect men presenting with mixed symptomology whose risk of suicide and poor mental health outcomes is significantly elevated. Therefore, the clinical utility of this measure may extend beyond screening and detection and into the therapy setting where it is necessary to determine, monitor and manage differing degrees of suicidality.
Limitations and suggestions for future research
The methodology adopted in this study is not without limitations. The majority of participants were recruited online, which may limit the generalisability of the findings to other populations.53 Future research should examine measurement invariance according to factors such as education level, income and cultural background. There was also a trend towards older men in the current sample. However, items retained in the MDRS-7 were those that performed best in both younger and older men to ensure the measure was appropriate across the lifespan. Future research should examine the psychometric properties of the MDRS-7 with additional populations, including clinical samples of men across the lifespan presenting to primary care. In addition, as data was self-report, diagnosis of depression could not be verified at clinical interview. The results of this study would be strengthened by a more rigorous assessment of psychopathology and comorbidity. It is also important to acknowledge that this study used a single item from the PHQ-9 to examine current suicidal ideation. Therefore, there is a need for additional research to examine the relationship between the MDRS-7 and other measures of suicidality, including recent suicide attempt.
Conclusion
The present study provides important preliminary information on the development and validation of the MDRS-7. Specifically, this study provides emerging support for the validity and reliability of the MDRS-7 as a measure of externalising and male-type depression symptoms in both younger and older men in terms of its psychometric properties as well as its relationship to prototypic depression symptoms, psychological distress and suicidality. Use of male-specific measures of depression such as the MDRS-7 may improve the detection of depression and suicide risk in men, and adjunctive use (alongside established prototypic scales such as the PHQ-9) may contribute to improved public health outcomes.
Supplementary Material
Acknowledgments
The authors thank all participants for contributing to this study. The authors would also like to acknowledge Lynn Ward for her valuable suggestions on earlier drafts of the manuscript.
Footnotes
Contributors: DH is the guarantor of the paper. DH, SR and IZ developed the study concept. DH and IZ performed the data analyses. DH drafted the paper and SR and IZ provided critical revisions. All authors approved the final version of the paper for submission.
Funding: DH is supported by an Australian Government Research Training Program Scholarship and a CSIRO Supplementary Scholarship. SR is supported by an NHMRC Career Development Fellowship (GNT1158881) from the Australian Government. These funding bodies had no influence on the design of the study and collection, analysis or interpretation of data or in writing the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data is available on reasonable request.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethics approval was obtained from the University of Adelaide Human Research Ethics Committee and the CSIRO Health and Medical Human Research Ethics Committee (approval number H-2019-109). All participants provided informed consent.
References
- 1.Friedrich MJ. Depression is the leading cause of disability around the world. JAMA 2017;317:1517. 10.1001/jama.2017.3826 [DOI] [PubMed] [Google Scholar]
- 2.Costantini L, Pasquarella C, Odone A, et al. Screening for depression in primary care with patient health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord 2021;279:473–83. 10.1016/j.jad.2020.09.131 [DOI] [PubMed] [Google Scholar]
- 3.Orgasnization WHOrganization WH, ed. Depression and other common mental disorders: global health estimates. Geneva: World Health Organization, 2017. [Google Scholar]
- 4.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 2014;13:153–60. 10.1002/wps.20128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mauvais-Jarvis F, Bairey Merz N, Barnes PJ, et al. Sex and gender: modifiers of health, disease, and medicine. The Lancet 2020;396:565–82. 10.1016/S0140-6736(20)31561-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization, . Preventing suicide: A global imperative. Geneva: World Health Organization, 2014. [Google Scholar]
- 7.American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-5. fifth ED. Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
- 8.World Health Organization . International classification of diseases for mortality and morbidity statistics, 2018
- 9.Whittle EL, Fogarty AS, Tugendrajch S, et al. Men, depression, and coping: are we on the right path? Psychol Men Masc 2015;16:426–38. 10.1037/a0039024 [DOI] [Google Scholar]
- 10.Cavanagh A, Wilson CJ, Caputi P, et al. Symptom endorsement in men versus women with a diagnosis of depression: a differential item functioning approach. Int J Soc Psychiatry 2016;62:549–59. 10.1177/0020764016653980 [DOI] [PubMed] [Google Scholar]
- 11.Martin LA, Neighbors HW, Griffith DM. The experience of symptoms of depression in men vs women: analysis of the National comorbidity survey replication. JAMA Psychiatry 2013;70:1100–6. 10.1001/jamapsychiatry.2013.1985 [DOI] [PubMed] [Google Scholar]
- 12.Rice SM, Kealy D, Seidler ZE, et al. Male-type and prototypal depression trajectories for men experiencing mental health problems. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17197322. [Epub ahead of print: 07 10 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Call JB, Shafer K. Gendered manifestations of depression and help seeking among men. Am J Mens Health 2018;12:41–51. 10.1177/1557988315623993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Australian Bureau of Statistics . Health service usage and health related actions, Australia, 2014-15. Canberra: Australian Bureau of Statistics, 2017. [Google Scholar]
- 15.Australian Institute of Family Studies . Mental health of Australian males: Depression, suicidality and loneliness 2020.
- 16.Martin S, Zajac I, Vincent A, et al. Effect of depression on health service utilisation in men: a prospective cohort study of Australian men aged 35 to 80 years. BMJ Open 2021;11:e044893. 10.1136/bmjopen-2020-044893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Hunt K, Nazareth I, et al. Do men consult less than women? an analysis of routinely collected UK general practice data. BMJ Open 2013;3:e003320. 10.1136/bmjopen-2013-003320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schaffer A, Sinyor M, Kurdyak P, et al. Population-Based analysis of health care contacts among suicide decedents: identifying opportunities for more targeted suicide prevention strategies. World Psychiatry 2016;15:135–45. 10.1002/wps.20321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lakkis NA, Mahmassani DM. Screening instruments for depression in primary care: a Concise review for clinicians. Postgrad Med 2015;127:99–106. 10.1080/00325481.2015.992721 [DOI] [PubMed] [Google Scholar]
- 20.Brownhill S, Wilhelm K, Eliovson G, et al. 'For men only'. A mental health prompt list in primary care. Aust Fam Physician 2003;32:443. [PubMed] [Google Scholar]
- 21.Zierau F, Bille A, Rutz W, et al. The Gotland male depression scale: a validity study in patients with alcohol use disorder. Nord J Psychiatry 2002;56:265–71. 10.1080/08039480260242750 [DOI] [PubMed] [Google Scholar]
- 22.Magovcevic M, Addis ME. The masculine depression scale: development and psychometric evaluation. Psychol Men Masc 2008;9:117–32. 10.1037/1524-9220.9.3.117 [DOI] [Google Scholar]
- 23.Rice SM, Fallon BJ, Aucote HM, et al. Development and preliminary validation of the male depression risk scale: furthering the assessment of depression in men. J Affect Disord 2013;151:950–8. 10.1016/j.jad.2013.08.013 [DOI] [PubMed] [Google Scholar]
- 24.Zajac IT, Rice S, Proeve M, et al. Suicide risk, psychological distress and treatment preferences in men presenting with prototypical, externalising and mixed depressive symptomology. J Ment Health 2020:1–8. 10.1080/09638237.2020.1755026 [DOI] [PubMed] [Google Scholar]
- 25.Ferenchick EK, Ramanuj P, Pincus HA. Depression in primary care: part 1-screening and diagnosis. BMJ 2019;365:l794. 10.1136/bmj.l794 [DOI] [PubMed] [Google Scholar]
- 26.Hutton C, Gunn J. Do longer consultations improve the management of psychological problems in general practice? A systematic literature review. BMC Health Serv Res 2007;7:71. 10.1186/1472-6963-7-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Royal Australian College of General Practitioners . General practice: health of the nation 2018. East Melbourne, Vic, 2018. [Google Scholar]
- 28.Mitchell AJ, Coyne JC. Do ultra-short screening instruments accurately detect depression in primary care? A pooled analysis and meta-analysis of 22 studies. Br J Gen Pract 2007;57:144–51. [PMC free article] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002;32:959–76. 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Guth D, Steer RA, et al. Screening for major depression disorders in medical inpatients with the Beck depression inventory for primary care. Behav Res Ther 1997;35:785–91. 10.1016/S0005-7967(97)00025-9 [DOI] [PubMed] [Google Scholar]
- 32.Rice SM, Kealy D, Oliffe JL, et al. Externalizing depression symptoms among Canadian males with recent suicidal ideation: a focus on young men. Early Interv Psychiatry 2019;13:308–13. 10.1111/eip.12667 [DOI] [PubMed] [Google Scholar]
- 33.Rice SM, Ogrodniczuk JS, Kealy D, et al. Validity of the male depression risk scale in a representative Canadian sample: sensitivity and specificity in identifying men with recent suicide attempt. J Ment Health 2019;28:132–40. 10.1080/09638237.2017.1417565 [DOI] [PubMed] [Google Scholar]
- 34.Herreen D, Rice S, Currier D, et al. Associations between conformity to masculine norms and depression: age effects from a population study of Australian men. BMC Psychol 2021;9:32. 10.1186/s40359-021-00533-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JBW, et al. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry 2010;32:345–59. 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 36.Stolk Y, Kaplan I, Szwarc J. Clinical use of the Kessler psychological distress scales with culturally diverse groups. Int J Methods Psychiatr Res 2014;23:161–83. 10.1002/mpr.1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Australian Bureau of Statistics . National health survey: Users' guide 2014-2015. Canberra: Australian Bureau of Statistics, 2019. [Google Scholar]
- 38.JASP Team . JASP (version 0.13.1), 2020
- 39.Uddin MN, Islam FMA. Psychometric evaluation of the modified Kessler seven-item version (K7) for measuring psychological distress using Rasch analysis: a cross-sectional study in a rural district of Bangladesh. BMJ Open 2020;10:e034523. 10.1136/bmjopen-2019-034523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pather S, Uys CS. Using scale reduction techniques for improved quality of survey information. S. Afr. j. inf. manag. 2008;10. 10.4102/sajim.v10i3.322 [DOI] [Google Scholar]
- 41.Stanton JM, SINAR EF, BALZER WK, et al. Issues and strategies for reducing the length of self-report scales. Pers Psychol 2002;55:167–94. 10.1111/j.1744-6570.2002.tb00108.x [DOI] [Google Scholar]
- 42.Hu Li‐tze, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal 1999;6:1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 43.Australian Bureau of Statistics . Census of population and housing - Quickstats, community profiles and datapacks user guide, Australia, 2016. Canberra: Australian Bureau of Statistics, 2017. [Google Scholar]
- 44.Addis ME. Gender and depression in men. Clinical Psychology: Science and Practice 2008;15): :153–68. 10.1111/j.1468-2850.2008.00125.x [DOI] [Google Scholar]
- 45.DeVellis RF. Scale development: theory and applications. 4th ED. applied social research methods series. 26. Thousand Oaks, Calif: Sage Publications, 2016. [Google Scholar]
- 46.Coleman D. Traditional masculinity as a risk factor for suicidal ideation: Cross-sectional and prospective evidence from a study of young adults. Arch Suicide Res 2015;19:366–84. 10.1080/13811118.2014.957453 [DOI] [PubMed] [Google Scholar]
- 47.Macdonald JA, Greenwood CJ, Francis LM, et al. Profiles of depressive symptoms and anger in men: associations with postpartum family functioning. Front Psychiatry 2020;11:578114. 10.3389/fpsyt.2020.578114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cavanagh A, Wilson CJ, Kavanagh DJ, et al. Differences in the expression of symptoms in men versus women with depression: a systematic review and meta-analysis. Harv Rev Psychiatry 2017;25:29–38. 10.1097/HRP.0000000000000128 [DOI] [PubMed] [Google Scholar]
- 49.Kendler KS, Gardner CO. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am J Psychiatry 2014;171:426–35. 10.1176/appi.ajp.2013.13101375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hetrick SE, Parker AG, Hickie IB, et al. Early identification and intervention in depressive disorders: towards a clinical staging model. Psychother Psychosom 2008;77:263–70. 10.1159/000140085 [DOI] [PubMed] [Google Scholar]
- 51.Rice SM, Fallon BJ, Aucote HM, et al. Longitudinal sex differences of externalising and internalising depression symptom trajectories: implications for assessment of depression in men from an online study. Int J Soc Psychiatry 2015;61:236–40. 10.1177/0020764014540149 [DOI] [PubMed] [Google Scholar]
- 52.Wilson S, Durbin CE. Effects of paternal depression on fathers' parenting behaviors: a meta-analytic review. Clin Psychol Rev 2010;30:167–80. 10.1016/j.cpr.2009.10.007 [DOI] [PubMed] [Google Scholar]
- 53.Choi I, Milne DN, Glozier N, et al. Using different Facebook advertisements to recruit men for an online mental health study: engagement and selection bias. Internet Interv 2017;8: :27–34. 10.1016/j.invent.2017.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053650supp001.pdf (142.8KB, pdf)
bmjopen-2021-053650supp002.pdf (66KB, pdf)