Abstract
Introduction
Periprosthetic femoral fracture around hip arthroplasty are growing in the world, nevertheless management and treatment options for fractures “around the stem” are still debated due to lack of high-level studies.
Materials and method
A 85-item survey were fill out by 40 Italian Orthopedic Surgeon member of SIOT (Società Italiana di Ortopedia e Traumatologia) and AIR (Associazione Italiana Riprotesizzazione) to assess their current opinion in the management of type B periprosthetic femoral fractures. Responses were summarized using proportions, and further stratified by practice type, case volume, surgeon age, and fellowship training.
Results
Vancouver/UCS fracture classification showed a good interobserver agreement (k value = .76). ORIF were the treatment of choice for UCS type B1 fractures (100%), revision stem for B2 (85%) and B3 (100%). Locked plates were preferred to cable plate and cerclage without a plate for B1 fractures (50% vs 40% vs 10%); revision with modular stem was preferred to monoblock stem for B2 fractures (50% vs 35%) and B3 (75% vs 15%). Responders tended to postpone at 1-month weight-bearing in patients with B1 fractures. Regarding postoperative pharmacological treatment there was absolute lack of consensus.
Discussion
The primary finding of our survey confirmed the preference of ORIF for B1 fractures and stem revision for B2 and B3 fractures. However, there is no definitive operative technique for all UCS B fractures. Surgeons tended to favor locked plating over cable plating, although only slightly. This general lack of consensus coincides with the inconclusive evidence that currently exists in the literature, which demonstrates both favorable and unfavorable outcomes for both techniques
Conclusions
The absence of complete homogeneity among participants showed the need for prospective randomized studies to set up stronger guidelines for classification, management, surgical treatment, rehabilitation, and pharmacological support of periprosthetic femoral fractures.
Keywords: periprosthetic fractures, hip revision surgery, Total hip arthroplasty, Vancouver type B, Survey, Locking plate
Introduction
The number of hip arthroplasty procedures performed in the developed countries is predicted to rise in the next decades with an annual rate of 1.2%, leading to an increase from 1.8 million per year in 2015 to 2.8 (2.6 - 2.9) in the year 2050. 1 Countries like Germany, the USA or Switzerland currently show rates that exceed 260 per 100 000 population, whereas other countries like Italy have rates of 175 per 100 000 inhabitants.
In Italy, according to the latest reports, every year more than 80.000 primary total hip arthroplasties (THAs), and more than 30.000 femoral hemiarthroplasties and THAs for proximal femoral fractures are performed, representing approximately 110.000 new patients at risk for periprosthetic fractures (PFs) every year. 2 Moreover, a further raising in the number of post-operative periprosthetic femoral fractures (PFFs) is expected due to the increased life expectancy combined with the effects of chronic diseases, frailty and falls. Therefore, PFFs have been already defined as the “next fragility fractures epidemic.” 3
Orthopedic surgeons are called to manage PFFs in elderly patients with poor bone quality and a wide spectrum of different functional demands.
The choice between osteosynthesis and revision surgery is mostly based on the assumptive stability of the femoral stem and the evaluation of the residual bone stock, as per the original Vancouver classification by Duncan and Masri in which Type A are fracture involving the trochanters, Type B stands for “bed of the implant or around the implant” and Type C are clear fractures or distant to the stem itself. 4 In 2014 Duncan et al proposed the new Unified Classification System (UCS) that completely incorporated the older Vancouver classification for periprosthetic fractures of the femur and extended its use to all periprosthetic fractures around a joint. Moreover, this classification system added types D, E, and F of PFs describing different patterns of skeletal involvement (see Table 1). 5
Table 1.
Unified Classification System Classification and PF Treatment Algorithm.
| Joint | Bone | |
|---|---|---|
| I: Shoulder | 1: Humerus | |
| II: Elbow | 14: Glenoid/scapula | |
| III: Wrist | 2: Radius/ulna | |
| IV: Hip | 3: Femur | |
| V: Knee | 4: Tibia | |
| VI: Ankle | 34: Patella | |
| 6: Acetabulum/pelvis | ||
| 7: Carpus/metacarpals | ||
| 8: Talus | ||
| Type of fractures | Treatment algorithm | |
|
A Apophyseal or extraarticular/periarticular Subtypes • A1 Avulsion of (e.g., great trochanter) • A2 Avulsion of (e.g., lesser trochanter) |
Depends on displacement and
importance of soft tissue attached, for example: • great trochanter, tibial tuberosity: surgical treatment • lesser trochanter, coracoid process: conservative treatment |
|
|
B Bed of the implant or around the implant Subtypes • B1: Prosthesis stable, good bone • B2: Prosthesis loose, good bone • B3: Prosthesis loose, poor bone or bone defect |
B1: Lower limb: reduction and
fixation, LCP and if possible MIPO technique
preferred. Upper limb: depends on displacement, conservative treatment preferred. B2: Revision surgery. B3: Revision surgery that may require complex reconstruction (megaprosthesis, allograft/stem composite). Depends on the bone loss and age/activity of the patients. |
|
|
C Clear of or distant to the implant |
Same management as no-periprosthetic fracture. | |
|
D Dividing the bone between two implants or interprosthetic or intercalary |
Decision-making depends on
“block-out analysis.”
a
Subtype A (both prostheses stable): reduction and fixation Subtype B (one stable and one loose): revision surgery Subtype C (both loose): both joint revision surgery, total replacement |
|
|
E Each of two bones supporting one arthroplasty or polyperiprosthetic |
Decision-making depends on “block-out analysis” a (e.g., separate assessment of femoral fracture with stem of THA and acetabular fracture with cup) | |
|
F Facing and articulating with a hemiarthroplasty |
Depends on displacement, conservative treatment preferred. | |
aBlock-out analysis= to analyze separately PF in relation with two joints.
Even considering the more recent developments in classifications, imaging, and treatment algorithms, the appropriate treatment for UCS type B periprosthetic fractures is still debated.6,7 B1 and B2 types both represent a fracture with good bone quality, but while in B1 fractures the stem is stable and in B2 fractures the stem is loose. Therefore, the main therapeutic strategy for B1 fractures is fixation, while for B2 is stem revision. B3 fractures are described as loose prosthesis with poor bone or bone defect and revision surgery represents the only option. Several different fixation or revision techniques are proposed, involving either locked plating, cable plating, or cortical strut allografts, revision surgery that may require complex reconstruction (megaprosthesis, allograft/stem composite) depending on the bone quality, bone stock, and age/activity of the patients (see Table 1). 8
Unfortunately, there are not unanimous guidelines for the treatment of PFFs due to the weakness of the available studies and the lack of prospective randomized trials. 9
In this study, we surveyed a sample of orthopedic surgeons with specific expertise in hip trauma and revision surgery, with 2 primary goals: (1) to evaluate the familiarity with classification systems and diagnostic procedures of orthopedic surgeons; (2) to define their current treatment choices for UCS type B periprosthetic femoral fractures.
Materials and Methods
An 85-item survey was designed regarding UCS B periprosthetic fracture treatment and practice choices.
We focused on minimizing all 4 types of survey error: sampling, coverage, measurement, and non-response. Items included 2 different question styles: multiple and yes/no choice. In the first section of the survey, we assessed the background of the physicians and their practice: 1) the number of cases treated per year, 2) the classification currently used, and 3) the average time from injury to surgery. Additional questions regarded the number of acetabular fractures treated yearly and the classification system used. In the second section, we proposed 9 cases of periprosthetic femoral fractures reporting the personal medical history of the patients and imaging with plain radiographs. The cases presented were 3 B1, 3 B2, and 3 B3 fractures.
A 10-items questionnaire was included for each case presented (Table 2) reporting questions about fractures’ classification, pre-operative, peri-operative, and post-operative care choices.
Table 2.
Case Reports Questionnaire.
| 1 |
Please classify this fracture using the
UCS Classification: 1) B1 2) B2 3) B3 |
| 2 |
Preoperative
treatments: 1) Blood transfusion at disposal: Yes/no 2) VTE prophylaxis drugs: Yes/no 3) Antibiotic prophylaxis one-shot: yes/no 4) Antibiotic prophylaxis > 24 hours: Yes/no |
| 3 |
Preoperative diagnostic
tools: 1) X-Ray before trauma (essential): Yes/no 2) Preoperative CT (essential): Yes/no 3) Inflammation blood tests (essential): Yes/no |
| 4 |
Which surgical treatment do you
choose: 1) ORIF (open reduction and internal fixation) 2) Stem revision |
| 5 |
Fixation device chosen (in case of
ORIF): 1) Cerclages alone 2) Cable plate 3) Locking plate |
| 6 |
i) Type of stem chosen (in case of stem
revision) 1) modular 2) Monoblock 3) PRF ii)Femur fixation during stem revision: 1) Cerclages 2) locking plate 3) cable plate |
| 7 |
Bone graft: 1) no 2) morselized 3) structural |
| 8 |
Acetabular surgical
treatment: 1) no 2) only polyethylene exchange 3) cup revision |
| 9 |
Weight-bearing: 1) immediate 2) 1 month 3) 3 months |
| 10 |
Pharmacological treatment for bone
healing: 1) none 2) vitamin D - Calcium 3) bisphosphonates 4) teriparatide |
The survey was e-mailed between September and October 2018 to 45 active member of the Italian Association of Revision Surgery (AIR, Associazione Italiana Riprotesizzazione) and the Italian Society of Orthopaedics and Traumatology (SIOT, Società Italiana di Ortopedia e Traumatologia) who gave consent to answer to the survey during the 2018 annual SIOT Congress. We sent a reminder email after 4 weeks, and the survey was open for 6 weeks. Respondents returned the filled-out survey by email. The assessment of the results and discussion was conducted during the Periprosthetic Fractures Management Instructional Course of 103rd National Congress of SIOT (Bari, 9-12 November 2018).
Statistical Analysis
Data were analyzed using SPSS software (SPSS, Inc Chicago, IL). Cohen kappa (k) coefficient was used to measure interobserver agreement for fracture classifications. 10 The k coefficient ranges from 1 (perfect agreement) to <0 (no more agreement than would be expected by chance alone). The generated k values were interpreted according to the criteria of Landis and Koch ≥.81, almost perfect agreement between .61 and .80, substantial agreement; between .41 and .60, moderate agreement; between .21 and .40, fair agreement; and ≤.2, slight agreement. 11 Non-weighted k coefficients were used to determine interobserver reliability. Overall k ranges between B1, B2, and B3 groups were calculated using the mean k value among the observers. Mean k coefficients were compared using the standard Student t-test, with a significance level of P < .05 and 95% confidence interval (CI). Fisher’s exact test, with significance set at P < .05, estimated nominal variables between 3 main groups (UCS B1, B2, B3).
Results
Demographic Data
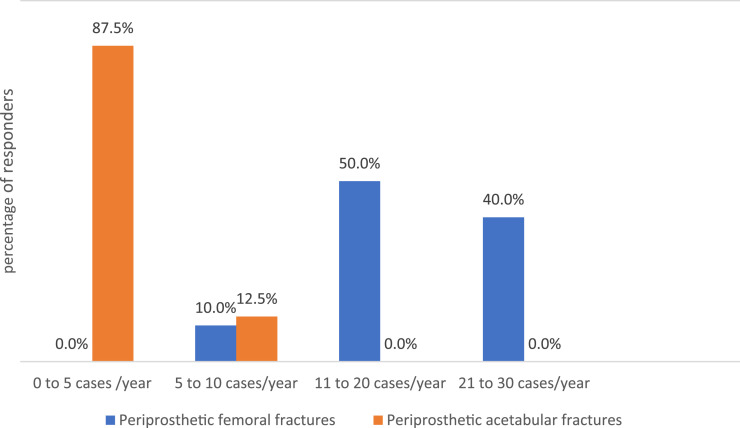
40 (89%) of the 45 orthopedic surgeons invited to participate, completed the survey. All 40 responders practiced orthopedic surgery in Italy: 15 (37.5%) in a teaching hospital of an academic institution and 25 (62.5%) in a community hospital. All surgeons were involved in residents training. Twenty (50%) of them worked in a surgical team that treat from 11 to 20 PFFs per year, sixteen (40%) more than 21 cases per year (Figure 1). Thirty-five (87.5%) surgeons worked in a surgical team that treated from 0 to 5 periprosthetic acetabular fractures per year and five (12,5%) usually treated from 5 to 10 (Table 2).
Figure 1.
The number of periprosthetic fractures around the hip treated every year in responders’ institution.
Periprosthetic Classification Preferences and Interobserver Agreement
All the responders endorsed the use of the same classification system: the original Vancouver classification was preferred for 31 (77.5%) attendees and the newer UCS for 9 of them (22.5%). The Paprosky classification 12 was the preferred system used to classify periprosthetic acetabular fractures for 21 (52.5%) attendees. 15 surgeons (37.5%) reported the use of UCS and the other 5 (12.5%) surgeons used the Peterson and Lewallen classification. 13 Nearly half of the responders, 19/40 (47.5%), declared that they usually treat PFFs in less than 48 hours from the time of trauma. 17 out of 40 (42.5%) surgeons perform surgery in 48 to 72 hours and 4 out of 40 (10%) surgeons in more than 72 hours since fracture occurred.
The mean interobserver agreement for Vancouver/UCS classification, regarding periprosthetic femoral fracture, was good (k value = .76). If we considered only B1 and B2 fractures, interobserver agreement decreased to a k value = .64, while a higher interobserver agreement was found in B2 and B3 fractures (k value = .82).
Unified Classification System Type B Femoral Fracture Preoperative Treatment Preferences (Table 3)
Table 3.
Surgeons Pre-Operative Treatment Preferences for UCS Type B Femoral Fractures.
| B1 (%) | B2 (%) | B3 (%) | |
|---|---|---|---|
| Preoperative blood transfusion at disposal: Yes | 40/40 (100%) | 40/40 (100%) | 40/40 (100%) |
| VTE prophylaxis drugs: Yes | 40/40 (100%) | 40/40 (100%) | 40/40 (100%) |
| Antibiotic prophylaxis: Yes | 40/40 (100%) | 40/40 (100%) | 40/40 (100%) |
| Antibiotic prophylaxis > 24 hours: Yes | 33/40 (82.5%) | 37/40 (92.5%) | 39/40 (97.5%) |
| ESV, CRP (essential): Yes | 36/40 (90%) | 34/40 (85%) | 37/40 (92.5%) |
| Collect previous X-Rays (essential): Yes | 35/40 (87.5%) | 36/40 (90%) | 33/40 (82,5%) |
| Preoperative CT (essential): Yes | 17/40 (42.5%) | 23/40 (57.5%) | 34/40 (85%) |
All surgeons considered essential blood transfusion at disposal before the surgery and venous thromboembolism (VTE) prophylaxis. About 90% of attendees would use antibiotic prophylaxis for more than 24 hours following surgery without differences in fracture types (P = .078).
Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein pre-operative measurements were commonly evaluated by more than 85% of surgeons, particularly for B3 fractures (37/40; 92.5%).
For B1, B2, and B3 more than 85% of attendees usually collect previous x-rays to compare the stem position and bone stock. The number of surgeons who needed preoperative CT scan was significantly higher for B3 fracture (P < .0003).
Unified Classification System Type B Femoral Fracture Operative Treatment Preferences (Table 4)
Table 4.
Surgeons Operative Treatment Preferences for UCS Type B Femoral Fractures.
| B1 | B2 | B3 | |
|---|---|---|---|
| ORIF | 40/40 (100%) | 6/40 (15%) | - |
| Plate (with screws and cerclages) | 36/40 (90%) | 6/40 (15%) | - |
| Locking plate | 20/36 (55.6%) | 5/6 (83.3%) | - |
| Cable plate | 16/36 (45.4%) | 1/6 (16.7%) | - |
| Cerclages alone | 4/10 (40%) | 1/40 (5%) | - |
| Stem revision | - | 34/40 (85%) | 40/40 (100%) |
| Monoblock stem | - | 14/34 (41.2%) | 6/40 (15%) |
| Modular stem | - | 20/34 (58.8%) | 30/40 (75%) |
| PFR/Megaprosthesis | - | - | 4/40 (10%) |
| Femur fixation during stem revision | - | 34/34 (100%) | 36/40 (90%) |
| Cerclages alone | - | 18/34 (52.9%) | 4/36 (11.1%) |
| Locking plate | - | 13/34 (38.2%) | 20/36 (55.5%) |
| Cable plate | - | 3/34 (8.8%) | 12/36 (33.3%) |
| Bone graft (femur) | - | 16/40 (40%) | 27/40 (67.5%) |
| Morselized bone graft | - | 7/40 (17.5%) | 12/40 (30%) |
| Structural allograft | - | 9/40 (22.5%) | 15/40 (37.5%) |
| Acetabular treatment | - | 6/40 (15%) | 5/40 (12.5%) |
| Cup revision | - | 5/40 (12.5%) | 5/40 (12.5%) |
| Polyethylene liner exchange | 1/40 (5%) | - |
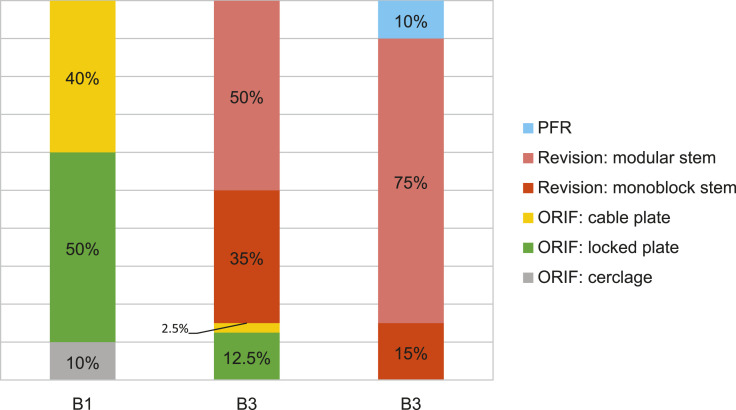
All the participants (40/40, 100%) indicated open reduction and internal fixation (ORIF) as the treatment of choice for B1 fractures. On the other hand, stem revision was the preferred treatment for B2 fractures (34/40, 85%) and B3 fractures (40/40, 100%).
B1 fractures were mainly treated with plate fixation (90%), while only 10% of surgeons choose fixation con cables alone (P > .99). There were no significant differences between the type of plate used (locking plate, 55.6% vs cable plate, 45.4%; P > .05)
Surgeons (6/40, 15%) who choose fixation for B2 fractures showed a preference for locking plates (83.3%). However, the majority of responders (34/40, 85%), treated B2 fractures with stem revision using a modular or a monoblock stem (41.2% vs 58.8%; P > .05). Stem revision was always associated to fracture fixation, mostly with cerclages alone and locking plates (18/34, 52.9% vs 13/34, 38.2%; P > .05).
B3 fractures, according to the attendees, always needed revision surgery (40/40, 100%). The most popular choice was revision with a modular stem for 30 out of 40 responders (75%), compared to 15 out of 40 (15%) who choose monoblock stems (P < .05). Proximal femoral replacement (PFR) or megaprosthesis was considered a valid option for B3 fractures by only 10% of responders. In these cases, no fixation and grafting techniques were associated with the main procedure.
Surgeons opted for bone grafting techniques to augment fixation or bone loss exclusively for B2 and B3 fractures in 40% and 67.5%, respectively (P < .05). Both morselized and structural bone grafts were used in B2 and B3 fracture with a slight preference for structural allografts. Particularly, structural allografts were associated to stem revision for B3 fractures by 37.4% of the surgeons.
Only a few participants 812.5%) considered mandatory acetabular revision for UCS type B2 and B3 femur fractures when treated with stem revision.
Among them, only 1 out of 40 considered polyethylene exchange alone instead of complete cup revision as an acceptable option.
Unified Classification System Type B Femoral Fracture Postoperative Treatment Preferences (See Table 5)
Table 5.
Surgeons Post-Operative Treatment Preferences for UCS Type B Femoral Fractures.
| B1 | B2 | B3 | |
|---|---|---|---|
| Early full weight-bearing (wb): Yes | 5/40 (12.5%) | 23/40 (57.5%) | 14/40 (35%) |
| Full weight-bearing after 1 month | 29/40 (72.5%) | 15/40 (37.5%) | 22/40 (55%) |
| Full weight-bearing after 3 months | 6/40 (15%) | 2/40 (5%) | 4/40 (10%) |
| Pharmacological treatment for bone metabolism: Yes | 21/40 (52.5%) | 13/40 (32.5%) | 14/40 (35%) |
| Calcium/VitaminD alone | 10/21 (47.6%) | 5/13 (38.5%) | 6/14 (42.9%) |
| Calcium/VitaminD + Bisphosphonates | 10/21 (47.6%) | 3/13 (23%) | 4/14 (28.6%) |
| Teriparatide | 1/21 (4.8%) | 5/13 (38.5%) | 4/14 (28.6%) |
Postoperative early full weight-bearing was indicated by the 57.5% (23/40) of the surgeons for B2 fractures and by 35% (14/40) of them for B3 fractures. For B1 fractures, 72.5% of surgeons (29/40) suggested full weight-bearing after 1 month from the surgery (Figure 2).
Figure 2.
Operative treatment preferences with percentages and stacked chart.
Regardless of fractures classification, postoperative immediate full weight-bearing was most likely suggested when the treatment of choice was stem revision (ORIF: 6/46, 13% vs stem revision:36/74, 48.6%).
When asked about the need for pharmacological treatment with calcium/vitamin-D, anti-resorptive and anabolic drugs to enhance bone metabolism and bone healing, surgeons opted for different strategies according to fracture types. More than 50% of responders proposed pharmacological treatments for B1 fractures, while only 32.5% and 35% of them suggested drug use for B2 and B3 fractures, respectively.
Discussion
The incidence of periprosthetic femoral fractures is expected to grow accordingly to increased life expectancy and growing utilization rates of hip arthroplasties over the last 3 decades. 13
However, nowadays there is no full consensus in the orthopedic community regarding their proper treatment. The main unsolved problem is due to the fractures occurring around the stem, the so-called “type B fractures,” which represent almost the 90% of post-operative fractures and 70% of intra-operative fractures. While for intra-operative fractures the assessment of the stem stability represents the only issue, for post-operative fractures the surgeon should assess both the stem stability and the residual bone stock quality. Classification of post-operative type B fractures and, consequently, the treatment choice is the real challenge for the orthopaedic surgeon since traditional xrays and even CT scan cannot offer overall low agreement between observers showed in the current literature.
In a study of Fan et al. 14 402 x-ray UCS periprosthetic femur fractures were classified by 3 expert consultant and 3 trainee surgeons. They found a good interobserver agreement: k value of 0,882 for consultants and 0,776 for trainees. Regarding UCS type B fractures (299 cases) they showed almost perfect agreement: k value = .849.
In our study we found good agreement (k = 0,76).
Low agreement was detected between B1 and B2 fractures due to frequent difficulties to detect stem loosening with preoperative X-Rays (k = .64).
In our survey we found complete participants agreement for all UCS type B fractures about general preoperative management preferences (antibiotic and VTE prophylaxis, blood transfusion at disposal).
The predominance of participants considered essential, during preoperative planning, to obtain femur and hip X-Rays prior to fracture and to rule out for infection with inflammation blood tests.
CT was considered useful, during preoperative planning, mostly for B3 fracture and this may be explained with the need to quantify bone loss.
In this survey a significant proportion of B2 fractures (15%) were treated with ORIF. This might reflect difficulties in determining whether the stem was loose preoperatively from the available imaging. As previously mentioned, differentiation between UCS type B1 and B2 fractures in not always easy and sometimes only considering previous x-rays and history of thigh pain we suspect a fracture with associated loosening of the stem.
In our study we detected for UCS type B1 and B2 a preference for locking plate instead of cable plate. 6
In a cross-sectional survey made by Bates et al 9 regarding Vancouver type B1 fractures surgeons tended to favor locked plates instead of cable plating.
This preference is a clear example of discrepancy between surgeons opinions and current evidence because the same authors made a systematic review where they found a higher rate of nonunion and increased risk of hardware failure by using locking plate alone instead of cable plate. 15
However recently some authors observed an increased healing ratio using locking plates with polyaxial screw fixation.16,17
In a recent study, Chatziagorou et al 18 reviewed data from Swedish Hip Arthroplasty, they found no significant difference of reoperation ratio among the type of stem used for revision of Vancouver B2-B3 fractures and no difference of reoperation ratio between locking and conventional plates for reduction and fixation of B1 fractures. They showed, no matter the type of treatment, higher risk of reoperation in interproshetic and Vancouver B1 fractures.
It has been proved that B2 and B3 fracture may also be successfully treated with ORIF when anatomic and stable reconstruction is obtainable. 19
However, a systematic review of B2 and B3 fractures made by Khan et al 17 showed higher rate of re-operation in patient treated without revision of the stem.
Bhattaharyya et al 20 reported 73 Vancouver type B fracture (22 type B1, 43 type B2, 8 type B3) and found a significant higher mortality ratio in patients treated with ORIF instead of stem revision (33% vs 12%).
It has been proved that modular uncemented long stems are versatile devices that allow diaphyseal femur fixation and facilitate biomechanic restoration of the hip. 21
Munro et al 22 showed at 54 months of mean follow-up good clinical results (Oxford score 76 of 100, WOMAC function and pain score 75 and 82 of 100) treating 46 femoral Vancouver B2 and B3 fractures with a modular tapered titanium stem. They found 24% of stem subsidence, but mostly without clinic correlation and with only one case that required stem revision.
Neumann et al 6 reviewed 55 patients with Vancouver B2 and B3 fractures treated with modular cementless stem without allografting at a mean of 67 months of follow-up showing a Harris Hip Score of 72 points and 4% of stem subsidence that required stem revision.
Our participants considered modular uncemented long stem the preferred device for stem revision.
This may be also due to an increase of uncemented stem arthroplasties detected in Italy during this decade and surgeons may be more confident with uncemented revision techniques.23
The modular uncemented stem provide reliable distal diaphyseal fixation through a tapered fluted section and facilitate to re-establish accurate reconstruction of biomechanics of the hip with different options of modular proximal components that restore length and version independently.
Regarding bone grafting, the lack of consensus, due to weakness of evidence, allows different treatment choices among surgeons based on surgeons’ individual experience.
Bates et al 9 reported a higher preference for bone graft augmentation among surgeons who achieved arthroplasty fellowship training: they found that revision arthroplasty with strut allograft was used by 39,3% of participants for Vancouver B2 and 70,8% for Vancouver B3.
In our study structural and morselized bone graft was a treatment choice for 40% of attendees in UCS B2 fractures and 67.5% in UCS B3.
PFR have a role in UCS type B3 fractures when the proximal femur bone loss is severe, when we treat low demand elderly patients that required immediate weight bearing and mobilization. In our survey PFR was proposed only by 10% of our attendees for B3 fractures.
McLean et al 21 treated 20 periprosthetic femur fracture with bone loss using femoral replacement (15 total and 5 proximal), at mean follow-up of 4 year they found acceptable clinic results but 30% of patients encountered major complications (three hip dislocations, two deep infection and a distal femur fracture).
In our study participants showed less concern to allow immediate full weight bearing in UCS type B2 and B3 fractures and this may be explained by the fact that these types of fractures were more likely to be treated with stem revision instead of ORIF.
Regarding osteoporosis postoperative treatment we found complete absence of consensus.
We thought that systemic pharmacological treatment was not related to fracture classification; patient’s age affect decision making drugs. 22
To our knowledge, our national cross-sectional survey is the first regarding periprostehtic UCS B1, B2 and B3 fractures
Our study presented several intrinsic limitations common to survey-methods.
We are conscious that real treatment decisions are single-case and single-patient custom, even though we tried to simulate all possible scenario with our cases proposed.
This survey was administered to only two orthopedic bodies and required active participation from surgeon members of the AIR and SIOT association, therefore the results may not reflect the opinions of Italian surgeon who were not active part of these associations.
In conclusion our survey showed that ORIF with locking plate is the preferred treatment for UCS type B1 periprosthetic femur fracture and modular uncemented stem revision for B2.
B3 femur fractures required a complex treatment with stem revision related to bone loss and patient’s condition.
We also confirmed the absence of consensus among surgeon and the need of prospective further studies for the right choice of B2 and B3 fractures treatment.
Acknowledgments
We would like to thank all the SIOT and AIR members who responded to the survey
Footnotes
Authors' Contributions: All the authors equally contributed to the conception and design of the work and the acquisition, analysis and interpretation of data. Contributed equally to manuscript’s drafting for important intellectual content and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
SC, AC and GM contributed to the conception and design of the work and the acquisition, analysis and interpretation of data.
GM and SC contributed to the conception and design of the work and the statistical analysis of the data.
All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee (Department of Surgical Sciences, Cagliari State University N°CM_18/12/2018) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study and consented to participate.
Consent for Publication: All patients gave consent for publication.
Availability of Data and Material: The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
ORCID iDs
Christian Carulli https://orcid.org/0000-0002-0845-7940
Stefano Congia https://orcid.org/0000-0003-2348-678X
Giuseppe Marongiu https://orcid.org/0000-0003-2163-454X
References
- 1.Pabinger C, Lothaller H, Portner N, Geissler A. Projections of hip arthroplasty in OECD countries up to 2050. HIP Int. 2018;28(5):498-506. doi: 10.1177/1120700018757940. [DOI] [PubMed] [Google Scholar]
- 2.Capone A, Congia S, Civinini R, Marongiu G. Periprosthetic fractures: Epidemiology and current treatment. Clin Cases Miner Bone Metab. 2017;14(2):189-196. doi: 10.11138/ccmbm/2017.14.1.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bates BD, Walmsley DW, Vicente MR, et al. An international, cross-sectional survey of the management of Vancouver type B1 periprosthetic femoral fractures around total hip arthroplasties. Injury. 2018;49(2):364-369. doi: 10.1016/j.injury.2017.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Duncan CP, Haddad FS. The unified classification system (UCS): Improving our understanding of periprosthetic fractures. Bone Joint Lett J. 2014;96-B(6):713-716. doi: 10.1302/0301-620X.96B6.34040. [DOI] [PubMed] [Google Scholar]
- 5.Yeo I, Rhyu K-H, Kim S-M, Park Y-S, Lim S-J. High union rates of locking compression plating with cortical strut allograft for type B1 periprosthetic femoral fractures. Int Orthop. 2016;40(11):2365-2371. doi: 10.1007/s00264-015-3107-x. [DOI] [PubMed] [Google Scholar]
- 6.Neumann D, Thaler C, Dorn U. Management of Vancouver B2 and B3 femoral periprosthetic fractures using a modular cementless stem without allografting. Int Orthop. 2012;36(5):1045-1050. doi: 10.1007/s00264-011-1371-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293-304. http://www.ncbi.nlm.nih.gov/pubmed/7797866. Accessed February 7, 2020. [PubMed] [Google Scholar]
- 8.Johansson JE, McBroom R, Barrington TW, Hunter GA. Fracture of the ipsilateral femur in patients wih total hip replacement. J Bone Joint Surg Am. 1981;63(9):1435-1442. http://www.ncbi.nlm.nih.gov/pubmed/7320034. Accessed February 7, 2020. [PubMed] [Google Scholar]
- 9.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. J Arthroplasty. 1994;9(1):33-44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 10.Peterson CA, Lewallen DG. Periprosthetic Fracture of the Acetabulum after Total Hip Arthroplasty. J Bone Jt Surg. 1996;78(8):1206-1213. doi: 10.2106/00004623-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Fan M-Q, Fan X-H, Chen X-L, et al. The reliability and validity of the modified Unified Classification System for periprosthetic femoral fractures after hip arthroplasty. J Orthop Sci. March. 2020. doi: 10.1016/J.JOS.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Dehghan N, McKee MD, Nauth A, Ristevski B, Schemitsch EH. Surgical Fixation of Vancouver Type B1 Periprosthetic Femur Fractures. J Orthop Trauma. 2014;28(12):721-727. doi: 10.1097/BOT.0000000000000126. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann MF, Lotzien S, Schildhauer TA. Outcome of periprosthetic femoral fractures following total hip replacement treated with polyaxial locking plate. Eur J Orthop Surg Traumatol. 2017;27(1):107-112. doi: 10.1007/s00590-016-1851-2. [DOI] [PubMed] [Google Scholar]
- 14.Ruchholtz S, El-Zayat B, Kreslo D, et al. Less invasive polyaxial locking plate fixation in periprosthetic and peri-implant fractures of the femur—A prospective study of 41 patients. Injury. 2013;44(2):239-248. doi: 10.1016/j.injury.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 15.Chatziagorou G, Lindahl H, Kärrholm J. Surgical treatment of Vancouver type B periprosthetic femoral fractures. Bone Joint Lett J. 2019;101-B(11):1447-1458. doi: 10.1302/0301-620X.101B11.BJJ-2019-0480.R2. [DOI] [PubMed] [Google Scholar]
- 16.Stoffel K, Blauth M, Joeris A, Blumenthal A, Rometsch E. Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: a systematic review. Arch Orthop Trauma Surg. 2020;140(10):1381-1394. doi: 10.1007/s00402-020-03332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan T, Grindlay D, Ollivere BJ, Scammell BE, Manktelow ARJ, Pearson RG. A systematic review of Vancouver B2 and B3 periprosthetic femoral fractures. Bone Joint Lett J. 2017;99-B(4_suppl e_B):17-25. doi: 10.1302/0301-620X.99B4.BJJ-2016-1311.R1. [DOI] [PubMed] [Google Scholar]
- 18.Bhattacharyya T, Chang D, Meigs JB, Estok DM, Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Jt Surgery-American. 2007;89(12):2658-2662. doi: 10.2106/JBJS.F.01538. [DOI] [PubMed] [Google Scholar]
- 19.Munro JT, Garbuz DS, Masri BA, Duncan CP. Tapered fluted titanium stems in the management of Vancouver B2 and B3 periprosthetic femoral fractures. Clin Orthop Relat Res. 2014;472(2):590-598. doi: 10.1007/s11999-013-3087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stea S, Bordini B, De Clerico M, Petropulacos K, Toni A. First hip arthroplasty register in Italy: 55,000 cases and 7 year follow-up. Int Orthop. 2009;33(2):339-346. doi: 10.1007/s00264-007-0465-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McLean AL, Patton JT, Moran M. Femoral replacement for salvage of periprosthetic fracture around a total hip replacement. Injury. 2012;43(7):1166-1169. doi: 10.1016/j.injury.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 22.Capone A, Orgiano F, Pianu F, Planta M. Orthopaedic surgeons’ strategies in pharmacological treatment of fragility fractures. Clin Cases Miner Bone Metab. 2014;11(2):105. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4172175/. Accessed May 18, 2020. [PMC free article] [PubMed] [Google Scholar]