Abstract
Introduction:
The once-in-a-generation COVID-19 pandemic accelerated the pace at which virtual care (VC) was advanced to triage, evaluate, and care for patients. An early adopter of VC delivery, Mayo Clinic had provided video visits and other remote care options for more than 5 years, yet the need for VC during the pandemic surpassed our available capacity for telehealth care.
Methods:
To continue providing high-quality care while preventing exposure of patients and staff to high-risk environments, staff from Primary Care and Express Care (minor acute services) collaborated to expand the outpatient VC service to triage patients with acute or chronic symptoms and to address concerns that could be managed remotely. We aimed to maximize the treatment options available outside of high-cost settings and also aimed to accelerate development of longer-term solutions for improving care coordination and continuous population management.
Results:
Patient use of virtual visits showed an unprecedented increase after changes were implemented that expanded the existing virtual visit menu, facilitated patient self-triage and direct scheduling, streamlined physical connections for virtual appointments, and incorporated additional language (medical interpreter) support. The combination of patient convenience, ease of scheduling, and added safety for providers and patients, in conjunction with other telehealth options, resulted in a better overall patient experience.
Conclusion:
Any organization that is considering deploying a sustainable program of VC must put patient needs and safety at the center. Organizations should seize opportunities to agilely adjust and advance any emergency-response solutions to serve a longer-term purpose.
Keywords: express care, telehealth, video visit, virtual care
Introduction
As soon as the World Health Organization declared the novel COVID-19 outbreak to be a global pandemic on March 11, 2020, the Mayo Clinic Primary Care Telehealth Strategy group and the Express Care Oversight committee began pivoting the practice to transition from face-to-face visits to virtual visits (VVs) to minimize the risk of virus transmission among patients and staff, in accordance with institutional infection prevention and control policies. 1 Patients requiring outpatient appointments were offered various remote care options. They could have synchronous, real-time telephone calls or video conferences with health care providers by using a smartphone, tablet, or computer. Other options were asynchronous, online messaging with providers through a patient portal (a secure website through which patients could access their protected health information such as records, test results, and appointments) and electronic consultation with providers (e-consults). Select patients were offered remote monitoring as a means of staying connected to their care teams.
The use of telehealth services was tracked, and within 4 months of the start of the pandemic, the data showed unprecedented growth of these services across the institution when compared with the total volume of virtual care (VC) provided since telehealth options first became available at our institution. Online interactions with the Express Care clinic and outpatient e-consults each increased by 30%, and acute care video consults (eg, ambulance, critical care, neonatology) increased by 890%. Video appointments with patients at their preferred locations (eg, their residence) increased by 10 880%, and telephone appointments increased by 13 650%. 2
During the early phase of our institution’s response to the COVID-19 pandemic, the Mayo Clinic Center for Connected Care identified 8 operational components that were essential for deploying a robust telemedicine program. These components were (1) dedicated staffing infrastructure; (2) functional support partnerships; (3) standardized systems of deployment; (4) refined operational processes and procedures; (5) data analytics; (6) practice partnerships; (7) performance reporting; and (8) provider instruction. 3 As the pandemic continued, a VC committee was formed that aimed to expand the telemedicine model beyond the COVID-19 emergency response. Building on the solid foundations laid by our institution’s Center for Connected Care, the VC committee was charged with determining how the institution would continue to meet the needs of our patients during and after the pandemic, as well as enhance the overall patient experience. With VC confirmed as a new, mainstream, value-based approach to providing health care, the committee’s mandate was to proactively prepare for the new telemedicine era and to ensure that patients and staff had a smooth transition in utilizing telehealth services.
The VC model, which initially prioritized services intended to prevent patient and health care worker exposure to COVID-19, thus was swiftly redesigned. We aimed to maximize the number of treatment options that would be available outside of high-cost settings and also aimed to accelerate development of longer-term solutions for improving care coordination and continuous population management. In this report, we describe the collaborative development and 3-phase implementation of a new patient-centered VC model that markedly expanded our institution’s telehealth offerings across the continuum of care.
Methods and Results
The VC committee led the synergistic and collaborative effort (Figure 1) to expand the VC model. VC committee members aimed to work effectively by avoiding making decisions in isolation from other relevant initiatives that were ongoing, completed by other practice areas, or governed by different committees. The group expedited decision-making processes and fast-tracked implementation of new procedures (ie, conducting rapid tests of change) through the collaborative efforts of all committee members. Transparent, cross-functional communication and information sharing was reinforced throughout the duration of the project.
Figure 1.
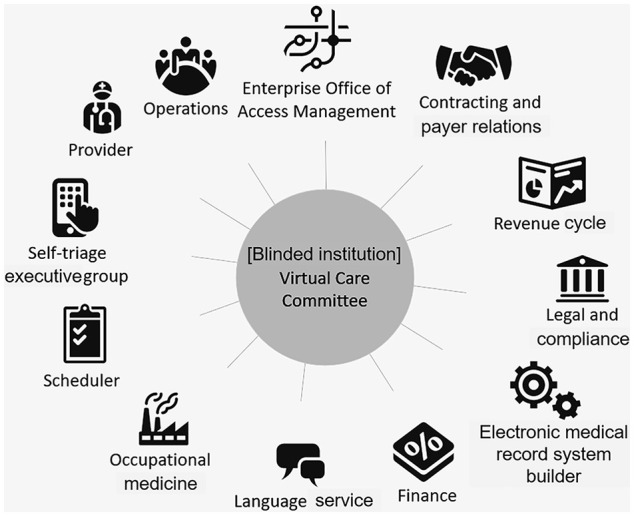
Twelve key stakeholder groups. All groups were engaged in development of the virtual care model, from defining problems to implementing and optimizing solutions.
The VC committee met virtually each week to coordinate goals and schedule tasks with short timelines. Their initial goal was to expand the range of services that could be delivered by the Express Care clinic’s existing VV providers. They also aimed to further develop the direct-scheduling initiative, in which patients would schedule their own in-person or virtual appointments through the patient portal.
Phase 1: VV Menu and End Point Optimization
The multidisciplinary VC committee reviewed 206 adult symptoms and 329 pediatric symptoms. They identified 82 adult symptoms (40%) and 117 pediatric symptoms (36%) that potentially were clinically appropriate for virtual management. The proposed symptoms were then comprehensively assessed (considerations included the level of acuity, technologic requirements and capability, financial feasibility, compliance with legal and other guidelines, and other factors) and tested with simulated patients to determine the most appropriate end points, including virtual and in-person appointments. Table 1 shows the iterative list of symptoms, conditions, and treatments that were eligible for virtual management from March 2020 through May 2021.
Table 1.
Symptoms, Conditions, and Treatments Selected for Scheduler Triage or Patient Self-Triage.
| Symptom, condition, or treatment a | March 2020 through February 2021 | March 2021 b | May 2021 c |
|---|---|---|---|
| Acne | VV | VV or F2F | VV or F2F |
| Bladder infections (females, age 12-75 years) | VV | F2F | F2F |
| Burns, minor | Not offered | VV or F2F | VV or F2F |
| Cold sores | VV | VV or F2F | VV or F2F |
| Cold symptoms | VV | VV | VV |
| Constipation | Not offered | VV or F2F | VV or F2F |
| Dental procedure prophylaxis | Not offered | VV | VV |
| Diarrhea | VV | VV | VV or F2F |
| Ear pain (without respiratory symptoms) | VV | F2F | F2F |
| Ear wash | Not offered | F2F | F2F |
| Fever (37.8°C or higher) | VV | Removed | Removed |
| Conjunctivitis | VV | VV | VV or F2F |
| Heartburn | Not offered | VV or F2F | VV or F2F |
| Influenza symptoms | VV | Removed | Removed |
| Injuries, minor (no head injury) d | VV | VV or F2F | VV or F2F |
| Lice | VV | VV | VV |
| Medication renewal (noncontrolled substance, short-term use) | Not offered | VV | VV |
| Nausea | VV | VV | VV or F2F |
| Oral contraceptives (females, age 18-34 years) | VV | VV or F2F | VV or F2F |
| Pregnancy testing (urine) | Not offered | F2F | F2F |
| Rashes | Not offered | VV or F2F | VV or F2F |
| Sinus symptoms or sinusitis | Not offered | VV | VV or F2F |
| Smoking cessation (age ≥18 years) | VV | VV or F2F | VV or F2F |
| Sore throat | VV | VV | VV or F2F |
| Sports/camp examination (age 11-24 years, excludes Division 1 or chronic medical conditions) | Not offered | F2F | F2F |
| Seasonal allergies | VV | VV | VV or F2F |
| Skin infection, minor | VV | VV or F2F | VV or F2F |
| Stye | VV | VV or F2F | VV or F2F |
| Suture removal | Not offered | F2F | F2F |
| Tick exposure | VV | VV or F2F | VV or F2F |
| Travel-related motion sickness | Not offered | VV | VV |
| Tuberculosis skin testing, test reading | Not offered | F2F | F2F |
| Vaginal yeast infection (females, age 18-65 years) | VV | VV or F2F | VV or F2F |
| Vomiting | VV | VV | VV or F2F |
| Wart removal (up to 4 warts/visit) | Not offered | F2F | F2F |
| Vaccines | Not offered | ||
| Hepatitis A and B (adult only) | F2F | F2F | |
| Human papillomavirus | F2F | F2F | |
| Influenza (flu) | F2F | F2F | |
| Meningococcal polysaccharide diphtheria toxoid conjugate | F2F | F2F | |
| Meningitis B | F2F | F2F | |
| Pneumonia (pneumococcal vaccine polyvalent and pneumococcal 13-valent conjugate vaccine) | F2F | F2F | |
| Shingles (zoster vaccine recombinant, adjuvanted) | F2F | F2F | |
| Tetanus (tetanus-diphtheria booster and tetanus-diphtheria-pertussis vaccine) | F2F | F2F |
Abbreviations: F2F, face to face; VV, virtual visit.
This table lists the symptoms, conditions, and treatments approved or denied for VV or F2F care in the Express Care clinic after multiple rounds of review and voting by the Virtual Care committee members. Symptoms that show the outcome “Removed” were withdrawn from the menu of possible conditions.
The Express Care clinic reopened in March 2021 and started seeing patients who could not be seen safely earlier in the pandemic.
The number of patients with COVID-19 infections decreased in May 2021.
After implementation, the definition of minor injury was changed to include only minor abrasions, cuts, and bruises because patients were presenting with major injuries that were beyond the scope of care provided by the Express Care clinic.
To test the VC model before the full rollout to the entire organization, a 2-week pilot implementation (a Plan-Do-Study-Act cycle) was conducted from September 28 through October 9, 2020, in 5 Mayo Clinic Health System clinics that served 130 000 patients in 3 departments (Family Medicine, Community Internal Medicine, and Community Pediatric and Adolescent Medicine). Scheduling instructions and decision-tree algorithms were built into the electronic health record system so that schedulers could offer VC options to every patient whose condition could be managed with a telehealth care visit. A JD Power national patient satisfaction survey regarding telehealth care had identified multiple factors that reduced patient satisfaction, advocacy, and loyalty; these factors included confusion about technology requirements, technologic issues during a VV, lack of information about VV costs, and the perception of limited services. 4 The scheduler team therefore was trained to assist patients with assessing and setting up videoconference technology capabilities at home, providing transparent cost information, setting patient expectations for the day of the appointment, and answering any other questions.
During the 2-week pilot, 551 VVs were scheduled. In comparison, the 2-week period before the pilot had 413 VVs scheduled and the 4-week period before the pilot had 763 VVs scheduled, reflecting an increase in scheduled VVs of 33% and 44%, respectively. A VV was considered “completed” if the patient was checked in to the VV system and met with a provider. VV completion rates were 398/551 (72%) during the pilot, 274/413 (66%) during the preceding 2 weeks, and 528/763 (69%) during the preceding 4 weeks. From September 28 through November 19, 2020, 3419 VVs were scheduled and 3207 were completed (94%). With the successful pilot results, the model was implemented throughout the institution in the first quarter of 2021. The number of scheduled video appointments per month from January through May 2021 ranged from 779 to 1429, and the completion rate was consistently high (range, 92%-95%). These data indicate that VV utilization during the pandemic dramatically increased after institution-wide implementation of the VC model.
Health care providers and patients were surveyed about the pilot, and the data showed that both groups were comfortable with the new way of providing and receiving care. After studying the pilot outcomes, survey results, and feedback solicited during the trial, the VC committee refined the list of symptoms to match patient demands more closely. The list of symptoms that can be addressed with a VV is dynamic and is continually updated on the basis of patient and provider input and experience with the system. The significant success of this pilot helped us further develop a menu of acute but minor symptoms that could be addressed with VC through the Express Care clinic. A list of future menu items for VV and in-person visits was sent to the Express Care Oversight committee. They were instructed to vote on whether these items should be implemented in the Express Care clinic after considering multiple factors such as impact on patient experience, appropriateness for primary care vs express care, cost effectiveness, and feasibility of implementation. Items were iteratively discussed by the committee, and outcomes are summarized in Table 2.
Table 2.
Symptoms, Conditions, and Treatments Considered for Implementation in the Express Care Clinic.
| Symptom, condition, or treatment | Proposed timing of implementation | Committee decision | Current status a | ||
|---|---|---|---|---|---|
| Immediate | Future | Should not implement a | |||
| Women’s health | |||||
| Sexually transmitted infection screening (urine test for gonorrhea, chlamydia, and trichomoniasis) | ✓ | Agree | Not activated | ||
| Pelvic examination for sexually transmitted infection or bacterial vaginosis | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Bacterial vaginosis | ✓ | Agree | Not activated | ||
| Papanicolaou test | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Oral contraceptives (new prescriptions, renewals for patients aged 18-34 years) | ✓ | Agree | Activated | ||
| Contraceptive injection | ✓ | Agree | Not activated | ||
| Health screening and preventive services (diet, exercise, risk factors, education, heart and lung examination) | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Minor trauma | |||||
| Minor cuts or abrasions | ✓ | Agree | Activated | ||
| Strains (no back pain) | ✓ | Agree | Removed | ||
| Sprains | ✓ | Agree | Removed | ||
| Wound care | |||||
| Abscess | ✓ | More discussion needed | Removed | ||
| Splinter removal | ✓ | Agree | Activated | ||
| Gout treatment | ✓ | May be considered in the future | Not activated | ||
| Pretravel consultation | |||||
| Traveler’s diarrhea, prevention | ✓ | Agree | Activated | ||
| Motion sickness, prevention | ✓ | Agree | Activated | ||
| Laboratory tests | |||||
| Glycated hemoglobin A1c | ✓ | Agree | Unsuitable for Express Care | ||
| Hyperlipidemia screening | ✓ | More discussion needed | Unsuitable for Express Care | ||
| High cholesterol monitoring | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Anticoagulation point-of-care testing | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Heartburn (gastroesophageal reflux disease) | ✓ | Agree | Activated | ||
| College sports examinations (age 18-24 years) | ✓ | Agree | Activated | ||
| Cosmetic procedures | |||||
| Botulinum toxin injection | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Eyelash lengthening | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Hair loss evaluation, treatment | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Alcohol remission (established medication) | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Erectile dysfunction | ✓ | More discussion needed | Unsuitable for Express Care | ||
| High blood pressure evaluation and risk-factor education | ✓ | More discussion needed | Unsuitable for Express Care | ||
| High blood pressure treatment | ✓ | Agree | Unsuitable for Express Care | ||
| Vitamin B12 injection | ✓ | Agree | Not activated | ||
| Nonnarcotic medication renewal, 1-time | ✓ | Agree | Activated | ||
| HIV, pre- or postexposure prophylaxis | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Weight loss program | ✓ | More discussion needed | Unsuitable for Express Care | ||
| Sleep apnea screening | ✓ | More discussion needed | Unsuitable for Express Care | ||
“Not activated” indicates that the committee agreed to have the symptom, condition, or treatment on menu, but it has not been put in place yet (eg, because of limited resources). “Removed” indicates that a menu item initially was offered but then withdrawn for various reasons (eg, subsequently judged to be more appropriate for primary care). “Unsuitable for Express Care” indicates that a service is not offered because it requires further staff training and/or is a service provided elsewhere at the institution.
The postpilot survey of providers and staff showed that “technology or connectivity issues” were among the top reasons that patients declined VV appointments, consistent with findings from the survey by JD Power. 4 Other reasons for declining a VV were patient preference, clinical need for an in-person visit, and provider or care concerns. Survey findings showed that providers believed that the scheduled VVs generally were appropriate to care for patients and meet their needs, but sometimes, an in-person follow-up visit was still required. For example, video-based evaluation of the ears or mouth could be difficult, and physical maneuvers needed to diagnose musculoskeletal concerns required considerable effort. Most patients were aware of and accepted the limitations of VVs and believed that their needs were met.
Phase 2A: Patient Self-Triage and Scheduling
Historically, Mayo Clinic offered a telephone-based system for symptom triage with a nurse. Calls had 5 possible end points—patients could be instructed to immediately call emergency services (911), visit an emergency department, schedule a face-to-face visit, or contact a health care provider, or they could receive self-care instructions directly from the triage nurse. The standard telephone triage system required patients to wait (on hold) to talk to a triage nurse, a scheduler, and sometimes also a health care provider before an appointment could be scheduled. Because of the long hold times, multiple transfers, and/or paucity of timely appointments with the patient’s provider, patients with nonurgent conditions routinely visited the emergency department to access information and care.
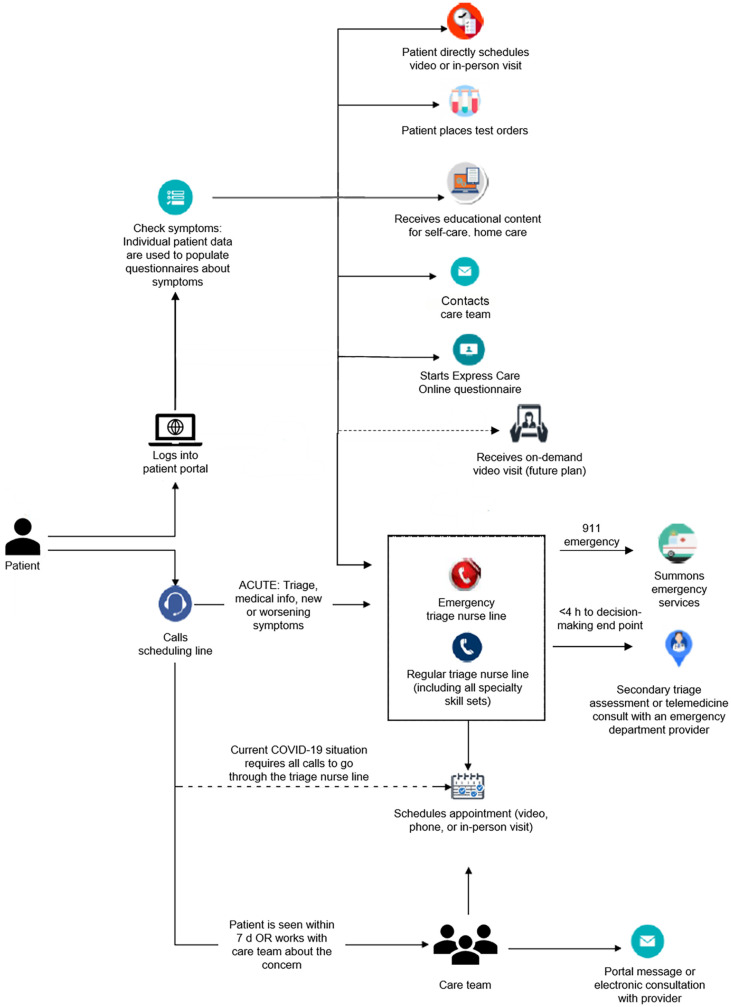
To improve the patient’s triage experience and scheduling process, the patient online service portal was updated to include a list of symptoms that qualified for self-triage. A patient who underwent self-triage would be presented with questions, and the information provided by the patient would be used to populate a decision-tree clinical algorithm. The patient then navigated through the algorithm, and the most appropriate end point would be provided. Currently, the end points of self-triage include patients directly scheduling in-person visits or VVs, placing orders for tests, accessing Mayo Clinic educational content for self-care or home care, using Express Care Online to submit a questionnaire and receive a response from their care team within 24 h, or receiving instructions for further evaluations (eg, contacting the redesigned telephone triage line, sending a secure message to their care team for additional assessment). Additional end points for online self-triage, such as on-demand VV scheduling, are planned for implementation in the near future. The flow of patients through existing and planned end points is shown in Figure 2.
Figure 2.
Decision-tree algorithm. The schematic summarizes the algorithm that is followed by patients and schedulers to appropriate end points.
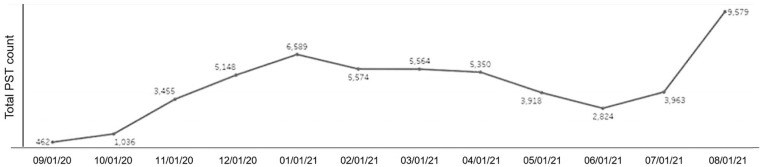
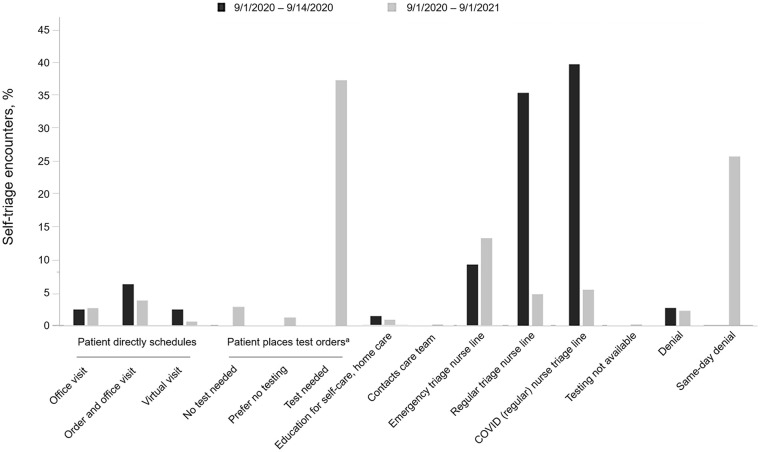
We did not formally survey patients about their satisfaction with the VV care model because of limited resources, but patients have spontaneously expressed great appreciation for the improved triage experience, the immediate access to information about the appropriate level of care for their current symptoms, and the tools that support self-care at home. The number of self-triage encounters has shown a corresponding increase from September 2020 through August 2021 (Figure 3). The most common end points of self-triage encounters also changed with time. Initially, patients often concluded self-triage by calling the nurse triage line, but 1 year after implementation of the self-triage system, calls to triage nurses have decreased by 30 or more percentage points (Figure 4). For example, a patient who previously might have called the triage nurse for pink eye symptoms could instead follow the algorithm to receive the same home care information.
Figure 3.
Self-triage encounters in a 12-month period. PST indicates patient self-triage.
Figure 4.
Comparison of common end points reached after patient self-triage. The first set of patients (n = 372) logged in from September 1 through September 14, 2020. The second set of patients (n = 58 853) logged in from September 1, 2020, through September 1, 2021. The “denial” outcome refers to problems with patient identity (eg, patient was not logged into the correct portal or proxy access account); the “same-day denial” outcome refers to a patient who attempted to access self-triage after already receiving a recommendation for that day.
aSpecific to COVID screening symptoms.
Phase 2B: Opportunities in the Employer Market
During phase 2, concurrent with our efforts to improve the patient self-triage experience, we recognized that employers also were critical factors for widespread adoption of transformative health care services. A survey that assessed health care strategies of large employers showed that most were responding to the burdens of COVID-19 for employees by making changes to improve access to VC. Further, most believed that virtual health care would continue to have a considerable role in how care would be delivered in the future. 5
At Mayo Clinic, our founders famously said “the needs of the patient come first”. In meeting the patients’ medical needs and developing new methods of health care delivery, we also learned that their employers’ needs were diverse. For example, companies located in densely populated areas, where traveling 1 to 2 miles could take an hour, prioritized a more comprehensive list of health care services that could be offered during VVs. In contrast, companies located in a more rural setting had non-English−speaking employees whose care needs were oriented more toward language (including sign language) and health literacy issues. We contracted with an independent medical interpreting and translating agency to begin providing interpreters for an additional 12 languages to ensure that patients with limited English proficiency could have their health questions and medical concerns resolved completely during VVs.
One employer group expressed concerns about the increased emergency department use among their employees. A retrospective data review showed that 61% of the group’s emergency department visits in 2019 occurred outside of usual business hours. As we investigated potential solutions to decrease unnecessary emergency department use, we expanded the availability for Express Care VVs to include evenings and weekends (new hours were Monday-Friday, 8 am-8 pm; Saturday-Sunday, 9 am-5 pm). In addition, a 24/7, real-time service for secondary physician triage assessment for patients with critical end points was implemented, with an approximately 40% decrease in avoidable ED use postimplementation. The new work model became “business as usual,” which would not have been conceivable a year prior.
Phase 3: Alignment With Accountable Care Organization–Supported Connected Care
The expansion of telehealth services has highlighted a major advantage of VC, namely that it improves continuity of care. Patients can have VVs when face-to-face interactions are not possible, and telehealth services may improve access to health care providers, offer tools that support self-care, and help patients receive information about the appropriate level of care for their current concerns or symptoms. The nature of telehealth will help bolster newly formed accountable care organizations (ACOs), such as the Mayo Clinic ACO. The VC model better supports connected care that advances ACO goals regarding cost, quality, access, and patient engagement, and it will also help ACOs prepare for the industry-wide shift toward value-based payment models.
Our experience with VC provider training and change management re-emphasized the importance of documenting the results of telemedicine encounters (ie, assessment outcomes, diagnoses). This information is relevant when patients need quick referrals back to primary care for vaccine updates, care for chronic conditions, or other services. Such efforts will help sustain continuous population management, a central element of all ACO programs.
Discussion
Although the importance and indispensability of functional support and practice partnerships 6 were well known during deployment of the telemedicine model, challenges remain that must be considered during the development of new programs. Enterprise-level collaborations can be difficult to achieve because they require leadership’s commitment and continual support for developing, expending, optimizing, and sustaining new programs. Provider and patient engagement is another key to success. Transparent communication and information sharing between leadership and frontline staff and between care providers and patients have also proven vital to this success.
The multidisciplinary VC committee benefitted from the close collaboration, transparent cross-functional communication, and information sharing between departments, practices, and committee members. This approach enabled us to identify an effective bundling strategy for employers that allowed easy access to extended services or tools within the patient portal. It also facilitated development of customized features, such as specific triage telephone numbers to coordinate care, and other options that are being considered to better meet patient needs.
We acknowledge limitations to this study. The project was conducted with the equipment and resources that were available at our institution at the start of the pandemic. Compared with smaller institutions, our institution may have had more resources available that could be used to support VV. However, these differences possibly will be less pronounced in the future because the increasing demand for VV likely will prompt institutions to budget more resources toward its support. More broadly, additional provider and staff training and change management will be necessary when resources that are currently dedicated to the institutional COVID-19 response are reverted back to their normal operations. We also were affected initially by the limited availability of staff with the appropriate technologic expertise because of the high demand for those employees across the institution at the start of the pandemic. We anticipate the need for continued development of on-demand telemedicine options and integration of consultations that require in-person assessment (eg, laboratory tests, imaging), and we are pursuing other efforts to smooth workflows between areas of health care delivery and to improve the patient experience overall.
Our institution recently was awarded a $1 million grant to further support the goal of achieving 30% VV use across the enterprise by 2030. The work of the multidisciplinary committee described here is just the start, and the new VC era ahead is yet to be explored.
Conclusion
In summary, we described our patient-centered VC model and expansion projects that were established to ensure consistency in the patient experience and accessibility to appropriate care. These VVs were as welcoming and reassuring for patients as in-person visits and enhanced continuity of care. The acute patient symptoms that we chose to manage with VVs have proven appropriate. Patients were successfully treated remotely, and VVs provided a robust system that met the patients’ and providers’ expectations for care. We continue to maintain high-quality care and prioritize the safety of our patients and staff as we embark on expanding the enhanced model of care for the postpandemic era.
Any organizations that are considering deploying a sustainable VC program must put patient needs and safety at the center of their model. We urge organizations to seize the opportunity within this crisis to agilely adjust and advance any emergency-response solutions to serve a longer-term purpose, just as our institution collaboratively and strategically worked toward realizing new care delivery models.
Acknowledgments
June Oshiro, PhD, ELS, Mayo Clinic, substantively edited the manuscript. The Scientific Publications staff at Mayo Clinic provided proofreading, administrative, and clerical support.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Joseph W. Furst  https://orcid.org/0000-0002-2778-7515
https://orcid.org/0000-0002-2778-7515
References
- 1. Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. Updated June 10, 2020. Accessed October 28, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html
- 2. Demaerschalk BM, Blegen RN, Ommen SR. Scalability of telemedicine services in a large integrated multispecialty health care system during COVID-19. Telemed J E Health. 2021;27(1):96-98. doi: 10.1089/tmj.2020.0290. [DOI] [PubMed] [Google Scholar]
- 3. Lokken TG, Blegen RN, Hoff MD, Demaerschalk BM. Overview for implementation of telemedicine services in a large integrated multispecialty health care system. Telemed J E Health. 2020;26(4):382-387. doi: 10.1089/tmj.2019.0079 [DOI] [PubMed] [Google Scholar]
- 4. Businesswire. Telehealth patient satisfaction surges during pandemic but barriers to access persist, JD power finds. Updated October 1, 2020. Accessed October 28, 2021. https://www.businesswire.com/news/home/20201001005094/en/Telehealth-Patient-Satisfaction-Surges-During-Pandemic-but-Barriers-to-Access-Persist-J.D.-Power-Finds
- 5. Business Group on Health. Large US employers accelerating adoption of virtual care, mental health services for 2021, Business group on health survey finds. Updated August 18, 2020. Accessed October 28, 2021. https://www.businessgrouphealth.org/en/who-we-are/newsroom/press-releases/large-us-employers-accelerating-adoption-of-virtual-care-mental-health-services-for-2021
- 6. Kreofsky BLH, Blegen RN, Lokken TG, Kapraun SM, Bushman MS, Demaerschalk BM. Sustainable telemedicine: designing and building infrastructure to support a comprehensive telemedicine practice. Telemed J E Health. 2018;24(12):1021-1025. doi: 10.1089/tmj.2017.0291 [DOI] [PubMed] [Google Scholar]