Abstract
Background:
Despite an abundance of injury research focusing on European professional soccer athletes, there are limited injury data on professional soccer players in the United States.
Purpose:
To describe the epidemiology of injury across multiple years in Major League Soccer (MLS) players.
Study Design:
Descriptive epidemiology study.
Methods:
A web-based health management platform was used to prospectively collect injury data from all MLS teams between 2014 and 2019. An injury was defined as an incident that required medical attention and was recorded into the health management platform anytime over the course of the 2014-2019 seasons. Injuries and exposure data were recorded in training and match settings to calculate injury incidence.
Results:
A total of 9713 injuries were recorded between 2014 and 2019. A mean 1.1 injuries per year per player were identified, with midfielders sustaining the largest number of injuries. The most common injuries were hamstring strains (12.3%), ankle sprains (8.5%), and adductor strains (7.6%). The mean time missed per injury was 15.8 days, with 44.2% of injuries resulting in no days missed. Overall injury incidence was 8.7 per 1000 hours of exposure, declining over the course of the investigation, with a 4.1-times greater mean incidence during matches (14.0/1000 h) than training (3.4/1000 h).
Conclusion:
Between 2014 and 2019, the most commonly reported injuries in MLS players were hamstring strains, ankle sprains, and adductor strains. Injury incidence during matches was 4.1 times greater when compared with training, while overall injury incidence was found to decline during the course of the study period.
Keywords: Major League Soccer, injury incidence, professional soccer, injury, hamstring, ankle
With >3 billion fans and 270 million athletes participating across 200 countries globally, soccer represents the world’s most popular sport. 18 As a complex contact sport, soccer is associated with high injury rates, with epidemiology studies indicating that professional soccer players sustain 4 to 35 injuries per 1000 hours of exposure. †† Owing to increasing speed and intensity, injuries have been reported to occur at a higher incidence in professional soccer players than amateur athletes. 2,12,36 Prior investigations have indicated that injuries occur more frequently during matches than training, 12,15,26 with muscle injuries representing up to 37% of all time-loss injuries in professional male soccer players. 17,37 Moreover, because of the unique demands of the game, the incidence of lower extremity injuries far exceeds the incidence of injuries to the upper extremities in professional players. 13,15,22,37
The majority of studies related to injury epidemiology in professional soccer players have focused on athletes participating in European professional leagues, ‡‡ with limited studies of athletes participating professionally in Africa, 4 Asia, 2,11 and Australia. 20 Moreover, several epidemiology studies have focused on injury incidence over the course of a single season or specific tournaments, following select teams within a league or including only match competition over multiple seasons. As such, no current investigation has analyzed injury incidence for all teams within the same league over multiple seasons. In the current study, we examined true exposure and injury incidence data among players in Major League Soccer (MLS).
Since its inception in 1996, MLS has grown to 26 teams, with plans for expansion in the coming years. The growth of MLS has outpaced studies describing its injury patterns, with just 1 prior study 29 documenting injury incidence from its inaugural season in 1996. In response, MLS established a league-wide injury database in 2010 to prospectively collect injury data with the aim of tracking injury incidence as a means of improving injury prevention program education and implementation. The purpose of the present study was to describe the epidemiology of the most commonly reported injuries in professional soccer players participating in MLS between 2014 and 2019. On the basis of prior literature, we hypothesized a high incidence of injuries in players, with lower extremity injuries being the most typical. 17,38,39
Methods
Study Population
Before study initiation, research approval was obtained from the Major League Soccer Medical Assessment Research Committee and the Rush University Institutional Review Board. Data between 2014 and 2019 were reviewed from Healthe Athlete (Cerner Corp): a secure web-based athlete health management platform that combines injury management, personal health records, and advanced reporting to efficiently manage athlete health and health-related data. The Healthe Athlete database comprises injury data from all MLS teams, including training and match data. Per MLS guidelines, all player injury data must be prospectively entered into the Healthe Athlete database by MLS team athletic trainers during the preseason, regular season, and postseason.
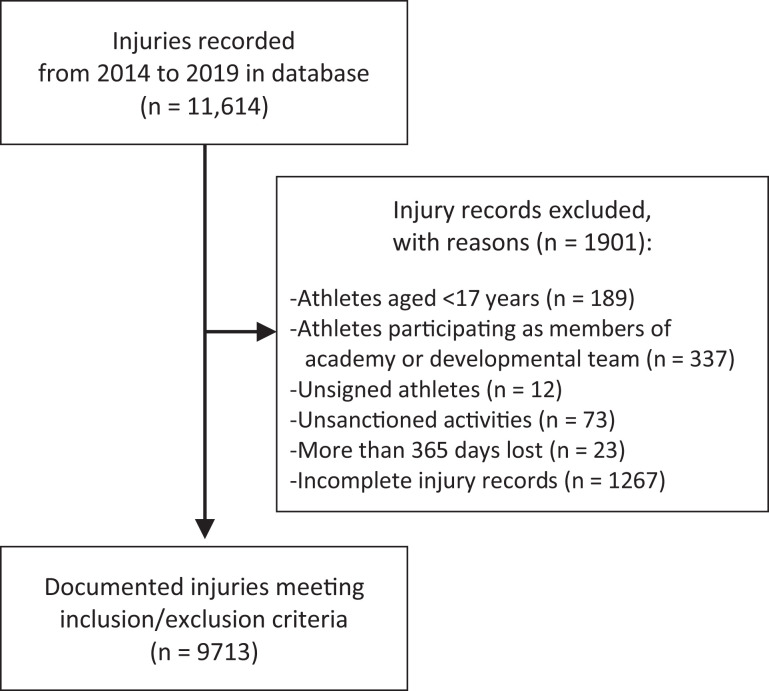
Injury was defined as an incident that required medical attention and was recorded into the health management platform anytime over the course of the 2014-2019 preseason, regular season, or postseason. Recorded data were as follows: player position (forward, midfielder, defender, goalkeeper), injury date based on year, injury setting (conditioning, match, team training, or sanctioned training), and body region of injury (spine, head/neck, upper extremity, thorax, abdomen, pelvis, hip, thigh, knee, leg, ankle, or foot), as well as total days, matches, and training sessions missed because of injury. Data were excluded for players participating in unsanctioned activities, players for whom injury setting was not recorded, players aged <17 years, and players who sustained injuries while not participating as a signed member of an MLS team (Figure 1). Furthermore, injuries resulting in >365 days missed were excluded to avoid recording inconsistencies and outliers.
Figure 1.
Flowchart of Major League Soccer athletes meeting inclusion and exclusion criteria.
Statistical Analysis
The recorded data in the Healthe Athlete database between 2014 and 2019 were analyzed. Data are presented as means with associated ranges. The total number of recorded injuries over the study period, as well injuries recorded during each year, were evaluated by injury setting (conditioning, match, training, sanctioned activity) and body region (spine, head/neck, upper extremity, thorax, abdomen, pelvis, hip, thigh, knee, leg, ankle, and foot). The top 5 injuries within each body region were then analyzed by year of injury and player position, as well as total number of days, matches, and training sessions missed because of injury. Injury incidence was calculated as the number of injuries per 1000 hours of exposure for the number of recorded injuries overall and during each year; it was also recorded for matches and training sessions. The formulas used for exposure rate and incidence were calculated using the total number of matches and training sessions performed each year:
Results
Injury and Player Characteristics
A total of 11,614 injuries were recorded between 2014 and 2019. After applying exclusion criteria, we documented 9713 injuries in 1472 individual players. The mean number of recorded injuries per athlete was 1.1 per year (range, 1-55 injuries). Athlete age at the time of injury was 27.0 ± 4.3 years (mean ± SD; range, 17.0-42.2 years).
Midfielders represented the most commonly injured position, representing 37.6% (n = 3650 injuries) of injuries, followed by defenders (34.1%; n = 3314), forwards (17.8%; n = 1731), and goalkeepers (10.5%; n = 1018). Per injury, players missed on average 15.8 days (range, 0-351 days), 1.3 games (range, 0-34 games), and 4.3 practices (range, 0-154 practices). An overall 45.0% (n = 4371) of injuries resulted in no days missed. The majority of injuries occurred during matches (51.1%) and training (46.6%) (Table 1).
Table 1.
Injuries by Setting, Overall, and During Each MLS Season, 2014-2019 a
| Injuries, n (%) | |||||||
|---|---|---|---|---|---|---|---|
| Injury Setting | Overall | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
| Conditioning | 62 (0.7) | 13 | 21 | 11 | 7 | 5 | 5 |
| Match | 4968 (51.1) | 886 | 899 | 838 | 778 | 786 | 781 |
| Team training | 4524 (46.6) | 805 | 849 | 712 | 714 | 722 | 722 |
| Sanctioned training | 159 (1.6) | 20 | 43 | 54 | 20 | 11 | 11 |
a MLS, Major League Soccer.
Injury Type
The most typically reported injuries based on body region across all 6 years were to the thigh (30.8% of all injuries), followed by the knee (13.5%) and ankle (12.5%) (Table 2). The 5 most common injuries were hamstring strains (12.3% of all injuries), ankle sprains (8.5%), adductor strains (7.6%), rectus strains (5.1%), and foot contusions (3.3%) (Table 3). Of the top 60 injuries by body region, leg fractures led to the largest number of mean days (120.9 days), matches (11.6 matches), and training sessions (30.9 training sessions) missed.
Table 2.
Injuries by Body Region, Overall, and During Each MLS Season, 2014-2019 a
| Injuries, n (%) | |||||||
|---|---|---|---|---|---|---|---|
| Body Region | Overall | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
| Spine | 352 (3.6) | 85 | 83 | 77 | 57 | 72 | 62 |
| Head/neck | 707 (7.3) | 117 | 116 | 128 | 131 | 108 | 127 |
| Upper extremity | 773 (8.0) | 130 | 139 | 126 | 149 | 122 | 117 |
| Thorax | 112 (1.2) | 20 | 20 | 29 | 12 | 22 | 16 |
| Abdomen | 90 (0.9) | 19 | 16 | 21 | 13 | 13 | 8 |
| Pelvis | 241 (2.5) | 41 | 34 | 29 | 27 | 33 | 78 |
| Hip | 373 (3.8) | 83 | 84 | 61 | 51 | 59 | 45 |
| Thigh | 2987 (30.8) | 539 | 588 | 502 | 412 | 504 | 462 |
| Knee | 1316 (13.5) | 226 | 265 | 250 | 211 | 197 | 187 |
| Leg | 704 (7.2) | 55 | 70 | 70 | 123 | 72 | 92 |
| Ankle | 1210 (12.5) | 241 | 231 | 178 | 191 | 195 | 194 |
| Foot | 848 (8.7) | 168 | 166 | 144 | 142 | 127 | 131 |
| Total | 9713 | 1724 | 1812 | 1615 | 1519 | 1524 | 1519 |
a MLS, Major League Soccer.
Table 3.
Injuries Based on Type and Player Position a
| No. of Injuries | Injury-Based Absence, Mean (Range), n | |||||||
|---|---|---|---|---|---|---|---|---|
| Injury Type | Overall | Forward | Midfielder | Defender | Goalkeeper | Days Missed | Matches Missed | Trainings Missed |
| Spine | ||||||||
| Lumbar soreness/tightness | 49 | 12 | 8 | 20 | 9 | 5.8 (0-41) | 0.5 (0-6) | 1.1 (0-11) |
| Lumbar spasm | 48 | 12 | 16 | 11 | 9 | 4.2 (0-20) | 0.5 (0-7) | 1.3 (0-10) |
| Lumbar pain/irritation | 42 | 5 | 17 | 10 | 10 | 9.4 (0-69) | 0.9 (0-7) | 2.1 (0-24) |
| Cervical strain | 36 | 6 | 8 | 17 | 5 | 4.4 (0-46) | 1.1 (0-3) | 4.7 (0-138) |
| Cervical spasm | 26 | 8 | 9 | 6 | 3 | 2.4 (0-36) | 0.2 (0-4) | 0.8 (0-14) |
| Head/neck | ||||||||
| Concussion | 310 | 66 | 43 | 148 | 53 | 25.9 (0-332) | 2.3 (0-34) | 8.5 (0-150) |
| Facial laceration | 79 | 13 | 24 | 38 | 4 | 2.9 (0-34) | 0.05 (0-2) | 0.16 (0-4) |
| Tooth avulsion/fracture | 56 | 5 | 15 | 28 | 8 | 0.3 (0-8) | 0.02 (0-1) | 0.9 (0-2) |
| Eye abrasion/laceration | 47 | 7 | 13 | 21 | 6 | 1 (0-12) | 0 | 0.09 (0-2) |
| Head abrasion/laceration | 40 | 0 | 39 | 1 | 0 | 1 (0-27) | 0 | 0.1 (0-1) |
| Upper extremity | ||||||||
| Shoulder sprain/strain | 136 | 21 | 31 | 46 | 38 | 12.0 (0-331) | 0.6 (0-23) | 1.7 (0-37) |
| Wrist sprain | 69 | 11 | 15 | 17 | 26 | 4.6 (0-86) | 0.03 (0-1) | 0.06 (0-3) |
| Digital sprain | 64 | 3 | 15 | 16 | 30 | 0.6 (0-34) | 0.05 (0-2) | 0.1 (0-4) |
| Thumb sprain | 51 | 2 | 14 | 20 | 15 | 7.2 (0-196) | 0.3 (0-5) | 0.7 (0-13) |
| Digit dislocation | 42 | 3 | 7 | 9 | 23 | 3.7 (0-111) | 0.4 (0-14) | 1.4 (0-50) |
| Thorax | ||||||||
| Rib contusion | 64 | 17 | 1 | 25 | 4 | 2.2 (0-24) | 0.15 (0-2) | 0.7 (0-9) |
| Rib fracture-dislocation | 14 | 0 | 14 | 0 | 0 | 8.4 (0-24) | 0.9 (0-3) | 1.9 (0-8) |
| Thoracic muscle spasm | 10 | 4 | 2 | 3 | 1 | 18.6 (0-93) | 0 | 1.2 (0-5) |
| Thoracic contusion | 6 | 0 | 3 | 2 | 1 | 0.8 (0-5) | 0 | 0 |
| Pneumothorax | 4 | 1 | 2 | 1 | 0 | 61.3 (8-158) | 3.8 (0-7) | 11.5 (0-26) |
| Abdomen | ||||||||
| Abdominal strain | 64 | 10 | 31 | 16 | 7 | 25.7 (0-185) | 1.9 (0-17) | 5.7 (0-53) |
| Abdominal hernia | 10 | 3 | 4 | 3 | 0 | 68 (2-196) | 7.9 (0-22) | 26.9 (0-80) |
| Abdominal soreness/tightness | 7 | 1 | 2 | 3 | 1 | 17.7 (0-78) | 2.9 (0-15) | 9.8 (0-53) |
| Abdominal inflammation/irritation | 6 | 0 | 2 | 3 | 1 | 6.2 (0-31) | 0 | 0.6 (0-2) |
| Abdominal contusion | 4 | 0 | 2 | 2 | 0 | 12.3 (0-32) | 1.5 (0-3) | 1.3 (0-5) |
| Pelvis | ||||||||
| Athletic pubalgia | 57 | 13 | 18 | 24 | 2 | 32.7 (0-201) | 2.1 (0-14) | 7.4 (0-48) |
| Pelvic strain | 47 | 7 | 20 | 17 | 3 | 25.6 (0-155) | 1.3 (0-16) | 5.8 (0-92) |
| Pelvis inflammation/irritation | 42 | 12 | 19 | 10 | 1 | 23.1 (0-262) | 2.3 (0-34) | 4.4 (0-126) |
| Pelvic soreness/tightness | 39 | 5 | 21 | 6 | 7 | 2.2 (0-20) | 0.3 (0-3) | 1.6 (0-26) |
| Pelvic contusion | 24 | 6 | 6 | 10 | 2 | 4.3 (0-18) | 0.17 (0-1) | 0.7 (0-8) |
| Hip | ||||||||
| Hip strain | 129 | 23 | 56 | 36 | 14 | 13.2 (0-223) | 0.7 (0-7) | 2.0 (0-22) |
| Impingement | 70 | 13 | 36 | 16 | 5 | 16.4 (0-271) | 0.8 (0-28) | 2.8 (0-82) |
| Hip soreness/tightness | 70 | 8 | 29 | 18 | 15 | 6.4 (0-52) | 0.7 (0-8) | 1.6 (0-26) |
| Hip contusion | 66 | 12 | 12 | 39 | 3 | 6.2 (0-91) | 0.4 (0-8) | 1.6 (0-40) |
| Hip inflammation/irritation | 32 | 3 | 14 | 13 | 2 | 7.6 (0-38) | 0.8 (0-7) | 2.5 (0-23) |
| Thigh | ||||||||
| Hamstring strain | 1190 | 258 | 396 | 463 | 73 | 18.7 (0-167) | 1.9 (0-19) | 5.9 (0-59) |
| Adductor strain | 740 | 113 | 330 | 245 | 52 | 12.3 (0-339) | 0.9 (0-19) | 3.2 (0-67) |
| Quadriceps strain | 491 | 87 | 211 | 150 | 43 | 20.8 (0-288) | 2.0 (0-33) | 6.2 (0-114) |
| Rectus contusion | 222 | 39 | 52 | 123 | 8 | 4.7 (0-113) | 0.3 (0-12) | 1.2 (0-34) |
| Hamstring inflammation/irritation | 110 | 26 | 46 | 30 | 8 | 8.2 (0-12) | 0.7 (0-12) | 2.1 (0-38) |
| Knee | ||||||||
| MCL strain | 267 | 48 | 102 | 105 | 12 | 22.6 (0-227) | 2.2 (0-26) | 7.1 (0-92) |
| Patellar tendinitis | 174 | 24 | 99 | 27 | 24 | 5.1 (0-191) | 0.4 (0-10) | 1.3 (0-28) |
| Contusion | 144 | 20 | 53 | 67 | 4 | 5.0 (0-66) | 0.5 (0-7) | 1.6 (0-31) |
| Meniscal injury | 104 | 13 | 46 | 35 | 10 | 59.3 (0-351) | 4 (0-34) | 13.4 (0-154) |
| Soreness/tightness | 64 | 6 | 30 | 18 | 10 | 9.1 (0-327) | 0.6 (0-24) | 1.0 (0-13) |
| Leg | ||||||||
| Strain | 255 | 48 | 110 | 77 | 20 | 19.8 (0-146) | 2.1 (0-17) | 6.7 (0-66) |
| Contusion | 223 | 50 | 50 | 107 | 16 | 3.9 (0-168) | 0.2 (0-7) | 0.7 (0-11) |
| Soreness/tightness | 96 | 15 | 52 | 18 | 11 | 5.9 (0-62) | 0.4 (0-7) | 1.2 (0-19) |
| Fracture | 19 | 0 | 8 | 10 | 1 | 120.9 (22-342) | 11.6 (0-34) | 30.9 (0-140) |
| Spasm | 17 | 4 | 6 | 6 | 1 | 8.4 (0-89) | 0.3 (0-4) | 1 (0-13) |
| Ankle | ||||||||
| Ankle sprain | 821 | 159 | 302 | 307 | 53 | 15.5 (0-348) | 1.1 (0-34) | 3.6 (0-149) |
| Ankle contusion | 152 | 32 | 39 | 70 | 11 | 10.7 (0-201) | 1.0 (0-18) | 2.7 (0-86) |
| Achilles tendinitis | 86 | 11 | 56 | 12 | 7 | 12.3 (0-127) | 0.8 (0-17) | 3.1 (0-54) |
| Ankle impingement | 41 | 6 | 18 | 13 | 4 | 12.9 (0-83) | 1.3 (0-11) | 4.5 (0-34) |
| Ankle tendinitis | 39 | 9 | 20 | 8 | 2 | 12.8 (0-158) | 1.9 (0-31) | 5.8 (0-84) |
| Foot | ||||||||
| Contusion | 316 | 76 | 80 | 140 | 20 | 5.3 (0-225) | 0.4 (0-14) | 1.2 (0-44) |
| Foot strain | 96 | 23 | 29 | 36 | 8 | 13 (0-287) | 1.3 (0-20) | 3.8 (0-80) |
| Plantar fasciitis | 70 | 9 | 36 | 11 | 14 | 13.2 (0-287) | 0.4 (0-6) | 1.3 (0-28) |
| Toe sprain | 52 | 11 | 20 | 18 | 3 | 17.2 (0-213) | 1.1 (0-22) | 3.3 (0-57) |
| Toe contusion | 46 | 8 | 12 | 25 | 1 | 3.9 (0-35) | 0.3 (0-5) | 1.0 (0-14) |
a MCL, medial collateral ligament.
Injury Incidence
Across the study period, players had a total exposure time of 1,107,829 hours during matches and trainings. The overall injury incidence was 8.7 injuries per 1000 hours of exposure during matches and trainings, which was 4.1 times greater during matches than training (Table 4).
Table 4.
Injury Incidence Based on Season a
| MLS, n | Injury Incidence per 1000 h | |||||
|---|---|---|---|---|---|---|
| Season | Teams | Matches | Trainings | Overall b | Matches | Training |
| 2014 | 19 | 655 | 3116 | 9.9 | 15.5 | 3.9 |
| 2015 | 20 | 691 | 3009 | 10.7 | 15.2 | 4.4 |
| 2016 | 20 | 691 | 3193 | 9.0 | 14.6 | 3.2 |
| 2017 | 22 | 759 | 3310 | 8.2 | 13.5 | 3.1 |
| 2018 | 23 | 793 | 3465 | 7.8 | 13.3 | 3.0 |
| 2019 | 24 | 829 | 3620 | 7.5 | 13.0 | 2.9 |
| Cumulative | 4418 | 19,713 | 8.7 | 14.0 | 3.4 | |
a MLS, Major League Soccer.
b Including matches and trainings.
Discussion
The primary findings of the study were that between 2014 and 2019, a total of 9713 unique injuries were recorded in MLS players, with each athlete sustaining a mean of 1.1 injuries per year. Midfielders represented the largest number of injuries, followed by defenders. The most often reported injuries based on body region were to the thigh, knee, and ankle, with hamstring strains, ankle sprains, and adductor strains the most commonly reported injuries. Injury incidence during matches was 4.1 times greater as compared with training, while the annual injury incidence declined over the course of the study period.
The overall injury incidence rate of 8.7/1000 h between 2014 and 2019 in MLS players is within the range of injury incidence rates in studies 12,15,21,25 evaluating professional European soccer players. In a study evaluating 1743 players from 27 teams across 10 European countries competing in the Union of European Football Associations Champions League between 2001 and 2012, Ekstrand et al 12 cited an overall injury rate of 7.6/1000 h. Of note, while our study included all injuries regardless of time lost, the study by Ekstrand et al included only injuries in which time loss was recorded. In the sole other investigation reporting on injury rates in MLS players, Morgan and Oberlander 29 noted an injury rate of 6.2/1000 h during the inaugural MLS season in 1996. Moreover, when prospectively analyzing injuries in professional Japanese soccer players between 1993 and 2007, Aoki et al 2 indicated an injury incidence rate of 19.11 to 24.37/1000 h; however, just the injuries in which >7 days were lost were included. As such, despite the use of various methodologies, we found that MLS athletes were not at substantially higher or lower risk for injury based on overall mean injury incidence when compared with prior investigations.
Players sustained injuries most commonly during matches, occurring with an approximately 4.1-times greater incidence versus training. This finding is in agreement with multiple prior investigations similarly reporting the higher incidence of injuries during match competition. 12,15,25 Ekstrand et al 13 cited a match injury rate 7 times greater than that with training (relative risk, 6.7; P < .001), while Morgan and Oberlander 29 found an injury rate of 35.3/1000 h of exposure during match competition, as opposed to only 2.9/1000 h for training. Similarly, Nilsson et al 30 indicated a 20-fold higher rate of head and neck injuries during match play than training, with a 78-fold higher rate of concussions. This finding is likely accounted for by the increased intensity and greater probability of contact that occur during competition than training. 2
Overall, a decline in injury incidence with each successive year of study was appreciated. Aoki et al 2 similarly cited a decline in injury rates among the top-division Japanese professional soccer leagues over a 15-year study period, despite no match rule changes. This trend was also noted in the prospective cohort study by Hägglund et al, 21 in which the authors evaluated injury rates in elite Swedish soccer players during 2 seasons (1982 and 2001). The authors indicated an injury incidence of 8.3/1000 h in 1982 versus 7.8/1000 h in 2001. Despite a progressive increase in exposure with each successive year of study, a concurrent increase in injury incidence was not appreciated, as in our investigation. Injury identification often relies on player reporting, which may cause medical staff to restrict participation. It is possible that players increasingly underreported injuries owing to fear of such restriction. While the exact reasons behind this decline are unclear, knowledge among teams and leagues regarding injury rates from previously published studies may play a contributing role as related to emphasizing the importance of athlete safety and injury prevention. 2
The most often recorded injuries over the 6 MLS years consisted of hamstring strains, ankle sprains, and adductor strains. These injuries are consistent with the most frequent injury types identified by Ekstrand et al, 12 who cited hamstring (12.8% of all injuries), adductor (9.2%), and ankle (6.9%) sprains as the most common injuries among the 1743 professional European soccer players. Moreover, Morgan and Oberlander 29 indicated that 77% of recorded injuries (n = 197/256) involved the lower extremities during the inaugural MLS season. Several other investigations examining the epidemiology of soccer-related injuries at the professional level have similarly identified that they most commonly affect the lower extremities, citing the unique demands placed on soccer athletes. 12,17,29 Specifically, injuries to the 4 major muscle groups of the lower extremity (adductors, hamstring, quadriceps, and calf) have been shown to account for >90% of all muscle injuries in professional soccer. 14 Hamstring injuries are typically encountered because of the high speeds at which players compete, with the demand for frequent acceleration, deceleration, and change of direction. 14,17 The ankle is at high risk for inversion injury during running, with passing and projecting the ball, which is most often performed by striking the ball with the medial aspect of the foot and forefoot and thereby placing the ankle in a vulnerable abducted and externally rotated position. 29 Meanwhile, injuries to the quadriceps musculature are prevalent because of the kicking actions. 33 As such, injury prevention measures should continue to focus on minimizing the risk for injury occurrence as well as time lost, especially for injuries to the lower extremities.
In contrast, injuries to the upper extremity and the head and neck occur with less frequency. Our study revealed that upper extremity injury accounts for 8.0% of injuries. In an investigation of 2914 players from 57 elite European soccer teams, Ekstrand et al 13 found that over the course of the 2001-2011 seasons, upper extremities accounted for 3% of the total injury incidence (n = 355/11,750 injuries). The authors also reported that upper extremity injuries resulted in 23 ± 34 days lost from play, with goal keepers possessing a 5-times greater incidence of upper extremity injuries when compared with field players. Meanwhile, head and neck injuries represented 7.3% of injuries in our investigation. This is in line with previous studies 1,30 finding that head injuries account for 2% to 22% of all injuries, with neck injuries being less frequent.
Concussions were the most often reported injury to the head and neck, while resulting in the longest time loss from competition. The high incidence of concussions has been similarly cited in prior studies 2,19 examining professional soccer players in the Japanese and Federation Internationale de Football Association international competitions. Soccer-related concussions have been postulated to be more prevalent than historically reported, 6 although many concussions likely still go unreported. 7,30 Three consensus statements on concussion in sport have been published, 3,27,28 recommending a minimum of 5 days to proceed through a full rehabilitation protocol after symptoms have resolved. Since athletes after a concussion are at higher risk of and more susceptible to future and more severe reinjury, 9 proper recognition, time off from play, and rehabilitation are essential to minimize the risk of sequelae. 34 As such, preventative therapies directed at injury prevention are vital to maintain athlete health and safety.
When injury rate was examined by athlete position, midfielders sustained the largest number of injuries, followed by defenders. The high injury incidence in midfielders is likely attributed to the dual offensive/defensive role that these athletes play on the field, requiring constant running with frequent change of direction and contact. Meanwhile, defenders had the largest number of head and neck injuries 30 likely because of the increased contact that they experience in protecting the ball from opposing teams, initiating tackles, and engaging in duels heading the ball. While goalkeepers possessed a lower rate of injury than did field athletes, 2 they have been reported to have a higher incidence of upper extremity injuries 13 owing to the unique demands of the position when compared with field athletes. Thus, injury-specific recommendations should be based on athlete position as a means of minimizing the risk of common injuries according to positional demands.
Limitations
This investigation was not without limitations. All injury data, including injury type, age, position, and time missed, as well as exposure times, were obtained from the records inputted in the Healthe Athlete database. As such, the reliability was dependent on accurate and timely data entry by athletic training staff from each team. Utilization of the Healthe Athlete database was limited in that it did not capture intrinsic characteristics that may have been predictive of injury, such as the role of previous injuries, athlete strength, flexibility, and race. 23 Prior studies have shown that soccer players may be more prone to injuries during the last 15 minutes of each half secondary to athlete fatigue 15,25 with increased game congestion 5 ; however, these variables were inconsistently reported and not included in the final analysis. Moreover, prior investigations have demonstrated that extrinsic factors, namely ground surface and weather conditions, are associated with injury occurrence, 4,16,32 although these variables were also infrequently included in the database.
Data were not available for injury diagnosis based on imaging workup or for those injuries requiring surgical versus nonsurgical intervention. While match-related factors such as type, location (home vs away), and result have been shown to influence injury rates, 8,11,23,24 these factors were not analyzed in our investigation. This investigation analyzed male professional soccer players only; therefore, the injury incidence in female professional soccer players cannot be inferred. Finally, caution must be exercised when interpreting data from our analysis against other epidemiology studies owing to the use of differing methodologies—namely, the lack of consensus regarding the definition of an injury, as well as differences in data collection among studies.
Despite these limitations, this is the first comprehensive analysis of injury in professional soccer players in MLS. This is also the first study to prospectively analyze the injury characteristics of all teams within the same league, including true incidence data for all matches and trainings over multiple years. The data entered into the health management platform since its inception have become more consistent and complete; therefore, future studies will offer a more in-depth analysis.
Conclusion
Between 2014 and 2019, the most commonly reported injuries in MLS players were hamstring strains, ankle sprains, and adductor strains. Injury incidence during matches was 4.1 times greater when compared with trainings, while overall injury incidence declined during the course of the study period. Additional studies identifying intrinsic and extrinsic risk factors for injury in MLS athletes are warranted to further injury education and preventative measures to minimize the risk of injury and time lost while maximizing player health and team performance.
Footnotes
Final revision submitted July 1, 2021; accepted August 10, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: B.F. has received grants from Arthrex and Stryker, research support from Smith & Nephew, education payments from Medwest, consulting fees from Stryker, and personal fees from Elsevier and has stock/stock options in Jace Medical. M.D.C. has received education payments from Smith & Nephew and hospitality payments from Abbott, Misonix, and Stryker. D.H. has received hospitality payments from Horizon Pharma and Sentnyl Therapeutics. B.R.M. has received consulting fees from Arthrex, Biomarin, DePuy, and Exactech; speaking fees from Arthrex; and hospitality payments from Aesculap, Bioventus, Ferring, Flexion, Sanofi, and Stryker. L.L. has received consulting fees from Aesculap and hospitality payments from Ferring, Fidia, Flexion, Orthofix, Pacira, Sanofi, and Si-bone. E.G. has received education payments from Sequoia; consulting fees from Arthrex, Ipsen, MedShape, and Zimmer; royalties from Arthrex and Zimmer; honoraria from In2Bones; and hospitality payments from ACELL, Evolution Surgical, Integra, Steelhead Surgical, and Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Rush University Medical Center (ORA No. 20111908-IRB01).
References
- 1. Al-Kashmiri A, Delaney J. Head and neck injuries in football (soccer). Trauma. 2006;8:189–195. [Google Scholar]
- 2. Aoki H, O’Hata N, Kohno T, et al. A 15-year prospective epidemiological account of acute traumatic injuries during official professional soccer league matches in Japan. Am J Sports Med. 2012;40(5):1006–1014. [DOI] [PubMed] [Google Scholar]
- 3. Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Azubuike SO, Okojie OH. An epidemiological study of football (soccer) injuries in Benin City, Nigeria. Br J Sports Med. 2009;43(5):382–386. [DOI] [PubMed] [Google Scholar]
- 5. Bengtsson H, Ekstrand J, Hägglund M. Muscle injury rates in professional football increase with fixture congestion: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):743–747. [DOI] [PubMed] [Google Scholar]
- 6. Boden BP, Kirkendall DT, Garrett WE, Jr. Concussion incidence in elite college soccer players. Am J Sports Med. 1998;26(2):238–241. [DOI] [PubMed] [Google Scholar]
- 7. Broglio SP, Vagnozzi R, Sabin M, et al. Concussion occurrence and knowledge in Italian football (soccer). J Sports Sci Med. 2010;9(3):418–430. [PMC free article] [PubMed] [Google Scholar]
- 8. Carling C, Orhant E, LeGall F. Match injuries in professional soccer: inter-seasonal variation and effects of competition type, match congestion and positional role. Int J Sports Med. 2010;31(4):271–276. [DOI] [PubMed] [Google Scholar]
- 9. Delaney JS, Lacroix VJ, Leclerc S, et al. Concussions among university football and soccer players. Clin J Sport Med. 2002;12(6):331–338. [DOI] [PubMed] [Google Scholar]
- 10. Dvorak J, Junge A. Football injuries and physical symptoms: a review of the literature. Am J Sports Med. 2000;28(5):S3–S9. [DOI] [PubMed] [Google Scholar]
- 11. Eirale C, Farooq A, Smiley FA, et al. Epidemiology of football injuries in Asia: a prospective study in Qatar. J Sci Med Sport. 2013;16(2):113–117. [DOI] [PubMed] [Google Scholar]
- 12. Ekstrand J, Hägglund M, Kristenson K, et al. Fewer ligament injuries but no preventive effect on muscle injuries and severe injuries: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):732–737. [DOI] [PubMed] [Google Scholar]
- 13. Ekstrand J, Hägglund M, Törnqvist H, et al. Upper extremity injuries in male elite football players. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1626–1632. [DOI] [PubMed] [Google Scholar]
- 14. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 15. Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553–558. [DOI] [PubMed] [Google Scholar]
- 16. Ekstrand J, Nigg BM. Surface-related injuries in soccer. Sports Med. 1989;8(1):56–62. [DOI] [PubMed] [Google Scholar]
- 17. Ekstrand J, Waldén M, Hägglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA Elite Club injury study. Br J Sports Med. 2016;50(12):731–737. [DOI] [PubMed] [Google Scholar]
- 18. FIFA Communications Division. FIFA big count 2006: 270 million people active in football. Published May 31, 2007. https://digitalhub.fifa.com/m/55621f9fdc8ea7b4/original/mzid0qmguixkcmruvema-pdf.pdf
- 19. Fuller CW, Junge A, Dvorak J. A six year prospective study of the incidence and causes of head and neck injuries in international football. Br J Sports Med. 2005;39(suppl 1):i3–i9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gouttebarge V, Hughes Schwab BA, Vivian A, et al. Injuries, matches missed and the influence of minimum medical standards in the A-League professional football: a 5-year prospective study. Asian J Sports Med. 2016;7(1):e31385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hägglund M, Waldén M, Ekstrand J. Exposure and injury risk in Swedish elite football: a comparison between seasons 1982 and 2001. Scand J Med Sci Sports. 2003;13(6):364–370. [DOI] [PubMed] [Google Scholar]
- 22. Hägglund M, Waldén M, Ekstrand J. Injury incidence and distribution in elite football—a prospective study of the Danish and the Swedish top divisions. Scand J Med Sci Sports. 2005;15(1):21–28. [DOI] [PubMed] [Google Scholar]
- 23. Hägglund M, Waldén M, Ekstrand J. Risk factors for lower extremity muscle injury in professional soccer: the UEFA Injury Study. Am J Sports Med. 2013;41(2):327–335. [DOI] [PubMed] [Google Scholar]
- 24. Hägglund M, Waldén M, Ekstrand J. UEFA injury study—an injury audit of European Championships 2006 to 2008. Br J Sports Med. 2009;43(7):483–489. [DOI] [PubMed] [Google Scholar]
- 25. Hawkins RD, Fuller CW. A prospective epidemiological study of injuries in four English professional football clubs. Br J Sports Med. 1999;33(3):196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hawkins RD, Hulse MA, Wilkinson C, et al. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001;35(1):43–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McCrory P, Meeuwisse W, Johnston K, et al. Consensus Statement on Concussion in Sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Br J Sports Med. 2009;43(suppl 1):i76–i90. [DOI] [PubMed] [Google Scholar]
- 29. Morgan BE, Oberlander MA. An examination of injuries in Major League Soccer: the inaugural season. Am J Sports Med. 2001;29(4):426–430. [DOI] [PubMed] [Google Scholar]
- 30. Nilsson M, Hägglund M, Ekstrand J, et al. Head and neck injuries in professional soccer. Clin J Sport Med. 2013;23(4):255–260. [DOI] [PubMed] [Google Scholar]
- 31. Noya Salces J, Gomez-Carmona PM, Moliner-Urdiales D, et al. An examination of injuries in Spanish Professional Soccer League. J Sports Med Phys Fitness. 2014;54(6):765–771. [PubMed] [Google Scholar]
- 32. Orchard J. Is there a relationship between ground and climatic conditions and injuries in football? Sports Med. 2002;32(7):419–432. [DOI] [PubMed] [Google Scholar]
- 33. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300–303. [DOI] [PubMed] [Google Scholar]
- 34. Price J, Malliaras P, Hudson Z. Current practices in determining return to play following head injury in professional football in the UK. Br J Sports Med. 2012;46(14):1000–1003. [DOI] [PubMed] [Google Scholar]
- 35. Stubbe JH, van Beijsterveldt AM, van der Knaap S, et al. Injuries in professional male soccer players in the Netherlands: a prospective cohort study. J Athl Train. 2015;50(2):211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. van Beijsterveldt AM, van de Port IG, Krist MR, et al. Effectiveness of an injury prevention programme for adult male amateur soccer players: a cluster-randomised controlled trial. Br J Sports Med. 2012;46(16):1114–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Waldén M, Hägglund M, Ekstrand J. UEFA Champions League study: a prospective study of injuries in professional football during the 2001-2002 season. Br J Sports Med. 2005;39(8):542–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Walls RJ, Ross KA, Fraser EJ, et al. Football injuries of the ankle: a review of injury mechanisms, diagnosis and management. World J Orthop. 2016;7(1):8–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wong P, Hong Y. Soccer injury in the lower extremities. Br J Sports Med. 2005;39(8):473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]