Abstract
This cohort study examines patterns in prescriptions of dual antiplatelet therapy after publication of important trials and release of updated guidelines.
Recommendations for dual antiplatelet therapy (DAPT; aspirin and clopidogrel) for secondary prevention in patients with acute ischemic stroke have evolved over time. Although long-term DAPT was not recommended because of excessive bleeding risk, the CHANCE (Clopidogrel in High-risk Patients With Acute Non-disabling Cerebrovascular Events) trial1 and the POINT (Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke) trial2 shifted the focus to short-term DAPT (21-90 days) in patients with minor ischemic stroke (National Institutes of Health Stroke Scale [NIHSS] score ≤3) and found that DAPT was effective in reducing the risk of recurrent ischemic stroke. The American Heart Association and American Stroke Association (AHA/ASA) subsequently updated recommendations for DAPT from “risk ≥ benefit” (class III) for routine secondary prevention after ischemic stroke in 2011, to “benefit ≥ risk” (class IIb) for minor ischemic stroke in 2014, to “benefit > > risk” (class IIa) in 2018, and eventually to “benefit > > > risk” (class I, level of evidence A) in 2019.3,4,5,6
Despite guideline recommendations, translation of knowledge from clinical trials to routine practice is often delayed and incomplete. The degree to which physicians in routine clinical practice follow these evidence-based DAPT recommendations remains unknown. The aim of this study was to evaluate discharge antiplatelet prescription patterns after the release of pivotal trials and serial AHA/ASA guideline updates in the US.
Methods
This retrospective cohort study analyzed 1 281 034 patients who were hospitalized for acute ischemic stroke and prescribed antiplatelet therapy at discharge from 2228 hospitals in the Get With The Guidelines–Stroke registry between October 1, 2012, and June 30, 2020 (eFigure in the Supplement). Data on race and ethnicity were recorded by hospital staff from various sources, including patient self-designation, by administrative personnel during the registration process, or on nursing intake forms. Antiplatelets prescribed at discharge were evaluated in 5 periods based on the dates of the CHANCE trial and POINT trial publications and the 2014, 2018, and 2019 AHA/ASA guideline updates. Antiplatelet agents were categorized into 5 groups: (1) aspirin monotherapy; (2) clopidogrel bisulfate monotherapy; (3) DAPT of aspirin and clopidogrel; (4) aspirin and dipyridamole; and (5) other antiplatelet agents, such as ticlopidine hydrochloride, prasugrel, ticagrelor monotherapy, or these drugs in combination with aspirin. The Cochran-Armitage test for trend was used to evaluate the proportions of antiplatelet medication over time. This study was approved by the institutional review board of Duke University, which waived the requirement for informed consent because deidentified data were used. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
All statistical analyses were performed using SAS, version 9.4 (SAS Institute, Inc). Two-sided P < .05 was considered to be statistically significant.
Results
Of 1 281 034 patients (median [IQR] age, 68 [59-78] years; 51.2% [656 364] were men and 48.8% [624 670] women; 3.1% were Asian, 7.9% Hispanic, 20.8% non-Hispanic Black, and 64.1% non-Hispanic White individuals, and 4.1% were individuals of another race [including American Indian or Alaska Native, Native Hawaiian or Pacific Islander, or unable to be determined]), 54.5% received aspirin monotherapy, 12.4% received clopidogrel monotherapy, 30.8% received DAPT, 1.8% received aspirin and dipyridamole, and 0.6% received other antiplatelet agents or combination at discharge. Baseline characteristics were similar across the entire study period (Table).
Table. Baseline Characteristics and Antiplatelet Treatment Patterns Before and After the Publication of Pivotal Trials and AHA/ASA Guideline Updates.
| Characteristics | No. (%) | ||||
|---|---|---|---|---|---|
| Before CHANCE trial (n = 106 725)a | Before AHA/ASA 2014 updates (n = 76 357)b | Before POINT trial and AHA/ASA 2018 updates (n = 653 883)c | Before AHA/ASA 2019 updates (n = 302 818)d | After AHA/ASA 2019 updates (n = 141 251)e | |
| Age, median (IQR), y | 68 (58-79) | 68 (58-79) | 68 (58-78) | 68 (59-78) | 68 (59-78) |
| Sex | |||||
| Women | 52 599 (49.3) | 37 584 (49.2) | 320 123 (49.0) | 145 954 (48.2) | 68 410 (48.4) |
| Men | 54 126 (50.7) | 38 773 (50.8) | 333 760 (51.0) | 156 864 (51.8) | 72 841 (51.6) |
| Race and ethnicity | |||||
| Asian | 3141 (2.9) | 2239 (2.9) | 20 142 (3.1) | 9922 (3.3) | 4511 (3.2) |
| Hispanic | 7556 (7.1) | 5488 (7.2) | 50 459 (7.7) | 25 493 (8.4) | 11 936 (8.5) |
| Non-Hispanic Black | 21 793 (20.4) | 15 963 (20.9) | 137 005 (21.0) | 62 977 (20.8) | 29 154 (20.6) |
| Non-Hispanic White | 70 404 (66.0) | 49 901 (65.4) | 419 133 (64.1) | 191 791 (63.3) | 89 661 (63.5) |
| Otherf | 3831 (3.6) | 2766 (3.6) | 27 144 (4.2) | 12 635 (4.2) | 5989 (4.2) |
| Insuranceg | |||||
| Private | 40 368/91 382 (44.2) | 28 998/66 310 (43.7) | 244 972/546 047 (44.9) | 112 494/261 213 (43.1) | 46 274/120 963 (38.3) |
| Medicare | 32 596/91 382 (35.7) | 23 878/66 310 (36.0) | 196 529/546 047 (36.0) | 97 786/261 213 (37.4) | 49 327/120 963 (40.8) |
| Medicaid | 10 606/91 382 (11.6) | 7808/66 310 (11.8) | 72 523/546 047 (13.3) | 35 938/261 213 (13.8) | 17 669/120 963 (14.6) |
| Self-pay | 7812/91 382 (8.5) | 5626/66 310 (8.5) | 32 023/546 047 (5.9) | 14 995/261 213 (5.7) | 7693/120 963 (6.4) |
| NIHSS score, median (IQR)h | 2 (1-5) | 2 (1-5) | 2 (1-5) | 2 (1-5) | 2 (1-5) |
| Medical history | |||||
| Stroke | 26 217 (24.6) | 19 131 (25.1) | 165 006 (25.2) | 75 713 (25.0) | 34 537 (24.5) |
| Transient ischemic attack | 9136 (8.6) | 6686 (8.8) | 53 968 (8.3) | 23 613 (7.8) | 10 682 (7.6) |
| CAD or MI | 22 980 (21.5) | 16 381 (21.5) | 131 960 (20.2) | 57 392 (19.0) | 26 075 (18.5) |
| Carotid stenosis | 3999 (3.7) | 2969 (3.9) | 22 864 (3.5) | 10 290 (3.4) | 5120 (3.6) |
| Diabetes | 39 152 (36.7) | 28 516 (37.3) | 252 683 (38.6) | 118 513 (39.1) | 55 162 (39.1) |
| Peripheral vascular disease | 4446 (4.2) | 3199 (4.2) | 25 245 (3.9) | 10 725 (3.5) | 4860 (3.4) |
| Hypertension | 81 745 (76.6) | 58 743 (76.9) | 502 382 (76.8) | 233 130 (77.0) | 108 926 (77.1) |
| Smoking status | 24 103 (22.6) | 17 046 (22.3) | 145 187 (22.2) | 67 681 (22.4) | 31 365 (22.2) |
| Dyslipidemia | 48 429 (45.4) | 35 469 (46.5) | 303 687 (46.4) | 144 846 (47.8) | 69 710 (49.4) |
| Heart failure | 5424 (5.1) | 4001 (5.2) | 35 636 (5.4) | 17 369 (5.7) | 8304 (5.9) |
| Chronic renal insufficiency | 5846 (5.5) | 4934 (6.5) | 50 995 (7.8) | 27 197 (9.0) | 13 889 (9.8) |
| Antiplatelet treatment before admission | |||||
| Aspirin monotherapy | 35 095 (32.9) | 25 564 (33.5) | 221 020 (33.8) | 100 159 (33.1) | 43 636 (30.9) |
| Clopidogrel monotherapy | 5588 (5.2) | 4201 (5.5) | 32 520 (5.0) | 13 433 (4.4) | 6029 (4.3) |
| DAPT of aspirin and clopidogrel | 6284 (5.9) | 4951 (6.5) | 47 858 (7.3) | 23 911 (7.9) | 11 633 (8.2) |
| Aspirin and dipyridamole | 1491 (1.4) | 932 (1.2) | 4510 (0.7) | 1117 (0.4) | 360 (0.3) |
| Other antiplatelet or combination | 488 (0.5) | 378 (0.5) | 3571 (0.5) | 1925 (0.6) | 1118 (0.8) |
| Antiplatelet type unknown | 21 (0) | 12 (0) | 86 (0) | 45 (0) | 17 (0) |
| Antiplatelet treatment at discharge | |||||
| Aspirin monotherapy | 60 961 (57.1) | 42 666 (55.9) | 369 514 (56.5) | 158 179 (52.2) | 66 537 (47.1) |
| Clopidogrel monotherapy | 18 430 (17.3) | 12 095 (15.8) | 88 271 (13.5) | 29 151 (9.6) | 10 388 (7.4) |
| DAPT of aspirin and clopidogrel | 20 662 (19.4) | 17 609 (23.1) | 180 514 (27.6) | 112 550 (37.2) | 63 480 (44.9) |
| Aspirin and dipyridamole | 5192 (4.9) | 3130 (4.1) | 11 935 (1.8) | 2112 (0.7) | 579 (0.4) |
| Other antiplatelet agents or combination | 1480 (1.4) | 857 (1.1) | 3649 (0.6) | 826 (0.3) | 267 (0.2) |
| Hospital characteristics | |||||
| No. of beds, median (IQR) | 368 (238-552) | 369 (239-554) | 365 (235-552) | 352 (225-540) | 348 (221-532) |
| Academic center | 82 179 (77.0) | 58 852 (77.1) | 494 999 (75.7) | 223 884 (73.9) | 103 133 (73.0) |
| Stroke center certification | |||||
| Primary stroke center | 26 383 (24.7) | 19 220 (25.2) | 160 510 (24.5) | 69 956 (23.1) | 31 360 (22.2) |
| Comprehensive stroke center | 59 845 (56.1) | 42 458 (55.6) | 359 725 (55.0) | 165 597 (54.7) | 77 825 (55.1) |
| Annual ischemic stroke case volume, median (IQR) | 257 (176-400) | 257 (176-401) | 258 (176-400) | 257 (172-393) | 254 (171-386) |
| Hospital region | |||||
| Northeast | 25 893 (24.3) | 19 099 (25.0) | 147 460 (22.6) | 61 547 (20.3) | 27 372 (19.4) |
| Midwest | 21 537 (20.2) | 15 153 (19.8) | 129 498 (19.8) | 62 251 (20.6) | 29 163 (20.6) |
| South | 40 233 (37.7) | 29 126 (38.1) | 267 081 (40.8) | 126 042 (41.6) | 59 744 (42.3) |
| West | 19 062 (17.9) | 12 979 (17.0) | 109 844 (16.8) | 52 978 (17.5) | 24 972 (17.7) |
| Rural hospital | 3961 (3.7) | 2785 (3.6) | 25 512 (3.9) | 14 588 (4.8) | 7319 (5.2) |
Abbreviations: AHA/ASA, American Heart Association and American Stroke Association; CAD, coronary artery disease; DAPT, dual antiplatelet therapy; MI, myocardial infarction; NIHSS, National Institutes of Health Stroke Scale.
Class of recommendations III, level of evidence A, October 2012 to July 2013.
Class of recommendations III, level of evidence A, August 2013 to February 2014.
Class of recommendations IIb, level of evidence B, March 2014 to February 2018.
Class of recommendations IIa, level of evidence B-R, March 2018 to September 2019.
Class of recommendations I, level of evidence A, October 2019 to June 2020.
Other included the following races and ethnicities: American Indian or Alaska Native, Native Hawaiian or Pacific Islander, or unable to determined.
The denominators in this section are different because of missing values in insurance status.
Data for NIHSS scores were missing for 25 112 (23.5%), 14 813 (19.4%), 80 541 (12.3%), 22 185 (7.3%), and 8434 (6.0%) patients, respectively.
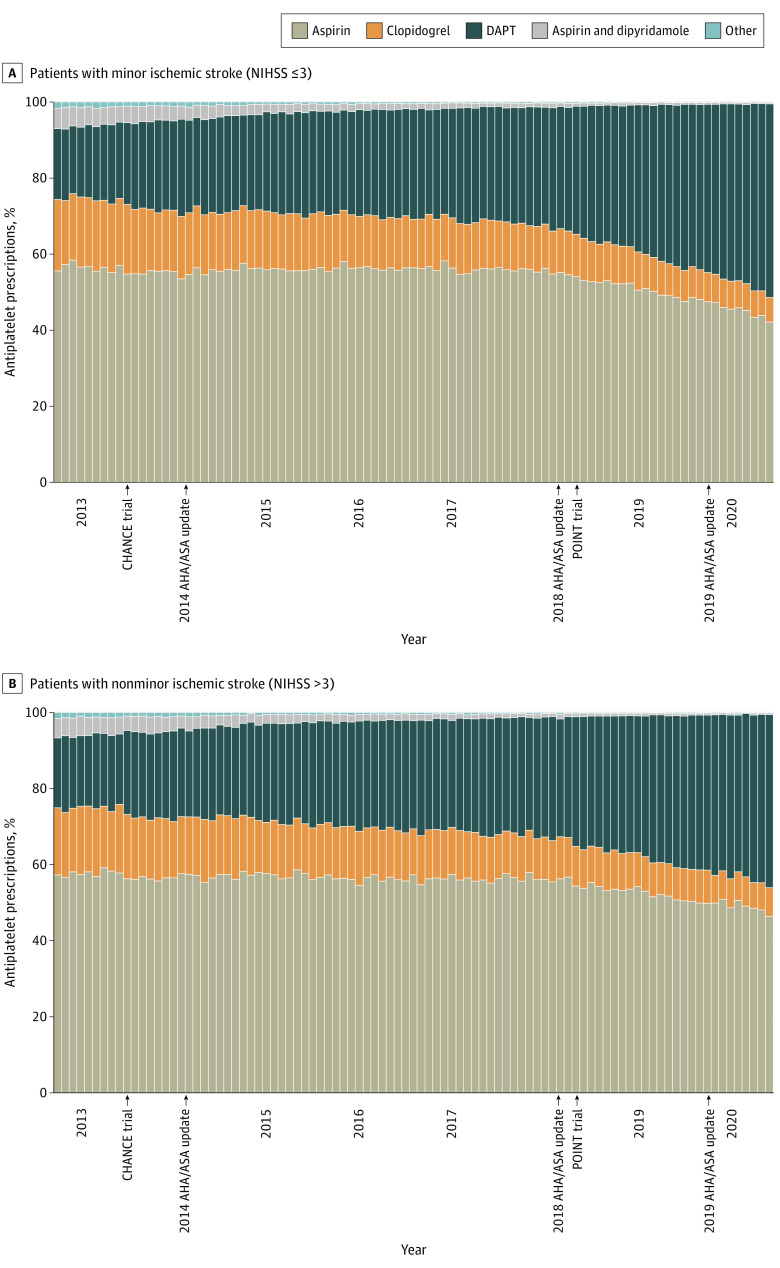
Use of DAPT gradually increased from 19.4% in the period before the CHANCE trial to 23.1% before the 2014 AHA/ASA guideline updates, 27.6% before the POINT trial and the 2018 AHA/ASA guideline updates, 37.2% before the 2019 AHA/ASA guideline updates, and 44.9% after the 2019 AHA/ASA guideline updates (P < .001) (Table). Although DAPT is indicated only for minor strokes with an NIHSS score of 3 or less, increases in use were observed over the same period for minor strokes (19.5%, 23.6%, 28.1%, 38.3%, and 47.0%, respectively; P < .001) and nonminor strokes with an NIHSS score higher than 3 (19.4%, 22.8%, 28.0%, 36.5%, and 42.6%, respectively; P < .001) (Figure). After the 2019 AHA/ASA guideline updates, 47.0% (95% CI, 46.7%-47.3%) of patients with minor strokes received DAPT, and 53.0% (95% CI, 52.7%-53.4%) did not receive DAPT, suggesting potential underuse of DAPT. By contrast, 42.6% (95% CI, 42.1%-43.0%) of patients with nonminor ischemic stroke (NIHSS score: median [IQR], 6 [5-9]) were prescribed DAPT at discharge, suggesting potential overuse of DAPT.
Figure. Patterns in Antiplatelet Prescriptions at Hospital Discharge.
AHA/ASA indicates American Heart Association and American Stroke Association; DAPT, dual antiplatelet therapy; NIHSS, National Institutes of Health Stroke Scale.
Discussion
Increased adoption of DAPT for secondary prevention in ischemic stroke was observed after publication of 2 pivotal trials and serial AHA/ASA guideline updates. This increase was observed in both minor ischemic strokes, for which guidelines recommended DAPT use, and in nonminor ischemic strokes, for which the risk-benefit ratio of DAPT has not been fully established. However, even after the release of the class I, level of evidence A recommendation, 53.0% of patients with minor ischemic strokes did not receive DAPT.
This study has limitations, including a lack of documented reasons for prescribing or not prescribing DAPT, the timing of the initiation, the duration of antiplatelet treatment, the generalizability to patients treated at nonregistry hospitals or in other countries, and the lack of information on prescribing trends after June 2020. Nonetheless, these study findings suggest an important opportunity to improve adherence to evidence-based antiplatelet therapy for secondary prevention in patients with acute ischemic stroke.
eFigure. Study Population.
References
- 1.Wang Y, Wang Y, Zhao X, et al. ; CHANCE Investigators . Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369(1):11-19. doi: 10.1056/NEJMoa1215340 [DOI] [PubMed] [Google Scholar]
- 2.Johnston SC, Easton JD, Farrant M, et al. ; Clinical Research Collaboration, Neurological Emergencies Treatment Trials Network, and the POINT Investigators . Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med. 2018;379(3):215-225. doi: 10.1056/NEJMoa1800410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Furie KL, Kasner SE, Adams RJ, et al. ; American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research . Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42(1):227-276. doi: 10.1161/STR.0b013e3181f7d043 [DOI] [PubMed] [Google Scholar]
- 4.Kernan WN, Ovbiagele B, Black HR, et al. ; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease . Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160-2236. doi: 10.1161/STR.0000000000000024 [DOI] [PubMed] [Google Scholar]
- 5.Powers WJ, Rabinstein AA, Ackerson T, et al. ; American Heart Association Stroke Council . 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110. doi: 10.1161/STR.0000000000000158 [DOI] [PubMed] [Google Scholar]
- 6.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi: 10.1161/STR.0000000000000211 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Study Population.